Abstract
INTRODUCTION
We aimed to evaluate the role of routine measurements of serum amylase and lipase in the diagnosis of acute abdominal pain.
PATIENTS AND METHODS
We identified all patients who had serum amylase and lipase assays over a 62-day period at a single university teaching hospital and reviewed their case notes.
RESULTS
We excluded 58 of the 1598 patients on grounds of ineligibility (< 18 years of age and those transferred from other hospitals). A complete data set was obtained for 1520 (98.7%) of the remaining 1540 patients. Only 9.1% of requests were based on a clinical suspicion of acute pancreatitis. Of the 44 (2.9%) patients who had acute pancreatitis, only 28 (63.6%) had an associated rise in serum amylase and/or lipase 3 times above the maximum reference range, the remainder being diagnosed radiologically. At this cut-off range, the sensitivity and specificity for serum amylase were 50% and 99%, and those for serum lipase 64% and 97%, respectively.
CONCLUSIONS
Routine measurements of serum amylase and lipase are unhelpful in the diagnosis of acute abdominal pain unless there is clinical suspicion of acute pancreatitis. In these patients, assay of lipase alone is preferable to assay of amylase alone or both enzymes.
Keywords: Amylase, Lipase, Acute pancreatitis, Abdominal pain, Diagnosis, Sensitivity, Specificity, Costs
Acute abdominal pain is a common condition presenting to both the emergency department and surgical admissions unit. With the introduction of the ‘four-hour wait’ in the UK, junior medical staff must assess and plan appropriate management for patients quickly and effectively.1 In order to facilitate this, nursing staff commonly request ‘routine’ blood tests on admission, so that the results are available when clinicians arrive to assess patients.
The incidence of acute pancreatitis in the UK is between 100–250 per 1,000,000 population per year,2,3 with most patients presenting with acute abdominal pain. Serum lipase and/or amylase are widely used as initial diagnostic tests. Current practice in our institution is to perform both these tests on all patients presenting with acute abdominal pain.
The accuracy of these tests depends on both the diagnostic threshold used, and the study population. In addition, both enzymes can be elevated in conditions other than pancreatitis;4,5 in some cases of pancreatitis, enzyme concentrations may be normal.6 Some studies suggest that both tests are needed to diagnose pancreatitis accurately,6–9 whilst others state that this is unnecessary.7,10 Where one test is used, lipase is believed to be superior in sensitivity and specificity.10–13
We performed this study to evaluate the role of routine serum amylase and lipase testing in the diagnosis of acute abdominal pain, establish the sensitivity and specificity of the tests, and identify any cost implications associated with their use.
Patients and Methods
Design and setting
An audit performed in a 1200-bed university teaching hospital.
Participants
All patients having serum amylase and lipase assayed over a 62-day period from 6 August 2007 to 7 October 2007 were identified by the clinical pathology laboratory. Patients under the age of 18 years and those transferred from other hospitals were excluded from the study. Patients having more than one assay performed over this time period had only the first episode recorded.
Methodology
Biochemical data of these patients were recorded directly into a Microsoft Access database. A review of the notes was undertaken by two individuals (FW and TW) and subsequently verified by one (PAS) while patients were still admitted. Where the request was from the emergency department, data were collected from the Emergency Department Information System (EDIS). The case notes were reviewed for those patients admitted to hospital from the emergency department and in those in whom the request was from the surgical admissions unit. Data analysis was performed using SPSS v.14.0 software (SPSS Inc.; Chicago, IL, USA), with the standard formulae for sensitivity and specificity being used.14 The study was approved by the audit department of Nottingham University Hospitals.
Data were collected to determine patient demographics, the source of the request and whether that request was based on a clinical suspicion of acute pancreatitis. The final diagnoses of all patients were recorded, and the positive and negative predictive values, sensitivities and specificities of amylase and lipase were calculated. The financial burden of routine screening was estimated using NHS reference costs.
Results
We identified 1598 patients over the study period and excluded 58 who were either < 18 years of age or transferred from other hospitals. Of the remaining 1540 patients, a complete data set was obtained for 1520 (98.7%); 722 (47.5%) were male with a mean (SD) age of 49.6 (27.4) years.
There were substantially more requests from the emergency department (85.5%) than the surgical admissions unit (14.5%). Only 6.8% of requests from the emergency department were based on a clinical suspicion of acute pancreatitis. The remainder were performed as routine screening tests, and no specific mention of pancreatitis was found in the notes as a differential diagnosis for the presentation. On the surgical admissions unit, 22.7% of requests were based on clinical suspicion of acute pancreatitis. Of those presenting to the emergency department, 799 (61.4%) were admitted to hospital, with a median (interquartile range [IQR]) length of stay of 1 (0–4) day. For the surgical admissions unit, 191 (86.8%) patients were admitted, with a median (IQR) length of stay of 3 (1–5) days.
