Abstract
Background
Little is known about the relationship between self-care in heart failure (HF) and outcomes like health status. The purpose of this study was to describe the relationship between HF self-care and Short Form-36 (SF-36) health status domains.
Methods and Results
A secondary analysis of cross-sectional data collected on 400 HF patients living in southern Thailand was completed using bivariate comparisons and hierarchical multiple regression modeling. Thai population norm-based SF-36 scores and Self-Care of Heart Failure Index (SCHFI) scores were used in the analysis. The sample was in older adulthood (65.7 ± 13.8 years), a slight majority of subjects were male (52%); the majority of subjects (62 %) had class III or IV HF. Each health domain was low in this sample compared to the general population. SCHFI maintenance and confidence scores were correlated significantly with each health status domain. SCHFI scores explained a significant amount of variance all domains, both in bivariate and multivariate models, except social functioning. In multivariate models, higher levels of self-care were associated with better health in certain domains, but only when both SCFHI management and confidence were high.
Conclusion
Improving HF self-care may be a mechanism through which future interventions can improve health in this population.
Keywords: heart failure, self-care, adherence, health status, self-management, SF-36
Introduction
Heart failure (HF) is a syndrome that has significant influence on the health of persons worldwide.(1) In Thailand, the incidence of death from HF increased by almost 280% between 1993 and 1998 alone.(2, 3) Health status domains (i.e. general health, physical functioning, role limitations due to physical or emotional problems, social functioning, bodily pain, vitality and mental health) are not only important subjective outcomes in HF, but are also significant predictors of other health outcomes in this population. As an example, there is evidence that the risk of death and re-hospitalization for HF are higher in patients with below average scores on certain Medical Outcomes Study Short Form-36 (SF-36) subscales.(4) Further, HF-specific indices of health status have been associated significantly with cardiovascular mortality, HF re-hospitalization,(5–7) and all-cause mortality.(6)
It is a commonly held view that self-care (treatment adherence and symptom management) can influence significantly health status and other health outcomes in persons with HF. Despite the fact that teaching and fostering effective self-care practices is a fundamental nursing practice, the scientific basis for the claim that self-care can influence HF health outcomes is quite limited. Accordingly, the purpose of this study is to describe the relationship between HF self-care and health status as measured by the SF-36. We hypothesized that persons who were more engaged in HF self-care would also report better health in each of the eight health status domains.
Methods
To test our hypothesis, we completed a secondary analysis of cross-sectional data collected during a previous study.(8) In that study, we tested the causal relationships among the components of sociodemographics, illness characteristics, HF self-care, and overall health status in patients with HF using raw SF-36 scores. The influence of HF self-care on each health status domain, however, was not assessed. Additionally, since our original investigation health status norms for Thailand have been published, which allowed for transformation of raw SF-36 domain scores to population norm-based scores: the recommended form for a robust analysis.(9) Accordingly, Thai population norm-based SF-36 domain scores were used in this analysis. Data were originally collected in 2006, after approval was obtained from the board of ethical review and/or the directors of six target hospitals in southern Thailand. The investigation conforms to the principles outlined in the Declaration of Helsinki.
Sample
The target population was Thai patients diagnosed with HF at least four weeks prior to the date of data collection, based on clinical symptoms, quantification of left ventricular ejection fraction or both. HF patients, who experience HF symptoms during the past four weeks, were 18 years of age or older, and able to comprehend the Thai language were included in the study. Informed consent was obtained from all study subjects. All subjects were assured of confidentially and the freedom to withdraw from participation at any time.
Measurement
Sociodemographics were measured using an investigator designed-instrument. Clinical characteristics, including duration of illness in months and prescribed pharmacological agents were extracted from the patient’s medical record. Severity of illness was measured using clinician-rated New York Heart Association (NYHA) functional class obtained through chart review. Comorbid conditions were assessed with the interview format of the widely-used 17-item Charlson Comorbidity Index.(10) A list of 17 comorbid diseases was evaluated with the possible score ranging from 0 to 30. Charlson Comorbidity Index scoring generated from self-report has similar predictive value as scores generated from administrative data.(11)
Self-care was measured with the Self-Care of Heart Failure Index (SCHFI) (12) Thai version. The SCHFI captures the following components of self-care: (a) maintenance or adherence behaviors that maintain physiologic homeostasis and prevent an acute exacerbation of HF (e.g., daily weighing); (b) the patient’s ability to recognize symptoms when they occur; (c) independent and interdependent self-care treatments implemented by the patient (e.g., take an extra diuretic for shortness of breath); (d) ability to evaluate the effectiveness of the treatments implemented; and (e) confidence in the ability to perform self-care. The SCHFI contains 15 items measured on a four-point Likert scale, which form three scales: self-care maintenance (adherence behaviors), self-care management (symptom evaluation, treatment, and treatment evaluation behaviors), and self-care confidence. Items measuring self-care confidence address the patient’s perceived ability to engage in each phase of self-care management (recognize symptoms, evaluate symptoms, treat symptoms, and evaluate effectiveness of symptom treatments). Scores on each of the SCHFI scales range from 0–100, with higher scores indicating better self-care.
