Abstract
Cardiopulmonary exercise testing (CPET) in paediatric cardiology differs in many aspects from the tests as performed in adult cardiology. Children's cardiovascular responses during exercise testing present different characteristics, particularly oxygen uptake, heart rate and blood pressure response, which are essential in interpreting haemodynamic data. Diseases that are associated with myocardial ischaemia are very rare in children. The main indications for CPET in children are evaluation of exercise capacity and the identification of exercise-induced arrhythmias. In this article we will review exercise equipment and test protocols for CPET in children with congenital heart disease. (Neth Heart J 2009;17:339-44.)
Keywords: exercise physiology, children, oxygen uptake, ergometry, exercise test
Children with congenital or acquired heart disease often have impairment of their functional capacity. This occurs in the preoperative, postoperative, as well as in the long-term setting and may be the result of the primary cardiac problem, treatment of that problem or hypoactivity leading to detraining.1,2 Lunt et al.3 found that adolescents with congenital heart disease (CHD) were less likely to reach minimum exercise requirements and perform vigorous exercises than were healthy adolescents.
Measurement of exercise capacity and other physiological responses provides objective information about the functional status of heart, lungs and peripheral muscle. This information can be of value in making clinical decisions resulting in a reduced use of hospital facilities, and improved functional capacity and quality of life.4
The aim of this article is to review the equipment, the main indications for CPET in children with congenital heart disease, the contraindications for exercise testing and the indications for terminating an exercise test. Moreover, we will address the interpretation of gas-exchange data from CPET in children with congenital heart disease.
Equipment for exercise testing
Laboratory and personnel
The exercise laboratory needs a special fitting. Exercise testing should be performed in a well-ventilated room with a temperature of ∽22±C and a relative humidity of ∽50%. Furthermore, it is recommended that the exercise lab is at least 23 m2 in size and when several ergometers, computers and other medical equipment are accommodated preferably 45 to 65 m2.5
Persons who are conducting the CPET (physicians, exercise physiologist or lab technicians) should have experience in paediatric exercise testing, especially in conducting CPET in children. When performing CPET, 50 supervised exercise tests and performing at least 25 tests per year are recommended to retain the skills of CPET.5
Although emergencies are rare in paediatric exercise testing, staff should be familiar with emergency manoeuvres and equipment should be available in case of exercise-induced problems. This equipment includes a cardiac defibrillator and a fully stocked crash cart. Furthermore, the lab should have medication readily available to treat exercise-induced asthma. A treatment table should be available for resuscitation or whenever the patient feels dizzy and needs to lie down following exercise. This table can also be used to record a standard supine ECG before CPET. In addition, having an emergency physician or paediatric cardiologist on site is recommended when performing a CPET in children with CHD.
Clinical laboratory testing
The basic premise for treadmill or cycle testing of young persons is not different from that for adults to assess symptoms, tolerance, and cardiopulmonary response to high-intensity exercise in a controlled setting. In general, satisfactory testing of children can be conducted equally well as in adults, even in subjects as young as four years. However, a number of particular features need to be appreciated when dealing with this age group.6 Most importantly, children are emotionally immature and need encouragement and positive support by an experienced testing staff to achieve an adequate exercise effort.
Ergometers
Both cycle and treadmill protocols have been used for exercise testing of children. However, the use of the treadmill is more appropriate when testing very young children, because this modality requires that the subject maintain the pace of the belt rather than provide the volitional effort to maintain a cycle cadence with increased workloads. Electronically braked cycle ergometers reduce the dependence on a specific cadence by allowing a range of cadence to achieve the same workload. However, appropriate small-sized ergometers are not available in most laboratories. To accommodate children, seat height, handlebar height and position, and pedal crank length may have to be modified for cycle ergometer testing. Most children who are ≥125 cm tall can be tested on a standard cycle ergometer. The greater potential for accidental falls on the treadmill requires greater attention by the testing staff. Regardless of the mode or protocol, children most be familiarised with all testing procedures to ensure the opportunity for a successful evaluation.
