Abstract
Psychotropic medications are used regularly to manage problem behaviours among people with intellectual disabilities. This causes concern because often these medications are used out of their licensed indications in this context. The WPA Section on Psychiatry of Intellectual Disability has recently developed an evidence and consensus-based international guide for practitioners for the use of psychotropic medications for problem behaviours among adults with intellectual disabilities. This guide advises on assessment of behaviours, producing a formulation, initiation of treatment, assessment of out-come and adverse effects, follow-up arrangements, and possibility of discontinuation of treatment.
Keywords: Intellectual disabilities, problem behaviours, psychotropic medications, international guide
Intellectual disability (ID) or mental retardation or learning disability is a lifelong condition included in the group of mental disorders in all the international classification systems. It is a syndrome grouping (meta-syndrome) including a heterogeneous range of clinical conditions characterized by a deficit in cognitive functioning prior to the acquisition of skills through learning 1. Over 30% of people with ID have a comorbid psychiatric disorder, which often has its onset in childhood and persists through adolescence and adulthood 2,3.
In spite of this evidence, ID and related conditions are still considered a marginal area of psychiatry. In many countries there is little or no training provision on ID during undergraduate medical training or psychiatric specialization. The World Health Organization (WHO) has recently highlighted the unmet care needs of persons with ID 4. Psychiatrists are the first health professionals in contact with this population group and there is a global gap in training and guidelines on mental health issues related to ID.
Within the ID field, the assessment, differential diagnosis and treatment of problem behaviours (PBs) deserve special attention. The rate of PBs in people with ID is high 5and their presentation is determined by many complex factors. The pathogenic contribution of organic conditions, psychiatric disorders, environmental influences, or a combination of these has to be carefully established for every single case.
The prevalence of PBs in people with ID seems to be sufficiently high 5,6to constitute a major concern in this population. Depending on the definition and methodology, rates have been reported to vary from 5.7 to 17% 7-10. Using the Diagnostic Criteria for Psychiatric Disorders for Use with Adults with Learning Disabilities (DC-LD) 11, Cooper et al 12,13recently found the point prevalence of aggression and self-injurious behaviour to be 9.8% and 4.9%, respectively, among adults (16 years and over) with ID in a community setting.
It has been reported that 20-45% of people with ID are receiving psychotropic medication and 14-30% are receiving psychotropic medication to manage PBs such as aggression or self-injurious behaviours 14,15in the absence of a diagnosed psychiatric disorder. Examples of psychotropic medications used for adults with ID are antipsychotics, antidepressants, anti-anxiety drugs (benzodi-azepines, buspirone, beta-blockers), mood stabilizers (lithium, anticonvulsants), psychostimulants, and opioid antagonists. Spreat et al 16reported that as many as two thirds of psychotropic medications prescribed to people with ID are antipsychotics.
Studies suggest that PBs are not only prevalent but also persistent in people with ID 17-19. Totsika et al 20found that serious physical attacks, self-injury and stereotypy were the most likely types of PBs to persist over time. It is therefore suggested that it may be necessary to start interventions as early as possible to prevent the behaviours from becoming more serious and to reduce the number of emergent behaviours. It has been pointed out that many of the behaviours that emerge are a direct consequence of limitations in people’s ability to communicate effectively 21-25. Replacing “learned behaviour” at an early age with more acceptable forms of communication may therefore not only reduce the number of emerging behaviours, but also reduce the severity of the behaviours that do occur.
The rate of prescription of psychotropic medications for the management of PBs is a source of concern, due to the scarce evidence concerning their effectiveness and adverse events and their impact on quality of life in people with ID 14,26-29. Many adults with ID receive multiple psychotropic medications and in high dose.
THE INTERNATIONAL GUIDE
Framework and development
The international guide is an adaptation from the recently developed guide on the subject 30in the UK. The UK guide followed the NICE guideline development procedure. This includes a systematic review of evidence and a broad consensus based on the available evidence on good practice. A very extensive stakeholder consultation was carried out before finalizing the recommendations.
