Abstract
INTRODUCTION
Patients who have previously undergone meniscectomy are known to potentially suffer subsequent knee problems including degenerative changes. Meniscal transplantation has been proposed as a possble solution to these problems. This article aims to review the current literature to consolidate the evidence surrounding the use of human meniscal allograft transplantation.
MATERIALS AND METHODS
Three databases (PubMed, Embase and Medline) were searched to find English language articles pertaining to meniscal allograft transplantation. Each article was critiqued by two authors using a structured appraisal tool, and stratified according to the level of evidence.
RESULTS
No Level I or II studies were identified. Many studies had small study groups with limited follow-up and patient selection and description of patient factors varied greatly. This made comparing data difficult. There were also very few papers concentrating on isolated meniscal transplantation. Four types of graft are used – fresh, fresh-frozen, cryopreserved and freeze-dried (lyophilised) graft. Cryopreserved and fresh-frozen allografts are deemed most suitable. Most authors advocate the use of non-irradiated grafts from screened donors to reduce transmission of infection. Best results occur when using bony anchors to fix the graft, although this requires accurate graft positioning. Patients have an improved outcome if they have less severe degenerative changes within the knee prior to transplantation.
CONCLUSIONS
No statistically significant studies looking at isolated meniscal transplantations have been found. The evidence suggests that meniscal allograft transplantation provides improvement of pain and function in the short and intermediate term. The effect on future joint degeneration is still unknown. The ideal patient group includes patients less than 40 years of age with knee pain, proven meniscal injury and a normally aligned, stable joint without severe degenerative changes.
Keywords: Meniscectomy - Meniscal allograft transplantation, Literature review
Approximately 1.5 million knee arthroscopic procedures are carried out each year, with over 50% involving meniscal surgery.1 Attitudes towards meniscal surgery have changed dramatically over the past century. Meniscal preservation in the form of meniscal repair is now sought in favour of partial or total meniscectomy. Unfortunately, meniscal repair is not always feasible. Resection of even 20% of meniscal tissue has been shown to increase contact forces through the articular cartilage by 350%.2 The association between osteoarthritis and meniscectomy was first established by Fairbanks in 1948 and is now well recognised.3 Milachowski and Wirth4 first performed meniscal transplantation in 1984. Meniscal transplantation has been seen by some as an answer to the problem of preventing degenerative changes in knees of patients who have previously undergone meniscectomy. This article will review the current evidence surrounding the use of human meniscal allograft transplantation.
Materials and Methods
There were no Cochrane reviews available on this topic. Three databases were searched (PubMed, Embase and Medline) and only English language papers were identified. Keywords used to perform this search were: ‘meniscal allograft transplantation’, ‘meniscal repair’, ‘meniscal’, and ‘transplant’. Each paper was reviewed by at least two of the authors. Templates from the Critical Appraisal Skills Programme (CASP) were used to appraise each paper.5 Data from each paper was recorded into an Excel spread sheet to allow ease of comparison. Each paper was stratified according to the Level-of-Evidence-Rating, as established by Wright et al.6
The literature search identified numerous studies, with almost as many review papers. There were no prospective randomised control studies, one systematic review, nine reviews, three observational studies and three studies. No Level I or II studies were identified. Many studies reporting meniscal transplants had only small study groups with relatively short follow-up. There is often large variability in inclusion criteria, graft types, fixation, concomitant procedures, outcome measures and rehabilitation. Comparing studies is, therefore, difficult.
Review
The menisci are two semilunar, fibrocartilage, wedge-shaped discs. The lateral meniscus is C-shaped with a short distance between its anterior and posterior horns. The medial meniscus is U-shaped with larger separation of the two horns.7,8 The medial meniscus is less mobile than the lateral meniscus. This is explained by the circumferential capsular attachment of the medial meniscus, including attachment to the deep fibres of the medial collateral ligament. The lateral meniscus lacks collateral ligament attachment, in addition to little significant tethering around the popliteal hiatus.9 Menisci have several important functions including load-bearing. Evidence suggests that the medial meniscus transfers 40% of the load through the medial compartment of the knee with 70% of the load through the lateral compartment taken by the lateral meniscus.10 The ultrastructure of the menisci, consisting of three layers of collagen matrix organised tangentially and circumferentially, converts these loading forces into hoop stresses.9 In addition to weight-bearing, menisci also increase joint congruency and act as secondary stabilisers preventing translation of the femur on the tibia in conjunction with the cruciate ligaments. They are also thought to contribute to articular cartilage nutrition and lubrication.
