Abstract
In this study, we evaluated predictors of resilience among 8- to 12-year-old children recruited from primarily low socioeconomic status neighborhoods, 117 of whom suffered from clinical levels of conduct problems and/or depression, and 63 of whom suffered from no significant symptoms. Tests of interactions were conducted between (a) paternal antisocial behavior and maternal depression and (b) several physiological indices of child temperament and emotionality in predicting (c) children’s conduct problems and depression. Both internalizing and externalizing outcomes among children were associated specifically with maternal melancholic depression, and not with nonmelancholic depression. In addition, low levels of respiratory sinus arrhythmia (RSA) among children conferred significant risk for depression, regardless of maternal melancholia, whereas high RSA offered partial protection. Furthermore, high levels of maternal melancholia conferred significant risk for child depression, regardless of paternal antisocial behavior, whereas low levels of maternal melancholia offered partial protection. Finally, low levels of electrodermal responding (EDR) conferred significant risk for conduct problems, regardless of paternal antisocial behavior, whereas high EDR offered partial protection. None of the identified protective factors offered complete immunity from psychopathology. These findings underscore the complexity of resilience and resilience-related processes, and suggest several potential avenues for future longitudinal research.
Several alternative definitions of resilience have been proposed by developmental psychopathologists, yet all include some form of adaptive functioning following significant exposure to adversity (see Luthar, Cicchetti, & Becker, 2000). Adverse risk exposure is central to any definition of resilience because without such experiences, psychopathological outcomes are far less likely, so the construct loses much of its meaning (Curtis & Cicchetti, 2003; Luthar, 2006). Accordingly, most researchers agree that some form of risk exposure is necessary to infer resilience or resilience-related processes. Nevertheless, both adaptation and adversity are often defined very differently across studies, sometimes quite broadly and other times quite specifically. For example, adaptation has been defined as a set of general competencies across multiple domains of functioning including social, occupational, and psychopathological; yet it has also been defined as the absence of a specific psychiatric condition such as major depression despite a strong familial loading for mood disorders (see Luthar, 2006). From a developmental psychopathology perspective, more broad definitions of adaptation are preferred because most adversities confer risk that extends to a wide range of multifinal outcomes. For example, in addition to increasing the risk for mood disorders among offspring, maternal depression also confers risk for conduct problems, delinquency, and antisocial behavior (Boyle & Pickles, 1997; Kim-Cohen, Moffitt, Taylor, Pawlby, & Caspi, 2005; Patterson, 1996). Thus, defining adaptation as the absence of mood disorders among children of depressed mothers restricts our understanding of resilience by excluding known sequelae of risk exposure. Moreover, it is possible for an individual to exhibit considerable resilience in one or more domains but not in others (Luthar et al., 2000).
Resilience researchers have traditionally focused on the study of psychological predictors of adaptation, yet more recent writings also emphasize genetic, epigenetic, neural, and other biological effects (e.g., Curtis & Cicchetti, 2003; Jaffee et al., 2005; Luthar, 2006; Luthar et al., 2000; Rutter, 2002; Seeger, Schloss, Schmidt, Ru¨ter-Jungfleisch, & Henn, 2004). Indeed, a comprehensive understanding of resilience requires consideration of the bidirectional influences between an individual and his or her environment over time, at multiple levels of analysis. In this sense, resilience is not static. Rather, it is the set of social, psychological, and biological processes through which one achieves comparative adjustment as developmental task demands are confronted across the life span. It is now widely recognized that family environments, social milieus, and psychological processes all affect the functioning of biological systems—including the expression of genes that are implicated in the regulation of behavior (e.g., Beauchaine, Gatzke-Kopp, & Mead, 2007; Cicchetti & Valentino, 2006; Cicchetti & Walker, 2001; Gunnar & Vazquez, 2001; Raine et al. 2001). In turn, an individual’s biological states and predispositions contribute to both the selection of particular environments, and to altering the responses of those environments to the individual (see, e.g., Moffitt, 2005; Moffitt, Caspi, & Rutter, 2006). Similar to multifinal pathways to psychopathology, pathways to resilience are likely to be complex and idiosyncratic, with reciprocal feedback among causal influences.
Mechanisms through which adversity leads to psychopathology are typically referred to as either vulnerabilities or risk factors. Although these terms have been used inconsistently and at times interchangeably throughout the history of resilience research (see Luthar et al., 2000), vulnerabilities are often assumed to be biologically based traits that render individuals particularly susceptible to psychopathology, such as behavioral inhibition (e.g., Woodward, Lenzenweger, Kagan, Snidman, & Arcus, 2000) and impulsivity (e.g., Beauchaine, 2001). In contrast, risk factors are often assumed to be environmental influences that interact with vulnerabilities to increase the likelihood of psychopathology. Examples include neighborhood characteristics that amplify risk for conduct problems among impulsive males (e.g., Lynam et al., 2000) and distressing experiences that elicit posttraumatic stress disorder in genetically predisposed individuals (e.g., Orr et al., 2003; Stein, Jang, Taylor, Vernon, & Livesley, 2002). This distinction between risk factors and vulnerabilities breaks down, however, when we consider the reciprocal and interactive roles that genes play in eliciting specific environments, and that environments play in the expression of genes. These interactive influences blur traditional boundaries between vulnerabilities and risk factors, and suggest that distinctions between genetic and environmental effects on behavior are often artificial. Perhaps more importantly, to the extent that genetic and environmental influences are dissociable, disambiguating them is extremely difficult in naturalistic settings where environments cannot be manipulated (Moffitt, 2005). Because of such ambiguities, we prefer the term potentiator to describe all influences that amplify the likelihood of psychopathology, relying on description of specific mechanisms to infer whether the source of potentiation is genetic, environmental, epigenetic, or interactive.1
In addition to exerting potentiating effects, both biological and environmental processes can attenuate the likelihood of psychiatric morbidity following adversity. Mechanisms through which psychopathology is prevented are typically referred to as either resilience or protective factors. These terms have also been used inconsistently and at times interchangeably (see Luthar et al., 2000). Many have assumed that resilience reflects constitutional characteristics that render individuals less vulnerable to psychopathology, such as intelligence (see Garmezy, Masten, & Tellegen, 1984). Recently, however, several authors have made strong distinctions between the terms resilience and resiliency, the latter of which is reserved for attributes of the child, and the former of which is assumed to reflect interactive processes between the child and his or her environment, with no assumptions about endogenous versus exogenous bases (Luthar et al., 2000; Masten, 2001). In contrast, protective factors are often assumed to be environmental influences that contribute to resilient outcomes, such as parental monitoring in high-risk neighborhoods (e.g., Buckner, Mezzacappa, & Beardslee, 2003; Dishion & Kavanagh, 2003). In keeping with these distinctions, we use the term protective factor to refer to any attenuative influence on psychiatric morbidity following exposure to adversity, and the term resilience to refer to outcomes that are better than expected given significant risk exposure. Unless noted specifically, we do not assume or imply purely heritable or purely environmental transmission of risk potentiation or attenuation given the difficulties outlined above toward disambiguating such influences.
Further complicating the study of resilience is the contextual nature of the phenomenon. A single trait may confer either vulnerability or resilience, depending on specific qualities of the environment to which one is exposed (Masten, 2001). Temperament is one individual characteristic that has been studied as both a potentiator and an attenuator of risk (e.g., Rutter, 2002). Temperament comprises individual differences in reactivity and self-regulation that are influenced strongly by heritable neurobiological bases (Rothbart & Bates, 1998; Rothbart, Evans, & Ahadi, 2000). Reactivity refers to the onset, intensity, and duration of positive and negative emotionality, whereas self-regulation refers to the ability to override prepotent behavioral and emotional responses through modulation of arousal, activity level, and attention. Individual differences in temperament can interact with environments to alter developmental trajectories in adjustment in different directions depending on the nature of risk exposure. For example, behavioral inhibition, a core component of temperament, confers resilience among those at risk for antisocial behavior (Rutter, 2002) but potentiates risk for social withdrawal and anxiety.
Risk Factors for Conduct Problems and Depression in Children
In our lab we recently finished participant recruitment for a longitudinal study examining the emergence of conduct problems and depression in middle childhood. Although the literature addressing these common psychiatric conditions has evolved somewhat separately, there are several compelling reasons to study the development of both disorders within a single sample. Despite their divergent presentations at the symptom level, conduct disorder (CD) and depression are highly comorbid conditions in childhood and adolescence. Epi-demiologic and clinical samples have yielded depression co-occurrence rates ranging from 15 to 82% among children and adolescents with CD (Angold & Costello, 1993; Bird, Gould, & Staghezza, 1993; Drabick, Beau-chaine, Gadow, Carlson, & Bromet, 2006; Fleming, Boyle, & Offord, 1993; Hewitt et al., 1997; Kashani et al., 1980; Pliszka, Sherman, Barrow, & Irick, 2000; Zoccolillo, 1992). Although this interval is wide, it is clear that the rate of depression among those with CD is significantly higher than the rate of depression in the population at large. Furthermore, several authors have reported especially high symptom severity among behavior-disordered youth who are depressed. Compared with their nondepressed counterparts, depressed children with CD exhibit higher rates of substance use (Costello, Erkanli, Federman, & Angold, 1999; Whitmore et al., 1997), social rejection (Cole & Carpentieri, 1990), anxiety disorders (Riggs, Baker, Mikulich, Young, & Crowley, 1995), and suicide (Rapp & Wodarski, 1997). Thus, comorbid depression confers heightened risk for a number of adverse outcomes among youth with CD, who are already among the most recalcitrant of all psychiatric groups. Finally, behavior genetics studies have indicated that much of the covariation between depression and antisocial behavior among adolescents is accounted for by a single latent trait (O’Connor, McGuire, Reiss, Hetherington, & Plomin, 1998). Behaviorally, this trait is likely expressed as negative emotionality, which predisposes affected individuals to a wide range of aversive emotions including guilt, anxiety, and irritability (Lilienfeld, 2003).
Although our study was not designed to address resilience directly, the data we have collected provide an opportunity to evaluate variables from multiple levels of analysis that might mollify or potentiate risk for conduct problems and/or depression. As discussed above, resilience is best assessed broadly, using indicators from multiple functional domains (e.g., behavioral, academic, psychopathological; Luthar et al., 2000; Masten, 2001). Nevertheless, the absence of psychopathology among those at high risk remains central to most theories of resilience. In the present paper, we evaluate levels of conduct problems and depression among children at risk for either or both psychiatric condition(s). Because we do not evaluate other important functional domains, our results should be interpreted as but one component in a broader network of resiliency processes. In the sections to follow, we describe the rationales behind our choices of specific variables that were evaluated. This discussion is not intended as a comprehensive review of the risk or resilience literatures vis-a`-vis conduct problems or depression. Rather, we focus on variables specific to our study.
Paternal antisocial behavior
Links to child conduct problems
Several authors have noted a distinct lack of research addressing the contribution of paternal characteristics and behaviors to child adjustment (e.g., Connell & Goodman, 2002; Phares & Compas, 1992). Although characteristics of mothers that predict adverse outcomes among children have frequently been studied, paternal attributes that confer risk for child maladjust-ment have received far less attention. Studies that have been conducted indicate that paternal psychopathology plays a powerful role in the adjustment of children, particularly for externalizing behavior disorders. Such findings may be especially true for sons of antisocial fathers (Phares & Compas, 1992).
The DSM IV (American Psychological Association, 2000) characterizes antisocial personality disorder (ASPD) as a persistent pattern of behavior reflecting both disregard for and frequent violation of the rights of others. Affected individuals are often deceitful, aggressive, irresponsible, and remorseless. Antisocial personality disorder likely reflects an extreme along a continuum of disruptive behavior. Thus, an individual need not qualify for a diagnosis in order to display serious interpersonal difficulties. An ever increasing body of research has demonstrated strong associations between paternal antisocial behavior and negative child outcomes.
In several studies of conduct problems among children, rates of paternal psychopathology have been compared across groups of probands and controls. For example, Frick and colleagues (1992) compared parental psychopathology rates for groups of children with CD, oppositional defiant disorder (ODD), or neither. They found that only 8% of fathers of control children met criteria for ASPD, whereas 19% of fathers of ODD children and 35% of fathers of CD children met criteria. Additional analyses indicated that having a father with ASPD significantly increased the odds of child CD, independent of maternal parenting. In contrast, the odds of a child having CD were not related to maternal parenting after controlling for paternal ASPD. Having a biological father with ASPD therefore outweighed the effects of parenting.
A study by Barnow, Lucht, and Freyberger (2005) produced similar results. These authors explored links between a number of family factors and two aspects of antisocial behavior among children, including aggression (e.g., fighting, temper tantrums, cruelty) and delinquency (e.g., lying, stealing, substance abuse). In separate structural models, parental ASPD was associated with increased aggression and delinquency among children. As in the Frick et al. (1992) study, these relations were not mediated by other factors (e.g., obstetric complications, parenting rejection, emotional warmth). Thus, the presence of ASPD among parents appears to have direct effects on child outcomes, over and above the contributions made by other variables.
