Abstract
Objective
To examine for differences in and predictors of health value/utility scores in adolescents with or without inflammatory bowel disease (IBD).
Study design
Adolescents with IBD and healthy controls were interviewed in an academic health center. We collected socio-demographic data and we measured health status; personal, family, and social characteristics; and spiritual well-being. We assessed time tradeoff (TTO) and standard gamble (SG) utility scores for current health. We performed bivariate and multivariable analyses using utility scores as outcomes.
Results
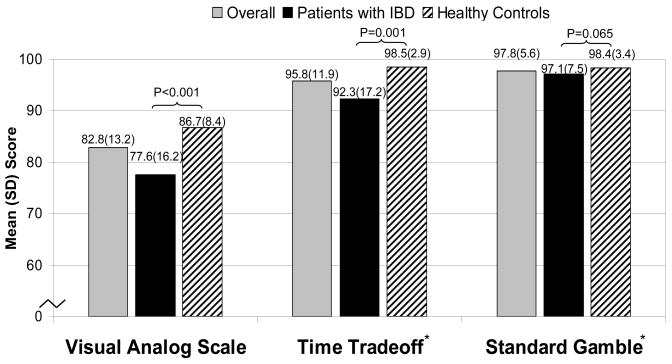
67 patients with IBD and 88 healthy controls 11 to 19 years of age participated. Among subjects with IBD, mean (SD) TTO scores were 0.92 (0.17) and mean (SD) SG scores were 0.97 (0.07). Among healthy controls, mean (SD) TTO scores were 0.99 (0.03) and mean (SD) SG scores were 0.98 (0.03). TTO scores were significantly lower (p=0.001) and SG scores trended lower (p=0.065) in patients with IBD when compared with healthy controls. In multivariable analyses controlling for IBD status, poorer emotional functioning and spiritual well-being were associated with lower TTO (R2=0.17) and lower SG (R2=0.22) scores.
Conclusion
Direct utility assessment in adolescents with or without IBD is feasible and may be used to assess outcomes. Adolescents with IBD value their health state highly, although less so than healthy controls. Emotional functioning and spiritual well-being appear to influence utility scores most strongly.
Keywords: adolescence, inflammatory bowel disease, health status, quality of life, outcome assessment (health care)
INTRODUCTION
Chronic illnesses such as inflammatory bowel disease (IBD) may be especially problematic for adolescents, who are already subject to rapid psychosocial transitions as a normal part of development. Truancy, social isolation, and behavior problems are common, and family dynamics can be affected by home-schooling, financial stresses, and forced parental career changes. 3–5 Because such factors affect many facets of patients’ lives, a broad-based multidisciplinary approach to assess and improve health-related quality of life (HRQOL) is paramount.
HRQOL may be assessed by 2 fundamentally different approaches: (1) health status measurement and (2) health value assessment. 6 In general, health status measures describe a person’s functioning in one or more specific domains such as physical and psychological functioning. Health status instruments have been used in pediatrics to monitor populations, to describe the natural history of disease, and to assess outcomes of interventions. 6–8 In contrast, health values (also known as preferences or utilities) ascertain the overall desirability of health states through one’s willingness to undergo risky treatments or sacrifice life expectancy in order to improve health. 6, 7, 9 Utility scores are most commonly used to adjust length of life for quality of life in calculating quality-adjusted life years (QALYs) for decision and cost-effectiveness analysis, which in turn are methods used to inform individual- or population-level medical decision-making and health policy decisions. 6, 7, 9 Previous investigations in adults have shown that utilities may reflect a broader domain than the health state per se and may be influenced by a number of factors, including personality traits, health status, social factors, and spiritual well-being.
Although utilities for health states have been elicited for many adult populations with or without chronic illness, only rarely have health values been derived directly from adolescents 10, 11, and never from adolescents with IBD. Moreover, extremely little is known regarding which factors are most important in determining values for health states in adolescents in general. We therefore conducted a study to elicit and characterize utilities from adolescents with IBD and to compare their utilities with those of a healthy control group. The objectives of this study were: 1) to investigate the feasibility of assessing health values in adolescents with IBD and in a control group of adolescents from the general population; 2) to examine differences in health values and other characteristics in adolescents with IBD vs. healthy adolescents; and 3) to evaluate relationships in both groups of adolescents between health values and socio-demographics; health status; personal, family, and social characteristics; and spiritual well-being.
METHODS
Study Population
We recruited patients with IBD and healthy control subjects 11–19 years of age from Cincinnati Children’s Hospital Medical Center and the University Hospital in Cincinnati, OH. Adolescents with any chronic psychiatric or medical illness or disability were excluded from the control group, with the exception of those having well-controlled attention deficit hyperactivity disorder (ADHD) or mild intermittent asthma. Due to their high prevalence in the general population, we allowed subjects with intermittent asthma (as opposed to persistent) or well-controlled ADHD to participate. Patients/parents were asked to self-define their asthma or ADHD severity. Patients with IBD and healthy subjects were recruited at their clinic visits, by telephone, or by advertisement. Informed consent and assent were obtained from all subjects and their families. The Institutional Review Boards at the participating centers approved the study. Two trained interviewers with extensive experience in assessing HRQOL (SNS, MSY) conducted interviews after clinic appointments or at pre-arranged times between October 2005 and April 2007. The questionnaire took approximately 50 minutes to complete on average. On the occasions that questions arose regarding the survey, the interviewer (SNS, MSY) was available to help clarify them.