It is advised to use an ergometer to get objective and reproduceable information. In table 1 we summarise several considerations regarding when to choose the treadmill or the cycle ergometer.
Table 1 .
Matching the ergometer with the desired information.
| Condition or question | Preferred ergometer | Rationale |
|---|---|---|
| Aortic stenosis/insufficiency (unrepaired/repaired) | Cycle | Ischaemia detection on ECG easier because there is less motion artifact |
| Repaired transposition of great arteries | Cycle | Ischaemia detection on ECG easier |
| Repaired tetralogy of Fallot | Cycle | Arrhythmia assessment during exercise essential |
| Coronary artery anomaly, (repaired/unrepaired) | Cycle | Ischaemia detection on ECG easier |
| (Functional) single ventricle | Cycle/treadmill | Ischaemia and arrhythmia detection on ECG easier |
| Coarctation of the aorta (unrepaired/repaired) | Cycle | Blood pressure assessment more accurate |
| Exercise-induced asthma/bronchospasm/chest pain | Treadmill | Running more likely to induce symptoms than cycling |
| Aerobic capacity | Cycle/treadmill | Higher VO2max with treadmill than with cycle |
| Arrhythmia assessment/ Long QT syndrome | Cycle | Arrhythmia detection and measurement of QT interval on ECG easier because there is less motion artifact |
| Assessment of rate responsive pacemakers | Treadmill | Better activation of accelerometer-based sensors |
Modified from Stephens et al.7
Treadmill
The treadmill is useful for a wide range of patient sizes and ages. Treadmill exercise testing yields a 5 to 10% higher VO2peak than cycle ergometry due to recruitment of more muscle groups. The amount of work performed depends on body weight rather than machine set resistances. Fatigue of the leg muscles is less likely to be the cause of test termination than would be the case on a cycle ergometer. This increases the likelihood of the cardiorespiratory system being the limiting factor.1
Cycle ergometer
The patient must be tall enough to reach the pedals. The cycling motion might be difficult for young children to perform. Workload on a cycle ergometer is not dependent on patients' weight and can be used with a continuous ramp protocol allowing the workload to be precisely determined. The upper body is more stable on a cycle ergometer than on a treadmill, so ECG and blood pressure measurements are more reliable.1
Sometimes semi-recumbent ergometers are used in combination with echocardiographic measurements. However, one must take into account the different cardiopulmonary response to exercise compared with upright cycling exercise.
Other equipment
An electrocardiographic (ECG) monitoring system, blood pressure monitor, metabolic cart and a pulse oximeter are also needed for exercise testing. An exercise ECG monitoring system is necessary to monitor cardiac rhythm and rate. Moreover, it can be used to detect cardiac ischaemia during the exercise test, although this is observed far less in paediatric patients than in adult populations. In addition, an exercise ECG system is valuable for detecting prolongation of the QT interval during exercise, as seen in patients with long-QT syndrome.
To minimise artifacts on the ECG, the recording system should have a muscle artifact filter system. It is also imperative to pay meticulous attention to the electrode placement. The skin should be prepared by cleaning with alcohol followed by scrubbing with an abrasive paper. We use disposable adhesive electrodes made from a breathable material to minimise skin transpiration. The connecting cables should be fixed to the skin with tape. The cable connector should hang above or behind the patient. This can be achieved by using a rack.
A metabolic cart is used to determine peak oxygen uptake (VO2peak), carbon dioxide production and ventilatory threshold. There is a variety of commercially available metabolic carts, which can be used for measuring ventilatory gas exchange.8 Moreover, several portable metabolic carts are available to measure VO2 during activities in the field.8
A pulse oximeter provides information about arterial oxygen saturation at rest and during exercise. It is important to consider that oximeters may have difficulty tracking the signal at peak exercise because they are motion-sensitive.1
Although blood pressure is sometimes difficult to measure reliably during exercise,9 especially during treadmill running, its measurement is important in children with aortic coarctation, aortic stenosis, cardiomyopathy and syncope, for instance. The laboratory should always have a variety of blood pressure cuffs available of appropriate sizes for the entire range of patients tested.
