Abstract
Patients with minimal hepatic encephalopathy (MHE) have impaired driving skills, but association of MHE with motor vehicle crashes is unclear. Standard psychometric tests (SPT) or inhibitory control test (ICT) can be used to diagnose MHE. The aim was to determine the association of MHE with crashes and traffic violations over the preceding year and on 1-year follow-up. Cirrhotics were diagnosed with MHE by ICT (MHEICT) and SPT (MHESPT). Self and department-of-transportation (DOT)-reports were used to determine crashes and violations over the preceding year. Agreement between self and DOT-reports was analyzed. Patients then underwent 1 year follow-up for crash/violation occurrence. Crashes in those with/without MHEICT and MHESPT were compared. 167 cirrhotics had DOT-reports, of which 120 also had self-reports. A significantly higher proportion of MHEICT cirrhotics experienced crashes in the preceding year compared to those without MHE by self-report (17% vs. 0%, p=0.0004) and DOT-reports (17% vs. 3%, p=0.004, relative risk:5.77). SPT did not differentiate between those with/without crashes. A significantly higher proportion of patients with crashes had MHEICT compared to MHESPT, both self-reported (100% vs. 50%, p=0.03) and DOT-reported (89% vs. 44%, p=0.01). There was excellent agreement between self and DOT-reports for crashes and violations (Kappa 0.90 and 0.80). 109 patients were followed prospectively. MHEICT patients had a significantly higher future crashes/violations compared to those without (22% vs. 7%, p=0.03) but MHESPT did not. MHEICT (Odds ratio:4.51) and prior year crash/violation (Odds ratio:2.96) were significantly associated with future crash/violation occurrence.
Keywords: Driving, accidents, cirrhosis, hepatic encephalopathy, inhibitory control test
Minimal hepatic encephalopathy (MHE) is a prevalent neuro-cognitive complication of cirrhosis that is diagnosed in up to 80% of patients with cirrhosis. It is associated with increased progression to overt hepatic encephalopathy (OHE) and impaired driving skills(1–3). MHE patients have impaired attention, response inhibition, visuo-motor coordination and psychomotor speed(4). Paper-pencil standard psychometric tests (SPT) or the computerized inhibitory control test (ICT) can be used to diagnose MHE(5). The ICT is has been validated for the diagnosis of MHE and is highly correlated with driving simulator performance(6–9). On a driving test, MHE patients required significantly higher interventions to prevent an accident compared to cirrhotics without MHE(10). A recent report showed that MHE patients have a higher risk of motor vehicle crashes and traffic violations on an anonymous driving survey(11). However, since these were not corroborated by the Department of Transportation (DOT) and poor insight in MHE could be associated with under-reporting, a prospective study is required(12).
The hypotheses tested during this study were (a) MHE patients have a higher motor vehicle crash rate compared to those without MHE on DOT records within 1 year of psychometric testing (b) Patients impaired on ICT have a higher crash rate compared to patients impaired on SPT (c) MHE patients have a higher motor vehicle crash risk compared to those without on prospective follow-up over 1 year and (d) there will be a significant under-reporting in motor vehicle crashes in MHE patients. Patients with cirrhosis have a higher risk of mortality and adverse economic outcomes when they experience crashes; therefore their prevention is an important goal(13). The deleterious impact of motor vehicle crashes to society and the high prevalence of MHE in cirrhosis make this research question important from a tertiary as well as a public health perspective
METHODS
All cirrhotics included were between 18 to 65 years of age and were recruited from Medical College of Wisconsin and Virginia Commonwealth University Medical Center. Cirrhotics with recent alcohol use (<3 months), on OHE therapy, on psychoactive drugs (anti-psychotics/ anti-anxiety medications/interferon) and those who drove <20 miles/week were excluded. Written informed consent was obtained from all patients and the psychometric testing was performed at one sitting after the consent was signed.
Definition of MHE and psychometric testing
All cirrhotics enrolled were administered a battery of 4 tests (SPT): (a) Number Connection test-A (NCT-A), (b) Number Connection test –B (NCT-B), (c) Digit Symbol test (DST) and (d) Block Design test (BDT) along with the ICT(6, 7). NCT-A and NCT-B evaluate mental processing speed and attention. BDT evaluates visuo-spatial coordination and DST tests for processing speed. The ICT is a dynamic and demanding test which consists of response to lures and targets in a timed manner; a high lure and low target response is indicative of poor psychometric performance. ICT is available for free download at www.hecme.tv. Control values for the local population had been determined a priori from a sample of 200 controls who were age and education-status balanced to the cirrhotics(6, 7, 9, 12). Impaired psychometric performance > 2 SD of controls on any two of the SPT components (NCT-A > 35 seconds, NCT-B >99 seconds, DST <66 or BDT < 28) was considered diagnostic of MHE using the SPT (MHE SPT)(5). The diagnosis of MHE using ICT was performed on the basis of >5 lure response (MHE ICT)(6, 7).
DOT driving history
The driving records for all patients were requested from the DOT in Wisconsin and Virginia which included all driving offenses (both motor vehicle crashes and traffic violations) within the last year.
Self Reported Driving history
All patients were required to complete a driving history questionnaire which inquired about driving duration and driving offenses within 1 year of psychometric testing.
Motor vehicle crashes were defined as an accident between the occupant’s car when they were driving with another vehicle or the environment. Traffic violations were defined as a moving violation (other than parking violations) that resulted in the issuing of a ticket. A separate analysis of crashes was performed for MHE SPT and MHE ICT patients. The focus of this study was on crashes but traffic violations were also assessed.
The IRB at Medical College of Wisconsin and Virginia Commonwealth University approved this protocol.
Statistical Analysis
Non-parametric data were analyzed using Fisher’s and continuous variables by t-tests.
