Abstract
Our analysis suggests it wouldn’t be enough—even though spending is lower in markets with more of them.
Spending on health care in markets with a larger percentage of primary care physicians (PCPs) is lower at any point in time than is true in other markets. The relationship between physician workforce composition and the rate of spending growth is less clear. This analysis of market-level Medicare spending data between 1995 and 2005 reveals that the proportion of PCPs is not associated with spending growth. Additional research is needed before the potential causal impact of PCPs can be fully assessed. However, these findings suggest that changes in the composition of the physician workforce will not be sufficient to address spending growth.
Health spending in the united states varies greatly by geography; this fact is well known. For example, in 2003, age-, sex-, and race-adjusted spending for traditional Medicare was $5,428 in the Minneapolis Hospital Referral Region (HRR) but $11,422 per enrollee—more than twice the Minneapolis level—in the Miami HRR.1 These large differences are known to correlate with the ratio of primary care to specialist physicians in an area.2–4 Specifically, a higher proportion of primary care physicians (PCPs) has been shown to be associated not only with lower Medicare spending in a given year but also with higher-quality care.5,6
In recent years a near-consensus has emerged that there are too few PCPs.7 The last time federal policymakers attempted to address physician workforce issues was President Bill Clinton’s proposed Health Security Act of 1993, which set a target ratio of primary to specialist physicians.8 Although that effort failed, the Balanced Budget Act (BBA) of 1997 included special provisions to support training in primary care,9 and physician workforce policy remains a topic of considerable policy debate. For example, in recent congressional testimony, Bruce Steinwald discussed the evidence relating primary care to lower spending and proposals intended to increase the supply of PCPs.10 Others have noted that improving access to primary care (and altering how primary care is financed) may help lower spending and increase the value of care provided by the U.S. health care system.11
Although the evidence suggests a relationship between physician supply and health care spending at any point in time, the existing literature has not examined the relationship between the physician workforce and spending growth—a subject that may be of even greater concern than the high level of spending. For example, Peter Orszag, while director of the Congressional Budget Office (CBO), noted: “Our country’s financial health will be determined primarily by the growth rate of per capita health care spending” (emphasis added).12,13 Thus, understanding whether the mix of generalist and specialist physicians affects health care spending growth is critical.
Conceptual Framework
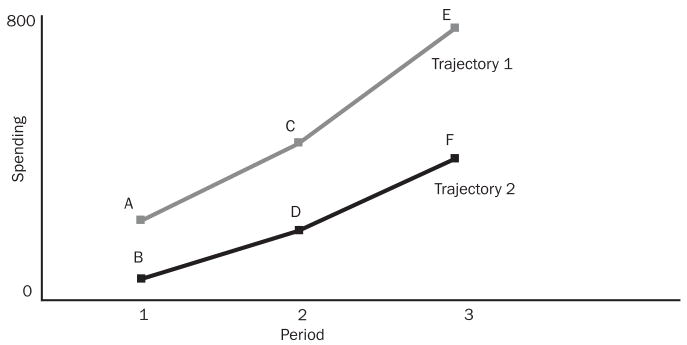
The distinction between the level of spending and spending growth is important. Exhibit 1 presents two hypothetical spending trajectories with the same rate of spending growth. In a particular time period, a change in the level of spending is captured by comparing the points vertically (for example, A versus B). On any given trajectory, spending growth is captured by comparing two points on the same trajectory at different points in time (for example, A versus C). Interventions that reduce the level of spending (that is, shift spending to a lower trajectory) will reduce the rate of spending growth if the base year for measuring growth is before the intervention or during the transition to the new spending curve. For example, an intervention that causes a shift to the lower trajectory between periods 1 and 2 will generate slower spending growth between those periods. Moreover, even if spending growth resumes its original rate after the intervention, the new level of spending will be lower at each point in time, leading to cumulative savings that can be sizable. If the intervention does not reduce the quality of care, it is unambiguously good, even if the steady-state growth rate is unaffected.
