Abstract
Objective
To examine the relationship between public health system network density and organizational centrality in public health systems and public health governance, community size, and health status in three public health domains.
Data Sources/Study Setting
During the fall and the winter of 2007–2008, primary data were collected on the organization and composition of eight rural public health systems.
Study Design
Multivariate analysis and network graphical tools are used in a case comparative design to examine public health system network density and organizational centrality in the domains of adolescent health, senior health, and preparedness. Differences associated with public health governance (centralized, decentralized), urbanization (micropolitan, noncore), health status, public health domain, and collaboration area are described.
Data Collection/Extraction Methods
Site visit interviews with key informants from local organizations and a web-based survey administered to local stakeholders.
Principal Findings
Governance, urbanization, public health domain, and health status are associated with public health system network structures. The centrality of local health departments (LHDs) varies across public health domains and urbanization. Collaboration is greater in assessment, assurance, and advocacy than in seeking funding.
Conclusions
If public health system organization is causally related to improved health status, studying individual system components such as LHDs will prove insufficient for studying the impact of public health systems.
Keywords: Public health systems, public health governance, rural, social networks
In its report “The Future of Public Health” the Institute of Medicine (IOM) argued for an expanded role of governmental public health agencies and the increased involvement of community organizations to address the public health needs of Americans. In a later report, the IOM embraced the public health system vision of public health agencies as a consensus builder and the convener of organizational partnerships spanning public, private, and voluntary sectors of the community (Committee on Assuring the Health of the Public in the 21st Century 2002). A key benefit of this systems approach is greater opportunity for identifying, leveraging, and concentrating resources.
Researchers define public health systems as community-based organizational networks that include “the full complement of public and private organizations that contribute to the delivery of public health services for a given population, including governmental public health agencies as well as private and voluntary entities” (Mays, Halverson, and Scutchfield 2003, p. 180). Public health systems researchers consider local health departments (LHDs) a nerve center of public health systems, facilitating “the actions of others in accomplishing systemwide goals” (Halverson 2002).
This paper extends the research on public health systems using a case comparative design to examine public health systems in eight rural communities. The research objectives are to (a) describe public health systems social network structural features of density and organizational centrality by health domain (adolescent health, senior health, and preparedness); and (b) examine the relationship between social network structure and state public health governance, community size, health domain, and health status. Density and organizational centrality are two key features of social networks (Sandström and Carlsson 2008). Density measures the amount of interconnectedness between the organizations in a network. Interconnectedness is important because it facilitates implementation through organizations working together. Organizational centrality is important for coordinating and focusing network actions.
BACKGROUND
Public health systems research has taken two broad forms, evaluation of efforts to build public health systems and survey/archival-based research on the role and function of public health system organizations. While each type of research has provided valuable information, the focus of the former on project-specific areas and of the latter on LHDs does not address public health systems as interorganizational networks.
Evaluations of the Turning Point Project (Berkowitz and Ray 2003; Padgett, Bekemeier, and Berkowitz 2004, 2005; Kassler and Goldsberry 2005; Nicola 2005), the Community Care Network Demonstration (Alexander et al. 2003; Calhoun 2006;), and the work of others (Roussos and Fawcett 2000; Easterling 2003; Campbell and Conway 2005;) demonstrate the important role of these collaborative interorganizational relationships in the function and performance of public health systems and their influence over population health.
One limitation of archival/survey-based studies of public health systems, though, is an implicit focus on LHDs even though the public health system includes all “partners providing public health services in a jurisdiction” (Scutchfield et al. 2004). For example, data on LHD and community characteristics are integrated to predict health status and public health performance (Mays et al. 2006; Mays 2007;). While some researchers have employed instruments that rely solely on LHD respondents to assess public health system performance (Driscoll et al. 2006), the recommended practice in the National Public Health Performance Standards Program is to include “a group that is broadly representative of these public health system partners in the assessment process” (Center for Disease Control and Prevention 2008; also see Mays et al. 2004; Scutchfield et al. 2004;). The reasons for representative involvement are to improve measurement reliability and to increase community engagement in the public health system. Zahner has provided valuable contributions in measuring public health systems by examining collaboration of LHDs with a variety of organizations (Zahner and Corrado 2004; Zahner 2005; Zahner, Kaiser, and Kapelke-Dale 2005;).
While this research is valuable, the reliance on LHDs as key informants may overlook collaborations that can maximize the potential for organizing limited resources to meet critical public health needs. For example, the efforts of local schools to promote asthma or substance abuse programs for youth could go unnoticed because data collection focused only on LHD funding or activities. The reliance on representative involvement for measurement may result in group processes biasing measurement or measurement being biased because the most active in a public health system are most likely to participate in the measurement process. Finally these approaches do not allow the assessment of public health systems as social networks.
Applying a social network perspective to public health systems research in a fashion similar to the approach used by Merrill and her colleagues (Merrill 2007; Merrill et al. 2008;) offers a promising approach for capturing the interorganizational relations that form public health systems. Building on the work of Varda et al. (2008), this paper extends the research of Merrill and her colleagues beyond LHD intraorganizational networks by focusing on the interorganizational networks that form the public health system.
This paper examines public health systems within the domains of adolescent health, senior health, and preparedness. These domains were selected because of their focus on distinct aspects of population health needs and the likelihood that contextual differences would significantly influence the nature and membership of organizational collaborations. Addressing adolescent health, such as risky youth behavior, involves schools, LHDs, family planning, and faith-based community partners among others. Significant ideological differences that exist among the partnering organizations can be important contextual factors for successful organizational collaborations (e.g., a harm reduction approach versus an abstinence approach). While senior health, such as caring for the elderly and frail, is less likely to be affected by ideological differences, it is challenging because of balancing the different economic and mission-focused interests of public and private sector service delivery organizations. Preparedness requires the organization and coordination of a highly focused set of providers (e.g., first responders such as fire, police, emergency medical services, the emergency rooms of local hospitals) as well as other organizations that are responsible for client safety in emergencies (e.g., nursing homes). In addition to the potential for status and role-related conflicts, the availability of federal funding to establish a preparedness infrastructure may contribute to confrontations over the allocation and control of the funding.
