Abstract
Purpose
The purpose of this study was to assess percutaneous femoral distal hemi-epiphysiodesis using transphyseal cannulated screws in order to correct valgus angular deformities of the knee in pediatric and adolescent patients.
Methods
This is a prospective longitudinal study in which our experience with 52 patients is described.
Results
We evaluated 100 knees surgically managed for pathologic genu valgum over a 68-month period. The average age at surgery for boys and girls was 14 years and 7 months (range 12.7–15.1 years) and 13 years and 6 months (range 12.9–14.8 years), respectively. The pre-surgical tibiofemoral (T–F) angle was measured at between 14.17° and 35.3°, and the postoperative T–F was measured at between 6.2° and 15.8° (7.2° ± 0.65°, mean ± standard deviation), for an average correction of 0.73° ± 0.45° per month). The mean follow-up after surgery was 3.2 years (range 2.3–5.3 years).
Conclusions
We demonstrate a simple, fast and reproducible surgical technique for percutaneous epiphysiodesis with low morbidity, rapid rehabilitation and a rapid return to school and sports activities. We experienced no complications, such as overcorrection, undercorrection, postoperative hematoma or infection. We conclude that percutaneous screw epiphysiodesis is an excellent option for the treatment of genu valgum in adolescents.
Keywords: Adolescent, Cannulated screw, Genu valgus, Hemiepiphysiodesis
Introduction
Idiopathic genu valgum, commonly called “knock-knees”, is observed frequently during adolescence, as a transitory hallmark, and it rarely needs surgical correction [1]. Normal alignment of the lower extremities includes equal leg lengths, with the mechanical axis of the leg bisecting the knee when the patient is standing erect with the patellae pointing forward. This position places relatively balanced forces on the medial and lateral compartments of the knee and on the collateral ligaments, while the patella remains stable and centered in the femoral sulcus. When we refer to the femoral–tibial angle, we are describing the angle defined by the mechanical axis of the femur intersecting with the mechanical axis of the tibia [2, 3].
In 1993, Phemister [4] described the first surgical epiphysiodesis procedure. He created a bone bridge across the physis by removing a medial and lateral rectangular segment of bone, including a small asymmetric portion of the metaphysis and epiphysis on either side of the physis, and then reinserted the fragment in the opposite direction, leading to the formation of a bone bridge. This method of surgical epiphysiodesis is permanent, and it requires an accurate prediction of remaining growth. It requires open medial and lateral exposure, postoperative protected weight bearing, and postoperative rehabilitation.
In 1945, following studies in animals and later in children, Haas [5] proposed stopping the growth of the physis with nails. He was able to see that after removing the nails, longitudinal growth was reestablished, suggesting new methods for the treatment of dysmetria and angular deformities of the limbs. Subsequently, in 1949, Blount and Clarke [6] presented a method involving a 5- to 8-cm-long longitudinal incision for the placement of surgical staples across the growth plate on the convex side of deformities. The aim of this procedure was to arrest growth under the staple and allow for gradual correction of angular deformities. These authors concluded that three staples should be used secondary to the high rate of complications, including loss fixation and metal failure with staple breakage. In 1979, Zuege [7], reported that epiphysiodesis with staples was an effective and secure technique for the treatment of angular deformities in lower limbs. He also noted the importance of adequate clinical evaluation and radiographic imaging to accurately predict timing for the removal of staples, as well as the “rebound” phenomenon.
Stevens [8] created an implant composed of a two-hole titanium plate with two cannulated screws that is used in a similar manner to staples in order to create a hemi-epiphysiodesis. This technique has the advantage of rapid correction of angular deformity, while avoiding compression of the physis and permanent physeal arrest. Loss of fixation and implant failure are rare. However, epiphysiodesis with staples has been used with success, even in the treatment of genu valgum secondary to skeletal dysplasia, blood or endocrine disorders or other pathologies where there is an alteration of the physis.
