Abstract
Purpose
Intramedullary (IM) nailing and plating are recognised fixation methods for both-bone midshaft forearm fractures. Although both methods are effective, IM nailing has recently been the accepted operative treatment for the paediatric population. The aim of the study was to compare the differences in the radiographic and functional outcomes of an age- and sex-matched cohort of children following treatment by IM fixation or plate fixation with screws for an unstable both-bone diaphyseal fracture.
Methods
A retrospective study was conducted and 17 age- and sex-matched pairs of patients returned for a research review clinic. The average age of our patients was 11.6 years at follow up, with 11 boys and six girls in each group. The mean follow up was similar in both groups (IM 31.5 months, plating 31.8 months).
Results
Plating and IM nailing result in good or excellent functional and radiological outcomes. Radiographs at the review clinic showed complete healing in the plating group, with reconstitution of the radial bow. Three patients in the IM group did not regain the natural radial bow radiographically. There were no significant differences between both groups for maximum radial bow and its location (P > 0.05). However, the maximum radial bow was significantly different from normative values in both groups (P = 0.003 plate, P = 0.005 IM). No non-union or malunion was observed. There were no significant differences in the loss of forearm motion and grip strength between both groups. There was no difference in the Pediatric Orthopaedic Society of North America (POSNA) scores between both groups. The plating group had a significantly worse Manchester scar score than the IM group (P = 0.012). One major complication was observed in each group: osteomyelitis for IM fixation and ulnar never palsy for plating.
Conclusion
Our study suggests that functional outcome is likely to be equivalent, regardless of which method of internal fixation is used.
Keywords: Forearm fracture, Children, Intramedullary nailing, Plating
Introduction
Forearm fractures are relatively common injuries, accounting for 41.1% of the fractures in the paediatric population [1]. Most are distal radius or ulna fractures. Diaphyseal radial and ulnar fractures make up approximately one-eighth of the total number of forearm fractures. As the bone remodeling potential in children is high, most forearm fractures can be successfully treated with immobilisation by plaster casting following closed reduction [2–4].
However, diaphyseal forearm fractures treated conservatively are known to remodel poorly compared to the distal one-third, with a higher incidence of malunion [5]. The residual deformity following malunited fractures does not always correct, especially in older children [6–8]. This could cause a loss of forearm motion and result in poor functional outcomes [6, 9]; therefore, operative treatment might be needed for the unstable, irreducible or open diaphyseal forearm fractures. The decision usually lies with the operating surgeon, although factors that the surgeon has to take into account are patient age and fracture characteristics (displacement, angulation and rotation). Generally, it has been accepted that children younger than 10 years of age have a better remodeling capacity than children older than 10 years [3, 6]. Off-ended fractures, rotational malalignment and angulation of >10° are other proposed criteria [3, 6, 7].
Intramedullary (IM) nailing [10–16] and plate fixation with screws [17, 18] are recognised operative management of mid-shaft forearm fractures and have been reported to be effective methods in treating paediatric midshaft forearm fractures. Although there have been a small number of studies comparing both methods of open reduction and internal fixation in the paediatric population, the numbers for each group are often unequal [18–23]. In addition, these studies are deficient in relating radiographic endpoints to functional outcomes, and outcome measures are usually subjective and arbitrary. The aim of our study was to evaluate the differences in radiographic and functional outcomes of an age- and sex-matched cohort of children following treatment by IM nailing or plate fixation with screws for an unstable both-bone diaphyseal fracture. We aim to determine which method of fixation gives a better overall outcome.
Materials and methods
We identified all patients in our paediatric centre with both-bone midshaft forearm fracture between July 2004 and July 2006. Our centre provides the only acute musculoskeletal trauma service for children in the local population, with a catchment of about 100,000 children. Those who were treated by open reduction and internal fixation (IM nailing or plate fixation) were eligible for inclusion. Open midshaft fractures, pathological fractures, Monteggia and Galeazzi fractures of the forearm were excluded from this study. Indications for open reduction and internal fixation in our centre were failure to achieve or maintain satisfactory reduction following manipulation under anaesthetics. The decision between IM nailing and plating is made by the supervising orthopaedic consultant. All operations were performed by either a consultant or a senior trainee. Ethical approval was obtained from our regional ethics committee to recall the patients for a research review clinic.