This paper also examines the relationship between public health systems governance, community size, and health status and public health system network density and organizational centrality. Density is the number of connections between organizations in a network divided by network size. Holding network size constant, density is measured as the number of connections between organizations in a network. Organizational centrality is the number of connections that a particular organization has with other organizations in the network. Density measures the degree of interconnectedness, which is important for working together for implementation and organizational centrality measures coordinative capacity in a network. Implementation is strongest when density in a health domain is high and is guided by a central set of organizations (Sandström and Carlsson 2008).
Public health governance is usually categorized into three broad groups: centralized (“LHDs are units of the state health agency”), decentralized (“LHDs are units of local government”), and mixed (Leep 2006). Because funding and control come from the state, centralized governance may result in a more bureaucratic approach with less need or opportunity to interact with local county officials to obtain funding. In contrast, a decentralized governance structure requires LHDs to work with county officials for funding. This may create greater opportunities or a greater need for LHDs to seek collaborative arrangements to support funding. This suggests that decentralized governance will be associated with denser public health systems than in centralized governance.
Community size is another important contextual dimension. This paper focuses on rural communities for two reasons. First, the general scarcity of financial and human resources in rural communities places a greater burden on the capacity of public health systems to address and manage population health needs. Compared with urban settings, rural public health systems contend with greater health care workforce shortages, lower levels of insurance coverage, smaller scale economies, weaker technical and transportation infrastructure, and greater issues of geographic and social isolation. Second, because the impact of scale increases at decreasing rate, scale effects are most likely to be observed in differences between very small communities and large rural communities. In order to capture these important differences, communities are categorized by micropolitan and noncore location using the Urban Influence Code (UIC) categories developed by the U.S. Department of Agriculture. Micropolitan and noncore categories represent the two main subdivisions for rural communities. Micropolitan counties account for approximately 60 percent of the nation's rural population and are centered on a core city or town of between 10,000 and 50,000 persons while noncore counties represent the remaining areas with populations under 10,000 persons (Economic Research Service 2003). The greater scarcity of resources in small (noncore) communities is assumed to be associated with greater public health system density and LHD centrality. In slightly larger (micropolitan) communities, public health systems will have lower density because of a greater number of organizations participating in the system and LHD centrality may be lower because of the availability of a greater number of organizations with the human resources and professional expertise to lead addressing public health issues.
The last contextual difference is health status. Within the tracer condition of risky youth behavior, for example, high levels of sexually transmitted diseases (STDs) may be associated with collaboration. However, the effect is difficult to predict. It may be that high levels of STDs, for example, cause intense collaboration to develop educational interventions, community clinics, and other programs to reduce the high STD rates. If these interventions are successful, it is likely they can be replaced with more standardized programs. Then, the intense problem-solving collaboration can be replaced with a less intensive collaboration focusing more on program maintenance and surveillance activities. Alternatively, it may be the case that ongoing intense collaboration is necessary to continue addressing the STD rates.
Public health systems networks are studied using collaborative relationships for the three core public health system functions of assurance, assessment, and advocacy (Corso et al. 2000) and efforts to obtain the resources support local efforts (cofunding). Graphical and multivariate analyses are used to examine the relationship between social network structure and governance, community size, health domain, and health status.
DATA AND METHODS
Eight rural communities were sampled to contrast (a) centralized/decentralized governance, (b) small (noncore) and large (micropolitan) rural communities, and (c) low and high community health status. Four communities were sampled from a centralized state and four from a decentralized state. The two states had similar levels of public health funding and were in a similar geographic and economic region. Within each state, two noncore and two micropolitan communities were sampled so that comparison communities within a category were similar in terms of demographics and LHD capacity and were dissimilar on adolescent and senior health outcomes (Appendix SA2 describes the sampling methodology in detail and Appendix SA3 describes the characteristics of the sampled communities).
Noncore and micropolitan communities were first grouped into sets of communities with similar demographic characteristics, health department capacity, health care supplier capacity (Center for the Evaluative Clinical Sciences at Dartmouth 2002; Health Resources and Services Administration 2006;), and crime rates using cluster analysis. Communities within a cluster that differed in risk-adjusted health status were sampled. Risk-adjusted health status was measured by regressing health outcomes related to adolescent health (percent prenatal first trimester visits, percent teen births, gonorrhea rate, and Chlamydia rate) and senior health (congestive heart disease and cancer death rate) on community demographics and health organizational capacity. The regression residuals were combined using factor analysis to obtain a single measure of adolescent health status and senior health status. This measure was multiplied by −1 so that lower measures represented worse health (higher STD rates or mortality than expected) and higher measures represented better health (lower STD rates or mortality than expected).
The sample consisted of demographically similar communities that differed in health status. State experts reviewed the selections for appropriateness. There were minor adjustments to assure contrast counties came from similar regions within the state. One county was replaced because an originally sampled county declined to participate in the study.
Measuring Relationships among Organizations in the Public Health System
Community data were collected by site visit interviews and a web-based survey. Key organizational informants for the site visit interviews were identified by the LHD administrator and through community websites. The interviews focused on organizational activities in each domain, background information on the community, and the identity of other community leaders engaged in one or more of the study domains of interest. Candidates for the site visit interviews were contacted to obtain their consent and to arrange an interview time. On average, 12–14 persons were interviewed in each community, including representatives from LHDs, emergency management and preparedness, fire departments, law enforcement, hospitals, senior services, schools, and local health collaboratives.