In the parent study, the SCHFI was translated into the Thai language and back translated into English in a process guided by the methods of Brislin.(13) Decentering and techniques of back translation were used to ensure a culturally equivalent version in the Thai language. Items with discrepancies between the English and Thai versions were modified and back translated again until translators agreed that the Thai version of the SCHFI conveyed the same meaning as the original. In the parent study, reliability of the SCHFI (Thai version) was 0.85. Cronbach’s alpha ranged from 0.63 (maintenance) to 0.91 (confidence) on the three SCHFI scales.
Health status was measured using a general health status measure: the SF-36v2 (Thai version).(14, 15) The SF-36 is a multi-purpose, short-form health survey containing 36 items that are aggregated into eight scales of 2–10 items each. The subscales reflect physical functioning, role limitations due to physical health (role-physical), bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems (role-emotional), and general mental health. The score for each scale was transforming to a scale ranging from 0–100, with a higher score indicating better health. In the parent study, the reliability of the SF-36 (Thai version) was 0.94. For the eight subscales, Cronbach’s alpha ranged from 0.70 (social functioning) to 0.93 (physical functioning).
Statistical Analysis
For this analysis, raw SF-36 health status domain scores were population norm-based transformed. This first involved computing z-scores for each raw SF-36 domain score. Then, scores were converted to norm-based (mean of 50, standard deviation of 10) scores.(9) Healthy Thai patient SF-36 data were abstracted from a recent published assessment of the health of 1,345 persons living in Thailand collected in 2005.(16) Thai population norm-based data on this sample of patients with HF were compared to the healthy population using student’s t-tests.
Bivariate comparisons between SCHFI scale scores and population norm-based health status domains scores were made using Pearson product-moment correlation coefficients and t-tests, without assuming equal variance, comparing patients with self-care scale scores above and below the sample mean. In addition, we compared health status domain scores between patients reporting adequate levels of HF self-care (SCHFI scale scores of ≥ 70 (out of 100))(17) using t-tests without assuming equal variance. This final bivariate comparison was used to determine if patients who reported adequate self-care had better health in each domain.
Linear regression modeling was used to determine how much variance in population norm-based health status domains was explained by SCHFI scale scores. Hierarchical multiple linear regression modeling was used to determine the influence of patient demographics, including self-reported age, gender, years of education and employment status, and comorbidity score in the first block of each model. Education had a direct effect on health status in the parent study.(8) Employment was identified as an important factor in the analysis of health status in a previous study of persons with HF.(18) The influence of HF illness characteristic (HF duration in months, NYHA functional class, and HF etiology) and treatment characteristics (the prescription of diuretics, angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARB), and β-aderenergic blockers (BB)) were taken into account in the second block of each model. Finally, the impact of the three SCHFI sub-scale scores was taken into account in the last block of the model. Our previous work provided evidence of a moderating effect between self-care confidence and self-care management on a different health outcome: HF inpatient costs.(19) For that reason, we also tested the moderating effect of self-care confidence on the relationship between HF self-care management and health status in the final step of each model. The significance of change in explained variance between blocks was evaluated using calculated F-statistics as well as the calculated change in F-statistic (F change). The significance of individual characteristics was evaluated by calculating slope coefficients, 95% confidence intervals and P-values. Post-hoc effect sizes were calculated using Cohen’s f2: . All analyses were performed using SPSS version 15.0 (Chicago, IL). Statistical significance was predetermined at P <.05.
Results
The sample (n = 400) was elderly, the slight majority was male, and most patients had a limited education and were currently unemployed (Table 1). The average duration of HF was just over two years, the majority of patients had NYHA class III or IV HF, and a slight majority had ischemic HF. Most subjects were prescribed diuretics, and ACE inhibitors or ARBs, while few were prescribed BBs. Overall, levels of self-care were low, with an average of each subscale score below 56 out of 100.
Table 1.