The international guide reflects the available knowledge and the perspectives of experts practicing in psychiatry of ID in different parts of the world. A PB is defined here as a “socially unacceptable behaviour that causes distress, harm or disadvantage to the persons themselves or to other people, and usually requires some intervention” 30. The guide neither supports nor refutes the use of psychotropic medications in this context, but provides clinicians and carers of adults with ID worldwide with good practice advice despite the lack of adequate good quality evidence on this subject. The main recommendations contained in the guide are summarized in the following sections.
Assessment and formulation
The primary aim of management of PBs in people with ID should be not to treat the behaviour per se but to identify and address the underlying cause of the behaviour. However, it is not always possible to find a cause for the PB. When a cause cannot be found, the management strategy should be to minimise the impact of the behaviour on the person, the environment around her/him and other people.
There may be many reasons for PBs, including physical or mental health problems. Many factors, internal (e.g., negative childhood experiences, maladaptive coping strategies) or external to the person (e.g., an under-stimulating or over-stimulating environment), may contribute to PBs. Sometimes behaviour may be used as a means of communication. For example, persons with severe ID who cannot speak or use a sign language may scream because they are in pain and they cannot communicate this message in any other way. Sometimes persons with ID may use behaviour to communicate their likes and dislikes.
Therefore, a thorough assessment of the causes of behaviour and their consequences, along with a formulation, is an absolute prerequisite in managing any PB. A comprehensive assessment may require input from several disciplines and from families and carers. It should cover personal, psychological, social, environmental, medical and psychiatric issues. A multi-axial/multilayered diagnostic formulation, such as that suggested in the DC-LD 11and the Diagnostic Manual – Intellectual Disability (DM-ID) 31, may be useful in this context. A formulation should be made even in the absence of a medical or psychiatric diagnosis.
As a general rule, the formulation should consist of the following:
– A list of the target PB(s) to be managed.
– A clear description of the PB, including frequency and severity.
– An assessment of causes giving rise to the PB.
– A record of reactions to and outcomes of the behaviour.
– An evaluation of predisposing, precipitating and perpetuating risk factors.
– Consideration of all management options and their outcome.
– The rationale for the proposed management option.
– A risk assessment for all the involved parties.
– Possible benefits and adverse effects from the proposed intervention(s).
– The likely effect of the proposed intervention(s) on the person’s and her/his family’s quality of life.
A proper assessment and formulation will often depend on input from the person with ID and/or her/his family and carers. This input should continue at every stage of management. It is important to share information with the person with ID in a way that he/she can understand. This may require additional time and effort on the part of the health professionals and other members of the multidisciplinary team. It may also involve using other methods of information sharing, such as pictures.
Multidisciplinary input may also be needed during implementation and monitoring of the management options. This may not always be possible to achieve, because of lack of resources or expertise in this field. Where relevant and if possible, an attempt should be made to secure multidisciplinary input throughout the process of assessment and management.
When to consider medication
If there is an obvious physical or psychiatric cause for the behaviour, this should be managed appropriately. The relevant guides governing the use of medication in the treatment of the particular psychiatric disorder should be followed 32,33.
If no treatable physical or psychiatric disorder can be recognized, then non-medication based management such as behavioural strategies should be considered first. Sometimes, after considering non-medication based management options, medication may be needed either on its own or as an adjunct to non-medication based management. However, it may also be possible to improve the PB of the person by providing counselling or addressing some adverse social and environmental factors, for example by finding more enjoyable activities to do during the day, and using medication simultaneously to make the person concerned less anxious. This may be seen as an interim strategy, which then needs to be monitored carefully at regular intervals to assess its effectiveness.
The exact situation under which medication and/or non-medication based management strategies should be implemented will depend on individual circumstances. Below are some of the situations under which the clinicians may consider using medication:
– Failure of non-medication based interventions.
– Risk/evidence of harm/distress to self.
– Risk/evidence of harm/distress to others or property.
– High frequency/severity of PB.
– To treat an underlying psychiatric disorder or anxiety.
– To calm the person to enable implementation of non-medication based interventions.