All patients received a routine post-operative regime using our integrated paediatric forearm fracture care pathway. The main difference was that the plating group had an above-elbow cast for 3–4 weeks until healing is noted on the radiographs. The cast is then removed to allow elbow and wrist range of motion exercises. The IM nailing patients are kept in an above-elbow cast for 2 weeks for comfort before initiating elbow and wrist range of motion exercises. All patients are seen up to 1 year post-operatively. All nails are removed following radiographic healing of the fracture being noted. This is usually between 4 and 6 months after the operation. In our centre, the plates are left in situ.
Eighteen patients were randomly matched for sex and age for each group and invited to attend a research fracture clinic. They were also matched for fracture pattern using the AO Pediatric Classification 22-D/4.1 or 22-D/5.1, indicating a simple complete transverse midshaft fracture or complete oblique or spiral fracture of the radius and ulna [24]. The matching of patients was undertaken using demographic data in isolation prior to recalling the patients for outcome assessment. The sample size was limited by the smaller number of IM nailing (18 patients) performed in our centre over the study period. In comparison, there were 30 patients requiring forearm plating over this time period. One patient was lost to follow up, as he was on holiday in our catchment area at the time of injury. Thirty-five patients returned for the clinic and consent was obtained. One patient who had IM nailing did not return for the research clinic. In total, we had 17 age- and sex-matched pairs of patients. All patients did not have a contralateral injury to the other forearm at any time and had a minimum follow up of 2 years. The patients were matched for age at the review clinic and not age at injury, as we would not be able to compare the functional outcomes objectively.
The patients who returned for the research clinic were assessed objectively by an unbiased clinical researcher who had not been involved in the treatment phase of the study for grip strength and range of movement of the forearm and elbow (pronation, supination, flexion, extension). Both forearms were assessed and the unaffected forearm was used as a control. The range of rotation of the forearm was measured by an in-house paediatric goniometer with the elbow flexed at 90° and the arm adducted. Tourniquets were used to secure the forearm in position at two different levels while the patient clasped the hand-held device and rotated it. Extension and flexion of the elbow were measured by a flexible goniometer placed along the lateral border of the forearm. Grip strength was assessed using a Jamar dynamometer (Sammons Preston, Bolingbrook, IL) and was based on standardised procedures from Mathiowetz et al. [25]. The dynamometer handle clamp was set at the second level for all patients. The mean of three attempts was used. The dominant hand was also noted and was taken into account when comparing with age- and sex-matched normative values. Scar assessment was evaluated using the validated Manchester scar score [26], which takes into account seven parameters (scar length, number of scars, colour, texture, border, appearance and contour), where 7 is the best possible score and 21 is the worst possible score. The Pediatric Orthopaedic Society of North America (POSNA) outcome questionnaire (parent-reported version 2.0) was also used to assess the functional health outcomes at follow up and this was completed by the parent attending with the child [27].
All patients had pre-operative, post-operative and final review clinic plain radiographs of the fractured forearm (anteroposterior and lateral). Ethical approval could not be obtained for obtaining plain radiographs of the unaffected contralateral side. All three sets of radiographs were measured for the angulation, shortening and translation of both the radius and ulnar bone. For the review clinic radiographs, the maximal radial bowing and location as described by Schemitsch and Richards [28] and modified by Firl and Wünsch [29] for use in children were also measured. On an anteroposterior radiograph of the forearm, the length of the radius (a), the location of maximum radial bow (b) and the maximal distance of the radius (c) from this point were measured. The distance a is measured from the bicipital tuberosity to the distal radial epiphysis. The maximal radial bowing and location b and c were expressed as percentages of the length of the radius a. Complete healing was defined as evidence of bony matrix crossing or bridging the fracture gap, in addition to the elimination of the initial fracture line on both radiographic views. Non-union, malunion or other radiological complications were also noted.