Thai Sample Demographics, Heart Failure and Treatment Characteristics, Heart Failure Self-Care, and Health Status (N = 400)
SCHFI scale scores range from 0–100 with higher values indicating better self-care. SD = standard deviation, SCHFI = Self-Care of Heart Failure Index, SF-36 = Medical Outcomes Short Form 36v2, NYHA = New York Heart Association, ACE = angiotensin converting enzyme, ARB = angiotensin receptor blocker.
| Patient Demographics | Mean (± SD) or n (%) |
|---|---|
| Age in Years | 64.73 (± 13.83) |
| Female | 192 (48.0%) |
| Education in Years | 4.75 (± 3.45) |
| Currently Employed | 104 (26.0%) |
| Charlson Comorbidity Category: | |
| Low (score of 1 to 2) | 102 (25.5%) |
| Medium (score of 3 or 4) | 208 (52.0%) |
| High (score of 5 or more) | 90 (22.5%) |
|
| |
| Heart Failure Illness and Treatment Characteristics | |
|
| |
| Duration of Heart Failure in Months | 26.89 (± 34.00) |
| NYHA functional class: | |
| I-II | 152 (38.0%) |
| III | 133 (33.3%) |
| IV | 115 (28.7%) |
| Heart failure etiology: | |
| Ischemic | 220 (55.0%) |
| Known, Non-Ischemic | 113 (28.2%) |
| Idiopathic | 67 (16.8%) |
| Prescribed diuretic | 277 (69.3%) |
| Prescribed ACE inhibitor or ARB | 238 (59.5%) |
| Prescribed Beta blocker | 97 (24.3%) |
|
| |
| Heart Failure Self-Care | |
|
| |
| SCHFI Maintenance | 55.80 (± 15.81) |
| SCHFI Management | 40.63 (± 16.30) |
| SCHFI Confidence | 49.30 (± 21.40) |
| Adequate (≥70) SCHFI Maintenance | 85 (21.3%) |
| Adequate (≥70) SCHFI Management | 20 (5.0%) |
| Adequate (≥70) SCHFI Confidence | 70 (17.5%) |
| Health Status | |
| Thai Population Norm-Based SF-36 | |
| Health Status Domains | |
| General Health | 37.44 (± 10.38) |
| Physical Functioning | 34.45 (± 11.72) |
| Role-Physical | 27.29 (± 13.26) |
| Role-Emotional | 30.34 (± 20.36) |
| Social Functioning | 36.94 (± 13.09) |
| Bodily Pain | 45.82 (± 12.12) |
| Vitality | 45.05 (± 12.33) |
| Mental Health | 40.54 (± 12.93) |
Heart Failure Self-Care and Health Status Domains
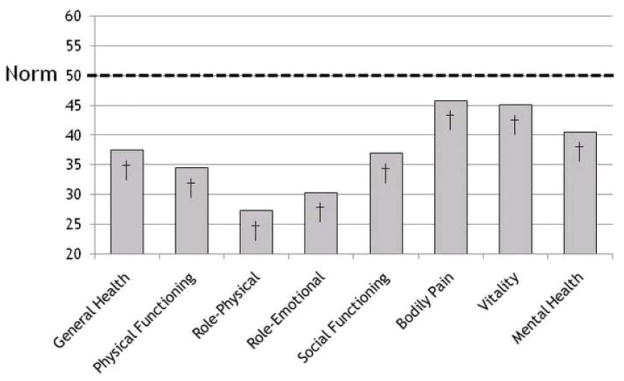
In this sample, HF had a significant influence on each of the eight SF-36 health domains compared to the healthy population in Thailand (Figure 1).
Figure 1.
The Influence of Heart Failure on Health Status in the Thai population.
Higher scores on each Thai population norm-based SF-36 domain indicate better health; the Thai population norm = 50. Thus, Thai patients with heart failure have significantly reduced health status in each domain compared to the general Thai population. We hypothesized that better self-care was associated with better health status in this population. That is, improving heart failure self-care may be one way of improving health status in the Thai and other heart failure populations. † P-value <.0001 compared to the Thai population norm (mean of 50, standard deviation of 10).
Self-care maintenance was correlated with each of the eight population norm-based health status domains (r =.156 to.427, all P<0.01). The strongest correlation was between self-care maintenance and the vitality domain. In contrast, self-care management was only correlated with the general health, physical functioning, role-physical, social functioning, and vitality domains (r =.099 to.167, all P<0.05); the strongest correlation being that between self-care management and physical functioning. Self-care confidence was also correlated with each of the eight health status domains (r =.108 to.336, all P<0.05), the strongest correlation being between self-care confidence and mental health. All correlations between measures of self-care and health status were positive, indicating that higher levels of self-care are generally associated with better health.