Patient selection description is variable within the studies critiqued. Most studies had patient numbers between 20–30.11 The largest study by Verdonk et al.12 had 101 patients. Only four studies had a mean follow-up period of over 5 years with Wirth et al.13 reporting after 14 years of patient follow-up. Most studies showed a male predominance. The time from previous meniscectomy to meniscal transplant varied widely, although was not even disclosed in some studies.12,14–16 One study reported mean time from meniscectomy to transplant of over 10 years.17 The number of previous knee operations was only described in three of the studies identified.18–20
Whilst many review articles proffer that surgical results are best in those patients with Outerbridge Grade 3 or less chondral damage (Table 1), very few studies actually describe pre-operative grades for their patient subsets. Only two papers identified radiographic criteria used for assessing suitability for the procedure.11
Table 1.
Outerbridge grading for cartilage damage
| Grade | Degree of chondral damage |
|---|---|
| 0 | Normal cartilage |
| 1 | Softening and swelling of cartilage |
| 2 | Partial-thickness defect with surface fissures |
| NOT down to subchondral bone or greater than 1.5 cm in diameter | |
| 3 | Fissures down to subchondral bone with a diameter greater than 1.5 cm |
| 4 | Subchondral bone exposed |
Most studies discussed ligament stability and leg alignment. It is widely accepted that both factors have a significant impact on meniscal graft outcome, and that any abnormalities should be corrected before, or at the time of, surgery.8,13 This is one of the difficulties with many series. Very few cases (∼20%) of isolated meniscal transplants are described.21 Therefore, interpretation of what impact the meniscal graft had on the clinical outcome is often impossible to elucidate.
Many areas pertaining to the surgical procedure itself are contentious. Early studies describe open procedures for meniscal transplant with progression to arthroscopically assisted or even entirely arthroscopic execution. There is insufficient evidence available to draw comparisons between each method with regard to outcome. It is believed by many authors that arthroscopic procedures convey benefits with regard to decreased postoperative morbidity and improved visualisation, although no studies directly compare open and arthroscopic procedures with these parameters in mind.
Four methods of graft type have been used. These include fresh allograft, fresh-frozen, cryopreserved and freeze-dried (lyophilised). After a study by Rodeo et al.,22 fresh graft was felt to be superior as preservation of viable fibrochondrocytes was achieved at the time of implantation. However, animal studies by Jackson et al.23 using goats demonstrated complete replacement of all donor cells by host cells within a few days of implantation. Rath et al.15 analysed outcomes of 18 patients after meniscal allograft transplantation at a mean time interval of 5.4 years. They reported that 36% of grafts tore following implantation.15 Stollsteimer et al.24 followed 22 patients who received cryopreserved grafts for a mean of 3 years after transplantation. They describe graft tears in 25% of their patients.24 This high rate of graft injury is postulated to be a result of the reduced numbers of fibrochondrocytes and lower cell activity, as demonstrated by Rodeo et al.22 and Jackson et al.23 Healing of all four graft types to the periphery has been demonstrated.7 Lyophilisation of grafts adversely affects their biomechanical properties and has led to graft shrinkage. It is no longer recommended as a means of graft preservation.25 Fresh allografts obviously present logistic problems with finding a suitable donor–recipient match within the 7 days before deterioration in graft cellularity is seen. There is a theoretical increase in the risk of disease transmission.7 Cryopreserved and fresh-frozen allografts are most commonly used.26
Disease transmission risk is a very real concern with meniscal transplant surgery. Human immunodeficiency virus (HIV), hepatitis B and C, and syphilis are potentially transferable via graft material. The documented risk for HIV transmission is estimated at 1 in 8 million.27 Secondary sterilisation of allografts has previously been undertaken using gamma radiation, ethylene oxide or chemical sterilisation. Unfortunately, the dose of gamma radiation deemed effective at eradicating HIV (2.5 mrad) produces detrimental changes in the mechanical structure of the allograft.28 Ethylene oxide is no longer used as one of its by-products has been shown to cause synovitis.29 Currently, most study groups recommend the use of non-irradiated grafts from ‘screened’ donors.