EXHIBIT 1.
Level Of Spending Versus Growth In Spending
SOURCE: Author’s analysis.
But if the intervention does not alter the trajectory of spending in the future (beyond period 2), the fiscal pressure faced by the system will return. Cumulative savings, which can be substantial, are the appropriate metric for evaluating the intervention. However, one-time savings (shifts in the level of the curve but not the rate of increase) only delay the fiscal crisis facing health care; they do not solve it. Specifically, although it is tempting to believe that an intervention that alters the level of spending will also alter its trajectory, such reasoning is false unless policy-makers keep finding new one-time interventions that lower the spending curve.
An implication of this reasoning is that factors related to high levels of spending, such as a high proportion of specialist physicians, do not necessarily relate to spending growth. For example, if use of medical services followed the upper line in Exhibit 1 in a specialist-saturated market and the lower line in a primary care–saturated market, the specialist-saturated market would have higher spending at each point in time but not higher steady-state spending growth.
Study Data And Methods
Data sources and type
We used Medicare data over the ten-year period 1995–2005 to examine the relationship between the mix of physicians and an area’s rate of health spending growth. These data show per capita age-, sex-, and race-adjusted Part A and Part B reimbursements for each of 306 HRRs in the United States.14 We excluded home health payments from our spending measure because of dramatic changes in payment for home health care due to the BBA of 1997, including adoption of the interim payment system and several provisions against fraud and abuse, which led to large changes in home health spending.
We drew data on the physician workforce and other area characteristics (demographics, managed care penetration, and hospital infrastructure) from the 2006 Area Resource File (ARF).15 Following Barbara Starfield and colleagues,2 we defined the number of PCPs in an HRR as active patient care physicians in general practice, general family medicine, and general internal medicine. We excluded pediatricians from the overall measure of active patient care physicians because they are unlikely to serve the Medicare population.
Because HRRs are defined as collections of ZIP codes, we aggregated the county-level data from the ARF to the HRR level using the 2001 ZIP code–HRR crosswalk from the Dartmouth Atlas of Health Care.1 In doing so, we weighted each ZIP code by the percentage of the county’s population residing in that ZIP code area in 2000, using data from the Missouri Census Data Center.16
Analysis methods
To explore how the composition of the physician workforce is related to both the level and growth of Medicare spending at the HRR level, we used least-squares linear regression and weighted observations by total HRR population. The primary variables of interest are Medicare spending per beneficiary (Parts A and B) and the percentage change in per beneficiary spending over time, computed as spending in 2005 minus spending in the base year divided by spending in the base year. We estimated the relationship between the percentage of the active patient care physician workforce who are PCPs and both the baseline level of health spending and the subsequent change in health spending (both percentage change and absolute change). We controlled for total patient care physicians per 10,000 population and hospital beds per capita in the base year and for managed care penetration in 1998, which is the only year for which these data are available in the ARF.
We focused on the percentage of physicians in primary care because we did not want to confound the relationship between spending growth and workforce composition with the relationship between spending growth and the absolute size of the physician workforce. However, we conducted sensitivity analysis replacing the percentage of physicians in primary care and the total physicians per capita with variables measuring the absolute numbers of PCPs and specialists per capita. These latter models measure the impact of adding PCPs to the market, as opposed to our base specification that measures the relationship between workforce composition (replacing a specialist with a PCP) and spending growth, holding the number of physicians constant.
In addition, we controlled for the HRR’s (log) per capita income, percentage nonwhite, and (log) total population in the base year, as well as the percentage of the HRR population with at least a high school education and the median age in 2000. In models using measures of change in spending as the dependent variable, we controlled for baseline spending.
Because Medicare payments were greatly affected by the BBA of 1997 and the antifraud efforts of the late 1990s, we repeated the analysis for 2001–2005. Although over the whole study period the percentage of PCPs was relatively stable, we tested the robustness of the findings to models that included the change in the percentage of PCPs (and other covariates) over the period under consideration.
