Abstract
Aims
College students experience high rates of problem and pathological gambling, yet little research has investigated methods for reducing gambling in this population. This study sought to examine the efficacy of brief intervention strategies.
Design
Randomized trial.
Setting
College campuses.
Participants
117 college student problem and pathological gamblers.
Interventions
Students were randomly assigned to: an assessment-only control, 10 minutes of Brief Advice, 1 session of motivational enhancement therapy (MET), or 1 session of MET plus 3 sessions of cognitive-behavioral therapy (CBT). The three interventions were designed to reduce gambling.
Measurements
Gambling was assessed at baseline, week 6, and month 9 using the Addiction Severity Index-Gambling (ASI-G) module, which also assesses days and dollars wagered.
Findings
Compared to the assessment-only condition, those receiving any intervention had significant decreases in ASI-G scores and days and dollars wagered over time. The MET condition significantly decreased ASI-G scores and dollars wagered over time, and it increased the odds of a clinically significant reduction in gambling at the 9-month follow-up relative to the assessment-only condition, even after controlling for baseline indices that could impact outcomes. The Brief Advice and MET+CBT conditions had benefits on some, but not all, indices of gambling. None of the interventions differed significantly from one another.
Conclusions
These results suggest the efficacy of brief interventions for reducing gambling problems in college students.
Keywords: gambling, brief interventions, motivational enhancement therapy, cognitive-behavioral therapy, treatment efficacy
Most college students gamble, with estimates indicating that up to 23% gamble weekly or more1-3. Popular activities include betting on sports, casino games, cards, and the internet4-5. Although most college students who gamble do so without problems, some develop difficulties. Pathological gambling is characterized as “persistent and recurrent maladaptive gambling behavior that disrupts personal, family, or vocational pursuits”6. Problem gambling is sub-diagnostic behavior that causes negative or adverse consequences. Combined prevalence rates of problem and pathological gambling in college students are 3-14%1,3-5,7. Problem and pathological gambling are associated with poor academic performance, heavy alcohol consumption, illicit drug use, nicotine use, and suicide attempts1-3.
Despite the prevalence and adverse consequences of problem and pathological gambling in college students, few studies have examined treatment strategies. Primarily, educational interventions have been evaluated8-12. Although some increased knowledge and decreased irrational beliefs, few impacted gambling behavior directly, and follow-up time frames for assessing behavior change were minimal.
Efficacious interventions exist for other disorders common in college students, such as heavy drinking, and may be applicable to gambling13. They include brief, motivational and cognitive-behavioral interventions. Brief Advice is more effective than no treatment, and often as effective as extended treatment, in reducing heavy drinking in college students14,15, and its simple directive nature may encourage behavioral change. A recent study in adult problem and pathological gamblers found that a 15-minute Brief Advice condition was more efficacious than an assessment-only condition in reducing gambling16.
Motivational Enhancement Therapy (MET) is efficacious in reducing heavy drinking in college students17,18. Based upon the trans-theoretical model of change, MET seeks to increase motivation to change19. In a trial for adult problem gamblers, MET delivered over the telephone in combination with a self-help workbook led to greater reductions in gambling than a wait-list control condition20. The workbook used Cognitive-Behavioral Therapy (CBT), which assumes cognitive restructuring and behavior modification can alter problem behaviors. CBT may be appropriate because students with greater gambling problems evidence more irrational beliefs21-24, and are more likely to use ineffective coping strategies25,26.
In this study, we evaluated each of these three interventions in problem and pathological gambling college students. The Brief Advice condition provided information about prevalence rates, personalized feedback about gambling, and simple strategies for decreasing it. The second condition was a single session of MET, in which students discussed their gambling and how it fit in with their life goals. The third condition consisted of one MET session followed by 3 sessions of CBT. In an initial omnibus analysis, we evaluated the efficacy of the combined interventions compared to an assessment-only condition, with the hypothesis that receiving any intervention would improve outcomes relative to assessment only. If the omnibus analysis was significant, we planned to investigate the efficacy of each individual intervention versus assessment only. In exploratory analyses, we compared the three active interventions to assess if any was particularly efficacious in reducing gambling. Prognostic factors associated with clinically significant reductions in gambling were also investigated, including pretreatment severity of gambling problems and alcohol use, which is linked to problem and pathological gambling27.
Method
Participants
Participants were recruited via screening efforts and flyers posted at college campuses, between the springs of 2005 and 2006. Recruitment was conducted primarily at two public universities, and flyers were also posted at four other campuses. A screen consisting of demographics, recent gambling activities, and the South Oaks Gambling Screen (SOGS)28 was administered in university common areas (e.g., student union), classrooms with instructor permission (no extra credit or course credit was provided, and screen completion was voluntary), or over the phone for those who called in response to flyers. Students who were ≥18 years, responded affirmatively to ≥3 SOGS items, and spent ≥$100 in total wagering and gambled on ≥4 days in the past 2 months were invited to participate in the full evaluation. Gambling frequency/intensity criteria were included to ensure study participants had levels of gambling that could decrease during the study period, and prior research revealed these levels of gambling were associated with problem gambling4,5.
