Abstract
Background and objectives: Treatment without catheter replacement (catheter salvage) has been described for bacteremia associated with tunneled venous catheters in hemodialysis patients, but few data are available on which to base an estimation of the likelihood of treatment success.
Design, setting, participants, & measurements: In a prospective cohort study, all cases of catheter-associated bacteremia that occurred in a large dialysis center were identified during a 12-mo period. Catheter salvage was attempted according to a standard protocol in all cases in which a favorable early response to antibiotic therapy was seen, and patients were followed for at least 6 mo. Bacteremias, catheter changes, and all major clinical events were recorded.
Results: During a period covering 252,986 catheter days, 208 episodes were identified involving 133 patients, 74% of which were selected for attempted salvage. Salvage was successful in 66.1% of incident bacteremias with a very low complication risk (0.9%). Some bacteremias, however, recurred as late as 6 mo after the initial infection; salvage was less likely to be successful in treating recurrences.
Conclusions: Appropriately used catheter salvage can be successful in approximately two thirds of cases; however, recurrences continue to occur up to 6 mo later and are unlikely to be cured without catheter replacement.
Tunneled venous catheters are a common form of hemodialysis access, despite general agreement that an arteriovenous fistula should be the first choice when possible (1). Rates vary among regions, being lower in Japan and much of Europe than in British or American units, where catheter prevalence is >25% (2), and have been increasing in some countries (3). Catheter use occurs when patients are waiting for access surgery or for fistulas to mature (4) but also in a significant number of patients without appropriate vascular anatomy for fistula creation (5).
One of the chief hazards associated with catheter use is infection, which is thought to account for the up to 50% increase in mortality reported relative to fistulas (6). A bacteremia frequency of 3.9 episodes per 1000 catheter days was typical in older studies (7), whereas rates of 1.7 to 2.2 per 1000 catheter days have been reported more recently (8,9). A rate of one episode per 1000 catheter days is now considered achievable with optimal practice, including prompt recognition and treatment of exit-site infection (10), as was found in a recent meta-analysis of studies that used topical prophylaxis (11). Lower rates and low mortality, however, have been reported with catheter use in studies from Italy and the United Kingdom (12,13).
Traditionally, management of bacteremia included catheter removal and replacement, but treatment with antibiotics alone, without catheter replacement, can be successful (14). This strategy of attempted catheter salvage is popular with patients; limits the number of access procedures, thereby reducing the risk for venous stenosis (15); and may be particularly useful for patients with previous complications.
Assessing the likelihood of success with this strategy, observational studies have reported treatment failure occurring in up to half of cases after attempted salvage (7,16,17). Most recently, Mokrzycki et al. (16) reported that catheter salvage was a risk factor for treatment failure in a study that included 49 cases of attempted salvage, with recurrence and complication rates of 20 and 18%, respectively. Catheter management decisions were not made according to a specific protocol, however, with a variety of treatment strategies used across units according to undefined criteria. In addition, less than one quarter of cases were selected for salvage, with younger patients without diabetes being overrepresented in this group. No substantial studies with random assignment of catheter management strategy have been published.
There is general agreement that catheters should be removed in patients who present with severe sepsis, as well as those who respond slowly or poorly to antibiotic therapy, but outside of these criteria (as the majority of patients present), salvage may be a reasonable strategy; the effect of attempted salvage in unselected patients from this majority is unknown. This prospective, observational study provides novel information by reporting outcomes in a large cohort of patients for whom salvage was attempted in all cases deemed to be clinically reasonable by specific criteria.
Materials and Methods
In a large renal center, we prospectively identified during a 12-mo period all cases of bacteremia that occurred in hemodialysis patients with tunneled venous catheters. The mean age of this predominantly white and South Asian dialysis population is 61.1, with 38.7 and 32.8% having diabetes or ischemic heart disease, respectively. The catheter prevalence within this hemodialysis population was 64.1%. Most cases were identified as they occurred by the nurse in charge of each unit during the year, but to prevent omissions, clinical notes and microbiology records were checked for possible bacteremia episodes for all hospital admissions and all deaths that occurred at home. All episodes of bacteremia in patients with tunneled dialysis catheters were defined as catheter related, unless an alternative source of infection was apparent at onset or subsequently identified.
