Abstract
Objective
We examined the effectiveness of motivational interviewing (MI) on club drug use and risky sex in non-treatment-seeking men who have sex with men (MSM).
Method
MSM (N=150) were assessed and randomly assigned to four sessions of MI or an educational control intervention. Follow up occurred at quarterly intervals for 1 year. Primary outcomes were days of any club drug use and number of unsafe sex acts.
Results
On average, club drug use declined during follow up. A significant interaction effect showed that MI was associated with less club drug use during follow up compared to education, but only among participants with lower severity of drug dependence (p<.02; small to medium effect size). MI did not result in a significant reduction in risky sex relative to education.
Conclusions
The results support the use of MI targeting club drug use in at-risk or mildly dependent users not seeking treatment, but not in more severely dependent users. MI does not appear effective in reducing risky sexual behavior in this population.
Keywords: MSM, club drugs, sexual risk behavior, motivational interviewing
Introduction
Illicit drug use continues to be a major worldwide public health problem. In the United States, 8.3% of adults and adolescents report using illicit drugs in the last month and 2.8% met criteria for a drug use disorder in the past year (SAMHSA, 2007). Studies estimate that the annual costs of illicit drug use are in excess of $160 billion (Office of National Drug Control Policy, 2001). Importantly, illicit drug use disproportionately affects young people (SAMHSA, 2007). Over the last three decades studies have established the efficacy of behavioral interventions for treating drug use disorders (Carroll & Onken, 2005). One limitation of the existing drug use disorder treatment efficacy literature is that studies primarily have tested relatively intensive interventions among moderate to severely dependent individuals willing to adopt an abstinence goal.
Individuals willing to attend intensive treatment and adopt abstinence as a goal – often labeled high threshold treatment - are a distinct minority of those who require help for a drug use problem. For example, studies show that only 1 in 5 individuals with a substance use disorder (SUD) seek treatment and even among this group early drop out from treatment is high (SAMHSA, 2007). Experts have speculated that high treatment thresholds serve as a barrier to entry and engagement in treatment (Humphreys & Tucker 2002).
In addition, high threshold treatments appeal to individuals in advance stages of dependence. Emerging neurobiological research suggest that once established drug dependence takes on a chronic course (Kalivas & Volkow, 2005). This understanding lends new importance to examining the efficacy of low threshold interventions, especially in a secondary prevention context: intervening with at-risk individuals to forestall development of a chronic drug dependence illness with its devastating consequences. The primary aim of this study was to test the efficacy of a low threshold – brief and goal choice oriented – intervention for at-risk and dependent drug users at especially high risk for HIV transmission. Specifically, we tested the efficacy of Motivational Interviewing (MI; Miller & Rollnick, 1991) among recreational or dependent club drug using men-who-have-sex-with-men (MSM).
Drug Use and Drug Use Disorders among MSM
Although drug use is a widespread problem, MSM represent a distinct risk group (Cochran, Ackerman, Mays, & Ross, 2004). Estimates of drug use are as high as 19% among gay/bisexual men, with drug-related problems estimated at 5.7% (Cochran et al., 2004); both figures are substantially higher than population base rates for U.S. men generally (10.2% and 3.5%, respectively; SAMHSA, 2007). The last decade of research has suggested that drug use, particularly methamphetamine, has been growing among MSM (Parsons, Halkitis, & Bimbi, 2006) with use as much as ten times higher than in the general population (Colfax & Shoptaw, 2005).
Among MSM, the most commonly used recreational drugs are often collectively referred to as “club drugs.” These drugs, including cocaine, methamphetamine, methylenedioxymethamphetamine (MDMA, commonly known as ecstasy), gamma hydroxybutyric acid (GHB), and ketamine are often used in combination with each other, are a frequent feature of gay-oriented nightclubs, bars, and circuit parties, and are commonly used as an enhancement to sexual encounters for MSM (Halkitis & Parsons, 2002). Because drug use, and particularly use of stimulants such as methamphetamine and cocaine, can reduce inhibitions (including those for unsafe sex) and increase sexual drive, it has been consistently linked to HIV-associated risk among MSM (Colfax et al., 2005; Halkitis & Parsons, 2002).
Because of the increased prevalence of drug use and associated risk of HIV transmission developing effective interventions for drug using MSM has a high public health priority. Although rigorous studies are lacking, it is thought that requiring abstinence as a treatment goal may be a greater disincentive to help seeking among MSM than other groups because the gay community may have more tolerant social norms for drug use. Thus, it is believed that low threshold interventions may be especially attractive for MSM (McVinney, 2006).