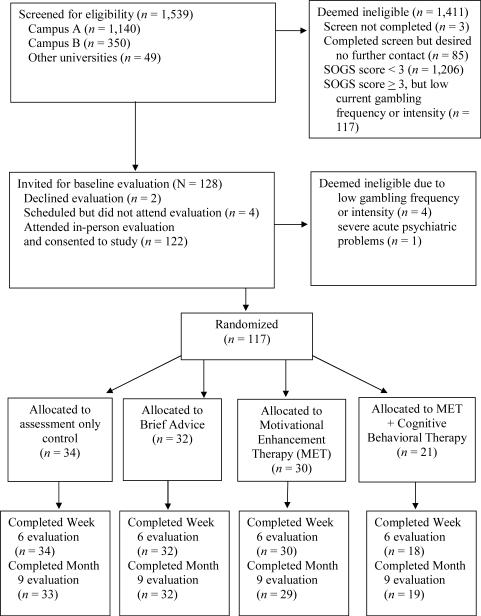
As approved by the Universities' Institutional Review Boards, students initially provided assent for screening. Those who appeared to meet inclusion criteria were invited to an in-person evaluation. After providing written informed consent, assessments were administered and exclusion criteria evaluated. The only exclusion criteria were past-month suicidal intentions, psychotic symptoms, or interest in receiving more intensive gambling treatment than provided in the study as an assessment-only condition was utilized; excluded individuals were provided treatment referrals. Figure 1 shows flow of participants, and 117 students were randomized. This sample size is sufficient to detect, with >80% power, medium effect sizes between the assessment-only condition and the combined group of participants receiving any intervention. A sample size of 25-30 per condition is also adequate to detect medium to large effect sizes between each intervention and the assessment-only condition29. Analyses comparing the brief interventions to one another were considered exploratory in nature, as effect sizes are generally smaller when examining differences between active interventions.
Figure 1.
Flow of participants through study protocol. Please note that the method of screening (in classrooms versus in response to flyers) was not recorded so this information cannot be separated out.
Assessments
Assessments were administered at baseline and 6 weeks (to allow sufficient time for completion of 4 weekly therapy sessions and detect acute treatment effects) and 9 months later (to investigate longer-term effects). Students received $20 in gift certificates for completing the in-person baseline evaluation, which took about 1.5 hours, and $15 for each follow-up, which took 20 minutes and was done via phone. Typically, research therapists conducting the baseline evaluation provided interventions (if so assigned). Seven research assistants (some of whom also were therapists) shared responsibilities for follow-ups, and were unaware of treatment assignment. Each research assistant was trained by the same individual before study initiation and monitored monthly during the study period for consistent administration of assessment instruments. Follow-up rates exceeded 96% at each post-baseline evaluation (see Figure 1).
The SOGS assessed past-month gambling problems at baseline, week 6 and month 9, with scores ≥5 indicating probable pathological gambling, and scores ≥3 indicating problem gambling. SOGS scores are highly correlated with DSM criteria and measures of gambling severity30,31. Intervention studies utilize SOGS scores as outcome measures32,33, and shortening the timeframe of assessment to 3 months does not affect psychometric properties34. In this sample, Cronbach's alpha was 0.73-0.78 across administrations, and use of a one-month time frame was necessary to assess behaviors in the relatively short period between baseline and the 6-week evaluation.
The National Opinion Research Center DSM-IV Screen for Gambling Problems (NODS), administered at baseline only, assessed the 10 lifetime pathological gambling criteria. The NODS identified 95% of treatment-seeking gamblers as pathological, and test-retest reliability is 0.9935. In our sample, Cronbach's alpha was 0.83.
The Addiction Severity Index-Gambling section (ASI-G)37-39 evaluated gambling problems at baseline and follow-ups. It is scored like the drug section of the ASI40, with a range of 0-1, and higher scores indicate more severe problems. The ASI-G has good internal consistency, test-retest reliability and validity in assessing gambling problems and changes over time37-39. Cronbach's alpha in this sample was adequate--0.7141. At month 9, the correlation between past-month SOGS and ASI-G scores was 0.74, p<.001.
The TimeLine Followback (TLFB)42 was administered at baseline only to assess days of alcohol and drug use and types of gambling, gambling days and net expenditures (not including monies won which are reinvested) in the past month. The TLFB provides a reliable and valid indicator of gambling43. In this sample, correlations between days and dollars wagered as assessed by the TLFB and similar items on the ASI-G at baseline were 0.86 and 0.88 (p's<.001).
The Treatment Service Review (TSR)44 evaluated services received, including professional gambling treatment and self-help (e.g., Gamblers Anonymous). Follow-up versions assessed services since the past evaluation to determine access of non-study services.
Randomization to interventions
Participants selected from envelopes containing slips of paper indicating the group to which they were randomly assigned. Staff prepared more envelopes than participants were randomized so sample sizes are not equal across groups.
The interventions were provided at no cost, but participation was voluntary and no compensation was provided for attendance. Hence, some participants attended only 1 of 4 sessions, and only about one-third came to all sessions. After the intervention (or a description of follow-up procedures for those assigned to the assessment-only condition), participants were instructed to contact research staff if gambling intensified or they desired additional gambling treatment, although none did so. No study-related adverse events were noted, but one student (assigned to MET+CBT) withdrew from the study as he did not want to complete follow-ups.
Assessment-only control
After the baseline evaluation, researchers informed students assigned to this condition they would be re-contacted in 6 weeks and 9 months for follow-ups.
Brief Advice
Participants assigned to this condition met with a therapist immediately after the evaluation for 10-15 minutes. Using a one-page handout, modified from Petry45, the therapist described the student's level of gambling in relation to the general college population, outlined risk factors, and provided four suggestions to curtail development of significant gambling problems. Suggestions included limiting amount of money spent gambling, reducing amount of time and days gambling, not viewing gambling as a way of making money, and spending time doing other things.
MET
Students in this condition received a 50-minute individual MET session after the evaluation. Therapists provided personalized feedback about the student's gambling. Next, they explored positive and negative consequences of gambling and discussed how gambling fit within their life goals and values. They then completed a change plan worksheet.
MET+CBT
These participants met with a therapist after the baseline evaluation for an MET session as above. They were encouraged to return for three weekly individual sessions of CBT that addressed: (1) identifying internal (mood) and external (e.g., peer pressure) gambling triggers, (2) coping with internal triggers, and (3) coping with external triggers. CBT handouts were modified from Petry45 to emphasize reductions, rather than abstinence, as the goal.