Treatment decisions were made by the physician in charge of the unit or ward. All patients were treated according to a uniform protocol, whereby catheter salvage was attempted when clinically reasonable (i.e., in all cases in which the clinical presentation was not severe [no hypotension or other features of severe sepsis] and an adequate initial response to antibiotic treatment was seen within 48 h [afebrile and symptoms largely resolved]). Empirical treatment consisted of vancomycin and meropenem, with subsequent therapy according to microbiology results, continuing for a total duration of 6 wk. All Gram-positive infections were treated with two agents: Usually intravenous vancomycin with oral fusidic acid or rifampicin, whereas Gram-negative infections were treated with meropenem or ciprofloxacin. Vancomycin dosage was adjusted between 500 mg and 1 g according to body weight and given twice or three times per week depending on trough levels (target 5 to 10 mg/L). The same systemic antibiotics were used in patients who were known to be colonized with methicillin-resistance Staphylococcus aureus. No antibiotic catheter locks were used for prophylaxis or treatment during this period of observation; most locking solutions consisted only of 5000 U/ml heparin.
When indicated (by features of severe sepsis or the persistence of fever after 48 h of antibiotic therapy), catheter removal was carried out within 24 h of the decision. The duration of the catheter-free interval before replacement depended on clinical circumstances but was at least 48 h in all cases. Antibiotics were continued for 2 wk after catheter replacement.
Outcomes were determined for all patients after a minimum follow-up period of 6 mo, from patients' records. Recurrence was defined as subsequent bacteremia with the same organism during the follow-up period, and complication was defined as infection-related death or a subsequent metastatic infection, such as osteomyelitis or endocarditis. Deaths were regarded as infection related when they occurred before clinical recovery or discharge from hospital or within 1 mo of a positive blood culture. χ2 and Fisher exact test were used as appropriate to test for differences in outcome frequencies between groups, with P < 0.05 regarded as significant.
Results
During an observation period covering 252,986 catheter days, 208 catheter-related bacteremia episodes were identified, giving an incidence of 0.82 per 1000 catheter days, which equates to one event per 40 mo. Bacteremia episodes involved 133 patients, aged 29 to 95 (mean 63.7), 39% of whom had diabetes and 47% of whom had clinical vascular disease. Less common comorbidities included sickle cell anemia, sclerosing peritonitis, liver transplantation, HIV infection (two patients), malignancy (three patients), and prosthetic valve or pacemaker (six patients). Incident bacteremia episodes closely followed a Poisson distribution, with bacteremia episodes occurring in 19.1% of patients per year at risk.
Organisms isolated were S. aureus in 15.9%, other Gram-positive organisms in 50.7% and Gram-negative organisms in 31.4%, with nontuberculous Mycobacteria accounting for two cases and Candida species in two others. Most cases were symptomatically mild, with less than half of bacteremia episodes (96 [46.2%] episodes) resulting in hospital admission. Initial catheter strategy was replacement in 49 (23.6%) and attempted salvage in 154 (74.0%); in the remaining five cases, the catheter was removed as was no longer needed, because a fistula was just maturing. Patients who were admitted to hospital were more likely to have catheters replaced (39.8% of those admitted versus 10.9% of outpatients; P < 0.001), reflecting the increased severity of the clinical presentation in this group.
Attempted salvage of incident bacteremias achieved a cure, defined as no recurrence or complication during follow-up, in 76 (66.1%) of 115 cases. The minimum and average follow-up periods were 6 and 8 mo, respectively. All bacteremias with the same organism were defined as recurrences, but within the cured group, new bacteremias (with a different organism) occurred slightly but not significantly more frequently than the baseline rate (risk ratio 1.39; P = 0.3).