Outcome Measures
We elicited values for subjects’ current health by using U-Maker software. 12 We first asked subjects to rate their current health on a visual analog scale (VAS), anchored by dead (0) and best possible health (100). The VAS is a rating scale and not a true utility measure because it does not involve considerations of risks or life expectancy trade-offs. Moreover, because there are no risks or tradeoffs, VAS ratings are generally relatively lower than utilities. Two assessment techniques were used to derive utilities for current health: 1) the time tradeoff (TTO); and 2) the standard gamble (SG). 9 The TTO approach assesses how much if any life expectancy the subject is willing to give up in exchange for living with the best possible health. The life expectancy of patients with IBD is reported to be similar to that of the general population. 13 Thus, we estimated remaining life expectancy both for adolescents with IBD and for healthy controls to be 60 years. 14 The SG assesses how a great a risk of the worst possible state of health (dead), if any, one is willing to accept in order to have the best possible health. Both the TTO and SG are scaled from dead (0.0) to best possible health (1.0), with a higher value representing a more desirable health state (less willingness to trade time or take a risk of dying). 6, 9, 15 For example, if a subject were willing to give up 20% of her remaining life expectancy in exchange for best possible health, the TTO utility would equal 0.80 (1.00 − 0.20 = 0.80). If she were willing to risk a 10% chance of the worst possible state of health (dead) in order to have a chance at best possible health, her SG utility would equal 0.90 (1.00 − 0.10 = 0.90).
Independent Measures
Demographics
We collected data regarding age, sex, race/ethnicity, maternal education, paternal education, and religious affiliation.
Clinical Data
Time since IBD diagnosis was obtained from patients, and patients’ type of IBD was obtained through chart review. In order to assess disease severity for both ulcerative colitis and Crohn’s Disease on the same scale, we used the modified version of the Clinical Score developed by Lloyd-Still and Green. 16, 17 This instrument ranks the disease severity based on objective laboratory and clinical exam findings; and the overall clinical score ranges from 11–85 points with lower scores representing more severe disease. Under a severity classification system, a score of ≥75 indicates inactive disease; a score of 55–74 indicates mild disease; a score of 35–54 indicates moderate disease; and a score of <35 indicates severe disease. 16
Health Status and General Health Perceptions
The PedsQL is an instrument developed and validated solely on the basis of the quality of life concerns of children and adolescents with or without chronic illness. 18, 19 The PedsQL™ 4.0 Generic Core Scales take approximately 4 minutes to complete and are designed to enable comparisons across patients with chronic conditions and healthy populations and to monitor change over time. The adolescent version of the PedsQL consists of 23 core items that assess 4 dimensions: physical functioning, emotional functioning, social functioning, and school functioning. Each subscale is scored from 0–100 so that higher scores indicate better functional status.
We used the 12-item scale from the Child Health Questionnaire to assess general health perceptions. 20 This scale assesses perceptions about one’s past health, current health, and prospects for future health, as well as susceptibility to illness. The scale is scored from 0 (worst general health perceptions) to 100 (best general health perceptions).
Personal Characteristics
Self Esteem
We used the 10-item Rosenberg Global Self-esteem Measure to assess self esteem. 21 Scores range from 0 (lowest self esteem) to 6 (highest).
Self Efficacy
Self efficacy describes one’s appraisal of whether he or she is capable of effectively reaching targeted goals. We used the 12-item General Self Efficacy Scale, on which scores range from 12 (lowest self efficacy) to 60 (highest). 22
Coping
We used the Kidcope to measure the frequency of positive and negative coping behaviors. 23 The Kidcope is a 10-item questionnaire, with each item assessing 1 of 10 coping strategies classified by 2 factors: Negative Coping (distraction, social withdrawal, self-criticism, blaming others, wishful thinking, resignation, and negative emotional regulation) and Positive Coping (cognitive restructuring, problem-solving, social support, and positive emotional regulation). Scores for Positive Coping range from 4 (lowest frequency) to 16 (highest frequency), and scores for Negative Coping range from 7 (highest frequency) to 28 (lowest frequency).
Stress
To examine overall life stress, we used the Perceived Stress Scale, a 10-item instrument measuring the degree to which life situations are appraised as stressful. 24 Assessment is based on a 5-point Likert scale and scored from 0–40, with higher scores representing less overall life stress.
Family and Social Characteristics
Family Competence
We used the Family Awareness Scale to assess family dynamics and competence. 25 Possible scores range from 12 (poorest family dynamics) to 108 (best).
Social Support
In order to assess social support outside of the family structure, we used the Social Support for Adolescents Scale (range 21 [least support] to 63 [most support]). 26 This scale captures social support from family, friends, peers, teachers, etc.
Spiritual Well-Being
Spirituality is defined as an individual’s sense of purpose/meaning and personal connectedness to the divine or the truth. 27 Because greater spiritual well-being has been shown to be associated with better health outcomes in a number of studies, 28–33 we administered the 10-item version of the Spiritual Well-Being Scale (range 10 [worst] to 50 [best]). 34, 35 Representative items include “I have a personally meaningful relationship with a Higher Power.” “I believe there is some real purpose for my life.” Responses are given on a 5-point Likert scale: “Strongly Agree; Agree; Neither Agree nor Disagree; Disagree; and Strongly Disagree.”