Brief, Goal-Choice Interventions for Drug Use and Drug Use Disorders
The efficacy of brief, stand-alone interventions for problem drinkers, including those diagnosed with alcohol dependence has been clearly established (Bien, Miller, & Tonigan, 1993; Hettema, Steele, & Miller, 2005). With the exception of marijuana (Stephens, Roffman, & Curtin, 2000), a drug typically considered as having a low problem profile in comparison to other illicit drugs, relatively little is known about the efficacy of brief, stand-alone interventions for illicit drugs. Motivational interventions, a form of brief intervention, have been studied mostly in drug abusers seeking or in treatment often with mixed results (Saunders, Wilkinson, & Phillips, 1995; Stotts, Schmitz, Rhoades, & Grabowski, 2001; Donovan, Rosengren, Downey, Cox, & Sloan, 2001; Miller, Yahne, & Tonigan, 2003). These studies do not inform us about the efficacy of stand-alone interventions for drug users not interested in seeking standard treatment.
Two recent random controlled trials have examined the effects of brief interventions on illicit drug use. Bernstein and colleagues tested a one session motivational intervention for cocaine and heroin users identified in an outpatient medical clinic. They found the single session intervention was more effective on reducing drug use compared to an education pamphlet control (2005). Baker and colleagues (2005) tested a 2– 4 session behavioral intervention among amphetamine users in early stages of change. There was no main effect for the brief intervention compared to an education pamphlet control, however, both groups significantly reduced their amphetamine use.
Overall, surprisingly few studies have tested a low threshold approach to treating illicit drug use, other than marijuana. To some extent, a set of assumptions about drug use disorders similar to those held in earlier decades about alcohol use disorders may be in play. Specifically, a drug use disorder, especially drug dependence, is too severe to be treated effectively by low intensity interventions. In addition, adoption of moderation as a goal for illicit drug use, an important component of goal choice, is more controversial for illicit drugs as compared to alcohol.
HIV interventions for MSM
MSM continue to be at high-risk for HIV transmission, yet evidence that behavioral interventions can be effective with this subgroup is lacking. For example, the most recent large-scale HIV prevention behavioral intervention among MSM failed to find a significant effect in reducing HIV risk behaviors (Explore Study Team, 2004). Substance use, especially use of club drugs is widely considered a co-factor for HIV transmission among MSM. For example, HIV incidence in Project Explore was 4 times higher for men using club drugs or drinking heavily one or more times per week compared to those with no alcohol or drug use (Koblin et al., 2006). Although, the causal relationship between HIV and substance use remains unclear, an important hypothesis is that an intervention targeted at both reducing club drug use and HIV transmission might be effective among MSM using club drugs. To the best of our knowledge, only one prior study has reported on that effect. Shoptaw and colleagues (2005) found that methamphetamine dependent MSM entering an intensive abstinence-oriented program that combined drug treatment and HIV prevention reduced drug use and unsafe sex. This study helped to establish the efficacy of a high threshold intervention for methamphetamine dependent MSM.
Study Aims
We examined the efficacy of 4 sessions of MI focused on reducing club drug use and HIV risk behaviors for MSM not currently in SUD treatment. Recruitment efforts focused on identifying MSM across a broad range of ethnicity, HIV status, and drug use severity, including recreational drug users at-risk for development of drug dependence. Our recruitment strategy was informed by the data suggesting that even weekly club drug users are at heightened risk for HIV transmission (Koblin et al., 2006). We hypothesized that (A) MI would be more effective than a 4-session education control condition in reducing days of any club drug use across a 12 month follow-up; (B) the effect of MI would be moderated by dependence severity such that MI would be more effective for those with lower dependence severity; and (C) MI would be more effective at reducing the frequency of unsafe sex behaviors across a 12 month follow-up.
Method
Participants
Participants were 150 MSM recruited between April 2004 and December 2006 in New York City. Participants were eligible for the study if they were: male, ages 18–65, reported at least 5 occasions of club drug use in the prior 90 days, reported sexual contact with a non-primary male partner in the past 90 days, were not enrolled in drug treatment in the prior month, reported that club drug use was at least as significant a problem as alcohol or opiate use, were stably housed, and were not repeated enrollees in other HIV research studies.