All information gathered in the study was recorded and analysed with use of the SPSS software package (version 13, SPSS Inc., Chicago, IL). The paired Student t-test (parametric data) or the Wilcoxon signed-rank test (non-parametric data) was used to compare differences between the groups. The grip strength values were individually compared with age- and sex-matched control values for the normal population using the Mann–Whitney U-test. The values of maximum radial bow and its location were compared to normative values [29] using the single tailed t-test.
Results
Demographics
The average age of our patients at injury was 9.45 years (range 4–13 years) for plating and 9.28 years (range 5–13 years) for nailing. The average age at the review clinic was as follows: 11.6 years for both groups (range 7–15 years). There were 11 boys and 6 girls in each group. In the IM nailing group, seven patients had both-bone IM nails, while ten patients had single-bone IM nails; in the plating group, nine patients had both-bone plating, while eight patients had single plates. Limb laterality of the fracture was as follows: IM nailing (9 right, 8 left), plating (5 right, 12 left). Using the AO classification, the fractures sustained in the IM nailing group were all 22-D/4.1, while the plating group consisted of 12 22-D/4.1 and five 22-D/5.1. All fractures united at the estimated time with no delayed union. The mean time to union was not analysed. The mean follow up was similar in both groups (P > 0.05): IM nailing, 31.5 months (range 24–45 months); plating, 31.8 months (range 23–44 months).
Radiographic outcome
A summary of the pre-operative fracture characteristics of the age- and sex- matched cohort of children is shown in Table 1. The radiographs at the review clinic showed complete healing in the plating group, with reconstitution of the radial bow. The average maximum radial bow was 5.98% (range 4.8–8.5%), location 63.3% (range 52.8–74.4%). In the IM nailing group, the average maximum radial bow was 5.77% (range 2.82–7.58%), location 65.2% (range 40.7–76.7%). Normal values by Firl for children are 7.21 ± 1.03 and 60.39 ± 3.74%, respectively. There was no significant differences between both groups for the values of maximum radial bow and its location (P > 0.05). However, the maximum radial bow was significantly different from normative values in both groups (P = 0.003 plate, P = 0.005 nailing), but there was no significant differences for the location of maximum radial bow (P > 0.05). One patient who had IM nailing developed heterotropic ossification of the ulna/radius. Three patients in the IM nailing group were observed to have not regained the natural radial bow radiographically, deviating towards the ulna. There was no displacement, malunion or non-union in both groups of patients.
Table 1.
Fracture characteristics
| IM nailing (n = 17) | Plating (n = 17) | P | |
|---|---|---|---|
| Radius | |||
| Angulation | 24° (5°–35°) | 25° (4°–75°) | 0.401 |
| Displacement | |||
| 100% | 6 (35%) | 9 (53%) | 0.402 |
| ≥50% | 3 (18%) | 3 (18%) | |
| <50% | 0 | 1 (6%) | |
| 0% | 8 (47%) | 4 (24%) | |
| Shortening | 1 (6%) | 4 (24%) | 0.146 |
| Ulna | |||
| Angulation | 23° (0–40°) | 28° (4°–105°) | 0.224 |
| Displacement | |||
| 100% | 5 (29%) | 5 (29%) | 0.232 |
| ≥50% | 3 (18%) | 4 (24%) | |
| <50% | 0 | 3 (18%) | |
| 0% | 9 (53%) | 5 (29%) | |
| Shortening | 2 (12%) | 4 (24%) | 0.368 |
Functional outcome
Table 2 shows the average range of forearm motion in each group. In both groups, there was a similar number of patients who had loss of forearm motion. Five patients had some loss of pronation and supination in the plating group, while six patients had some loss of pronation and supination in the IM group; six patients had some loss of flexion and extension in each group. Any loss of 5° or less was not considered to be significant to account for measuring errors.