Statistical Analysis
All analyses were performed by using SAS software, version 9.1 (SAS Institute, Inc., Cary, NC). Descriptive statistics included means and standard deviations. In order to facilitate comparisons between utilities and other variables, we normalized the TTO and SG scores to a 0 to 100 scale. Pearson and Spearman correlations, the t-test, and the Kruskal-Wallis test, as appropriate, were used to perform bivariate analyses. For our analysis, for those scores statistically significantly different between the IBD group and the control group, we inferred clinically important differences by using standardized effect sizes. [(mean score Control Group − mean score IBD Group)/SD Control Group]. 36 As proposed by Samsa and others, an effect size of 0.80 or greater indicates a large clinical difference, an effect size of 0.50 – 0.79 indicates a moderate difference, and an effect size of 0.20 – 0.49 indicates a small difference between groups. We performed separate multivariable linear regressions with backward elimination to determine significant predictors of VAS ratings and TTO and SG utility scores in all subjects. Conceptually, and based on information from adult populations, we felt that having a chronic illness would influence how one valued one’s state of health, so in the final models, we controlled for whether a subject did or did not have IBD. Candidate variables included socio-demographic variables; health status; health perceptions; personal, family, and social characteristics; and spiritual well-being. Those variables significantly associated with VAS, TTO, or SG scores at p<0.15 in bivariate analyses were entered into the respective multivariable models.
RESULTS
Sixty-seven adolescents with IBD and 88 adolescent controls completed the interview (Table I). All of the subjects appeared to understand the survey and completed the questionnaire, with exception of 1 subject who did not complete a portion due to time constraints. As such, we included that individual’s responses only in bivariate analyses of variables for which the subject provided answers. Of the controls, 3 reported a history of intermittent asthma and 1 reported a history of well-controlled ADHD. Of patients with IBD, 52 (78%) had Crohn’s disease, 13 (19%) had ulcerative colitis, and 2 (3%) had “indeterminate disease” or “other.” The mean (SD) time since diagnosis was 3.1 (2.5) years. Of the patients interviewed with IBD, mean (SD) Lloyd-Still and Green clinical severity scores were 63.6 (13.4; range 34–85), with the possible range being 11 (most severe) to 85 (inactive disease). Under the severity classification system, 20 (30%) patients had inactive disease, 26 (39%) had mild disease, 20 (30%) had moderate disease, and 1 (2%) had severe disease.
Table 1.
Demographic Characteristics
| Variable | Overall (N=155) | IBD (N=67) | Controls (N=88) |
|---|---|---|---|
| Mean (SD) age, yrs | 15.1 (2.0) | 15.5 (2.1)* | 14.8 (1.9) |
| Male, N (%) | 80 (51.6) | 30 (44.8) | 50 (56.8) |
| White, N (%) | 121 (78.1) | 53 (79.1) | 68 (77.3) |
| Highest median parental education level† | College | College | College |
| Christian, N (%) | 128 (82.6) | 60 (89.6) | 68 (77.3) |
IBD: inflammatory bowel disease
p<0.05 for IBD vs. controls;
indicates education level of the more highly educated parent
Differences Between Adolescents with IBD vs. Healthy Controls
Health Status
Adolescents with IBD reported significantly poorer general health perceptions and physical functioning than did healthy adolescents. However, emotional, social, and school functioning scores were not significantly different between the 2 groups (Table II).
Table 2.
Health Status and Other Characteristics
| Variable | Overall (N=155) | IBD (N=67) | Controls (N=88) |
|---|---|---|---|
| PedsQL Physical Functioning, mean (SD) | 83.2 (15.0) | 77.4 (18.6)* | 87.6 (9.5) |
| PedsQL Emotional Functioning, mean (SD) | 73.5 (17.2) | 72.2 (19.1) | 74.5 (15.6) |
| PedsQL Social Functioning, mean (SD) | 85.6 (14.0) | 85.7 (15.3) | 85.6 (13.1) |
| PedsQL School Functioning, mean (SD) | 72.9 (17.1) | 70.2 (19.4) | 75.0 (15.0) |
| General Health Perceptions, mean (SD) | 64.7 (20.0) | 52.1 (21.0)* | 74.4 (12.5) |
| Rosenberg Global Self-esteem Measure, mean (SD) | 3.7 (0.7) | 3.7 (0.8) | 3.7 (0.6) |
| General Self-Efficacy Scale, mean (SD) | 46.1 (6.7) | 45.0 (6.9) | 47.0 (6.4) |
| Perceived Stress Scale, mean (SD) | 33.9 (6.2) | 31.5 (6.1)* | 35.8 (5.7) |
| Kidcope Positive Coping, mean (SD) | 11.5 (2.3) | 11.2 (2.4) | 11.8 (2.2) |
| Kidcope Negative Coping, mean (SD) | 20.2 (3.1) | 20.5 (3.0) | 20.0 (3.2) |
| Social Support for Adolescents Scale, mean (SD) | 45.0 (5.7) | 46.0 (6.3) | 44.3 (5.1) |
| Family Awareness Scale, mean (SD) | 70.7 (15.2) | 72.8 (14.4) | 69.1 (15.6) |
| Spiritual Well Being, mean (SD) | 40.3 (6.3) | 40.6 (6.8) | 40.1 (5.9) |
IBD: inflammatory bowel disease
p<0.05 for IBD vs. controls; statistical results were the same after controlling for demographics (age, race, sex)
Personal, Family, Social, and Spiritual Well-being Characteristics
Adolescents with IBD reported greater overall stress in their lives, but, on average, all other personal, family, social, and spiritual well-being characteristics were similar to those of healthy adolescents (Table II).