Therapists
Six therapists (1 Bachelors level, 2 Masters level, 2 clinical psychology doctoral students, and 1 Ph.D. psychologist) delivered each of the three interventions. They received didactic training and close supervision of at least one case. Ongoing supervision consisted of review of therapy notes and audiotapes and case discussion. Using a modification of the Yale Adherence Competence Scale46, five independent therapists rated 49 randomly selected audiotapes for Brief Advice, MET, and CBT items on a 7-point Likert scale (1=none/poor, 3=some/adequate, 7=extensive/exceptional). One of four Brief Advice items rated was: “To what extent did the therapist provide concrete recommendations for reducing gambling?” An example of one of three MET items was: “To what extent were the therapist's questions open-ended and reflective?” One of the three CBT items was, “To what extent did the therapist attempt to teach, model, or rehearse specific coping skills?” Inter-rater reliability was 0.94.
Means and standard deviations of Brief Advice items were 6.4±0.5 (reflecting average rankings of “good/quite a bit”) in the Brief Advice sessions, and ratings on MET and CBT items were 1.3±0.3 and 1.0±0.0, respectively (reflecting average ratings of “none/poor”). In MET sessions (including the MET session of the MET+CBT condition), adherence to MET items was rated 5.4±0.9, versus 1.0±0.1 for Brief Advice items and 1.1±0.1 for CBT items. CBT sessions were rated 4.2±1.1 on CBT items, 2.4±0.7 on MET items, and 1.0±0.0 on Brief Advice items. Thus, therapies were distinguishable (p's<.05).
Data analysis
Analysis of variance and Chi-square tests examined differences across groups at baseline. Dollars wagered were log transformed and days gambled square root transformed to normalize data before analyses.
Using intent-to-treat analyses including all participants randomized, the primary analytic strategy was hierarchical linear models (HLM)47, which takes into account all data available and models slopes based upon actual time of assessments. The primary outcome was a priori selected as ASI-G scores. To provide a more intuitive account of gambling, days and dollars wagered in the prior month, taken from the ASI-G, were evaluated as secondary outcomes. The initial omnibus analysis compared those receiving any intervention (Brief Advice, MET, or MET+CBT) to those receiving assessment-only, and contrast by time analyses examined differences over time. When significant, three additional contrasts were conducted, each comparing an active intervention to the assessment-only condition. Contrast weights of 1 were assigned to the interventions and 0 to the control condition. Finally, each active intervention was contrasted with the others in exploratory analyses to ascertain if any appeared more efficacious.
As an indicator of clinically significant change48, logistic regressions evaluated predictors of “substantial improvement,” defined as post-treatment dollars wagered <10.5% of monthly income at month 9. (No students substantially increased gambling or gambling problems relative to baseline). This classification was based on literature showing that college students who gamble at this level are unlikely to be classified as problem/pathological gamblers49, and indeed, 92.7% of students who gambled below this level were classified as non-problem gamblers by SOGS scores <2 at month 9. Gender, baseline SOGS scores, and days drank alcohol in the past month were entered in Step 1. All variables were continuous with the exception of gender. In Step 2, condition was entered as a categorical variable, with the control condition indicated as the reference category, to determine if the interventions increased odds of substantial improvement relative to assessment-only. The significance level was p<.05, two-tailed. All analyses other than HLM (HLM for Windows, version 5.5) were conducted using SPSS for Windows (version 15).
Results
Sample description and treatment participation
Baseline data appear in Table 1. Groups did not differ significantly on any demographic variables or measures of gambling.
Table 1.
Demographic and Baseline Characteristics.
| Control | Brief Advice | MET | MET + CBT | Statistic (df) | P value | |
|---|---|---|---|---|---|---|
| n | 34 | 32 | 30 | 21 | ||
| Age, mean (SD) | 20.5 (2.0) | 20.2 (1.9) | 20.5 (1.4) | 20.1 (1.4) | F(3,116) = .27 | .85 |
| Male, No. (%) | 29 (85.3) | 25 (78.1) | 26 (86.7) | 19 (90.5) | χ2(3) = 1.70 | .64 |
| Ethnicity, No. (%) | χ2(6) = 6.86 | .33 | ||||
| European American | 29 (85.3) | 25 (78.1) | 25 (83.3) | 21 (100) | ||
| Asian/Pacific Islander | 4 (11.8) | 4 (12.5) | 2 (6.7) | 0 (0.0) | ||
| Other | 1 (2.9) | 3 (9.4) | 3 (10.0) | 0 (0.0) | ||