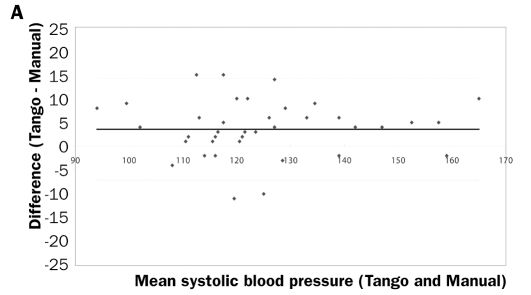
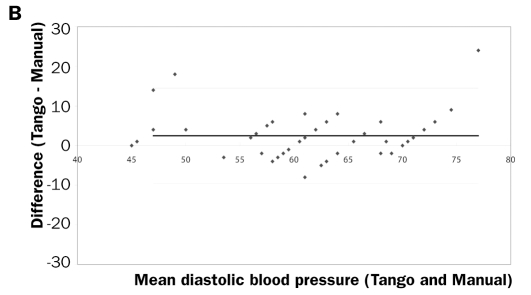
There are only a few automatic systems that can measure blood pressure during exercise. It is our experience that the Suntech Tango® system (SunTech Medical Instruments, Morrisville, North Carolina, USA) is a valid and reliable system to measure blood pressure during cycling exercise in children (figure 1).10
Figure 1 .
Bland-Altman plot of systolic(left) and diastolic (right) blood pressure (in mmHg) during exercise as measured with the Suntech Tango® system compared with auscultatory blood pressure measurement. (Takken et al., unpublished observations).
All equipment should, of course, be calibrated before use following the specifications of the manufacturer.
Testing protocols
Because of the wide ranges of ages and testing indications, there is no single standard testing protocol for children. There are a number of established treadmill exercise testing protocols, of which the Bruce protocol is the most commonly used.11 This protocol is appropriate for most young, physically active patients; however, the incremental increases in workloads may be too great for others. Treadmill testing protocols that may be more appropriate for less-fit patients include Cornell, McNaughton, and Balke,12,13 which have a slower increase in workload.
When a cycle ergometer is available, the most commonly used protocols are McMaster protocol,14 James protocol,15 Godfrey protocol,16 and recently a continuous ramp protocol.17 Increments in workload can be increased by 5, 10, 15 or 20 Watt per unit of time depending on height, weight or body surface area.1,16 The aim is to reach a maximum of 6 to 10 minutes of exercise for young children18 and 8 to 12 minutes for adolescents.19
In the early days of exercise physiology, it was quite common to use a discontinuous protocol.20,21 In such protocols, exercise stages were performed on consecutive days until a subject reached his VO2 plateau. These protocols were very impractical in clinical and occupational settings because of the time constraints of both the subject and the lab personnel. Therefore, exercise protocols were designed with a much shorter time between exercise stages (several minutes). The intervals between the exercise stages allowed physiologists to perform several measurements such as blood sampling, and other invasive measurements such as muscle biopsies. Currently, most laboratories use continuous exercise protocols while many different exercise protocols are available. Exercise stages vary from a couple of seconds in the so-called ramp protocols to three to five minutes if a steady state for most physiological functions (heart rate and oxygen uptake) is required. The use of computerised treadmills allows smaller work increments at a higher frequency. These ramp protocols provide better haemodynamic and gas exchange responses during exercise than the protocols with longer exercise stages (i.e. three to five minutes).22,23 Determination of the ventilatory threshold, for instance, is easier in protocols with a shorter stage duration.23,24 Since Nobel laureate A.V. Hill described the concept of VO2max in 1924,25 many different test protocols have been designed for testing or predicting VO2max. In the following section we will describe several exercise testing protocols including maximal and submaximal exercise tests.