Health Values
Visual Analog Scale Scores
Adolescents with IBD reported approximately a mean (SD) health rating that was 9.2 (12.4) points lower when compared with health ratings of healthy peers (p<0.0001; Figure). In patients with IBD, disease severity correlated moderately with the VAS (r = 0.35).
Time Tradeoff Utilities
Adolescents with IBD reported TTO utilities for their current health that were, on average, 6.2 (11.6) points (normalized to a 0 to 100 scale) lower than TTO utilities of healthy peers (p=0.001; Figure). That is, given an estimated remaining life expectancy of 60 years, adolescents with IBD were willing to trade on average 4.6 years of life expectancy (=60 years × [100.0 − 92.3]/100) for best possible health, whereas healthy adolescents were willing to trade on average only 0.9 years (=60 years × [100.0 − 98.5]/100) of life expectancy for best possible health. In patients with IBD, disease severity correlated fairly with TTO scores (r = 0.23).
Standard Gamble Utilities
Adolescents with IBD reported a SG utility that was, on average, 1.4 (5.6) points lower for their current health (normalized to a 0 to 100 scale) when compared with SG utilities of healthy peers. That is, patients with IBD would be willing to incur, on average, up to a 2.9% risk of death in exchange for best possible health, and healthy adolescents would be willing to incur up to a 1.6% risk. Although the difference was not statistically significant, there was a trend (p=0.065) towards lower SG utilities in adolescents with IBD. In patients with IBD, disease severity correlated fairly with SG scores (r = 0.19).
Clinically Important Differences
There were large differences in effect sizes in PedsQL Physical Functioning (effect size=1.07), general health perceptions (1.78), VAS (1.08), and TTO (2.14) scores. The effect sizes were moderate for perceived stress (0.75), and small for the SG (0.38). For those domains, differences were clinically significant, although the magnitude of effect ranged from small to large.
Predictors of Health Value Scores Among All Patients
Visual Analog Scale Scores
In bivariate analyses of data from all study patients, higher VAS ratings were significantly associated (p<0.05) with being male; with being younger; with having better physical, emotional, social, and school functioning; with having better general health perceptions; with having greater self-esteem and self-efficacy; with having lower levels of negative coping and life stress; and with having greater levels of spiritual well-being. In multivariable analyses controlling for IBD status, higher VAS ratings were associated with better physical functioning and better general health perceptions (R2 = 0.52; Table III).
Table 3.
Multivariable Predictors of Health Value Scores
| Outcome Measure | Significant Multivariable Predictors* | β-Coefficient | P-Value | R2 |
|---|---|---|---|---|
| Visual analog scale | Physical Functioning | 0.29 | < 0.0001 | 0.52 |
| score | General Health Perceptions | 0.33 | < 0.0001 | |
|
| ||||
| Time tradeoff | Emotional Functioning | 0.13 | 0.018 | 0.17 |
| score† | Spiritual Well-being | 0.44 | 0.003 | |
|
| ||||
| Standard gamble | Emotional Functioning | 0.10 | < 0.0001 | 0.22 |
| score† | Spiritual Well-being | 0.26 | 0.0001 | |
Controlling for inflammatory bowel disease status
Normalized to a 0–100 scale
Time Tradeoff Utilities
In bivariate analyses, higher TTO utilities were significantly associated (p<0.05) with better physical and emotional functioning and general health perceptions; greater self efficacy and positive coping; less life stress; and greater spiritual well-being. In multivariable analyses controlling for IBD status, higher TTO utility scores were associated with better emotional functioning and greater spiritual well-being (R2 = 0.17; Table III).
Standard Gamble Utilities
In bivariate analyses, higher SG utilities were significantly associated (p<0.05) with better physical and emotional functioning and general health perceptions; greater self esteem; less life stress; and greater spiritual well-being. In multivariable analyses controlling for IBD status, higher SG utility scores were associated with better emotional functioning and greater spiritual well-being (R2 = 0.22; Table III).
DISCUSSION
Adolescent patients with IBD live with a chronic, often unpredictable illness and endure the side effects of potent treatments and procedures. Beyond the physical impact of IBD, patients may experience difficulties in emotional, behavioral, and social dimensions of HRQOL. Children with IBD have been shown to have relatively high rates of mood problems and anxiety 37–40, although objective measures of disease appear to be inconsistently related to their psychological and behavioral outcomes. 41, 42 Although IBD may restrict participation in social activities in young patients with IBD, they appear to be able to develop and maintain close peer relationships. 43
On the other hand, utilities have never been directly elicited from adolescents with IBD. Our aims, therefore, were to investigate the feasibility of assessing health values in adolescents with IBD; to compare health values of adolescents with vs. without IBD; and to examine whether individual, family, social, and spiritual well-being characteristics – factors that may make young patients resilient in the face of stress such as chronic illness – influence health values of adolescents living with IBD and of their peers. 44–47
First, adolescents with IBD and their control counterparts appeared to understand health value assessment procedures. Furthermore, we found that in general, patients with IBD have similar personal traits and family and social functioning when compared with healthy adolescents. Additionally, levels of spiritual well-being were similar in both groups. Our IBD cohort’s relatively similar personal and social characteristics vis-à-vis controls corroborate reports of resiliency and adaptability exhibited in other young people with disabilities or chronic illness. 10, 48–50
In contradistinction, levels of HRQOL variables that may be more directly related to the effects of a physically disabling illness such as IBD (e.g., physical functioning) were significantly lower in adolescents with IBD. Likewise, overall life stress was greater in patients with IBD. Adolescence is a developmental period featuring a number of role transitions occurring simultaneously – at home, in school, in one’s social life, and even potentially at work. We speculate that in adolescents with IBD, having to deal with an illness such as IBD in the context of their already busy lives may have influenced perceptions regarding overall stress.