Appropriate size-matching of the graft to the donor site is believed to be vital to effective meniscal function postoperatively.30 Whilst most authors accept a size mismatch of less than 5%, no studies have formerly quantified this value or the effects of meniscal sizing errors. Controversy as to the most suitable methods of pre-operative sizing still remains. Many centres use bony landmarks on plain radiographs. However, with accuracy of only 92% with significant variability in meniscal length and width in comparison to the bony landmarks, this remains suboptimal.31 Shaffer et al.21 used magnetic resonance imaging (MRI) scans to evaluate meniscal size and reported increased accuracy compared to plain radiographs, but still only 36% of scans were accurate to within 2 mm. Computed tomography (CT) was compared favourably to MRI and plain radiographs in a further study, although MRI was more accurate in determining meniscal height.32 Further research is required to improve the accuracy of graft sizing and also to define the tolerance of the knee to size mismatch.33
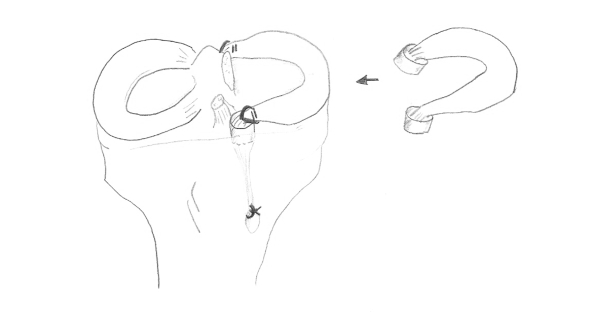
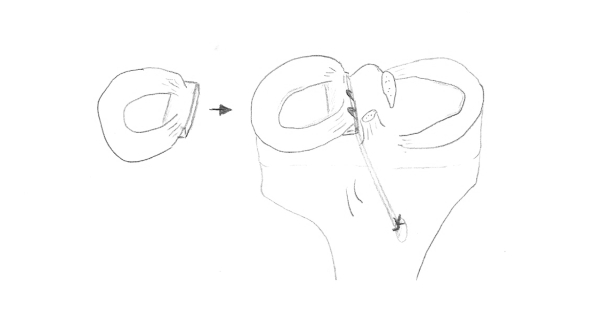
Fixation of the graft is another area stimulating debate. This can be achieved by soft-tissue sutures, bony plugs or a bony bridge. Cadaveric studies suggest that bony fixation of the anterior and posterior horns are required to restore normal tibial contact forces and recreate the hoop stresses on loading, a function that serves to protect the articular cartilage. This is not provided by suture fixation alone.34,35 Better results were described for grafts using bony fixation.22 Verdonk et al.,12 however, described satisfactory results using only soft-tissue fixation. Whilst it would appear that bony fixation is superior, it does require accurate anatomical graft placement. Malpositioning of the bony anchors has produced poor results in both cadaveric and animal studies.36,37 It is widely accepted that two bony plugs (one attached to each horn) should be used for medial meniscal allografts (Fig. 1). In the lateral meniscus, the anterior and posterior horns are much closer together as previously highlighted, thus making a bony bridge anchoring both horns more appropriate (Fig. 2).
Figure 1.
The use of two bony plugs attached to each horn of the medial meniscus.
Figure 2.
The use of one bony plug attached to both horns of the lateral meniscus.
