Abstract
Objective
Recommendations for lower extremity osteoarthritis (OA) and exercise have been primarily based on knee studies. To provide more targeted recommendations for the hip, we gathered evidence for the efficacy of exercise for hip OA from randomized controlled trials.
Methods
A bibliographic search identified trials that were randomized, controlled, completed by ≥60% of subjects, and involved an exercise group (strengthening and/or aerobic) versus a nonexercise control group for pain relief in hip OA. Two reviewers independently performed the data extraction and contacted the authors when necessary. Effect sizes (ES) of treatment versus control and the I2 statistic to assess heterogeneity across trials were calculated. Trial data were combined using a random-effects meta-analysis.
Results
Nine trials met the inclusion criteria (1,234 subjects), 7 of which combined hip and knee OA; therefore, we contacted the authors who provided the data on hip OA patients. In comparing exercise treatment versus control, we found a beneficial effect of exercise with an ES of −0.38 (95% confidence interval [95% CI] −0.68, −0.08; P = 0.01), but with high heterogeneity (I2 = 75%) among trials. Heterogeneity was caused by 1 trial consisting of an exercise intervention that was not administered in person. Removing this study left 8 trials (n = 493) with similar exercise strategy (specialized hands-on exercise training, all of which included at least some element of muscle strengthening), and demonstrated exercise benefit with an ES of −0.46 (95% CI −0.64, −0.28; P < 0.0001).
Conclusion
Therapeutic exercise, especially with an element of strengthening, is an efficacious treatment for hip OA.
Introduction
Symptomatic hip osteoarthritis (OA) occurs in 3% of the elderly (1) and is associated with poor general health status (2). Treatment strategies for hip pain have traditionally involved pharmacologic (acetaminophen, nonsteroidal antiinflammatory drugs [NSAIDs], intraarticular steroids), nonpharmacologic (exercise, education, weight reduction, appliances, heat, cold therapy, transcutaneous electrical nerve stimulation, pulsed electromagnetic field, laser and galvanic stimulation), and surgical intervention (joint replacement) (3). Exercise regimens that are commonly recommended for hip OA include muscle strengthening and aerobic activity (4).
Despite the frequent incorporation of exercise into the treatment regimen for hip OA, the recommendations for exercise in lower extremity OA have been based on knee OA studies. The American College of Rheumatology (ACR) Subcommittee on OA Guidelines (5), the OASIS group (6), and the MOVE consensus (7) have suggested, with a high level of supporting scientific evidence, that performing structured strengthening exercises has a favorable effect on pain and functioning in sedentary patients with knee OA. Conversely, exercise as part of the management of hip OA has been assigned with a category 4 evidence (expert opinion) or not applicable owing to absent hip-specific data according to the MOVE consensus (7) and the European League Against Rheumatism (EULAR) evidence-based recommendations (8), respectively. In the ACR guidelines (5), consulting a physical therapist is considered part of the overall management of hip OA, but no further recommendation regarding exercise is provided.
Therefore, there is a lack of information regarding exercise for patients with hip OA (8), and when data are available there are potential concerns. First, trials that studied hip OA often recruited patients with hip OA in combination with patients with knee OA (9–23). Second, in these trials results have been presented only overall, not in a joint-specific manner. Third, not all of the studies were randomized controlled trials (RCTs) (18–23). Furthermore, 2 Cochrane reviews (24,25) and 2 systematic literature reviews (26,27) presented data for exercise in patients with knee and hip OA, but again, results were not joint specific and too few patients with hip OA were included, precluding valid conclusions for the hip joint. The current reviews also combined studies evaluating 2 types of exercise: therapeutic exercise, which implies a clinically-based intervention (delivered by a health care professional such as a physical therapist), and community-based exercise (delivered by trained leaders, not necessarily health care providers). So far, there has just been one RCT that addressed exercise in subjects with hip as the index joint with OA (28), and it demonstrated a favorable and significant effect on pain.
In light of the limitations of the available data, the aim of this study was to gather evidence for the efficacy of exercise in patients with hip OA provided by RCTs of exercise. We included both trials limited to those with hip OA and trials that combined hip and knee OA with an attempt to obtain data on patients with hip OA from the latter trials. Our goal was to perform a meta-analysis to assess the benefit of exercise for the management of pain in patients with hip OA.
Materials and Methods
Identification of the literature
A bibliographic search was performed on the Medline (January 1966 to July 2007), EMBase, PEDro, and Cochrane databases by a single reviewer (GH-M) using the medical subject heading key words: hip osteoarthritis and coxarthrosis, each exploded and coupled with exercise, therapy, physical therapy, range of motion, rehabilitation, exercise therapy trial, exercise training, physiotherapy, watertherapy, balneotherapy, Tai-chi, and yoga. No limits were established. The search details are provided in Appendix A (available at the Arthritis Care & Research Web site at http://www.interscience.wiley.com/jpages/0004-3591:1/suppmat/index.html). Bibliographic references contained in the articles and abstract publications from the ACR Annual Scientific Meeting (1990–2006) and the EULAR Annual European Congress of Rheumatology (1990–2007) were also sought to complete the search. Results from all of the searches were combined and duplicate references excluded.