Maximal exercise tests
Treadmill tests
A large number of treadmill protocols have been developed for measuring VO2max, of which the Bruce and the Balke protocol are the most popular ones.
The Bruce protocol is the most widely used treadmill protocol in clinical exercise testing.11,26,27 This test was originally developed for cardiac patients by Robert A. Bruce in the 1960s.28 The test involves a change of speed and elevation every three minutes, so that the incremental increases for each stage are relatively large (2–3 METS). Oxygen uptake values expressed in METS were derived from tests of normal subjects and were established for each minute of testing for the Bruce treadmill protocol.29 In the modified version of the Bruce treadmill protocol, the speed stays constant for the first three stages, starting at 2.7 km/h at 0% incline. After the third stage, both the speed and grade increase every three minutes. McInnis et al. compared the modified Bruce and the Bruce protocol in patients with documented coronary artery disease and found that the physiological responses at matched submaximal rates were similar.30
Disadvantages of the Bruce test are: (1) largeinterstage increments in work that can make estimation of VO2max less accurate and (2) a fourth stage that can be either run or walked, resulting in different oxygen costs.31
The Bruce protocol can be performed by small children whose legs may be too short to reach the pedals of a cycle ergometer. Treadmill protocols are useful in the evaluation of motion-sensitive, rate-responsive pacemakers because the upper torso is in constant motion.32
In the 1950s, Bruno Balke described a treadmill protocol which he used in exercise tests on Air Force personnel. In this protocol the workload is increased by increasing the angle of the treadmill while the walking speed remains unchanged during the test. Originally Balke used a speed of 5.3 km/h and a horizontal angle of the treadmill, with a 1± increase in angle of every minute.33,34 Based on the endurance time or the final angle of the treadmill an estimation of the VO2max could be made using the following formula:34
VO2max=walking speed (metres/min) × body mass (kg) × (0.73 × angle/100) × 1.8
In this formula, the given fraction of the angle in degrees is needed, and 1.8 is the factor of the oxygen uptake for generating 1 m/kg of work. Since Balke's original study, many modifications have been made.35 These modifications were made to limit the exercise time during the treadmill test. The optimal time for an aerobic capacity test is between 8 to 12 minutes on average.36 In table 2, modifications of the Balke protocol are provided.
Table 2 .
Modified Balke protocol.
| Patient | Speed (km/h) | Angle % (start) | Angle % (increase/min) |
|---|---|---|---|
| Original | 5.3 | 0 | 1 |
| Poor condition | 4.8 | 6 | 2 |
| Inactive | 5.2 | 6 | 2 |
| Active | 8 | 0 | 2.5 |
| Athlete | 8.5 | 0 | 2.5 |
From Rowland.35
Bicycle ergometry testing
Cycle ergometry is one of the oldest methods to measure the exercise capacity of a subject. The first cycle ergometer was developed in 1896 by the French medical student Elisée Bouny. Later, several other mechanical braked and electromagnetically braked cycle ergometers were developed in both the United States37 and Europe.38
Maximal cycle ergometer protocols
In Europe most maximal exercise tests are performed on the cycle ergometer, while in North America the treadmill is more commonly used. This probably reflects the use of the bicycle as a mode of transportation in daily life in Europe. Cycle ergometry has some advantages over treadmill exercise testing. The advantage of bicycle testing is that it is portable and less expensive than treadmill testing. Because the body is more stable during cycling and the bicycle is less noisy, blood pressure can be determined more easily and fewer motion artifacts are observed in electrocardiograms during exercise. Moreover, during cycle ergometry the workload and work efficiency can be precisely determined, while in treadmill exercise only an estimate can be made. In addition, the VO2max can be easily predicted from the peak workload (Wpeak). As a rule of the thumb, every Watt costs about 10.3 ml O2/min. Wpeak can be computed as follows when a non-ramped protocol has been used:39
Wpeak=POf + (t/T × D)
where POf is the power output (W) of the last completed workload, t is the time (in s) the last uncompleted workload was maintained, T is the duration (in s) of each completed workload, and D is the power-output difference (Watt) between consecutive workloads.