Study Findings
Health spending
Inflation-adjusted health spending in the average HRR rose from about $5,300 in 1995 to over $7,200 in 2005, representing an annual increase of 3.2 percentage points above inflation (Exhibit 2). Health spending grew even more rapidly during 2001–2005.
EXHIBIT 2.
Average Medicare Reimbursement And Physician Supply In 306 Hospital Referral Regions (HRRs), Selected Years 1995–2005
| 1995 | 1997 | 2001 | 2005 | |
|---|---|---|---|---|
| Medicare (Parts A and B) reimbursement per enrollee, 2005 dollars | ||||
| Mean (all HRRs) | $5,324 | $5,833 | $6,245 | $7,272 |
| By quartile | ||||
| Q1 mean | 4,171 | 4,593 | 5,048 | 6,039 |
| Q2 mean | 4,909 | 5,408 | 5,775 | 6,827 |
| Q3 mean | 5,499 | 6,035 | 6,414 | 7,504 |
| Q4 mean | 6,729 | 7,308 | 7,764 | 8,730 |
| PCPs as percent of total patient care physicians | ||||
| Mean (all HRRs) | 29.0% | 29.0% | 29.9% | 29.7% |
| By quartile | ||||
| Q1 mean | 20.8 | 21.4 | 22.1 | 22.1 |
| Q2 mean | 26.4 | 26.5 | 27.4 | 27.4 |
| Q3 mean | 30.9 | 30.9 | 32.0 | 31.7 |
| Q4 mean | 37.9 | 37.4 | 38.1 | 37.7 |
| Total patient care physicians per 10,000 population Mean (all HRRs) | 17.0 | 18.0 | 18.6 | 19.2 |
SOURCE: Authors’ calculations using data from the Dartmouth Atlas of Health Care and the Area Resource File.
NOTE: PCP is primary care physician.
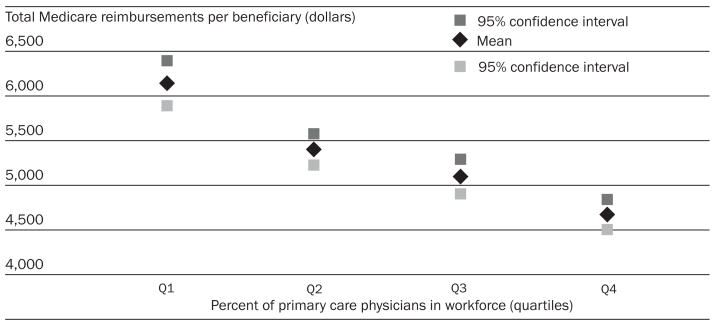
Health spending and PCP prevalence
Consistent with the existing literature, the percentage of PCPs shows a consistent negative association with the level of Medicare reimbursement per beneficiary.6,17 In our data, unadjusted per beneficiary spending falls across quartiles of PCP prevalence (Exhibit 3). These conclusions are robust to multivariate analysis. For example, the multivariate analysis suggests that in 1995 a ten-percentage-point (1.5 standard deviations) greater proportion of PCPs in an HRR is associated with 6.9 percent ($367) lower spending per beneficiary (95 percent confidence interval: −10.9, −2.9; data not shown). The comparable estimates for 2001 and 2005 are within this confidence interval (−9.6 percent and −9.2 percent, respectively) and are statistically different from zero.
EXHIBIT 3.
Mean Unadjusted Average Medicare Reimbursements Per Beneficiary, By Quartile Of Relative Primary Care Physician Supply In 1995
SOURCE: Author’s calculations using data from the Dartmouth Atlas of Health Care and the Area Resource File.