Analysis of motor vehicle crashes within 1 year of psychometric testing
was performed between cirrhotics with MHE (using SPT and ICT) to those without MHE. Relative risk for developing crashes in those with and without MHE was computed. Univariate and backward multivariate logistic regressions were performed using occurrence of crashes as the outcome and with age, gender, educational status, driving duration and diagnosis of MHE by ICT and SPT as predictors.
Prospective analysis of driving records for future driving offenses
Based on the classification at enrollment, patients were followed up prospectively for the development of crashes and violations as confirmed by DOT records. Patients who had died, had a liver transplant, had stopped driving or had developed OHE during the follow-up period were excluded as well as those patients with objective evidence in their driving records as having resumed alcohol or illicit drugs. A time to failure analysis using Kaplan Meier analysis with comparison of the groups using Wilcoxon rank sum test was performed. In addition, a Fisher’s exact test was used to examine the association between new crashes in the prospective follow-up period and previously assessed MHE separately by SPT and ICT, and between MHE SPT and MHE ICT. Multivariate logistic regression was conducted to model future driving offenses, as the outcome, using age, gender, educational status, prior crashes and violations within 1 year, MHE status using SPT, MHE status using ICT, and driving duration. The rate of future driving offenses in those with prior problems was also determined.
Agreement analysis
between self and DOT reports were calculated by kappa coefficient. These analyses were conducted using the self-reported crashes as well as the DOT-reported crashes, and were repeated using violations as the outcome in place of crashes. To assess the discrepancies between self-reported driving history and DOT-reported number of crashes and violations in these cirrhotics, kappa coefficients corrected for chance were computed to quantify the level of agreement between measures. Confidence intervals on the kappa coefficients for crashes and traffic violations as well as statistical tests of the kappa value were used to quantify the extent that the agreement between the self-reported measures and the DOT measures differed from chance.
RESULTS
A total of 167 patients with cirrhosis were included; all had DOT records. Of these 120 had self-report and 109 patients had prospective 1 year records (Figure 1). Demographic, driving and cirrhosis characteristics of the entire cirrhosis group are shown in Table 1. 127 patients were from Wisconsin and 40 were from Virginia.
Figure 1. Patient flow through the study.
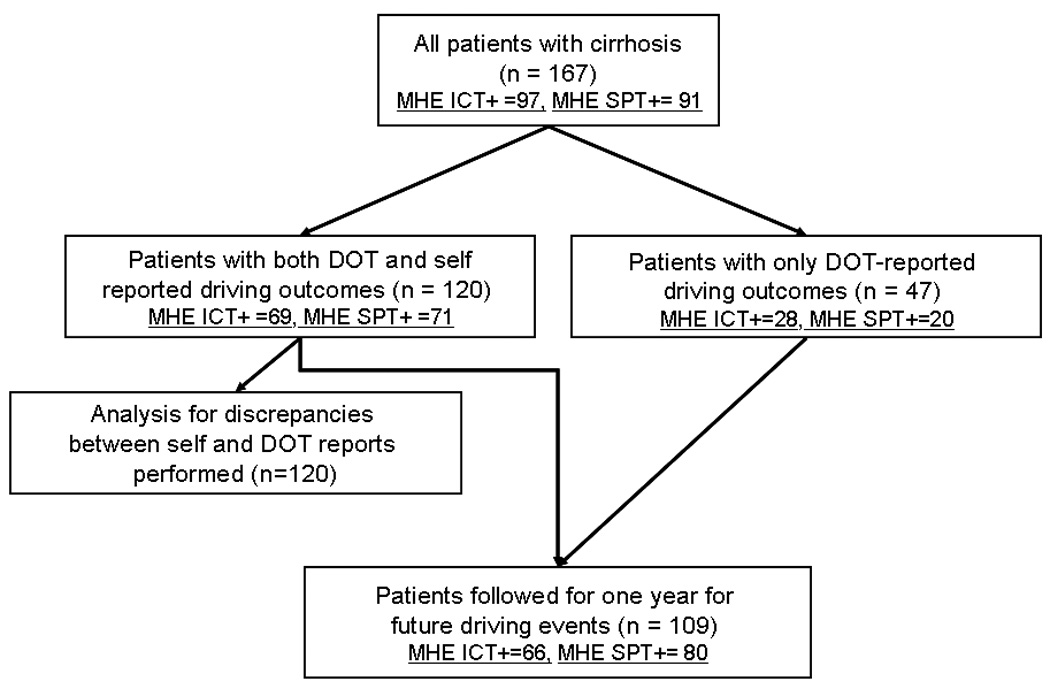
Patient flow throughout the study is displayed. At each stage, the number diagnosed with MHE using ICT and SPT are displayed. 47 patients only had DOT reports while 120 had both self and DOT assessments. Those 120 were used to study agreement between the self and DOT assessments. MHE: minimal hepatic encephalopathy, ICT: inhibitory control test, SPT: standard psychometric tests, DOT: department of transportation, MHE ICT+: those diagnosed with MHE using ICT, MHE SPT+: those diagnosed with MHE using SPT.
Table 1.
Baseline demographic variable
| Baseline variable | Patients with cirrhosis (n =167) |
|---|---|
| Age (years) | 53 ± 9 |
| Gender (Male/Female) | 95 / 72 |
| Educational status (years) | 13 ± 2 |
| Race (Caucasian/African- American/Other) |
110 / 23 / 13 / 21 |
| MELD score | 11 ± 2 |
| Child Class (A/B/C) | 107 / 52 / 8 |
| Etiology of cirrhosis (HCV/ Alcohol/ HCV+alcohol/ Cryptogenic/ Others) |
86 / 26 / 15 / 15 / 25 |
| Driving experience (years since obtaining a driving license) |
36 ± 11 |
| MHE diagnosis using SPT (any 2 of the following: NCT-A > 35 seconds, NCT-B >99 seconds, DST <68 or BDT < 28) |
91 (55%) |
| MHE diagnosis using ICT (lures >5) | 97 (58%) |
MHE: minimal hepatic encephalopathy, HCV: chronic hepatitis C, MELD: model for end-stage liver disease, ICT: inhibitory control test, NCT-A: number connection test-A, NCT-B: number connection test –B, DST: digit symbol test, BDT: block design test.