Compared with the catheter replacement group, recurrent bacteremia was more common after salvage, occurring in 33.0% of cases versus 8.1% in the replacement group (P < 0.001; Table 1). Complications were uncommon, however, occurring in 0.9% (compared with 14.3% in the replacement group; P < 0.001); thus, complications were largely restricted to those with a more severe clinical presentation, who therefore were selected for catheter replacement. After recurrence of bacteremia, a subsequent attempt to salvage the catheter was less likely to be successful (Table 1), with a greater likelihood of recurrence (53.8 versus 33.0% for first salvage attempt; P = 0.02) and a greater risk for complications (7.7 versus 0.9%; P = 0.05). There was no influence of age, diabetes, or the presence of vascular disease on outcome after salvage.
Table 1.
Outcome by catheter management
| Parameter | Replaced | Salvage Attempted |
P | |
|---|---|---|---|---|
| First | Subsequent | |||
| Total | 49 | 115 | 39 | |
| Recurrences (n [%]) | 4 (8.1) | 38 (33.0) | 21 (53.8) | 0.02 |
| Complications (n [%]) | 7 (14.3) | 1 (0.9) | 3 (7.7) | 0.05 |
Catheter replacement is associated with lower recurrence rates but more complications; this is because complications are largely restricted to those whose clinical presentation is more severe, who are therefore selected for catheter replacement. If the first salvage attempt fails, then subsequent salvage attempts are followed by a greater likelihood of recurrence, as well as complications. P values refer only to the difference between first and subsequent salvage outcomes.
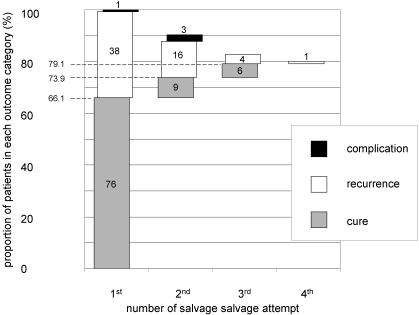
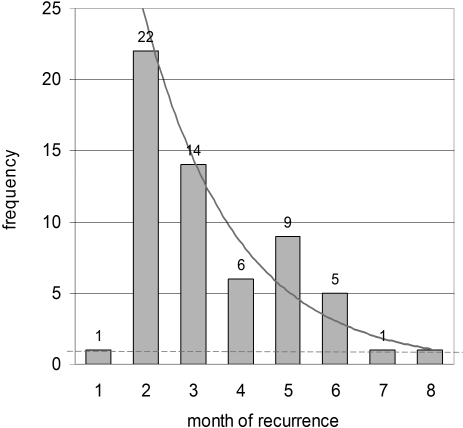
Allowing successive attempts did increase the number of catheters that were ultimately salvaged successfully (Figure 1), but the complication risk was increased, and, of the 91 catheters ultimately salvaged, 76 (83.5%) were successfully treated at the first attempt. In those with recurrence after salvage, time to recurrence was distributed exponentially, as expected, returning to baseline levels at approximately 6 mo after initial infection (Figure 2). Of 59 recurrences after attempted salvage, 22 (37.3%) occurred after the first 3 mo of follow-up. Recurrence time in these cases was not influenced by microbiological isolate.
Figure 1.
Outcome over successive salvage attempts in those with incident infections that first were managed with attempted salvage. Of those with recurrent bacteremia after the initial salvage attempt (□, left), most were deemed suitable for an additional salvage attempt and are represented in the second column. Actual patient numbers are given within the chart. The total percentage successful salvage increases with multiple attempts, but the proportion of cures at each subsequent stage is smaller.
Figure 2.
Distribution of recurrence times after attempted salvage from the date of positive blood culture. After finishing antibiotic therapy, the recurrence times closely follow an exponential distribution (solid line) not returning to baseline until after 6 mo. For comparison, the expected background rate is shown (dashed line).
Of the three main groups of organism, Gram-positive organisms other than S. aureus were less likely to result in hospital admission (P = 0.02) and tended to be selected for salvage more often (P = 0.1), but there were no significant differences in salvage outcomes between organisms (Table 2). Catheter salvage was not attempted for fungal or mycobacterial infections. In the replacement group, S. aureus was associated with more complications than other organisms, accounting for four of the seven complications (P = 0.04). Significant adverse events clearly related to antibiotic therapy were rare but included one widespread rash and two diarrheal illnesses that resulted in hospital admission.