It was apparent, on review of the case notes to identify the primary diagnosis, that a number of requests were inappropriate (Table 1). Only 54.5% of patients having serum amylase and lipase assays had gastrointestinal pathology.
Table 1.
Final diagnoses of all patients having serum amylase and lipase measured
| Gastrointestinal pathology | |
| Gallstone disease | 177 (11.6%) |
| Non-specific abdominal pain | 166 (10.9%) |
| Blunt abdominal trauma | 132 (8.7%) |
| Gastrointestinal bleeding | 55 (3.6%) |
| Peptic ulcer disease | 45 (3.0%) |
| Acute pancreatitis | 44 (2.9%) |
| Gastroenteritis | 43 (2.8%) |
| Appendicitis | 42 (2.8%) |
| Bowel obstruction | 37 (2.5%) |
| Other | 27 (1.8%) |
| Perforated viscus | 26 (1.7%) |
| Constipation | 18 (1.2%) |
| Postoperative pain (non-specific) | 16 (1.1%) |
| Total | 828 (54.5%) |
| Other systems | |
| Cardiovascular | 182 (11.9%) |
| Urology | 181 (11.9%) |
| Gynaecology | 80 (5.3%) |
| Other medical | 80 (5.3%) |
| Orthopaedics | 47 (3.1%) |
| Respiratory | 43 (2.8%) |
| Alcohol intoxication without pancreatitis | 37 (2.5%) |
| Neurology | 28 (1.8%) |
| Vascular | 10 (0.7%) |
| Died in emergency department (cause unknown) | 4 (0.3%) |
| Total | 692 (45.5%) |
We identified 44 cases (2.9%) of acute pancreatitis in the study. Only 28 cases (63.6%) were associated with a rise in serum amylase and/or lipase above the diagnostic threshold of 3 times the upper limit of the laboratory reference range; in this instance 900 IU/l for lipase and 330 IU/l for amylase. Acute pancreatitis was diagnosed radiologically in the remaining 16 patients, 7 by ultrasound scan and 9 by computed tomography (CT). A total of 41 false-positive tests were identified, mostly attributable to other upper gastrointestinal conditions such as perforated peptic ulcer disease. Radiological evidence of acute pancreatitis was not found in this group of 41 patients.
At a diagnostic threshold of 5 times the upper limit of the laboratory reference range, the specificity and sensitivity of amylase were 99% and 39%, respectively (Table 2). By reducing the diagnostic threshold to 3 times the upper limit, the specificity remained unchanged, but the sensitivity increased to 50%. Similarly for lipase, at 5 times the upper limit of the laboratory reference range the specificity was 98% and the sensitivity 57%. By reducing the diagnostic threshold to 3 times the upper limit, the specificity reduced to 97%, but the sensitivity increased to 64%.
Table 2.
Serum amylase and lipase for the diagnosis of acute pancreatitis
| Test | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|
| Amylase ≥ 3× reference | 50% | 99% | 51% | 99% |
| Amylase ≥ 5× reference | 39% | 99% | 50% | 98% |
| Lipase ≥ 3× reference | 64% | 97% | 41% | 99% |
| Lipase ≥ 5× reference | 57% | 98% | 50% | 99% |
| Amylase and lipase ≥ 3× reference | 50% | 99% | 51% | 99% |
| Amylase and lipase ≥ 5× reference | 32% | 99% | 47% | 98% |
The negative predictive value of both tests was 98–99% irrespective of the threshold used, with positive predictive values for amylase of 50% at a cut-off of 5 times the upper limit of the laboratory reference range, and 51% at a cut-off of 3 times. The positive predictive value for lipase was 50% at a cut-off of 5 times the upper limit of the laboratory reference range, and 41% at a cut-off of 3 times.
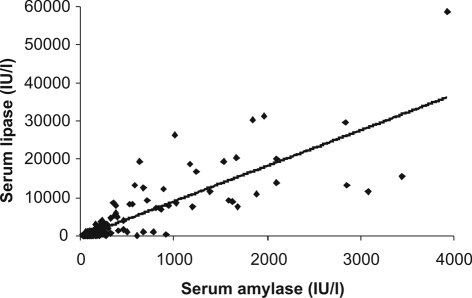
There was no additional benefit in performing both tests, with comparable sensitivities, specificities, positive and negative predictive values to amylase and lipase measured individually. There was a positive correlation (r2 = 0.74) between serum amylase and lipase concentrations (Fig. 1).