| College campus, No. (%) | χ2(6) = 1.10 | .98 | ||||
| Campus A | 19 (55.9) | 18 (56.3) | 16 (53.3) | 14 (66.7) | ||
| Campus B | 8 (23.5) | 7 (21.9) | 7 (23.3) | 4 (19.1) | ||
| Other campuses | 7 (20.6) | 7(21.9) | 7 (23.3) | 3 (14.3) | ||
| Yearly Income, mean (SD), $ | 7,122 (9,501) | 5,981 (4,983) | 10,298 (11,912) | 8,761 (9,876) | F(3,116) = 1.25 | .29 |
| Years of education | 14.5 (2.0) | 14.1 (1.5) | 14.4 (1.2) | 13.7 (1.2) | F(3,116) = 1.56 | .20 |
| Cumulative Grade Point Average | 3.1 (.7) | 3.0 (.6) | 3.1 (.4) | 3.1 (.5) | F(3,46) = 0.16 | .92 |
| Days drank alcohol in past month | 8.2 (7.9) | 8.1 (6.6) | 9.9 (7.1) | 8.7 (8.0) | F(3,116) = 0.37 | .78 |
| Used marijuana in past month, No. (%) | 11 (32.4) | 6 (18.8) | 9 (30.0) | 7 (33.3) | χ2(3) = 2.02 | .57 |
| Used other illicit drug in past month, No.(%) | 4 (11.8) | 5 (15.6) | 10 (33.3) | 5 (23.8) | χ2(3) = 5.23 | .16 |
| Age started gambling | 14.4 (3.3) | 15.5 (3.7) | 13.8 (3.0) | 14.3 (3.8) | F(3,116) = 1.33 | .27 |
| NODS Lifetime Score | 4.0 (2.2) | 3.6 (2.5) | 3.5 (2.1) | 4.7 (2.6) | F(3,116) = 1.32 | .27 |
| NODS Pathological Gambler, No. (%) | 13 (38.2) | 11 (34.4) | 10 (33.3) | 11 (52.4) | χ2(3) = 2.28 | .52 |
| SOGS Past-Month Score | 4.3 (3.3) | 3.9 (2.9) | 4.2 (3.3) | 4.9 (4.4) | F(3,116) = .37 | .78 |
| Bet >10.5% income in past month, No. (%) | 33 (97.1) | 31 (96.9) | 29 (96.7) | 20 (95.2) | χ2(3) = 0.15 | .99 |
| Preferred Gambling Activity, No. (%) | χ2 (12) = 10.14 | .60 | ||||
| Cards/Poker | 21 (61.8) | 17 (53.1) | 13 (43.3) | 11 (52.4) | ||
| Sports | 1 (2.9) | 5 (15.6) | 5 (16.7) | 4 (19.1) | ||
| Scratch tickets/Lottery | 3 (8.8) | 2 (6.3) | 4 (13.3) | 3 (14.3) | ||
| Internet | 5 (14.7) | 3 (9.4) | 2 (6.7) | 0 (0.0) | ||
| Other | 4 (11.8) | 5 (15.6) | 6 (20.0) | 3 (14.3) |
Note. MET = Motivational Enhancement Therapy. MET + CBT = Motivational Enhancement Therapy plus Cognitive-Behavioral Therapy. NODS = National Opinion Research Center DSM-IV Screen. SOGS = South Oaks Gambling Screen.
All participants assigned to Brief Advice and MET received their assigned intervention. One participant (4.8%) assigned to MET+CBT scheduled the MET session for another day and failed to attend. Only 7 participants (33.3%) attended all four sessions, and 3 (14.3%) came to three, 2 (9.5%) to two, and 8 (38.1%) to only one (the initial MET session).
No randomized students requested additional gambling treatment. TSR data revealed only 1 participant (from the assessment-only condition) received other non-study gambling treatment. Because this level of non-study gambling treatment was low (<1%), this participant was retained in all analyses.
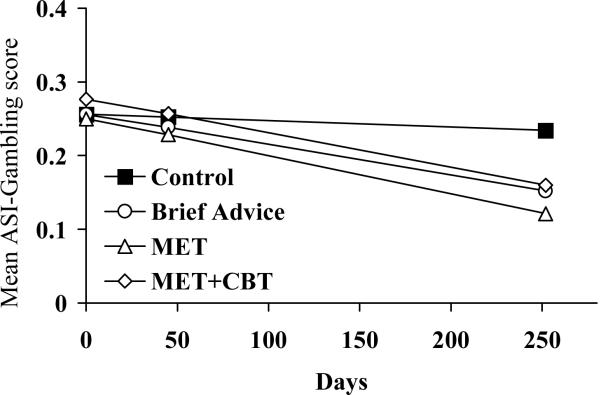
Effects of interventions on gambling
Table 2 shows gambling variables over time in the three conditions. For ASI-G scores, the group-by-time interaction effect was significant for the contrast of any treatment versus no treatment, t(115) = 2.28, p<.05, and for each of the three interventions compared to the assessment-only condition (Table 2). Figure 2 shows that although ASI-G scores remained generally unchanged over time in the assessment-only condition, they decreased in all three of the active interventions. There were no significant differences between active interventions with respect to changes in ASI-G scores over time (all p's>.35).
Table 2.
Gambling outcomes and results from random regression models analyses (n=117)
| Outcome measures, raw means (SD) | Baseline through month 9, T (df), p-values | ||||
|---|---|---|---|---|---|
| Variable | Baseline N=117 | Week 6 N=114 | Month 9 N=113 | Time | Group × Time |
| ASI-Gambling | |||||
| Control | 0.30 (0.12) | 0.21 (0.13) | 0.24 (0.19) | ||
| Brief Advice | 0.30 (0.15) | 0.19 (0.14) | 0.16 (0.12) | -0.67, p=.51 | -1.92 (64), p<.05 |
| MET | 0.30 (0.15) | 0.17 (0.12) | 0.13 (0.13) | -0.70, p=.49 | -2.54 (62), p=.01 |
| MET+CBT | 0.33 (0.11) | 0.18 (0.10) | 0.17 (0.15) | -0.76, p=.45 | -2.10 (53), p<.05 |
| Days gambled | |||||
| Control | 14.2 (8.2) | 9.9 (8.3) | 10.3 (10.0) | ||
| Brief Advice | 13.3 (7.7) | 8.0 (7.3) | 5.9 (6.7) | -2.03, p<.05 | -1.00 (64), p=.32 |
| MET | 14.1 (8.9) | 7.4 (7.1) | 5.5 (7.5) | -2.03, p<.05 | -1.75 (62), p=.08 |
| MET+CBT | 15.7 (8.7) | 8.9 (8.7) | 6.1 (7.8) | -2.08, p<.05 | -1.88 (53), p=.06 |
| Dollars gambled* | |||||
| Control | 275 (672) | 100 (528) | 150 (628) | ||
| Brief Advice | 158 (298) | 80 (223) | 65 (195) | -1.42, p=.15 | -0.96 (64), p=.34 |
| MET | 250 (605) | 100 (365) | 14 (235) | -1.45, p=.15 | -2.11 (62), p<.05 |
| MET+CBT | 192 (350) | 40 (180) | 50 (753) | -1.42, p=.16 | -0.20 (53), p=.85 |
Note. ASI = Addiction Severity Index. MET = Motivational Enhancement Therapy. MET + CBT = Motivational Enhancement Therapy plus Cognitive-Behavioral Therapy.