Sample Characteristics
Table 1 presents descriptive data on the sample. Participants had a mean age of 37.8 (SD=8.8), and 72% had attended at least some college. The sample was ethnically diverse: white (35%) and African-American (32.7%), with a smaller number considering themselves Hispanic (14%) or of mixed or other race/ethnicity (15.4%). Participants reported an average of 23.4 (SD=16.6) days of any club drug use in the last 90 days, with cocaine/crack being the most commonly reported drug, followed by methamphetamine and MDMA. Use of ketamine and GHB was rare. Ninety participants (60%) met DSM-IV diagnostic criteria for dependence on one or more club drugs, and only 16% had ever enrolled in formal treatment for SUD. In terms of sexual risk behavior, participants reported a mean of 6.9 (SD=8.3) non-primary or casual sex partners in the prior 30 days, with 50% of participants reporting one or more occasions of unprotected anal sex, and 15% of all sexual encounters involving unprotected anal sex. Fifty-eight percent of the sample was HIV-positive at baseline.
Table 1.
Baseline characteristics of study sample (N = 150)
| Overall Sample | Treatment | Control Condition | ||||
|---|---|---|---|---|---|---|
| (N=150) | Condition (N=70) | (N=80) | ||||
| Variable | M or % | SD | M or % | SD | M or % | SD |
| Demographics | ||||||
| Age | 37.8 | 8.8 | 37.5 | 9.1 | 38.1 | 8.6 |
| Employment | ||||||
| Unemployed or not currently working | 56.2% | 58.1% | 54.1% | |||
| Education | ||||||
| Some college or more | 76.7% | 79.1% | 74.3% | |||
| Ethnicity | ||||||
| White | 36.3% | 31.9% | 40.2% | |||
| African-American | 33.6% | 30.6% | 36.4% | |||
| Hispanic | 14.4% | 15.9% | 13% | |||
| Other | 15.7% | 21.6% | 10.4% | |||
| HIV status | ||||||
| Positive | 59.5% | 58% | 61% | |||
| Days of club drug use in past 90-days | ||||||
| Any club drug use | 23.4 | 16.6 | 22.7 | 15.9 | 24.1 | 17.3 |
| Cocaine use | 12.8 | 16.2 | 12.7 | 15.7 | 12.6 | 16.8 |
| Methamphetamine use | 9.8 | 14.3 | 9.7 | 14.4 | 9.8 | 14.2 |
| Ecstasy Use | 7.1 | 11.6 | 6.2 | 8.6 | 7.7 | 13.7 |
| Ketamine Use | 0.9 | 3 | 0.4 | 1.2 | 1.3 | 3.9 |
| GHB Use | 1.1 | 3.7 | 1.2 | 4.5 | 0.9 | 2.9 |
| Drug dependence | ||||||
| SCID severity score | 5.44 | 4.95 | 6.0 | 5.1 | 4.95 | 4.8 |
| Cocaine dependence | 37.7% | 42.9% | 32.5% | |||
| Methamphetamine dependence | 31.8% | 38.6% | 26.3% | |||
| Ecstasy dependence | 17.2% | 18.6% | 16.3% | |||
| Alcohol and other drug use in past 90- days | ||||||
| Alcohol Use (% weekly binge drinkers) | 33.3% | 35.7% | 31.3% | |||
| Marijuana Use | 19.9 | 28.1 | 26.9 | 32.1 | 13.3 | 21.9 |
| Treatment History | ||||||
| Ever had substance abuse treatment | 16% | 18.6% | 13.8% | |||
| Substance abuse treatment in past 5-years | 11.3% | 14.3% | 8.8% | |||
| Sexual Risk Behaviors in past 30 days | ||||||
| Number of unprotected sex acts | 3.47 | 7.7 | 3.49 | 6.1 | 3.46 | 8.9 |
| High-risk unsafe sex acts | .37 | 2.1 | .33 | 1.5 | .41 | 2.5 |
| Number of Non-primary partners | 6.91 | .83 | 7.39 | 8.8 | 6.49 | 7.9 |
Note: There were no significant differences between conditions on all baseline covariates, except for marijuana use
Recruitment
Recruitment was accomplished in two phases, the first lasting from March 2004 through June 2005, and the second from June 2005 through December 2006. Throughout both phases of recruitment a multi-method approach designed to recruit from a diverse geographic area in New York City was utilized consisting of both active (direct outreach) and passive (print and online advertising) recruitment strategies. Phase 1 of recruitment involved direct enrollment of prospective participants into the randomized controlled trial. During this period, 54 men completed a baseline/screening assessment for the trial, and 34 met inclusion criteria and were randomized to treatment. As a consequence of this relatively low rate of recruitment, we modified recruitment procedures in an attempt to enhance enrollment by lowering the initial demand on participants.
