Abstract
Objective
To explore, using recent data, whether and how risk factors for rheumatoid arthritis (RA) work disability may differ from previous studies.
Methods
Subjects were 953 individuals with RA from a US cohort who provided data semiannually over 18 months (years 2002–2005). A nested case–control design was used with matching on time of baseline data collection. All subjects were employed at baseline; cases were consistently not employed at followup, whereas controls remained employed. Hierarchical conditional logistic regression assessed the roles of demographic, RA disease, general health, and work factors as predictors of work disability. Recursive partitioning and causal modeling procedures were also used.
Results
Sample characteristics were mean age 51 years, 82% female, and 92% white. Older age (odds ratio [OR] 1.2, 95% confidence interval [95% CI] 1.1–1.4) and lower income (OR 1.7, 95% CI 1.0–2.7) predicted work disability, whereas more hours worked (OR 0.9, 95% CI 0.8–0.9) and preference to work full time (OR 0.2, 95% CI 0.1–0.4) or part time (OR 0.4, 95% CI 0.2–0.6) versus not to work were protective in the regression analysis. In recursive partitioning analyses, RA disease factors predicted work disability among older subjects, and functional limitation was the fourth most important factor. Job physical demand was not a significant or important factor.
Conclusion
In this contemporary data from a large RA cohort, older age, lower income, fewer working hours, and preference not to work were the risk factors for work disability. The impact of disease factors was limited to subjects ages ≥56 years. Job physical demand level had little impact.
Introduction
Work disability is a serious and common outcome for persons with rheumatoid arthritis (RA) (1–6). In previous studies, age, certain disease-related factors, and the characteristics of individuals' jobs have consistently been risk factors for RA work disability (1,2,6). However, changes over the past 10 to 20 years, such as improved pharmaceutical treatment of RA (7), possibly milder disease course (8), increased workforce participation of older workers (9), and decreased physical demand of US jobs (10,11) might have affected risk factors for RA work disability.
In recent studies we have provided evidence on changing patterns in the prevalence of work disability in people with RA (12–14). Although the prevalence of work disability remains high at ∼35% over 10 years (13), the rate of disability may be declining from the 50% rate reported in earlier RA studies (3,13). Risk of work disability among women newly diagnosed with RA also appears to be declining (12). The purpose of this study was to use recently collected data to explore whether and how risk factors for RA work disability may differ from previous studies.
Subjects and Methods
Data source
Data were obtained from the National Data Bank (NDB) longitudinal study of RA outcomes. NDB participants have rheumatologist-diagnosed RA and reside in the US. Approximately two-thirds were recruited consecutively from rheumatology practices, 90% of which are private, and one-third were from pharmaceutical company-sponsored registries. Participants are added continuously, and 8% per year decline to participate. Data are collected every 6 months by mail or online survey. The Boston University Medical Center Institutional Review Board granted ethical approval of this study.
Subjects
To be eligible for this study, NDB participants had to complete surveys conducted between January 2002 and July 2005, because detailed questions about employment were asked then. Second, they had to be employed during the period the survey was conducted. Because some individuals participate in surveys on a periodic basis, eligibility also required data provision over the next 3 surveys following the initial survey in which a participant reported being employed to ensure complete followup employment data. The survey in which a participant was employed was the subject's baseline survey, and the next 3 surveys were a subject's first, second, and third followup surveys. Finally, to avoid so-called “normal” age-related retirement, participants had to be age 63 years in the first followup survey.
Design
We used a nested case–control design. All subjects were employed at their baseline survey. Case (work disabled) subjects were not employed in the first followup survey and also in both subsequent followup surveys. This 12- to 18-month period of work cessation was required to eliminate short periods of unemployment. Control subjects remained employed in all surveys.
Cases and controls were matched on 2 possible confounding factors: time of subjects' baseline survey and completeness of data supplied. The time when subjects' baseline survey occurred varied over a 2-year period, and this could affect employment outcomes. Although we aimed to include only NDB participants with data over 4 consecutive surveys, to increase sample size we included those who did not complete the second followup survey, but who had the same employment status at first and third followup (not employed or employed in both surveys) under the assumption that their employment status was the same in all followup surveys. Examination of the strata formed by these 2 factors revealed that a maximum of 3 controls were available in all strata, so controls were matched 3:1 to cases.
Variables
Outcome measure
The work disability outcome was consistent not-employed status across the 3 followup surveys. Employment status at baseline had been based on responses to 3 questions. The first question asked whether subjects' “main form of work” was “unemployed, paid work, retired, housework, student, or disabled,” and the second question asked subjects whether they did any amount of employment work. Subjects whose response to the first question was “paid work” were classified as employed. Subjects whose response to the first question was “unemployed, retired, housework, student, or disabled,” but who simultaneously reported doing some amount of employment work, were also classified as employed. In addition, subjects had to report weekly or monthly work hours to be classified as employed. This definition of employment is similar to that used in the US Current Population Survey (15).