Table 2.
Outcome by organism
| Parameter | SA | GP | GN | P |
|---|---|---|---|---|
| Total incident | 23 | 72 | 44 | |
| Admitted (n [%]) | 12 (57.1) | 28 (38.4) | 28 (65.1) | 0.02 |
| Salvage attempted (n [%]) | 18 (78.3) | 64 (88.9) | 33 (75.0) | 0.1 |
| Recurrence after salvage (n [%]) | 7 (38.9) | 19 (29.7) | 12 (36.4) | 0.8 |
| Complication after salvage (n [%]) | 0 (0.0) | 1 (1.6) | 0 (0.0) | 0.7 |
Gram-positive infections were less likely to result in admission to hospital, but there were no significant differences in the likelihood of salvage being attempted or in salvage outcomes between the main groups of organism. GN, Gram-negative organisms; GP, other Gram-positive organisms; SA, Staphylococcus aureus.
All of the catheters in this study were sited in the internal jugular vein apart from three inferior vena cava catheters; salvage was attempted for all of these, with two cures and one recurrence. Salvage was not attempted in bacteremia episodes that were associated with clinical evidence of exit-site or tunnel infection, but despite prompt catheter removal, complications were more common in these cases, occurring in four of 11 (P = 0.04).
Discussion
Several studies have suggested that although catheter salvage is often successful, recurrent bacteremia occurs in approximately half of cases, with complications in up to 13% (17,18). In this study, in which salvage was attempted in all clinically reasonable cases (74%), we found that treatment was successful in two thirds of cases, with recurrence occurring in one third but very few complications. These data, in patients selected only by early clinical criteria, are broadly applicable and will help physicians to give accurate advice to patients and to determine the role of catheter salvage within their dialysis programs.
The outcomes that we observed were generally more favorable than one might have expected from previous literature. Selection bias, perhaps favoring salvage in patients with fewer alternative access options, may have contributed to poorer outcomes in previous studies. In addition, the relatively higher incidence of bacteremia in previous studies may have led to the misclassification of more de novo cases as recurrences. Although in this study different types of antibiotics may have been used, it is perhaps more likely to be the longer antibiotic duration of treatment (6 wk), similar to that used in other biofilm infections such as endocarditis, which accounts for some of the improved outcome observed in this series. Various antibiotic durations were used in previous studies, with a median of approximately 3 wk but also including some cases that were treated for <2 wk.
We identified an important outcome difference between first and subsequent salvage attempts, indicating, perhaps not surprising, that salvage failure identifies a group with more extensive biofilm, which is not curable with antibiotics alone. The clinical implication is that salvage may be a reasonable initial strategy, but if recurrent bacteremia occurs, then the catheter should be replaced.
We found to our surprise that recurrence is often a late event, occurring up to 6 mo after the initial infection. Time to recurrence has not been assessed in previous studies, which all used a fixed follow-up period beyond which further events were deemed to be unrelated. These late recurrences are unlikely to be coincidental, because they occurred more frequently than could be explained by chance and can be seen to be the “tail” of an exponential distribution (Figure 2). Neither do they simply reflect a catheter with a greater chance of reinfection, because the risk for bacteremia with a different organism during follow-up was only slightly, not significantly, above baseline. This suggests, therefore, that recurrence rates may have been underestimated in previous studies, which typically followed patients for <3 mo. It is particularly important to recognize the potential for long latency if incident and recurrent events are to be managed differently. Any same-organism bacteremia that occurs within 6 mo should therefore be regarded as a genuine recurrence and treated accordingly.
Several studies have suggested that S. aureus infections may be harder to eradicate and more likely to cause complications (19,20). Our data supported this concept for the catheter replacement group but found little or no microbiology effect in those who were selected for salvage. This may reflect the gradually reducing incidence of this organism over time and documented shift toward other Gram-positive and Gram-negative infections (7,9) and suggests that initial management decisions can be made clinically, before the microbiological isolate is known.