Ultimately, the success of meniscal allograft transplantation is judged on three outcome measures: (i) improvement in short-term symptoms of pain (and instability); (ii) improvement in patient function; and (iii), most importantly, whether meniscal transplant surgery prevents the onset or progression of degenerative changes seen historically following partial or total meniscectomy. The results from the studies identified are difficult to compare due to the variability in outcome measures assessed. The most commonly assessed validated outcome measures used include the Lysholm, Tegner and International Knee Documentation Committee outcome scores. A recent review article reported that over 75% of patients were satisfied with the procedure in terms of pain relief and functional improvement over a relatively short follow-up of up to 6 years.26 Wirth et al.13 reported satisfactory results over a 14-year follow-up period in 23 patients. Unfortunately, in addition to variable outcome measure, most series report results for patients undergoing concomitant procedure such as ACL reconstruction or corrective tibial osteotomies. What effect these additional procedures have on outcome is unclear, despite being investigated in three studies. These studies included only small numbers of isolated meniscal transplants.12,13,18 Over 90% of patients reported good-to-excellent results with isolated meniscal transplantation in one series.19 Subjective assessment criteria have been shown to have poor correlation with graft morphology.14 Objective assessment of the graft has been undertaken using MRI or second-look arthroscopy. The long-term effect of meniscal transplant surgery on prevention of degenerative changes remains unanswered. Stollsteimer et al.24 reported a decrease in joint space of 1 mm in 22 patients over a 3-year follow-up. Rath et al.15 reported no change in 18 patients over a 5-year period. Further long-term results of level one or two studies are required.
As it would seem with most aspects of meniscal transplant surgery, no agreed uniform protocol exists for patient postoperative rehabilitation. Many regimens are described and tend to be governed by the concomitant procedure undertaken (e.g. ACL reconstruction).38,39 Further research with standardised protocols would clarify optimal rehabilitation strategies. Perhaps most pertinent is the return to sports following meniscal transplantation. Matava11 recommended that strenuous sports, involving running, jumping, cutting, and pivoting, should be avoided until further research clarifies the effect of such activities on graft healing and survival.
Conclusions
The current body of evidence suggests that meniscal allograft transplantation provides improvement in the short and intermediate term with regard to pain and level of function for daily activities. Patient selection appears critical with the best results obtained in patients under 40 years of age who complain of knee pain, with a normal aligned and stable knee joint (or correctable at the time of surgery) and limited early degenerative changes (Outerbridge Grade 3 or less). Graft selection, sizing, sterilisation and preservation remain controversial areas. The protective effect of meniscal allograft transplantation against progression of degenerative joint disease remains unproven. Further long-term results are required to provide definitive evidence.
References
- 1.Peters G, Wirth CJ. The current state of meniscal allograft transplantation and replacement. Knee. 2003;10:19–31. doi: 10.1016/s0968-0160(02)00139-4. [DOI] [PubMed] [Google Scholar]
- 2.Seedhom BB, Hargreaves DJ. Transmission of load in the knee joint with special reference to the role of the menisci, part II: experimental results, discussions, and conclusions. Eng Med. 1979;8:220–8. [Google Scholar]