Table 2.
Average range of motion
| Plating (°) | IM nailing (°) | |
|---|---|---|
| Pronation in unaffected forearm Pronation in affected forearm |
79 (70–90) 70 (60–85) |
85 (75–90) 76 (65–90) |
| Supination in unaffected forearm Supination in affected forearm |
75 (70–90) 71 (60–90) |
85 (75–90) 77 (60–90) |
| Flexion in unaffected elbow Flexion in affected elbow |
136 (120–145) 134 (120–145) |
134 (110–150) 133 (105–150) |
| Extension in unaffected elbow Extension in affected elbow |
0 (−5–10) 5 (−5–15) |
0 (−10–10) 0 (−10–5) |
Grip strength was compared to normative values taking into account the limb dominance. There was no significant difference in the grip strength between both groups, irrespective of hand dominance. However, grip strength at review for the right limb was significantly weaker than the age- and sex- matched normative values for both groups (IM nailing P = 0.031, plate P = 0.05).
Manchester scar score
The plating group had a significantly worse Manchester scar score than the IM nailing group (P = 0.012). This was apparent with their longer scar incisions and larger number of scars.
POSNA score
Comparisons between the groups and to the normative mean were performed. There was no significant differences between the two groups (P > 0.05). When we compared each group individually to the normative scores provided by the American Academy of Orthopaedic Surgeons (AAOS), there was also no significant difference for each group (P > 0.05). The POSNA score for each group is shown in Fig. 1.
Fig. 1.
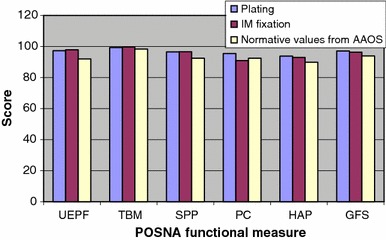
The Pediatric Orthopaedic Society of North America (POSNA) functional measure: plating vs. intramedullary (IM) fixation vs. normative values from the American Academy of Orthopaedic Surgeons (AAOS). UEPF upper extremity and physical function, TBM transfers and basic mobility, SPP sports/physical functioning, PC pain/comfort, HAP happiness, GFS global functioning score
Complications
Complications in the IM nailing group included one pin track infection causing osteomyelitis, which was successfully treated with antibiotics. In the plating group, one patient had an initial ulna palsy, which resolved with time. There was no significant loss of forearm motion. Another patient had a loose ulnar screw which was causing irritation and the ulnar plate had to be removed under general anaesthetic. The radial plate was left in situ.
Discussion
Functional outcome following a midshaft both-bone paediatric forearm fracture is one of the main considerations for a surgeon deciding between operative treatment and conservative management. Unlike adults, the majority of these fractures can be treated non-operatively with full restoration of forearm function. This is due to the presence of a tough periosteum, an open physis and the rapid remodeling capacity of children. However, these characteristics feature prominently in younger children but diminish with age, with older children having unpredictable remodeling capacities. A number of studies in the literature have revealed that some children do not regain full forearm function following conservative management [3, 6, 9]. Cadaveric studies have provided some insight into the cause of this [30, 31]. Both conclude that angular and rotatory deformities of the forearm of 10° or less result in minimum significant loss of forearm rotation. Additionally, supination is found to be more markedly affected in a midshaft forearm fracture compared to a distal forearm fracture, and rotational deformities produce loss of pronation–supination that were proportional to the degree of deformity.