In 1984, Bowen and colleagues [9–11] proposed a percutaneous epiphysiodesis technique using fluoroscopic imaging and curettage of the physis. A permanent physeal arrest is created with this technique. Other percutaneous techniques have since been described, including the use of other instruments, such as a broach, cannulated drill and Steinmann pins. Among the complications that have been described, damage to the popliteal nerve has been related to the use of broaches that generate heat near the proximal tibia. [11–16].
Biological agents affecting physeal growth, including stromal cell-derived growth factor 1 (SDF-1), may offer therapeutic alternatives for the treatment of length discrepancies and angular deformities [17, 18]. Metaizeau et al. in 1988 [18] and Khoury et al. in 2007 [19] described a percutaneous technique for creating a surgical, reversible epiphysiodesis using transphyseal screws. The advantages of this technique included shortened operative times, rapid rehabilitation, reversibility, and few complications, such as fracture or loosening of the implant.
Materials and methods
This is a case series of 52 patients who were treated between May 2003 and January 2009 at the Pediatric Hip and Knee Service of the Orthopaedic and Traumatology Department, Bogotá, Colombia. The last follow-up of patients was performed in January 2009, and the last surgery was performed in July 2008. All patients presented severe genu valgum, and all participated in this study with parental consent.
An EXCEL database was used, and the statistical program StatCalc of Epi-Info, ver. 3.3.2, was used to perform the statistical analysis. The objectives of our study are presented in Table 1.
Table 1.
Objectives of percutaneous hemi-epiphysiodesis with cannulated screws for the treatment of genu valgum
| General objective | Specific objectives |
|---|---|
| Describe our experience with percutaneous hemi-epiphysiodesis with transphyseal cannulated screws for the correction of genu valgum | Evaluate the resulting correction of the tibiofemorall angle |
| Evaluate the early rehabilitation of the patient as related to his/her resumption of normal daily activities | |
| Report on our failure and success cases as related to the surgical techniques |
The degree of correction per month was calculated, the reversibility of the procedure was analyzed, and complications were evaluated.
The indications included measurement of the intermalleolar distance (IMD) >8 cm and radiological measurement of the tibiofemoral angle (T–F) >10° [18, 19] (Fig. 1).
Fig. 1.
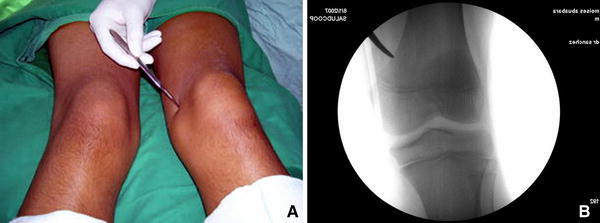
a, b Intraoperative photographs showing the incision used for the percutaneous hemi-epiphysiodesis with cannulated screws
Radiographic techniques used for this study were standardized. All coronal plane imaging was performed with the patella pointed straight ahead and standardized distances between the subject and the X-ray tube. The tibiofemoral angle was measured as the angle formed by the intersection of the mechanical axis of the femur versus the mechanical axis of the tibia. The Bowen method [10] was utilized to calculate the appropriate timing of the hemiepiphysiodesis based on measurement of physeal width and the magnitude the valgus deformity.
Growth parameters were assessed according to Anderson [20] (Table 2).
Table 2.
Criteria applied for the inclusion and exclusion of patients
| Inclusion criteria | Exclusion criteria |
|---|---|
| Patients between 12 and 16 years of age | Personal history of correction osteotomies in proximal femur |
| Diagnosis of genu valgum with a T–F angle >10° | Post-traumatic angular deformities |
| A minimum of 3 months of follow-up |
T–F angle Tibiofemoral angle
Surgical technique
The surgical approach consisted of the following steps:
The patient is placed in a supine position on the operating table after being given general anesthesia.
A radiolucent operating room table and a fluoroscope are used without placement of a tourniquet.
The knee is flexed 20° and a 1-cm incision is made on the lateral aspect of the distal femur approximately 2 cm above the insertion of the medial collateral ligament. A Kelly clamp is used to bluntly dissect down to bone (see Figs. 1, 2).
Under fluoroscopic control, the drill guide for the 7.0-mm cannulated drill is positioned with a 10° medial and 35° posteriorly directed inclination; see Fig. 3.