Because antisocial behavior in children is often comorbid with attention-deficit/hyperactivity disorder (ADHD), a number of authors have investigated patterns of paternal psychopathology in samples of hyperactive children. Findings from these studies indicate that the effects of paternal ASPD on children’s behavior are specific to conduct problems and delinquency. For example, Pfiffner, McBurnett, Rathouz, and Judice (2005) compared families of children with ADHD, ADHD and ODD, or ADHD and CD, and found that fathers’ ASPD symptoms were associated specifically with conduct problems. For each additional symptom of ASPD among fathers, the odds of comorbid CD among their offspring increased by 1.4. Even when paternal depression was controlled, paternal ASPD predicted CD among children.
In addition to strong main effects of paternal ASPD on child outcomes, Pfiffner et al. (2005) documented a moderating effect of paternal ASPD. Fathers’ ASPD symptoms interacted with maternal parenting such that associations between maternal parenting and child CD were not significant when a father was high on ASPD symptoms, but were significant when a father was low on antisocial behaviors. As with the studies cited above, this finding suggests that paternal ASPD confers such strong risk for child CD that maternal parenting exerts minimal mollifying effects given an antisocial father. Consistent with such an interpretation, Beauchaine, Gartner, and Hagen (2000) reported attenuated sympathetic nervous system (SNS) tone, a consistent marker of delinquent tendencies (see Beauchaine et al., 2007; Crowell et al., 2006) among the inpatient offspring of incarcerated fathers, even for children who had not been reared in their fathers’ presence.
Links to child depression
As noted above, the majority of research addressing the impact of paternal antisocial behavior on children has focused on externalizing outcomes. In fact, almost no studies have assessed relations between paternal ASPD and child depression. Nevertheless, some evidence suggests that antisocial behavior among fathers is also associated with child internalizing psychopathology. As expected, Marmorstein, Malone, and Iacono (2004) found evidence of increased CD among children of fathers who met criteria for CD or ASPD. However, they also found elevated levels of major depression among these children. Because men with antisocial behavior frequently partner with women who are prone to depression (Kim-Cohen et al., 2005; Marmorstein et al., 2004), many of these children had mothers who were or had been depressed. Nevertheless, paternal antisocial behavior provided independent prediction to child CD and depression, over and above the effects of maternal psychopathology.
Maternal depression
Links to child conduct problems
Relations between maternal depression and child conduct problems are well documented (e.g., Boyle & Pickles, 1997; Kim-Cohen et al., 2005; Patterson, 1996). As outlined above, maternal depression provides independent prediction to both mood disorders and conduct problems among adolescents (Marmorstein & Iacono, 2004). Furthermore, maternal depression may interact with paternal psychopathology to predict especially poor adjustment outcomes among children (Conrad & Hammen, 1989). Given that depressed mothers often engage in assortative mating with antisocial males (Kim-Cohen et al., 2005; Marmorstein et al., 2004), their children may be placed in double jeopardy for psychiatric morbidity.
Despite clear links between maternal depression and externalizing behaviors among children, we are not aware of any studies in which the effects of different subtypes of maternal depression on child conduct problems have been evaluated. This is a potentially important oversight given findings indicating that melancholic depression represents a more severe variant of mood disorder with an especially virulent course. Probands suffer from melancholic depression if they meet criteria for a distinct quality of anhedonic mood. This includes failure to derive pleasure from all or nearly all activities and/or a lack of appetitive responding to usually pleasurable stimuli (American Psychiatric Association, 2000). Those who suffer from melancholia must also experience at least three of the following: (a) depressive symptoms that are usually worse in the morning, (b) early morning awakening, (c) psychomotor retardation, (d) weight loss, and/or (e) inappropriate guilt. Melancholic depression has been identified in children as young as preschool age (Luby, Mrakotsky, Heffelfinger, Brown, & Spitznagel, 2004) and confers especially high suicide risk among adults (e.g., Carroll, Greden, & Feinberg, 1980).
Taxometric analyses have identified melancholia as a discrete and more severe subtype of depression in both adolescent and adult samples (e.g., Ambrosini, Bennett, Cleland, & Haslam, 2002; Beach & Amir, 2003). Furthermore, evidence suggests that melancholia arises from different etiologic mechanisms than other forms of depression (see Beauchaine, 2003b; Beauchaine & Marsh, 2006; Leventhal & Rehm, 2005). Indeed, melancholic depression has been associated with both hypothalamic– pituitary–adrenal axis hyperactivity and alterations in 5-hydroxytryptamine 2a receptor density compared with nonmelancholic depression (e.g., Akin, Manier, Sanders-Bush, & Shelton, 2004; Dinan, O’Brien, Lavelle, & Scott, 2004). Elucidating the differential nature of risk conferred to children by melancholic versus nonmelancholic maternal depression is especially important given the elevated likelihood of mortality associated with the former (Carroll et al., 1980; Coryell & Schlesser, 2001). Thus, one of our objectives was to examine the strength of association between maternal melancholia and child conduct problems within our sample, and to evaluate possible potentiators and attenuators of risk.
Links to child depression
Associations between maternal depression and child depression are also well documented. Mood disorders aggregate strongly within families (e.g., Klein, Lewinsohn, Rhode, Seeley, & Shankman, 2003), and parental depression is the most robust predictor of depression in children (see Beardslee, Versage, & Gladstone, 1998). Evidence from a number of studies indicates that familial transmission occurs through both genetic and environmental mechanisms (e.g., Rende, Plomin, Reiss, & Hetherington, 1993). As with most psychiatric disorders, genetic influences on depression increase as children move into adolescence (Thapar & McGuffin, 1997). Nevertheless, unique environmental events often potentiate genetic risk for depression (Eaves et al., 1997). As with the literature addressing maternal depression and child conduct problems, we are not aware of any studies that have examined differential links between maternal melancholic and nonmelancholic depression and child depression. Two additional objectives of this study were to perform such an analysis, and to evaluate possible potentiators of risk for depression among participant children.
Temperamental Indices of Risk Potentiation and Resilience
Approach tendencies
Individual differences in approach and passive avoidance tendencies are core components of temperament that can interact with adverse environmental events to potentiate psychopathology (Clark, 2005; Sanson & Prior, 1999). Considerable evidence suggests that the relative strengths of these temperamental traits are rooted in distinct neurobiological substrates (e.g., Beauchaine, 2003; Brenner, Beauchaine, & Sylvers, 2005; Cloninger, Svrakic, & Przybeck, 1993; Corr, 2004; Gray & McNaughton, 2000). Neural pathways involved in appetitive behaviors have been established in a long tradition of research with animals, and more recently among humans using positron emission tomography and functional magnetic resonance imaging. These pathways include both the mesolimbic and mesocortical dopamine systems, which are strongly implicated in the development of impulse control disorders such as ADHD, CD, and substance dependencies (for a review, see Gatzke-Kopp & Beauchaine, in press). Several studies have indicated reduced activation in striatal regions and their projections to the anterior and prefrontal cortices during reward tasks among children and adolescents with ADHD and conduct problems (e.g., Bush et al., 1999; Durston et al., 2003; Vaidya et al., 1998). Hypoactivation within these structures, which are subsumed within the dopaminergic reward pathways, is consistent with sensation-seeking models of impulsivity, delinquency, and aggression.
At the autonomic nervous system level, this reward insensitivity is reflected in attenuated SNS-linked cardiac activity both at baseline and during incentives, which has been demonstrated in children with conduct problems ranging in age from preschool to adolescence (Beauchaine, 2003a; Beauchaine, Katkin, Strassberg, & Snarr, 2001; Beauchaine et al., 2007; Crowell et al., 2006). As we have described in detail elsewhere, SNS-linked cardiac activity, a peripheral index of central dopamine function under appropriate stimulus conditions, provides for noninvasive assessment of appetitive motivational tendencies (Brenner et al., 2005). In the present study, we used impedance cardiography to assess SNS-linked cardiac activity to incentives. The potentiating effects of reward insensitivity, defined as a lack of SNS response to incentives, were assessed by examining interactions between children’s SNS-linked cardiac activity and parental psychopathology in predicting child adjustment problems.
Passive avoidance tendencies
Neural pathways involved in passive avoidance learning and passive avoidance behaviors, which are linked closely with trait anxiety, are also well characterized (e.g., Corr, 2004; Gray & McNaughton, 2000). These pathways include the amygdala and the septohippocampal system, which is innervated by serotonergic projections of the raphe nucleus and noradrenergic projections of the locus coeruleus. Through induction of anxiety, these structures, often referred to collectively as the behavioral inhibition system (BIS), inhibit prepotent behaviors when impending punishment is anticipated. This has direct implications for both anxiety sensitivity and self-regulation (see, e.g., Beauchaine, 2001; Corr, 2004). Children and adolescents with deficiencies in impulse control also exhibit poor passive avoidance learning, and have difficulty inhibiting previously rewarded behaviors when contingent punishment cues are introduced (see Oosterlaan, Logan, & Sergeant, 1998). Presumably, punishment cues do not elicit sufficient anxiety to halt ongoing behavior among these children (e.g., Corr, 2004).
There is a long tradition of assessing individual differences in BIS activation using autonomic measures (e.g., Fowles, 1980). Baseline electrodermal responding (EDR), which indexes peripheral SNS activity, has long been associated with both state and trait anxiety (e.g., Beauchaine, 2001; Fowles, 2000; Katkin, 1965). Indeed, EDR lability is observed among those with psychological disorders characterized by excessive anxiety, whereas EDR hyporesponding has been observed repeatedly among delinquent and aggressive children, adolescents, and adults (e.g., Beauchaine et al., 2001; Crowell et al., 2006; Freedman, 1985; Gatzke-Kopp, Raine, Loeber, Stouthamer-Loeber, & Steinhauer, 2002; Loeber, 2004). We assessed the potentiating effects of electrodermal hypoactivity by evaluating interactions between children’s EDR and parental psychopathology in predicting child adjustment problems.
Negative emotionality
As noted above, self-regulation is also an important facet of temperament, with significant implications for psychological adjustment (Rothbart & Bates, 1998; Rothbart et al., 2000). An important component of self-regulation is the ability to modulate negative emotionality. Research spanning an impressively broad range of psychopathology, including both internalizing and externalizing psychiatric disorders, suggests that reductions in respiratory sinus arrhythmia (RSA), a peripheral index of parasympathetic nervous system (PNS)-linked cardiac activity, marks individual differences in negative emotionality (Beauchaine, 2001). Reduced RSA has been observed among both adolescents and adults with depression (Crowell et al., 2005; Rechlin, Weis, Spitzer, & Kaschka, 1994; Rottenberg, Wilhelm, Gross, & Gotlib, 2003), among patients with anxiety and panic disorders (Lyonfields, Borkovec, & Thayer, 1995; Thayer, Friedman, & Borkovec, 1996; Yeragani et al., 1993), among trait hostile adults (Sloan et al., 1994), and among both children and adolescents with conduct problems (Beauchaine et al., 2001, 2007; Crowell et al., 2006; Mezzacappa et al., 1997). Furthermore, several reports have suggested that heightened RSA predicts resilience among children exposed to adversity. For example, children with high RSA who witness marital conflict and hostility or are exposed to problem drinking by their parents appear to be buffered from the associated risk of developing both internalizing and externalizing behavior patterns (El-Sheikh, 2005; El-Sheikh, Harger, & Whitson, 2001; Katz & Gottman, 1995, 1997). RSA is also positively associated with children’s social engagement (Fox & Field, 1989), with teacher reports of social competence (Eisenberg et al., 1995), and with expressions of empathy toward others who are in distress (Fabes, Eisenberg, & Eisenbud, 1993). Taken together, these findings suggest that high RSA is associated with attenuated rates of psychopathology among at risk children. Following from this literature, we evaluated whether RSA served such a role for children in our sample.
Method
Participants
The sample consisted of 121 boys and 59 girls between the ages of 8 and 12 (mean age = 9.89, SD = 1.51). The racial/ethnic composition included 25 (13.9%) African Americans, 2 (1.1%) Asian Americans, 129 (71.7%) Caucasians, 10 (5.6%) Latinos/Latinas, 2 (1.1%) Native Americans, and 12 (6.7%) children of mixed or unspecified heritage. Children were accompanied by one biological parent, who was the mother in all but four cases. After obtaining institutional review board approval, participants were recruited from predominantly lower socioeconomic status (SES) neighborhoods in the greater Seattle metropolitan area through King County bus advertisements, local newspaper advertisements, community publications, direct mailings, flyers placed in community centers, and radio ads. Separate ads were used targeting children who were either “well adjusted,” “down or depressed,” or “experiencing behavior problems.” Ads were placed in English, Spanish, Vietnamese, Mandarin, and Korean. Each ad stated that parents and their child could earn up to $175 by participating in a study about children’s adjustment at the University of Washington. Median family income was $47,000, which was 33% below the median family income of $69,795 for the Seattle metropolitan area (United States Census Bureau, 2005).