Inclusion criteria
In order to be considered, trials had to be randomized, controlled, completed by at least 60% of the baseline participants, involve exercise programs of at least 4 weeks' duration, and include patients who met the criteria presented below.
Trials had to include subjects with hip OA, defined by authors' statements or by ACR criteria (hip pain and at least 2 of the 3 following features: erythrocyte sedimentation rate <20 mm/hour, radiographic femoral or acetabular osteophyte, or radiographic joint space narrowing) (29). In the studies that combined subjects with hip and knee OA, we contacted the primary author to request the hip OA subject information. Only trials with complete information for the hip joint were included.
Trials needed to include at least 1 group performing exercise and a control group where no exercise was prescribed or only range of motion instructions were given. Exercise was defined as a structured activity prescribed or recommended by a health care professional with a view of maintaining or improving health (6) that involved strengthening (isometric and/or isotonic), aerobic activity, or a combination of both, performed in water or on land. Patients could exercise either at home (unsupervised) or at an outpatient gymnasium or pool under supervision; individually or in a group. We required trials to include 1 or more exercise sessions with a duration of ≥30 minutes per session per week. Trials were excluded if they used passive mobilization (manual therapy) or if they focused only on postoperative exercise therapy.
Trials must have included at least 1 of the pain outcome measures currently recommended for OA clinical trials (30). If more than 1 pain outcome was reported, we selected the pain outcome with the following hierarchy (30): global pain score for the index joint (visual analog scale [VAS] or Likert scale), pain on walking in the index joint (VAS or Likert scale), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale (VAS or Likert version), Lequesne index, pain in the index joint during activities other than walking (VAS or Likert scale), or the Harris Hip Score. The outcome was evaluated ideally within 3 months after the intervention was finished. If the study did not provide data at that time, data from the next available time were considered (with a maximum time for evaluating the outcome of 18 months).
Two reviewers (GH-M and SR) independently decided whether a trial should be included. When there was a discrepancy, a third reviewer (DTF) adjudicated.
Hip OA trial types
Trials often studied 2 different types of persons with hip OA. One subtype had hip OA with coexistent knee OA, and in the other subtype the hip was the index joint. For the primary analysis we included both subtypes, but in a secondary analysis we examined only the subgroup with the hip as the index joint. When data were not available from the original articles, we asked the first authors to provide information on both subtypes separately, or in case it was not possible to split the information, to inform us.
Data extraction
The same 2 reviewers performed the data extraction independently using a standardized form. When there was a discrepancy, the opinion of a third reviewer was asked, and disagreements were resolved by consensus. We obtained the pain information from baseline and followup for both the control and intervention groups from tables, text in the manuscript when available, and/or by contacting the authors.
Quality assessment
The 2 reviewers also independently evaluated the methods used in each trial with a standard questionnaire adapted from the quality assessment instrument by Rochon et al (31). This questionnaire evaluated allocation concealment, sample size calculation, compliance testing, inclusion of pretreatment variables in the analysis, presentation of statistical results, evaluation of Type II error, presentation of confidence intervals, withdrawals, discussion of side effects, and quality of statistical analysis. Additional details regarding quality assessment are provided in Appendix B (available at the Arthritis Care & Research Web site at http://www.interscience.wiley.com/jpages/0004-3591:1/suppmat/index.html). Disagreements were adjudicated after both reviewers discussed the discordant items.
Statistical analysis
Results obtained by intent-to-treat analyses were used whenever possible. Because the values for the mean and SD could correspond to different pain outcomes (i.e., VAS, WOMAC, etc.), mean differences were standardized using the following formula (32):
where x̄1 and x̄2 are the mean values of treatment and control at followup, SD1 and SD2 are the SD, and n1 and n2 are the sample sizes of treatment and control, respectively.
We calculated the size of treatment effects for each trial as the difference in mean outcome value between the treatment group and the control group, divided by the pooled SD of the outcome value in the treatment and control groups at followup (32). Trials were combined using a random-effects approach (33). The effect size (ES) was considered small if it was from 0.2–0.4, moderate if it was from 0.5–0.7, and large if it was ≥0.8 (34). To describe heterogeneity across trials, we calculated the I2 statistic based on Cochran's heterogeneity statistic (Q) using the following formula (33,35):
where
Statistical analyses were performed using R software (The R Project for Statistical Computing, Vienna, Austria).
Sensitivity analysis
To check whether a specific trial could have exerted excessive influence on the results, we repeated analyses after identifying and excluding any trial employing different methodology and/or exercise strategy included in the meta-analysis.