A 4.5 drill broach is used to make a tunnel for the cannulated 7.0-mm screw with a 16-mm thread (or a 3.2 broach for the 4.5-mm screw). A washer is used, and the screw is inserted up to 7 mm from the articular surface in order to avoid joint cartilage injury. An attempt is made to place all of the 16-mm threads within the epiphysis in order to achieve transphyseal compression.
Closure of the skin is done, anda dry sterile dressing is applied without rigid immobilization; see Fig. 4.
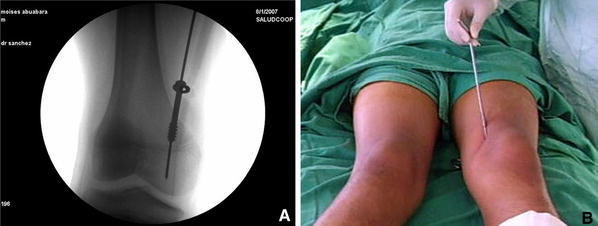
Fig. 2.

Under fluoroscopic control, the elastic nail guide is placed (a ) directing the tunnel from cephalic to caudal and towards the lateral part of the condyle (b, c)
Fig. 3.
Tunnel for the cannulated 7.0-mm screw with a 16-mm thread and a washer (a) that is up to 7 mm from the articular cartilage surface in the direction established (b)
Fig. 4.
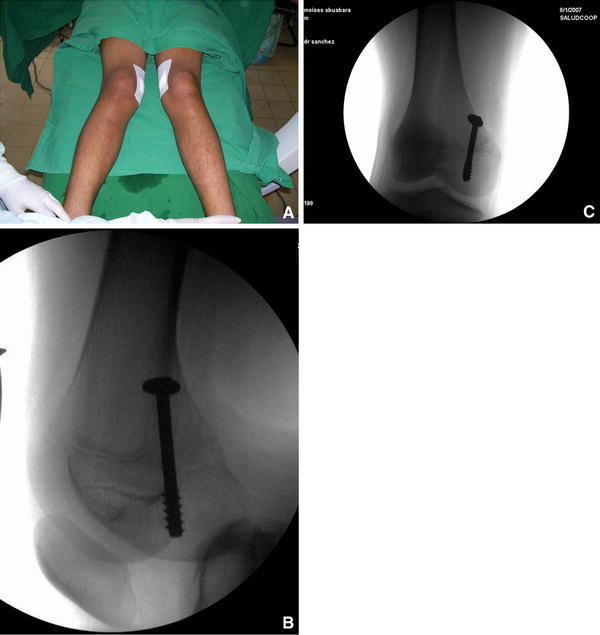
a The opening is covered without the need of rigid immobilization, b, c post-surgical of hemi-epiphysiodesis with cannulated screws with transphyseal compression
Post-surgical recommendations
Standing and ambulation was encouraged 2 h after surgery without the need for formal physical therapy. We recommend avoidance of activities resulting in excess axial loads to the lower limbs, including jumping and running for 2 weeks from the date of surgery. Postoperative evaluation was performed 3, 15, and 30 days after surgery, and then every 6 months with long leg radiographs of the lower extremities and clinical assessment, including intermalleolar distance.
Results
A total of 43 adolescent boys and nine adolescent girls comprised the study population, and 100 knees were surgically treated for pathologic genu valgum over a 68-month interval. The average age of the boys and girls at surgery was 14 years and 7 months (range 12.7–15.1 years) and 13 years and 6 months (range 12.9–14.8 years), respectively.
Mean follow-up after surgery was 3.2 years (range 2.3–5.3 years). None of the patients required physical therapy, and full functional recovery was achieved within 3 months post-surgery in 50 patients (96.1%), which was considered to be a satisfactory success rate. The surgical results on female patients (3.8%) older than 15 years were described as unsatisfactory secondary to premature closure of the growth plate.