Parents who responded to the ads completed a 20- to 30-min telephone screening interview with a trained research assistant who administered a computerized diagnostic interview including portions of the Child Symptom Inventory (CSI; Gadow & Sprafkin, 1997) and the Child Behavior Checklist (CBCL; Achenbach, 1991). The CSI yields both dimensional scores and diagnostic cutoffs for many DSM-IV disorders. Symptoms are rated on a 4-point scale (0 = never, 1 = sometimes, 2 = often, 3 = very often), with ratings of 2 or higher considered positive for a given diagnostic criterion. Sensitivity and specificity of the scales used in this study are adequate to excellent. Parents completed the CSI CD, ADHD, ODD, major depressive disorder (MDD), and dysthymia (DYS) scales. From the CBCL, parents completed the aggression, attention problems, and anxious/depressed subscales. Of the 445 parents who completed the phone interview, 210 (47.2%) were accepted into the study based on their CSI and CBCL profiles. Those who were not accepted failed to meet required cutoffs for the study groups (see below). Among those accepted, fully coded data from the first of three longitudinal assessment waves were available for 180 families, who are described herein. The remaining 30 families had not completed their lab visits at the time of data analysis, so they are not included.
Children were admitted into the study based on meeting criteria for one of four groups, as assessed during the structured phone interview. Children meeting CSI criteria for CD and/or ODD, but not for DYS or MDD, were placed into a conduct problems group (n = 36, 20% of sample; 78% male). Children meeting CSI criteria for DYS and/or MDD, but not CD or ODD were placed into a depression/dysthymia group (n = 24, 13.3% of sample; 63% male). Children meeting criteria for both the CP and DEP groups were placed in a comorbid group (n = 57, 31.7% of sample; 81% male). A control group (n = 63, 35% of sample; 51% male) was also formed, consisting of children who did not meet criteria for any disorder, and who did not exceed a T score of 60 on any CBCL scale. For purposes of this study, however, all data were analyzed using continuous scores of symptom severity rather than groupings. This decision was based on the many advantages of analyzing continuous variables, provided that assumptions of normality are met (see Beauchaine, 2003a; MacCallum, Zhang, Preacher, & Rucker, 2002). In the present case, all reported scales were characterized by acceptable values of both skew (≤1.02) and kurtosis (≤1.04).
Lab visit
Child
Children were seated in a sound-attenuated room that was monitored by a microphone and video camera. Cardiac and EDR data were collected while children sat alone for a 5-min baseline, followed by a task consisting of reward and nonreward trials. This task is described in detail by Iaboni, Douglas, and Ditto (1997) and Beauchaine et al. (2001). Briefly, large single-digit odd numbers were presented in random order on a screen in front of participants, slightly above eye level. Participants were required to use their dominant hand to press the corresponding number on a 10-key keypad mounted in front of them. They were then required to press the enter key to advance to the next stimulus. Following 2 min of practice, participants were paid $0.06 and heard a signal tone for each correct response during conditions of reward. Incorrect responses were not accompanied by monetary incentives or signal tones. During conditions of extinction, participants earned no money and heard no signal tone, regardless of whether their responses were correct or incorrect. The amount of money earned was displayed at all times in the upper right corner of the screen. In total, there were six 2-min blocks, each of which was followed by a 2-min rest period. The first three blocks consisted entirely of reward. The fourth block consisted of 30 s of reward and 90 s of extinction. The fifth block consisted of entirely reward. Finally, the sixth block consisted of 90 s of extinction followed by 30 s of reward. Children made correct responses 83.13% (SD = 17.83%) of the time with an average response time of 0.94 s (SD = 0.29 s). There were no group differences in performance. Following the task, participant children also completed the Children’s Depression Inventory (CDI; Kovacs, 1992), in addition to several other measures not reported in this study. The CDI provided an independent self-report measure of child depression, which was obtained because of low levels of agreement between parent and child reports of psychopathology, particularly for internalizing disorders (De Los Reyes & Kazdin, 2005).
Parent
While children completed the lab task, their participating parent was interviewed in a separate room. Parental psychopathology was assessed using the Structured Clinical Interview for DSM-IV, Nonpatient Version (SCID-NP; Spitzer, Williams, Gibbon, & First, 1992), which was administered by a graduate-level trained research assistant. After the SCID was finished, the participating parent completed the Family Interview for Genetics Studies (FIGS; Maxwell, 1992) to assess for psychopathology in the child’s first-degree relatives. The FIGS assesses depression, mania, substance use, and schizophrenia on Axis I, and schizoid, schizo-typal, paranoid, and antisocial personality disorders on Axis II. The participating parent was asked to report on all first-degree relatives of the child, including the other parent.
The decision to interview only one parent was dictated by pragmatic concerns. Among participant families, 52% did not have the father living at home. As expected, this percentage was highest among families of children with conduct problems. Previous studies have demonstrated that antisocial characteristics of children are higher in families where the father is not present in the home and cannot be recruited for research (Pfiffner, McBurnett, & Rathouz, 2001). Requiring father participation therefore biases samples toward lower severity. Accordingly, only one parent was required to participate. Because the mother was unlikely to have detailed knowledge of the father’s childhood behavior, the evidence of CD criterion for ASPD was waived, a procedure that is commonly used in family history studies (e.g., Barnow et al., 2005; Chronis et al., 2003). Using this method, 53 fathers were positive for ASPD. In addition, 91 mothers met lifetime criteria for depression or dysthymia.
Psychophysiological measures
RSA
Parasympathetic-linked cardiac activity was assessed by spectral analyzing the electrocardiographic R-wave time series using software developed by Richard Sloan and colleagues at Columbia University. PNS activity is confined to the high frequency band of the fast Fourier transformed time series (>0.15 Hz). The validity of RSA as an index of PNS-linked cardiac activity has been established using cholinergic blockade (see Berntson et al., 1997). High-frequency spectral densities were calculated in 30s epochs. As is customary when assessing RSA, all data were log transformed to obtain normal distributions.
Preejection period (PEP)
Sympathetic influences on heart rate were indexed by PEP, the time interval between the onset of left ventricular depolarization and ejection of blood into the aorta. The validity of PEP as an index of SNS-linked cardiac activity has been established via β-adrenergic blockade (see Sherwood et al., 1990). Greater SNS influences are represented by shorter PEPs (Sherwood, Allen, Obrist, & Langer, 1986). Both the electrocardiographic and impedance cardiographic signals were sampled at 1 kHz using an HIC 2000 Impedance Cardiograph (Chapel Hill, NC). PEP values were extracted by ensemble-averaging data in 30-s epochs using Bio-Impedance Technology’s CopWin software system (Chapel Hill, NC).
EDR
Electrodermal activity was assessed by measuring nonspecific fluctuations in skin conductance. Skin conductance signals were recorded using a Grass model 15LT Physiodata Amplifier System with a 15A12 DC amplifier (West Warwick, RI). Electrodermal signals were collected using two 0.8 cm2 silver/silver chloride electrodes with Parker Laboratories Signa Gel (Fairfield, NJ). The electrodes were secured to the thenar eminence on the participant’s nondominant hand using adhesive masking collars. The skin conductance signal was sampled at 1 kHz using the Grass Poly VIEW software system. Nonspecific skin conductance responses were scored as the number of fluctuations exceeding 0.05 μS.
Analytic Strategy
Resilience and resilience-related processes are suggested when the relation between a risk factor and an outcome differs as a function of a protective factor (see Luthar et al., 2000). In other words, protective factors moderate relations between exposure to adversity and adjustment. Evaluating the significance of a putative moderator is accomplished by regressing the focal outcome variable on the putative adversity variable, the putative protective factor, and the Adversity Variable × Protective Factor interaction. A resilience model is supported when the interaction term is significant, regardless of the significance of the main effects (see Baron & Kenny, 1986; Beauchaine & Mead, in press). In the present study, we were interested in evaluating potential protective factors (moderators) in attenuating relations between parent and child psychopathology. These included relations among (a) paternal antisocial behavior and child conduct problems, (b) paternal antisocial behavior and child depression, (c) maternal depression and child conduct problems, and (d) maternal depression and child depression.
Our list of putative moderators included (a) parental psychopathology, including both paternal ASPD and maternal melancholic depression; (b) baseline EDR, our psychophysiological marker of inhibition; (c) PEP during reward, our psychophysiological marker of reward insensitivity; and (d) baseline RSA, our psychophysiological marker of emotionality. Accordingly, regressions were computed in which the significance of each of these was tested as a possible moderator of the relation between parent and child psychopathology. Although main effects have no bearing on inferences drawn from resilience interactions (Baron & Kenny, 1986; Beauchaine & Mead, in press), we nevertheless report them for interested readers.
Results
Descriptive statistics
Descriptive statistics for participant parents and children are presented in Table 1. As expected given the high-risk nature of the sample, mean psychopathology scores were elevated on all measures. This is evident on the CBCL scales, where mean scores for the sample fell about 1.5 SD above national norms (i.e., T≈65). Nevertheless, given that children who were low on psychopathology were actively recruited, wide ranges of scores on all scales were observed.
Table 1.
Descriptive statistics for participant children and parents
| Variable | Mean | SD | Range |
|---|---|---|---|
| Child | |||
| CBCL attention problems T score | 66.1 | 12.8 | 50.0–95.0 |
| CBCL aggression T Score | 64.8 | 13.0 | 50.0–100.0 |
| CBCL anxious/ depressed T score | 65.5 | 12.2 | 50.0–93.0 |
| CSI conduct disorder symptoms | 3.8 | 3.8 | 0.0–21.0 |
| CSI inattention symptoms | 13.2 | 7.2 | 0.0–27.0 |
| CSI hyperactive symptoms | 10.3 | 7.4 | 0.0–27.0 |
| CSI oppositional defiant symptoms | 10.3 | 6.6 | 0.0–24.0 |
| CSI major depression symptoms | 4.4 | 4.8 | 0.0–25.0 |
| CSI dysthymia symptoms | 4.5 | 4.2 | 0.0–18.0 |
| CDI score | 6.2 | 6.2 | 0.0–33.0 |
| Baseline RSA (log[beats/min2/Hz]) | 9.2 | 1.2 | 6.3–12.0 |
| Baseline PEP (ms) | 102.4 | 18.2 | 64.0–140.0 |
| Baseline EDR (nonspecific fluctuations/min) | 5.0 | 2.4 | 0.0–22.0 |
| Parent | |||
| Mother SCID depression score | 19.3 | 5.8 | 11.0–29.0 |
| Mother SCID melancholia score | 10.9 | 3.5 | 6.0–18.0 |
| Father FIGS antisocial personality symptoms | 1.5 | 2.2 | 0.0–6.0 |
Note: CBCL, Child Behavior Checklist (Achenbach, 1991); CSI, Child Symptom Inventory (Gadow & Sprafkin, 1997); CDI, Children’s Depression Inventory (Kovacs, 1992); RSA, respiratory sinus arrhythmia; PEP, preejection period; EDR, electrodermal responding; SCID, Structured Clinical Interview for DSM-IV (Spitzer et al., 1992); FIGS, Family Interview for Genetic Studies (Maxwell, 1992).
In order to obtain a better understanding of the degree of resilience demonstrated by study participants, the number of children who scored at least 1.0 SD below the sample mean on each psychopathology outcome measure was determined. These outcomes included conduct problems, parent-report depression, and self-report depression (see below for details regarding the computation of each scale). Children who scored at least 1.0 SD below the sample mean included 32 (17.8%) for self-reported depression, 27 (15.0%) for parent-report depression, and 40 (22.2%) for conduct problems.
Moderation analyses
Parent reports of conduct problems
Results from the moderational analyses for parent reports of child conduct problems are reported in Table 2. In performing the regressions, a composite index of conduct problems was computed by first z scoring and then adding CSI CD symptoms (Gadow & Sprafkin, 1997), CSI oppositional defiant disorder symptoms, and CBCL aggression scores. Father antisocial behavior was indexed by the number of ASPD criteria endorsed on the FIGS. Because the SCID does not provide distinct scales for classifying subtypes of major depression, both melancholic and nonmelancholic symptoms were extracted and summed to form separate scales. Each symptom was rated on a severity index of 1−3, where 1 = the absence of the symptom and 3 = clinically significant impairment. Severity indices for melancholic and nonmelancholic symptoms were summed for each participant.
Table 2.
Regressions assessing potential moderators of parent-reported child conduct problems
| Main Effect |
Main Effect |
Predictor × Moderator Interaction |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | β | ta | η | Moderator | β | ta | η | β | ta | η |
| Paternal ASPD symptoms | 0.58 | 2.50** | .19 | Maternal melancholia | 0.16 | 1.68 | .13 | −0.34 | 1.40 | .11 |
| 0.49 | 4.45*** | .33 | EDR | 0.21 | 2.40* | .19 | −0.29 | 2.45** | .19 | |
| 0.12 | 1.22 | .12 | RSA | −0.16 | −1.67 | .17 | 0.36 | 3.75*** | .35 | |
| 0.28 | 3.51*** | .27 | ΔPEP | −0.04 | 0.11 | .01 | −0.05 | 0.63 | .05 | |
| Maternal melancholia | 0.08 | 0.96 | .07 | EDR | 0.05 | 0.57 | .04 | −0.31 | 1.10 | .09 |
| −0.09 | −0.18 | .02 | RSA | −0.23 | −0.83 | .07 | 0.21 | 0.37 | .03 | |
| 0.11 | 1.34 | .11 | ΔPEP | 0.07 | 0.23 | .02 | −0.04 | 0.02 | .01 | |
Note: Child conduct problems were indexed by summing participants’ z scores on the CSI conduct disorder, CSI oppositional defiant disorder, and CBCL aggression scales. CSI, Child Symptom Inventory (Gadow & Sprafkin, 1997); CBCL, Child Behavior Checklist (Achenbach, 1991); RSA, respiratory sinus arrhythmia; PEP, preejection period; EDR, electrodermal responding; ASPD, antisocial personality disorder.