– Risk of breakdown to the person’s placement.
– Good previous response to medication.
– Person/carer choice.
The lack of adequate or available non-medication based interventions should not be the only reason for using medication, although in practice this may happen. Under such circumstances, the medication should be used for as short a period as possible.
The management of PB should always be person-centred. The plan should be discussed with the person with ID and/or her/his carers and should be designed according to the person’s best interests. The prescribing should not take place in isolation but should always be part of a much broader person-centred care plan.
Monitoring the effectiveness of medication
The effectiveness and possible adverse effects of the prescribed medication should be monitored at regular intervals. This should include collecting objective information from family members, carers, staff of the multi-disciplinary team as well as the person with ID, where necessary and possible. Physical examination and relevant investigations such as blood tests and ECG/EKG should also be performed when necessary.
The medication should be prescribed at the lowest possible dose and for the minimum duration. Non-medication based management strategies and the withdrawal of medication should always be considered at regular intervals. If the improvement of the PB is unsatisfactory, an attempt should be made to revisit and re-evaluate the formulation and the management plan.
Communication issues
The management plan should be communicated clearly to the person with ID and/or her/his family and carers and all other relevant professionals involved on a need-to-know basis. This process should be updated at regular intervals. Accessible format may be needed when communicating with adults with ID. The prescribing should be carried out according to the country’s legal frame-work and clearly documented in medical records.
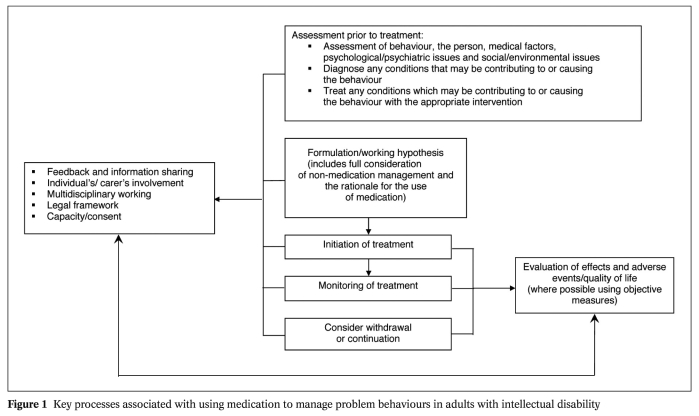
In Figure 1 we present a flow chart summarising the main activities involved in the process of prescribing and monitoring of its effect.
Figure 1.
General principles for prescribing psychotropic medications
Anyone prescribing medication to manage PBs in adults with ID should keep the following good practice points in mind:
– Medication should be used only in the best interests of the person.
– All non-medication management options should be considered, and medication should be seen as necessary under the circumstances, or alongside non-medication management.
– If possible, evidence to show that the medication is cost-effective should be taken into account.
– Information about which medications worked before and which did not should be noted.
– If medication used previously produced unacceptable adverse effects, the details should be noted.
– The effect of availability or non-availability of certain services and therapies on the treatment plan should be taken into account.
– Relevant local and national protocols and guidelines should be followed.
Once the decision to prescribe is taken, the following points should be followed:
– Ensure that the appropriate physical examinations and laboratory investigations are carried out at regular intervals.
– Explain to the person and/or her/his family or carers if the medication is being used outside its licensed indications. In this case, they should be told about the evidence that is available to demonstrate its effectiveness.
– Identify a key person who will ensure that medication is administered appropriately and communicate all changes to the relevant parties.
– If possible, provide the person and/or her/his family or carers with a copy of the agreed recommended treatment plan at the time of prescribing.
– As far as possible, there should be an objective way to assess outcomes, including adverse effects (where possible the use of standardized scales or the monitoring of the severity and frequency of the target behaviour is recommended) 34.
– Ensure there will be follow-up assessments for continued monitoring.
– As far as possible, one medication for the PB should be prescribed at a time.
– As a general rule, the medication should be used within the standard recommended dose range.
– A dose of medication above the maximum recommended should only be used in exceptional circumstances after full discussion with all the relevant stakeholders under appropriate safeguards and regular reviews.