Results
Trials
Our search yielded 286 potentially eligible studies. Of these, 206 were excluded after reviewing the abstract because the study did not assess hip OA or exercise, included manual therapy or acupuncture, or focused on postsurgical hip rehabilitation (Figure 1). Eighty reports were retrieved for detailed evaluation. We excluded 71 reports (70 trials) due to duplicate publication of a trial, no exercise intervention (only cognitive–behavioral intervention), no RCT, no pain outcome, article not available (trials in this category were not in English, dated before 1970, and did not have even an abstract), postsurgical exercise trials, or trials with incomplete information after contacting the author (authors did not respond to our query or answered that the knee/hip information was impossible to break down) (Figure 1).
Figure 1.
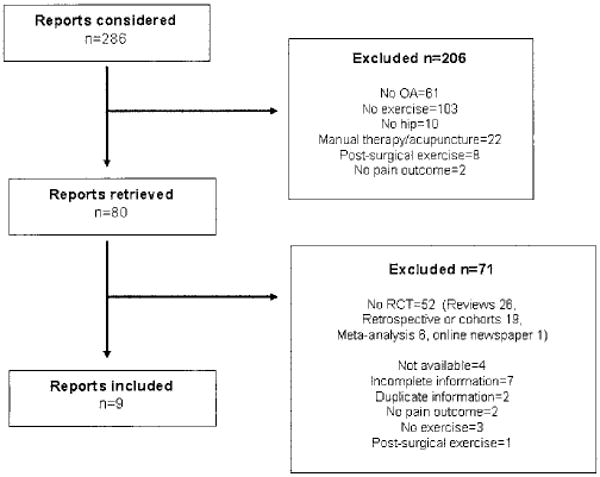
Flow diagram of study selection. OA = osteoarthritis; RCT = randomized controlled trial.
Therefore, our meta-analysis was based on 9 trials. We obtained the hip data from the original articles in 2 trials (28,36), and by authors' provision of information in 7 trials (9–14,17). Six studies (11–14,17,28) defined hip OA according to the ACR criteria and 3 studies (9,10,36) defined hip OA from authors' statements. All of the studies included were published as full-text journal articles. One of the studies (36) involved patients awaiting hip replacement, in which there were baseline and followup evaluations before surgery. The characteristics of the included studies are shown in Table 1.
Table 1. Characteristics of trials included*.
| Author, year (ref.) | Pain outcome | Program duration | Exercise type and control arms | Exercise description |
|---|---|---|---|---|
| Fransen et al, 2007 (11) | WOMAC pain subscale (0–100), Likert version | 2 weekly 1-hour sessions for 12 weeks. Evaluation at 12 weeks. | Aquatic: walking, bar work, seated, deep water noodle, step, free standing, steps, running, stairs, knee and hip flexion/extension/abduction/adduction. Tai Chi: warm-up 10 minutes, Sun style Tai Chi. | |
| Hinman et al, 2007 (14) | VAS (0–10) | 2 weekly 45–60-minute sessions for 12 weeks. Evaluation at 6 weeks. | Warm-up (walking forward, backward, sideways), lower extremity exercise (leg squats, calf raises, dynamic lunge, single-leg stance with contralateral knee flexion/extension or with contralateral hip abduction/adduction or with contralateral hip hitching, step-ups, steps-downs), cool-down (walking). Sets of 2 × 10 to 5 × 10. | |
| Rooks et al, 2006 (36) | WOMAC pain subscale (0–20) | 3 weekly 30–60-minute sessions for 6 weeks. Evaluation at 6 weeks. | Week 1–3: 1–2 sets of 8–12 repetitions of single-joint movements of the cervical spine, shoulders, elbows, wrists, hands, hips, knees, and ankles while standing in chest-deep, 93°F water. Week 4–6: stationary bicycle or elliptical device for 10 minutes with moderate intensity, then 2 sets of 8–12 repetitions of strength activities: seated row, chest press, leg press movements using resistance machines. Flexibility exercises for hip, knee, ankle flexors/extensors, and hip adductors holding each position for 20 seconds and repeating twice. Intensity was tailored. | |
| Cochrane et al, 2005 (10) | WOMAC pain subscale (0–20) | 2 weekly 1-hour sessions for 52 weeks. Evaluation at 26 weeks. | Warm-up, lower extremity strengthening, ROM, and stretches. General cardiovascular conditioning, balance, free use of floats, coordination, individual exercise, and swimming. Increments in the number of repetitions and/or complexity of exercise every 6–8 weeks. | |
| Tak et al, 2005 (28) | VAS (0–10) | 1-hour weekly session for 8 weeks. Evaluation at 8 weeks. | Warm-up, use of fitness equipment (leg press, leg raise, rotation in sitting position, leaping squat, pull down, treadmill, home trainer, pulleys, bow flex, walking), cool-down exercise. Two intensity levels (light and moderate) modulated as fitness equipment as participants progressed. | |
| Ravaud et al, 2004 (13)¶ | VAS (0–100) | 4 weekly 30-minute sessions for 12–24 weeks. Evaluation at 24 weeks. | Five exercise routines to improve joint mobility and muscle power. Each exercise was repeated 10 times and then in increments of 5 repetitions each week up to 30 according to each patient. | |
| Foley et al, 2003 (9) | WOMAC pain subscale (0–20) | 3 weekly 30-minute sessions for 6 weeks. Evaluation at 6 weeks. | Aquatic: warm-up (walking) and strengthening exercises (hip flexion/extension/adduction/abduction, knee flexion/extension, knee cycling). 1 × 10 repetitions were progressively increased to sets of 3 × 15, then weighted gaiters were fastened on ankles and repetitions were performed as tolerated. Land-based: warm-up (stationary cycling), strengthening (seated bench press, hip adduction/abduction, knee extension, double-leg press). Same intensity protocol as in the aquatic program. | |
| Hopman-Rock and Westhoff, 2000 (12) | VAS (0–100) | 1 weekly 1-hour session for 6 weeks. Evaluation at 6 weeks. | Warm-up, exercises for hip/knee (with the help of a chair), cool-down, and relaxation. Dynamic exercise alternated with static exercise and a standard resistance protocol. | |
| Van Baar et al, 1998 (17) | VAS (0–100) | 1–3 weekly 30-minute sessions for 12 weeks. Evaluation at 12 weeks. | Content and intensity according to the patient. Exercise for muscle functioning (strength and length), mobility, exercises for elementary movement, locomotion abilities, and coordination. |
WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; VAS = visual analog scale; ROM = range of motion.