N = 180. The degrees of freedom varied slightly across tests because of missing data.
p < .05.
p < .01.
p < .001.
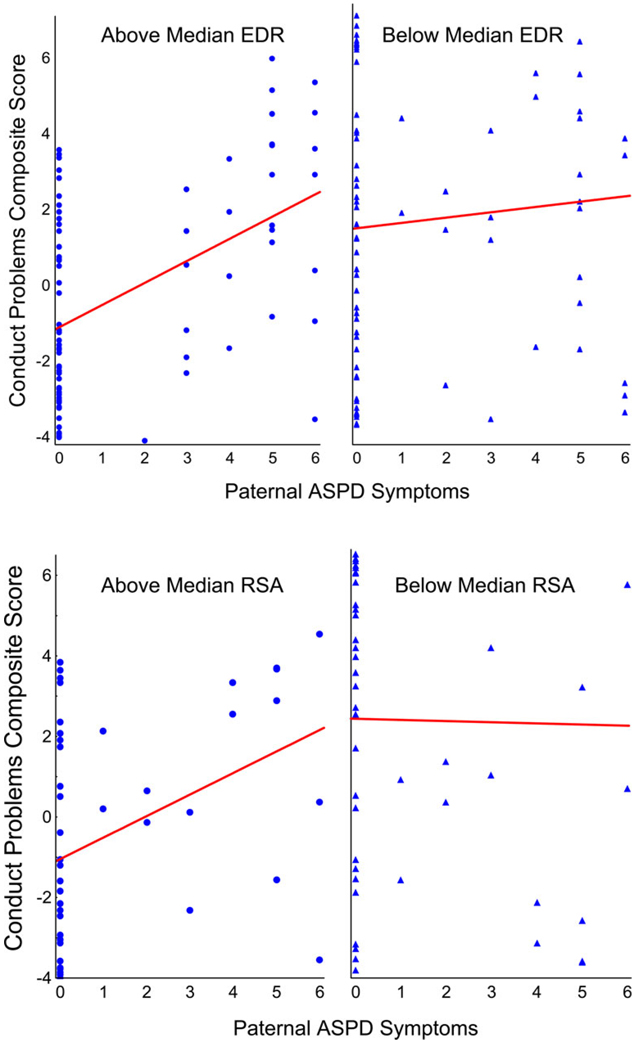
As indicated, both EDR and RSA moderated the relation between paternal ASPD symptoms and child conduct problems. These interactions are depicted in Figure 1. For children scoring above the sample median on baseline EDR, there was a significant relation between paternal ASPD and conduct problems (b = 0.49, p < .001). In contrast, there was no relation between paternal ASPD symptoms and conduct problems for children below the sample median on baseline EDR (b = 0.06, p = .47). These children tended to score high on conduct problems regardless of their father’s ASPD status.
Figure 1.
Relations between paternal antisocial personality disorder symptoms and conduct problems for (top) children above and below the sample median on baseline electrodermal responding and (bottom) children below and above the sample median on respiratory sinus arrhythmia. [A color version of this figure can be viewed online at www.journals.cambridge.org]
Similarly, for children scoring above the sample median on RSA, there was a significant relation between paternal ASPD and conduct problems (b = 0.32, p = .02). In contrast, there was no relation between paternal ASPD symptoms and conduct problems for children below the sample median on RSA (b = 20.02, p = .87). These children tended to score high on conduct problems regardless of their father’s ASPD status.
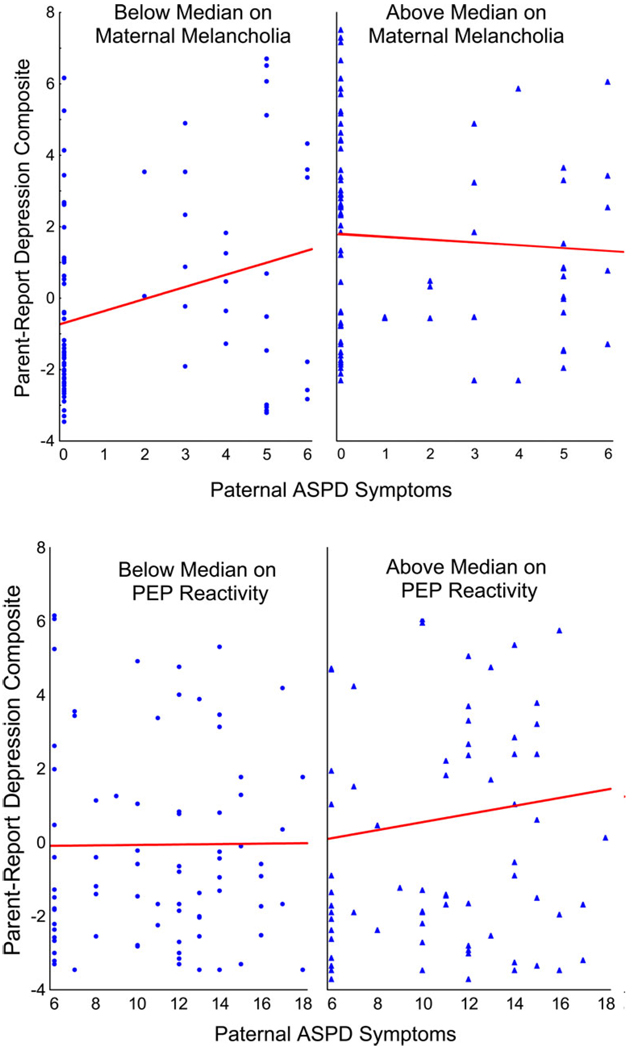
Parent reports of child depression
Results from the moderational analyses for parent reports of child depression appear in Table 3. In these regressions, a composite index of child depression was computed by first z scoring and then adding CBCL anxious/depressed, ASI major depression, and ASI dysthymia scores to form a parent-report depression construct. Because these measures are not well suited for assessing melancholia, subscales for different subtypes of child depression were not formed. As in the previous analyses, father antisocial behavior was indexed by the number of ASPD criteria endorsed on the FIGS, and maternal melancholia was indexed by the number of melancholic symptoms endorsed on the SCID. As indicated, both maternal melancholia and PEP reactivity to reward moderated the relation between paternal ASPD symptoms and child depression. These interactions are depicted in Figure 2. In families with mothers scoring below the sample median on melancholia, there was a significant relation between paternal ASPD symptoms and child depression (b = 0.34,p = .01). However, there was no such relation between paternal ASPD symptoms and child depression when mothers scored above the sample median on melancholia (b = −0.06, p = .41). Of note, no such moderational effect was found for nonmelancholic symptoms, where the interaction between paternal ASPD and maternal depression was nonsignificant (β = 0.16, p = .49).
Table 3.
Regressions assessing potential moderators of parent-reported child depression
| Main Effect |
Main Effect |
Predictor × Moderator Interaction |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | β | ta | η | Moderator | β | ta | η | β | ta | η |
| Paternal ASPD symptoms | 0.49 | 1.65 | .16 | Maternal melancholia | 0.24 | 2.09* | .19 | −0.50 | 2.59** | .24 |
| 0.01 | 0.13 | .01 | EDR | −0.05 | −0.67 | .05 | −0.14 | 0.95 | .08 | |
| 0.71 | 0.94 | .10 | RSA | −0.12 | −1.00 | .10 | −0.64 | 0.84 | .07 | |
| 0.13 | 1.58 | .13 | ΔPEP | −0.01 | −0.15 | .01 | −0.25 | 2.00* | .16 | |
| Maternal melancholia | 0.05 | 0.21 | .02 | EDR | −0.03 | −0.33 | .03 | 0.02 | 0.21 | .02 |
| −0.02 | −0.07 | .01 | RSA | −0.11 | −0.91 | .10 | 0.05 | 0.18 | .02 | |
| 0.06 | 0.74 | .06 | ΔPEP | −0.25 | −0.86 | .07 | 0.37 | 1.10 | .09 | |
Note: Child depression was indexed by summing participants’ z scores on the CSI major depression, CSI dysthymia, and CBCL anxious/depressed scales. CSI, Child Symptom Inventory (Gadow & Sprafkin, 1997); CBCL, Child Behavior Checklist (Achenbach, 1991); RSA, respiratory sinus arrhythmia; PEP, preejection period; EDR, electrodermal responding; ASPD, antisocial personality disorder.
N = 180. The degrees of freedom varied slightly across tests because of missing data.
p < .05.
p < .01.
Figure 2.
Relations between paternal antisocial personality disorder symptoms and parent-reported depression when mothers scored (top) below and above the sample median on melancholia and (bottom) below and above the sample mean on preejection period reactivity to reward. [A color version of this figure can be viewed online at www.journals.cambridge.org]
The PEP x Paternal ASPD Symptoms interaction revealed that among participants who were low on PEP reactivity, there was no relation between paternal ASPD symptoms and parent reports of depression (b = 0.01, p = .95). In contrast, paternal ASPD was related to parent reports of depression for children who exhibited high PEP reactivity to reward (i.e., PEP shortening), indicating SNS engagement (b = 0.29, p = .04). This interaction effect is summarized in Table 3 and depicted in Figure 2.
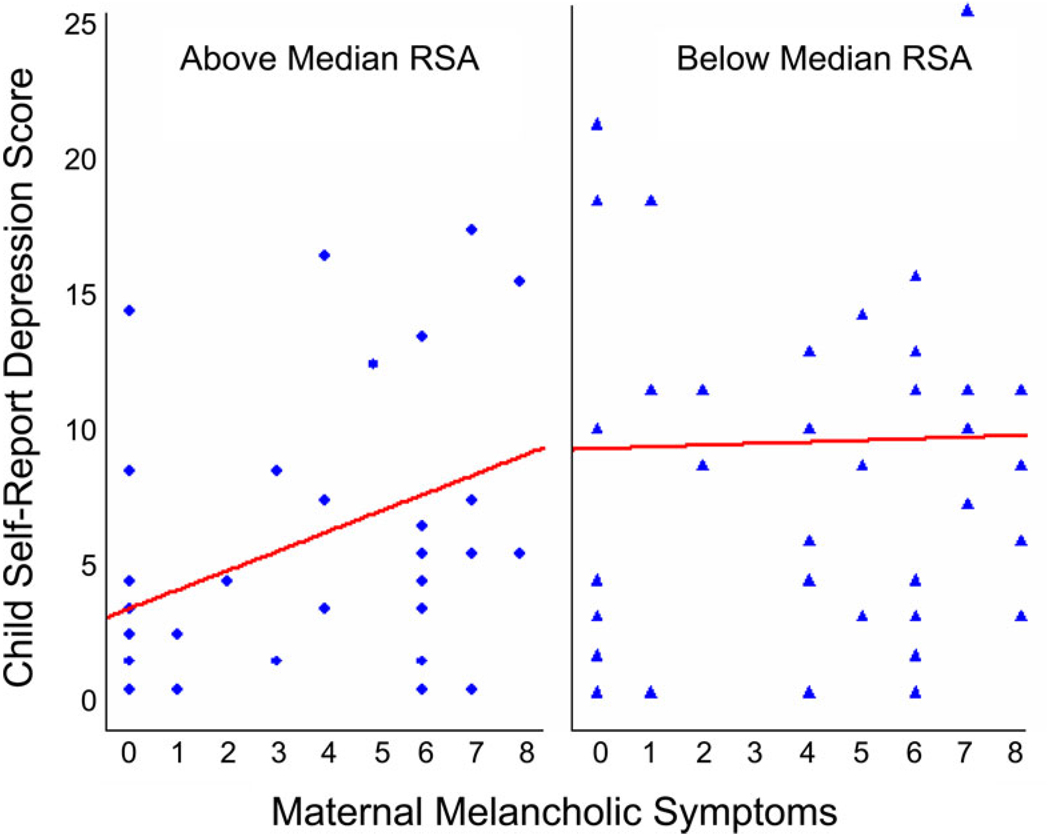
Self-reports of child depression
Results from the moderational analyses for self-reports of child depression appear in Table 4. In these regressions, child depression was indexed by the CDI. The only significant moderating effect was for RSA in the relation between maternal melancholia and child depression (see Figure 3). For children above the sample median on RSA, there was a significant relation between maternal melancholia and self-reported depression (b = 0.38, p < .01). However, no such relation was found for children low in RSA (b = 0.01, p = .87), who scored high on self-reported depression regardless of their mother’s melancholia score. Of note, no such moderating effect was found for nonmelancholic depression (β = 0.20, p = .24).