The data for the network analyses were collected using a web-based survey instrument administered to the site visit participants and other community representatives identified during the interviews. Of the 225 individuals interviewed or identified during the site visits or from community health-oriented meeting rosters, 142 completed a survey (63 percent). Follow-up calls were made by the research staff and by the LHD administrators to encourage participation and to locate individuals whose survey e-mail invitations could not be delivered (e.g., unknown host, undeliverable, etc.). Excluding the bounced e-mails from individuals who were unable to be reached resulted in a cooperation rate of 70 percent. There were no systematic differences existing across communities in types of organizations represented by the respondents.
Within each community, 12 networks were measured, four in each of the three study domains. Each respondent indicated which of 18 types of organizations they or their organization worked with in four collaboration areas in each domain.1 For adolescent health and senior health, the areas were assessment, assurance, advocacy, and cofunding. Assurance, assessment, and advocacy were included because they are core public health functions under which essential services are grouped (Corso et al. 2000), were easily grasped by the site visit participants, and because asking about the 10 essential public health services (Handler, Issel, and Turnock 2001) would have added to respondent burden and lowered the survey response rate. Cofunding was defined as working with another organization to obtain local, regional, state, or national funding to support efforts in the tracer condition. Slightly different areas of collaboration were used for preparedness to better reflect the activities identified during the site visits and included assessment or planning activities, equipment purchases, training/simulations, and emergency response.
Although financial collaboration, cofunding, and equipment purchases are not identified as essential public health services, they were included in the study because of the dependence of LHDs on multiple and diverse funding sources (e.g., ongoing grant writing and funds solicitation efforts). Collaboration in cofunding activities such as supporting the establishment of a community center for youth and senior programs target public health objectives and are viewed positively by state and county governments as mechanism for leveraging limited governmental funds. But competing for limited resources can make collaboration difficult (Leviss 2008; Orton, Menkens, and Santos 2009;). Collecting information about cofunding networks allows measurement of these competing pressures.
Methodology
For the multivariate analysis, the dependent variable was the number of times each organization was mentioned as a collaborator in each of the 96 networks (eight communities each having four networks in each of the three domains). Network density effects were measured using collaboration area, health status, and governance × community size × domain. Organizational centrality effects were measured using community size × domain × organization. The interactions allow effects to vary across contexts. A second regression estimated differences in health status effects differ across contexts (this could not be done in the initial regression because of perfect collinearity). The density and centrality effects are presented using least-squares means with 95 percent confidence intervals. This allows effect magnitudes to be compared. The health status effects are reported using standard regression estimates.
The final models were selected using a stepwise approach. Initially a model with only linear effects for governance, community size, domain, collaboration area, and health status was estimated. Then models with interaction effects were nested within the linear model. Those models that significantly improved the fit, as measured by χ2-tests, were selected.
SAS 's Proc GLIMMIX was used to estimate the models. Because the dependent variable was a count measure and because the count was likely to be overly dispersed (the variance exceeds the mean), a negative binomial model was used (Gardner, Mulvey, and Shaw 1995). A random effect at the community level was used because there are multiple observations within each community violating the assumption of independent errors (Greene 1993).
Social network graphical techniques were also used for analysis and are presented where appropriate. Two-mode social networks graphs were used for graphical analysis. Two-mode networks display organizational participation by activity (Borgatti and Everett 1997; Hanneman and Riddle 2005;).2 A two-mode network was used because it provides an integrated view of participation by activity. UCINET VI 's tool Visualize/Netdraw was used for graphing (Analytic Technologies Inc. 2008).3
RESULTS
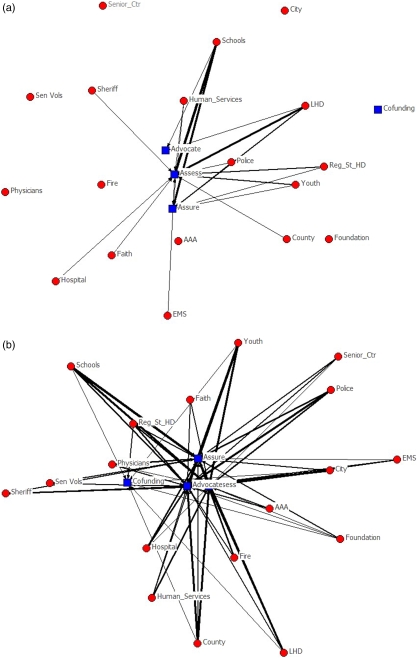
Table 1 shows the effects of governance, community size, domain, and health status on public health system network density. The presented estimates are the predicted density and its 95 percent confidence interval associated with a specific governance, community size, and public health domain. Within the centralized state, public health systems in micropolitan communities are less dense than public health systems in noncore communities in the areas of senior health and preparedness (the confidence intervals do not overlap). Within the decentralized state, public health systems in micropolitan communities are denser than public health systems in noncore communities. These differences are striking, as shown by Figure 1's depiction of network organization for adolescent health by community size. Across states, the decentralized noncore communities have less dense public health systems than the public health systems in the centralized state and the public health systems in decentralized micropolitan communities are denser than public health systems in the centralized state. These effects suggest two observations. First, it may be that greater funding for noncore communities in centralized than in decentralized states is associated with greater public health system density in noncore communities. Second, the entrepreneurial nature of decentralization combined with the scale of micropolitan communities may be associated with greater public health system density in decentralized micropolitan communities.