The clinical preoperative evaluation was carried out with the patient in the standing position, during which time the IMD was measured in order to assess the degree of genu valgum. The patients with genu valgum had an average IMD of 23 cm [range 14–55 cm, standard deviation (SD) ±1.35 cm] with a T–F angle of 26.5° (range 14.1–35.3°, SD ±2.34 cm), resulting in a T–F angle of 7.2 ± 0.65° (range 6.2–15.8°) and average angular correction of 7.6° (range 7.2–10.6°, SD ±5.25°) or 0.73° per month (SD ±0.45° per month), see Table 3.
Table 3.
Salient preoperative radiological indices versus the postoperative indices
| Age | Boys | Girls | Average initial measurements | POP at 3 months | POP at 6 months | POP at 36 months | Average initial measurements | POP at 3 months | POP at 6 months | POP at 36 months | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T–F | SD | T–F | SD | T–F | SD | T–F | SD | IMD | SD | IMD | SD | IMD | SD | IMD | SD | |||
| 12–13 years-old | 25 patients | 10 patients | 21–35° p < 0.02 |
2.80 | 8–12° p < 0.04 |
1.32 | 7–12° p < 0.02 |
0.45 | 6–12° p < 0.03 |
1.26 | 14–55 cm p < 0.02 |
1.23 | 6–16 cm p < 0.02 |
0.26 | 6–12 cm p < 0.02 |
0.26 | 5–9 cm p < 0.02 |
0.26 |
| 14–15 years-old | 12 patients | 5 patients | 14–32° p < 0.02 |
0.80 | 12–15° p < 0.03 |
6.32 | 8–12° p < 0.03 |
5.18 | 6–12° p < 0.02 |
3.12 | 22–43 cm p < 0.02 |
0.26 | 9–20 cm p < 0.02 |
8.23 | 7–16 cm p < 0.02 |
5.51 | 5–10 cm p < 0.02 |
3.12 |
All data were analyzed using univariate and multivariate analysis of variance
CI Confidence interval, SD standard deviation, POP postoperative, IMD intermalleolar distance
During the follow-up period, none of the patients complained of pain or discomfort while walking or during school physical activities. The average surgical timing was 12 min for each knee (range 10.2–15.8 min). Average bleeding was 10 ml. There were no complications, such as vascular injuries, infection, chondrolysis or compartment syndrome.
Satisfactory results were defined as an IMD <6 cm, and 98% of the treated physes were considered to be satisfactory in this study.
When the IMD was >6 cm, the result was considered to be unsatisfactory. An unsatisfactory result was seen in one patient (two physes) in a girl who was 15 years of age at surgery. The radiographic results were considered satisfactory when the T–F angle of the knee was ≤7° in the adolescent male patients and ≤9° in the adolescent female patients. Four patients were evaluated at the end of growth, after a radiographic physeal closure was observed. The cannulated screws were percutaneously removed after an average of 20.2 months (range 18.9–25 months). In all cases, the screws were removed after angular correction. The screws were removed during normal growth in 39 patients and prior to the end of growth in seven patients. The others had not reached complete angular correction at the end of the follow-up.
Discussion
In children under 6 years of age, genu valgum may be physiological. In contrast, idiopathic juvenile genu valgum is not benign, and it presents with the mechanical axis deviated over the lateral compartment of the knee, which may result in clinical problems, such as increased tension in the medial collateral ligament and knee pain. The patellofemoral articulation may become incongruent or unstable, producing anterior pain with physical activity and, in extreme cases, resulting in dislocation of the patella with or without osteochondral fractures. Patellar dislocation is seen as an insidious, progressive interruption of growth because of the premature and excentric tension of the knee with a hypoplasia of the lateral femoral condile, meniscal rupture, and chondromalacia that may lead to arthrosis of the lateral and anterior compartments.
Since the staples were introduced by Walter Blount in 1949 [6], this procedure has waxed and waned in popularity, remaining to this day controversial. Indeed, some recent review articles and book chapters dismiss stapling as a historical procedure, citing unpredictability and the fear of permanent physeal arrest as results of stapling. While stapling can work well, occasional breakage or migration of the staples can necessitate revision of the hardware or premature abandonment of this method of treatment. However, this procedure has its supporters who recommend it as the optimum treatment [19–22].
