Abstract
We report the case of a patient presenting with abdominal pain as a result of a thoracic disc prolapse. The literature is reviewed, highlighting the associated morbidity by the often extensive and invasive procedures patients may undergo when a thoracic disc prolapse presents with abdominal pain.
Keywords: Abdominal pain, Thoracic disc prolapse
The incidence of thoracic disc prolapse is reported to be between 0.15% and 4% of all intervertebral disc prolapses.1,2 Due to the rarity of this condition, the presenting symptoms are often attributed to pulmonary, cardiac, gastrointestinal or genito-urinary causes.1 This can lead to unnecessary investigations and procedures. Moreover, a missed diagnosis can potentially have a high morbidity.1
We report the case of a 52-year-old woman, who presented with intermittent abdominal pain; for which she was initially investigated by the general surgeons and urologists. A careful review of her abdominal computed tomography (CT) scan revealed a calcified prolapsed thoracic disc. This is a rare cause of abdominal pain, but one which clinicians must be aware of when forming a differential diagnosis.
Case report
A 52-year-old woman presented to the casualty department with a 4-week history of left loin pain radiating to the left groin. The pain was described as having both sharp, intermittent ‘colicky’ nature, as well as a dull constant component. Initial abdominal examination revealed only mild left iliac fossa tenderness with no other significant findings.
At the time, it was felt that her symptoms might be due to her irritable bowel syndrome and the patient was discharged from the department. She returned within 9 days, complaining of similar persisting symptoms.
She was admitted to the hospital by the surgical team with the provisional differential diagnoses of diverticular disease, renal colic or simple constipation. A plain abdominal radiograph, intravenous uretergram and CT of the abdomen failed to reveal any significant abnormality.
The symptoms failed to resolve with conservative measures and analgesia. She subsequently underwent a laparoscopy, colonoscopy and cystoscopy. No significant pathology was noted during these investigations, except for mild diverticular disease.
Following these investigations a neurosurgical opinion was sought to evaluate the patient for the possibility of an underlying spinal nerve root pathology.
The neurosurgeon reviewed the patient's history and on examination, was unable to elicit any abnormal findings. Magnetic resonance imaging (MRI) of the thoracolumbar spine was performed. This revealed an extradural lesion at the T12 level, with both signal and morphological characteristics that were most in keeping with a calcified disc fragment. The disc had extended inferolaterally into the left lateral recess where it was causing impingement of the left T12 nerve root (Fig. 1). Retrospective review of the CT scan confirmed a calcified lesion emanating from the T11/12 disc and extending inferiorly within the spinal canal, consistent with a calcified disc extrusion (Fig. 2).
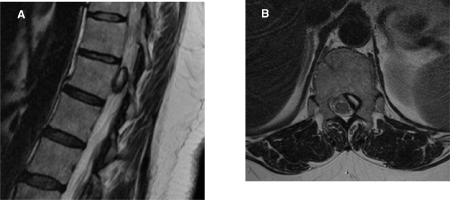
Figure 1.
(A) Sagittal and (B) axial T2 images show an intraspinal lesion lying in an epidural left paracentral location at the upper T12 level. It consists of T2 high signal with a thick rim of T2 low signal. It causes distortion of the theca and potential impingement of the left T12 nerve root. The T11/12 disc is noted to be slightly reduced in height.
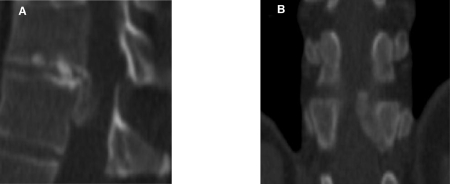
Figure 2.
(A) Sagittal and (B) coronal CT reformats show that the abnormality is contiguous with the T11/12 disc and is consistent with a extruded disc, emanating from the T11/12 level. It shows heavy calcification of its periphery (corresponding to the T2 low signal shown on MRI).
The patient underwent a thoracic hemilaminectomy and microdiscectomy. Intra-operatively, calcified degenerative disc fragments were removed from below and around the affected nerve root, allowing for adequate nerve root decompression.
Postoperatively the patient's pain dissipated immediately and she was discharged 2 days later. At her follow-up appointment, she reported no further complications or recurrence of her symptoms.
Discussion
Symptomatic thoracic disc prolapse is a rare pathology, reported to occur in 1 per million per year,2,3 accounting for 0.15–4% of all symptomatic disc prolapses.1,2 It occurs more commonly in those aged 30–50 years,with a male:female ratio ranging from 1.5:1 to almost equal.1–3 Wood et al.4 reported 37% of the subjects in their study to have asymptomatic thoracic disc prolapse evident onMRI.
Up to 75% of thoracic disc prolapses occur below T8, with T11/12 being the commonest level.1–3 Disc calcification is common and is reported to occur in up to 65% of case.2 As in our case, calcified discs can fragment with migration of these fragments resulting in compression of the nerve roots.
Pain is the commonest symptom associated with thoracic disc prolapse.1,2 Typical thoracic spinal pain can be unilateral, bilateral or radicular.1,2 Its nature can be variable – sharp, cutting, shooting, constant or intermittent.1,2 Pain can also present as non-spinal pain including abdominal pain, testicular or groin pain, upper limb and cardiac pain.1,5–9
Abnormal neurological symptoms are the second most common presentation.1–3 These include, sensory (para esthesia, dysaesthesia and numbness), motor and bladder or bowel disturbance.1–3
There are few case reports describing abdominal pain, resulting from a thoracic disc prolapse.5–9 These indicate that there is no consistent mode of presentation of the pain in its nature, site or duration. In the case we have described, the site (left iliac fossa) and nature of the pain (intermittent or ‘colicky’) has, to our knowledge, not been previously reported.