Table 1.
Effect of Governance, Community Size, Collaboration Area, and Health Status on Predicted Degree Centrality (95% CI)
| Governance | Community Size | Domain | |
|---|---|---|---|
| Centralized | Noncore | Adolescent health | 1.36 (1.18, 1.57) |
| Senior health | 1.55 (1.35, 1.77) | ||
| Preparedness | 1.89 (1.67, 2.16) | ||
| Micropolitan | Adolescent health | 1.25 (1.08, 1.44) | |
| Senior health | 0.72 (0.59, 0.87) | ||
| Preparedness | 1.44 (1.25, 1.65) | ||
| Decentralized | Noncore | Adolescent health | 0.74 (0.61, 0.88) |
| Senior health | 1.14 (0.99, 1.33) | ||
| Preparedness | 1.44 (1.25, 1.66) | ||
| Micropolitan | Adolescent health | 2.63 (2.36, 2.92) | |
| Senior health | 2.47 (2.21, 2.75) | ||
| Preparedness | 2.59 (2.31, 2.89) | ||
| F for governance × size × domain 74.87 (p<.001) | |||
| Collaboration area | |||
| Assess | 2.75 (2.61, 2.91) | ||
| Assure | 2.25 (2.08, 2.44) | ||
| Advocacy | 2.18 (2.01, 2.37) | ||
| Training | 1.63 (1.44, 1.84) | ||
| Responded | 1.46 (1.29, 1.66) | ||
| Equipment | 0.71 (0.61, 0.84) | ||
| Cofunding | 0.65 (0.57, 0.75) | ||
| F for collaboration area 117.26 (p<.001) | |||
| Governance | Community Size | Domain | Estimate (T-Statistic) |
| Health status | |||
| Centralized | Noncore | Adolescent health | −0.21 (−5.86)* |
| Senior health | 0.71 (6.16)* | ||
| Micropolitan | Adolescent health | −0.06 (−2.01)* | |
| Senior health | 0.47 (3.28)* | ||
| Decentralized | Noncore | Adolescent health | 3.16 (5.06)* |
| Senior health | −0.02 (−0.29) | ||
| Micropolitan | Adolescent health | −0.11 (−1.65) | |
| Senior health | −5.37 (−2.64)* | ||
| F for governance × size × domain × health status 15.30 (p<.001) | |||
p<.05.
Figure 1.
Organizational Participation in Risky Youth Behavior Areas: (a) Noncore; (b) Micropolitan
Across collaboration areas, assessment networks are denser than assurance and advocacy networks. The next densest networks are preparedness training and response. The least dense collaboration area networks are equipment purchase and cofunding. The latter is consistent with the argument that cofunding is a more difficult relationship to develop.
Although six of the eight health status effects are significant, the effects are mixed. In the centralized state, greater public health system density is associated with worse adolescent health and better senior health. In the decentralized state, greater public health system density is associated with worse senior health in micropolitan communities and greater public health system density is associated with better adolescent health in noncore communities.
Table 2 presents the analysis of organizational centrality. The estimates show that organizational centrality varies by problem domain. In adolescent health, the players are schools, youth organizations, and local and regional health departments. In senior health, the players are the Area Agency on Aging, the hospital, senior centers, the LHD, and human services. For the preparedness domain, the players are fire departments, the LHD, the city and county officials, emergency medical services, and the sheriff.
Table 2.
Predicted Organizational Centrality (95% CI) by Domain × Community Size
| Adolescent Health |
Senior Health |
Preparedness |
||||
|---|---|---|---|---|---|---|
| Organization | Centrality | Rank | Centrality | Rank | Centrality | Rank |
| Noncore | ||||||
| Area Agency on Aging | 0.40 (0.22, 0.74) | 17 | 2.51 (1.95, 3.23) | 1 | 1.17 (0.78, 1.73) | 11 |
| City | 0.89 (0.59, 1.34) | 10 | 1.40 (1.00, 1.95) | 9 | 3.22 (2.53, 4.10) | 2 |
| County | 1.25 (0.89, 1.77) | 8 | 1.35 (0.96, 1.89) | 10 | 3.17 (2.48, 4.04) | 4 |
| EMS | 0.89 (0.59, 1.34) | 11 | 1.12 (0.77, 1.62) | 12 | 3.17 (2.48, 4.04) | 5 |
| Faith | 0.76 (0.49, 1.18) | 14 | 1.81 (1.35, 2.43) | 6 | 0.83 (0.52, 1.33) | 15 |
| Fire | 0.72 (0.45, 1.13) | 15 | 0.65 (0.40, 1.06) | 17 | 3.22 (2.53, 4.10) | 3 |
| Foundation | 0.80 (0.52, 1.24) | 13 | 0.56 (0.33, 0.94) | 18 | 0.44 (0.23, 0.84) | 18 |
| Hospital | 1.12 (0.77, 1.61) | 9 | 2.19 (1.67, 2.86) | 3 | 2.83 (2.19, 3.66) | 7 |
| Human services | 1.43 (1.03, 1.98) | 6 | 2.00 (1.51, 2.65) | 4 | 1.17 (0.78, 1.73) | 12 |
| LHD | 2.19 (1.68, 2.85) | 2 | 2.00 (1.51, 2.65) | 5 | 3.50 (2.78, 4.41) | 1 |
| Physicians | 0.89 (0.59, 1.34) | 12 | 1.30 (0.92, 1.84) | 11 | 1.17 (0.78, 1.73) | 13 |
| Police | 1.47 (1.07, 2.03) | 5 | 1.12 (0.77, 1.62) | 13 | 2.44 (1.85, 3.22) | 8 |