A number of studies have detailed some of the potential adverse effects of staples over growth plates. Most of these studies have consisted of observations of the histological and biomechanical consequences of the restriction of the expansion of the physis. The generally accepted belief is that the physeal changes are irreversible and that staples result in premature physeal closure if the staples are not removed within 2 years of the surgery. This has lead to the practice of avoiding the use of staples in adolescents whose physes are near natural closure. It is estimated that males reach skeletal maturity by the age of 21 years and girls by the age of 17 years. Methods for estimating bone age are associated with significant variability. A review of the literature reveals that staples inhibit the whole physis in order to stop the growth [22, 23].
In cases of recurrence, osteotomy is recommended [23, 24]. There is no general agreement on the ideal treatment. The objective of this article is to show the indications, surgical technique, complications and the results observed in correction of genu valgum during growth [25–30].
The percutaneous hemi-epiphysiodesis with cannulated screws with transphyseal compression for the correction of pathologic valgum of the knee in adolescents is a controversial method, but it has many benefits and no complications, such as malunion, nonunion, delay in consolidation, infection, neurovascular damage or compartmental syndrome. The difficulties with this technique are related to the expertise of the surgeon and the ability to determine the ideal age to operate. Advantages of this technique are that it is percutaneous, ambulatory and does not require rigid immobilization or post-surgical physical therapy. There is no need to wait for bone consolidation as is necessary with osteotomies, and gradual correction avoids associated danger to the neurovascular structures.
Contributor Information
Pedro Antonio Sánchez Mesa, Phone: +57-1-6770981, FAX: +57-1-7030651, Email: pedroantonio.sanchezmesa@gmail.com, http://www.clubcaderayrodilla.com.
Fernando Helo Yamhure, Email: ferhelo@cable.net.co, http://www.clubcaderayrodilla.com.
References
- 1.Blair VP, Walker SJ, Sheridan JJ, et al. Epiphysiodesis: a problem of timing. J Pediatr Orthop. 1982;2:281–284. doi: 10.1097/01241398-198208000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Sánchez M, Pedro A. Manual Práctico para Residentes de Ortopedia. Bogotá: Editorial Carbel; 2004. [Google Scholar]
- 3.Bylski-Austrow DI, Wall EJ, Rupert MP, et al. Growth plate forces in the adolescent human knee: a radiographic and mechanical study of epiphyseal staples. J Pediatr Orthop. 2001;21(6):817–823. [PubMed] [Google Scholar]
- 4.Phemister DB. Operative arrestment of longitudinal growth of bones in the treatment of deformities. J Bone Joint Surg Am. 1933;15:1–15. [Google Scholar]
- 5.Hass SL. Retardation of bone growth by a wire loop. J Bone Joint Surg (Am) 1945;27:25–36. [Google Scholar]
- 6.Blount WP. Control of bone growth by epiphyseal stapling: a preliminary report. J Bone Joint Surg Am. 1949;31:464–478. [PubMed] [Google Scholar]
- 7.Zuege RC, Kempken TG, Blount WP. Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am. 1979;61:320–329. [PubMed] [Google Scholar]
- 8.Stevens PM, Maguire M, Dales MD, Robins AJ (1999) Physeal stapling for idiopathic genu valgum. J Pediatr Orthop 19(5):645–649 [PubMed]
- 9.Bowen JR, Johnson WJ. Percutaneous epiphysiodesis. Clin Orthop. 1984;190:170–173. [PubMed] [Google Scholar]