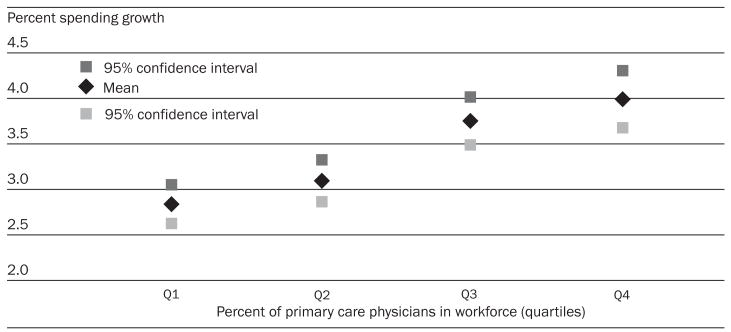
Health spending growth
In contrast, when we consider health spending growth, the percentage of the physician workforce consisting of PCPs in the base year shows either no association or a small positive association with the percentage change in Medicare reimbursement per beneficiary. For the entire period (1995–2005), unadjusted data demonstrate that spending grew more rapidly in markets in the top two quartiles of the proportion of physicians in primary care practice (Exhibit 4).18 Point estimates from our multivariate analysis support the positive association between PCP prevalence and spending growth for the entire study period. They indicate that a ten-point higher percentage of PCPs in the physician workforce (roughly the difference between the twenty-fifth and seventy-fifth percentiles of PCP percentage) is associated with about a 1.8-percentage-point higher rate of spending growth over the study period. The 95 percent CIs suggest a range as high as 4.9 percentage points or as low as −1.3 percentage points (slower growth). Similar results are obtained for the 2001–2005 subperiod.
EXHIBIT 4.
Mean Unadjusted Average Annual Percentage Growth (1995–2005) In Health Spending, By Quartile Of Relative Primary Care Physician Supply In 1995
SOURCE: Author’s calculations using data from the Dartmouth Atlas of Health Care and the Area Resource File.
For example, in 1995, the Sioux City, Iowa, HRR had a high share of PCPs in the workforce (44.6 percent unadjusted, placing it in the top 2 percent of HRRs) and low adjusted per beneficiary Medicare spending ($3,763 per beneficiary, placing it in the lowest 18 percent of HRRs). In contrast, the Pontiac, Michigan, HRR had a low share of PCPs in the workforce (18.9 percent, placing it in the bottom 6 percent of HRRs) and high adjusted per beneficiary Medicare spending ($7,859 per beneficiary, placing it above 98 percent of HRRs).
When we consider percentage spending growth over the period 1995–2005, however, Pontiac was below average (12.0 percent, in the lowest 2 percent of HRRs) and Sioux City was well above average (66.2 percent, in the ninety-sixth percentile of HRRs). Similar examples exist if we consider absolute, rather than percentage, growth over this period.
Robustness of our results
Our conclusions hold up under several specification changes. Models that analyzed the absolute, rather than percentage, change in per beneficiary spending in each HRR did not substantively change the findings. Similarly, models including average spending in an HRR over the first three years of the period (instead of just the first year) generated similar results. Models including the change in the percentage of PCPs over the period (in addition to the baseline level) also yielded results consistent with the finding that markets with a greater share of PCPs have lower spending but do not have systematically slower spending growth. In addition, models based on the total number of PCPs per capita, as opposed to the percentage of physicians in primary care, and models using an alternative definition of PCPs that includes pediatricians also yield similar results. Finally, our results were similar if we controlled for the share of beneficiaries in Medicare managed care (as opposed to the marketwide managed care penetration rate).19
Discussion
There is extensive, influential literature documenting geographic variation in the level of health care spending. Yet growth in spending may be a more serious problem than high spending at any point in time, and the literature that explores factors related to geographic variation in spending growth is scant. Despite extensive interest in physician workforce composition, to our knowledge this is the first study that examines the relationship between workforce composition and spending growth. We exploited variations across geographic areas to investigate the relationship between the percentage of physicians working in primary care in an area and both the level of and growth in Medicare spending.