| Regional and state HD | 1.52 (1.11, 2.08) | 4 | 1.49 (1.08, 2.06) | 8 | 1.72 (1.24, 2.39) | 10 |
| Schools | 2.55 (1.99, 3.26) | 1 | 0.98 (0.66, 1.45) | 14 | 1.83 (1.33, 2.52) | 9 |
| Senior volunteers | 0.54 (0.32, 0.91) | 16 | 1.72 (1.27, 2.33) | 7 | 1.06 (0.70, 1.60) | 14 |
| Senior center | 0.27 (0.13, 0.56) | 18 | 2.47 (1.91, 3.18) | 2 | 0.78 (0.48, 1.26) | 16 |
| Sheriff | 1.30 (0.92, 1.82) | 7 | 0.84 (0.55, 1.29) | 15 | 3.05 (2.38, 3.91) | 6 |
| Youth organizations | 1.70 (1.26, 2.29) | 3 | 0.74 (0.47, 1.17) | 16 | 0.72 (0.44, 1.19) | 17 |
| Micropolitan | ||||||
| Area Agency on Aging | 1.12 (0.78, 1.60) | 17 | 2.05 (1.58, 2.66) | 1 | 1.40 (0.98, 2.00) | 11 |
| City | 2.06 (1.58, 2.70) | 7 | 1.38 (1.01, 1.89) | 8 | 3.22 (2.54, 4.09) | 7 |
| County | 2.45 (1.92, 3.14) | 3 | 1.54 (1.14, 2.07) | 4 | 3.28 (2.59, 4.15) | 6 |
| EMS | 1.46 (1.07, 2.00) | 12 | 1.06 (0.75, 1.52) | 16 | 3.55 (2.83, 4.45) | 3 |
| Faith | 1.33 (0.96, 1.85) | 16 | 0.99 (0.68, 1.43) | 17 | 0.86 (0.55, 1.35) | 17 |
| Fire | 1.72 (1.29, 2.30) | 11 | 1.14 (0.81, 1.61) | 15 | 3.97 (3.21, 4.93) | 1 |
| Foundation | 1.42 (1.03, 1.95) | 15 | 1.30 (0.94, 1.80) | 11 | 0.81 (0.50, 1.29) | 18 |
| Hospital | 1.76 (1.32, 2.35) | 10 | 1.62 (1.21, 2.16) | 3 | 2.85 (2.21, 3.66) | 8 |
| Human services | 1.85 (1.40, 2.45) | 9 | 1.42 (1.04, 1.94) | 7 | 1.13 (0.76, 1.68) | 13 |
| LHD | 2.37 (1.84, 3.04) | 5 | 1.66 (1.24, 2.21) | 2 | 3.38 (2.68, 4.27) | 5 |
| Physicians | 1.46 (1.07, 2.00) | 13 | 1.22 (0.88, 1.71) | 12 | 1.34 (0.93, 1.93) | 12 |
| Police | 2.19 (1.69, 2.84) | 6 | 1.22 (0.88, 1.71) | 13 | 3.87 (3.11, 4.81) | 2 |
| Regional and state HD | 2.41 (1.88, 3.09) | 4 | 1.18 (0.84, 1.66) | 14 | 2.79 (2.17, 3.60) | 9 |
| Schools | 2.92 (2.33, 3.67) | 2 | 1.46 (1.07, 1.98) | 5 | 1.72 (1.24, 2.37) | 10 |
| Senior volunteers | 1.46 (1.07, 2.00) | 14 | 1.46 (1.07, 1.98) | 6 | 0.97 (0.63, 1.48) | 15 |
| Senior center | 1.12 (0.78, 1.60) | 18 | 1.38 (1.01, 1.89) | 9 | 0.97 (0.63, 1.48) | 16 |
| Sheriff | 1.89 (1.43, 2.50) | 8 | 0.91 (0.62, 1.33) | 18 | 3.44 (2.73, 4.33) | 4 |
| Youth organizations | 3.01 (2.41, 3.76) | 1 | 1.38 (1.01, 1.89) | 10 | 1.07 (0.72, 1.61) | 14 |
Note. F for size × domain × organization 7.15 (p<.001).
Bold indicates the top-ranked organizational type within health domain within community size.
HD, health department; LHD, local health department.
While LHDs are significant participants in all networks, their centrality appears to vary by community size. In noncore communities, the LHD is ranked second, fifth, and first most central in adolescent health, elderly health, and preparedness. In micropolitan communities, the LHD is ranked fifth, second, and fifth.
DISCUSSION
The results support the argument that LHDs are relatively central. However, they are not usually the most central organization. The differences between noncore and micropolitan communities in organizational centrality hint that community size may influence the role of LHDs. Smaller communities, due to their limited workforce capacity and economic base, tend to have fewer organizations available to address local health needs and may be more reliant on their LHD to take on that role. In larger communities, public health systems may fragment into specialized collaborations, such as a network organization (Powell 1990) for children's insurance and health. Perhaps as community size increases, LHDs may not have as central a role in public health systems.
The results suggest that context influences the development of public health systems. Public health system density was highest in decentralized micropolitan communities and lowest in the decentralized noncore communities. Perhaps the former is due to LHDs in decentralized micropolitan communities having a large enough operational scale, enough autonomy, and pressures to be entrepreneurial. Both LHDs in the decentralized micropolitan communities had their own budgets, grant writing infrastructure, as well as control over their hiring and internal procedures. If it is the case that a bureaucratic environment in the centralized state reduces public health entrepreneurial activities, it may be useful for centralized states to encourage more entrepreneurial activity by delegating more responsibility, autonomy, and decision authority to LHDs while holding them accountable for achieving public health goals.