– Start with a low dose and titrate the dose up slowly.
– Medication should be used at the lowest required dose for the minimum period of time necessary.
– Consideration for withdrawing medication and exploring non-medication management options should be ongoing.
Currently, it is not possible to recommend the type of medication for the treatment of specific PBs because there is no evidence to support such specificity 35.
Risks associated with prescribing medication in adults with ID and PB
Most medications carry a potential risk associated with adverse events. However, evidence is largely gathered from studies among patients who do not have ID. For example, current evidence shows that several newer antipsychotic medications may produce weight gain and some metabolic abnormalities related to glucose tolerance, lipid metabolism and prolactin secretion 36.
There is no good-quality evidence to either support or refute concerns that people with ID may be at greater risk of the adverse effects of medication than people from the general population who do not have ID. The shortage of good-quality evidence does not mean that medication is associated with an unacceptable risk specifically for adults with ID.
In view of the above, the following general points should be kept in mind:
– Discuss with the person and/or her/his family or carers about both common and serious adverse events related to the medication (where possible provide accessible information in writing).
– Advise what action should be taken if a serious adverse event occurs.
– All adverse events should be recorded properly.
– Once a medication is prescribed, the risk-benefit profile should be evaluated regularly, with particular emphasis on the person’s and her/his family or carers’ quality of life.
Withdrawing medication that has been prescribed for a long period
Studies of withdrawing medication show that, in some people with ID, the medication can be successfully withdrawn after a long period of use 37,38. In another group, the dose can be reduced, but total withdrawal is not possible. Lastly, there remain certain cases where medications cannot be reduced even after a very long period of use. Many factors affect the success of withdrawal of medication, including social and environmental factors such as the training and the attitude of care staff. However, on the basis of such evidence, it is not possible to recommend which medication to withdraw and the rate of withdrawal, but the following general recommendations are proposed:
– Try to stabilise the person’s PB on a minimum number of medications prescribed at the lowest possible dose.
– Withdraw one medication at a time.
– Withdraw medication slowly.
– If necessary, allow time (sometimes a few weeks) after withdrawing one medication and before starting to withdraw another.
FUTURE DIRECTIONS
There are plans to publish this guide in other languages as it has been done with previous guides produced by the WPA Section on Psychiatry of Intellectual Disabilities. Spanish and Italian translations will be available this year. The Section also plans to develop training materials on assessment of PBs among adults with ID, and to enhance links with other international organizations on this topic.
Acknowledgements
We are grateful to Nick Bouras for his support for the guide. We also acknowledge the support from the Italian Society of Intellectual Disability for the development of the Italian version of the guide, and from Juan Carlos García-Gutierrez and the Spanish Society of Scientific Research in Intellectual Disability (AEECRM) and Virginia Otón and the Spanish Dowńs Syndrome Federation (FESM) for the development of the Spanish version.