This prospective cohort study comes from a single center and is limited by its observational nature. Direct comparison between catheter salvage and replacement would be biased by the clinical selection criteria; however, this design is well suited to the description of a predefined cohort treated in the same manner (i.e., the group whose presentation and favorable early response make them potential candidates for catheter salvage). Valid conclusions can therefore be drawn concerning the likely outcome when salvage is attempted in a clinically reasonable situation. A randomized study of catheter strategy would be superior but might suffer from bias as a result of nonparticipation by the large number of patients with strong treatment preferences.
The generous definition of catheter-associated bacteremia may have led to the inclusion of some bacteremias that arose from other sources, without an infected catheter, but this definition is appropriate because it accurately reflects clinical reality. Another potential weakness is that locking solutions, which have been found to improve outcomes in some previous studies (21–23), were not used for treatment in this study; treatment failures might therefore have been further reduced.
Conclusions
This study demonstrates that the strategy of catheter salvage in clinically reasonable cases is frequently successful, with catheter replacement being avoided in up to two thirds of cases and few complications. Clinical reasonableness may be defined by the absence of features of severe sepsis and an adequate clinical response to 48 h of antibiotic therapy. Recurrent bacteremia may occur up to 6 mo later, at which point catheter replacement seems a better strategy.
Disclosures
None.
Acknowledgments
D.R.A. is supported by a Translational Medicine Fellowship from the Hammersmith Hospitals Trustees Research Committee.
Part of this work was the subject of a poster presentation at the annual meeting of the American Society of Nephrology; Philadelphia, Pennsylvania; November 6 through 9, 2008.
We are grateful to Tara Watson, Claire Edwards, Kathleen Lynch, Kate Reed, Virginia Prout, Marion Garrett, Elizabeth Dalby, Maura Applebe, and Roopkishor Hurril for assistance. We are also grateful to Kathleen Bamford, Claire Thomas, and staff at the Department of Microbiology, Hammersmith Hospital.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.National Kidney Foundation: KDOQI Clinical practice guidelines for vascular access, 2000. Am J Kidney Dis 37[ Suppl 1]: S137– S181, 2001 [DOI] [PubMed] [Google Scholar]
- 2.Ethier J, Mendelssohn DC, Elder SJ, Hasegawa T, Akizawa T, Akiba T, Canaud BJ, Pisoni RL: Vascular access use and outcomes: An international perspective from the Dialysis Outcomes and Practice Patterns Study. Nephrol Dial Transplant 23: 3219– 3226, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moist LM, Trpeski L, Na Y, Lok CE: Increased hemodialysis catheter use in Canada and associated mortality risk: Data from the Canadian Organ Replacement Registry 2001–2004. Clin J Am Soc Nephrol 3: 1726– 1732, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee T, Barker J, Allon M: Tunneled catheters in hemodialysis patients: Reasons and subsequent outcomes. Am J Kidney Dis 46: 501– 508, 2005 [DOI] [PubMed] [Google Scholar]
- 5.Graham J, Hiremath S, Magner PO, Knoll GA, Burns KD: Factors influencing the prevalence of central venous catheter use in a Canadian haemodialysis centre. Nephrol Dial Transplant 23: 3585– 3591, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J: Type of vascular access and survival among incident hemodialysis patients: The Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 16: 1449– 1455, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Marr KA, Sexton DJ, Conlon PJ, Corey GR, Schwab SJ, Kirkland KB: Catheter-related bacteremia and outcome of attempted catheter salvage in patients undergoing hemodialysis. Ann Intern Med 127: 275– 280, 1997 [DOI] [PubMed] [Google Scholar]