Patients who reported better than average self-care maintenance scored significantly better in each health status domain, save the role-emotional domain (Table 2), compared to those who reported self-care maintenance below the sample mean. Patients who reported better than average self-care management had better scores only in physical functioning compared to patients who reported self-care management below the sample mean. Patients who reported better self-care confidence had higher scores in all but two health status domains, compared to patients who reported self-care confidence below the sample mean.
Table 2.
Mean Differences in Thai Population Norm-Based SF-36 Health Status Domain Scores Comparing Above Below Average Heart Failure Self-Care
Values shown are the mean difference and 95% confidence intervals comparing Thai population norm-based domain scores between patients who reported above average heart failure self-care to those who reported below average self-care. CI = confidence interval of the mean difference in health status domain score, Mean = mean difference in health status domain score, SCHFI = Self-Care of Heart Failure Index, SF-36 = Medical Outcomes Short Form 36v2.
| Mean(95%CI) Difference in Norm-Based SF-36 Scores |
|||
|---|---|---|---|
| SCHFI Scale Mean Cut-off | Maintenance (≥55.8 vs.<55.8) | Management (≥40.6 vs.<40.6) | Confidence (≥49.3 vs.<49.3) |
| General Health | 4.10(2.07–6.12)** | −0.10(−2.14–1.95) | 3.76(1.76–5.75)** |
| Physical Functioning | 6.33(4.10–8.56)** | 2.39(0.08–4.69)* | 3.91(1.64–6.20)** |
| Role Physical | 4.09(1.46–6.74)** | 0.25(−2.36–2.87) | 1.63(−0.96–4.23) |
| Role Emotional | 2.56(−1.51–6.22) | −2.22(−6.23–1.78) | 2.59(−1.40–6.59) |
| Social Functioning | 5.58(3.09–8.07)** | 2.14(−0.45–4.73) | 4.49(1.96–7.03)** |
| Bodily Pain | 3.80(1.46–6.14)** | −0.35(−2.75–2.05) | 3.53(1.17–5.89)** |
| Vitality | 7.31(4.97–9.65)** | 0.69(−1.74–3.12) | 6.87(4.55–9.19)** |
| Mental Health | 3.91(1.37–6.44)** | −2.28(−4.81–0.25) | 7.52(5.01–9.94)** |
P-value <.05
P-value <.01.
Using the standard cut-point of adequate self-care maintenance (score of 70 out of 100), patients who reported adequate levels of self-care maintenance had significantly higher scores in each domain compared to patients who did not report self-care maintenance at an adequate level (Table 3). Patients who reported adequate levels of self-care management had significantly higher scores in five of the eight health status domains. Patients with adequate confidence in self-care had better scores in each health status domain.
Table 3.
Mean Differences in Thai Population Norm-Based SF-36 Health Status Domain Scores Comparing Adequate and Inadequate Heart Failure Self-Care
Values shown are the mean difference and 95% confidence intervals comparing population norm-based domain scores between patients who reported adequate heart failure self-care to those who reported inadequate heart failure self-care. Self-Care of Heart Failure Index (Thai version) scale score of ≥ 70 were used to differentiate adequate from inadequate self-care. CI = confidence interval of the mean difference in health status domain score, Mean = mean difference in health status domain score, SCHFI = Self-Care of Heart Failure Index, SF-36 = Medical Outcomes Short Form 36v2.
| Mean (95%CI) Difference in Norm-Based SF-36 Scores |
|||
|---|---|---|---|
| SCHFI Scale | Maintenance | Management | Confidence |
| General Health | 7.32(4.76–9.89)** | 7.91(1.73–14.08)* | 5.04(1.96–8.13)** |
| Physical Functioning | 8.02(5.37–10.67)** | 4.51(−2.20–11.23) | 5.29(2.13–8.44)** |
| Role Physical | 6.36(2.91–9.82)** | 8.43(1.26–15.60)* | 4.79(0.94–8.64)* |
| Role Emotional | 7.58(2.69–12.46)** | 7.24(−3.37–17.86) | 8.88(3.51–14.24)** |
| Social Functioning | 6.70(3.66–9.74)** | 7.75(1.33–14.18)* | 5.15(1.56–8.73)** |
| Bodily Pain | 5.46(2.63–8.29)** | 0.47(−4.20–5.15) | 6.03(2.9–9.14)** |
| Vitality | 10.72(7.84–13.59)** | 12.67(6.30–19.04)** | 7.80(4.35–11.25)** |
| Mental Health | 7.32(4.13–10.51)** | 11.74(4.91–18.58)** | 9.04(5.53–12.54)** |
P-value <.05
P-value <.01.
Without controlling for confounding factors, measures of HF self-care explained a significant amount of variance in each health domain (Table 4). Adding measures of self-care to the multivariate models also added a significant amount of explained variance in all health status domains except social-functioning.