MHE diagnosis
Of the 167 patients, 97 had MHE ICT and 91 were diagnosed with MHE SPT. 111 patients had concordance between their MHE diagnosis using both techniques (65 positive and 44 negative by both). 32 patients had MHE by ICT and not SPT and 26 were diagnosed as MHE by SPT but not ICT. These were highly correlated (r=0.4, p=0.0001) but kappa was 0.29 with a 95% CI 0.02–0.57 indicating fair agreement.
Motor vehicle crashes: DOT reports
In the 167 patients in whom DOT data was available, there were 18 motor vehicle crashes. Three patients had one traffic violation and one crash each. All crashes were car crashes adjudged to be the patient’s fault. None were associated with alcohol. The crashes were property damage in 13 cases and were associated with injury in 5 cases. The details of MHE ICT vs. SPT and individual tests are shown in figure 2, figure 3 and figure 4 and table 2.
Figure 2.
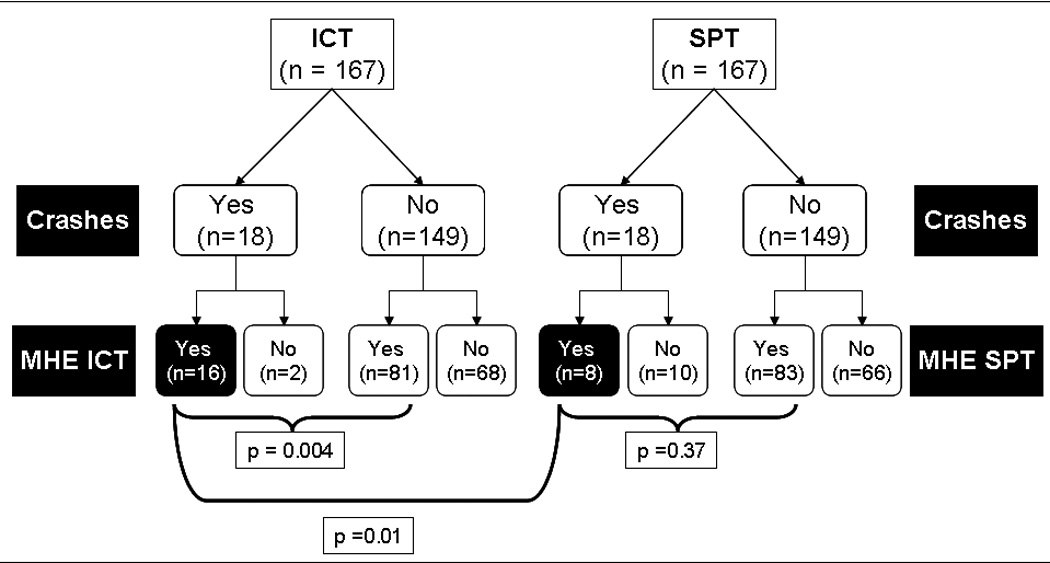
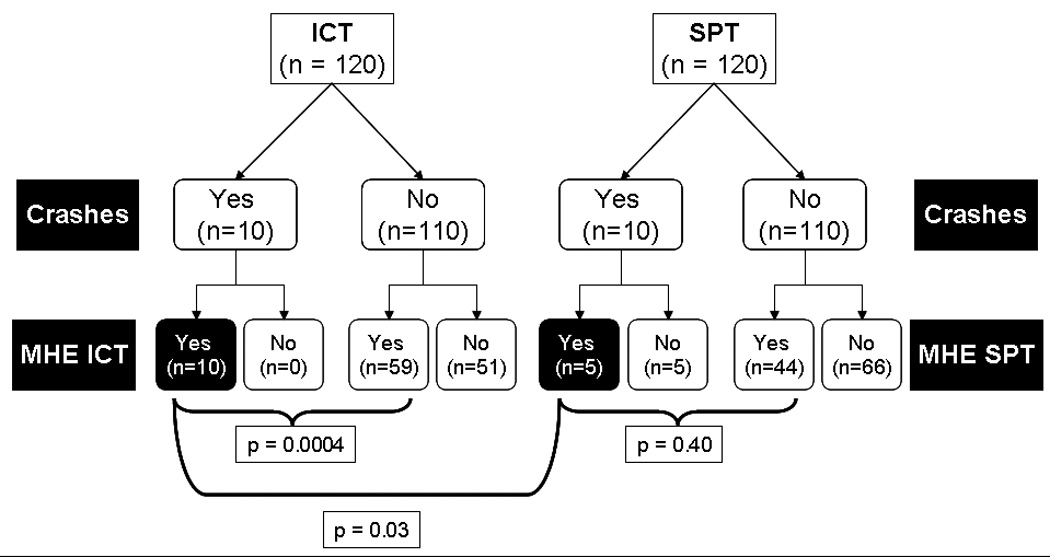
Figure 2a: Comparison of the mode of diagnosis of MHE with the motor vehicle crashes reported by the department of transportation in patients with cirrhosis. Detailed patient flow according to DOT-report of the patients with motor vehicle crashes who were diagnosed with MHE using ICT or SPT. A total of 167 patients were given both SPT and ICT and their subsequent classification according to DOT-reported motor vehicle crashes within the past 1 year and their comparison is shown.
Figure 2b: Comparison of the mode of diagnosis of MHE with motor vehicle crashes self-reported by the patients with cirrhosis. Detailed patient flow according to self-report of the patients with motor vehicle crashes who were diagnosed with MHE using ICT or SPT. A total of 120 patients were given both SPT and ICT and their subsequent classification according to self-reported motor vehicle crashes within the past 1 year and their comparison is shown. MHE: minimal hepatic encephalopathy, ICT: inhibitory control test, SPT: standard psychometric tests, MHE ICT: patients diagnosed with MHE using ICT, MHE SPT: patients diagnosed with MHE using SPT.