Predictor measures
Literature review indicated there were 4 categories of RA work disability risk factors: demographic, RA disease, general health, and work characteristics (1,2,6,16). Demographic variables were age, sex, race, marital status, educational attainment, and personal income from employment. Education was dichotomized at high school versus > high school education. Personal employment income was dichotomized at the 2004 US median income for individuals ($25,000) versus greater income (17).
Rheumatoid arthritis disease risk factors noted in the literature and available in our database were disease duration in years, functional limitation, pain, fatigue, and disease activity joint count (1,2,6). We also included a measure of RA global severity, and use of an anti—tumor necrosis factor (anti-TNF) agent based on work presented in a previous study (18). Functional status was assessed by the Health Assessment Questionnaire (HAQ) (19). Pain and fatigue were measured using 0–10 scales. Disease activity joint count was measured by the Rheumatoid Arthritis Disease Activity Scale (20,21). Global RA severity was assessed by the question, “Considering all the ways your illness affects you, rate how you are doing on the following scale,” with response measured on a 0 (very well) to 10 (very poor) scale.
General health risk factors were overall health status (excellent, good, fair, and poor), comorbidities, and depression. Comorbidity was measured by a patient-reported composite score (range 0–9) comprised of 11 present or past conditions including pulmonary disorders, myocardial infarction, other cardiovascular disorders, stroke, hypertension, diabetes, spine/hip/leg fracture, depression, gastrointestinal ulcer, other gastrointestinal disorders, and cancer (22,23). Depression was measured by the Arthritis Impact Measurement Scale depression items (24).
Work characteristics included number of hours worked per week, commuting difficulty, physical demand of a subject's job, self-employment, job type, presence and use of health insurance or retirement benefits, stressful job (25), co-worker and supervisor support (25), and preference to work (26). Commuting difficulty was assessed by 1 item with a 0–10 response scale (27). Job physical demand was assessed by 8 relevant items from a scale used in a US disability study (28,29). Subjects identified their type of job from 7 types modified from 1990 US Census Bureau occupational classifications (30); these were dichotomized into professional or managerial jobs versus other types. Stressful jobs were high demand and low control jobs (25,31). Subjects who responded positively to the question, “My job requires me to keep up with the pace set by others,” and negatively to the question, “I have a lot of freedom to decide how to do my work,” had stressful jobs. Coworker and supervisor support were assessed by the items, “People I work with are helpful and friendly,” and “My supervisor is helpful,” (31). Responses to each question were examined singly and in combination. Preference to work, assessed by the question, “Would you prefer to work full time, part time or not to work?” (26), was converted to 2 dummy variables, preference to work full time and preference to work part time, each versus not to work.
Statistical analyses
The sample was characterized using descriptive procedures. Baseline values of case and control subjects on the predictor variables were then compared using t-test or chi-square procedures. Baseline values of predictors were used in all analyses.
Multivariable regression analyses
The main analysis was conditional logistic regression to assess the roles of the independent variables as predictors of work disability (case/control status). Due to the large number of predictor variables, we constructed preliminary conditional logistic regression models of the predictors within each of the 4 variable categories. A final conditional logistic regression model was then constructed, which included variables that were significant in the preliminary regressions with P values equal to or less than 0.1, as well as variables generally considered to be important work disability factors, e.g., sex. The variables were entered in hierarchical fashion; demographic characteristics were entered first, followed by RA disease characteristics, general health, and finally work characteristics. In the work variable preliminary model, the level of the overall physical demand of subjects' jobs did not meet the level of P ≤ 0.1. Since a previous study (34) had shown that subjects with RA in all types of jobs reported extensive occupational hand use, the score for this single item from the job physical demand scale was substituted for the overall job physical demand score. It was significant at P = 0.05 and so was included in the final model.
Classification tree and random forest analyses
Although logistic regression analysis was our primary method of determining the roles of multiple variables in predicting work disability, it does not model all possible interactions among predictors, some of which are unforeseen. Complex interactions among demographic, disease and health, and work characteristics in relation to RA work disability are likely. Therefore, we used the nonparametric techniques of recursive partitioning to detect synergistic interactions among the various risk factors without requiring that interactions be specified in advance (33,34). We used the R software Rpart, version 3.1-38 (R Foundation for Statistical Computing, Vienna, Austria) for the construction of classification trees (34,35). Because recursive partitioning is designed to select important predictors out of a large pool of candidates, a wider variety of variables than in the conditional logistic regression models was included. Work disability (case/control status) was the outcome. We also used random forest techniques (R package RandomForest, R foundation for Statistical Computing) to provide a robust determination of which variables were most important in predicting work disability across a wide variety of classification trees for prediction of work disability (36,37).
Causal modeling
In the multivariable regression analyses, the preference to work variables were each strongly significant (P < 0.0001) in all models. To determine the basis of these relationships, we hypothesized that the preference to work variables mediated the effects of demographic, socioeconomic, disease and health, or work factors. We examined 2 pathways by which this could happen. In the first pathway, demographic and socioeconomic characteristics influenced work conditions, which in turn influenced preference to work. Preference to work then mediated the effect of these variables on employment status at followup. In the second pathway, demographic and socioeconomic characteristics influenced RA disease and health, which in turn influenced preference to work. As in the first pathway, preference to work mediated the influence of these variables on employment status at followup. We used hierarchical conditional logistic regression analyses to test each pathway.