Values represent means and standard deviations unless otherwise noted.
Values represent medians and interquartile ranges and were log-transformed prior to analyses.
Figure 2.
Addiction Severity Index (ASI) Gambling scores by days since randomization to a treatment condition. Values represent past-month measures and are estimates from random effects regression analyses, and as such do not always match raw means presented in Table 2. MET = Motivational Enhancement Therapy; MET+CBT = Motivational Enhancement Therapy plus Cognitive-Behavioral.
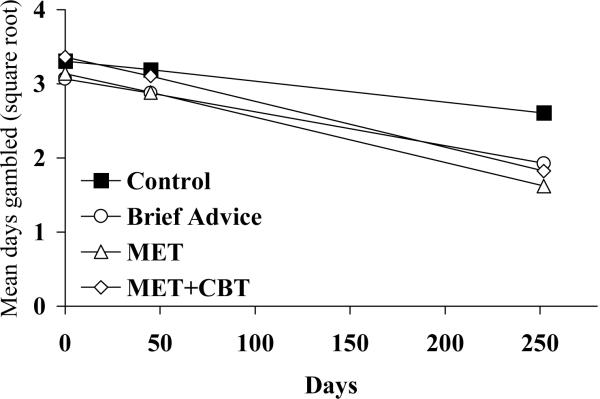
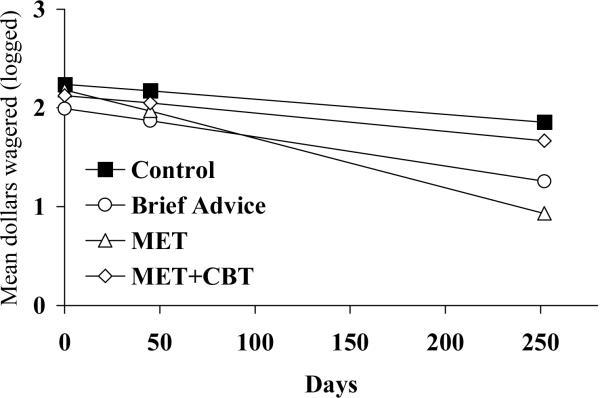
Table 2 also shows two supplementary indices of gambling. In terms of days gambled, time effects were significant over the 9-month study period, showing a general decline in days gambling (Figure 3). The omnibus analysis comparing any intervention to the assessment only condition revealed a significant treatment-by-time effect, t(115) = 2.24, p<.04, but none of the three interventions differed significantly from the assessment-only condition in terms of days gambled. With respect to dollars wagered, again, the omnibus analysis comparing any treatment to no treatment found a significant treatment-by-time effect, t(115) = 2.22, p<.05. Only the MET condition showed a significantly greater reduction in dollars wagered over time compared to the control condition (Table 2; Figure 4). None of the active interventions differed significantly from one another with respect to days or dollars gambled over time (all p's>.28).
Figure 3.
Days wagered per month by days since randomization to a treatment condition. Values plotted are square root transformed means. Values represent past-month measures and are estimates from random effects regression analyses, and as such do not always match raw means presented in Table 2. MET = Motivational Enhancement Therapy; MET+CBT = Motivational Enhancement Therapy plus Cognitive-Behavioral.
Figure 4.
Dollars wagered per month by days since randomization to a treatment condition. Values plotted are log transformed means. Values represent past-month measures and are estimates from random effects regression analyses, and as such do not always match raw means presented in Table 2. MET = Motivational Enhancement Therapy; MET+CBT = Motivational Enhancement Therapy plus Cognitive-Behavioral.
Clinically significant improvements
At month 9, proportions (and n) of students classified as “substantially improved” based on wagering <10.5% of income were 36.4% (n = 12 of 33), 46.9% (n = 15 of 32), 62.1% (n = 18 of 29), and 52.6% (n = 10 of 19) in the assessment only, Brief Advice, MET, and MET+CBT conditions, respectively. Table 3 shows results from the logistic regression examining variables putatively associated with “substantially improved” status at month 9. Step 1, with baseline characteristics included, was not significant, χ2(df=3, n=113) = 6.98, p = .07, but the inclusion of group was significant, χ2(df=6, n=113) = 12.54, p<.05. Relative to the assessment-only group, the MET group had a significant positive relationship, with an odds ratio (OR) of 3.41, indicating that those receiving MET had over a 3-fold increased chance of being classified as “substantially improved” relative to those in the assessment-only condition. Neither the Brief Advice nor MET+CBT groups significantly altered odds of substantial improvement.
Table 3.
Logistic regression analysis predicting substantial reductions in gambling at month 9.
| Beta (Standard error) | Wald | Significance | Odds ratio (95% Confidence interval) | |
|---|---|---|---|---|
| Step 1 | ||||
| Female gender | 0.71 (0.58) | 1.52 | 0.22 | 2.04 (0.66-6.36) |
| Baseline SOGS | -0.11 (0.07) | 2.85 | 0.09 | 0.89 (0.79-1.02) |
| Days drank alcohol in past month | -0.05 (0.03) | 3.20 | 0.07 | 0.95 (0.89-1.01) |
| Step 2 - Treatment group | ||||
| Brief Advice | 0.39 (0.53) | 0.54 | 0.46 | 1.47 (0.52-4.11) |
| MET | 1.23 (0.56) | 4.89 | p<0.05 | 3.41 (1.15-10.11) |
| MET+CBT | 0.79 (0.62) | 1.64 | 0.20 | 2.20 (0.66-7.36) |
Note. SOGS = South Oaks Gambling Screen; ASI = Addiction Severity Index; MET = Motivational Enhancement Therapy; MET+CBT = Motivational Enhancement Therapy plus Cognitive-Behavioral.