Table 4.
Regressions assessing potential moderators of self-reported child depression
| Main Effect |
Main Effect |
Predictor × Moderator Interaction |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | β | ta | η | Moderator | β | ta | η | β | ta | η |
| Paternal ASPD symptoms | −0.17 | 0.59 | .06 | Maternal melancholia | 0.26 | 2.24* | .21 | −0.16 | 0.56 | .04 |
| 0.03 | 0.19 | .02 | EDR | 0.01 | 0.01 | .01 | −0.00 | 0.02 | .01 | |
| 0.10 | 0.12 | .01 | RSA | −0.10 | −0.79 | .08 | 0.09 | 0.12 | .01 | |
| −0.04 | −0.37 | .04 | ΔPEP | 0.11 | 0.88 | .09 | 0.11 | 0.88 | .07 | |
| Maternal melancholia | 0.34 | 2.55** | .24 | EDR | 0.34 | 1.01 | .10 | −0.42 | 1.17 | .09 |
| 0.07 | 0.27 | .03 | RSA | −0.17 | −1.44 | .16 | 0.36 | 2.35** | .18 | |
| 0.23 | 2.28* | .23 | ΔPEP | −0.26 | −0.81 | .08 | 0.32 | 0.97 | .08 | |
Note: Child depression was indexed by the Children’s Depression Inventory (Kovacs, 1992). CBCL, Child Behavior Checklist (Achenbach, 1991); RSA, respiratory sinus arrhythmia; PEP, preejection period; EDR, electrodermal responding; ASPD, antisocial personality disorder.
N = 180. The degrees of freedom varied slightly across tests because of missing data.
p < .05.
p < .01.
Figure 3.
The relation between maternal melancholia and child depression for (left panel) children above the sample median on respiratory sinus arrhythmia (RSA) and (right panel) children below the sample median on RSA. As indicated by the regression lines, there is a strong relation between maternal melancholia and child depression for children high in RSA, yet there is no relation between maternal melancholia and child depression for children low in RSA. Note that there are many points of overlap because responses on both plotted variables were discrete. [A color version of this figure can be viewed online at www.journals.cambridge.org.]
Discussion
In this study, we examined the moderating effects of paternal ASPD, maternal melancholia, and several biological markers of temperament and emotionality on relations between parent and child psychopathology. Results from these analyses suggested several protective processes in which children recruited from low SES urban neighborhoods, most of whom suffered from significant internalizing and/or externalizing symptoms, exhibited better than expected outcomes, as assessed by psychopathology scores (Masten, Best, & Garmezy, 1990). Although any conclusions reached from these analyses are restricted by the cross-sectional nature of the data that were available, several of the findings are intriguing, and suggest possible avenues for future research. We discuss these findings in the sections that follow.
Child conduct problems
In our first set of analyses, which evaluated potential moderators of child conduct problem outcomes, we assessed EDR hypoactivity as a possible potentiator of risk. One of the most widely replicated findings in the child and adult psychopathology literatures is attenuated baseline EDR among aggressive and antisocial probands compared with controls (e.g., Beauchaine, 2001; Crowell et al., 2006; Gatzke-Kopp et al., 2002; Lorber, 2004). Rather than focusing on main effects, the approach typically followed in previous research, we sought to assess the moderating effect of EDR on the relation between paternal antisocial behavior and child conduct problems. These analyses uncovered an interaction between children’s EDR and paternal ASPD in predicting conduct problems. For children below the sample median on EDR, no relation between paternal ASPD symptoms and child conduct problems was observed. As a group, these children scored high on conduct problems regardless of their father’s level of ASPD. In contrast, a strong relation between paternal ASPD and child conduct problems was observed among children above the sample median on EDR. According to the nomenclature proposed by Luthar et al. (2000), this exemplifies a protective–reactive interaction. Children high in EDR, a peripheral marker of anxiety sensitivity, were protected from conduct problems, but less so the more antisocial their fathers were.
As discussed above, EDR nonresponding has been linked to difficulties with passive avoidance learning and problems with impulse control, functions subserved by serotonergic and noradrenergic pathways comprising the BIS. Indeed, numerous studies have indicated inverse relations between aggression and both serotonin and its metabolites (Kruesi et al., 1990; Oliver & van Oorschot, 2005). Similarly, Rogeness and colleagues have repeatedly found attenuated levels of plasma dopamine-beta-hydroxylase, a precursor of norepinephrine, among emotionally disturbed youth (Rogeness et al., 1988; Rogeness, Hernandez, Macedo, Suchakorn, & Hoppe, 1986). Furthermore, Gabel, Stadler, Bjorn, Shindledecker, and Bowden (1994) found that high sensation-seeking behavior was inversely correlated with plasma levels of 3-methoxy-4-hydroxyphenylglycol, a norepinephrine metabolite, among adolescent boys. Although EDR is far removed from the central nervous system substrates of impulsivity and aggression, our findings may suggest protective–reactive interactions for serotonergic and noradrenergic functioning in predicting child aggression from paternal ASPD.
Although it may be tempting to infer a genetic mechanism of protection from conduct problems given the role of EDR as a biological marker of trait anxiety, relations between genes and behavior are often moderated by environmental experiences. For example, polymorphisms in the monoamine oxidase A gene interact with adversity to predict antisocial behavior (Caspi et al., 2002). Because we did not collect data regarding traumatic or otherwise adverse experiences from our sample, we are not in a position to speculate about specific mechanisms through which resilience among children with high levels of EDR was conferred.
As with previous research addressing potential attenuators of risk for conduct problems among children of antisocial fathers (Barnow et al., 2005; Frick et al., 1992; Pfiffner et al., 2005), high levels of paternal ASPD outweighed the protective effects conferred by EDR lability among children. These results indicate that the influence of paternal ASPD on child externalizing outcomes is remarkably robust. Future research aimed at identifying environmental moderators of risk for conduct problems given paternal ASPD is therefore of utmost importance as we seek to prevent intergenerational transmission of this costly mental health outcome (Beauchaine, Webster-Stratton, & Reid, 2005; Moffitt et al., 2006).
A second protective–reactive interaction was found for RSA, which also moderated the relation between paternal ASPD symptoms and child conduct problems. Children high on RSA, a peripheral marker of emotional stability (Beauchaine, 2001; Beauchaine et al., 2007), were protected from conduct problems, but less so the more antisocial their fathers were. This provides yet another example of RSA as a protective factor. As noted above, high RSA among children marks protection from psychopathology following exposure to both marital conflict and problem drinking by parents, findings that extend to both internalizing and externalizing outcomes (El-Sheikh, 2005; El-Sheikh et al., 2001; Katz & Gottman, 1995, 1997). The protective effects of RSA are consistent with the growing literature linking PNS-linked cardiac control to effective emotion regulation strategies and social competencies (see Beauchaine, 2001; Eisenberg et al., 1995; Fabes et al., 1993; Fox & Field, 1989). To date, few if any protective factors have proven as robust as RSA in marking adjustment despite risk.
RSA is mediated by brainstem structures that are distinctly mammalian and have been linked to the evolution of social affiliative behaviors (Beauchaine et al., 2007; Porges, 1995, 1997). RSA is also influenced by frontal brain regions that play integral roles in executive functioning, long-term planning, and behavior regulation (e.g., Hansen, Johnsen, & Thayer, 2003). Behavior genetics studies have indicated that RSA is roughly 50% heritable and 50% environmentally determined (Kupper et al., 2005). This may imply that effective modulation of emotion, the behavioral trait most closely linked with RSA, could be affected by environmental interventions (see Beauchaine et al., 2007), thereby conferring protective effects on at risk children. We are currently evaluating this possibility in an intervention study with externalizing preschoolers.
Parent-report child depression
In our second set of analyses, we examined the possible moderating role of maternal melancholia on the relation between paternal ASPD and child depression. As noted above, Marmorstein et al. (2004) found that paternal antisocial behavior predicted child depression, over and above the effects of maternal depression. However, these authors did not examine this relation across subtypes of maternal depression. Our findings indicate that maternal melancholic symptoms in particular moderate the relation between paternal ASPD and child depression. For children whose mothers scored low on melancholia, we found a strong relation between paternal ASPD symptoms and child depression. In contrast, for children whose mothers scored high on melancholia, child depression scores were high and invariant of paternal ASPD. This represents another protective–reactive interaction. Low maternal melancholia appears to protect against child depression, yet this advantage is reduced when paternal ASPD is high.
It is important that no such relation was found for nonmelancholic maternal depression. As we have discussed elsewhere, melancholia is a particularly virulent form of mood disorder that is highly heritable and confers especially high risk for psychiatric mortality (Beauchaine & Marsh, 2006). Our results suggest that children of melancholic mothers are at high risk for depression themselves, regardless of paternal ASPD status. If these results are replicated, it may suggest that melancholia be evaluated in research examining risk and resilience among at-risk children.
An additional moderator of the relation between paternal ASPD and parent reports of child depression was PEP reactivity to reward. Low PEP reactivity indicates hyporesponding of the SNS to incentives, which has been demonstrated repeatedly as a main effect in children and adolescents with conduct problems, including those within this sample (Beauchaine et al., 2007). Nevertheless, we found a significant moderating effect of PEP reactivity in the relation between paternal ASPD and child depression. For children high in PEP reactivity, indicating a strong SNS response, risk for depression increased as paternal ASPD symptoms increased. In contrast, among children low in PEP reactivity, there was no relation between paternal ASPD symptoms and child depression. This suggests a protective role of low PEP reactivity among children with an antisocial father. These results demonstrate a protective–stabilizing interaction (Luthar et al., 2000) whereby low PEP reactivity confers a low rate of child depression despite increases in paternal ASPD symptoms.
This effect should be interpreted with caution, particularly given the modest effect size. Considering the number of tests conducted, it is possible that this interaction was arrived at by chance. We are therefore reluctant to speculate about neural mechanisms before replicating the effect in future waves of data collected from this sample, or in independent samples. Only one study to date has examined PEP in a depressed sample (Light, Kothandapani, & Allen, 1998). Results from this study indicated reduced PEP in depressed women at baseline, following a postural change, during an upsetting task, and during recovery compared with controls. However, no group differences in PEP reactivity to any condition were reported.
Self-report child depression
We also sought to evaluate the potential moderating effect of children’s RSA on the relation between maternal melancholia and child depression. In a previous analysis of a subset of these data reported elsewhere (Shannon et al., 2005), we found a significant relation between SCID-assessed maternal melancholic depression and CDI-assessed child depression, but not between maternal nonmelancholic depression and child depression. This finding was consistent with our hypothesis of a stronger genetic loading for melancholic versus non-melancholic forms of mood disturbance. More interesting for the present investigation, however, was the finding that the relation between maternal melancholia and child depression was moderated by children’s RSA. Specifically, for children above the sample median on RSA, there was a strong relation between maternal melancholia and child depression. In contrast, there was no relation between maternal melancholia and child depression for children low in RSA, who tended to score high on self-reported depression regardless of their mothers’ melancholia scores. This form of interaction reflects what Luthar et al. (2000) refer to as a protective but reactive moderator. High RSA among children confers protection from depression, but the level of protection varies as a function of maternal melancholia.
Implications for developmental psychopathology
At the broadest level, developmental psychopathology involves the study of how biological, psychological, and social factors influence the onset and course of individual patterns of adaptation and maladaptation, resulting in varying levels of adjustment (Cicchetti, 2006; Sroufe & Rutter, 1984). As such, it is important to uncover pathways that lead to positive adjustment despite significant exposure to adversity (Cicchetti, 1993). The study of resilience involves specifying interactive processes between individuals and their environments that result in both equifinal and multifinal outcomes.
In the current study, several moderating effects of parental psychopathology and child temperament on internalizing and externalizing outcomes among at-risk children were examined. By their very nature, interactive effects of resilience speak to the complexity of psychopathological development by revealing nonlinear associations between adjustment and risk, at different levels of risk and protective factors. Until recently, psychopathology researchers have focused almost exclusively on main effects of risk in predicting psychiatric morbidity. A major contribution of the developmental psychopathology perspective is the recognition that similar environmental experiences affect children differently, depending on a wide range of individual difference variables including temperament and emotionality. This recognition is reflected in a number of recent calls for more sophisticated evaluations of Gene × Environment interactions in studies of psychopathology (e.g., Moffitt, 2005; Moffitt et al., 2006; Rutter, 2002).
Despite the reduced statistical power associated with tests of interaction effects compared with tests of main effects (Aiken & West, 1991; Whisman & McClelland, 2005), we uncovered several moderators of outcome, discussed above. However, much more will be gleaned from this study following future waves of data collection that enable us to evaluate trajectories in both internalizing and externalizing symptoms over time. At present, we cannot offer statements regarding the development of psychopathology, or regarding moderators of psychopathological development. Nevertheless, findings that (a) electrodermal responding, a marker of trait anxiety, provides protection from conduct problems; (b) RSA, a marker of self-regulatory capabilities, provides protection from depression; and (c) maternal melancholia confers risk for depression, are all new and theoretically plausible. Longitudinal evaluation of these interactions will therefore be a high priority as we follow the sample into late adolescence.
