Abstract
Down syndrome is the most common chromosomal abnormality. A simultaneous occurrence with Marfan syndrome is extremely rare. We present a case of a 28-year-old female with Down syndrome and a mutation in the fibrillin-1 gene. The patient showed strikingly few manifestations of Marfan syndrome. Although variable expression is known to be present in Marfan syndrome, phenotypic expression of Marfan syndrome in our patient might be masked by the co-occurrence of Down syndrome. (Neth Heart J 2009;17:345-8.)
Keywords: Marfan syndrome, Down syndrome, trisomy 21, coexistence, FBN1
Down syndrome (DS) is the most common chromosomal abnormality among live-born infants and the most frequent form of intellectual disability, with a prevalence of 1 to 2 per 1000 live births.1
DS is characterised by various congenital malformations, characteristic dysmorphic features and other health-related problems. Marfan syndrome (MFS) is an autosomal dominantly inherited connective tissue disorder, with an estimated prevalence of 1 to 2 per 10,000. It affects various organs, in particular the skeleton, the heart and the eyes, with variable phenotypic expression.2 Diagnosis of MFS is made according to the Ghent nosology.3 This requires ‘major’ criteria in at least two systems and the involvement of a third system with ‘minor’ criteria. The condition is caused by mutations in the fibrillin-1 (FBN1) gene, located on chromosome 15.4 Mutations in this gene have also been reported in Marfan-related diseases such as ectopia lentis syndrome and familial ascending aortic aneurysms.5 In 10% of the cases that fulfil the criteria of MFS, no mutation in the FBN1 gene is identified. Mutations in the transforming growth factor-beta receptor 2 (TGFBR2) on chromosome 3 and TGFBR1 on chromosome 9 have been linked to the Marfan phenotype in some of these patients.6 Here, we present a patient with DS and a mutation in the FBN1 gene. To the authors' knowledge, this is the first reported case described in the English literature. Both DS and MFS are associated with specific phenotypic characteristics. Therefore, the phenotypic appearance in our patient is clinically intriguing.
Case report
A 28-year-old woman was born with extreme hypotonia and typical dysmorphic features of DS. DS was diagnosed three days after birth by karyotyping (karyotype 47, XX, +21). Throughout childhood, major health care problems were progressive weight gain and multiple orthopaedic surgical interventions because of luxation of the patella. A congenital heart defect was absent.
The patient's paternal grandfather and uncle had both died of aortic dissection at the age of 47 years. Her father was suspected of having MFS when he was 39 years of age, because of the presence of an increased arm span-to-height ratio of 1.08, thoracolumbar scoliosis, arachnodactyly with positive wrist sign, striae atrophicae on the shoulder and surgery for a hernia in the past. Ocular signs were a flat cornea and slight myopia, but cardiovascular symptoms were absent. At that time, our patient was 8 years old. Physical examination of our patient revealed clinical manifestation of DS, including short stature (height was 123 cm (P75 for DS)), mild upslanting palpebral fissures, flat nose, epicanthic folds and intellectual disability. Except for a highly arched palate, joint hypermobility (Beighton score 5/9) and flat feet, no other physical manifestations of MFS were present. Echocardiography revealed no abnormalities. Ophthalmologic examination showed cataract and strabismus associated with DS, but no major signs of MFS. Therefore suspicion of MFS was low. Characteristic signs and symptoms of MFS and DS and patient characteristics are shown in table 1.
Table 1 .
Syndrome and patient characteristics.