Figure 1.
Correlation between serum lipase and amylase (r2 = 0.74).
Current laboratory costs for these tests in our institution are £1.94 for amylase, and £2.50 for lipase. A total of 1382 routine requests were instigated, which identified only 12 cases of acute pancreatitis by elevated serum amylase and/or lipase. This equates to a total financial burden of £6136 over a 62-day period with 115 people needing to be screened at a cost of £511 for each diagnosis of acute pancreatitis.
Discussion
It is evident from this study that our laboratory receives a large number of unnecessary and inappropriate requests for amylase and lipase tests, including those for patients presenting with extra-abdominal pathology. The 1382 routine tests performed identified only 12 cases of acute pancreatitis, highlighting that routine testing has a low yield (0.9%). This is associated with an undesirable financial burden, with 115 patients needing to be screened at a cost of £511 for each diagnosis of acute pancreatitis. The positive correlation (r2 = 0.74) between amylase and lipase suggests that both tests need not be performed; as lipase is the more sensitive test for acute pancreatitis, it should be the investigation of choice where available.
Whilst some studies report that a rise in serum amylase of greater than 3 times the upper limit of the laboratory reference range is supportive of a diagnosis of acute pancreatitis,15,16 a greater than 5-fold increase has also been suggested.17 In our study, the sensitivity for amylase at 5 times the upper limit of normal was 39%. A sensitivity of 50% was achieved, without any associated decrease in specificity (99%), by lowering the diagnostic threshold to 3 times the upper limit of normal. The sensitivity for lipase at 5 times the upper limit of normal was 57% in our study. By dropping the diagnostic threshold to 3 times the upper limit of normal a sensitivity of 64% was achieved, with only a 1% decrease in specificity (98% to 97%). A number of false positives have been identified, although all are well-known causes of elevated amylase and/or lipase.18 A substantial number of patients with acute pancreatitis in our study had only a mild elevation of serum amylase and lipase, which may be due to delayed presentation,19 pancreatic exocrine failure,20 or hypertriglyceridaemia,18 which interferes with some amylase assays.
Our data are comparable to other studies, with sensitivities for amylase previously reported as low as 61% and specificities as high as 95%,18 and sensitivities as low as 55% and specificities higher than 95% for lipase.18,21 Previous studies have suggested that the most sensitive test for the diagnosis of acute pancreatitis is lipase, at a threshold of 3 times the upper limit of normal.11,13 This clinically important message has been confirmed by our study, with no increase in sensitivity or specificity found by performing both tests.
Whilst this is a substantial study of 1520 patients, there are some limitations. As patients have been identified by amylase and lipase request, it is possible that a diagnosis of acute pancreatitis has been made without these tests having ever been requested. Whilst this is unlikely, it is possible that a few cases may have been missed. The performance of these tests in addition to other biochemical markers may allow for some cost reduction, but accurate ascertainment of this is difficult.
At present, serum amylase and lipase assays are requested for all patients presenting with acute abdominal pain. Our data suggest that indiscriminate testing for serum amylase and lipase is associated with unnecessary expenditure, and that targeted assays requested by a clinician who has seen and examined the patient may minimise this, especially as routine measurements of serum amylase and lipase are unhelpful in the diagnosis of acute abdominal pain unless there is clinical suspicion of acute pancreatitis.
Conclusions
In view of the high correlation between amylase and lipase, performing both tests is not necessary. Based on the evidence that a serum lipase concentration of ≥ 3 times the upper limit of the laboratory reference range is has a sensitivity and specificity of 64% and 97%, respectively, for a diagnosis of acute pancreatitis when compared with corresponding values of 50% and 99% for amylase, we suggest that assay of a single enzyme (lipase) based on clinical suspicion may result in cost savings.