Figure 3. Motor vehicle crash occurrence and mode of diagnosis of MHE.
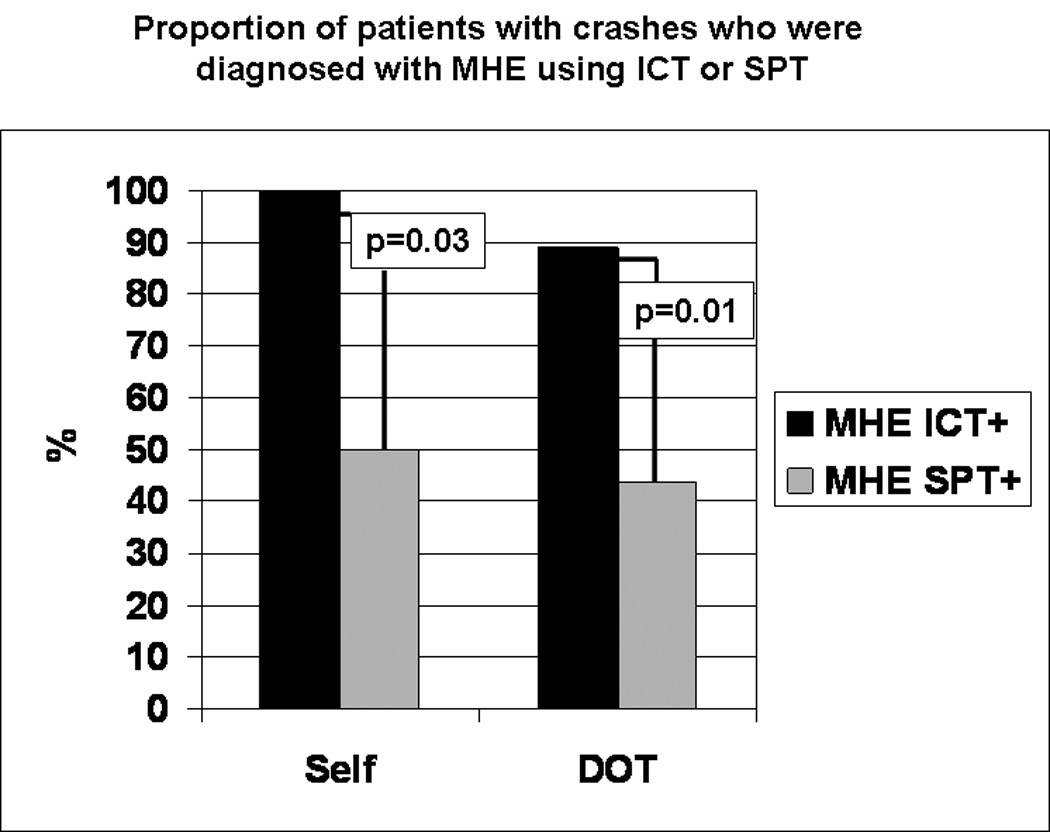
Percentage of patients with motor vehicle crashes with MHE according to ICT or SPT are displayed in this figure. 100% of patients with self-reported crashes had MHE according to ICT compared to 50% who had MHE according to SPT which was highly significant. Similarly, 89% of patients with DOT-reported crashes had MHE according to ICT compared to only 44% of those diagnosed by MHE using SPT. MHE: minimal hepatic encephalopathy, ICT: inhibitory control test, SPT: standard psychometric tests, DOT: department of transportation.
Figure 4.
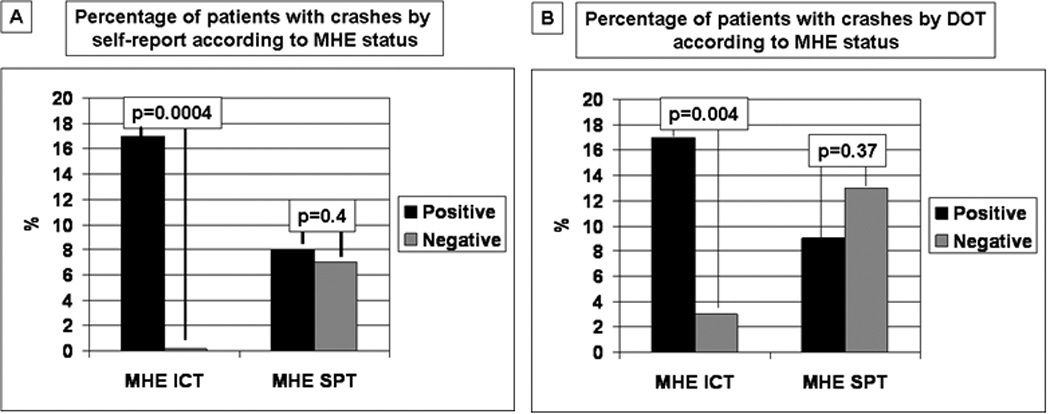
Figure 4a: Percent of patients with crashes by self report. Percentage of patients who had motor vehicle crashes according to self-report in those diagnosed with MHE using ICT (17%) were significantly higher compared to 0% in those who were negative for MHE using ICT. In contrast, there was no significant difference in the percentage of patients with MHE according to SPT performance. The relative risk for crashes according to MHE ICT status was 5.77.
Figure 4b: Percent of patients with crashes by DOT reports. Similarly there was a significantly higher percentage of patients diagnosed with MHE using ICT who had DOT-reported motor vehicle crashes (16%) compared to those who were negative by ICT (3%). Again, there was no significant difference in those with and without MHE diagnosed by SPT vis-à-vis motor vehicle crashes reported by the DOT.
Table 2.