References
- 1.Salvador-Carulla L, Bertelli M. ‘Mental retardation’ or ‘intellectual disability’: time for a conceptual change. Psychopathology. 2008;41:10–16. doi: 10.1159/000109950. [DOI] [PubMed] [Google Scholar]
- 2.Cooper S-A, Smiley E, Morrison J. Prevalence of and associations with mental ill-health in adults with intellectual disabilities. Br J Psychiatry. 2007;190:27–35. doi: 10.1192/bjp.bp.106.022483. [DOI] [PubMed] [Google Scholar]
- 3.Einfeld SL, Piccinin AM, Mackinnon A. Psychopathology in young people with intellectual disability. JAMA. 2006;296:1981–1989. doi: 10.1001/jama.296.16.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Atlas on country resources in intellectual disabilities. Geneva: World Health Organization; 2007. [Google Scholar]
- 5.Deb S, Thomas M, Bright C. Mental disorder in adults with intellectual disability. 2: The rate of behaviour disor-ders among a community-based population aged between 16 and 64 years. J Intellect Disabil Res. 2001;45:506–514. doi: 10.1046/j.1365-2788.2001.00373.x. [DOI] [PubMed] [Google Scholar]
- 6.Smith S, Branford D, Collacott R. Prevalence and cluster typology of maladaptive behaviours in a geographically defined population of adults with learning disabilities. Br J Psychiatry. 1996;169:219–227. doi: 10.1192/bjp.169.2.219. [DOI] [PubMed] [Google Scholar]
- 7.Qureshi H, Alborz A. Epidemiology of challenging behaviour. Ment Hand Res. 1992;5:130–145. [Google Scholar]
- 8.Kiernan C, Reeves D, Hatton C. The HARC Challenging Behaviour Project. Report 1: Persistence and change in the challenging behaviour of people with a learning disability. Manchester: Hester Adrian Research Centre, University of Manchester; 1997. [Google Scholar]
- 9.Emerson E, Kiernan C, Alborz A. The prevalence of challenging behaviours: a total population study. Res Dev Disabil. 2001;22:77–93. doi: 10.1016/s0891-4222(00)00061-5. [DOI] [PubMed] [Google Scholar]
- 10.Lowe K, Allen D, Jones E. Challenging behaviours: prevalence and topographies. J Intellect Disabil Res. 2007;51:625–636. doi: 10.1111/j.1365-2788.2006.00948.x. [DOI] [PubMed] [Google Scholar]
- 11.Royal College of Psychiatrists. Diagnostic criteria for psychiatric disorders for use with adults with learning disabili-ties/mental retardation (DC-LD) London: Gaskell; 2001. [Google Scholar]
- 12.Cooper S-A, Smiley E, Allan LM. Adults with intellectual disabilities: prevalence, incidence and remission of ag-gressive behaviour and related factors. J Intellect Disabil Res. 2009;53:217–232. doi: 10.1111/j.1365-2788.2008.01127.x. [DOI] [PubMed] [Google Scholar]
- 13.Cooper S-A, Smiley E, Allan LM. Adults with intellectual disabilities: prevalence, incidence and remission of self-injurious behaviour, and related factors. J Intellect Disabil Res. 2009;53:200–216. doi: 10.1111/j.1365-2788.2008.01060.x. [DOI] [PubMed] [Google Scholar]
- 14.Clarke DJ, Kelley S, Thinn K. Psychotropic drugs and mental retardation: 1. Disabilities and the prescription of drugs for behaviour and for epilepsy in 3 residential settings. J Ment Defic Res. 1990;28:229–233. doi: 10.1111/j.1365-2788.1990.tb01549.x. [DOI] [PubMed] [Google Scholar]
- 15.Deb S, Fraser W. The use of medication in people with learning disability: towards more rational prescribing. Hum Psychopharmacol. 1994;9:259–272. [Google Scholar]
- 16.Spreat S, Conroy J, Jones J. Use of psychotropic medication in Oklahoma: a statewide survey. Am J Ment Retard. 1997;102:80–85. doi: 10.1352/0895-8017(1997)102<0080:UOPMIO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Emerson E, Kiernan C, Alborz A. Predicting the persistence of severe self-injurious behaviour. Res Dev Disabil. 2001;22:67–75. doi: 10.1016/s0891-4222(00)00062-7. [DOI] [PubMed] [Google Scholar]
- 18.Einfeld SL, Tonge BJ. Population prevalence of psychopathology in children and adolescents with intel-lectual disability: II. Epidemiological findings. J Intellect Disabil Res. 1996;40:99–109. doi: 10.1046/j.1365-2788.1996.768768.x. [DOI] [PubMed] [Google Scholar]