From a developmental psychopathology perspective, longitudinal evaluations of adaptation and maladaptation are crucial. Individuals may move between states of pathological and normative functioning over time (Cicchetti, 2006; Sroufe, 1997). Furthermore, even within a psychopathological state, individuals may express adaptive and maladaptive behaviors that reveal a deeper understanding of the true components related to underlying psychopathology (Cicchetti, 2006). Although change may be possible at many points in development, such changes are constrained by prior adaptation (Sroufe, 1997). For example, as Moffitt (1993) has shown, individuals who engage early and often in defiant and aggressive behavior are likely to persist on a course toward antisocial behavior and criminality as adults, particularly without early intervention.
Resilience-focused interventions can be used to target both person-centered and environmental factors that lead to adaptive outcomes. Unlike deficit-driven intervention programs, resilience-based treatments seek to increase adaptive behavior, rather than decrease maladaptive behavior. Such increases in adaptive behavior then reduce maladaptive behavior (Smokowski, 1998). Masten (1994) has proposed four avenues for promoting resilience through interventions. These consist of (a) reducing vulnerability and risk, (b) reducing stressors, (c) increasing available resources, and (d) mobilizing protective processes.
One important contribution of resilience research toward designing interventions aimed at fostering adaptive outcomes is identifying processes related to risk potentiation and attenuation (Smokowski, 1998). In the current study, we recruited young children at high risk of developing stable patterns of conduct problems and/or depression. By examining psychophysiological moderators of risk, we identified subgroups of children who appear to be especially vulnerable to continued risk. These children may be targeted with additional intervention resources aimed at reducing this risk.
Additional considerations
Rater effects
Differences in both levels of psychopathology and interrelations among correlates of psychopathology are often observed across raters (for a recent review, see De Los Reyes & Kazdin, 2005). In the present study, moderators of child depression differed for mother reports and self-reports. Although we did not have multiple informants for other study constructs, these might also differ as a function of reporter. Previous studies have shown low agreement among mother reports and self-reports of adolescent symptoms (e.g., Andrews, Garrison, Jackson, Addy, & McKeown, 1993; Weissman et al., 1987). Typically, adolescents endorse a higher frequency and severity of internalizing symptoms than their mothers (Andrews et al., 1993). Thus, mothers tend to underreport adolescent symptoms that are either internalized or do not impinge upon others directly (e.g., Ivens & Rehm, 1988). Although mother–child agreement is often better for reports of externalizing behaviors, mothers may nevertheless underreport adolescent conduct problems because of their lack of knowledge regarding their child’s behavior. Furthermore, maladaptive behaviors may be underreported by youth because of shame, denial, or lack of trust regarding confidentiality.
In the current study, maternal melancholia and cardiac PEP moderated relations between mother reports of paternal ASPD and child depression. It is possible that mothers who experienced melancholia also rated their children as more depressed and/or rated their children’s fathers as higher on ASPD because of rater biases. Although this possibility cannot be eliminated, any such rater bias would have to be nonlinear to explain the observed interaction effect. For the psychophysiological variables such as PEP, rater biases across instruments cannot explain observed effects given the objective nature of the measures. A similar argument applies to RSA as a moderator of the relation between maternal melancholia and self-reported child depression. Thus, although we cannot explain the difference in moderators across informants for child depression, rater biases are unlikely to explain all of the effects.
It is also of potential concern whether maternal reports of father antisocial behavior were accurate. Mothers who have poor relationships with fathers may overreport negative aspects of the father’s behavior, whereas mothers who themselves exhibit antisocial behavior may underreport because of skewed perceptions of normality. However, previous research has indicated that results regarding father antisocial behavior remain largely unchanged, regardless of whether self-reports or partner reports are used (e.g., Pfiffner et al., 2005).
Interpretational ambiguities with moderators
In examining any moderational effect, it is important to consider that independent variables and moderators are always interchangeable statistically. Given that the criterion for moderation is a significant interaction between the independent variable and the moderator, deciding which variable to designate as the moderator depends entirely on conceptual considerations. For example, the finding that maternal melancholia moderates the relation between paternal ASPD and child depression could also be interpreted as suggesting that paternal ASPD moderates the relation between maternal melancholia and child depression; the significance of the interaction effect implies nothing about the precedence of variables or the direction of causality. In the present case, our findings suggest that both maternal melancholia and paternal ASPD potentiate child depression. However, neither variable should be granted a higher causal status in the absence of longitudinal research.
Characterizing resilience
Resilience is probably best defined as adaptive functioning across multiple life domains following significant exposure to adversity. Given this definition, studies of resilience should include indicators of social adjustment, academic achievement, and psychological well-being, among other variables (see Luthar, 2006). Because our study was not designed specifically to address resilience, we were unable identify children who may have demonstrated adaptive functioning in areas beyond psychopathology. Nevertheless, our findings indicate several markers of risk and protection that to date have not been reported. It is our hope that others will use these markers as components of broader assessment batteries in future research that examines resilience among children at risk for internalizing and externalizing psychopathology.
Acknowledgments
This paper was supported by Grant R01 MH63699 to Theodore P. Beauchaine from the National Institute of Mental Health. We express our gratitude to Sheila Crowell, Penny Marsh, and Hilary Mead for their invaluable contributions to this project.
Footnotes
Although other distinctions have been proposed to distinguish between vulnerabilities and risk factors, most of these have also been used inconsistently, and are subject to similar ambiguities when directions of causality are either unclear, polydirectional, and/or interactive. Our intent here is not to review all usages of the terms. Interested readers are referred to Luthar et al. (2000).
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Akin D, Manier DH, Sanders-Bush E, Shelton RC. Decreased serotonin 5-HT(2A) receptor-stimulated phosphoinositide signaling in fibroblasts from melancholic depressed patients. Neuropsychopharmacology. 2004;29:2081–2087. doi: 10.1038/sj.npp.1300505. [DOI] [PubMed] [Google Scholar]
- Ambrosini PJ, Bennett DS, Cleland CM, Haslam N. Taxonicity of adolescent melancholia: A categorical or dimensional construct? Journal of Psychiatric Research. 2002;36:247–256. doi: 10.1016/s0022-3956(02)00011-0. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 2000. Text Revision. [Google Scholar]
- Andrews VC, Garrison CZ, Jackson KL, Addy CL, McKeown RE. Mother—adolescent agreement on the symptoms and diagnoses of adolescent depression and conduct disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:731–738. doi: 10.1097/00004583-199307000-00005. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ. Depressive comorbidity in children and adolescents: Empirical, theoretical, and methodological issues. American Journal of Psychiatry. 1993;150:1779–1791. doi: 10.1176/ajp.150.12.1779. [DOI] [PubMed] [Google Scholar]
- Barnow S, Lucht M, Freyberger HJ. Correlates of aggressive and delinquent conduct problems in adolescence. Aggressive Behavior. 2005;31:24–39. [Google Scholar]
- Baron RM, Kenny D. The moderator- mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beach SRH, Amir N. Is depression taxonic, dimensional, or both? Journal of Abnormal Psychology. 2003;112:228–236. doi: 10.1037/0021-843x.112.2.228. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TR. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP. Vagal tone, development, and Gray’s motivational theory: Toward an integrated model of autonomic nervous system functioning in psychopathology. Development and Psychopathology. 2001;13:183–214. doi: 10.1017/s0954579401002012. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP. Autonomic substrates of heart rate reactivity in adolescent males with conduct disorder and/or attention-deficit/hyperactivity disorder. In: Prester TA, editor. Psychology of adolescents. New York: Nova Science; 2003a. pp. 133–145. [Google Scholar]
- Beauchaine TP. Taxometrics and developmental psychopathology. Development and Psychopathology. 2003b;15:501–527. doi: 10.1017/s0954579403000270. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Gartner J, Hagen B. Comorbid depression and heart rate variability as predictors of aggressive and hyperactive symptom responsiveness during inpatient treatment of conduct-disordered, ADHD boys. Aggressive Behavior. 2000;26:425–441. [Google Scholar]
- Beauchaine TP, Gatzke-Kopp L, Mead HK. Polyvagal theory and developmental psychopathology: Emotion dysregulation and conduct problems from preschool to adolescence. Biological Psychology. 2007;74:174–184. doi: 10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Katkin ES, Strassberg Z, Snarr J. Disinhibitory psychopathology in male adolescents: Discriminating conduct disorder from attention-deficit/hyperactivity disorder through concurrent assessment of multiple autonomic states. Journal of Abnormal Psychology. 2001;110:610–624. doi: 10.1037//0021-843x.110.4.610. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Marsh P. Taxometric methods: Enhancing early detection and prevention of psychopathology by identifying latent vulnerability traits. In: Cicchetti D, Cohen D, editors. Developmental psychopathology. 2nd ed. Hoboken, NJ: Wiley; 2006. pp. 931–967. [Google Scholar]
- Beauchaine TP, Mead HK. Some recommendations for testing mediating and moderating effects in treatment-outcome research. Journal of Psychological Research. in press. [Google Scholar]
- Beauchaine TP, Webster-Stratton C, Reid MJ. Mediators, moderators, and predictors of one-year outcomes among children treated for early-onset conduct problems: A latent growth curve analysis. Journal of Consulting and Clinical Psychology. 2005;73:371–388. doi: 10.1037/0022-006X.73.3.371. [DOI] [PubMed] [Google Scholar]
- Berntson GG, Bigger T, Eckberg DL, Grossman P, Kaufman PG, Malik M, et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology. 1997;34:623–648. doi: 10.1111/j.1469-8986.1997.tb02140.x. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza BM. Patterns of diagnostic comorbidity in a community sample of children aged 9 through 16 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:361–368. doi: 10.1097/00004583-199303000-00018. [DOI] [PubMed] [Google Scholar]
- Boyle MH, Pickles AR. Influence of maternal depressive symptoms on ratings of childhood behavior. Journal of Abnormal Child Psychology. 1997;25:399–412. doi: 10.1023/a:1025737124888. [DOI] [PubMed] [Google Scholar]
- Brenner SL, Beauchaine TP, Sylvers PD. A comparison of psychophysiological and self-report measures of BAS and BIS activation. Psychophysiology. 2005;42:108–115. doi: 10.1111/j.1469-8986.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- Buckner JC, Mezzacappa E, Beardslee WR. Characteristics of resilient youth living in poverty: The role of self-regulatory processes. Development and Psychopathology. 2003;15:139–162. doi: 10.1017/s0954579403000087. [DOI] [PubMed] [Google Scholar]
- Bush G, Frazier JA, Rauch SL, Seidman LJ, Whalen PJ, Jenike MA, et al. Anterior cingulated cortex dysfunction in attention-deficit/hyperactivity disorder revealed by fMRI and the counting Stroop. Biological Psychiatry. 1999;45:1542–1552. doi: 10.1016/s0006-3223(99)00083-9. [DOI] [PubMed] [Google Scholar]
- Carroll BJ, Greden JR, Feinberg M. Suicide, neuroendocrine dysfunction and CSF 5-HIAA concentrations in depression. In: Angrist B, editor. Proceedings of the 12th CINP Congress. Oxford: Pergamon Press; 1980. pp. 307–313. [Google Scholar]
- Caspi A, McClay J, Moffitt TE, Mill J, Martin J, Craig IW, et al. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297:851–854. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Lahey BB, Pelham WE, Kipp HL, Baumann BL, Lee SS. Psychopathology and substance abuse in parents of young children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:1424–1432. doi: 10.1097/00004583-200312000-00009. [DOI] [PubMed] [Google Scholar]