References
- 1.Department of Health. Reforming Emergency Care: First Steps to a New Approach. London: DH; 2001. < http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4008702>. [Google Scholar]
- 2.Toh SK, Phillips S, Johnson CD. A prospective audit against national standards of the presentation and management of acute pancreatitis in the South of England. Gut. 2000;46:239–43. doi: 10.1136/gut.46.2.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldacre MJ, Roberts SE. Hospital admission for acute pancreatitis in an English population, 1963–98: database study of incidence and mortality. BMJ. 2004;328:1466–9. doi: 10.1136/bmj.328.7454.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gumaste VV, Roditis N, Mehta D, Dave PB. Serum lipase levels in nonpancreatic abdominal pain versus acute pancreatitis. Am J Gastroenterol. 1993;88:2051–5. [PubMed] [Google Scholar]
- 5.Treacy J, Williams A, Bais R, Willson K, Worthley C, et al. Evaluation of amylase and lipase in the diagnosis of acute pancreatitis. Aust NZ J Surg. 2001;71:577–82. doi: 10.1046/j.1445-2197.2001.02220.x. [DOI] [PubMed] [Google Scholar]
- 6.Orebaugh SL. Normal amylase levels in the presentation of acute pancreatitis. Am J Emerg Med. 1994;12:21–4. doi: 10.1016/0735-6757(94)90191-0. [DOI] [PubMed] [Google Scholar]
- 7.Corsetti JP, Cox C, Schulz TJ, Arvan DA. Combined serum amylase and lipase determinations for diagnosis of suspected acute pancreatitis. Clin Chem. 1993;39:2495–9. [PubMed] [Google Scholar]
- 8.Lin XZ, Wang SS, Tsai YT, Lee SD, Shiesh SC, et al. Serum amylase, isoamylase, and lipase in the acute abdomen. Their diagnostic value for acute pancreatitis. J Clin Gastroenterol. 1989;11:47–52. doi: 10.1097/00004836-198902000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Frank B, Gottlieb K. Amylase normal, lipase elevated: is it pancreatitis? A case series and review of the literature. Am J Gastroenterol. 1999;94:463–9. doi: 10.1111/j.1572-0241.1999.878_g.x. [DOI] [PubMed] [Google Scholar]
- 10.Smith RC, Southwell-Keely J, Chesher D. Should serum pancreatic lipase replace serum amylase as a biomarker of acute pancreatitis? Aust NZ J Surg. 2005;75:399–404. doi: 10.1111/j.1445-2197.2005.03391.x. [DOI] [PubMed] [Google Scholar]
- 11.Gumaste V, Dave P, Sereny G. Serum lipase: a better test to diagnose acute alcoholic pancreatitis. Am J Med. 1992;92:239–42. doi: 10.1016/0002-9343(92)90070-r. [DOI] [PubMed] [Google Scholar]
- 12.Clave P, Guillaumes S, Blanco I, Nabau N, Merce J, et al. Amylase, lipase, pancreatic isoamylase, and phospholipase A in diagnosis of acute pancreatitis. Clin Chem. 1995;41:1129–34. [PubMed] [Google Scholar]
- 13.Chase CW, Barker DE, Russell WL, Burns RP. Serum amylase and lipase in the evaluation of acute abdominal pain. Am Surg. 1996;62:1028–33. [PubMed] [Google Scholar]
- 14.Altman DG, Bland JM. Statistics notes: diagnostic tests 1: sensitivity and specificity. BMJ. 1994;308:1552. doi: 10.1136/bmj.308.6943.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kazmierczak SC, Catrou PG, Van Lente F. Diagnostic accuracy of pancreatic enzymes evaluated by use of multivariate data analysis. Clin Chem. 1993;39:1960–5. [PubMed] [Google Scholar]
- 16.Lankisch PG, Burchard-Reckert S, Lehnick D. Underestimation of acute pancreatitis: patients with only a small increase in amylase/lipase levels can also have or develop severe acute pancreatitis. Gut. 1999;44:542–4. doi: 10.1136/gut.44.4.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smotkin J, Tenner S. Laboratory diagnostic tests in acute pancreatitis. J Clin Gastroenterol. 2002;34:459–62. doi: 10.1097/00004836-200204000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Yadav D, Agarwal N, Pitchumoni CS. A critical evaluation of laboratory tests in acute pancreatitis. Am J Gastroenterol. 2002;97:1309–18. doi: 10.1111/j.1572-0241.2002.05766.x. [DOI] [PubMed] [Google Scholar]
- 19.Clavien PA, Robert J, Meyer P, Borst F, Hauser H, et al. Acute pancreatitis and normoamylasaemia. Not an uncommon combination. Ann Surg. 1989;210:614–20. doi: 10.1097/00000658-198911000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spechler SJ, Dalton JW, Robbins AH, Gerzof SG, Stern JS, et al. Prevalence of normal serum amylase levels in patients with acute alcoholic pancreatitis. Dig Dis Sci. 1983;28:865–9. doi: 10.1007/BF01317034. [DOI] [PubMed] [Google Scholar]
- 21.Kylanpaa-Back ML, Kemppainen E, Puolakkainen P, Hedstrom J, Haapiainen R, et al. Comparison of urine trypsinogen-2 test strip with serum lipase in the diagnosis of acute pancreatitis. Hepatogastroenterology. 2002;49:1130–4. [PubMed] [Google Scholar]