Phase 2 involved a two-stage enrollment process. First, participants completed a brief self-report survey of club drug use and related psychosocial factors that also served as a screening assessment for the treatment trial. Eligible participants were then invited to participate in the treatment trial, and if willing, provided separate informed consent, followed by a baseline assessment. During Phase 2, 454 men completed the initial screening survey, of whom 257 were eligible for and 116 agreed to enroll in the clinical trial. Figure 1 presents a schematic of the recruitment and enrollment procedures throughout the trial. Participants were excluded for the following reasons: less than five days of any club drug use (12%), currently in drug treatment (13%), homeless or unstable housing (29%), did not have sex with a man other than a primary partner in last 90 days (20%), opiate use greater than use of any club drugs (24%), enrolled in other research studies (2%). We also examined differences in demographics or baseline frequency of club drug use or unsafe sex acts among eligible participants in Phase 2 who accepted (n=116) or refused (n=141) randomization using t tests and chi-square analyses. We found no significant differences (p<.05) in any variables tested suggesting the sample was representative of those deemed eligible on demographics and were not more nor less severe with regard to drug use or risky sex. Finally, we examined the geographic representation of the sample. The Phase 2 sample reported residing in 55 different zip codes in the NYC area with no more than 5% living in any one zip code.
Figure 1.
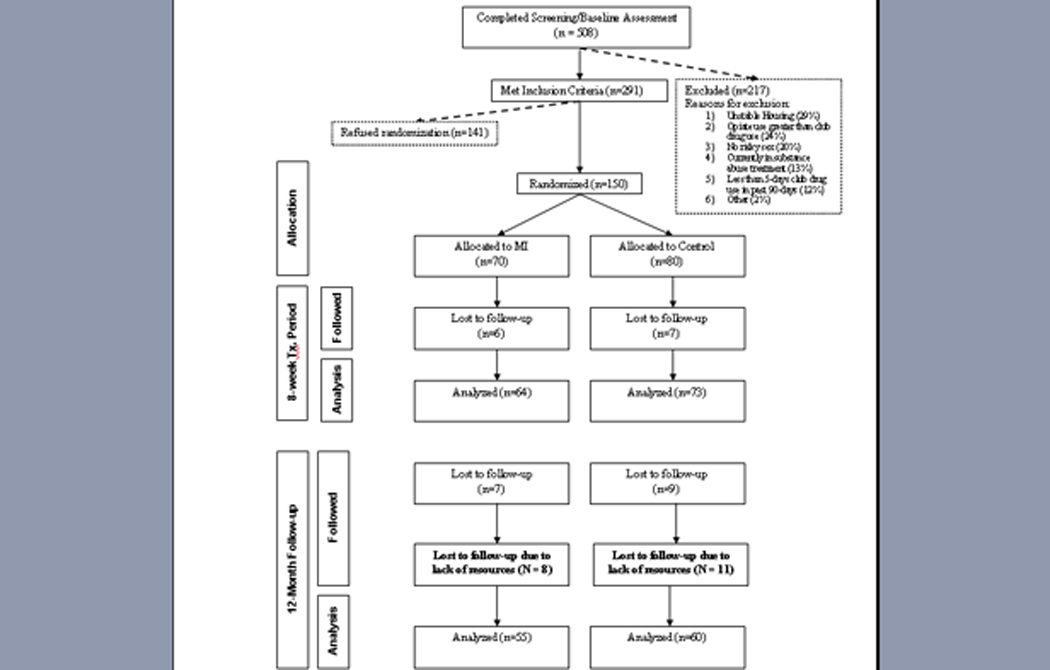
Participant Recruitment and Retention
Measures
Demographics & health
Several questions collected basic demographic information, as well as HIV status and history of other sexually transmitted infections. Participants reporting HIV-negative status provided a blood sample for confirmatory testing; HIV-positive participants were required to provide medical documentation of their HIV status.