- 10.Bowen JR, Torres RR, Forlin E. Partial epiphysiodesis to address genu varum or genu valgum. J Pediatr Orthop. 1992;12:359–364. doi: 10.1097/01241398-199205000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Timperlake RW, Bowen JR, Guille JT, et al. A prospective evaluation of fifty-three consecutive percutaneous epiphysiodesis of the distal femur and proximal tibia and fibula. J Pediatr Orthop. 1991;11:350–357. doi: 10.1097/01241398-199105000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Horton GA, Olney B. Epiphysiodesis of the lower extremity: results of the percutaneous technique. J Pediatr Orthop. 1996;16:180–182. doi: 10.1097/01241398-199603000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Canale ST, Russell TA, Holcomb RL. Percutaneous epiphysiodesis: experimental study and preliminary clinical results. J Pediatr Orthop. 1986;6:150–156. doi: 10.1097/01241398-198603000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Nouth F, Kuo LA. Percutaneous epiphysiodesis using transphyseal screws (PETS): prospective case study and review. J Pediatr Orthop. 2004;24:721–725. doi: 10.1097/01241398-200411000-00023. [DOI] [PubMed] [Google Scholar]
- 15.Gabriel KR, Crawford AH, Roy DR, et al. Percutaneous epiphysiodesis. J Pediatr Orthop. 1994;14(3):358–362. doi: 10.1097/01241398-199405000-00016. [DOI] [PubMed] [Google Scholar]
- 16.De Brauwer V, Moens PMD (2008) Temporary hemiepiphysiodesis for idiopathic genua valga in adolescents: percutaneous transphyseal screws (PETS) versus stapling. J Pediatr Orthop 28(5):549–554 [DOI] [PubMed]
- 17.Burghardt RD, Herzenberg JE, Shawn C, et al. Temporary hemiepiphyseal arrest using a screw and plate device to treat knee and ankle deformities in children: a preliminary report. J Child Orthop. 2008;2(3):187–197. doi: 10.1007/s11832-008-0096-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Metaizeau JP, Wong-Chung J, Bertrand H, et al. Percutaneous epiphysiodesis using transphyseal screws (PETS) J Pediatr Orthop. 1998;18:363–369. [PubMed] [Google Scholar]
- 19.Khoury J, Tavares J, Mcconnell S, et al. Results of screw epiphysiodesis for the treatment of limb length discrepancy and angular deformity. J Pediatr Orthop. 2007;27(6):623–628. doi: 10.1097/BPO.0b013e318093f4f4. [DOI] [PubMed] [Google Scholar]
- 20.Gómez A, Turriago CA, Jiménez ML (1996) Epifisiodesis química con quimopapaína Intrafisiaria: modelo experimental en conejos. Rev Colomb Ortop Traumatol 10(3):217–222
- 21.Lee C, Bier AD, Nickisch F, et al. Epiphysiodesis with infusion of stromal. J Bone Joint Surg Am. 2007;89:102–113. doi: 10.2106/JBJS.F.00198. [DOI] [PubMed] [Google Scholar]
- 22.Paley D, Tetsworth KT. Mechanical axis deviation of the lower limbs: preoperative planning of uniapical angular deformities of the tibia and femur. Clin Orthop. 1992;280:48–64. [PubMed] [Google Scholar]
- 23.Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57:259–261. [PubMed] [Google Scholar]
- 24.Guarniero R, Luzo CAM, Arena EC, et al. Correção de deformidade angular dos membros inferiores pela técnica de agrafagem. Genuvalgo. Rev Bras Ortop. 1994;29:19–23. [Google Scholar]
- 25.Fraser RK, Dickens DRV, Cole WG. Medial physeal stapling for primary and secondary genu valgum in late childhood and adolescence. J Bone Joint Surg Br. 1995;77:733–735. [PubMed] [Google Scholar]
- 26.Healy WL, Anglen JO, Wasilewski SA, Krackow KA. Distal femoral varus steotomy. J Bone Joint Surg Am. 1988;70(1):102–109. [PubMed] [Google Scholar]
- 27.Canale ST, Christian CA. Techniques for epiphysiodesis about the knee. Clin Orthop. 1990;255:81–85. [PubMed] [Google Scholar]
- 28.Liotta FJ, Ambrose TA, 2nd, Eilert RE. Fluoroscopic technique versus Phemister technique for epiphysiodesis. J Pediatr Orthop. 1992;12(2):248–251. doi: 10.1097/01241398-199203000-00019. [DOI] [PubMed] [Google Scholar]
- 29.Kramer A, Stevens PM. Anterior femoral stapling. J Pediatr Orthop. 2001;21(6):804–807. [PubMed] [Google Scholar]
- 30.Sharma L, Song J, Felson DT. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]