Table 4.
The Influence of Heart Failure Self-Care on Thai Population Norm-Based Health Status Domains. Standardized Coefficients, Variance and Effect Size
Measures of heart failure self-care were significant in explaining variance in all health status domains. The effect of adding measures of self-care to multivariate models ranged from small to large. Better self-care was associated with better health in several domains only when confidence in self-care was also high. All values controlling for age, gender, education in years, employment, comorbidities, heart failure duration and etiology, New York Heart Association functional class, ACE or ARB, Beta blocker, and/or diuretic. Effect sizes are the effect of adding measures of self-care to the multivariate model. ACE = angiotensin converting enzyme, ARB = angiotensin receptor blocker, HF = heart failure, Mgt × Con = moderating effect of confidence on the relationship between self-care management and health status, SC = Self-Care as measured by the Self-Care of Heart Failure Index, SF-36= short form-36v2.
| SF-36 Health Status Domain |
||||||||
|---|---|---|---|---|---|---|---|---|
| Standardized Coefficients | General Health | Physical Functioning | Role-Physical | Role-Emotional | Social Functioning | Bodily Pain | Vitality | Mental Health |
| SC Maintenance Total | .232 | .219 | .195 | .263 | .185 | |||
| SC Management Total | −.358 | −.308 | −.347 | −.578 | ||||
| SC Confidence Total | −.251 | −.315 | −.264 | −.134 | ||||
| SC Mgt × Con (Interaction) | .713 | .506 | .610 | .694 | ||||
|
| ||||||||
| Explained Variance (R2) | ||||||||
|
|
||||||||
| Model | .334* | .574* | .427* | .348* | .339* | .259* | .481* | .350* |
| Measures of Self-Care Without Adjustment | .142* | .141* | .071* | .043* | .103* | .081* | .222* | .182* |
| Measures of Self-Care Adjusted for Covariates | .085* | .040* | .052* | .047* | .026 | .078* | .106* | .109* |
|
| ||||||||
| Effect Size (Cohen’s f2) | .128 | .094 | .092 | .072 | .039 | .105 | .204 | .168 |
P-value <.05.
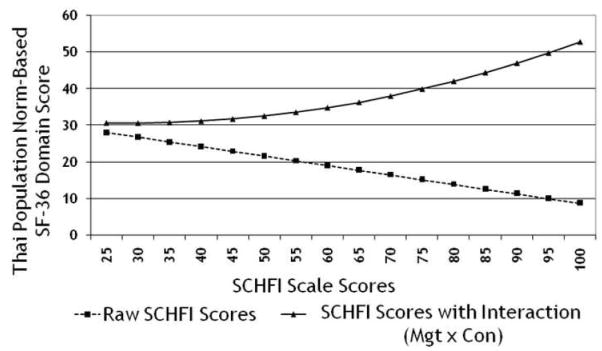
Considering the health status domains of general health, role-physical, vitality, and mental health, the moderating effect of self-care confidence on the relationship between self-care management was the strongest in the model (βs ranging from.506 to.713). Because the strength and direction of the relationship between self-care management and health status domain was changed by level of self-care confidence, higher levels of self-care were associated with better health in these domains only when both self-care management and self-care confidence were high (Figure 2).
Figure 2.
How Self-Care Confidence Moderates the Relationship Between Heart Failure Self-Care Management and The Role-Physical Health Status Domain
If the influence of raw scores were interpreted, one could conclude that persons who are more engaged in self-care have poorer heath status. When the moderating effect (interaction) of self-care confidence on the relationship between self-care management and health status is taken into consideration, however, it appears that higher levels of self-care are associated with better health status, but only when self-care confidence is also high. Mgt × Con = moderating interaction between self-care management and self-care confidence. SF-36 = Medical Outcomes Study Short Form 36, SCHFI = Self-Care of Heart Failure Index.
Discussion
Our most significant findings are that 1) HF has a significant influence on each health domain in the Thai population, 2) higher levels of self-care maintenance and confidence in self-care are correlated with better health, while better self-care management is associated with better health in a few domains, 3) self-care explains a significant amount of variance in each health status domain, with the exception of social functioning, even when the influence of common confounders are controlled, and 4) confidence changes the strength and direction of the relationship between self-care management and several health status domains.