- 3.Fairbanks TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664–70. [PubMed] [Google Scholar]
- 4.Milachowski KA, Weismeier K, Wirth CJ. Homologous meniscal transplantation, experimental and clinical results. Int Orthop. 1989;13:1–11. doi: 10.1007/BF00266715. [DOI] [PubMed] [Google Scholar]
- 5.Critical Appraisal Skills Programme. Evidence-based Health Care: supporting evidence based decision making in practice. Oxford: CASP; 2005. A CASP CD-ROM and workbook. [Google Scholar]
- 6.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85:1–4. [PubMed] [Google Scholar]
- 7.Rijk PC. Meniscal allograft transplantation. Part I: background, results, graft selection and preservation, and surgical considerations. Arthroscopy. 2004;20:728–43. doi: 10.1016/j.arthro.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 8.Alford W, Cole BJ. The indications and techniques for meniscal transplant. Orthop Clin North Am. 2005;36:469–84. doi: 10.1016/j.ocl.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Klimkiewicz JJ, Shaffer B. Meniscal surgery 2002 update: indications and techniques for resection, repair, regeneration, and replacement. Arthroscopy. 2002;18(Suppl 2):14–25. doi: 10.1053/jars.2002.36505. [DOI] [PubMed] [Google Scholar]
- 10.Walker BF, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop. 1975;109:184–92. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 11.Matava MJ. Meniscal allograft transplantation. A systematic review. Clin Orthop. 2007;455:142–57. doi: 10.1097/BLO.0b013e318030c24e. [DOI] [PubMed] [Google Scholar]
- 12.Verdonk P, Demurie A, Almqvist K, Veys E, Verbruggen G, Verdonk R. Transplantation of viable meniscal allograft: survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87:715–24. doi: 10.2106/JBJS.C.01344. [DOI] [PubMed] [Google Scholar]
- 13.Wirth CJ, Peters G, Milachowski KA, Weismeier KG, Kohn D. Long-term results of meniscal allograft transplantation. Am J Sports Med. 2002;30:174–81. doi: 10.1177/03635465020300020501. [DOI] [PubMed] [Google Scholar]
- 14.Garrett JC. Meniscal transplantation: a review of 43 cases with 2- to 7-year follow-up. Sports Med Arthrosc Rev. 1993;1:164–7. [Google Scholar]
- 15.Rath E, Richmond JC, Yassir W, Jeffreys DA, Albright JD, Gundogan F. Meniscal allograft transplantation. Two to eight year results. Am J Sports Med. 2001;29:410–4. doi: 10.1177/03635465010290040401. [DOI] [PubMed] [Google Scholar]
- 16.Ryu RKN, Dunbar WH, Morse GG. Meniscal allograft replacement: a 1-year to 6-year experience. Arthroscopy. 2002;18:989–94. doi: 10.1053/jars.2002.36104. [DOI] [PubMed] [Google Scholar]
- 17.Van Arkel ERA, de Boer HH. Survival analysis of human meniscal transplantations. J Bone Joint Surg Br. 2002;84:227–33. doi: 10.1302/0301-620x.84b2.12443. [DOI] [PubMed] [Google Scholar]
- 18.Yoldas E, Sekiya J, Irrgang J, Fu F, Harner C. Arthroscopically assisted meniscal allograft transplantation with and without combined anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2000;11:173–82. doi: 10.1007/s00167-003-0362-y. [DOI] [PubMed] [Google Scholar]
- 19.Cameron JC, Saha S. Meniscal allograft transplantation for unicompartmental arthritis of the knee. Clin Orthop. 1997;337:164–71. doi: 10.1097/00003086-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Noyes FR, Barber-Westin SD, Rankin M. Meniscal transplantation in symptomatic patients less than fifty years old: surgical technique. J Bone Joint Surg Am. 2005;87:149–67. doi: 10.2106/JBJS.E.00347. [DOI] [PubMed] [Google Scholar]
- 21.Shaffer B, Kennedy S, Kimkiewicz J, Yao L. Pre-operative sizing of meniscal allografts in meniscal transplantation. Am J Sports Med. 2000;28:524–33. doi: 10.1177/03635465000280041301. [DOI] [PubMed] [Google Scholar]