Individual psychometric tests and the risk of motor vehicle crashes
| Self-reported motor vehicle crashes (n=120) |
DOT-reported motor vehicle crashes (n=167) |
|||
|---|---|---|---|---|
| Yes (n=10) |
No (n=110) |
Yes (n=18) |
No (n=149) |
|
| Age (years) | 56 ± 4 | 54 ± 9 | 56 ± 4 | 54 ± 9 |
| Duration of Driving (years) | 40 ± 7 | 36 ± 11 | 40 ± 7 | 36 ± 11 |
| Alcoholic etiology of cirrhosis (%) |
3 (30%) | 27 (24%) | 5 (28%) | 36 (24%) |
| NCT-A (seconds) |
37 ± 16 | 32 ± 13 | 32 ± 8 | 31 ± 11 |
| NCT-B (seconds) |
100 ± 28 | 97 ± 55 | 86 ± 27 | 87 ± 41 |
| DST (raw score) |
52 ± 12* | 61 ± 17 | 59 ± 16 | 66 ± 18 |
| BDT (raw score) |
50 ± 35 | 35 ± 29 | 50 ± 35 | 35 ± 29 |
| ICT lures (maximum = 40) |
14 ± 5† | 10 ± 8 | 11 ± 5‡ | 7 ± 6 |
| ICT targets (%) | 95 ± 4 | 92 ± 9 | 94 ± 5 | 93 ± 8 |
There was a significantly worse performance on ICT and DST in those with self-reported motor vehicle crashes compared to those who did not have a self-reported crash. ICT lures were also significantly higher in patients who had a DOT-reported crash compared to those who did not. A high ICT lure and low DST raw score indicate poor psychometric performance. There were no significant differences in the demographics, alcoholic etiology and other psychometric tests between the groups. The statistically significant comparisons between those with and without crashes are in bold.
p=0.04,
p=0.03,
p=0.04. MHE: minimal hepatic encephalopathy, ICT: inhibitory control test, NCT-A: number connection test-A, NCT-B: number connection test –B, DST: digit symbol test, BDT: block design test, DOT: department of transportation.
On logistic regression, MHE ICT was the only variable significantly associated with motor vehicle crashes (OR 5.72, 95% CI:1.22–26.76, p=0.0009). The relative risk calculated for patients with MHE ICT experience a DOT-reported crash was 5.77 with a 95% CI ranging from 2.01 to 16.6.
Motor vehicle crashes: Self-reports
Of the 120 patients, 69 were diagnosed with MHE ICT and 71 with MHE SPT (Figure 2b). In these 120 patients with cirrhosis, 10 had crashes (all had 1 each) over the last year. These were all crashes between cars, all were the patient’s fault and none were associated with a high blood alcohol level. The details of MHE ICT vs. SPT and individual tests are shown in figure 2, figure 3 and figure 4 and table 2.
All patients who self-reported crashes had MHE diagnosed by ICT. In this instance, the RR becomes too large to compute as the probability in the control condition (those without MHE) for the denominator of the ratio was zero.
Traffic Violations: DOT reports over 1 year
There were 18 violations that were confirmed by the state DOT. Three patients had 1 violation and 1 crash each. The majority (14, 80%) of traffic violations was speeding tickets, two were failure to stop and one was for driving too slow. Of the twelve speeding tickets, 8 were given for speed between 11–19 mph over the limit, 3 for less than 10 mph over the limit and two for driving more than 20 mph over the speed limit.
Of the 18 violations reported by the DOT, 12 (67%) were caused by patients who had MHE ICT compared to 9 (50%) with MHE SPT. This comparison was not statistically significant (p = 0.31).
Rate of violations according to the DOT were similar between patients with MHE ICT (12 out of 97, 12.3%) compared to patients without MHE diagnosed with ICT (6 out of 70, 9%, p = 0.33). Similarly, rates of traffic violations were not significantly different between patients with MHE SPT (9 of 91, 10%) compared to those diagnosed without MHE using SPT (9 of 76, 12%, p=0.54).
None of the variables, age, educational status, duration of driving, MHE ICT and MHE SPT were statistically associated with violations on multi-variate regression. There were no significant differences in individual psychometric tests between those with and without a violation reported by the DOT.
Traffic Violations: self-reports over 1 year
In these 120 cirrhotics who self-reported, 14 admitted to traffic violations (all had 1 each) of which 12 were speeding tickets, 1 was failure to obey signal and 1 was driving the wrong way. Of the 14 violations, 10 (71%) were MHE ICT and 12 (86%) were MHE SPT (p=0.64). There was no statistical difference between presence of MHE ICT and self-reported violations (MHE ICT positive: 10 out of 69, 15% versus MHE ICT negative: 4 out of 51, 8%, p=0.4). There was a statistically higher prevalence of self-reported traffic violations in MHE SPT positive patients (12 out of 91, 13%) compared to those were negative for MHE using SPT (2 out of 76, 3%, p=0.001). There were no significant differences in the demographics, driving duration and individual psychometric tests in patients who had admitted to a traffic violation or not within the last year. None of the individual SPT components were able to reliably predict the occurrence of crashes and violations over the preceding year.
Agreement analysis
The 120 patients who had both self-assessment and DOT reports were compared for discrepancies in the traffic violation and motor vehicle crashes. The discrepancies were divided into those in which the self-reported offenses were more than the DOT-reported ones (Self>DOT) and vice-versa (DOT>self).
Motor vehicle crashes
There was a discrepancy in only 2 patients and both these patients had not mentioned a crash which was discovered on the DOT records. Kappa coefficients calculated for agreement between the DOT and self-report for motor vehicle crashes was 0.90 (95% CI: 0.72–1.08), indicating a strong agreement.