The disadvantage of bicycle protocols is that many (North American) subjects may not be accustomed to cycling and muscular fatigue may occur prematurely, preventing subjects from reaching their maximal capacity. VO2max is 10 to 15% lower in cycle versus treadmilltesting in those not accustomed to cycling.40
With computerised ergometers it is possible to bypass the conventional protocols in which the workload is increased every one to five minutes. Using this ramp approach, there is a smaller increase in workload per time unit, providing a more linear increase of workload, which facilitates the determination of the ventilatory threshold.41 Usually, the ventilatory threshold occurs at an exercise intensity between 40 to 60% of VO2max. As mentioned previously, the best quality and quantity of data during clinical exercise tests are collected when the exercise time is between eight to 12 minutes in adults and adolescents and six to ten minutes in children.18,19 This implies that a ramp protocol should be individualised, based on the subject's fitness status. For children the following method is used.17 First, an estimation of basal VO2 is made using the formula:
Basal VO2 (ml/min)=height (in cm) × 2 −100.
The increase in workload per minute (RAMP) is calculated as follows:
(VO2peak predicted − VO2basal)/82.5.
This will lead to exhaustion in approximately 8 minutes.
Another approach has been proposed by Tanner et al. They standardised the ramp protocol using a constant load in children of 0.25 W/kg/min.42 In healthy children they found no difference in VO2peak between the ramp protocol and a conventional James protocol. In children with exercise intolerance, the ramp protocol was preferable.43
Test termination
During a CPET, a patient can develop several exerciseinduced physiological signs or complaints that warrant a termination of the test. Criteria for terminating a CPET are listed in table 3.
Table 3 .
Criteria for terminating a CPET in children.
| 1 Clinical |
|
| 2 ECG |
|
| 3 Blood pressure |
|
| 4 Progressive fall in oxygen saturation to <90% or a 10-point drop from resting saturation in a symptomatic patient. |
Modified from Paridon et al. and Bar-Or.27,44
Conclusion
Cardiopulmonary exercise testing in children with congenital heart disease differs in many ways from adult cardiological exercise testing.
In this article we have reviewed exercise equipment and protocols, the main indications for cardiopulmonary exercise testing in children with congenital heart disease, the contraindications for exercise testing and the indications for terminating an exercise test. Moreover, we have addressed the interpretation of gas exchange data from cardiopulmonary exercise testing in children with congenital heart disease.
Acknowledgement
We would like to thank Professor Emeritus David A. de Wolf for his valuable comments on our manuscript.
References
- 1.Connuck DM. The role of exercise stress testing in pediatric patients with heart disease. Prog Pediatr Cardiol 2005;20:45–52. [Google Scholar]
- 2.Bar-Or O. Pathophysiological factors which limit the exercise capacity of the sick child. Med Sci Sports Exerc 1986;18:276–82. [DOI] [PubMed] [Google Scholar]
- 3.Lunt D, Briffa T, Briffa NK, Ramsay J. Physical activity levels of adolescents with congenital heart disease. Aust J Physiother 2003; 49:43–50. [DOI] [PubMed] [Google Scholar]
- 4.Rich MW. Heart failure disease management: a critical review. J Card Fail. 1999;5:64–75. [DOI] [PubMed] [Google Scholar]