The gold standard for the operative treatment of a midshaft forearm fracture in an adult is plate fixation with screws [32]. Similar excellent outcomes were also obtained in the paediatric population [17, 18]. However, one main disadvantage is the need for a large incision for internal fixation. Complications of plate fixation include refracture, failure of hardware, nerve palsy and infection [5, 19, 20]. Currently, there has been a trend favouring IM nailing for the paediatric population, mainly because it is less invasive and there is no risk of periprosthetic fracture, as with a plate. Other benefits of IM nailing for children are better cosmesis and easy removal of the nail, although an anaesthetic is required [19]. However, as with any surgical intervention, complications can arise. These include pin tract infection, osteomyelitis, synostosis, loss of reduction, hardware migration, hardware irritation, nerve palsy and delayed union [15, 16, 33].
Our study shows that excellent results were obtained for both operative interventions, with near-normal restoration of forearm function. Radiological outcomes were not significantly related to the function of the forearm. Grip strength appeared to be globally reduced in both limbs in both groups when compared to normative values but it was not statistically significant. All fractures were shown to have complete bone remodeling following open reduction, internal fixation (ORIF) at follow up. POSNA scores were similar in both groups and also to normative values. Unsurprisingly, scar scores were better in the IM group. There was one major complication in each group. We have reviewed similar studies comparing IM nailing with plating in the literature and the results are shown in Table 3 [18–23]. These studies did not find any significant difference in functional outcomes or complication rates between either operative method. Most of these measurements were performed subjectively. In comparison, we used objective assessments for these outcome measurements and found similar results.
Table 3.
Comparison of the literature for similar studies (IM nails vs. plating)
| Study period (years) | IM/plate (total no.) | Age (IM/plate) | Sex (IM/plate) | Functional outcome | Complications | ||
|---|---|---|---|---|---|---|---|
| IM | Plate | ||||||
| Our study | 2.5 | 17/17 (34) | 9.3/9.5 | 11 M 7 F | Similar POSNA scores, grip strength and range of motion IM nail—better scar score |
1 major (6%) | 1 major (6%) |
| Reinhardt et al. [23] | 9 | 19/12 (31) | 12.5/14.4 | 13 M 6 F/10 M 2 F | IM: 2 loss of forearm rotation Plate: 4 loss of forearm rotation |
4 major, 8 minor (63%) |
4 major, 4 minor (66%) |
| Fernandez et al. [19] | 4 | 45/19 (64) | 9.3/11.1 | 32 M 13 F/15 M 4 F | IM: all content/v. content Plate: 1 discontent |
9 (20%) | 3 (16%) |
| Smith et al. [20] | 5 | 21/15 (36) | 9.7/11.3 | 12 M 9 F/13 M 2 F | Not mentioned in detail | 9 (42%) | 5 (33%) |
| Van der Reis et al. [22] | 6 | 23/18 (41) | 10/11 | 14 M 9 F/12 M 6 F | IM: poor in 5 (22%) Plate: poor in 4 (22%) |
5 (21%) | 6 (33%) |
Plate fixation usually provides excellent anatomical reduction for fracture healing. IM nailing provides near-accurate reduction with reliable maintenance of the fracture alignment, but does not guarantee correct rotational alignment. In our patients, no individual radius had a negative bow (towards the ulna) with plate fixation. Three patients with IM nailing were observed to have completely lost their physiological radial bowing, with obvious deviation of the bow towards the ulna: two patients had significant loss of motion (loss of 20° supination, loss of 15° pronation). Interestingly, the other patient who had an associated heterotropic ossification between the radius and ulna had full forearm rotation and strength. Our results showed that both treatments restored the location of the maximum radial bow, but the maximum radial bow was significantly smaller than normative values [29]. This was in contrast to Reinhardt et al. [23], who also found that only the plating group restored the location of the radial bow. Physiological bowing is of importance to forearm function and strength [34]. However, we could not find any relationship between radial bow and functional outcome. This was proven by the comparatively small number of patients with a minor loss of forearm and elbow movement. Where the loss of radial bowing is relatively minor, these findings suggest that no direct relationship with loss of function can be demonstrated.