Drug use & sexual behavior
Frequency of club drug use and sexual activity was collected using the Time-Line Follow-Back method (Sobell & Sobell, 1996). Participants reported on each occasion of club drug use over the past 90 days. Participants likewise reported on each occasion of sexual activity during the same interval, with detailed information on the type of partner (primary, casual, or anonymous); HIV status of partner (positive, negative, or unknown); type of sexual activity (oral, anal, manual; insertive or receptive); condom use; and whether sex ended with ejaculation inside the anus or mouth. In addition, frequency of drinking and use of marijuana was collected via standard self-report questions about patterns of use in the last 90 days.
Four outcome variables were constructed based on this interview: occasions of any club drug use, occasions of unprotected sex, occasions of highest-risk unsafe sex acts, and number of sexual partners. Days of any club drug use were calculated as the sum of all days on which the respondent reported use of any club drug during the past 90. Occasions of unprotected sex were calculated as the total number of sexual encounters during the last 30 days reported by the respondent involving either insertive or receptive anal sex without use of a condom, and without respect for the serostatus of the respondent or partner. Occasions of highest-risk sexual behavior during the last 30 days were defined according to the HIV status of the participant. For HIV-negative participants, the variable was defined as the number of occasions of unprotected, receptive anal sex with a partner of unknown or discordant serostatus; for HIV-positive participants, it was defined as the number of occasions of unprotected, insertive anal sex with a partner of unknown or discordant status. Thus, the second sexual risk variable captured occasions of sex that carried the highest risk of viral transmission (Vittinghoff et al., 1999). Number of partners was defined as the number of non-primary or casual partners with whom the participant reported having sex in the last 30 days. We used a 30 day assessment window for sexual behavior because of concerns about the reliability of recall for sexual behaviors across a 90 day period.
DSM-IV Dependence Symptoms
Symptoms of DSM-IV drug dependence were assessed at baseline using the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 2001). Participants reported on dependence symptoms for each club drug they reported using over the prior 90 days. This information was used to generate both DSM dependence diagnoses for each club drug, as well as to construct an overall dependence severity score, which constituted the sum of all DSM dependence symptoms across all 5 club drugs, and which had a possible range of 0–35.
Negative Consequences of Substance Use
The Short Inventory of Problems-Alcohol and Drug Version (SIP-AD) is a 15-item measure designed to assess the frequency of negative consequences related to alcohol and drug use in the last 90 days. The SIP-AD is a shortened version of the Inventory of Drug Use Consequences (INDUC-2R, Miller et al., 1995) and has shown adequate psychometric properties (Blanchard, Morgenstern, Morgan, Labouvie, & Bux, 2003). The SIP-AD was administered at baseline.
Treatments
Motivational Interviewing (MI)
MI was a 4 session individual treatment adapted from the Motivation Enhancement Therapy protocol (MET; Miller, Zweben, DiClemente & Rychtarik, 1994). The intervention was adapted for the present study in several ways. First, the intervention was adapted to address the dual, parallel problem behaviors of club drug use and high-risk sexual activity, typically by structuring the first session to address one behavior, and the second to address the other. Second, because normative data on club drug use and sexual behavior are relatively scarce, the intervention did not incorporate feedback on the individual’s ranking with respect to these behaviors relative to other groups; instead, feedback consisted largely of a summary of the participant’s self-reported drug use and sexual activity, and of his self-report of problems related to club drug use. Feedback was also not offered as a standard element of the intervention, but rather used when the therapist deemed it suitable. All other elements of MET protocol such as developing a change plan were delivered. MI was delivered in four, 1-hour sessions that could take place over as few as 4 or as many as 8 weeks.
Education Control
An education control condition was developed that consisted of four, hour-long videotapes developed specifically for the present study. On-camera interviews were conducted with eight gay men who were current/former drug users regarding their experiences. These interviews were edited into segments highlighting negative consequences of club drug use, the connection between club drug use and risky sex, and the role of club drugs in the social and sexual lives of gay men. These video segments were combined with segments pulled from previously developed educational videos regarding the dangers of cocaine use, the dangers of club drugs, and the ways in which club drug use negatively impacts the immune system, particularly for HIV positive men. A pair of ethnically diverse “hosts” was videotaped providing introductions and commentary on the various segments, such that four cohesive final videos were produced. Attention was taken to ensure that the videos were entertaining as well as informative, in order to ensure a credible attention-control intervention as well as to protect against attrition due to disinterest. Videos were presented in 4 one-hour sessions across 4–8 weeks.