Discussion
In this study, participants assigned to any brief intervention reduced gambling to a greater extent than those assigned to an assessment-only control. In terms of specific interventions, MET had consistently beneficial effects relative to assessment-only. The emphasis of MET on personal autonomy may be particularly appealing considering the social development of college-aged students.
The Brief Advice and MET+CBT interventions showed significant effects on some outcome measures. In another study using a similar design, strong and consistent benefits of Brief Advice were noted16. In that study, many participants were recruited from substance abuse treatment programs. Demographic characteristics varied and severity of baseline gambling problems was higher in that sample, which may have influenced treatment response.
MET+CBT was associated with some benefits in the present study. The somewhat mixed findings with this intervention may relate to the low proportion of participants who attended CBT sessions, with only 33% attending all three sessions. Consistent with an intent-to-treat approach, all participants assigned to the condition were included in the analyses, as providing an effective intervention may not be useful if few individuals engage in it. Limiting analyses to only attendees did not substantially alter results (data not shown, available on request), probably because few participants remained in the analyses when non-completers were excluded, and power to detect between-group differences was limited. Further, those who substantially reduce gambling after the baseline assessment or the MET session may have little desire to receive additional sessions. In any case, the data fail to support benefits of this more extended intervention relative to briefer ones, and no significant effects, or even trends, emerged between the active interventions.
Longitudinal studies of youth demonstrate that gambling problems wax and wane over time, even without treatment50-52. However, those identified as problem gamblers in longitudinal surveys are more likely than non-problem gamblers to report some degree of gambling difficulties at later time points. Thus, providing a brief intervention that reduces gambling even in the short-term may assist some students in overcoming their gambling problems and preventing long-term adverse effects.
Among students particularly, gambling patterns may vary throughout the academic year, but participants in this study were recruited and randomized at all times so any semester-related effects on gambling occurred equally across groups. Use of outcome measures assessing relatively brief time spans (one month) may obscure the ability to evaluate sustained changes, but again randomization occurring throughout the academic year likely minimized any effect that assessment of short timeframes had on outcomes. Nevertheless, future studies ought to include more global and long-term measures of gambling behavior. A potential limitation of this study is that it evaluated gambling over only a 9-month period. Either relapses or further reductions in gambling may have occurred later, and additional benefits of MET+CBT may have been uncovered if gambling were measured over longer time frames.
Another consideration is that duration of contact time differed across conditions. However, this design was planned, and all interventions were modeled after those with empirical and theoretical support. In addition, there is debate regarding gambling outcome measures53,54. Several were utilized in this study, and most showed concordance. The present study did not include independent confirmation of gambling behaviors, but other studies found high agreement between gamblers and collaterals33,39,55. If biases are noted, they are in the direction of participants reporting more gambling than collaterals are aware. Although these self-report data are thought to be reliable and valid, future studies may include objective or independent reports.
Finally, these students were not seeking treatment, and results of this study may not generalize to those specifically desiring gambling treatment. Few students assigned to the 4-session intervention attended all the sessions, and the sample size in this condition was low, perhaps further obscuring ability to detect between-group differences. The study was not powered to detect differences in efficacy between active interventions, but no clear pattern emerged with respect to relative efficacy among the interventions, suggesting that any of these treatments may be useful for reducing gambling in college students.
Many therapists provided interventions, thereby potentially reducing impact of particular therapists on outcomes. However, the use of multiple therapists potentially increases variability of outcomes, and evaluation of therapist by condition analyses were not possible due to the large number of therapists and few participants per condition per therapist.
Strengths of this study include the very high follow-up rates and application of intent-to-treat analyses. Employing few exclusion criteria enhances generalization of the findings. Participants were not actively seeking treatment for gambling, making this sample similar to the majority of problem and pathological gambling college students.
Including both problem and pathological gamblers is a strength with respect to external validity, but also could be interpreted as a weakness as more intensive therapies may be necessary for those with severe gambling problems. Future studies should examine more intensive interventions for students with more severe gambling problems, but challenges remain with respect to engagement as few attended the 4-session intervention. Participants were not seeking gambling treatment, thereby perhaps leading to poor adherence in the most intensive intervention.
Results from this study show that identifying problem gamblers and administering very brief intervention strategies such as one MET session can assist in substantially decreasing gambling for nine months in almost two-thirds of college student problem and pathological gamblers. Given the lack of efficacious interventions for this population, these results are noteworthy. As awareness of gambling problems on college campuses grows, more counselors, administrators and professors are expressing interest in learning about this disorder56, and these data provide support for brief interventions in this population.
Footnotes
Clinical trial registration #: NCT00183599
The authors declare no conflicts of interest.