Our central finding was that patients with IBD reported significantly lower VAS ratings and TTO utilities, and tended to have lower SG utilities (p=0.065) for their current health state than did controls. Health values assessment explicitly inquires into perceptions of the subject’s current health through health ratings (VAS), life expectancy tradeoffs (TTO), or willingness to risk dying (SG).
Our next aim was to examine factors that may influence utilities for current health among all of our study subjects and then to ascertain what factors were related to utilities, taking into account disease status. In multivariable analyses, lower VAS scores – which are ratings and not true utilities – were significantly associated with poorer physical functioning and poorer general health perceptions. Every 3-point decrease in physical functioning or general health perceptions scores translated to a 1-point decrease in VAS scores, and the model R2 was 0.52 (Table III). VAS ratings scores therefore appear to reflect variables that measure physical aspects of health and perceptions directly linked to health.
In contrast to VAS scores, our subjects’ TTO and SG utilities were not related to their physical functioning or their general health perceptions. In multivariable analyses, only emotional functioning and spiritual well-being were associated with TTO and SG scores. Spirituality encompasses an individual’s sense of purpose or meaning and their personal connectedness to the sacred or to the truth. 27 Spirituality has been shown to be important to adults with or without chronic illness, and may provide resiliency against the negative effects of stressors related to long-standing illness or disability. 29–31 Moreover, spirituality also appears to be important for adolescents and young adults in general. 51 Spirituality may exert a salutary effect on health and well-being by: promoting positive health behaviors and lifestyle choices; fostering a sense of belonging and facilitating access to social supports; and reinforcing psychological resources, such as self esteem and sense of mastery. 29–31, 52–54 It is perhaps not surprising then, that when one is asked to consider how much life expectancy one would be willing to give up or how great a risk of death one would be willing to incur in order to achieve a better state of health, that emotional health and one’s spiritual well-being are important predictors. Health utilities measure a broader construct than that assessed by other HRQOL constructs. To wit, utilities have been proposed to measure one’s “value of life,” given one’s state of health. 55 For patients with chronic illnesses such as IBD, the consequences of having a disease with an unpredictable course, the effects of the treatment process, and future illness prospects may influence many other facets of life beyond those traditionally considered to belong under the purview of health care.
Our study had several limitations. Because of the high prevalence of asthma and ADHD in the general population, we allowed patients with a history of intermittent asthma or well controlled ADHD to participate in the control group. Although only 4 subjects reported such a history, the control groups’ health values scores may have been lowered by their participation. We did not match controls to patients with IBD for age, sex, and race. However, when we controlled for those variables, there were no differences in results. Moreover, although all eligible subjects were notified of our study and invited to participate, our sample size reflects only those who agreed to do so. Also, because we recruited from one Midwestern medical center and participants may have had less severe disease, the generalizability of our findings is uncertain.
Comprehensive evaluation of health outcomes must incorporate patients’ perspectives. In that respect, adults may conceptualize health and develop beliefs about tests and treatments in ways different from adolescents. 56–58 Although the utility approach of HRQOL assessment has been employed widely in adult populations and is used to incorporate quality of life information into decision analysis and cost-effectiveness analysis to inform health-related interventions, programs, and polices, utilities have rarely been directly assessed from chronically ill adolescent patients. Because proxy reports of health status and utilities have often been shown to be inaccurate when compared with patients’ self-completed reports, assessing health outcomes directly from the patient’s perspective, be they adolescents or adults, is important. 59–63 Patients’ own preferences for outcomes may be particularly important to measure when they are considering clinical decisions that carry both potential benefits and risks. Accordingly, patient-specific health values are increasingly being incorporated into decision support tools to facilitate more informed decision-making using patients’ own preferences. 64 In adolescents living with a chronic illness such as IBD, patients would be able to use their preferences for clinical outcomes when considering a potentially risky medical regimen or a surgical intervention. Moreover, health values have arguably been the gold-standard measure of incorporating HRQOL information directly into decision analyses and cost-effectiveness analyses. Health values from adolescents with a chronic illness such as IBD or from the general population could be used as outcomes not only for patient-level decisions, but more widely for systematic evaluation of medical interventions or for healthcare policy.
In conclusion, our study shows that utility elicitation is feasible in adolescents with IBD and their healthy counterparts and that in most respects, adolescents with IBD and their healthy peers have similar personal, family, and social characteristics. However, adolescents with IBD generally reported lower general health perceptions and health values. We also found that the only factors associated with TTO and SG health utility scores were emotional and spiritual well-being.
Our findings suggest that in order to improve overall HRQOL, addressing the spiritual and emotional health needs of patients may be at least as important as addressing their physical health concerns. Future work should center on further elucidating the nature of health utilities in adolescents with chronic illnesses or disability, on whether utilities can be improved by interventions targeted to domains such as emotional or spiritual well-being, and on the relationship between spiritual well-being and overall health in adolescent patients with chronic illness or disability.
Figure 1.