Hip is the index joint.
Participants may or may not have coexistent knee osteoarthritis (OA).
The number before the slash corresponds to participants with coexistent knee and hip OA; the number after the slash corresponds to participants with hip as the index joint with OA.
All groups also used pain assessment tools.
Did not use pain assessment tools. Hip is the index joint.
Among the 9 trials, the number of exercise sessions per week ranged from 1–4 (median 3) and the duration of each session ranged from 30–60 minutes (median 52.5). In 7 trials, the intensity of exercise was individually adjusted for each patient, and in the remaining 2 trials, this information was not available (11,12). Exercise was performed on land (9,11–13,17,28), in water (9–11,14), or involved a combination of both modalities (36). Most of the time, participants performed exercise at a gymnasium or pool under the supervision of a physical therapist, whereas in 2 trials (12,13), exercise was performed at home. In 1 of these home-based exercise trials (12), physical exercise was taught at the beginning of the study by a physical therapist, whereas in the other trial (13), a videotape showing how to exercise (by a trained demonstrator) was provided.
All trials included at least 1 group with a strengthening exercise program and some of them combined strengthening and aerobic exercise (9–11,14,36). Table 1 shows detailed exercise descriptions of each trial. The followup evaluations were performed between 6 and 26 weeks (median 8) after starting the exercise program.
Quality scores
Four studies used an intent-to-treat analysis (9,11,14,17), 4 used a completer analysis (10,12,28,36), and 1 used both types of analysis (13). All trials were randomized; however, in 1 trial (13), randomization was applied to the rheumatologists instead of the participants. Allocation concealment was adequate in 5 of the trials (9,11,14,17,28) and sample size calculation and compliance were reported in all of them. Three studies reported minor and infrequent adverse events related to exercise such as mild joint discomfort, lumbar pain, and cramps in the calf (11,14,17). See Appendix B for additional details regarding quality scores of each trial (available at the Arthritis Care & Research Web site at http://www.interscience.wiley.com/jpages/0004-3591:1/suppmat/index.html).
Meta-analysis
For the hip OA analysis (n = 1,234), the exercise group consisted of 602 patients and the control group consisted of 632 patients. When we analyzed these trials, we found an overall significant ES for exercise of −0.38 (95% confidence interval [95% CI] −0.68, −0.08; P = 0.01), where negative values favor exercise over control (Figure 2A). Table 2 shows detailed information on the ES of each trial. However, the test for heterogeneity was I2 = 0.75, indicating that 75% of the variation in pain results was due to heterogeneity between trials rather than chance.
Figure 2.
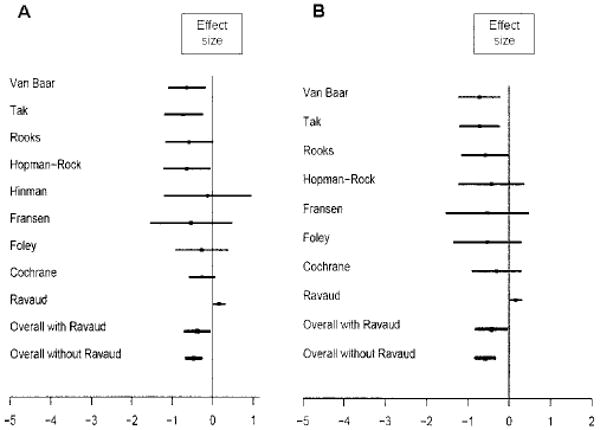
A, Forest plot of hip osteoarthritis (OA) data (patients may have coexistent knee OA). B, Forest plot of hip as the index joint with OA.