References
- 1.Engwall D, Hunter R, Steinberg M. Gambling and other risk behaviors on university campuses. J Am Coll Health. 2004;52:245–55. doi: 10.3200/JACH.52.6.245-256. [DOI] [PubMed] [Google Scholar]
- 2.LaBrie RA, Shaffer HJ, LaPlante DA, Wechsler H. Correlates of college student gambling in the United States. J Am Coll Health. 2003;52:53–62. doi: 10.1080/07448480309595725. [DOI] [PubMed] [Google Scholar]
- 3.Winters KC, Bengston P, Dorr D, Stinchfield R. Prevalence and risk factors among college students. Psychol Addict Behav. 1998;12:127–35. [Google Scholar]
- 4.Weinstock J, Whelan JP, Meyers AW, Watson JM. Gambling behavior of student athletes and a student cohort: What are the Odds? J Gambl Stud. 2007;23:13–24. doi: 10.1007/s10899-006-9043-3. [DOI] [PubMed] [Google Scholar]
- 5.Petry NM, Weinstock J. Internet gambling is common in college students and is associated with poor health. Am J Addict. 2007;16:325–30. doi: 10.1080/10550490701525673. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- 7.Shaffer HJ, Hall MN, Vander Bilt J. Estimating the prevalence of disordered gambling behavior in the United States and Canada: A research synthesis. Am J Public Health. 1999;89:1369–76. doi: 10.2105/ajph.89.9.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doiron JP, Nicki RM. Prevention of pathological gambling: a randomized controlled trial. Cogn Behav Ther. 2007;36:74–84. doi: 10.1080/16506070601092966. [DOI] [PubMed] [Google Scholar]
- 9.Floyd K, Whelan JP, Meyers AW. Use of warning messages to modify gambling beliefs and behavior in a laboratory investigation. Psychol Addict Behav. 2006;20:69–74. doi: 10.1037/0893-164X.20.1.69. [DOI] [PubMed] [Google Scholar]
- 10.Steenbergh TA, Whelan JP, Meyers AW, May RK, Floyd K. Impact of warning and brief intervention messages on knowledge of gambling risk, irrational beliefs and behaviour. Journal of International Gambling Studies. 2004;4:3–16. [Google Scholar]
- 11.Takushi RY, Neighbors C, Larimer ME, Lostutter TW, Cronce JM, Marlatt GA. Indicated prevention of problem gambling among college students. J Gambl Stud. 2004;20:83–93. doi: 10.1023/B:JOGS.0000016705.58903.8f. [DOI] [PubMed] [Google Scholar]
- 12.Williams RJ, Connolly D. Does learning about mathematics of gambling change gambling behavior? Psychol Addict Behav. 2006;20:62–8. doi: 10.1037/0893-164X.20.1.62. [DOI] [PubMed] [Google Scholar]
- 13.Larimer ME, Cronce JM. Identification, prevention, and treatment: A review of individual-focused strategies to reduce problematic alcohol consumption by college students. J Stud Alcohol. 2002;14S:148–63. doi: 10.15288/jsas.2002.s14.148. [DOI] [PubMed] [Google Scholar]
- 14.Carey KB, Scott-Sheldon LAJ, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addict Behav. 2007;32:2469–94. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Larimer ME, Cronce JM. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999-2006. Addict Behav. 2007;32:2439–68. doi: 10.1016/j.addbeh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 16.Petry NM, Weinstock J, Ledgerwood DM, Morasco B. A randomized trial of brief interventions for problem and pathological gamblers. J Consult Clin Psychol. 2008;76:318–28. doi: 10.1037/0022-006X.76.2.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baer JS, Kivlahan DR, Blume AW, McKnight P, Marlatt GA. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. Am J Public Health. 2001;91:1310–16. doi: 10.2105/ajph.91.8.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. J Consult Clin Psychol. 2000;68:728–33. [PubMed] [Google Scholar]
- 19.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. Guilford; New York: 2002. [Google Scholar]
- 20.Hodgins DC, Currie SR, el-Guebaly N. Motivational enhancement and self-help treatments for problem gambling. J Consult Clin Psychol. 2001;69:50–7. doi: 10.1037//0022-006x.69.1.50. [DOI] [PubMed] [Google Scholar]
- 21.Baboushkin HR, Hardoon KK, Derevensky JL, Gupta R. Underlying cognitions in gambling behavior among university students. Journal of Applied Social Psychology. 2001;31:1409–30. [Google Scholar]
- 22.Moore SM, Ohtsuka K. Beliefs about control over gambling among young people, and their relation to problem gambling. Psychol Addict Behav. 1999;13:339–47. [Google Scholar]
- 23.Steenbergh TA, Meyers AW, May RK, Whelan JP. Development and validation of the gamblers' beliefs questionnaire. Psychol Addict Behav. 2002;16:143–9. [PubMed] [Google Scholar]
- 24.Wohl MJA, Young MM, Hart KE. Untreated young gamblers with game-specific problems: Self-concept involving luck, gambling ecology and delay in seeking professional treatment. Addiction Research and Theory. 2005;13:445–59. [Google Scholar]
- 25.Lightsey OR, Hulsey CD. Impulsivity, coping, stress, and problem gambling among university students. Journal of Counseling Psychology. 2002;49:202–11. [Google Scholar]
- 26.Nower L, Derevensky JL, Gupta R. The relationship of impulsivity, sensation seeking, coping, and substance use in youth gamblers. Psychol Addict Behav. 2004;18:49–55. doi: 10.1037/0893-164X.18.1.49. [DOI] [PubMed] [Google Scholar]
- 27.Petry NM, Stintson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66:564–74. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- 28.Lesieur HR, Blume SB. The South Oaks Gambling Screen (SOGS): A new instrument for the identification of pathological gamblers. Am J Psychiatry. 1987;144:1184–88. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- 29.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- 30.Stinchfield R. Reliability, validity, and classification accuracy of the South Oaks Gambling Screen (SOGS) Addict Behav. 2002;27:1–19. doi: 10.1016/s0306-4603(00)00158-1. [DOI] [PubMed] [Google Scholar]