Results
Sample characteristics
Of 1,088 eligible NDB participants, 953 subjects had complete baseline survey data, and 92% of these supplied data in all 4 surveys. The sample was predominantly middle-aged (mean age 51 years), female (82%), and white (92%) (Table 1). Mean RA duration was 13 years (range 1–57 years), and the mean HAQ score was 0.8, representing moderate functional limitation (Wolfe F: personal communication). Two-thirds (66%) of the sample were employed full time, and 43% held professional or managerial jobs.
Table 1. Sample characteristics at baseline (n = 953)*.
| Characteristic | Full sample |
|---|---|
| Age, mean ± SD years | 51 ± 9 |
| Women | 82 |
| White | 92 |
| More than high school education | 72 |
| Personal income from employment ≤$25,000† | 50 |
| RA duration, mean ± SD years | 13 ± 10 |
| Functional limitation, mean ± SD HAQ score‡ | 0.8 ± 0.6 |
| RA global severity, mean ± SD§ | 3.0 ± 2.3 |
| Use anti-TNF agent | 48 |
| Number of comorbidities, mean ± SD | 1.0 ± 1.4 |
| Employed full time | 66 |
| Professional/managerial job | 43 |
| Prefer to work full time | 42 |
| Prefer to work part time | 42 |
| Prefer not to work | 16 |
Values are the percentage unless indicated otherwise. RA = rheumatoid arthritis; HAQ = Health Assessment Questionnaire; anti-TNF = anti–tumor necrosis factor.
US median.
Range 0–3, where 0 = no limitation.
Status considering all effects of RA illness. Range 0–10, where 0 = very well and 10 = poor.
On average, 231 cases were 4 years older, less likely to have education beyond high school, and more likely to have a personal income that was less than or equal to the US median income than 722 controls (Table 2). Cases had RA for 2 years longer than controls and poorer health, including greater functional limitation, RA global severity, and more comorbidities. In regards to employment, cases worked fewer hours per week, had more difficulty in commuting to and from work, and were less likely to have a professional/managerial job or to prefer to work.
Table 2. Risk factors for work disability: comparison of work disability in cases and controls, and ORs (95% CIs) in preliminary regression models*.
| Risk factor | Cases (n = 231) |
Controls (n = 722) |
Preliminary model, OR (95% CI) |
|---|---|---|---|
| Demographic | n = 933 | ||
| Age, mean ± SD years | 54 ± 8 | 50 ± 8† | 1.3 (1.2–1.5)‡ |
| Women | 85 | 81 | 0.9 (0.6–1.4) |
| White | 94 | 92 | 1.4 (0.7–2.5) |
| Married | 76 | 73 | 1.0 (0.7–1.4) |
| More than high school education | 63 | 75† | 1.3 (0.9–1.8) |
| Personal income from employment ≤$25,000§ | 69 | 44† | 2.8 (1.9–4.0)¶ |
| RA disease | n = 860 | ||
| Duration | 15 ± 9.9 | 13 ± 9.4† | 1.1 (0.9–1.2)# |
| Functional limitation, mean ± SD** | 1.0 ± 0.7 | 0.7 ± 0.6† | 1.9 (1.3–2.6)¶ |
| RA global severity, mean ± SD†† | 3.8 ± 2.6 | 2.7 ± 2.2† | 1.1 (1.0–1.3)¶ |
| Pain, mean ± SD | 4.0 ± 2.7 | 3.2 ± 2.6† | 1.0 (0.9–1.1) |
| Arthritis activity, mean ± SD | 4.7 ± 2.7 | 3.8 ± 2.7† | 1.0 (1.0–1.1) |
| Fatigue, mean ± SD | 4.6 ± 2.9 | 3.9 ± 2.8† | 1.0 (0.9–1.0) |
| Stiffness ≥1 hour | 27 | 17† | 1.0 (0.9–1.2) |
| Use anti-TNF agent | 46 | 49 | 0.9 (0.6–1.3) |
| General health | n = 759 | ||
| Number of comorbidities, mean ± SD | 1.2 ± 1.4 | 0.9 ± 1.4† | 1.0 (0.9–1.2) |
| Depression, mean ± SD | 2.5 ± 1.9 | 2.1 ± 1.5† | 1.0 (0.9–1.2) |
| Fair or poor health status | 48 | 29† | 1.7 (1.2–2.2)¶ |
| Work | n = 820 | ||
| Hours worked/week, mean ± SD | 29 ± 16 | 37 ± 13† | 0.9 (0.8–0.9)‡‡ |
| Commuting difficulty, mean ± SD | 4.8 ± 5.2 | 3.7 ± 4.1† | 1.1 (1.0–1.1)¶ |
| Job physical demand, mean ± SD | 0.8 ± 0.4 | 0.9 ± 0.4 | 0.6 (0.4–1.1) |
| Job hand demand | 0.7 (0.5–1.0) | ||
| None/little | 8 | 3† | |
| Some | 21 | 16 | |
| A lot | 71 | 81 | |
| Stressful job | 23 | 19 | 1.4 (0.9–2.3) |
| Professional/managerial job | 30 | 48† | 0.7 (0.5–1.0) |
| Health or retirement benefits (versus none) | |||
| Either | 16 | 16 | 1.3 (0.7–2.3) |
| Both | 44 | 60 | 1.0 (0.6–1.7) |
| Coworker/supervisor support most or all the time | 72 | 73 | 0.9 (0.6–1.4) |
| Work preference (versus not working) | |||
| Part time | 43 | 42 | 0.3 (0.2–0.5)¶ |
| Full time | 21 | 46† | 0.2 (0.1–0.3)¶ |
Values are the percentage unless otherwise indicated. OR = odds ratio, 95% CI = 95% confidence interval; RA = rheumatoid arthritis; anti-TNF = anti–tumor necrosis factor.