- 5.James FW, Blomqvist CG, Freed MD, Miller WW, Moller JH, Nugent EW, et al. Standards for exercise testing in the pediatric age group. American Heart Association Council on Cardiovascular Disease in the Young. Ad hoc committee on exercise testing. Circulation 1982;66:1377A–97A. [PubMed] [Google Scholar]
- 6.Rowland TW. Aerobic exercise testing protocols. In: Rowland TW, editor. Pediatric Laboratory Exercise Testing: Clinical Guidelines. Champaign, Ill: Human Kinetics; 1993. p. 19–41. [Google Scholar]
- 7.Stephens P Jr, Paridon SM. Exercise testing in Pediatrics Pediatr Clin North Am. 2004;51:1569–87, viii. [DOI] [PubMed] [Google Scholar]
- 8.Macfarlane DJ. Automated metabolic gas analysis systems: a review. Sports Med. 2001;31:841–61. [DOI] [PubMed] [Google Scholar]
- 9.Lightfoot JT. Can blood pressure be measured during exercise? A review. Sports Med. 1991;12:290–301. [DOI] [PubMed] [Google Scholar]
- 10.Cameron JD, Stevenson I, Reed E, McGrath BP, Dart AM, Kingwell BA. Accuracy of automated auscultatory blood pressure measurement during supine exercise and treadmill stress electrocardiogram-testing. Blood Press Monit. 2004;9:269–75. [DOI] [PubMed] [Google Scholar]
- 11.Chang RK, Gurvitz M, Rodriguez S, Hong E, Klitzner TS. Current practice of exercise stress testing among pediatric cardiology and pulmonology centers in the United States. Pediatr Cardiol. 2006;27:110–6. [DOI] [PubMed] [Google Scholar]
- 12.Balke B, Ware RW. An experimental study of “physical fitness” of air force personnel. U S Armed Forces Med J 1959;10:675–88. [PubMed] [Google Scholar]
- 13.Ellestad M. Stress Testing. Oxford: Oxford University Press; 2003. [Google Scholar]
- 14.Bar-Or O, Rowland TW. Pediatric Exercise Medicine. From Physiologic principles to healthcare Application. Champaign, IL: Human Kinetics; 2004. [Google Scholar]
- 15.James FW, Kaplan S, Glueck CJ, Tsay JY, Knight MJ, Sarwar CJ. Responses of normal children and young adults to controlled bicycle exercise. Circulation 1980;61:902–12. [DOI] [PubMed] [Google Scholar]
- 16.Godfrey S. Exercise testing in children. London: W.B. Saunders Company Ltd; 1974. [Google Scholar]
- 17.Karila C, de Blic J, Waernessyckle S, Benoist MR, Scheinmann P. Cardiopulmonary exercise testing in children: an individualized protocol for workload increase. Chest. 2001;120:81–7. [DOI] [PubMed] [Google Scholar]
- 18.Hebestreit H. Exercise testing in children - What works, what doesn't, and where to go to? Paediatr Respir Rev. 2004;5:S11–S4. [DOI] [PubMed] [Google Scholar]
- 19.Buchfuhrer MJ, Hansen JE, Robinson TE, Sue DY, Wasserman K, Whipp BJ. Optimizing the exercise protocol for cardiopulmonary assessment. J Appl Physiol. 1983;55:1558–64. [DOI] [PubMed] [Google Scholar]
- 20.Taylor HL, Buskirk E, Henschel A. Maximal oxygen intake as an objective measure of cardiorespiratory performance. J Appl Physiol. 1955;8:73–80. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell JH, Blomqvist G. Maximal oxygen uptake. N Engl J Med. 1971;284:1018–22. [DOI] [PubMed] [Google Scholar]
- 22.Will PM, Walter JD. Exercise testing: improving performance with a ramped Bruce protocol. Am Heart J. 1999;138:1033–7. [DOI] [PubMed] [Google Scholar]
- 23.Myers J, Buchanan N, Walsh D, Kraemer M, McAuley P, Hamilton-Wessler M, et al. Comparison of the ramp versus standard exercise protocols. J Am Coll Cardiol. 1991;17:1334–42. [DOI] [PubMed] [Google Scholar]
- 24.Whipp BJ, Davis JA, Torres F, Wasserman K. A test to determine parameters of aerobic function during exercise. J Appl Physiol. 1981;50:217–21. [DOI] [PubMed] [Google Scholar]