- 31.Weinstock J, Whelan J, Meyers AW, Mccausland C. The performance of two pathological gambling screens in college students. Assessment. 2007;14:399–407. doi: 10.1177/1073191107305273. [DOI] [PubMed] [Google Scholar]
- 32.Hodgins DC, Currie SR, el-Guebaly N, Peden N. Brief motivational treatment for problem gambling: A 24-month follow-up. Psycho Addict Behav. 2004;18:293–96. doi: 10.1037/0893-164X.18.3.293. [DOI] [PubMed] [Google Scholar]
- 33.Petry NM, Ammerman Y, Bohl J, Doersch A, Gay H, Kadden R, et al. Cognitive-behavioral therapy for pathological gamblers. J Consult Clin Psychol. 2006;74:555–67. doi: 10.1037/0022-006X.74.3.555. [DOI] [PubMed] [Google Scholar]
- 34.Wulfert E, Hartley J, Lee N, Wang M, Franco C, Sodano R. Gambling screens: Does shortening the time frame affect their psychometric properties? J Gambl Stud. 2005;21:521–36. doi: 10.1007/s10899-005-5561-7. [DOI] [PubMed] [Google Scholar]
- 35.Gerstein DR, Volberg RA, Toce MT, Harwood H, Johnson RA, Buie T, et al. Gambling Impact and Behavior Study: Report to the National Gambling Impact Study Commission. National Opinion Research Center; Chicago, IL: 1999. [Google Scholar]
- 36.Hodgins DC. Using the NORC DSM screen for gambling problems as an outcome measure of pathological gambling: Psychometric evaluation. Addict Behav. 2004;29:1685–90. doi: 10.1016/j.addbeh.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 37.Lesieur HR, Blume SB. Evaluation of patients treated for pathological gambling in a combined alcohol, substance abuse and pathological gambling treatment unit using the Addiction Severity Index. Addiction. 1991;86:1017–28. doi: 10.1111/j.1360-0443.1991.tb01863.x. [DOI] [PubMed] [Google Scholar]
- 38.Petry NM. Validity of the Addiction Severity Index in assessing gambling problems. J Nerv Ment Dis. 2003;191:399–407. doi: 10.1097/01.NMD.0000071589.20829.DB. [DOI] [PubMed] [Google Scholar]
- 39.Petry NM. Psychometric properties of the Addiction Severity Index in pathological gamblers. Am J Addict. 2007;16:272–82. doi: 10.1080/10550490701389849. [DOI] [PubMed] [Google Scholar]
- 40.McLellan AT, Luborsky L, Cacciola J, Griffith J, McGahan P, O'Brien CP. Guide to the Addiction Severity Index: Background, Administration, and Field Testing Results. 1988. pp. 88–1419. U.S. DHHS Publication No. (ADM) [Google Scholar]
- 41.Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. McGraw-Hill; New York: 1994. [Google Scholar]
- 42.Sobell LC, Sobell MB. Timeline Followback User's Guide: A Calendar Method for Assessing Alcohol and Drug Use. Addiction Research Foundation; Toronto, Canada: 1992. [Google Scholar]
- 43.Weinstock J, Whelan JP, Meyers AW. Behavioral assessment of gambling: An application of the Timeline Followback Method. Psychol Assess. 2004;16:72–80. doi: 10.1037/1040-3590.16.1.72. [DOI] [PubMed] [Google Scholar]
- 44.McLellan AT, Alterman AI, Cacciola J, Metzger D, O'Brien CP. A new measure of substance abuse treatment. Initial studies of the Treatment Services Review. J Nerv Ment Dis. 1992;180:101–10. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- 45.Petry NM. Pathological Gambling: Etiology, Comorbidity and Treatments. American Psychological Association Press; Washington, DC: 2005. [Google Scholar]
- 46.Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57:225–38. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- 47.Raudenbush SW, Bryk AS. Hierarchical Linear Models. 2nd ed. Sage Publications, Inc; Thousand Oaks, CA: 2002. [Google Scholar]
- 48.Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- 49.Weinstock JW, Whelan JP, Meyers AW. College students' gambling behavior: When does it become harmful? J Am Coll Health. 2008;56:513–21. doi: 10.3200/JACH.56.5.513-522. [DOI] [PubMed] [Google Scholar]
- 50.Slutske WS, Jackson KM, Sher KJ. The natural history of problem gambling from age 18 to 29. J Abnorm Psychol. 2003;112:263–74. doi: 10.1037/0021-843x.112.2.263. [DOI] [PubMed] [Google Scholar]
- 51.Winters KC, Stinchfield RD, Botzet A, Anderson N. A prospective study of youth gambling behaviors. Psychol Addict Behav. 2002;16:3–9. doi: 10.1037//0893-164x.16.1.3. [DOI] [PubMed] [Google Scholar]
- 52.Winters KC, Stinchfield RD, Slutske WS, Botzet A. Pathways of youth problem gambling severity. Psychol Addict Behav. 2005;19:104–7. doi: 10.1037/0893-164X.19.1.104. [DOI] [PubMed] [Google Scholar]
- 53.National Research Council . Pathological Gambling: A Critical Review. National Academy Press; Washington, DC: 1999. [Google Scholar]
- 54.Walker M, Toneatto T, Potenza MN, Petry N, Ladouceur R, Hodgins DC, et al. A framework for reporting outcomes in problem gambling treatment research: The Banff, Alberta Consensus. Addiction. 2006;101:504–11. doi: 10.1111/j.1360-0443.2005.01341.x. [DOI] [PubMed] [Google Scholar]
- 55.Hodgins DC, Makarchuk K. Trusting problem gamblers: Reliability and validity of self-reported gambling behavior. Psychol Addict Behav. 2003;17:244–48. doi: 10.1037/0893-164X.17.3.244. [DOI] [PubMed] [Google Scholar]
- 56.Shaffer HJ, Forman DP, Scanlan KM, Smith F. Awareness of gambling-related problems, policies and educational programs among high school and college administrators. J Gambl Stud. 2000;16:93–101. doi: 10.1023/a:1009435518147. [DOI] [PubMed] [Google Scholar]