Health values overall and by disease state. Mean (SD) health values for all study subjects are in gray bars, for patients with inflammatory bowel disease (IBD) in black bars, and for controls in diagonally striped bars. Scores for the time tradeoff and standard gamble are normalized to a 0–100 scale. Statistical results were similar after controlling for demographics (age, race, sex).
Acknowledgments
This study was funded by the National Institute of Child Health and Human Development (#K23HD044556) and the National Center for Complementary and Alternative Medicine (#K24AT001676).
We would like to dedicate this manuscript to the memory of Dr. Susan Moyer, who touched so many lives as a friend, a teacher, a mentor, and a caregiver. Her boundless energy and her selfless dedication to her patients and colleagues will be sorely missed.
The authors gratefully thank Karen Mandell, PharmD, for data management and Ruth Wise, MSN, for study coordination.
ABBREVIATIONS
- IBD
Inflammatory bowel disease
- HRQOL
Health-related quality of life
- QALYs
Quality-adjusted life years
- VAS
Visual analog scale
- TTO
Time tradeoff
- SG
Standard gamble
Footnotes
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kim S, Ferry G. Inflammatory bowel diseases in children. Curr Probl Pediatr Adolesc Health Care. 2002;32(4):108–132. doi: 10.1067/mps.2002.122638. [DOI] [PubMed] [Google Scholar]
- 2.Baldassano RN, Piccoli DA. Inflammatory bowel disease in pediatric and adolescent patients. Gastroenterol Clin North Am. 1999;28(2):445–458. doi: 10.1016/s0889-8553(05)70064-9. [DOI] [PubMed] [Google Scholar]
- 3.Ferry GD. Quality of life in inflammatory bowel disease: background and definitions. J Pediatr Gastroenterol Nutr. 1999;28(4):S15–18. doi: 10.1097/00005176-199904001-00001. [DOI] [PubMed] [Google Scholar]
- 4.MacPhee M, Hoffenberg EJ, Feranchak A. Quality-of-life factors in adolescent inflammatory bowel disease. Inflamm Bowel Dis. 1998;4(1):6–11. doi: 10.1097/00054725-199802000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Gortmaker SL, Walker DK, Weitzman M, Sobol AM. Chronic conditions, socioeconomic risks, and behavioral problems in children and adolescents. Pediatrics. 1990;85(3):267–276. [PubMed] [Google Scholar]
- 6.Tsevat J, Weeks JC, Guadagnoli E, et al. Using health-related quality-of-life information: clinical encounters, clinical trials, and health policy. J Gen Intern Med. 1994;9(10):576–582. doi: 10.1007/BF02599287. [DOI] [PubMed] [Google Scholar]
- 7.Patrick DL, Erickson P. Health status and health policy: quality of life in health care evaluation and resource allocation. New York: Oxford University Press; 1993. [Google Scholar]
- 8.Lamas GA, Orav EJ, Stambler BS, et al. Quality of life and clinical outcomes in elderly patients treated with ventricular pacing as compared with dual-chamber pacing. Pacemaker Selection in the Elderly Investigators. N Engl J Med. 1998;338(16):1097–1104. doi: 10.1056/NEJM199804163381602. [DOI] [PubMed] [Google Scholar]
- 9.Torrance GW. Measurement of health state utilities for economic appraisal. J Health Econ. 1986;5(1):1–30. doi: 10.1016/0167-6296(86)90020-2. [DOI] [PubMed] [Google Scholar]
- 10.Saigal S, Feeny D, Rosenbaum P, Furlong W, Burrows E, Stoskopf B. Self-perceived health status and health-related quality of life of extremely low-birth-weight infants at adolescence. JAMA. 1996;276(6):453–459. [PubMed] [Google Scholar]
- 11.Juniper EF, Guyatt GH, Feeny DH, Griffith LE, Ferrie PJ. Minimum skills required by children to complete health-related quality of life instruments for asthma: comparison of measurement properties. Eur Respir J. 1997;10(10):2285–2294. doi: 10.1183/09031936.97.10102285. [DOI] [PubMed] [Google Scholar]
- 12.Clinical Informatics Research Group. UMaker User’s Manual. Picastaway (NJ): UMDNJ; 1999. [Google Scholar]
- 13.Farrokhyar F, Swarbrick ET, Irvine EJ. A critical review of epidemiological studies in inflammatory bowel disease. Scand J Gastroenterol. 2001;36(1):2–15. doi: 10.1080/00365520150218002. [DOI] [PubMed] [Google Scholar]
- 14.Arias E. United States life tables, 2002. Natl Vital Stat Rep. 2004;53(6):1–38. [PubMed] [Google Scholar]
- 15.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 16.Bunn SK, Bisset WM, Main MJ, Golden BE. Fecal calprotectin as a measure of disease activity in childhood inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2001;32(2):171–177. doi: 10.1097/00005176-200102000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Lloyd-Still JD, Green OC. A clinical scoring system for chronic inflammatory bowel disease in children. Dig Dis Sci. 1979;24(8):620–624. doi: 10.1007/BF01333706. [DOI] [PubMed] [Google Scholar]