Health status domains in this sample were significantly lower than the general population. These data confirm the result of studies in different populations that also indicated that HF impacts significantly each health status domain.(18, 20) Although health status was generally poor in this population, we have provided evidence that patients who report better HF self-care also report better health. Rodríguez-Artalejo and colleagues(4) recently reported that SF-36 scale scores above the sample median were associated significantly with a decreased adjusted risk of re-hospitalization and death in persons with HF. In this study, we have provided evidence that above average self-care maintenance and confidence were associated significantly with better health in each domain. Thus, patients with HF who practice above average self-care maintenance as well as those who are more confident in self-care have better health and also may be at less risk of re-hospitalization and death. Although it has been put forth that scores on SCHFI scales of 70 or greater indicate adequate self-care,(17) this cut-off of 70 has not undergone quantitative testing. In this study, however, adequate self-care maintenance and self-care confidence (using scores of 70 as cut-offs) were associated with markedly greater health in each of the eight domains. Therefore, the hypothesized cut-off of adequate self-care maintenance and self-care confidence was associated with clinically meaningful differences in health status in this sample.
The direct and linear relationship between self-care management (symptom recognition and management) was more complex. In sum, higher levels of self-care management were associated with better health in fewer domains than self-care maintenance and confidence, reporting above average self-care management did not come with markedly better health in most domains, and patients reporting adequate self-care management (i.e. SCHFI scores ≥ 70) also reported better self-care in only five health domains. In contrast, adequate self-care management helped differentiate average differences in vitality in mental health that approximated an improvement by one standard deviation in each population norm-based health scores. Thus, the relationship between self-care management and health status is quite variable, and most likely non-linear.
The results of our multivariate models reveal patterns that may help explain which aspects of health status HF self-care influences. First, indices of self-care did not hold individual significance in determining social functioning or role-emotional domains. In this sample, the social functioning domain had the lowest index of internal consistency, which may help explain our findings. Social functioning, the level of interference with social activities due to physical/emotional problems, and the role-emotional domain, problems with work or other activities due emotional problems,(14) just may not be aspects of health status that vary in parallel with HF self-care. As a related example, a clear relationship between HF self-care and another subjective outcome with an emotional and social component, quality of life, also has not been established.(21) Thus, factors other than self-care have greater import in explaining variance in role-emotional and social functioning.
The second emergent pattern was that self-care maintenance was the only index of self-care that was significant in explaining variance in physical functioning, and bodily pain. Simply put, that means the evaluation and management of HF symptoms and confidence in these self-care skills held little value in terms of explaining variance in these health status domains. It may be that controlling for NYHA functional class interfered with the interpretation of the relationship between self-care and physical functioning. Our full model explained less variance in bodily pain and the average bodily pain score most closely approximated healthy Thai population norms than any other health status domain, potentially indicating that this population of HF patients does not suffer greatly with pain. Moreover, based on the work of Godfrey and colleagues,(22, 23) it may be that pain is a barrier to effective HF self-care, limiting inferences that could be made about the direction of the relationship between self-care and pain in this population.
The third emergent pattern was that self-care management and the moderating effect of self-care confidence and the relationship between self-care management and health status domain held significance in explaining variance in general health, role-physical, vitality and mental health. It is in these domains that adding measures of self-care also had greater effect sizes. These results suggest that persons with confidence in every step of HF self-care management may be able to improve health status and potentially other health outcomes. Symptom misinterpretation, low confidence in the ability to ameliorate symptoms, and low confidence in preventing untoward outcomes are common in this population.(24, 25) Perhaps some key differences in the subgroup of patients with high confidence are confidence in their ability to assess the severity and urgency of specific HF symptoms, the ability to associate their symptoms with their chronic condition, and their confidence in the ability to both ameliorate symptoms when they occur and avoid severe exacerbations or hospitalization.
If the important moderating effect of self-care confidence on the relationship between self-care management and health status was not taken into account, we would be forced to conclude incorrectly that in this sample of HF patients higher levels of HF self-care were associated with worse health status. In contrast, when the net effect of HF self-care is taken into account, it becomes clear that higher levels of self-care were associated with higher levels of health in the domains of general health, role-physical, vitality, and mental health (Figure 2). We have previously reported a similar moderating effect of confidence on the relationship between HF self-care management and economic outcomes.(19) Our results are also similar to the work of Arnold et al.,(26) in that confidence in self-care behaviors played an important role in explaining health status in persons with HF. There is, however, one critical difference between our results and that of Arnold; the relationship between confidence and self-care management was important in our study but not that between confidence and maintenance behaviors. In our view, self-care maintenance behaviors do not require high levels of confidence. That is, little confidence is needed to follow prescribed therapy. In contrast, self-care management (those behaviors aimed to evaluate and ameliorate symptoms when they occur) requires active decision-making,(27) and can be influenced by varying degrees of confidence.