Traffic Violations
There were a total of 5 patients with discrepancies in the self and DOT-reported violations, 2 of which were self>DOT and 3 were DOT> self. Two of three patients whose DOT reports had traffic violations that were not reported by them had been diagnosed with MHE by both SPT and ICT and all these three violations were speeding tickets. Kappa for agreement between DOT and self-reported violations were significant with a kappa of 0.80 (95% CI: 0.62–0.98).
Future driving offenses: prospective follow-up
Of the 109 patients who had data at 1 year follow-up, 66 were MHE ICT and 80 were MHE SPT. Thirty-two were lost to follow-up, 10 were followed for <1 year, 8 developed OHE, 4 died due to liver-related complications and 4 stopped driving for reasons unrelated to their liver disease.
Eighteen patients had experience a traffic violation or motor vehicle crash over 1 year (11 crashes and 7 violations). All motor vehicle crashes involved cars and all violations were speeding tickets. None of the patients had alcohol-associated crashes and all of them were their fault.
There was no significant difference between the percent of patients who had future driving offenses with MHE ICT (n=18, offenses 15, 83%) compared to those with MHE SPT (n=18, offenses 17, 94%, p=0.62).
There was a significantly higher rate of future driving offenses in the MHE ICT (15 of 66, 22%) compared to those without (3 of 43, 7%, p=0.03). There was no difference between those positive (17 of 80, 21%) and negative (1 of 29, 4%, p=0.18) for MHE SPT. Using a Kaplan Meier method with Wilcoxon rank test, patients with MHE ICT were significantly more likely to have future driving offenses compared to those without MHE ICT (p=0.031). 28 patients had prior DOT-reported crash or traffic violation, of which 36% had a future event compared to only 14% of those without prior DOT-reported crash or violation (p=0.01).
On multi-variate logistic regression with future offenses as the outcome, MHE ICT was statistically associated as a risk factor (OR 4.51, 95% CI, 1.12–19.39), DOT reports of prior crash or violation (OR 2.96, 95% CI: 1.12–7.82) while age was protective (OR 0.94, 95% CI 0.86 to 0.99).
DISCUSSION
The current study demonstrates a significantly higher rate of motor vehicle crashes in MHE patients defined by the ICT over the preceding year using official driving records and self-report compared to patients without MHE. The findings also demonstrate that ICT was superior to SPT for identification of patients at risk of developing crashes on prospective follow-up and in the prior year. There was also a significant agreement between the number of crashes and traffic violations admitted by the patients compared to the official DOT records.
The striking observation is the significantly higher rate of motor vehicle crashes in the MHE ICT patients (16%) compared to those without MHE ICT (4%). This is far in excess of the baseline rates of crashes in the population of Virginia and Wisconsin that range between 3–3.3% annually(14, 15). The crashes were the fault of the drivers and none were associated with alcohol use. The inherent attention deficits and response disinhibition contribute to the driving impairment, along with the predisposition to fatigue(16–20) These results are in line with prior studies that have shown that MHE patients have poor on-road driving test performance(10, 21). This paper also confirms and extends these findings by comparing the self and DOT-reported rates of motor vehicle crashes and traffic violations in patients with cirrhosis with and without MHE. These findings should be specifically considered in the light of the fact that the included age-range of patients is considered the safest group with regards to driving outcomes compared to the very young and those over >70 years of age. This makes the case for an intrinsic difficulty in driving rather than age or lack of driving experience to be the factors associated with the high rate of crashes in the MHE ICT group. Interestingly, traffic violations were not significantly associated with the presence or absence of MHE by SPT or ICT in this paper. Using violations was not part of the a priori hypothesis because they are highly dependent on the underlying behavior of the patient and also on the chance of a traffic police presence when they occur. In contrast, most motor vehicle crashes are registered in the official DOT database and represent an immediate and extreme driving outcome.
This paper shows that ICT performance is a significantly better indicator of real-world consequences of MHE than the SPT. This may be in part due to the relatively stringent criteria required for MHE diagnosis using SPT i.e. > 2 standard deviations beyond controls on 2 tests. However, this is also in line with our a priori hypothesis since the ICT is a dynamic and demanding test that involves the subject reacting within a fixed time period to certain pre-determined stimuli, similar to the demands of driving. A high ICT lure response is a sign of frontal lobe immaturity that results in impaired response inhibition(8). Response inhibition involves selective attention to a subset of a complex environment requiring activation of appropriate meanings during learning and activation of appropriate memories at encoding and retrieval. DST is affected by poor processing speed and is a sensitive test for the detection of early impairment. Therefore it is not surprising that the ICT and DST, which rely on intact frontal lobe activation, would be significantly impaired in patients with prior crashes compared to those who do not. These findings extend the correlation between ICT lures and driving simulator results into the field of actual driving. This should increase the implementation of this test in practice, especially since a normal ICT performance is only associated with crashes in 3% of cases, similar to the background rates.
The current study demonstrates that patients with cirrhosis, with or without MHE, were to a large extent truthful about their crashes and violations. There were 5 instances in which crashes and violations were not admitted on the self-report but were found on the DOT report. While it may be possible that this could be a willful misrepresentation, it could also be due to confusion as to the actual date of these events. None of the traffic violations and crashes were driving-under-the influence, which indicates that this was not an outcome that patients would need to conceal from a hepatologist who may be evaluating them for transplant in the future. On the other hand, there were 2 instances where the self-admitted questionnaire yielded a higher number of violations than those reported by the DOT. This is was due to the violations having occurred out-of-state. This is against our a priori hypothesis. These findings, however, are in line with those with obstructive sleep apnea patients(22). MHE patients over-estimate their driving skills when directly questioned, even though they admit to most driving outcomes truthfully(12). This demonstrates a disconnect between their driving history and their personal interpretation of it and affirms the appropriateness of the directly asking the patients for events in their driving history, not their personal assessment of their driving skills, without the need for DOT inquiry.