- 25.Hill AV, Long CNH, Lupton H. Muscular exercise, lactic acid and the supply and use of oxygen. Parts I-III. Proc R Soc Biol. 1924;96:438–75. [Google Scholar]
- 26.Bruce RA. Exercise testing for evaluation of ventricular function. New Engl J Med. 1977;296:671–5. [DOI] [PubMed] [Google Scholar]
- 27.Paridon SM, Alpert BS, Boas SR, Cabrera ME, Caldarera LL, Daniels SR, et al. Clinical stress testing in the pediatric age group: a statement from the American Heart Association Council on Cardiovascular Disease in the Young, Committee on Atherosclerosis, Hypertension, and Obesity in Youth. Circulation 2006; 113:1905–20. [DOI] [PubMed] [Google Scholar]
- 28.Bruce RA, Blackmon JR, Jones JW, Strait G. Exercise testing in adult normal subjects and cardiac patients. Pediatrics 1963;32: Suppl-56 [PubMed] [Google Scholar]
- 29.American College of Sports M. Guidelines for exercise testing and prescription. Philadelphia: Lea and Febiger;. 1991. [Google Scholar]
- 30.McInnis K, Balady G, Weiner D, Ryan T. Comparison of ischaemic and physiologic responses during exercise tests in men using the standard and modified Bruce protocols. Am J Cardiol.. 1992;69: 84–9. [DOI] [PubMed] [Google Scholar]
- 31.Fletcher GF, Balady GJ, Amsterdam EA, Chaitman B, Eckel R, Fleg J, et al. Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation 2001;104:1694–740. [DOI] [PubMed] [Google Scholar]
- 32.Barber G. Pediatric exercise testing: methodology, equipment and normal values. Prog Pediatr Cardiol 1993;2:4–10. [Google Scholar]
- 33.Balke B. [Optimum physical working capacity, its measurement and change as a result of the working fatigue]. Arbeitsphysiologie. 1954;15:311–23. [DOI] [PubMed] [Google Scholar]
- 34.Balke B, Ware RW. An experimental study of physical fitness of Air Force personnel. U S Armed Forces Med J 1959;10:675–88. [PubMed] [Google Scholar]
- 35.Rowland TW. Crusading for the Balke protocol. Pediatr Exer Sci. 1999;11:189–92. [Google Scholar]
- 36.Buchfuhrer M, Hansen J, Robinson T, Sue D, Wasserman K, Whipp B. Optimizing the exercise protocol for cardiopulmonary assessment. J Appl Physiol. 1983;55:1558–64. [DOI] [PubMed] [Google Scholar]
- 37.Benedict FG, Cady WG. A bicycle ergometer with an electric brake. Washington DC: Carnegie Institute of Washington; 1912. Report No: Publication no. 167. [Google Scholar]
- 38.Krogh A. A bicycle ergometer and respiration apparatus for the experimental study of muscular work. Scand Arch Physiol 1913;33:375–80. [Google Scholar]
- 39.Kuipers H, Verstappen FT, Keizer HA, Geurten P, van Kranenburg G. Variability of aerobic performance in the laboratory and its physiologic correlates. Int J Sports Med. 1985;6:197–201. [DOI] [PubMed] [Google Scholar]
- 40.Astrand P, Rodahl K. Textbook of work physiology, physiological bases of exercise. New York: McGraw-Hill Book Company; 1986. [Google Scholar]
- 41.Wasserman K, Hansen JE, Sue DY, Casaburi R, Whipp BJ. Principles of Exercise Testing and Interpretation. Baltimore, MD: Lippincott, Williams and Wilkins; 1999. [Google Scholar]
- 42.Tanner CS, Heise CT, Barber G. Correlation of the physiologic parameters of a continuous ramp versus an incremental James exercise protocol in normal children. Am J Cardiol.. 1991;67: 309–12. [DOI] [PubMed] [Google Scholar]
- 43.Barber G. Pediatric exercise testing: methodology, equipment and normal values. Progr Pediatr Cardiol. 1993;2:4–10. [Google Scholar]
- 44.Bar-Or O. Pediatric sports medicine for the practitioner. New York: Springer-Verlag; 1983. [Google Scholar]