Therapists
Therapists providing MI were 6 Masters or Doctoral-level psychologists. All therapists completed a minimum of 60 hours of training in MI techniques, and received both individual and group supervision on a weekly basis. Individual supervision was provided by the second author and a senior, Master’s level clinician who is a certified MI trainer. Individual supervision included regular review of session videotapes for direct feedback to clinicians.
Treatment integrity
Adherence to MI was evaluated using the Motivational Interviewing Treatment Integrity (MITI) Scale (Moyers, Martin, Manuel, Hendrickson, & Miller, 2005). The MITI consists of two components: global scores and behavior counts. Two global dimensions are rated: empathy and MI spirit. Behavior count requires the coder to tally instances of the counselor exhibiting MI-specific (e.g., open-ended questions, reflections) and non-MI-specific behaviors (e.g., closed questions). For the present study, 10% of session recordings were coded by independent coders.
Coders consisted of graduate and undergraduate psychology students. Inter-rater reliability was estimated through intraclass correlation coefficients for all pairs of coders (Fleiss & Shrout, 1978). The ICCs ranged from .620 to .977, with the majority of the correlations falling above .80. MITI scores indicated overall high adherence to MI principles and techniques, including a ‘Spirit’ rating of 6.13 (SD=.66) and an ‘Empathy’ rating of 6.31 (SD=.69); reflection to question ratio of 2.6 (SD=2.4); 64.1% open questions (SD=16.7); 66.5% complex reflections (SD=14.4); and an MI-adherent rating of 100% (SD=0). These scores meet or exceeded the criteria for “Competency” in MI skills as set out by the authors of the MITI in all cases but % open questions, where the level was intermediate between “Beginning Proficiency” and “Competency” (Moyers, Martin, Manuel, Miller, & Ernst, 2007).
Procedures
Recruitment
During both phases of recruitment, participants were instructed to call the study offices directly to complete a brief phone screening interview and to schedule an initial appointment. During Phase 1, information was collected during the phone screen to permit entry into the urn program for randomization. Participants in Phase 1 were scheduled for a baseline appointment and if eligible were randomized to treatment condition and provided their first counseling/education session during the same appointment. In Phase 2, participants were initially scheduled for the survey/screening interview. After completing the survey and upon confirmation of eligibility, participants were invited to enroll in the trial, and provided separate informed consent. They were scheduled for a separate baseline assessment for the treatment trial, and immediately after completing that assessment were randomized to treatment and attended their first intervention session during the same office visit. The strategy of scheduling the initial intervention session during the same visit as the baseline assessment was intended to ensure that participants would receive at least one intervention session.
Assessments
Participants first completed several self-report and individual clinical interviews to ensure study eligibility and to establish baseline levels of target behaviors. Self-report measures were administered on a computer via the Audio Computer Administered Self-Interview (ACASI). Studies have shown that ACASI increases the proportion of individuals admitting sexual behaviors and illicit drug use (Tourangeau & Smith, 1996). Interview assessments were conducted in a private office by interviewers who had received extensive didactic and experiential training. Blood and urine samples were also collected at baseline, for HIV serological testing of HIV negative participants and for confirmation of self-reported drug use, respectively. HIV testing was conducted using Oraquick rapid HIV testing; urine samples were tested for metabolites of major drug classes using the OnTrack Test Cup 5 by Roche Laboratories. Staff were extensively trained in HIV pre- and post-test counseling.
Randomization and Treatment
Participants were randomized using an URN randomization procedure, balancing on HIV status and days of club drug use. After assessment, participants were randomized to treatment and informed of their treatment condition, and then completed their first counseling/education session. Subsequent sessions were scheduled usually at weekly intervals; in all cases intervention sessions were completed within 8 weeks. Mean number of sessions attended was 1.9 (SD=1.6) in the experimental condition and 2.4 (SD=1.6) in the control condition (t(148) = 1.82, p<.10).
Follow-up
Participants were reinterviewed at intervals of 3 months from baseline, for up to 12 months. Follow up assessments largely mirrored those completed at baseline, with the exception that the SCID was not readminstered at these follow up points. Participants who were HIV-negative at baseline were re-tested at 12 months.