- 18.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care. 1999;37(2):126–139. doi: 10.1097/00005650-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Landgraf JM, Abetz L, Ware JE. The CHQ User’s Manual. 1. Boston, MA: The Health Institute, New England Medical Center; 1996. [Google Scholar]
- 21.Rosenberg M. Society and the adolescent self-image. Princeton, N.J.: Princeton University Press; 1965. [Google Scholar]
- 22.Sherer M, Maddux JE, Mercadante B, Prentice-Dunn S, Jacobs B, Rogers RW. The self-efficacy scale: Construction and Validation. Psychological Reports. 1982;51:663–671. [Google Scholar]
- 23.Spirito A. Manual for Kidcope. Providence, Rhode Island: Brown University; 1988. [Google Scholar]
- 24.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 25.Kolevzon MS, Green RG. Family Awareness Scale. In: Fischer J, Corcoran K, editors. Measures for clinical practice: a sourcebook. 2. Vol. 1. New York: Free Press; 1994. pp. 259–262. [Google Scholar]
- 26.Cauce A, Felner RD, Primavera J. Social support in high-risk adolescents: Structural components and adaptive impact. American Journal of Community Psychology. 1982;10:417–428. doi: 10.1007/BF00893980. [DOI] [PubMed] [Google Scholar]
- 27.Hill PC, Pargament KI. Advances in the conceptualization and measurement of religion and spirituality. Implications for physical and mental health research. Am Psychol. 2003;58(1):64–74. doi: 10.1037/0003-066x.58.1.64. [DOI] [PubMed] [Google Scholar]
- 28.Tsevat J, Sherman SN, McElwee JA, et al. The will to live among HIV-infected patients. Ann Intern Med. 1999;131(3):194–198. doi: 10.7326/0003-4819-131-3-199908030-00006. [DOI] [PubMed] [Google Scholar]
- 29.Chatters LM. Religion and health: public health research and practice. Annu Rev Public Health. 2000;21:335–367. doi: 10.1146/annurev.publhealth.21.1.335. [DOI] [PubMed] [Google Scholar]
- 30.Ellison CG, Levin JS. The religion-health connection: evidence, theory, and future directions. Health Educ Behav. 1998;25(6):700–720. doi: 10.1177/109019819802500603. [DOI] [PubMed] [Google Scholar]
- 31.Levin JS, Chatters LM. Research on religion and mental health: a review of empirical findings and theoretical issues. In: Koenig HG, editor. Handbook of Religion and Mental Health. San Diego, Calif: Academic Press; 1998. pp. 33–50. [Google Scholar]
- 32.Mrus JM, Leonard AC, Yi MS, et al. Health-related quality of life in veterans and nonveterans with HIV/AIDS. J Gen Intern Med. 2006;21 (Suppl 5):S39–47. doi: 10.1111/j.1525-1497.2006.00644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yi MS, Mrus JM, Wade TJ, et al. Religion, spirituality, and depressive symptoms in patients with HIV/AIDS. J Gen Intern Med. 2006;21 (Suppl 5):S21–27. doi: 10.1111/j.1525-1497.2006.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ellison CW. Spiritual well-being: Conceptualization and measurement. J Psychol Theol. 1983;11:330–340. [Google Scholar]
- 35.Cotton S, Larkin E, Hoopes A, Cromer BA, Rosenthal SL. The impact of adolescent spirituality on depressive symptoms and health risk behaviors. J Adolesc Health. 2005;36(6):529. doi: 10.1016/j.jadohealth.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 36.Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D. Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics. 1999;15(2):141–155. doi: 10.2165/00019053-199915020-00003. [DOI] [PubMed] [Google Scholar]
- 37.Burke P, Meyer V, Kocoshis S, Orenstein D, Chandra R, Sauer J. Obsessive-compulsive symptoms in childhood inflammatory bowel disease and cystic fibrosis. J Am Acad Child Adolesc Psychiatry. 1989;28(4):525–527. doi: 10.1097/00004583-198907000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Burke P, Meyer V, Kocoshis S, et al. Depression and anxiety in pediatric inflammatory bowel disease and cystic fibrosis. J Am Acad Child Adolesc Psychiatry. 1989;28(6):948–951. doi: 10.1097/00004583-198911000-00022. [DOI] [PubMed] [Google Scholar]
- 39.Engstrom I. Mental health and psychological functioning in children and adolescents with inflammatory bowel disease: a comparison with children having other chronic illnesses and with healthy children. J Child Psychol Psychiatry. 1992;33(3):563–582. doi: 10.1111/j.1469-7610.1992.tb00891.x. [DOI] [PubMed] [Google Scholar]
- 40.Engstrom I, Lindquist BL. Inflammatory bowel disease in children and adolescents: a somatic and psychiatric investigation. Acta Paediatr Scand. 1991;80(6–7):640–647. doi: 10.1111/j.1651-2227.1991.tb11923.x. [DOI] [PubMed] [Google Scholar]
- 41.Steinhausen HC, Kies H. Comparative studies of ulcerative colitis and Crohn’s disease in children and adolescents. J Child Psychol Psychiatry. 1982;23(1):33–42. doi: 10.1111/j.1469-7610.1982.tb00047.x. [DOI] [PubMed] [Google Scholar]