Table 2. Effect sizes of trials of subjects with hip OA (subjects may have coexistent knee OA)*.
| Author, year (ref.) | Control followup | Exercise followup | Effect size (95% CI) | Effect size SD | P | ||
|---|---|---|---|---|---|---|---|
| Mean ± SD | No. | Mean ± SD | No. | ||||
| Fransen et al, 2007 (11) | 8.40 ± 3.44 | 5 | 6.58 ± 3.28 | 19 | −0.53 (−1.53, 0.46) | 0.50 | 0.29 |
| Hinman et al, 2007 (14) | 5.73 ± 2.10 | 11 | 5.40 ± 3.21 | 5 | −0.12 (−0.18, 0.93) | 0.54 | 0.81 |
| Rooks et al, 2006 (36) | 9.90 ± 2.90 | 24 | 7.80 ± 4.10 | 25 | −0.58 (−1.15, −0.008) | 0.29 | 0.04 |
| Cochrane et al, 2005 (10) | 9.77 ± 3.16 | 80 | 8.91 ± 3.42 | 78 | −0.25 (−0.57, 0.05) | 0.15 | 0.10 |
| Tak et al, 2005 (28) | 5.10 ± 2.30 | 39 | 3.50 ± 2.10 | 35 | −0.71 (−1.19, −0.24) | 0.24 | 0.003 |
| Ravaud et al, 2004 (13) | −17.49 ± 24.37 | 388 | −13.75 ± 23.90 | 352 | 0.15 (0.01, 0.29) | 0.07 | 0.03 |
| Foley et al, 2003 (9) | 10.07 ± 4.01 | 15 | 9.00 ± 3.76 | 26 | −0.27 (−0.91, 0.36) | 0.32 | 0.40 |
| Hopman-Rock and Westhoff, 2000 (12) | 46.36 ± 22.46 | 28 | 32.00 ± 21.90 | 22 | −0.63 (−1.21, −0.06) | 0.29 | 0.02 |
| Van Baar et al, 1998 (17) | 41.85 ± 22.22 | 39 | 26.64 ± 25.11 | 39 | −0.63 (−1.09, −0.18) | 0.23 | 0.006 |
OA = osteoarthritis; 95% CI = 95% confidence interval.
For the analysis of the hip as the index joint (n = 1,063), the exercise group consisted of 515 patients and the control group consisted of 548 patients. The direction of the result was similar and also significant, with an ES for exercise of −0.43 (95% CI −0.80, −0.06; P = 0.02) (Figure 2B). Table 3 shows detailed information on the ES of each trial. For this subset of studies, heterogeneity was I2 = 76%.
Table 3. Effect sizes of trials with hip as the index joint with osteoarthritis*.
| Author, year (ref.) | Control followup | Exercise followup | Effect size (95% CI) | Effect size SD | P | ||
|---|---|---|---|---|---|---|---|
| Mean ± SD | No. | Mean ± SD | No. | ||||
| Fransen et al, 2007 (11) | 8.40 ± 3.44 | 5 | 6.58 ± 3.28 | 19 | −0.53 (−1.53, 0.46) | 0.50 | 0.29 |
| Hinman et al, 2007 (14)† | |||||||
| Rooks et al, 2006 (36) | 9.90 ± 2.90 | 24 | 7.80 ± 4.10 | 25 | −0.58 (−1.15, −0.008) | 0.29 | 0.04 |
| Cochrane et al, 2005 (10) | 9.29 ± 3.55 | 24 | 8.14 ± 3.86 | 21 | −0.30 (−0.89, 0.28) | 0.30 | 0.31 |
| Tak et al, 2005 (28) | 5.10 ± 2.30 | 39 | 3.50 ± 2.10 | 35 | −0.71 (−1.19, −0.24) | 0.24 | 0.003 |
| Ravaud et al, 2004 (13) | −17.49 ± 24.37 | 388 | −13.75 ± 23.90 | 352 | 0.15 (0.01, 0.29) | 0.07 | 0.03 |
| Foley et al, 2003 (9) | 10.58 ± 4.12 | 12 | 8.50 ± 3.49 | 12 | −0.52 (−1.34, 0.28) | 0.41 | 0.20 |
| Hopman-Rock and Westhoff, 2000 (12) | 47.20 ± 20.50 | 15 | 37.00 ± 26.00 | 11 | −0.43 (−1.22, 0.35) | 0.40 | 0.28 |
| Van Baar et al, 1998 (17) | 43.42 ± 21.61 | 33 | 26.00 ± 25.85 | 35 | −0.71 (−1.21, −0.23) | 0.25 | 0.004 |
95% CI = 95% confidence interval.
Did not provide subjects for this categorization.
As a sensitivity analysis, we excluded the study by Ravaud and colleagues (13) for the following reasons: 1) it was the only trial where exercise was not taught personally by a health professional (instead, a motivational videotape showing how to exercise by a trained demonstrator was provided), 2) because it randomized rheumatologists instead of patients, there was a concern about selection bias, and 3) it was the only trial where adherence to exercise was low (1 of 3 patients adhered to exercise compared with at least 59% in the other studies). It was also by far the largest study (n = 741), suggesting its results may have had a major influence on the overall results.