P ≤ 0.05
Per 5 years; P ≤ 0.10.
US median.
P ≤ 0.10.
Per 5 years.
Health Assessment Questionnaire score, range 0–3, where 0 = no limitation.
Status considering all effects of RA illness. Range 0–10, where 0 = very well and 10 = poor.
Per 4 hours. P ≤ 0.10.
Analyses of multivariable regression
In the preliminary demographic variable regression model, only older age and lower income significantly predicted work disability (P < 0.0001 for each) (Table 2). However, we also included sex and education in the final regression model, as each has been a significant risk factor in several other studies (1,2,6). The RA joint count variable was strongly correlated with several other disease variables and so was excluded. Of the remaining RA variables, greater functional limitation (P = 0.0003), RA global severity (P = 0.004), and disease duration (P = 0.1) were included in the final multivariable model. The only significant variable in the general health preliminary model was poorer health status (P = 0.0007). Significant work characteristics in the preliminary model were number of hours worked per week (P = 0.0001), commuting difficulty (P = 0.01), self-employment (P = 0.001), and work preference (P < 0.0001). Professional/managerial job type (P = 0.06) and occupational hand use demand (P = 0.06) were also included in the final model.
In the final regression model, older age and income less than or equal to the US median increased the odds for work disability in step 1 and continued to do so after all other variables were entered (odds ratio [OR] 1.2 per 5 years of age, 95% confidence interval [95% CI] 1.1–1.4, and OR 1.7, 95% CI 1.0–2.7 respectively) (Table 3). Greater functional limitation and RA global severity increased the odds for work disability when added to age and income in step 2 and continued to predict it when health status was entered in step 3; however, their influence was diminished when work characteristics were entered in the final step. The work factors of greater number of hours worked per week (OR 0.9, 95% CI 0.8–0.9) and preference to work part time (OR 0.4, 95% CI 0.2–0.6) or full time (OR 0.2, 95% CI 0.1–0.4) each decreased the odds for work disability. Neither occupational hand use demand, nor overall job physical demand when substituted in the model, were significant.
Table 3. Results of the hierarchical conditional logistic regression predicting work disability (n = 772)*.
| Step | ||||
|---|---|---|---|---|
| Variable | 1 | 2 | 3 | 4 |
| Age, per 5 years | 1.3 (1.2–1.5) | 1.3 (1.2–1.5) | 1.3 (1.2–1.5) | 1.2 (1.1–1.4) |
| Sex | 0.9 (0.6–1.4) | 0.8 (0.5–1.3) | 0.8 (0.5–1.3) | 1.0 (0.6–1.8) |
| Education | 1.3 (0.9–1.8) | 1.2 (0.9–1.8) | 1.2 (0.9–1.7) | 1.1 (0.7–1.7) |
| Personal income from employment ≤$25,000 | 2.7 (1.9–3.9) | 2.4 (1.7–3.5) | 2.4 (1.6–3.4) | 1.7 (1.0–2.7) |
| Disease duration, per 5 years | 1.0 (0.9–1.1) | 1.0 (0.9–1.1) | 1.0 (0.9–1.2) | |
| HAQ functional limitation score | 1.5 (1.1–2.0) | 1.4 (1.0–1.9) | 1.2 (0.8–1.7) | |
| RA global severity† | 1.1 (1.0–1.2) | 1.1 (1.0–1.2) | 1.1 (0.9–1.2) | |
| General health status | 1.2 (0.9–1.6) | 1.2 (0.8–1.7) | ||
| Hours worked/week, per 4 hours | 0.9 (0.8–0.9) | |||
| Occupational hand demand | 0.8 (0.7–1.1) | |||
| Commuting difficulty | 1.0 (0.9–1.1) | |||
| Self-employment | 1.5 (0.9–2.4) | |||
| Professional/managerial job | 0.8 (0.5–1.2) | |||
| Prefer to work part time‡ | 0.4 (0.2–0.6) | |||
| Prefer to work full time‡ | 0.2 (0.1–0.4) | |||
Values are the odds ratio (95% confidence interval). HAQ = Health Assessment Questionnaire; RA = rheumatoid arthritis.