- 42.Wood B, Watkins JB, Boyle JT, Nogueira J, Zimand E, Carroll L. Psychological functioning in children with Crohn’s disease and ulcerative colitis: implications for models of psychobiological interaction. J Am Acad Child Adolesc Psychiatry. 1987;26(5):774–781. doi: 10.1097/00004583-198709000-00027. [DOI] [PubMed] [Google Scholar]
- 43.Rabbett H, Elbadri A, Thwaites R, et al. Quality of life in children with Crohn’s disease. J Pediatr Gastroenterol Nutr. 1996;23(5):528–533. doi: 10.1097/00005176-199612000-00003. [DOI] [PubMed] [Google Scholar]
- 44.Garmezy N. Stress-resistant children: the search for protective factors. 1. Oxford [Oxfordshire]; New York: Pergamon Press; 1985. pp. 213–233. [Google Scholar]
- 45.Garmezy N. Resilience in children’s adaptation to negative life events and stressed environments. Pediatr Ann. 1991;20(9):459–460. 463–456. doi: 10.3928/0090-4481-19910901-05. [DOI] [PubMed] [Google Scholar]
- 46.Haggerty RJ. Stress, risk, and resilience in children and adolescents: processes, mechanisms, and interventions. Cambridge [England]; New York, NY, USA: Cambridge University Press; 1994. [Google Scholar]
- 47.Luthar SS, Zigler E. Vulnerability and competence: a review of research on resilience in childhood. Am J Orthopsychiatry. 1991;61(1):6–22. doi: 10.1037/h0079218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bjerager M, Steensberg J, Greisen G. Quality of life among young adults born with very low birthweights. Acta Paediatr. 1995;84(12):1339–1343. doi: 10.1111/j.1651-2227.1995.tb13565.x. [DOI] [PubMed] [Google Scholar]
- 49.Appleton PL, Minchom PE, Ellis NC, Elliott CE, Boll V, Jones P. The self-concept of young people with spina bifida: a population-based study. Dev Med Child Neurol. 1994;36(3):198–215. doi: 10.1111/j.1469-8749.1994.tb11833.x. [DOI] [PubMed] [Google Scholar]
- 50.King GA, Shultz IZ, Steel K, Gilpin M, Cathers T. Self-evaluation and self-concept of adolescents with physical disabilities. Am J Occup Ther. 1993;47(2):132–140. doi: 10.5014/ajot.47.2.132. [DOI] [PubMed] [Google Scholar]
- 51.Associated Press. [Accessed August 24, 2007];AP Poll: God Vital to Young Americans. http://surveys.ap.org/data/KnowledgeNetworks/2007-08-20%20AP-MTV%20Youth%20Happiness.pdf.
- 52.Levin JS. How religion influences morbidity and health: reflections on natural history, salutogenesis and host resistance. Soc Sci Med. 1996;43(5):849–864. doi: 10.1016/0277-9536(96)00150-5. [DOI] [PubMed] [Google Scholar]
- 53.Levin JS, Vanderpool HY. Is frequent religious attendance really conducive to better health? Toward an epidemiology of religion. Soc Sci Med. 1987;24(7):589–600. doi: 10.1016/0277-9536(87)90063-3. [DOI] [PubMed] [Google Scholar]
- 54.Ellison CG. Religion, the life stress paradigm, and the study of depression. In: Levin JS, editor. Religion in Aging and Health: Theoretical Foundations and Methodological Frontiers. Thousand Oaks London New Delhi: Sage Publications; 1994. pp. 78–121. [Google Scholar]
- 55.Tsevat J. What do utilities measure? Med Care. 2000;38(9 Suppl):II160–164. [PubMed] [Google Scholar]
- 56.Jenney ME, Campbell S. Measuring quality of life. Arch Dis Child. 1997;77(4):347–350. doi: 10.1136/adc.77.4.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ladd RE, Forman EN. Adolescent decision-making: giving weight to age-specific values. Theor Med. 1995;16(4):333–345. doi: 10.1007/BF00995480. [DOI] [PubMed] [Google Scholar]
- 58.Eiser C. Children’s quality of life measures. Arch Dis Child. 1997;77(4):350–354. doi: 10.1136/adc.77.4.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Saigal S, Stoskopf BL, Feeny D, et al. Differences in preferences for neonatal outcomes among health care professionals, parents, and adolescents. JAMA. 1999;281(21):1991–1997. doi: 10.1001/jama.281.21.1991. [DOI] [PubMed] [Google Scholar]
- 60.Hays RD, Vickrey BG, Hermann BP, et al. Agreement between self reports and proxy reports of quality of life in epilepsy patients. Qual Life Res. 1995;4(2):159–168. doi: 10.1007/BF01833609. [DOI] [PubMed] [Google Scholar]
- 61.Guyatt GH, Juniper EF, Griffith LE, Feeny DH, Ferrie PJ. Children and adult perceptions of childhood asthma. Pediatrics. 1997;99(2):165–168. doi: 10.1542/peds.99.2.165. [DOI] [PubMed] [Google Scholar]
- 62.Tsevat J, Cook EF, Green ML, et al. Health values of the seriously ill. SUPPORT investigators. Ann Intern Med. 1995;122(7):514–520. doi: 10.7326/0003-4819-122-7-199504010-00007. [DOI] [PubMed] [Google Scholar]
- 63.Tsevat J, Dawson NV, Wu AW, et al. Health values of hospitalized patients 80 years or older. HELP Investigators. Hospitalized Elderly Longitudinal Project. JAMA. 1998;279(5):371–375. doi: 10.1001/jama.279.5.371. [DOI] [PubMed] [Google Scholar]
- 64.Sommers BD, Beard CJ, D’Amico AV, et al. Decision analysis using individual patient preferences to determine optimal treatment for localized prostate cancer. Cancer. 2007;110(10):2210–2217. doi: 10.1002/cncr.23028. [DOI] [PubMed] [Google Scholar]