When this trial was excluded from the analysis, no heterogeneity remained among trial results (I2 = 0), and the ES also showed an exercise benefit among the remaining trials (ES = −0.47; 95% CI −0.65, −0.28) (P < 0.0001) (Figure 2A). When we reperformed the meta-analysis looking at the subset with hip as the index joint with OA and again removed the study by Ravaud et al, we also found a benefit for exercise therapy (ES for exercise = −0.58; 95% CI −0.81, −0.35) (P < 0.0001), and heterogeneity among trials was also removed (I2 = 0) (Figure 2B).
Discussion
Currently, there is a lack of information to support the benefit of performing exercise for relieving hip OA pain. So far, only 1 RCT has assessed the hip as the index joint with OA (28) with a positive result. The overall results of our meta-analysis showed a significant treatment effect in favor of exercise, but moderate to high heterogeneity among trials was present. Furthermore, we found a stronger favorable effect of exercise when we excluded the trial that was the source of heterogeneity. This latter study used a different prescribed exercise strategy (no therapeutic exercise) and poor exercise adherence, which may have accounted for its unique results.
Exercise trials in lower extremity OA have reported small (0.2) to moderate (0.7) ES for pain (37). These effects could be compared with pharmacologic treatment such as acetaminophen (ES = 0.2) and NSAIDs (ES = 0.69 only for hip joint) (8). Here, we found a small benefit of exercise in patients with coexistent hip and knee OA (ES = −0.38), as in a subset of patients with hip as the index joint with OA (ES = −0.43).
First, we decided to include the study by Ravaud et al because it was by far the largest trial addressing exercise in patients with lower extremity OA and because it met our inclusion criteria. Nevertheless, we considered this study to be different from the rest of the trials in the meta-analysis because it was the only one that used an unsupervised exercise program where exercise was not taught personally by a health professional at least once. Moreover, as the authors have previously commented (13), it is possible that the participants did not carry out exercises properly. There was also a poor compliance (2 of 3 subjects did not attain the specified adherence standard); however, the impact of this factor is still controversial (38). Therefore, in the remainder of the trials in our meta-analysis, exercise regimens were taught personally to subjects by a physiotherapist (therapeutic exercise) at least once.
Currently, the most effective therapeutic exercise for lower extremity OA involves regular aerobic activity and/or a strengthening program (4). For knee OA, 2 meta-analyses have not shown any association between pain relief and exercise intensity (24) or duration of the program or frequency of sessions (39).
Among the trials included in our meta-analysis, one common element was the performance of strengthening exercise and repeated in-person attempts to refine and individualize the program, suggesting that this type of exercise might be effective. Although not necessarily a comprehensive assessment of adverse events, the data from these trials suggest that exercise may be safe in these patients.
The current meta-analysis has limitations. First, because most of the data (with the exception of 2 trials) were obtained from trials where hip and knee OA were originally combined but not stratified, it is possible that when we selected only those subjects with hip OA, the initial randomization of the treatment and control groups was lost. Second, post hoc removal of trial data from a meta-analysis may lead to misleading conclusions (40). However, this strategy has been used when individual study results are in conflict or for the generation of new hypotheses (41). In our sensitivity analysis, we removed a trial in which the administration of exercise was remote and not provided by a health professional, a qualitatively different strategy than the other trials. Ultimately, combining data from multiple small trials on patients with hip OA may not be equivalent to carrying out a trial in which direct teaching of exercise is used and a large number of patients is enrolled.
Even so, our meta-analysis provides insight into the effectiveness of exercise therapy for pain relief in patients with hip OA. Overall, we found a small favorable effect for therapeutic exercise; moreover, when we focused on trials of subjects with hip as the index joint with OA, this effect was moderate. This leads us to suggest that therapeutic exercise constitutes efficacious treatment for pain in patients with hip OA.
Acknowledgments
We are extremely grateful to Professor Tom Cochrane, Professor Maria Crotty, Dr. Marlene Fransen, Dr. Rana Hinman, Dr. Marijke Hopman-Rock, Dr. Erwin Tak, Dr. Philippe Ravaud, and Dr. Margriet van Baar for kindly providing the specific data from their trials.
Supported by the NIH (grant AR-47785).
Footnotes
Author Contributions: Dr. Felson had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study design. Hernández-Molina, Reichenbach, LaValley, Felson.
Acquisition of data. Hernández-Molina, Reichenbach.
Analysis and interpretation of data. Hernández-Molina, Reichenbach, Zhang, LaValley, Felson.
Manuscript preparation. Hernández-Molina, Reichenbach, Zhang, LaValley, Felson.
Statistical analysis. Zhang, LaValley.