Measure of overall effect of rheumatoid arthritis
Versus preference to not work.
Analyses of classification tree and random forest
The classification tree with the least error produced splits on only 3 risk factors (age, RA global severity, and functional limitation) and provided little information. The second tree, which had an acceptable level of error, split on 3 additional factors (Figure 1). The first split was by age, <56 years and ≥56 years. Younger subjects were more likely to be employed than older subjects (83% versus 59%), and in these younger subjects lower income, self-employment, and lower job physical demand helped classify work disability cases. In contrast, greater RA global severity and functional limitation helped to classify work disability cases among older subjects. In the random forest analysis, age was ranked the most important variable, followed by duration of RA, number of work hours, functional limitation, and RA global severity (Table 4).
Figure 1.
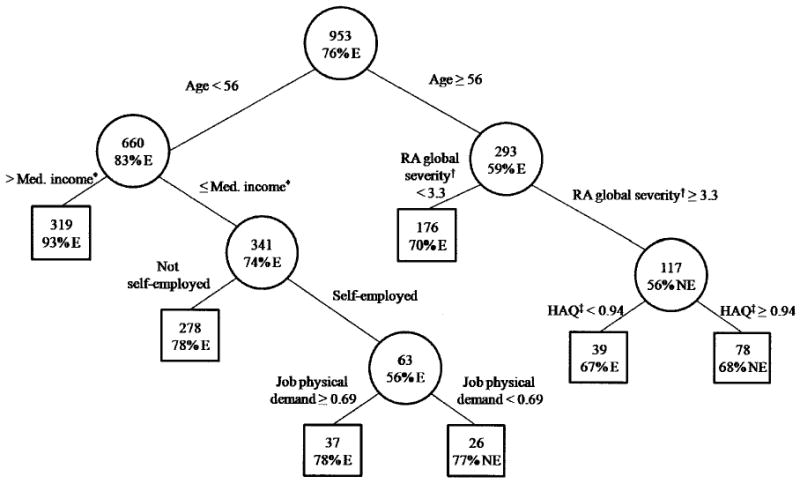
Classification tree of employment status at followup. Boxes are final nodes. The top number is number of subjects, and the bottom number is the percentage is the dominant proportion; E = employed; NE = not employed; * = personal income from employment, range 0–1 where 1 = ≤ US median income; † = status considering all RA effects, where higher score = poorer status; ‡ = Health Assessment Questionnaire (HAQ) measure of functional limitation, where higher scores = greater limitations.
Table 4. Importance of risk factors for work disability: results of random forest analysis*.
| Variable† | Decrease in Gini index‡ | Importance rank§ |
|---|---|---|
| Age | 54.04 | 1 |
| RA duration | 39.94 | 2 |
| Hours worked/week | 35.77 | 3 |
| HAQ score | 32.97 | 4 |
| RA global severity | 30.05 | 5 |
| Job physical demand | 26.77 | 6 |
| Commuting difficulty | 25.78 | 7 |
| Health status | 11.43 | 9 |
| Prefer to work full time | 11.11 | 10 |
| Income | 10.07 | 11 |
| Education | 7.48 | 12 |
| Prefer to work part time | 7.24 | 13 |
| Professional/managerial job | 7.22 | 14 |
| Self-employment | 6.56 | 15 |
| Sex | 4.15 | 19 |
RA = rheumatoid arthritis; HAQ = Health Assessment Questionnaire.
From the hierarchical conditional logistic regression. High school education or less; personal income from employment ≤$25,000; HAQ measure of functional limitation; measure of overall effect of rheumatoid arthritis; excellent, good, fair, poor health; preference to work part or full time vs. not working.
Evaluates how discrimination into employed vs. unemployed categories degrades when a predictor is removed from classification trees in the random forest; larger decreases imply better discrimination when that variable is used.
Variables not shown: race, marital status, comorbidities, stressful job, use of an anti-tumor necrosis factor agent.
Causal model analyses
In both pathways all variables remained significant when the preference to work-related variables were entered. Preference to work therefore did not mediate work conditions or RA and health factors.
Discussion
In these recent data from a US national cohort of subjects with RA, older age and the work-related factors of lower income from employment, fewer hours worked per week, and preference not to work predicted work disability in the main analysis using multivariable regression. Four reviews of the RA work disability literature (1,2,6,16) found that greater functional limitation and physically demanding jobs were prominent risk factors in almost all studies. The results from our main analysis therefore differ from most prior studies in that neither of these factors predicted work disability.
The significance of functional limitation and RA global severity in the hierarchical regression model was reduced when work-related factors were entered, suggesting their effect was mediated by the characteristics of subjects' work. This is surprising given the strength of functional limitation, or other disease variables, in prior studies and raises the possibility that disease factors are now less prominent due to improved disease status.