The current study exhibits certain advantages in the matched design compared with other published data investigating ORIF of both-bone midshaft forearm fractures, which are from case series describing a particular treatment or retrospective comparisons of nails and plates. Often, the numbers comparing each surgical intervention are unequal in these studies. Most importantly, such studies are open to bias, especially in the paediatric population. Boys and girls have different physiological rates of skeletal maturity, with girls reaching skeletal maturity about 2 years earlier than boys. An age- and sex- matched study would eliminate these two interconnected and potentially confounding factors. The comparison between the two surgical techniques is made within each matched pair and, thus, the treatment effect will be more precisely estimated than would be the case with a parallel group study with the same number of subjects. Although the disadvantage of matching is a possible inability to match some subjects, thus, reducing the total number of available subjects in the study, we did not experience such a problem due to a large excess of plates being performed in our centre. Although there were only 34 patients in this study, they were recruited over a 2-year period. Compared to other studies in the literature, the average number of patients per year with a both-bone forearm fracture needing treatment with ORIF was similar. One main difference of our study was the use of validated scoring systems, which has been lacking in similar papers.
There were other confounding factors that were not addressed in our study but have been shown in the literature to not affect outcome. Not all of our patients underwent fixation to both bones. However, single-bone fixation has been shown to be sufficient with excellent outcomes if, following reduction and fixation of one bone, the second bone is stable [12, 16, 35–37]. A subanalysis of our patients comparing single-bone fixation with both-bone fixation showed no significant difference in their range of motion.
To date, there are no randomised controlled trials comparing IM nailing and plating in the literature. One of the reasons for this could be the difficulty in obtaining ethical approval to randomised children into different treatment arms. However, the increasing numbers of comparative studies in the literature have shown that both methods of fixation provide similar good to excellent outcomes. The present study suggests that functional outcome is likely to be equivalent, no matter which method of internal fixation is used. Although this has been shown in previous studies, there has been a lack of validated tools used to assess the outcomes. We, therefore, believe that any future potential research for both-bone diaphyseal forearm fractures should be a prospective multi-centre randomised study with appropriate follow ups at regular intervals to include satisfaction assessment instruments, including cosmesis, scar effects and social implications of each method employed to confirm the findings of retrospective studies currently available in the literature.
References
- 1.Rennie L, Court-Brown CM, Mok JY, Beattie TF. The epidemiology of fractures in children. Injury. 2007;38(8):913–922. doi: 10.1016/j.injury.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 2.Voto SJ, Weiner DS, Leighley B. Redisplacement after closed reduction of forearm fractures in children. J Pediatr Orthop. 1990;10(1):79–84. doi: 10.1097/01241398-199001000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Price CT, Scott DS, Kurzner ME, Flynn JC. Malunited forearm fractures in children. J Pediatr Orthop. 1990;10(6):705–712. doi: 10.1097/01241398-199011000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Zionts LE, Zalavras CG, Gerhardt MB. Closed treatment of displaced diaphyseal both-bone forearm fractures in older children and adolescents. J Pediatr Orthop. 2005;25(4):507–512. doi: 10.1097/01.bpo.0000158005.53671.c4. [DOI] [PubMed] [Google Scholar]