References
- 1.Felson DT. An update on the pathogenesis and epidemiology of osteoarthritis. Radiol Clin North Am. 2004;42:1–9. doi: 10.1016/S0033-8389(03)00161-1. [DOI] [PubMed] [Google Scholar]
- 2.Dawson J, Linsell L, Zondervan K, Rose P, Randall T, Carr A, et al. Epidemiology of hip and knee pain and its impact on overall health status in older adults. Rheumatology (Oxford) 2004;43:497–504. doi: 10.1093/rheumatology/keh086. [DOI] [PubMed] [Google Scholar]
- 3.Di Domenica F, Sarzi-Puttini P, Cazzola M, Atzeni F, Cappadonia C, Caserta A, et al. Physical and rehabilitative approaches in osteoarthritis. Semin Arthritis Rheum. 2005;34(6 Suppl 2):62–9. doi: 10.1016/j.semarthrit.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 4.Minor M. Impact of exercise on osteoarthritis outcomes. J Rheumatol. 2004;31 70:81–6. [PubMed] [Google Scholar]
- 5.American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum. 2000;43:1905–15. doi: 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 6.Vignon E, Valat JP, Rossignol M, Avouac B, Rozenberg S, Thoumie P, et al. Osteoarthritis of the knee and hip and activity: a systematic international review and synthesis (OASIS) Joint Bone Spine. 2006;73:442–55. doi: 10.1016/j.jbspin.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Roddy E, Zhang W, Doherty M, Arden NK, Barlow J, Birrell F, et al. Evidence-based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee: the MOVE consensus. Rheumatology (Oxford) 2005;44:67–73. doi: 10.1093/rheumatology/keh399. [DOI] [PubMed] [Google Scholar]
- 8.Zhang W, Doherty M, Arden N, Bannwarth B, Bijlsma J, Gunther KP, et al. EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT) EULAR evidence based recommendations for the management of hip osteoarthritis: report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT) Ann Rheum Dis. 2005;64:669–81. doi: 10.1136/ard.2004.028886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foley A, Halbert J, Hewitt T, Crotty M. Does hydrotherapy improve strength and physical function in patients with osteoarthritis: a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis. 2003;62:1162–7. doi: 10.1136/ard.2002.005272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cochrane T, Davey RC, Matthes Edwards SM. Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis. Health Technol Assess. 2005;9:1–114. doi: 10.3310/hta9310. [DOI] [PubMed] [Google Scholar]
- 11.Fransen M, Nairn L, Winstanley J, Lam P, Edmonds J. Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum. 2007;57:407–14. doi: 10.1002/art.22621. [DOI] [PubMed] [Google Scholar]
- 12.Hopman-Rock M, Westhoff M. The effects of a health educational and exercise program for older adults with osteoarthritis of the hip or knee. J Rheumatol. 2000;27:1947–54. [PubMed] [Google Scholar]
- 13.Ravaud P, Giraudeau B, Logeart I, Larguier JS, Rolland D, Treves R, et al. Management of osteoarthritis (OA) with an unsupervised home based exercise programme and/or patient administered assessment tools: a cluster randomized controlled trial with a 2×2 factorial design. Ann Rheum Dis. 2004;63:703–8. doi: 10.1136/ard.2003.009803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hinman RS, Heywood SE, Day AR. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther. 2007;87:32–43. doi: 10.2522/ptj.20060006. [DOI] [PubMed] [Google Scholar]
- 15.Halbert J, Crotty M, Weller D, Ahern M, Silagy C. Primary care–based physical activity programs: effectiveness in sedentary older patients with osteoarthritis symptoms. Arthritis Rheum. 2001;45:228–34. doi: 10.1002/1529-0131(200106)45:3<228::AID-ART253>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 16.Minor MA, Hewett JE, Webel RR, Anderson SK, Kay DR. Efficacy of physical conditioning exercise in patients with rheumatoid arthritis and osteoarthritis. Arthritis Rheum. 1989;32:1396–405. doi: 10.1002/anr.1780321108. [DOI] [PubMed] [Google Scholar]
- 17.Van Baar ME, Dekker J, Oostendorp RA, Bijl D, Voorn TB, Lemmens JA, et al. The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized clinical trial. J Rheumatol. 1998;25:2432–9. [PubMed] [Google Scholar]
- 18.Green J, McKenna F, Redfern EJ, Chamberlain MA. Home exercises are as effective as outpatient hydrotherapy for osteoarthritis of the hip. Br J Rheumatol. 1993;32:812–5. doi: 10.1093/rheumatology/32.9.812. [DOI] [PubMed] [Google Scholar]
- 19.De Jong OR, Hopman-Rock M, Tak EC, Klazinga NS. An implementation study of two evidence-based exercise and health education programmes for older adults with osteoarthritis of the knee and hip. Health Educ Res. 2004;19:316–25. doi: 10.1093/her/cyg028. [DOI] [PubMed] [Google Scholar]