Patients with cirrhosis have a higher risk of mortality and economic outcomes when they experience motor vehicle crashes; therefore the prevention of these crashes is essential(13). However, the medico-legal aspect of crashes in MHE cannot be ignored, considering the recent reports(23). Complicating this are varying clinician responsibilities to report to the DOT in different US states(24, 25). Although this study shows that MHE patients are statistically more likely to have a history of crashes and develop future problems, this still only applies to 8–16% of MHE patients (depending on mode of diagnosis). There are several competing inputs that have to be balanced while driving and medical impairments only affect them partially. Decisions while operating a car are made on a strategic, tactical and operational level. The strategic or topmost level such as route planning etc, are not likely to be affected by MHE(26). However the tactical decisions, including passing and operational decisions such as handling the steering and brakes are likely impacted by MHE(10). These are similar to the struggles faced by those performing assessments in older adults and those with attention-deficit disorder(27–29). Importantly, a history of prior crashes and violations was also significantly associated with future driving offenses. Therefore, the merely being diagnosed with MHE should not trigger a referral to DOT and should not pose any medico-legal liability to the testing physician. Also, since testing for MHE and subsequent treatment can improve the patients’ quality of life, potential liability issues should not hinder the diagnosis of MHE (30). However, a careful elicitation of the driving history and discussion with the patients and their families should be performed during clinic visits. Those patients with a higher prior motor vehicle crash and violation rate and with MHE may benefit from official DOT assessment.
The current study is limited by the use of the individual state DOTs which would necessarily restrict the DOT reports to that state; this may under-estimate the DOT-reported traffic outcomes. Since the number of MHE ICT patients in the whole group were higher than MHE SPT, it could be possible that the increased rates of crashes in MHE ICT are higher due to this high number. However, despite this increased number, there was a statistically higher lure number in those with crashes both by their report and by the DOT.
In conclusion, the study demonstrates that patients with MHE diagnosed with ICT have a significantly higher rate of motor vehicle crashes both over the last 1 year and on prospective follow-up for 1 year compared to those without MHE and the background rate in the state. There was a high agreement between patients’ self-report and report on the DOT with respect to motor vehicle crashes and traffic violations. Further research into the effect of MHE therapy on these driving outcomes is warranted.
Acknowledgments
Grant support: This was supported in part by the American College of Gastroenterology Junior Faculty Development Award, and by clinical research center grants MO1-RR00065 and MO1-RR00058, NCRR, NIH (awarded to JSB).
Abbreviations
- MHE
minimal hepatic encephalopathy
- ICT
inhibitory control test
- NCT-A
number connection test-A
- NCT-B
number connection test –B
- DST
digit symbol test
- BDT
block design test
- DOT
department of transportation
- MVC
motor vehicle crashes
- TV
traffic violations
Footnotes
Conclusions: Cirrhotics with MHEICT have a significantly higher crash rate over the preceding year and on prospective follow-up compared to patients without MHE. ICT, but not SPT performance is significantly associated with prior and future crashes and violations. There was an excellent agreement between self- and DOT-reports.
REFERENCES
- 1.Hartmann IJ, Groeneweg M, Quero JC, Beijeman SJ, de Man RA, Hop WC, Schalm SW. The prognostic significance of subclinical hepatic encephalopathy. Am J Gastroenterol. 2000;95:2029–2034. doi: 10.1111/j.1572-0241.2000.02265.x. [DOI] [PubMed] [Google Scholar]
- 2.Romero-Gomez M, Boza F, Garcia-Valdecasas MS, Garcia E, Aguilar-Reina J. Subclinical hepatic encephalopathy predicts the development of overt hepatic encephalopathy. Am J Gastroenterol. 2001;96:2718–2723. doi: 10.1111/j.1572-0241.2001.04130.x. [DOI] [PubMed] [Google Scholar]
- 3.Groeneweg M, Quero JC, De Bruijn I, Hartmann IJ, Essink-bot ML, Hop WC, Schalm SW. Subclinical hepatic encephalopathy impairs daily functioning. Hepatology. 1998;28:45–49. doi: 10.1002/hep.510280108. [DOI] [PubMed] [Google Scholar]
- 4.Ortiz M, Jacas C, Cordoba J. Minimal hepatic encephalopathy: diagnosis, clinical significance and recommendations. J Hepatol. 2005;42 Suppl:S45–S53. doi: 10.1016/j.jhep.2004.11.028. [DOI] [PubMed] [Google Scholar]
- 5.Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathy--definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716–721. doi: 10.1053/jhep.2002.31250. [DOI] [PubMed] [Google Scholar]
- 6.Bajaj JS, Hafeezullah M, Franco J, Varma RR, Hoffmann RG, Knox JF, Hischke D, et al. Inhibitory control test for the diagnosis of minimal hepatic encephalopathy. Gastroenterology. 2008;135:1591–1600. doi: 10.1053/j.gastro.2008.07.021. e1591. [DOI] [PubMed] [Google Scholar]
- 7.Bajaj JS, Saeian K, Verber MD, Hischke D, Hoffmann RG, Franco J, Varma RR, et al. Inhibitory control test is a simple method to diagnose minimal hepatic encephalopathy and predict development of overt hepatic encephalopathy. Am J Gastroenterol. 2007;102:754–760. doi: 10.1111/j.1572-0241.2007.01048.x. [DOI] [PubMed] [Google Scholar]
- 8.Garavan H, Ross TJ, Stein EA. Right hemispheric dominance of inhibitory control: an event-related functional MRI study. Proc Natl Acad Sci U S A. 1999;96:8301–8306. doi: 10.1073/pnas.96.14.8301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bajaj JS, Hafeezullah M, Hoffmann RG, Varma RR, Franco J, Binion DG, Hammeke TA, et al. Navigation skill impairment: Another dimension of the driving difficulties in minimal hepatic encephalopathy. Hepatology. 2008;47:596–604. doi: 10.1002/hep.22032. [DOI] [PubMed] [Google Scholar]
- 10.Wein C, Koch H, Popp B, Oehler G, Schauder P. Minimal hepatic encephalopathy impairs fitness to drive. Hepatology. 2004;39:739–745. doi: 10.1002/hep.20095. [DOI] [PubMed] [Google Scholar]
- 11.Bajaj JS, Hafeezullah M, Hoffmann RG, Saeian K. Minimal hepatic encephalopathy: a vehicle for accidents and traffic violations. Am J Gastroenterol. 2007;102:1903–1909. doi: 10.1111/j.1572-0241.2007.01424.x. [DOI] [PubMed] [Google Scholar]
- 12.Bajaj JS, Saeian K, Hafeezullah M, Hoffmann RG, Hammeke TA. Patients with minimal hepatic encephalopathy have poor insight into their driving skills. Clin Gastroenterol Hepatol. 2008;6:1135–1139. doi: 10.1016/j.cgh.2008.05.025. quiz 1065. [DOI] [PubMed] [Google Scholar]
- 13.Bajaj JS, Ananthakrishnan AN, McGinley EL, Hoffmann RG, Brasel KJ. Deleterious effect of cirrhosis on outcomes after motor vehicle crashes using the nationwide inpatient sample. Am J Gastroenterol. 2008;103:1674–1681. doi: 10.1111/j.1572-0241.2008.01814.x. [DOI] [PubMed] [Google Scholar]
- 14. http://www.dmv.state.va.us/webdoc/pdf/vacrashsummary_07.pdf. In.