A strength of the centralized state appears to be the provision of stable funding for noncore LHDs. In the decentralized state, site visits suggested that funding in noncore community activities was problematic. Providing state core funding for LHDs in noncore communities in decentralized states may result in significant public health dividends by underwriting a capacity for pursuing more entrepreneurial-based public health activities.
While health status had a significant effect, its effect was mixed. Some of the differences may be due to contextual differences between health domains, community size, and governance. It also may be that there are two causal paths. It may be that poor health outcomes are associated with the formation of dense networks to address the problem. Once the problem is addressed and routine procedures are put in place, the level of collaboration decreases. This results in an inverse relationship between network density and health status. Or it may be that strong ongoing collaborations in public health systems are necessary to obtain in better health outcomes. This results in a positive relationship between network density and health status. Overall, the results suggest that while health status is related to network structure, the nature of the relationship is complicated by contextual factors and causal processes. Significantly more research at the level of a public health system for a health domain in communities will be necessary to understand the effects.
The results for organizational centrality also suggest that there may be significant opportunities for tapping as yet unused resources by reaching out to engage additional community groups. Faith-based organizations and senior volunteers are excellent examples of these untapped resources. Site visit interviews uncovered numerous examples of local stakeholders taking on added responsibilities independent of LHD efforts (e.g., the role of the faith-based community in answering the need for lodging and food by refugees of Katrina and other local natural disasters). Other examples included faith community organized youth teams to build ramps for individuals with disabilities and supporting education and testing services to reduce the rate of STDs. Interestingly, the survey data did not show their strong involvement in public health systems. This may be due to these activities being organized by the faith-based community independently of the public health system.
Even though the pursuit of external funding can be a major source of support for health department activities, our findings revealed a significant lack of collaboration in cofunding activities. The cofunding collaboration that was observed tended to revolve around programs such as emergency preparedness where project goals and objectives were prescribed by the funding agency rather than proposed by the participating organizations in response to a broad project agenda. The success of federal and state programs in encouraging collaboration around preparedness may provide a model for encouraging collaboration around funding in other domains, such as adolescent or senior health.
A barrier to cofunding identified in the site interviews was the lack of skilled grant writers and grant managers. While the micropolitan communities had the scale economies to support individuals with these skills, noncore rural communities often did not. In the decentralized state, regional collaborations between noncore and micropolitan counties proved effective (e.g., with the micropolitan counties providing the specialized grant-related skills). However, even in cases of fundraising success, some communities had difficulty implementing their funded projects because of a lack of trained personnel. For example, one community found funding to support a program to provide discounted pharmaceuticals for the elderly but had difficulty keeping the program going because it was difficult to fill even the part-time position required to implement the program. The biggest difficulty filling the position was that the LHD could not take the risk of hiring someone because of the uncertainty of the funding. Luckily, the local hospital was able to make the financial commitment to cover insufficient funds if the program did not work as expected. Interestingly, it was not the money that was needed—it was the carrying of risk if the program did not work as expected.
State public health policy could provide solutions to these cofunding barriers. The example of micropolitan counties providing infrastructure and expertise for grant writing and management could be duplicated in a centralized state through its regional public health offices or micropolitan health departments. Building public health systems at a local level becomes more likely if a state specifies community responsibilities and holds them accountable for taking the lead in those local efforts. While state and regional health departments can provide invaluable support, state and regional health departments leading and organizing activities such as assessments can be counter-productive if it reduces the engagement at the community level. The state and regional support has to be focused carefully so that it does not become a substitute for community involvement.
Study findings have implications for research, such as measuring the impact of LHDs on health status. Using adolescent health as an example, one might be interested in the impact of LHD funding on STDs and teen pregnancies as health status. If county funding for schools, public safety, and public health is positively correlated, then omitting the funding levels of the other key players in the domain could seriously bias regression results and overstate the effect of local health funding. As Handler, Issel, and Turnock (2001) point out, “the structural capacity of the public health system is the cumulative resources and relationships necessary to carry out the important processes of public health.” Obtaining unbiased estimates of the effect of public health spending requires measuring the cumulative resources.
The results also suggest that public health system research should take public health domain into account. In the area of adolescent health, a school district may be resistant to health education campaigns focusing on sexuality because of parental attitudes. This can drive a wedge between local and regional health department actions related to sexual practices and youth education rendering even the most appropriate LHD efforts ineffective. Information provided at the site visits and findings about the across domain differences in organizational centrality are consistent with this argument. For adolescent health, activities such as health education and community centers are organized around involving youth. For senior health, activities are organized around service delivery, such as meals on wheels, senior centers, and elder-focused health care services. For preparedness, activities are organized around federal and state funding that mandate organizational interaction and involvement. Given the variability in the relationship between public health system characteristics and health status within the public health domains included in this study, public health system development and improvement will be difficult without the guidance of domain-specific research. Theoretical models of how organizational participation in domains affects population health are needed to further advance the field of public health systems research.
This study has two key limitations affecting the interpretation of its findings. First, the generalizability of our findings is limited because of the small number of communities included in the study. The importance of conducting an intense examination of each community coupled with limited funding and time for conducting the study precluded the inclusion of additional communities. Extending the research by examining a greater number of communities would allow more precise testing of the relation between health system organization and health status.
The second limitation is related to the way in which the site visits were conducted. LHD administrators assisted in the planning and implementation of the site visits, endorsed the e-mail requests for participation in the web-based survey, and helped follow up contacts to encourage completion of the surveys. The intensity of their involvement may have resulted in an increase in the measured centrality for the LHD. The research team attempted to reduce the risk of this bias by collecting names of potential survey respondents from public listings (e.g., attendance rosters from community meetings on public health issues and staff listings available from the websites of local organizations), including a survey item asking about collaboration with other organizations, and identifying potential participants from community and organizational websites.