However, there are other possible explanations. The first is our use of a work disability definition that includes any work cessation, irrespective of its cause, e.g., whether attributed to RA or to early retirement. We used this definition for 3 reasons. First, we wished to make our results comparable with other US studies, and 2 prominent studies had defined work disability as any work cessation (3,5). Disease factors were significant predictors of work disability in both studies. A third prominent study used RA-attributed work cessation as the outcome (4), and when we used this outcome in our study, disease factors remained significant in the final regression model. A second reason for using the any work cessation definition is that although a decision to stop working is likely to be influenced by a person's health (Yelin E: personal communication), this influence may be partial and not recognized. The any work cessation definition includes work cessation partly, as well as mostly, due to RA. Finally, subjects who cite RA as the cause of their work cessation may have more severe disease. So RA-attributed work disability, as well as definitions such as self-reported disability or Social Security disability (14), may be defined in part by severe disease. It could be expected then that disease factors would predict this level of work disability.
Another possible explanation for the lack of significance of disease factors is that functional limitation and RA global severity are both self-reported measures and therefore subject to response set bias, e.g., influenced by adaptation to disease. Studies using rheumatologist-reported clinical indicators like number of disease flares showed such indicators have their greatest impact on employment early in the disease process (5,12,26). The mean disease duration of our sample was 13 years, and this could explain the diminished effect of disease variables in our study. However, Eberhardt et al found that self-reported functional limitation, measured by the HAQ, was a strong predictor of RA work disability at all lengths of disease duration (38). Furthermore, the importance of clinical indicators in predicting work disability was diminished in a cohort recruited in 1998 compared with a cohort recruited in 1987 (12), which could indicate improved disease status.
Results of the recursive partition analyses revealed that disease factors have some continuing influence. Disease duration was ranked as the second most important factor in the random forest analysis, and functional limitation and RA global severity classified work disability cases among older subjects and were ranked fourth and fifth in importance.
The lack of predictive capacity of greater job physical demand in our study could be due to our sample's relatively long mean disease duration. Subjects with the most demanding jobs may already have stopped working and therefore were not eligible for our sample. The study by Eberhardt et al suggested that the effect of heavy manual jobs was greatest in the early years of disease (38). The physical demand of jobs in the US has been declining for some time, however, and is a possible explanation of reduced prevalence of RA work disability (16).
Older age was the most prominent predictor of work disability. It was significant in the regression analysis, and ranked first in importance. An interaction between age and RA disease variables emerged through recursive partitioning analysis, showing that disease severity was an important determinant of work disability in older subjects. It is not clear why disease factors were so important among older subjects. We considered the possibility of treatment disparity (39); however, equal portions of older and younger subjects used an anti-TNF agent.
Other significant predictors of work disability in the regression analysis were lower income, fewer hours worked per week, and personal preference not to work versus to work either full or part time. Many studies (40) concur in finding that the structure of work and reduced number of hours worked increases risk for work disability. Reisine et al found that subjects with RA who worked <30 hours/week were more apt to stop working and suggested this could indicate lower work commitment (26). In our study, number of hours worked was ranked third in importance in the random forest analysis.
Reisine et al were the first to assess preference to work, and they also found it predicted which subjects became work disabled (26). The causal modeling analyses indicated that neither the conditions of subjects' jobs nor their degree of disease severity affected their preference to work. Although preference not to work was significant in the regression analysis, it was ranked low in importance by the random forest analysis, probably because few subjects preferred not to work.
Our data suggest that older patients may be particularly vulnerable to the effects of disease on employment. Employment maintenance among older workers is an increasingly important goal, both for individuals and society (11). Our results suggest that reducing employment hours is not an effective employment maintenance strategy, most likely due to its impact on income. Two prior studies (5,25) found self-employment was associated with work retention. However, in our study it was not significant in the regression analysis. The classification tree analysis may offer an explanation of this discrepancy; self-employment predicted work disability only when it was combined with low job physical demand. Low job physical demand could be a marker for minimal work effort capacity, and if so, self-employment is effective only when the individual is capable of making a substantial work effort.
Strengths of our study are availability and use of recent data from a US national cohort of patients with rheumatologist-diagnosed RA and detailed assessment of employment information. Furthermore, we used several different methods of analysis, and this has provided a more complete picture of the relative importance of the risk factors, as well as information about the basis of work preference.
The generalizability of our findings may be restricted because our sample is not representative of all persons with RA. One-third of NDB participants are from pharmaceutical registries. Registry subjects were more likely to be male (23% versus 16%), have shorter disease duration (12 versus 14 years), have greater functional limitation (mean HAQ score 0.9 versus 0.8), and less likely to have a professional/managerial job (38% versus 46%) than non-registry subjects. However, the difference in the proportion of registry subjects among cases and controls (34% versus 31%) was quite small. About 12% of NDB participants were not eligible for this study because they fill out short questionnaires containing no questions about employment. These individuals were less likely to be white (84% versus 89%), married (68% versus 73%), or have education beyond high school (45% versus 61%) than subjects. Participants (n = 3,680) who supplied data on an irregular basis were 1 year younger, more likely to be male (22% versus 18%) or nonwhite (90% versus 92%), and had 1 year shorter disease duration than 1,088 eligible participants. Our sample was not population based. Subjects were more often white and had higher educational attainment than the US population. Consequently, persons with physically demanding jobs were probably under-represented in our sample.