| Down syndrome | Marfan syndrome | Presented case | |
|---|---|---|---|
| Characteristic phenotypic features | |||
| Dysmorphic features | |||
| Small brachiocephalic head | + | − | + |
| Epicanthic folds | + | − | + |
| Flat nasal bridge | + | − | + |
| Up-slanting palpebral fissures | + | − | + |
| Small ears | + | − | + |
| Excessive skin at the nape of the neck | + | − | + |
| Single transverse palmar crease | + | − | − |
| Wide space between first and second toes | + | − | − |
| Highly arched palate | − | + | + |
| Dolichochephaly | − | + | − |
| Malar hypoplasia | − | + | − |
| Retrognathia | − | + | − |
| Enophthalmus | − | + | − |
| Down-slanting palpebral fissures | − | + | − |
| Cardiovascular signs | |||
| Congenital heart defect | + | − | − |
| Dilatation or dissection ascending aorta | − | + | − |
| Dilatation or dissection descending aorta <50 years | − | + | − |
| Mitral valve prolapse | − | + | − |
| Dilatation main pulmonary artery | − | + | − |
| Calcification mitral valve annulus <40 years | − | + | − |
| Ophthalmologic signs | |||
| Brushfield spots | + | − | − |
| Strabismus | + | − | − |
| Cataract | + | − | + |
| Nystagmus | + | − | − |
| Myopia | + | + | + |
| Lens dislocation | − | + | − |
| Flat cornea | − | + | − |
| Hypoplastic iris | − | + | − |
| Orthopaedic signs | |||
| Atlantoaxial instability | + | − | − |
| Joint hypermobility | + | + | + |
| Pes planus | + | + | + |
| Scoliosis | + | + | − |
| Pectus carinatum/ excavatum | − | + | − |
| Dolichostenomelia | − | + | − |
| Arachnodactyly | − | + | − |
| Reduced extension of elbows (<170º) | − | + | − |
| Protrusio acetabulae | − | + | − |
| Dermatological signs | |||
| Folliculitis | + | − | + |
| Dry skin | + | − | + |
| Alopecia areata | + | − | − |
| Fissured tongue | + | − | − |
| Palmoplantar hyperkeratosis | + | − | − |
| Striae atrophiae | − | + | + † |
| (Recurrent) herniae | − | + | + † |
| Pulmonary signs | |||
| Obstructive sleep apnoea | + | − | − |
| Spontaneous pneumothorax | − | + | − |
| Apical blebs | − | + | − |
| Other signs | |||
| Mental impairment | + | − | + |
| Hypothyroidism | + | − | + |
| Hypotonia | + | − | + |
| Obesity | + | − | + |
| Dural ectasia | − | + | ? |
| Genetic defect | |||
| Trisomy chromosome 21 | + | − | + |
| Pathogenic mutation: FBN1 or TGFBR1 or TGFBR2 gene | − | + | +* |
+ syndromal sign present, − syndromal sign absent, ? unknown presence of sign,* major criterion, † minor criterion. FBN1=fibrillin 1, TGFBR=transforming growth factor beta receptor. According to the Ghent nosology our patient has one major and one minor criterion of Marfan syndrome.
When our patient was 25 years old, DNA analysis was performed in her father and a mutation in the FBN1 gene (IVS 11+5G>A) was found. The mutation was also present in our patient. Physical examination as well as echocardiography did not reveal any additional manifestations of MFS as seen at the age of 8 years. Pictures of her face (figure 1) and hands (figure 2) are shown. Her final height was 155 cm (P50 for DS). Neither our patient nor her father could be diagnosed with MFS according to the Ghent nosology.3 However, a magnetic resonance imaging (MRI) to evaluate dural sac ratio was not performed. The father has skeletal and ocular manifestations and two other relatives died of aortic dissection, which suggests the FBN1 mutation to be present in these relatives. Our patient, however, showed strikingly few signs of MFS.
Figure 1 .
Picture of patient's face: front and side. Note facial features of Down syndrome, e.g. upslanting palpebral fissures, epicanthal folds and small ear. (Published with permission from the patient and her family).
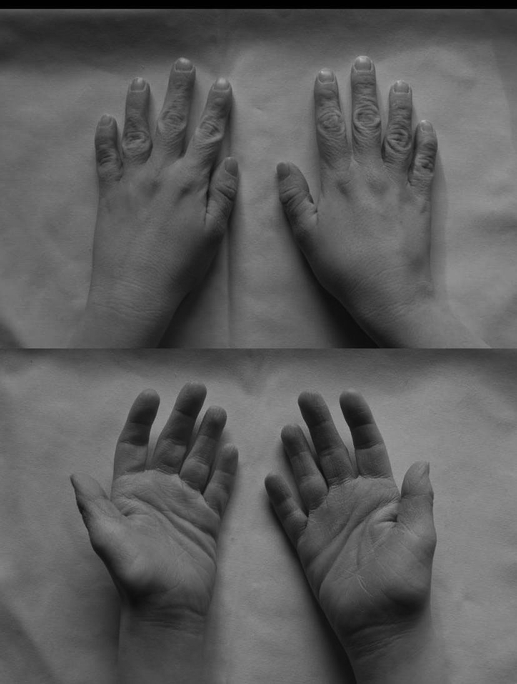
Figure 2 .
Picture of patient's hands. Note that there are no signs of arachnodactyly. A single transverse palmar crease is absent.
Discussion
We present a case of a 28-year-old female with DS and a mutation in the FBN1 gene. Because of a relatively high prevalence of DS, simultaneous occurrence with other syndromes and diseases is quite possible. Dupre et al. reported an unusual case in which an eruption of syringomas, DS, MFS and Ehlers-Danlos syndrome were associated.7 MFS and DS were both evident, but some specific anomalies were missed because of interaction between the two syndromes. A cooccurrence of DS and Ehlers-Danlos syndrome has been reported in the past by Meyer et al.,8 Schachter9 and Korting.10 Recently Pasmatzi et al. put forward the possibility of a link between DS and Ehlers-Danlos syndrome that is currently unknown.11
Features of MFS were not obvious in our patient. Phenotypic expression with respect to presence and severity of symptoms of MFS is known to be variable, even within families. The mutation (IVS 11+5G>A) has been described before in other studies.5,12 In at least one case, the mutation caused an incomplete MFS.12 This is consistent with the incomplete MFS in the patient and her father.