- Cicchetti D. Developmental psychopathology: Reactions, reflections, projections. Developmental Review. 1993;13:471–502. [Google Scholar]
- Cicchetti D. In: Developmental psychopathology: Vol. 1 Developmental psychopathology, theory and method. 2nd ed. Cicchetti D, Cohen DJ, editors. Hoboken, NJ: Wiley; 2006. pp. 1–23. [Google Scholar]
- Cicchetti D, Valentino K. An ecological-transactional perspective on child maltreatment: Failure of the average expectable environment and its influence on child development. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology Vol. 3 Risk, disorder, and adaptation. 2nd ed. Hoboken, NJ: Wiley; 2006. pp. 739–795. [Google Scholar]
- Cicchetti D, Walker EF. Stress and development: Biological and psychological consequences. Development and Psychopathology. 2001;13:413–418. [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Archives of General Psychiatry. 1993;50:975–990. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- Cole DA, Carpentieri S. Social status and the comorbidity of child depression and conduct disorder. Journal of Consulting and Clinical Psychology. 1990;58:748–757. doi: 10.1037//0022-006x.58.6.748. [DOI] [PubMed] [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Conrad M, Hammen C. Role of maternal depression in perceptions of child maladjustment. Journal of Consulting and Clinical Psychology. 1989;57:663–667. doi: 10.1037//0022-006x.57.5.663. [DOI] [PubMed] [Google Scholar]
- Corr PJ. Reinforcement sensitivity theory and personality. Neuroscience and Biobehavioral Reviews. 2004;28:317–332. doi: 10.1016/j.neubiorev.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Coryell W, Schlesser M. The dexamethasone suppression test and suicide prediction. American Journal of Psychiatry. 2001;158:748–753. doi: 10.1176/appi.ajp.158.5.748. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescents. Journal of Clinical Child Psychology. 1999;28:298–311. doi: 10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- Crowell S, Beauchaine TP, Gatzke-Kopp L, Sylvers P, Mead H, Chipman-Chacon J. Autonomic correlates of attention-deficit/hyperactivity disorder and oppositional defiant disorder in preschool children. Journal of Abnormal Psychology. 2006;115:174–178. doi: 10.1037/0021-843X.115.1.174. [DOI] [PubMed] [Google Scholar]
- Crowell S, Beauchaine TP, McCauley E, Smith C, Stevens AL, Sylvers P. Psychological, autonomic, and serotonergic correlates of parasuicidal behavior in adolescent girls. Development and Psychopathology. 2005;17:1105–1127. doi: 10.1017/s0954579405050522. [DOI] [PubMed] [Google Scholar]
- Curtis WJ, Cicchetti D. Moving research on resilience into the 21st century: Theoretical and methodological considerations in examining the biological contributors to resilience. Development and Psychopathology. 2003;15:773–810. doi: 10.1017/s0954579403000373. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Dinan TG, O’Brien S, Lavelle E, Scott LV. Further neuroendocrine evidence of enhanced vasopressin V3 receptor responses in melancholic depression. Psychological Medicine. 2004;34:169–172. doi: 10.1017/s0033291703001004. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Kavanagh K. Intervening in adolescent problem behavior: A family-centered approach. New York: Guilford Press; 2003. [Google Scholar]
- Drabick DAG, Beauchaine TP, Gadow KD, Carlson GA, Bromet EJ. Risk factors for conduct problems and depressive symptoms in a cohort of Ukrainian children. Journal of Clinical Child and Adolescent Psychology. 2006;35:244–252. doi: 10.1207/s15374424jccp3502_8. [DOI] [PubMed] [Google Scholar]
- Durston S, Tottenham NT, Thomas KM, Davidson MC, Eigsti I-M, Yang Y, et al. Differential patterns of striatal activation in young children with and without ADHD. Biological Psychiatry. 2003;53:871–878. doi: 10.1016/s0006-3223(02)01904-2. [DOI] [PubMed] [Google Scholar]
- Eaves LJ, Silberg JL, Maes HH, Simonoff E, Pickles A, Rutter M, et al. Genetics and developmental psychopathology: 2. The main effects of genes and environment on behavior problems in the Virginia Twin Study of Adolescent Behavioral Development. Journal of Child Psychology and Psychiatry. 1997;38:965–980. doi: 10.1111/j.1469-7610.1997.tb01614.x. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Murphy B, Maszk P, Smith M, Karbon M. The role of emotionality and regulation in children’s social functioning: A longitudinal study. Child Development. 1995;66:1360–1384. [PubMed] [Google Scholar]
- El-Sheikh M. Does poor vagal tone exacerbate child maladjustment in the context of parental problem drinking? A longitudinal examination. Journal of Abnormal Psychology. 2005;114:735–741. doi: 10.1037/0021-843X.114.4.735. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Harger J, Whitson SM. Exposure to interparental conflict and children’s adjustment and physical health: The moderating role of vagal tone. Child Development. 2001;72:1617–1636. doi: 10.1111/1467-8624.00369. [DOI] [PubMed] [Google Scholar]
- Fabes RA, Eisenberg N, Eisenbud L. Behavioral and physiological correlates of children’s reactions to others in distress. Developmental Psychology. 1993;29:655–663. [Google Scholar]
- Fleming JE, Boyle MH, Offord DR. The outcome of adolescent depression in the Ontario Child Health Study follow-up. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:28–33. doi: 10.1097/00004583-199301000-00005. [DOI] [PubMed] [Google Scholar]
- Fowles DC. The three arousal model: Implications of Gray’s two-factor learning theory for heart rate, electrodermal activity, and psychopathy. Psychophysiology. 1980;17:87–104. doi: 10.1111/j.1469-8986.1980.tb00117.x. [DOI] [PubMed] [Google Scholar]
- Fowles DC. Electrodermal hyporeactivity and antisocial behavior: Does anxiety mediate the relationship? Journal of Affective Disorders. 2000;61:177–189. doi: 10.1016/s0165-0327(00)00336-0. [DOI] [PubMed] [Google Scholar]
- Fox NA, Field TM. Individual differences in preschool entry behavior. Journal of Applied Developmental Psychology. 1989;10:527–540. [Google Scholar]
- Frick PJ, Lahey BB, Loeber R, Stouthamer-Loeber M, Christ MG, Hanson K. Familial risk factors to oppositional defiant disorder and conduct disorder: Parental psychopathology and maternal parenting. Journal of Consulting and Clinical Psychology. 1992;60:49–55. doi: 10.1037//0022-006x.60.1.49. [DOI] [PubMed] [Google Scholar]
- Freedman RR. Psychophysiological factors in panic disorder. Psychopathology. 1985;17:66–73. doi: 10.1159/000284079. [DOI] [PubMed] [Google Scholar]
- Gabel S, Stadler J, Bjorn J, Shindledecker R, Bowden CL. Sensation seeking in psychiatrically disturbed youth: Relationship to biochemical parameters and behavior problems. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:123–129. doi: 10.1097/00004583-199401000-00016. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J. Adolescent Symptom Inventory 4 Screening manual. Stony Brook, NY: Checkmate Plus; 1997. [Google Scholar]
- Garmezy N, Masten AS, Tellegen A. The study of stress and competence in children: A building block for developmental psychopathology. Child Development. 1984;55:97–111. [PubMed] [Google Scholar]
- Gatzke-Kopp L, Beauchaine TP. Central nervous system substrates of impulsivity: Implications for the development of attention-deficit/hyperactivity disorder and conduct disorder. In: Coch D, Dawson G, Fischer K, editors. Human behavior and the developing brain: Atypical development. New York: Guilford Press; 2007. pp. 239–263. [Google Scholar]
- Gatzke-Kopp LM, Raine A, Loeber R, Stouthamer-Loeber M, Steinhauer SR. Serious delinquent behavior, sensation seeking, and electrodermal arousal. Journal of Abnormal Child Psychology. 2002;30:477–486. doi: 10.1023/a:1019816930615. [DOI] [PubMed] [Google Scholar]
- Gray JA, McNaughton N. The neuropsychology of anxiety. 2nd ed. New York: Oxford University Press; 2000. [Google Scholar]
- Gunnar MR, Vazquez DM. Low cortisol and a flattening of the expected daytime rhythm: Potential indices of risk in human development. Development and Psychopathology. 2001;13:516–538. doi: 10.1017/s0954579401003066. [DOI] [PubMed] [Google Scholar]
- Hansen AL, Johnsen BH, Thayer JF. Vagal influence on working memory and attention. International Journal of Psychophysiology. 2003;48:263–274. doi: 10.1016/s0167-8760(03)00073-4. [DOI] [PubMed] [Google Scholar]
- Hewitt JK, Silberg JL, Rutter M, Simonoff E, Meyer JM, Maes H, et al. Genetics and developmental psychopathology: 1. Phenotypic assessment in the Virginia twin study of adolescent behavioral development. Journal of Child Psychology and Psychiatry. 1997;38:943–963. doi: 10.1111/j.1469-7610.1997.tb01613.x. [DOI] [PubMed] [Google Scholar]
- Iaboni F, Douglas V, Ditto B. Psychophysiological response of ADHD children to reward and extinction. Psychophysiology. 1997;34:116–123. doi: 10.1111/j.1469-8986.1997.tb02422.x. [DOI] [PubMed] [Google Scholar]
- Ivens C, Rehm L. Assessment of childhood depression: correspondence between reports by child, mother, and father. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;6:738–741. doi: 10.1097/00004583-198811000-00012. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Caspi A, Moffitt TE, Dodge KA, Rutter M, Taylor A, et al. Nature × nurture: Genetic vulnerabilities interact with physical maltreatment to promote conduct problems. Development and Psychopathology. 2005;17:67–84. doi: 10.1017/s0954579405050042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashani JH, Manning GW, McKnew DH, Cytryn L, Simonds JF, Wooderson PC. Depression among incarcerated delinquents. Psychiatry Research. 1980;3:185–191. doi: 10.1016/0165-1781(80)90035-9. [DOI] [PubMed] [Google Scholar]
- Katkin ES. Relationship between manifest anxiety and two indices of autonomic response to stress. Journal of Personality and Social Psychology. 1965;2:324–333. doi: 10.1037/h0022303. [DOI] [PubMed] [Google Scholar]
- Katz LF, Gottman JM. Vagal tone protects children from marital conflict. Development and Psychopathology. 1995;7:83–92. [Google Scholar]
- Katz LF, Gottman JM. Buffering children from marital conflict and dissolution. Journal of Clinical Child Psychology. 1997;26:157–171. doi: 10.1207/s15374424jccp2602_4. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Moffitt, T E, Taylor A, Pawlby SJ, Caspi A. Maternal depression and children’s antisocial behavior. Archives of General Psychiatry. 2005;62:173–181. doi: 10.1001/archpsyc.62.2.173. [DOI] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Rhode P, Seeley JR, Shankman SA. Family study of co-morbidity between major depressive disorder and anxiety disorders. Psychological Medicine. 2003;33:703–714. doi: 10.1017/s0033291703007487. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory. Niagara Falls, NY: Multi-Health Systems; 1992. [Google Scholar]
- Kruesi MJP, Rapoport JL, Hamburger S, Hibbs E, Potter WZ, Lenane M, et al. Cerebrospinal fluid monoamine metabolites, aggression, and impulsivity in disruptive behavior disorders of children and adolescents. Archives of General Psychiatry. 1990;47:419–426. doi: 10.1001/archpsyc.1990.01810170019003. [DOI] [PubMed] [Google Scholar]
- Kupper N, Willemsen G, Posthuma D, De Boer D, Boomsma DI, De Geus EJC. A genetic analysis of ambulatory cardiorespiratory coupling. Psychophysiology. 2005;42:202–212. doi: 10.1111/j.1469-8986.2005.00276.x. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Rehm LP. The empirical status of melancholia: Implications for psychology. Clinical Psychology Review. 2005;25:25–44. doi: 10.1016/j.cpr.2004.09.001. [DOI] [PubMed] [Google Scholar]
- Light KC, Kothandapani RV, Allen MT. Enhanced cardiovascular and catecholamine responses in women with depressive symptoms. International Journal of Psychophysiology. 1998;28:157–166. doi: 10.1016/s0167-8760(97)00093-7. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO. Comorbidity between and within childhood externalizing and internalizing disorders: Reflections and directions. Journal of Abnormal Child Psychology. 2003;31:285–291. doi: 10.1023/a:1023229529866. [DOI] [PubMed] [Google Scholar]
- Lorber MF. Psychophysiology of aggression, psychopathy, and conduct problems: A meta-analysis. Psychological Bulletin. 2004;130:531–552. doi: 10.1037/0033-2909.130.4.531. [DOI] [PubMed] [Google Scholar]
- Luby JL, Mrakotsky C, Heffelfinger A, Brown K, Spitznagel E. Characteristics of depressed preschoolers with and without anhedonia: Evidence for a melancholic depressive subtype in young children. American Journal of Psychiatry. 2004;161:1998–2004. doi: 10.1176/appi.ajp.161.11.1998. [DOI] [PubMed] [Google Scholar]
- Luthar SS. Resilience in development: A synthesis of research across five decades. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 3. Risk, disorder, and adaptation. 2nd ed. Hoboken, NJ: Wiley; 2006. pp. 739–795. [Google Scholar]
- Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Development. 2000;71:543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam DR, Caspi A, Moffitt TE, Wikström PH, Loeber R, Novak S. The interaction between impulsivity and neighborhood context on offending: The effects of impulsivity are stronger in poorer neighborhoods. Journal of Abnormal Psychology. 2000;109:563–574. doi: 10.1037//0021-843x.109.4.563. [DOI] [PubMed] [Google Scholar]