In conclusion, the results are very consistent with the view that a public health system “includes the full complement of public and private organizations that contribute to the delivery of public health services for a given population, including governmental public health agencies as well as private and voluntary entities” (Mays et al. 2003, p. 180). Further, the analysis shows that the organization of the public health system varies by the type of public health domain being addressed. If public health system organization is causally related to improved health status, studying individual components such as LHDs will prove insufficient for the effective study of public health systems.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was funded through the Robert Wood Johnson Foundation's Changes in Health Care Financing and Organization (HCFO) Initiative. We thank the local health directors and members of the eight rural communities we studied for their time and willingness to help us learn about public health systems in rural communities.
Disclosures: None.
Disclaimers: None.
NOTES
The organizations listed on the survey in each domain were as follows: Area Agency on Aging, City Government (Mayor, City Counsel, public works), community-based organizations focusing on youth, community-based organizations such as Retired & Senior Volunteers, County Government (Commissioner, Board of Health), Emergency Medical Services, Fire Department, Hospital, Local Health Department, Local Foundation, Ministerial Alliance, Physician Practice/Clinic, Police Department, Regional or State Health Department, Schools (K through 12, alternative), Senior Center, Sheriff's Department, Social, Human, or Rehabilitative Services.
For those interested in using UCINET VI to examine social networks, the Hanneman and Riddle online text is an excellent resource.
The Layout/Graph-Theoretic layout/Spring embedding tool was used so that organizations with similar relationships to other organizations are close to each other. Organizations mentioned only two or more times are shown to reduce the noise. Heavier lines represent being mentioned more times.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Measuring Residual Health Status.
Appendix SA3: Characteristics of Sampled Communities.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Alexander JA, Bazzoli GJ, Contrad DA, Hasnain-Wynia R, Shortell SM, Sofaer S. Public–Private Partnerships to Improve Health Care: Balancing Short Term Successes with Long Term Plans. Chicago: Health Research and Educational Trust; 2003. [Google Scholar]
- Analytic Technologies Inc. UCINET VI (Release 6.198) Lexington, KY: Analytic Technologies Inc; 2008. [Google Scholar]
- Berkowitz BN, Ray M. Public Health Infrastructure System Change: Outcomes from the Turning Point Initiative. Journal of Public Health Management and Practice. 2003;9(3):224–7. doi: 10.1097/00124784-200305000-00007. [DOI] [PubMed] [Google Scholar]
- Borgatti SP, Everett MG. Network Analysis of 2-Mode Data. Social Networks. 1997;19(3):243–69. [Google Scholar]
- Calhoun M. “Evaluation Finds Local Community Care Networks Do Not Reduce Costs, Show Some Improvement in Health Status” [accessed on July 25, 2006]. Available at http://www.rwjf.org/reports/grr/029519.htm.
- Campbell P, Conway A. Developing a Local Public Health Infrastructure: The Maine Turning Point Experience. Journal of Public Health Management and Practice. 2005;11(2):158–64. doi: 10.1097/00124784-200503000-00009. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. National Public Health Standards Performance Program Local Public Health System Performance Assessment Instrument, Version 2.0. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- Center for the Evaluative Clinical Sciences at Dartmouth. “The Primary Care Service Area Project” [accessed on August 23, 2002]. Available at http://www.dartmouth.edu/~cecs/pcsa/pcsa.html.
- Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public's Health in the 21st Century. Washington, DC: The National Academies Press; 2002. [Google Scholar]
- Corso LC, Wiesner PJ, Halverson PK, Brown CK. Using the Essential Services as a Foundation for Performance Measurement and Assessment of Local Public Health Systems. Journal of Public Health Management and Practice. 2000;6(5):1–18. doi: 10.1097/00124784-200006050-00003. [DOI] [PubMed] [Google Scholar]
- Driscoll D, Rojas Smith L, Sotnikov S, Gadsden Knowles K, Perry NB, Lenaway DD, Halverson PK. An Instrument for Assessing Public Health System Performance: Validity in Rural Settings. Journal of Rural Health. 2006;22(3):254–9. doi: 10.1111/j.1748-0361.2006.00041.x. [DOI] [PubMed] [Google Scholar]
- Easterling D. What Have We Learned about Community Partnerships? Medical Care Research and Review. 2003;60(4, Suppl):161S–6S. doi: 10.1177/1077558703260221. [DOI] [PubMed] [Google Scholar]
- Economic Research Service. Measuring Rurality: Urban Influence Codes. Washington, DC: U.S. Department of Agriculture; 2003. [Google Scholar]
- Gardner W, Mulvey E, Shaw E. Regression Analyses of Counts and Rates: Poisson, Overdispersed Poisson, and Negative Binomial Models. Psychological Bulletin. 1995;118(3):392–404. doi: 10.1037/0033-2909.118.3.392. [DOI] [PubMed] [Google Scholar]
- Greene WH. Econometric Analysis. 2d Edition. New York: MacMillan Publishing Company; 1993. [Google Scholar]
- Halverson PK. Embracing the Strength of the Public Health System: Why Strong Government Public Health Agencies Are Vitally Necessary but Insufficient. Journal of Public Health Management and Practice. 2002;8(1):98–100. doi: 10.1097/00124784-200201000-00019. [DOI] [PubMed] [Google Scholar]
- Handler A, Issel M, Turnock B. A Conceptual Framework to Measure Performance of the Public Health System. 2001;91(8):1235–9. doi: 10.2105/ajph.91.8.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanneman RA, Riddle M. Introduction to Social Network Methods. Riverside, CA: Robert A. Hanneman and Mark Riddle; 2005. [Google Scholar]
- Health Resources and Services Administration. “Primary Care Service Areas” [accessed on August 1, 2009]. Available at http://datawarehouse.hrsa.gov/pcsa.aspx.