- 5.Kay S, Smith C, Oppenheim WL. Both-bone midshaft forearm fractures in children. J Pediatr Orthop. 1986;6(3):306–310. doi: 10.1097/01241398-198605000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Daruwalla JS. A study of radioulnar movements following fractures of the forearm in children. Clin Orthop Relat Res. 1979;139:114–120. [PubMed] [Google Scholar]
- 7.Fuller DJ, McCullough CJ. Malunited fractures of the forearm in children. J Bone Joint Surg Br. 1982;64(3):364–367. doi: 10.1302/0301-620X.64B3.7096406. [DOI] [PubMed] [Google Scholar]
- 8.Högström H, Nilsson BE, Willner S. Correction with growth following diaphyseal forearm fracture. Acta Orthop Scand. 1976;47(3):299–303. doi: 10.3109/17453677608991994. [DOI] [PubMed] [Google Scholar]
- 9.Nilsson BE, Obrant K. The range of motion following fracture of the shaft of the forearm in children. Acta Orthop Scand. 1977;48(6):600–602. doi: 10.3109/17453677708994804. [DOI] [PubMed] [Google Scholar]
- 10.Amit Y, Salai M, Chechik A, Blankstein A, Horoszowski H. Closing intramedullary nailing for the treatment of diaphyseal forearm fractures in adolescence: a preliminary report. J Pediatr Orthop. 1985;5(2):143–146. doi: 10.1097/01241398-198505020-00003. [DOI] [PubMed] [Google Scholar]
- 11.Lascombes P, Prevot J, Ligier JN, Metaizeau JP, Poncelet T. Elastic stable intramedullary nailing in forearm shaft fractures in children: 85 cases. J Pediatr Orthop. 1990;10(2):167–171. doi: 10.1097/01241398-199003000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Pugh DM, Galpin RD, Carey TP. Intramedullary Steinmann pin fixation of forearm fractures in children. Long-term results. Clin Orthop Relat Res. 2000;376:39–48. doi: 10.1097/00003086-200007000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Rabinovich A, Adili A, Mah J. Outcomes of intramedullary nail fixation through the olecranon apophysis in skeletally immature forearm fractures. J Pediatr Orthop. 2005;25(5):565–569. doi: 10.1097/01.bpo.0000173249.04561.10. [DOI] [PubMed] [Google Scholar]
- 14.Shoemaker SD, Comstock CP, Mubarak SJ, Wenger DR, Chambers HG. Intramedullary Kirschner wire fixation of open or unstable forearm fractures in children. J Pediatr Orthop. 1999;19(3):329–337. [PubMed] [Google Scholar]
- 15.Cullen MC, Roy DR, Giza E, Crawford AH. Complications of intramedullary fixation of pediatric forearm fractures. J Pediatr Orthop. 1998;18(1):14–21. [PubMed] [Google Scholar]
- 16.Luhmann SJ, Gordon JE, Schoenecker PL. Intramedullary fixation of unstable both-bone forearm fractures in children. J Pediatr Orthop. 1998;18(4):451–456. [PubMed] [Google Scholar]
- 17.Nielsen AB, Simonsen O. Displaced forearm fractures in children treated with AO plates. Injury. 1984;15(6):393–396. doi: 10.1016/0020-1383(84)90204-3. [DOI] [PubMed] [Google Scholar]
- 18.Wyrsch B, Mencio GA, Green NE. Open reduction and internal fixation of pediatric forearm fractures. J Pediatr Orthop. 1996;16(5):644–650. doi: 10.1097/01241398-199609000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Fernandez FF, Egenolf M, Carsten C, Holz F, Schneider S, Wentzensen A. Unstable diaphyseal fractures of both bones of the forearm in children: plate fixation versus intramedullary nailing. Injury. 2005;36(10):1210–1216. doi: 10.1016/j.injury.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Smith VA, Goodman HJ, Strongwater A, Smith B. Treatment of pediatric both-bone forearm fractures: a comparison of operative techniques. J Pediatr Orthop. 2005;25(3):309–313. doi: 10.1097/01.bpo.0000153943.45396.22. [DOI] [PubMed] [Google Scholar]