As demonstrated in the case, many of these patients undergo unnecessary invasive procedures and surgery for suspected intra-abdominal or pelvic pathology, before a thoracic disc prolapse is diagnosed (e.g. endoscopic retrograde cholangiopancreatography,8 laparoscopy,9 laparotomy,5 thoracotomy,5 hysterectomy and salpingio-oopherectomy,5 appendicectomy,6 cholesystectomy7 and Roux-en-Y pancreaticojejunostomy3).
MRI is currently considered to be the most informative method of investigation, though plain X-ray and CT scanning or myelography may also be used to aid diagnosis and treatment.3,4,10
The management of thoracic disc prolapse may be determined by the symptoms. Pain without any neurological abnormalities may initially be amenable to nonoperative management, with non-steroidal analgesia and physiotherapy.2,11 Brown et al.11 reported that over 75% of their case series returned to normal activity with conservative management alone.
In patients with severe intractable pain and neurological symptoms, surgical management is advocated.2,11 Early studies reported the use of laminectomy for excision of thoracic disc to be suboptimal.1–3,8,12 Following these results, alternative safer approaches have been used. These approaches include the posterior and posteriolateral lateral (lateral extracavitary and costotransversectomy) 1,2,10 and the anterior transthoracic (trans- or extrapleural) approaches via thoracotomy or thoracoscopy.1–3,10 Minimally invasive techniques for these approaches are being increasingly employed and actively investigated.2,10 The unilateral interlaminar laminotomy (a variation of the transpedicular approach) was successfully used in the case we have described.12
Conclusions
Symptomatic thoracic disc prolapse presenting with abdominal pain is rare and can easily be misdiagnosed, leading to unnecessary investigations, procedures and morbidity. Clinicians should, therefore, consider thoracic disc prolapse when forming a differential diagnosis and investigating the cause of unexplained abdominal pain.
References
- 1.Arce CA, Dohrmann GJ. Herniated thoracic disks. Neurol Clin. 1985;3:383–92. [PubMed] [Google Scholar]
- 2.Stillerman CB, Chen TC, Couldwell WT, Zhang W, Weiss MH. Experience in the surgical management of 82 symptomatic herniated thoracic discs and review of the literature. J Neurosurg. 1998;88:623–33. doi: 10.3171/jns.1998.88.4.0623. [DOI] [PubMed] [Google Scholar]
- 3.Russell T. Thoracic intervertebral disk protrusion: experience of 67 cases and review of the literature. Br J Neurosurg. 1989;3:153–60. doi: 10.3109/02688698909002790. [DOI] [PubMed] [Google Scholar]
- 4.Wood KB, Garvey TA, Gundry C, Heithoff KB. Magnetic resonance imaging of the thoracic spine. Evaluation of asymptomatic individuals. J Bone Joint Surg Am. 1995;77:1631–8. doi: 10.2106/00004623-199511000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Epstein JA. The syndrome of herniation of lower thoracic intervertebral diskswith nerve root and spinal cord compression: a presentation of four cases with review of the literature, methods of diagnosis and treatment. J Neurosurg. 1954;11:525–38. doi: 10.3171/jns.1954.11.6.0525. [DOI] [PubMed] [Google Scholar]
- 6.Jooma R, Torrens MJ, Veerapen RJ. Spinal disease presenting as acute abdominal pareport of two cases. BMJ. 1983;287:117–8. doi: 10.1136/bmj.287.6385.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rohde RS, Kang JD. Thoracic disc herniation presenting with chronic nausea and abdominal pain. A case report. J Bone Joint Surg Am. 2004;86:379–81. doi: 10.2106/00004623-200402000-00026. [DOI] [PubMed] [Google Scholar]
- 8.Whitcomb DC, Martin SP, Schoen RE, Jho HD. Chronic abdominal pain caused by thoracic disk herniation. Am J Gastroenterol. 1995;90:835–7. [PubMed] [Google Scholar]
- 9.Xiong Y, Lachmann E, Marini S, Nagler W. Thoracic disk herniation presenting as abdominal and pelvic paa case report. Arch PhysMed Rehabil. 2001;82:1142–4. doi: 10.1053/apmr.2001.24897. [DOI] [PubMed] [Google Scholar]
- 10.Sheikh H, Samartzis D, Perez-Cruet M. Techniques for the operative management of thoracic disc herniation: minimally invasive thoracic microdiscectomy. Orthop ClinNorth Am. 2007;38:351–61. doi: 10.1016/j.ocl.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Brown CW, Deffer PA, Jr, Akmakjian J, Donaldson DH, Brugman JL. The natural history of thoracic disc herniation. Spine. 1992;17(Suppl):S97–102. doi: 10.1097/00007632-199206001-00006. [DOI] [PubMed] [Google Scholar]
- 12.Black P. Laminotomy/medial facet approach in the excision of thoracic disc herniation. Neurosurg Focus. 2000;9:e6. doi: 10.3171/foc.2000.9.4.6. [DOI] [PubMed] [Google Scholar]