- 22.Rodeo SA, Seneviratne A, Suzuki K, Felder K, Wickiewicz TL, Warren RF. Histological analysis of human meniscal allografts. A preliminary report. J Bone Joint Surg Am. 2000;82:1071–82. doi: 10.2106/00004623-200008000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Jackson DW, Whelan J, Simon TM. Cell survival after transplantation of fresh meniscal allografts. DNA probe analysis in a goat model. Am J Sports Med. 1993;21:540–50. doi: 10.1177/036354659302100411. [DOI] [PubMed] [Google Scholar]
- 24.Stollsteimer GT, Shelton WR, Dukes A, Bomboy AL. Meniscal allograft transplantation: a 1–5-year follow-up of 22 patients. Arthroscopy. 2000;16:343–7. doi: 10.1016/s0749-8063(00)90077-x. [DOI] [PubMed] [Google Scholar]
- 25.Sekiya JK, Ellingson CI. Meniscal allograft transplantation. J Am Acad Orthop Surg. 2006;14:164–74. doi: 10.5435/00124635-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Cook JL. The current status of treatment for large meniscal defects. Clin Orthop. 2005;435:88–95. doi: 10.1097/00003086-200506000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Buck BE, Resnick L, Shah SM, Malinin TI. Human immunodeficiency virus cultured from bone. Implications for transplantation. Clin Orthop. 1990;251:249–53. [PubMed] [Google Scholar]
- 28.Vangsness TC, Garcia IA, Mills R, Kainer MA, Roberts MR, Moore TM. Allograft transplantation in the knee: tissue regulation, procurement, processing, and sterilization. Am J Sports Med. 2003;31:474–81. doi: 10.1177/03635465030310032701. [DOI] [PubMed] [Google Scholar]
- 29.Jackson DW, Windler GE, Simon TM. Intraarticular reaction associated with the use of freezedried, ethylene oxide-sterilized bone–patella–bone allografts in reconstruction of the anterior cruciate ligament. Am J Sports Med. 1990;18:1–10. doi: 10.1177/036354659001800101. [DOI] [PubMed] [Google Scholar]
- 30.Rodeo SA. Meniscal allografts – where do we stand? Am J Sports Med. 2001;29:246–60. doi: 10.1177/03635465010290022401. [DOI] [PubMed] [Google Scholar]
- 31.Pollard ME, Kang Q, Berg EE. Radiographic sizing for meniscal transplantation. Arthroscopy. 1995;11:684–7. doi: 10.1016/0749-8063(95)90110-8. [DOI] [PubMed] [Google Scholar]
- 32.Carpenter JE, Wojtys EM, Huston LJ, Crabbe JP, Aisen AM. Pre-operative sizing of meniscal allografts [Abstract] Athroscopy. 1993;9:344. [Google Scholar]
- 33.Rijk PC. Meniscal allograft transplantation. Part II: alternative treatments, effects on articular cartilage, and future directions. Arthroscopy. 2004;20:851–9. doi: 10.1016/j.arthro.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 34.Chen MI, Branch TP, Hutton WC. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy. 1996;12:174–81. doi: 10.1016/s0749-8063(96)90007-9. [DOI] [PubMed] [Google Scholar]
- 35.Alhalki MM, Howell SM, Hull ML. How three months for fixing a medial meniscal allograft affect tibial contact mechanics. Am J Sports Med. 1999;27:320–8. doi: 10.1177/03635465990270030901. [DOI] [PubMed] [Google Scholar]
- 36.Szomer ZL, Martin TE, Bonar F, Murrell GAC. The protective effects of meniscal transplantation on cartilage: an experimental study in sheep. J Bone Joint Surg Am. 2000;82:80–9. doi: 10.2106/00004623-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Sekaran SV, Hull ML, Howell SM. Non-anatomic location of the posterior horn of a medial meniscal autograft implanted in a cadaveric knee adversely affects the pressure distribution on the tibial plateau. Am J Sports Med. 2002;30:74–82. doi: 10.1177/03635465020300012601. [DOI] [PubMed] [Google Scholar]
- 38.Fritz JM, Irrgang JJ, Harner CD. Rehabilitation following allograft meniscal transplantation: a review of the literature and case study. J Orthop Sports Phys Ther. 1996;24:98–106. doi: 10.2519/jospt.1996.24.2.98. [DOI] [PubMed] [Google Scholar]
- 39.Heckmann TP, Barber-Westin SD, Noyes FR. Meniscal repair and transplantation: indications, techniques, rehabilitation, and clinical outcome. J Orthop Sports Phys Ther. 2006;36:795–814. doi: 10.2519/jospt.2006.2177. [DOI] [PubMed] [Google Scholar]