- Lyonfields JD, Borkovec TD, Thayer JF. Vagal tone in generalized anxiety disorder and the effects of aversive imagery and worrisome thinking. Behavior Therapy. 1995;26:457–466. [Google Scholar]
- MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. Psychological Methods. 2002;7:19–40. doi: 10.1037/1082-989x.7.1.19. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG. Major depression and conduct disorder in youth: Associations with parental psychopathology and parent-child conflict. Journal of Child Psychology and Psychiatry. 2004;45:377–386. doi: 10.1111/j.1469-7610.2004.00228.x. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Malone SM, Iacono WG. Psychiatric disorders among offspring of depressed mothers: Associations with paternal psychopathology. American Journal of Psychiatry. 2004;161:1588–1594. doi: 10.1176/appi.ajp.161.9.1588. [DOI] [PubMed] [Google Scholar]
- Masten A. Resilience in individual development: Successful adaptation despite risk and adversity. In: Wang MC, Gordon EW, editors. Educational resilience in inner-city America: Challenges and prospects. Hillsdale, NJ: Erlbaum; 1994. pp. 3–25. [Google Scholar]
- Masten A. Ordinary magic: Resilience processes in development. American Psychologist. 2001;56:227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- Masten A, Best K, Garmezy N. Resilience and development: Contributions from the study of children who overcome adversity. Development and Psychopathology. 1990;2:425–444. [Google Scholar]
- Maxwell ME. Family interview for genetic studies. Washington, DC: National Institute of Mental Health, Clinical Neurogenetic Branch, Intramural Research Program; 1992. [Google Scholar]
- Mezzacappa E, Tremblay RE, Kindlon D, Saul JP, Arseneault L, Seguin J, et al. Anxiety, antisocial behavior, and heart rate regulation in adolescent males. Journal of Child Psychology and Psychiatry. 1997;38:457–469. doi: 10.1111/j.1469-7610.1997.tb01531.x. [DOI] [PubMed] [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course persistent antisocial behavior: A developmental taxonomy. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Moffitt TE. A new look at behavioral genetics in developmental psychopathology: Gene-environment interplay in antisocial behaviors. Psychological Bulletin. 2005;131:533–554. doi: 10.1037/0033-2909.131.4.533. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Rutter M. Measured gene-environment interactions in psychopathology: Concepts, research strategies, and implications for research, intervention, and public understanding of genetics. Perspectives on Psychological Science. 2006;1:5–27. doi: 10.1111/j.1745-6916.2006.00002.x. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, McGuire S, Reiss D, Hetherington EM, Plomin R. Co-occurrence of depressive symptoms and antisocial behavior in adolescence: A common genetic liability. Journal of Abnormal Psychology. 1998;107:27–37. doi: 10.1037//0021-843x.107.1.27. [DOI] [PubMed] [Google Scholar]
- Oliver B, van Oorschot R. 5-HT1B receptors and aggression: A review. European Journal of Pharmacology. 2005;526:207–217. doi: 10.1016/j.ejphar.2005.09.066. [DOI] [PubMed] [Google Scholar]
- Oosterlaan J, Logan GD, Sergeant JA. Response inhibition in AD/HD, CD, comorbid AD/ HD + CD, anxious, and control children: A meta-analysis of studies with the stop task. Journal of Child Psychology and Psychiatry. 1998;39:411–425. [PubMed] [Google Scholar]
- Orr SP, Metzger LJ, Lasko NB, Macklin ML, Hu FB, Shalev AY, et al. Physiologic responses to sudden, loud tones in monozygotic twins discordant for combat exposure: Association with posttraumatic stress disorder. Archives of General Psychiatry. 2003;60:283–288. doi: 10.1001/archpsyc.60.3.283. [DOI] [PubMed] [Google Scholar]
- Patterson GR. Some characteristics of a developmental theory for early onset delinquency. In: Lenzenweger MF, Haugaard JJ, editors. Frontiers of developmental psychopathology. New York: Oxford University Press; 1996. pp. 81–124. [Google Scholar]
- Pfiffner LJ, McBurnett K, Rathouz PJ. Father absences and familial antisocial characteristics. Journal of Abnormal Child Psychology. 2001;29:357–367. doi: 10.1023/a:1010421301435. [DOI] [PubMed] [Google Scholar]
- Pfiffner LJ, McBurnett K, Rathouz PJ, Judice S. Family correlates of oppositional and conduct disorders in children with attention deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2005;33:551–563. doi: 10.1007/s10802-005-6737-4. [DOI] [PubMed] [Google Scholar]
- Phares V, Compas BE. The role of fathers in child and adolescent psychopathology: Make room for daddy. Psychological Bulletin. 1992;111:387–412. doi: 10.1037/0033-2909.111.3.387. [DOI] [PubMed] [Google Scholar]
- Pliszka SR, Sherman JO, Barrow MV, Irick S. Affective disorder in juvenile offenders: A preliminary study. American Journal of Psychiatry. 2000;157:130–132. doi: 10.1176/ajp.157.1.130. [DOI] [PubMed] [Google Scholar]
- Porges SW. Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology. 1995;32:301–318. doi: 10.1111/j.1469-8986.1995.tb01213.x. [DOI] [PubMed] [Google Scholar]
- Porges SW. Emotion: An evolutionary by-product of the neural regulation of the autonomic nervous system. Annals of the New York Academy of Sciences. 1997;807:62–77. doi: 10.1111/j.1749-6632.1997.tb51913.x. [DOI] [PubMed] [Google Scholar]
- Raine A, Venables PH, Dalais C, Mellingen K, Reynolds C, Mednick SA. Early educational and health enrichment at age 3–5 years is associated with increased autonomic and central nervous system arousal and orienting at age 11 years: Evidence from the Mauritius Child Health Project. Psychophysiology. 2001;38:254–266. [PubMed] [Google Scholar]
- Rapp LA, Wodarski JS. The comorbidity of conduct disorder and depression in adolescents: A comprehensive interpersonal treatment technology. Family Therapy. 1997;24:81–100. [Google Scholar]
- Rechlin T, Weis M, Spitzer A, Kaschka WP. Are affective disorders associated with alterations of heart rate variability? Journal of Affective Disorders. 1994;32:271–275. doi: 10.1016/0165-0327(94)90091-4. [DOI] [PubMed] [Google Scholar]
- Rende RD, Plomin R, Reiss D, Hetherington EM. Genetic and environmental influences on depressive symptomotology in adolescence: Individual differences and extreme scores. Journal of Child Psychology and Psychiatry. 1993;8:1387–1398. doi: 10.1111/j.1469-7610.1993.tb02097.x. [DOI] [PubMed] [Google Scholar]
- Riggs PD, Baker S, Mikulich SK, Young SE, Crowley TJ. Depression in substance-dependent delinquents. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:764–771. doi: 10.1097/00004583-199506000-00017. [DOI] [PubMed] [Google Scholar]
- Rogeness GA, Hernandez JM, Macedo CA, Suchakorn AA, Hoppe SK. Near-zero dopamine-b-hydroxylase and conduct disorder in emotionally disturbed boys. Journal of the American Academy of Child Psychiatry. 1986;25:521–527. doi: 10.1016/s0002-7138(10)60012-x. [DOI] [PubMed] [Google Scholar]
- Rogeness GA, Maas JW, Javors MA, Macedo CA, Harris WR, Hoppe SK. Diagnoses, catecholamine metabolism, and plasma dopamine-β-hydroxylase. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;27:121–125. doi: 10.1097/00004583-198801000-00019. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Bates JE. Temperament. In: Damond W, editor. Handbook of child psychology: Vol. 3. Social, emotional, and personality development. New York: Wiley; 1998. [Google Scholar]
- Rothbart MK, Evans DE, Ahadi SA. Temperament and personality: Origins and outcomes. Journal of Personality and Social Psychology. 2000;78:122–135. doi: 10.1037//0022-3514.78.1.122. [DOI] [PubMed] [Google Scholar]
- Rottenberg J, Wilhelm FH, Gross JJ, Gotlib IH. Vagal rebound during resolution of tearful crying among depressed and nondepressed individuals. Psychophysiology. 2003;40:1–6. doi: 10.1111/1469-8986.00001. [DOI] [PubMed] [Google Scholar]
- Rutter M. The interplay of nature, nurture, and developmental influences: The challenge ahead for mental health. Archives of General Psychiatry. 2002;59:996–1000. doi: 10.1001/archpsyc.59.11.996. [DOI] [PubMed] [Google Scholar]
- Sanson A, Prior M. Quay HC, Hogan AE. Handbook of disruptive behavior disorders. New York: Kluwer Academic/Plenum Press; 1999. Temperament and behavioral precursors to oppositional defiant disorder and conduct disorder. [Google Scholar]
- Seeger G, Schloss P, Schmidt MH, Ru¨ter-Jungfleisch A, Henn FA. Gene-environment interaction in hyperkinetic conduct disorder (HD + CD) as indicated by season of birth variations in dopamine receptor (DRD4) gene polymorphism. Neuroscience Letters. 2004;366:282–286. doi: 10.1016/j.neulet.2004.05.049. [DOI] [PubMed] [Google Scholar]
- Shannon KE, Beauchaine TP, Gatzke-Kopp LM, Brenner SL, Crowell SE, Mead HK, et al. Respiratory sinus arrhythmia moderates the relation between maternal melancholia and child depression. Psychophysiology. 2005;42:S115. [Google Scholar]
- Sherwood A, Allen MT, Fahrenberg J, Kelsey RM, Lovallo WR, van Doornen LJP. Committee report: Methodological guidelines for impedance cardiography. Psychophysiology. 1990;27:1–23. doi: 10.1111/j.1469-8986.1990.tb02171.x. [DOI] [PubMed] [Google Scholar]
- Sherwood A, Allen MT, Obrist PA, Langer AW. Evaluation of beta-adrenergic influences on cardiovascular and metabolic adjustments to physical and psychological stress. Psychophysiology. 1986;23:89–104. doi: 10.1111/j.1469-8986.1986.tb00602.x. [DOI] [PubMed] [Google Scholar]
- Sloan RP, Shapiro PA, Bigger JT, Bagiella M, Steinman RC, Gorman JM. Cardiac autonomic control and hostility in healthy subjects. American Journal of Cardiology. 1994;74:298–300. doi: 10.1016/0002-9149(94)90382-4. [DOI] [PubMed] [Google Scholar]
- Smokowski PR. Prevention and intervention strategies for promoting resilience in disadvantaged children. The Social Science Review. 1998;72:337–364. [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID) I: History, rationale, and description. Archives of General Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Sroufe LA. Psychopathology as an outcome of development. Development and Psychopathology. 1997;9:251–268. doi: 10.1017/s0954579497002046. [DOI] [PubMed] [Google Scholar]
- Sroufe LA, Rutter M. The domain of developmental psychopathology. Child Development. 1984;55:17–29. [PubMed] [Google Scholar]
- Stein MB, Jang KL, Taylor S, Vernon PA, Livesley WJ. Genetic and environmental influences on trauma exposure and posttraumatic stress disorder symptoms: A twin study. American Journal of Psychiatry. 2002;159:1675–1681. doi: 10.1176/appi.ajp.159.10.1675. [DOI] [PubMed] [Google Scholar]
- Thapar A, McGuffin P. Anxiety and depressive symptoms in childhood: A genetic study of comorbidity. Journal of Child Psychology and Psychiatry. 1997;38:651–656. doi: 10.1111/j.1469-7610.1997.tb01692.x. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Friedman BH, Borkovec TD. Autonomic characteristics of generalized anxiety disorder and worry. Biological Psychiatry. 1996;39:255–266. doi: 10.1016/0006-3223(95)00136-0. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. [Retrieved September 4, 2006];2005 American Community Survey data profile highlights. 2005 from http://factfinder.census.gov.
- Vaidya CJ, Austin G, Kirkorian G, Ridlehuber HW, Desmond JE, Glover GH, et al. Selective effects of methylphenidate in attention deficit hyperactivity disorder: A functional magnetic resonance study. Proceedings of the National Academy of Sciences USA. 1998;95:14494–14499. doi: 10.1073/pnas.95.24.14494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Warner V, John K, Prusoff BA, Merikangas KR, et al. Assessing psychiatric disorders in children: Discrepancies between mothers and children’s report. Archives of General Psychiatry. 1987;44:747–753. doi: 10.1001/archpsyc.1987.01800200075011. [DOI] [PubMed] [Google Scholar]
- Whisman MA, McClelland GH. Designing, testing, and interpreting interactions and moderator effects in family research. Journal of Family Psychology. 2005;19:111–120. doi: 10.1037/0893-3200.19.1.111. [DOI] [PubMed] [Google Scholar]
- Whitmore EA, Mikulich SK, Thompson LL, Riggs PD, Aarons GA, Crowley TJ. Influences on adolescent substance dependence: Conduct disorder, depression, attention deficit hyperactivity disorder, and gender. Drug and Alcohol Dependence. 1997;47:87–97. doi: 10.1016/s0376-8716(97)00074-4. [DOI] [PubMed] [Google Scholar]
- Woodward SA, Lenzenweger MF, Kagan J, Snidman N, Arcus D. Taxonic structure of infant reactivity: Evidence from a taxometric perspective. Psychological Science. 2000;11:296–301. doi: 10.1111/1467-9280.00259. [DOI] [PubMed] [Google Scholar]
- Yeragani VK, Pohl R, Berger R, Balon R, Ramesh C, Glitz D, et al. Decreased heart rate variability in panic disorder patients: A study of power-spectral analysis of heart rate. Psychiatry Research. 1993;46:89–103. doi: 10.1016/0165-1781(93)90011-5. [DOI] [PubMed] [Google Scholar]
- Zoccolillo M. Co-occurrence of conduct disorder and its adult outcomes with depressive and anxiety disorders: A review. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:547–556. doi: 10.1097/00004583-199205000-00024. [DOI] [PubMed] [Google Scholar]