In summary, we can conclude that in this sample, higher levels of self-care were associated with better health in several domains. Thus, it is quite plausible that improving self-care in this population would also improve health. If this is also the case in other diverse populations remains an unanswered research question. These preliminary data support, however, the fundamental nursing practice of teaching and fostering self-care practices in persons with HF; a conclusion that may be reinforced by the results of ongoing and future research initiatives. The effects of adding measures of HF self-care care to multivariate models determining health were considered small to medium. Our results also indicate that the relationship between HF self-care and health may not be linear, and is likely influenced by other factors, including confidence in self-care.
Strengths and Limitations
There are several strengths and limitations to these data that need to be taken into consideration. First, these data were not collected to answer the research questions posed in this analysis. Second, the sample was ethnically homogeneous, potentially limiting inferences to larger and/or ethnically diverse populations. In fact, by using data from a Thai healthy population to compute population norm-based health status data, we have limited future comparisons to US population normed SF-36 data. Significant differences exist, however, between US population and Thai population SF-36 data. Thus, we view our choice of healthy patient data as a strength of this study. Third, the average age of patients in this sample was 12 years less than that of the sample in a related research report,(4) but similar to the age in many studies involving HF-specific health status indices.(5–7) The relatively young population studied in this analysis may, however, limit generalizability. Fourth, unlike other instruments that were not used in the study, the SF-36 health status measure is not HF-specific. Fifth, we used the historical cutoff value of 70 on the SCHFI scale scores to identify adequate engagement in HF self-care. Although this threshold of self-care was associated with a significant differences in health status, sample-specific methods to categorize self-care could have been implemented. Finally, we did not correct for multiple measures during our analysis of the SF-36 subscale scores. Thus, although the majority of our conclusions would meet the level of significance required for multiple measure inferences, some of our conclusions come with less confidence.
Conclusion
Our research findings provide evidence in support of the commonly held view that higher levels of self-care are associated with better outcomes in persons with HF. In this sample, higher levels of HF self-care were associated significantly with better health. When the influence of other confounders factors are taken into account, this condition is dependent on concurrent high levels of confidence in self-care. Due to the homogeneous nature of this sample and other limiting factors, follow-up studies are needed to determine the extent of the relationship between self-care and health outcomes in the HF population.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Christopher S. Lee, Lecturer, University of Pennsylvania School of Nursing, Philadelphia, USA.
Jom Suwanno, Walailak University School of Nursing, Nakhon Si Thammarat, Thailand.
Barbara Riegel, Professor, University of Pennsylvania School of Nursing, Philadelphia, USA.
References
- 1.Young JB. The global epidemiology of heart failure. Med Clin North Am. 2004 Sep;88(5):1135–43. ix. doi: 10.1016/j.mcna.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Ministry of Public Health. Division of Health Statistics, Health Report. Bangkok, Thailand: Ministry of Public Health of Thailand; 1997. [Google Scholar]
- 3.Chooprapawan J, Phoraphak-kham Y, Jirawatkul A, Phao-in W. A study of mortality causes in 5 provinces: Khon Khaen, Nakhon Si Thammarat, Nakhon Sawan, Nan, Ranong, and Bangkok. Bangkok, Thailand: Ministry of Public Health; 2000. [Google Scholar]
- 4.Rodriguez-Artalejo F, Guallar-Castillon P, Pascual CR, Otero CM, Montes AO, Garcia AN, et al. Health-related quality of life as a predictor of hospital readmission and death among patients with heart failure. Arch Intern Med. 2005 Jun 13;165(11):1274–9. doi: 10.1001/archinte.165.11.1274. [DOI] [PubMed] [Google Scholar]
- 5.Soto GE, Jones P, Weintraub WS, Krumholz HM, Spertus JA. Prognostic value of health status in patients with heart failure after acute myocardial infarction. Circulation. 2004 Aug 3;110(5):546–51. doi: 10.1161/01.CIR.0000136991.85540.A9. [DOI] [PubMed] [Google Scholar]