In summary, the results of these recent data from a US national cohort differ from previous studies in that neither disease factors nor job physical demand were significant risk factors for RA work disability in the main analysis. Disease factors were important risk factors in alternative analyses, however, especially among older subjects. Older age, lower income from employment, fewer hours worked per week, and preference not to work were the significant risk factors for work disability in the main analysis.
Acknowledgments
Supported by grant P60-AR47785 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Footnotes
Author Contributions: Dr. Allaire had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study design. Allaire, LaValley.
Acquisition of data. Allaire, Wolfe.
Analysis and interpretation of data. Allaire, Wolfe, Niu, LaValley, Zhang, Reisine.
Manuscript preparation. Allaire, Wolfe, Reisine.
Statistical analysis. Allaire, Niu, LaValley, Zhang.
References
- 1.Allaire SH. Update on work disability in rheumatic diseases. Curr Opin Rheumatol. 2001;13:93–8. doi: 10.1097/00002281-200103000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Verstappen SM, Bijlsma JW, Verkleij H, Buskens E, Blaauw AA, ter Borg EJ, et al. Overview of work disability in rheumatoid arthritis patients as observed in cross-sectional and longitudinal surveys. Arthritis Rheum. 2004;51:488–97. doi: 10.1002/art.20419. [DOI] [PubMed] [Google Scholar]
- 3.Yelin E, Henke C, Epstein W. The work dynamics of the person with rheumatoid arthritis. Arthritis Rheum. 1987;30:507–12. doi: 10.1002/art.1780300504. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe F, Hawley DJ. The longterm outcomes of rheumatoid arthritis work disability: a prospective 18 year study of 823 patients. J Rheumatol. 1998;25:2108–17. [PubMed] [Google Scholar]
- 5.Reisine S, Fifield J, Walsh SJ, Feinn R. Factors associated with continued employment among patients with rheumatoid arthritis: a survival model. J Rheumatol. 2001;28:2400–8. [PubMed] [Google Scholar]
- 6.Sokka T. Work disability in early rheumatoid arthritis. Clin Exp Rheumatol. 2003;21(5 Suppl 31):S71–4. [PubMed] [Google Scholar]
- 7.Kremers HM, Nicola P, Crowson CS, O'Fallon WM, Gabriel SE. Therapeutic strategies over a 40-year period. J Rheumatol. 2004;31:2366–73. [PubMed] [Google Scholar]
- 8.Welsing PM, Fransen J, van Riel PL. Is the disease course of rheumatoid arthritis becoming milder? Time trends since 1985 in an inception cohort of early rheumatoid arthritis. Arthritis Rheum. 2005;52:2616–24. doi: 10.1002/art.21259. [DOI] [PubMed] [Google Scholar]
- 9.Toosi M. Labor force projections to 2016: more workers in their golden years. Mon Labor Rev. 2007;11:33–52. [Google Scholar]
- 10.Toosi M. A century of change: the US labor force, 1950–2000. Mon Labor Rev. 2002;5:15–28. [Google Scholar]
- 11.Hecker DE. Occupational employment projections to 2010. Mon Labor Rev. 2001;11:57–84. [Google Scholar]
- 12.Reisine S, Fifield J, Walsh S, Dauser D. Work disability among two cohorts of women with recent-onset rheumatoid arthritis: a survival analysis. Arthritis Rheum. 2007;57:372–80. doi: 10.1002/art.22620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Allaire S, Wolfe F, Niu J, LaValley MP. Contemporary prevalence and incidence of work disability associated with rheumatoid arthritis in the US. Arthritis Rheum. 2008;59:474–80. doi: 10.1002/art.23538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wolfe F, Allaire S, Michaud K. The prevalence and incidence of work disability in rheumatoid arthritis, and the effect of anti-tumor necrosis factor on work disability. J Rheumatol. 2007;34:2211–7. [PubMed] [Google Scholar]
- 15.U.S. Census Bureau. Basic monthly survey CPS questionnaire. URL: http://www.bls.census.gov/cps/bqestair.htm.