- 15. http://www.dot.wisconsin.gov/safety/motorist/crashfacts/docs/crash-general.pdf. In.
- 16.Schiff S, Vallesi A, Mapelli D, Orsato R, Pellegrini A, Umilta C, Gatta A, et al. Impairment of response inhibition precedes motor alteration in the early stage of liver cirrhosis: a behavioral and electrophysiological study. Metab Brain Dis. 2005;20:381–392. doi: 10.1007/s11011-005-7922-4. [DOI] [PubMed] [Google Scholar]
- 17.Weissenborn K, Ennen JC, Schomerus H, Ruckert N, Hecker H. Neuropsychological characterization of hepatic encephalopathy. J Hepatol. 2001;34:768–773. doi: 10.1016/s0168-8278(01)00026-5. [DOI] [PubMed] [Google Scholar]
- 18.Weissenborn K, Giewekemeyer K, Heidenreich S, Bokemeyer M, Berding G, Ahl B. Attention, memory, and cognitive function in hepatic encephalopathy. Metab Brain Dis. 2005;20:359–367. doi: 10.1007/s11011-005-7919-z. [DOI] [PubMed] [Google Scholar]
- 19.Weissenborn K, Heidenreich S, Ennen J, Ruckert N, Hecker H. Attention deficits in minimal hepatic encephalopathy. Metab Brain Dis. 2001;16:13–19. doi: 10.1023/a:1011654210096. [DOI] [PubMed] [Google Scholar]
- 20.Bajaj JS, Hafeezullah M, Zadvornova Y, Martin E, Schubert CM, Gibson DP, Hoffmann RG, et al. The Effect of Fatigue on Driving Skills in Patients With Hepatic Encephalopathy. Am J Gastroenterol. 2009 doi: 10.1038/ajg.2009.7. [DOI] [PubMed] [Google Scholar]
- 21.Watanabe A, Tuchida T, Yata Y, Kuwabara Y. Evaluation of neuropsychological function in patients with liver cirrhosis with special reference to their driving ability. Metab Brain Dis. 1995;10:239–248. doi: 10.1007/BF02081029. [DOI] [PubMed] [Google Scholar]
- 22.Wu H, Yan-Go F. Self-reported automobile accidents involving patients with obstructive sleep apnea. Neurology. 1996;46:1254–1257. doi: 10.1212/wnl.46.5.1254. [DOI] [PubMed] [Google Scholar]
- 23.Annas GJ. Doctors, drugs, and driving--tort liability for patient-caused accidents. N Engl J Med. 2008;359:521–525. doi: 10.1056/NEJMhle0802548. [DOI] [PubMed] [Google Scholar]
- 24. http://www.ama-assn.org/ama1/pub/upload/mm/433/chapter8.pdf. In.
- 25.Snyder KM, Ganzini L. Outcomes of Oregon's Law Mandating Physician Reporting of Impaired Drivers. J Geriatr Psychiatry Neurol. 2009 doi: 10.1177/0891988709332943. [DOI] [PubMed] [Google Scholar]
- 26.Marshall SC. The role of reduced fitness to drive due to medical impairments in explaining crashes involving older drivers. Traffic Inj Prev. 2008;9:291–298. doi: 10.1080/15389580801895244. [DOI] [PubMed] [Google Scholar]
- 27.Martin AJ, Marottoli R, O'Neill D. Driving assessment for maintaining mobility and safety in drivers with dementia. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD006222.pub2. CD006222. [DOI] [PubMed] [Google Scholar]
- 28.Reimer B, D'Ambrosio LA, Coughlin JF, Fried R, Biederman J. Task-induced fatigue and collisions in adult drivers with attention deficit hyperactivity disorder. Traffic Inj Prev. 2007;8:290–299. doi: 10.1080/15389580701257842. [DOI] [PubMed] [Google Scholar]
- 29.Barkley RA, Murphy KR, Dupaul GI, Bush T. Driving in young adults with attention deficit hyperactivity disorder: knowledge, performance, adverse outcomes, and the role of executive functioning. J Int Neuropsychol Soc. 2002;8:655–672. doi: 10.1017/s1355617702801345. [DOI] [PubMed] [Google Scholar]
- 30.Prasad S, Dhiman RK, Duseja A, Chawla YK, Sharma A, Agarwal R. Lactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology. 2007;45:549–559. doi: 10.1002/hep.21533. [DOI] [PubMed] [Google Scholar]