- 6.Kosiborod M, Soto GE, Jones PG, Krumholz HM, Weintraub WS, Deedwania P, et al. Identifying heart failure patients at high risk for near-term cardiovascular events with serial health status assessments. Circulation. 2007 Apr 17;115(15):1975–81. doi: 10.1161/CIRCULATIONAHA.106.670901. [DOI] [PubMed] [Google Scholar]
- 7.Heidenreich PA, Spertus JA, Jones PG, Weintraub WS, Rumsfeld JS, Rathore SS, et al. Health status identifies heart failure outpatients at risk for hospitalization or death. J Am Coll Cardiol. 2006 Feb 21;47(4):752–6. doi: 10.1016/j.jacc.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 8.Suwanno J, Petpichetchian W, Riegel B, Issaramalai SA. A model predicting health status of patients with heart failure. J Cardiovasc Nurs. 2009 Mar–Apr;24(2):118–26. doi: 10.1097/JCN.0b013e318197a75c. [DOI] [PubMed] [Google Scholar]
- 9.Ware JEKM, Dewey JE. How to score version 2 of the SF-36 Health Survey. Lincoln: Quality Metric Inc; 2000. [Google Scholar]
- 10.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 11.Chaudhry S, Jin L, Meltzer D. Use of a self-report-generated Charlson Comorbidity Index for predicting mortality. Med Care. 2005 Jun;43(6):607–15. doi: 10.1097/01.mlr.0000163658.65008.ec. [DOI] [PubMed] [Google Scholar]
- 12.Riegel B, Carlson B, Moser DK, Sebern M, Hicks FD, Roland V. Psychometric testing of the self-care of heart failure index. J Card Fail. 2004 Aug;10(4):350–60. doi: 10.1016/j.cardfail.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Brislin RW. Translation and content analysis of oral and written materials: Methodology. In: Triandis HC, Berry JW, editors. Handbook of cross-cultural psychology. Boston: Allyn & Bacon; 1980. pp. 389–444. [Google Scholar]
- 14.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–83. [PubMed] [Google Scholar]
- 15.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993 Mar;31(3):247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Lim LL, Seubsman SA, Sleigh A. Thai SF-36 health survey: tests of data quality, scaling assumptions, reliability and validity in healthy men and women. Health Qual Life Outcomes. 2008;6:52. doi: 10.1186/1477-7525-6-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riegel B, Dickson VV. A situation-specific theory of heart failure self-care. J Cardiovasc Nurs. 2008 May–Jun;23(3):190–6. doi: 10.1097/01.JCN.0000305091.35259.85. [DOI] [PubMed] [Google Scholar]
- 18.Juenger J, Schellberg D, Kraemer S, Haunstetter A, Zugck C, Herzog W, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart. 2002 Mar;87(3):235–41. doi: 10.1136/heart.87.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee C, Carlson B, Riegel B. Heart Failure Self-Care Improves Economic Outcomes, but Only When Self-Care Confidence is High. Journal of Cardiac Failure. 2007;13(6):S75. [Google Scholar]
- 20.Alonso J, Ferrer M, Gandek B, Ware JE, Jr, Aaronson NK, Mosconi P, et al. Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004 Mar;13(2):283–98. doi: 10.1023/b:qure.0000018472.46236.05. [DOI] [PubMed] [Google Scholar]
- 21.Grady KL. Self-care and quality of life outcomes in heart failure patients. J Cardiovasc Nurs. 2008 May-Jun;23(3):285–92. doi: 10.1097/01.JCN.0000305092.42882.ad. [DOI] [PubMed] [Google Scholar]
- 22.Godfrey C, Harrison MB, Medves J, Tranmer JE. The symptom of pain with heart failure: a systematic review. J Card Fail. 2006 May;12(4):307–13. doi: 10.1016/j.cardfail.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Godfrey CM, Harrison MB, Friedberg E, Medves JM, Tranmer JE. The symptom of pain in individuals recently hospitalized for heart failure. J Cardiovasc Nurs. 2007 Sep–Oct;22(5):368–74. doi: 10.1097/01.JCN.0000287035.77444.d9. discussion 6–7. [DOI] [PubMed] [Google Scholar]
- 24.Riegel B, Carlson B. Facilitators and barriers to heart failure self-care. Patient Educ Couns. 2002 Apr;46(4):287–95. doi: 10.1016/s0738-3991(01)00165-3. [DOI] [PubMed] [Google Scholar]
- 25.Horowitz CR, Rein SB, Leventhal H. A story of maladies, misconceptions and mishaps: effective management of heart failure. Soc Sci Med. 2004 Feb;58(3):631–43. doi: 10.1016/s0277-9536(03)00232-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arnold R, Ranchor AV, DeJongste MJ, Koeter GH, Ten Hacken NH, Aalbers R, et al. The relationship between self-efficacy and self-reported physical functioning in chronic obstructive pulmonary disease and chronic heart failure. Behav Med. 2005 Fall;31(3):107–15. doi: 10.3200/BMED.31.3.107-115. [DOI] [PubMed] [Google Scholar]
- 27.Dickson VV, Tkacs N, Riegel B. Cognitive influences on self-care decision making in persons with heart failure. Am Heart J. 2007 Sep;154(3):424–31. doi: 10.1016/j.ahj.2007.04.058. [DOI] [PubMed] [Google Scholar]