Comparison with other studies
As have others, we found that a higher proportion of PCPs in an area is associated with a lower level of spending. For example, Elliott Fisher and colleagues investigated differences between HRRs by quintile of Medicare end-of-life spending and found that HRRs in lower-spending quintiles had fewer specialists and more family practitioners and general practitioners than did HRRs in higher-spending quintiles.17,20 Similarly, Katherine Baicker and Amitabh Chandra found that states with a greater proportion of general practitioners had lower spending per Medicare beneficiary compared with other states.6 These studies, however, did not consider the effect of physician workforce composition on spending growth.
Our analysis indicates that physician workforce composition has no relationship with spending growth. This type of finding is consistent with the literature on managed care, which suggests that the impact of managed care on spending at a point in time differs from its impact on spending growth.21
Limitations
Our work shares several limitations with much of the literature on geographic variations. Specifically, like much of the literature, our spending measure is based on data from Medicare, which may differ from total health care spending. Moreover, our Medicare data exclude spending for beneficiaries enrolled in Medicare Advantage (private managed care) plans. Other researchers have reported that this does not materially affect their findings, and our results hold up when the Medicare managed care penetration rate is included.17,20 Finally, although we controlled for many market characteristics, we cannot infer a causal relationship between workforce composition and spending. These findings suggest that primary care–oriented strategies might not slow spending growth; however, our inability to assess causality suggests that additional research is needed before the potential impact of PCPs on spending growth can be fully assessed.
Long-term spending growth
Our results in no way diminish the findings of previous studies. In particular, if one believes that the association between greater primary care availability and lower spending with similar health outcomes is causal, major efficiencies may be achieved by altering the composition of the physician workforce. These efficiencies may be an important source of savings for the system and delay the time when the system is no longer sustainable.
However, even if the proportion of PCPs were to rise and the relationship were causal, our results suggest that the ensuing efficiencies would represent one-time reductions in the level of spending and that subsequent spending growth would remain a concern. A 7 percent one-time savings (equivalent to a change of about 1.5 standard deviations in the proportion of PCPs) will delay the time that spending reaches any given level by about two years. In short, although policies that lower spending levels but do not affect spending growth rates may generate important benefits to the health care system, they will not ultimately address the overarching problem of financing health care.
Acknowledgments
This work was funded by a grant from the Robert Wood Johnson Foundation’s Health Care Financing and Organization (HCFO) Initiative, titled “Variation in Health Care Cost Growth,” Grant no. 64040. Michael Chernew has been a paid author, speaker, or consultant for the following entities: ActiveHealth Management; Altarum; America’s Health Insurance Plans; Anthem; the Association of American Medical Colleges; Avalere; and the Robert Wood Johnson Foundation (RWJF). He has received research grants from the Pharmaceutical Research and Manufacturers of America (PhRMA), Pfizer, RWJF, and the Commonwealth Fund (CMWF). He is on advisory boards for Abbott; the Centers for Medicare and Medicaid Services; CMWF; the Congressional Budget Office; Genentech; the Medicare Payment Advisory Commission; and Pfizer. Amitabh Chandra was funded in part by a grant from the National Institute on Aging, Grant no. NIA P01 AG19783-06. Along with the named funding agencies, the authors also thank seminar participants at Dartmouth.