- 19.Green V, O’Reilly M, Itchon J. Persistence of early emerging aberrant behaviour in children with developmental disabilities. Res Dev Disabil. 2005;26:47–55. doi: 10.1016/j.ridd.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Totsika V, Toogood S, Hastings RP. Persistence of challenging behaviours in adults with intellectual disability over a period of 11 years. J Intellect Disabil Res. 2008;52:446–457. doi: 10.1111/j.1365-2788.2008.01046.x. [DOI] [PubMed] [Google Scholar]
- 21.Carr EG, Levin L, McConnachie G. Communication-based intervention for problem behavior: a user’s guide for producing positive change. Baltimore: Brookes; 1994. [Google Scholar]
- 22.Didden R, Duker PC, Korzilius H. Meta-analytic study on treatment effectiveness for problem behaviors with indi-viduals who have mental retardation. Am J Ment Retard. 1997;101:387–399. [PubMed] [Google Scholar]
- 23.Durand VM. Problem behaviour as communication. Behaviour Change. 1993;10:126–197. [Google Scholar]
- 24.Schroeder SR, Tessel RE, Loupe PS. Severe behavior problems among people with developmental disabilities. In: MacLean WE, Jr., editor. Ellis’ handbook of mental deficiency, psychological theory and research, 3rd ed. Mahwah: Lawrence Erlbaum; 1997. pp. 439–464. [Google Scholar]
- 25.Sigafoos J. Communication development and aberrant behaviour in children with develop-mental disabilities. Educ Train Ment Retard Dev Disabil. 2000;35:168–176. [Google Scholar]
- 26.McGillivray JA, McCabe MP. Pharmacological management of challenging behavior of individuals with intellec-tual disability. Res Dev Disabil. 2004;25:523–537. doi: 10.1016/j.ridd.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Deb S. The role of medication in the management of behaviour problems in people with learning disabilities. Advances in Mental Health and Learning Disabilities. 2007;1:26–31. [Google Scholar]
- 28.Tyrer P, Oliver-Africano PC, Ahmed Z. Risperidone, haloperidol, and placebo in the treatment of aggressive challenging behaviour in patients with intellectual disability: a randomised controlled trail. Lancet. 2008;371:57–63. doi: 10.1016/S0140-6736(08)60072-0. [DOI] [PubMed] [Google Scholar]
- 29.Aman M, Gharabawi G. Treatment of behaviour disorders in mental retardation: report on transitioning to atypical antipsychotics, with an emphasis on risperidone. J Clin Psychiatry. 2004;65:1197–1210. [PubMed] [Google Scholar]
- 30.Deb S, Clarke D, Unwin G. Using medication to manage behaviour problems among adults with a learning disabil-ity: Quick Reference Guide (QRG) 2006. www.ld-medication.bham.ac.uk. [Google Scholar]
- 31.Fletcher R, Loschen E, Stavrakaki C, editors. Diagnostic Manual-Intellectual Disability (DM-ID): a textbook of diagnosis of mental disorders in persons with intellectual disability. Washington: National Association for the Dually Diagnosed Press and American Psychi-atric Association; 2007. [Google Scholar]
- 32.National Institute for Health and Clinical Excellence. www.nice.org.uk.
- 33.Mezzich JE. Psychiatry for the Person: articulating medicine’s science and humanism. World Psychiatry. 2007;6:1–3. [PMC free article] [PubMed] [Google Scholar]
- 34.Unwin G, Deb S. Psychiatric and behavioural assessment scales for adults with learning disabili-ties. Advances in Mental Health in Learning Disability. 2008;2:37–45. [Google Scholar]
- 35.Unwin G, Deb S. Use of medication for the management of behaviour problems among adults with intellectual disabilities: a clinicians’ consensus survey. Am J Ment Retard. 2008;113:19–31. doi: 10.1352/06-034.1. [DOI] [PubMed] [Google Scholar]
- 36.Ucok A, Gaebel W. Side effects of atypical antipsychotics: a brief overview. World Psychiatry. 2008;7:58–62. doi: 10.1002/j.2051-5545.2008.tb00154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ahmed Z, Fraser W, Kerr MP. Reducing antipsychotic medication in people with a learning disability. Br J Psychiatry. 2000;178:42–46. doi: 10.1192/bjp.176.1.42. [DOI] [PubMed] [Google Scholar]
- 38.Branford D. Factors associated with the successful or unsuccessful withdrawal of antipsy-chotic drug therapy prescribed for people with learning disabilities. J Intellect Disabil Res. 1996;40:322–329. [PubMed] [Google Scholar]