In addition, the relatively young age of our patient may partly account for the lack of symptoms of MFS. However, in our patient, phenotypic features of MFS might possibly be camouflaged by a co-existence with DS. For example, DS is associated with typical facial features, short stature, small hands and short fingers that could diminish the manifestations of MFS.
On the other hand, symptoms of DS overlap with MFS. For example, acquired hip dislocation occurs in 6% of DS patients13 and 2% of MFS patients have a dysplasia of the hip.14 Flat feet occur in 60% of patients with DS15 and in 25% of MFS patients.14 In the case presented here, joint hypermobility and flat feet may be associated with both syndromes. Cardiovascular manifestations are common in both syndromes. It is remarkable that our patient showed no signs of cardiovascular disease.
People with DS show physical changes related to ageing about 20 to 30 years ahead of people of the same age in the general population (decreased skin tone, early greying or loss of hair, cataract, hearing loss, Alzheimer disease). Therefore DS may hypothetically influence progression of MFS by acceleration of aortic dilatation. However, this could not (yet) be observed in our patient. Nevertheless, she is at risk for cardiovascular complications associated with this syndrome. Therefore regular cardiac ultrasound examination is performed.
Since the care of patients with DS has improved in recent decades with improved survival, increased practitioner awareness of unusual features in DS may facilitate earlier diagnosis of a second syndrome. Possible harmful consequences may be prevented and will optimise care in DS patients.
Acknowledgements
We wish to thank the patient and her family for their kind cooperation.
References
- 1.Frid C, Drott P, Lundell B, Rasmussen F, Anneren G. Mortality in Down's syndrome in relation to congenital malformations. J Intellect Disabil Res. 1999;43(Pt 3):234–41. [DOI] [PubMed] [Google Scholar]
- 2.Judge DP, Dietz HC. Marfan's syndrome. Lancet 2005;366: 1965–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Paepe A, Devereux RB, Dietz HC, Hennekam RC, Pyeritz RE. Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet. 1996;62:417–26. [DOI] [PubMed] [Google Scholar]
- 4.Ho NC, Tran JR, Bektas A. Marfan's syndrome. Lancet 2005;366: 1978–81. [DOI] [PubMed] [Google Scholar]
- 5.Comeglio P, Johnson P, Arno G, Brice G, Evans A, Ragon-Martin J, et al. The importance of mutation detection in Marfan syndrome and Marfan-related disorders: report of 193 FBN1 mutations. Hum Mutat. 2007;28:928. [DOI] [PubMed] [Google Scholar]
- 6.Mizuguchi T, Collod-Beroud G, Akiyama T, Abifadel M, Harada N, Morisaki T, et al. Heterozygous TGFBR2 mutations in Marfan syndrome. Nat Genet 2004;36:855–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dupre A , Bonafe JL. Syringomas mongolism, Marfan's disease and Ehlers-Danlos' disease. Ann Dermatol Venereol. 1997;104:224–30. [PubMed] [Google Scholar]
- 8.Meyer J, Weill J, Guilaine J. Syndrome d' Ehlers-Danlos. EMC Pediatrie. 1956;10:12 [Google Scholar]
- 9.Schachter MA. Arrieration Mongolienne et syndrome d' Ehlers-Danlos: a propos d'une observation. Rome: Ediz Medica SpA; 1956. [Google Scholar]
- 10.Korting GW. Atlas de dermatologie pediatrique. Paris: Masson; 1969, p. 98. [Google Scholar]
- 11.Pasmatzi E, Vlastos D, Monastirli A, Stephanou G, Georgious S, Sakkis T, et al. Ehlers-Danlos type IV syndrome in a patient with Down syndrome: simple co-occurrence or true association? Am J Med Sci. 2006;331:48–50. [DOI] [PubMed] [Google Scholar]
- 12.Liu WO, Oefner PJ, Qian C, Odom RS, Francke U. Denaturing HPLC-identified novel FBN1 mutations, polymorphisms, and sequence variants in Marfan syndrome and related connective tissue disorders. Genet Test. 1997;1:237–42. [DOI] [PubMed] [Google Scholar]
- 13.American Academy of Pediatrics: Health supervision for children with Down syndrome. Pediatrics 2001;107:442–9. [DOI] [PubMed] [Google Scholar]
- 14.Giampietro PF, Raggio C, Davis JG. Marfan syndrome: orthopedic and genetic review. Curr Opin Pediatr 2002;14:35–41. [DOI] [PubMed] [Google Scholar]
- 15.Concolino D, Pasquzzi A, Capalbo G, Sinopoli S, Strisciuglio P. Early detection of podiatric anomalies in children with Down syndrome. Acta Paediatr 2006; 95:17–20. [DOI] [PubMed] [Google Scholar]