- 16.Burton W, Morrison A, Maclean R, Ruderman E. Systematic review of studies of productivity loss due to rheumatoid arthritis. Occup Med (Lond) 2006;56:18–27. doi: 10.1093/occmed/kqi171. [DOI] [PubMed] [Google Scholar]
- 17.US Census Bureau. Statistical abstract of the United States. Washington DC: 2007. Table 682. www.census.gov/prod/2006pubs/07statab/income.pdf. [Google Scholar]
- 18.Allaire S, Wolfe F, Niu J, Zhang Y, Zhang B, LaValley MP. Evaluation of the effect of anti–tumor necrosis factor agent use on rheumatoid arthritis work disability: the jury is still out. Arthritis Rheum. 2008;59:1082–9. doi: 10.1002/art.23923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fries JF, Spitz PW. Dimensions of health outcome: the Health Assessment Questionnaire. J Rheumatol. 1982;9:789–93. [PubMed] [Google Scholar]
- 20.Stucki G, Liang MH, Stucki S, Bruhlmann P, Michel BA. A self-administered rheumatoid arthritis disease activity index (RADAI) for epidemiologic research: psychometric properties and correlation with parameters of disease activity. Arthritis Rheum. 1995;38:795–9. doi: 10.1002/art.1780380612. [DOI] [PubMed] [Google Scholar]
- 21.Fransen J, Langenegger T, Michel BA, Stucki G. Feasibility and validity of the RADAI, a self-administered rheumatoid arthritis disease activity index. Rheumatology (Oxford) 2000;39:321–7. doi: 10.1093/rheumatology/39.3.321. [DOI] [PubMed] [Google Scholar]
- 22.Michaud K, Wolfe F. The development of a rheumatic disease research comorbidity index for use in outpatients with RA, OA, SLE and fibromyalgia (FMS) [abstract] Arthritis Rheum. 2007;56 9:S596. [Google Scholar]
- 23.Michaud K, Wolfe F. Comorbidities in rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2007;21:885–906. doi: 10.1016/j.berh.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Meenan RF, Mason JH, Anderson JJ, Guccione AA, Kazis LE. AIMS2: the content and properties of a revised and expanded Arthritis Impact Measurement Scales Health Status Questionnaire. Arthritis Rheum. 1992;35:1–10. doi: 10.1002/art.1780350102. [DOI] [PubMed] [Google Scholar]
- 25.Lacaille D, Sheps S, Spinelli JJ, Chalmers A, Esdaile JM. Identification of modifiable work-related factors that influence the risk of work disability in rheumatoid arthritis. Arthritis Rheum. 2004;51:843–52. doi: 10.1002/art.20690. [DOI] [PubMed] [Google Scholar]
- 26.Reisine S, McQuillan J, Fifield J. Predictors of work disability in rheumatoid arthritis patients: a five-year followup. Arthritis Rheum. 1995;38:1630–7. doi: 10.1002/art.1780381115. [DOI] [PubMed] [Google Scholar]
- 27.Allaire SH, Anderson JJ, Meenan RF. Reducing work disability associated with rheumatoid arthritis: identification of additional risk factors and persons likely to benefit from intervention. Arthritis Care Res. 1996;9:349–57. doi: 10.1002/1529-0131(199610)9:5<349::aid-anr1790090503>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 28.Bye B, Schecter E. 1978 survey of disability and work: technical introduction. Washington, DC: US Social Security Administration; 1982. pp. 13–11745. [Google Scholar]
- 29.US Social Security Administration. User's manual: 1978 survey of disability and work. Washington, DC: US Social Security Administration; 1981. pp. 13–11732. [Google Scholar]
- 30.US Census Bureau. Statistical abstract of the United States: 2000. Washington, DC: US GPO; 2001. Labor force, employment and earnings, and employed civilians by occupation, sex, race and Hispanic origin: 1983 and 1999; p. 401. [Google Scholar]
- 31.Karasek RA, Theorell T. Healthy work: stress, productivity and the reconstruction of working life. New York: Basic Books; 1990. [Google Scholar]
- 32.Allaire S, Wolfe F, Niu J, Baker N, Michaud K, LaValley M. Extent of occupational hand use among persons with rheumatoid arthritis. Arthritis Rheum. 2006;55:294–9. doi: 10.1002/art.21839. [DOI] [PubMed] [Google Scholar]
- 33.Bloch DA, Moses LE, Michel BA. Statistical approaches to classification. Arthritis Rheum. 1990;33:1137–44. doi: 10.1002/art.1780330813. [DOI] [PubMed] [Google Scholar]
- 34.Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and regression trees. Monterey (CA): Wadsworth; 1984. [Google Scholar]
- 35.R Development Core Team. Vienna (Austria): R Foundation for Statistical Computing; 2008. R: a language and environment for statistical computing. URL: http://www.R-project.org. [Google Scholar]
- 36.Breiman L. Random forests. Mach Learn. 2001;45:5–32. [Google Scholar]
- 37.Breiman L. Manual on setting up, using, and understanding random forests v3.1. 2002 URL: http://oz.berkeley.edu/users/breiman/Using_random_forests_V3.1.pdf.
- 38.Eberhardt K, Larsson BM, Nived K, Lindqvist E. Work disability in rheumatoid arthritis: development over 15 years and evaluation of predictive factors over time. J Rheumatol. 2007;34:481–7. [PubMed] [Google Scholar]
- 39.Schmajuk G, Schneeweiss S, Katz JN, Weinblatt ME, Setoguchi S, Avorn J, et al. Treatment of older adult patients diagnosed with rheumatoid arthritis: improved but not optimal. Arthritis Rheum. 2007;57:928–34. doi: 10.1002/art.22890. [DOI] [PubMed] [Google Scholar]
- 40.Yelin E. Work disability in rheumatic diseases. Curr Opin Rheumatol. 2007;19:91–6. doi: 10.1097/BOR.0b013e3280126b66. [DOI] [PubMed] [Google Scholar]