- 21.Ortega R, Loder RT, Louis DS. Open reduction and internal fixation of forearm fractures in children. J Pediatr Orthop. 1996;16(5):651–654. doi: 10.1097/01241398-199609000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Van der Reis WL, Otsuka NY, Moroz P, Mah J. Intramedullary nailing versus plate fixation for unstable forearm fractures in children. J Pediatr Orthop. 1998;18(1):9–13. [PubMed] [Google Scholar]
- 23.Reinhardt KR, Feldman DS, Green DW, Sala DA, Widmann RF, Scher DM. Comparison of intramedullary nailing to plating for both-bone forearm fractures in older children. J Pediatr Orthop. 2008;28(4):403–409. doi: 10.1097/BPO.0b013e31816d71f2. [DOI] [PubMed] [Google Scholar]
- 24.Slongo TF, Audigé L, AO Pediatric Classification Group Fracture and dislocation classification compendium for children: the AO pediatric comprehensive classification of long bone fractures (PCCF) J Orthop Trauma. 2007;21(10 Suppl):S135–S160. doi: 10.1097/00005131-200711101-00020. [DOI] [PubMed] [Google Scholar]
- 25.Mathiowetz V, Wiemer DM, Federman SM. Grip and pinch strength: norms for 6- to 19-year-olds. Am J Occup Ther. 1986;40(10):705–711. doi: 10.5014/ajot.40.10.705. [DOI] [PubMed] [Google Scholar]
- 26.Beausang E, Floyd H, Dunn KW, Orton CI, Ferguson MW. A new quantitative scale for clinical scar assessment. Plast Reconstr Surg. 1998;102(6):1954–1961. doi: 10.1097/00006534-199811000-00022. [DOI] [PubMed] [Google Scholar]
- 27.Daltroy LH, Liang MH, Fossel AH, Goldberg MJ. The POSNA pediatric musculoskeletal functional health questionnaire: report on reliability, validity, and sensitivity to change. Pediatric Outcomes Instrument Development Group. Pediatric Orthopaedic Society of North America. J Pediatr Orthop. 1998;18(5):561–571. doi: 10.1097/00004694-199809000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Schemitsch EH, Richards RR. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am. 1992;74(7):1068–1078. [PubMed] [Google Scholar]
- 29.Firl M, Wünsch L. Measurement of bowing of the radius. J Bone Joint Surg Br. 2004;86(7):1047–1049. doi: 10.1302/0301-620X.86B7.14294. [DOI] [PubMed] [Google Scholar]
- 30.Tarr RR, Garfinkel AI, Sarmiento A. The effects of angular and rotational deformities of both bones of the forearm. An in vitro study. J Bone Joint Surg Am. 1984;66(1):65–70. [PubMed] [Google Scholar]
- 31.Matthews LS, Kaufer H, Garver DF, Sonstegard DA. The effect on supination–pronation of angular malalignment of fractures of both bones of the forearm. J Bone Joint Surg Am. 1982;64(1):14–17. [PubMed] [Google Scholar]
- 32.Chapman MW, Gordon JE, Zissimos AG. Compression-plate fixation of acute fractures of the diaphyses of the radius and ulna. J Bone Joint Surg Am. 1989;71(2):159–169. [PubMed] [Google Scholar]
- 33.Schmittenbecher PP, Fitze G, Gödeke J, Kraus R, Schneidmüller D. Delayed healing of forearm shaft fractures in children after intramedullary nailing. J Pediatr Orthop. 2008;28(3):303–306. doi: 10.1097/BPO.0b013e3181684cd6. [DOI] [PubMed] [Google Scholar]
- 34.Richards RR. Chronic disorders of the forearm. J Bone Joint Surg Am. 1996;78(6):916–930. doi: 10.2106/00004623-199606000-00017. [DOI] [PubMed] [Google Scholar]
- 35.Flynn JM, Waters PM. Single-bone fixation of both-bone forearm fractures. J Pediatr Orthop. 1996;16(5):655–659. doi: 10.1097/01241398-199609000-00020. [DOI] [PubMed] [Google Scholar]
- 36.Kirkos JM, Beslikas T, Kapras EA, Papavasiliou VA. Surgical treatment of unstable diaphyseal both-bone forearm fractures in children with single fixation of the radius. Injury. 2000;31(8):591–596. doi: 10.1016/S0020-1383(00)00057-7. [DOI] [PubMed] [Google Scholar]
- 37.Myers GJ, Gibbons PJ, Glithero PR. Nancy nailing of diaphyseal forearm fractures. Single bone fixation for fractures of both bones. J Bone Joint Surg Br. 2004;86(4):581–584. [PubMed] [Google Scholar]