NOTES
- 1.Wennberg JE, McAndrew CM, editors. The Dartmouth atlas of health care [Internet] Hanover (NH): Dartmouth Institute for Health Policy and Clinical Practice; 2009. Jul, [cited 2009 Jul 20]. Available from http://www.dartmouthatlas.org. [Google Scholar]
- 2.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baicker K, Chandra A. The productivity of physician specialization: evidence from the Medicare program. Am Econ Rev. 2004;94(2):357–61. doi: 10.1257/0002828041301461. [DOI] [PubMed] [Google Scholar]
- 4.Sepulveda MJ, Bodenheimer T, Grundy P. Primary care: can it solve employers’ health care dilemma? Health Aff (Millwood) 2007;27(1):151–8. doi: 10.1377/hlthaff.27.1.151. [DOI] [PubMed] [Google Scholar]
- 5.Mark DH, Gottlieb MS, Zellner BB, Chetty VK, Midtling JE. Medicare costs in urban areas and the supply of primary care physicians. J Fam Pract. 1996;43(1):33–9. [PubMed] [Google Scholar]
- 6.Baicker K, Chandra A. Medicare spending, the physician workforce, and beneficiaries’ quality of care. Health Aff (Millwood) 2004;23:w184–97. doi: 10.1377/hlthaff.w4.184. [DOI] [PubMed] [Google Scholar]
- 7.Whitcomb ME, Cohen JJ. The future of primary care medicine. New Engl J Med. 2004;351(7):710–2. doi: 10.1056/NEJMsb045003. [DOI] [PubMed] [Google Scholar]
- 8.Epstein AM. Changes in the delivery of care under comprehensive health care reform. New Engl J Med. 1993;329(22):1672–6. doi: 10.1056/NEJM199311253292229. [DOI] [PubMed] [Google Scholar]
- 9.Dunn MR, Miller RS, Richter TH. Graduate medical education, 1997–1998. JAMA. 1998;280(9):809–12. doi: 10.1001/jama.280.9.809. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Government Accountability Office. Statement of Bruce Steinwald, director, Health Care [Internet] Washington (DC): GAO; 2008. Primary care professionals: recent supply trends, projections, and valuation of services. [cited 2009 Jun 26]. Pub. no. GAO-08-472T. Available from: http://www.gao.gov/new.items/d08472t.pdf. [Google Scholar]
- 11.Davis K. Slowing the growth of health care costs—learning from international experience. New Engl J Med. 2008;359(17):1751–5. doi: 10.1056/NEJMp0805261. [DOI] [PubMed] [Google Scholar]
- 12.Orszag PR. Testimony before the U.S. Senate Committee on the Budget [Internet] Washington (DC): Congressional Budget Office; 2007. Health care and the budget: issues and challenges for reform. [cited 2009 Jun 26]. Available from: http://www.cbo.gov/ftpdocs/82xx/doc8255/06-21-HealthCareReform.pdf. [Google Scholar]
- 13.Orszag PR, Ellis P. The challenge of rising health care costs—a view from the Congressional Budget Office. New Engl J Med. 2007;357(18):1793–5. doi: 10.1056/NEJMp078190. [DOI] [PubMed] [Google Scholar]
- 14.We adjusted all values for inflation using the all-items Consumer Price Index (CPI) and express results in 2005 dollars; we used the Bureau of Labor Statistics Inflation calculator. Available from: http://www.bls.gov/data/home.htm.
- 15.U.S. Department of Health and Human Services, National Center for Health Workforce Analysis. Area resource file [Internet] Washington (DC): DHHS; [cited 2009 Jun 26]. Available from: http://bhpr.hrsa.gov/healthworkforce/data/arf.htm. [Google Scholar]
- 16.Missouri Census Data Center. MABLE/Geocorr2K: geographic correspondence engine with Census 2000 geography [Internet] Jefferson City (MO): Missouri Census Data Center; 2009. Apr, [cited 2009 Jun 26]. Available from: http://mcdc2.missouri.edu/websas/geocorr2k.html. [Google Scholar]
- 17.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in medicare spending. Part 1: The content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–87. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 18.We performed the same analyses using cost and physician workforce measures adjusted for other market characteristics. Exhibits showing these results are available online at http://content.healthaffairs.org/cgi/content/full/28/5/1327/DC1.
- 19.Our Medicare managed care data were obtained from InterStudy at the MSA level and assigned to HRRs using an MSA/HRR crosswalk. The crosswalk and missing InterStudy data necessitated dropping ninety HRRs in 1995, fifty-eight in 1997, and seventeen in 2001.
- 20.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2:. health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–98. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 21.Chernew ME, Hirth RA, Sonnad SS, Ermann R, Fendrick AM. Managed care, medical technology, and health care cost growth: a review of the evidence. Med Care Res Rev. 1998;55(3):259–88. doi: 10.1177/107755879805500301. [DOI] [PubMed] [Google Scholar]