- 8.Develter W, De Cubber A, Van Biesen W, Vanholder R, Lameire N: Survival and complications of indwelling venous catheters for permanent use in hemodialysis patients. Artif Organs 29: 399– 405, 2005 [DOI] [PubMed] [Google Scholar]
- 9.Araya CE, Fennell RS, Neiberger RE, Dharnidharka VR: Hemodialysis catheter-related bacteremia in children: Increasing antibiotic resistance and changing bacteriological profile. Am J Kidney Dis 50: 119– 123, 2007 [DOI] [PubMed] [Google Scholar]
- 10.Beathard GA, Urbanes A: Infection associated with tunneled hemodialysis catheters. Semin Dial 21: 528– 538, 2008 [DOI] [PubMed] [Google Scholar]
- 11.James MT, Conley J, Tonelli M, Manns BJ, MacRae J, Hemmelgarn BR: Meta-analysis: Antibiotics for prophylaxis against hemodialysis catheter-related infections. Ann Intern Med 148: 596– 605, 2008 [DOI] [PubMed] [Google Scholar]
- 12.Quarello F, Forneris G, Borca M, Pozzato M: Do central venous catheters have advantages over arteriovenous fistulas or grafts? J Nephrol 19: 265– 279, 2006 [PubMed] [Google Scholar]
- 13.Duncan ND, Singh S, Cairns TD, Clark M, El-Tayar A, Griffith M, Hakim N, Hamady M, McLean AG, Papalois V, Palmer A, Taube D: Tesio-Caths provide effective and safe long-term vascular access. Nephrol Dial Transplant 19: 2816– 2822, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Capdevila JA, Segarra A, Planes AM, Ramirez-Arellano M, Pahissa A, Piera L, Martinez-Vazquez JM: Successful treatment of haemodialysis catheter-related sepsis without catheter removal. Nephrol Dial Transplant 8: 231– 234, 1993 [PubMed] [Google Scholar]
- 15.MacRae JM, Ahmed A, Johnson N, Levin A, Kiaii M: Central vein stenosis: A common problem in patients on hemodialysis. ASAIO J 51: 77– 81, 2005 [DOI] [PubMed] [Google Scholar]
- 16.Mokrzycki MH, Zhang M, Cohen H, Golestaneh L, Laut JM, Rosenberg SO: Tunnelled haemodialysis catheter bacteraemia: Risk factors for bacteraemia recurrence, infectious complications and mortality. Nephrol Dial Transplant 21: 1024– 1031, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Saad TF: Bacteremia associated with tunneled, cuffed hemodialysis catheters. Am J Kidney Dis 34: 1114– 1124, 1999 [DOI] [PubMed] [Google Scholar]
- 18.Troidle L, Eisen T, Pacelli L, Finkelstein F: Complications associated with the development of bacteremia with Staphylococcus aureus. Hemodial Int 11: 72– 75, 2007 [DOI] [PubMed] [Google Scholar]
- 19.Poole CV, Carlton D, Bimbo L, Allon M: Treatment of catheter-related bacteraemia with an antibiotic lock protocol: Effect of bacterial pathogen. Nephrol Dial Transplant 19: 1237– 1244, 2004 [DOI] [PubMed] [Google Scholar]
- 20.Alexandraki I, Sullivan R, Zaiden R, Bailey C, McCarter Y, Khan A, Offutt JK, Bhatt UY, Plott D, Nahman NS, Jr: Blood culture isolates in hemodialysis vascular catheter-related bacteremia. Am J Med Sci 336: 297– 302, 2008 [DOI] [PubMed] [Google Scholar]
- 21.Onder AM, Chandar J, Simon N, Diaz R, Nwobi O, Abitbol CL, Zilleruelo G: Comparison of tissue plasminogen activator-antibiotic locks with heparin-antibiotic locks in children with catheter-related bacteraemia. Nephrol Dial Transplant 23: 2604– 2610, 2008 [DOI] [PubMed] [Google Scholar]
- 22.Krishnasami Z, Carlton D, Bimbo L, Taylor ME, Balkovetz DF, Barker J, Allon M: Management of hemodialysis catheter-related bacteremia with an adjunctive antibiotic lock solution. Kidney Int 61: 1136– 1142, 2002 [DOI] [PubMed] [Google Scholar]
- 23.Maya ID, Carlton D, Estrada E, Allon M: Treatment of dialysis catheter-related Staphylococcus aureus bacteremia with an antibiotic lock: A quality improvement report. Am J Kidney Dis 50: 289– 295, 2007 [DOI] [PubMed] [Google Scholar]