- Kassler WJ, Goldsberry YP. The New Hampshire Public Health Network: Creating Local Public Health Infrastructure through Community-Driven Partnerships. Journal of Public Health Management and Practice. 2005;11(2):150–7. doi: 10.1097/00124784-200503000-00008. [DOI] [PubMed] [Google Scholar]
- Leep CJ. 2005 National Profile of Local Health Departments. Washington, DC: National Association of County & City Health Officials; 2006. [DOI] [PubMed] [Google Scholar]
- Leviss PS. Financing the Public's Health. In: Novick LF, Morrow CB, Mays GP, editors. Public Health Administration: Principles for Population-Based Management. 2d Edition. Sudbury, MA: Jones and Bartlett; 2008. pp. 189–224. [Google Scholar]
- Mays GP. Causes and Consequences of Change in Local Public Health Spending. Orlando, FL: AcademyHealth Annual Research Meeting; 2007. [Google Scholar]
- Mays GP, Halverson PK, Scutchfield FD. Behind the Curve? What We Know and Need to Learn from Public Health Systems Research. Journal of Public Health Management and Practice. 2003;9(3):179–82. doi: 10.1097/00124784-200305000-00001. [DOI] [PubMed] [Google Scholar]
- Mays GP, McHugh MC, Shim K, Perry N, Halverson PK, Lenaway D, Moonesinge R. Identifying Dimensions of Performance in Local Public Health Systems: Results from the National Public Health Performance Standards Program. Journal of Public Health Management and Practice. 2004;10(3):193–203. doi: 10.1097/00124784-200405000-00003. [DOI] [PubMed] [Google Scholar]
- Mays GP, McHugh MC, Shim K, Perry N, Lenaway D, Halverson PK, Moonesinghe R. Institutional and Economic Determinants of Public Health System Performance. American Journal of Public Health. 2006;96(3):523–31. doi: 10.2105/AJPH.2005.064253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill J. Examining How Intra-Organizational Public Health Networks Are Linked to Process and Outcomes. New York: Columbia University Health Sciences, Department of Biomedical Informatics; 2007. [Google Scholar]
- Merrill J, Caldwell M, Rockoff ML, Gebbie K, Carley KM, Bakken S. Findings from an Organizational Network Analysis to Support Local Public Health Management. Journal of Urban Health. 2008;85(4):572–84. doi: 10.1007/s11524-008-9277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola RM. Turning Point's National Excellence Collaboratives: Assessing a New Model for Policy and System Capacity Development. Journal of Public Health Management and Practice. 2005;11(2):101–8. doi: 10.1097/00124784-200503000-00002. [DOI] [PubMed] [Google Scholar]
- Orton SN, Menkens AJ, Santos P. Public Health Business Planning: A Practical Guide. Sudbury, MA: Jones and Barlett; 2009. [Google Scholar]
- Padgett SM, Bekemeier B, Berkowitz B. Collaborative Partnerships at the State Level: Promoting Systems Changes in Public Health Infrastructure. Journal of Public Health Management and Practice. 2004;10(3):251–7. doi: 10.1097/00124784-200405000-00009. [DOI] [PubMed] [Google Scholar]
- Padgett SM, Bekemeier B, Berkowitz B. Building Sustainable Public Health Systems Change at the State Level. Journal of Public Health Management and Practice. 2005;11(2):109–15. doi: 10.1097/00124784-200503000-00003. [DOI] [PubMed] [Google Scholar]
- Powell WW. Neither Market Nor Hierarchy: Network Forms of Organization. Research in Organizational Behavior. 1990;12:295–336. [Google Scholar]
- Roussos ST, Fawcett SB. A Review of Collaborative Partnerships as a Strategy for Improving Community Health. Annual Review of Public Health. 2000;21:369–402. doi: 10.1146/annurev.publhealth.21.1.369. [DOI] [PubMed] [Google Scholar]
- Sandström A, Carlsson L. The Performance of Policy Networks: The Relation between Network Structure and Network Performance. Policy Studies Journal. 2008;36(4):497–524. [Google Scholar]
- Scutchfield FD, Knight EA, Kelly AV, Bhandari MW, Vasilescu IP. Local Public Health Agency Capacity and Its Relationship to Public Health System Performance. Journal of Public Health Management and Practice. 2004;10(3):204–15. doi: 10.1097/00124784-200405000-00004. [DOI] [PubMed] [Google Scholar]
- Varda DMP, Chandra AD, Stern SAMA, Lurie NMDM. Core Dimensions of Connectivity in Public Health Collaboratives. Journal of Public Health Management and Practice. 2008;14(5):E1–7. doi: 10.1097/01.PHH.0000333889.60517.46. [DOI] [PubMed] [Google Scholar]
- Zahner SJ. Local Public Health System Partnerships. Public Health Report. 2005;120(1):76–83. doi: 10.1177/003335490512000113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahner SJ, Corrado SM. Local Health Department Partnerships with Faith-Based Organizations. Journal of Public Health Management and Practice. 2004;10(3):258–65. doi: 10.1097/00124784-200405000-00010. [DOI] [PubMed] [Google Scholar]
- Zahner SJ, Kaiser B, Kapelke-Dale J. Local Partnerships for Community Assessment and Planning. Journal of Public Health Management and Practice. 2005;11(5):460–4. doi: 10.1097/00124784-200509000-00016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.