- 20.Klassbo M, Larsson G, Harms-Ringdahl K. Promising outcome of a hip school for patients with hip dysfunction. Arthritis Rheum. 2003;49:321–7. doi: 10.1002/art.11110. [DOI] [PubMed] [Google Scholar]
- 21.Lin SY, Davey RC, Cochrane T. Community rehabilitation for older adults with osteoarthritis of the lower limb: a controlled clinical trial. Clin Rehabil. 2004;18:92–101. doi: 10.1191/0269215504cr706oa. [DOI] [PubMed] [Google Scholar]
- 22.Angst F, Aeschlimann A, Steiner W, Stucki G. Responsiveness of the WOMAC osteoarthritis index as compared with the SF-36 in patients with osteoarthritis of the legs undergoing a comprehensive rehabilitation intervention. Ann Rheum Dis. 2001;60:834–40. [PMC free article] [PubMed] [Google Scholar]
- 23.Sylvester K. Investigation of the effect of hydrotherapy in the treatment of osteoarthritic hips. Clin Rehabil. 1989;4:223–8. [Google Scholar]
- 24.Brosseau L, MacLeay L, Robinson V, Wells G, Tugwell P. Intensity of exercise for the treatment of osteoarthritis. Cochrane Database Syst Rev. 2003;2:CD004259. doi: 10.1002/14651858.CD004259. [DOI] [PubMed] [Google Scholar]
- 25.Fransen M, McConnell S, Bell M. Exercise for osteoarthritis of the hip and knee. Cochrane Database Syst Rev. 2003;3:CD004286. doi: 10.1002/14651858.CD004286. [DOI] [PubMed] [Google Scholar]
- 26.Fransen M, McConnell S, Bell M. Therapeutic exercise for people with osteoarthritis of the hip or knee: a systematic review. J Rheumatol. 2002;29:1737–45. [PubMed] [Google Scholar]
- 27.Van Baar ME, Assendelft WJ, Dekker J, Oostendorp RA, Bijlsma JW. Effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic review of randomized clinical trials. Arthritis Rheum. 1999;42:1361–9. doi: 10.1002/1529-0131(199907)42:7<1361::AID-ANR9>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 28.Tak E, Staats P, Van Hespen A, Hopman-Rock M. The effects of an exercise program for older adults with osteoarthritis of the hip. J Rheumatol. 2005;32:1106–13. [PubMed] [Google Scholar]
- 29.Altman R, Alarcon G, Appelrouth D, Bloch D, Borenstein D, Brandt K, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505–14. doi: 10.1002/art.1780340502. [DOI] [PubMed] [Google Scholar]
- 30.Altman R, Brandt K, Hochberg M, Moskowitz R, Bellamy N, Bloch DA, et al. Design and conduct of clinical trials in patients with osteoarthritis: recommendations from a task force of the Osteoarthritis Research Society. Results from a workshop Osteoarthritis Cartilage. 1996;4:217–43. doi: 10.1016/s1063-4584(05)80101-3. [DOI] [PubMed] [Google Scholar]
- 31.Rochon PA, Gurwitz JH, Cheung CM, Hayes JA, Chalmers TC. Evaluating the quality of articles published in journal supplements compared with the quality of those published in the parent journal. JAMA. 1994;272:108–13. [PubMed] [Google Scholar]
- 32.Hedges LV, Olkin I. Statistical methods for meta-analysis. San Diego: Academic Press; 1985. [Google Scholar]
- 33.Whitehead A. Combining estimates of a treatment difference across trials. In: Whitehead A, editor. Meta-analysis of controlled clinical trials. Chichester (UK): The Atrium Southern Gate; 2002. pp. 59–60.pp. 88–91. [Google Scholar]
- 34.Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale (NJ): Lawrence Erlbaum; 1998. [Google Scholar]
- 35.Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10:102–29. [Google Scholar]
- 36.Rooks DS, Huang J, Bierbaum BE, Bolus SA, Rubano J, Connolly CE, et al. Effect of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis Rheum. 2006;55:700–8. doi: 10.1002/art.22223. [DOI] [PubMed] [Google Scholar]
- 37.Bischoff HA, Roos E. Effectiveness and safety of strengthening, aerobic, and coordination exercises for patients with osteoarthritis. Curr Opin Rheumatol. 2003;15:141–4. doi: 10.1097/00002281-200303000-00010. [DOI] [PubMed] [Google Scholar]
- 38.Sisto SA, Malanga G. Osteoarthritis and therapeutic exercise. Am J Phys Med Rehabil. 2006;85(11 Suppl):S69–78. doi: 10.1097/01.phm.0000245509.06418.20. [DOI] [PubMed] [Google Scholar]
- 39.Lund H, Christensen R, Bliddal H. The relationship between applied exercise dosage and clinical effect size for patients with knee osteoarthritis [abstract] Ann Rheum Dis. 2006;65 2:397. [Google Scholar]
- 40.Egger M, Smith G, Altman D. Going beyond the grand mean: subgroup analysis in meta-analysis of randomized trials. In: Egger M, Smith GD, Altman DG, editors. Systematic reviews in health care: meta-analysis in context. 2nd. London: BMJ Publishing; 2001. pp. 143–6. [Google Scholar]
- 41.Elliot HL. Post hoc analysis: use and dangers in perspective. J Hypertens Suppl. 1996;14:S21–4. doi: 10.1097/00004872-199609002-00006. [DOI] [PubMed] [Google Scholar]