Attrition analyses
Of 150 individuals randomized to the study, follow-up data was available for 137 (91.3%), 136 (90.6%), 130 (86.7%), and 115 (76%) participants for the 3-, 6-, 9-, and 12-month follow-up periods, respectively. We had resources available to follow all participants only up to the 9-month follow-up. Consequently, 19 subjects were not contacted due to lack of resources at 12-month follow-up. To examine if differential attrition occurred, we conducted a series of analyses. First, we examined whether rates of follow-up differed by condition at each assessment point. Results indicated no significant differences. Second, baseline differences for socio-demographic, alcohol and any club drug use, dependence severity, and risky sex between those lost to follow-up and not lost to follow-up for the four follow-up periods were examined. No significant differences occurred between the groups at follow-up periods on all variables (all effect sizes < .25), except for baseline club drug use at the 12-month follow-up (p < .05). Participants lost to follow-up reported greater club drug use at baseline compared to those who had complete data. The next analysis examined baseline differences between the 19 cases at the 12-month, who were not followed due to lack of resources, and those followed up at 12-months. There were no significant baseline differences between these two groups.
Confirmation of Self Report
Self-reported drug use was confirmed by urine toxicology testing, using the OnTrack Test Cup 5 by Roche Laboratories, which screens for cocaine, methamphetamine, MDMA (as amphetamine and methamphetamine), and ketamine (as phencyclidine); toxicology testing for GHB is not possible with current technology. It should be noted that urine test kits results may be problematic because of cross reactivity for MDMA and methamphetamines increasing the likelihood of a false positive result. Self-reported use of each club drug was dichotomized to reflect either presence or absence of use at each time point. We then conducted cross-tabulations between toxicology tests and the dichotomized self-reports for each club drug category. Overall, the correspondence between self reported club drug use and urine toxicology reports (i.e., % agreement ranging from 97 to 100) was high, either indicating exact agreement, or that the subject reported greater use across each assessment period.
Data Analyses
Our primary analysis applied a Generalized Estimating Equations approach (Liang & Zeger, 1986), which is appropriate for longitudinal data because it allows for a within subject repeated measures examination of change over time as well as correction of variance estimates for correlated data within subject. The GEE analytical plan was comprised of a series of steps. The primary outcome for the first model was number of days of any club drug use during the prior 90 days measured at four time points (i.e., 3, 6, 9. 12-months). First, to account for factors that may confound an association between condition and club drug use, we undertook a process of model building in which we examined the association between sets of demographic factors (i.e., age, HIV status, race/ethnicity, most frequently used drug, employment), alcohol and marijuana use, baseline club drug use, and substance use severity. In step 2, covariates that had a marginal statistical association (p < 0.10) were retained for subsequent models. In step 3, we examined whether condition assignment was associated with club drug use. Next, we added time and a time X condition interaction term in the model. In the last step, we added a drug dependence severity by condition interaction where dependence severity was modeled as a continuous variable as described above. For these steps, club drug use was treated as a count variable. The data were first modeled as a Poisson distribution. However a histogram of club drug use showed large variances relative to the mean, and poor model fit parameters (e.g., Deviance, Scaled Deviance) indicated over-dispersed data. With over-dispersed data, the Poisson regression would under-estimate variances and inflate the probability of Type I errors whereas in such cases Negative Binomial models provide better estimates of variances and are more appropriate for inference testing. Therefore, the data were modeled using Negative Binomial regression models with log link function specifying an exchangeable working correlation structure, which provided a good fit to the data.
We used the same analytic plan for assessing HIV risk transmission. Unsafe sex (i.e., number of unprotected sex acts during the prior 30-days) was the specified outcome variable for these analyses and was measured at the same four time points. Overall, we did not find a significant main effect for condition or significant interactions for time X condition and drug dependence severity X condition for the risky sex outcome analyses. Consequently, additional post-hoc analyses were conducted to further understand this relationship. For both outcome models, all analyses were conducted with SAS 9.1 using the PROC GENMOD procedure.
Results
Baseline condition equivalence
Baseline characteristics of the sample have been described in Table 1. Briefly, both conditions did not differ significantly on select demographic, substance use, and risky sex measures at baseline except those in the MI condition reported greater marijuana use M = 26.9 (SD = 32.1) compared to those in the control condition M = 13.3 (SD = 21.9).
Club Drug Use Outcomes
Initial analyses indicated that the following covariates were retained in the model: race/ethnicity (B =−.263; z = −1.73, p < .08), HIV status (B = .366; z = 2.35, p < .01), baseline club drug use (B = .034; z = 9.22, p < .0001) and drug dependence (B = .029; z = 1.85, p < .06). Specifically, individuals who were either HIV negative, reported more club drug use at baseline, or had greater drug dependence were more likely to be using club drugs during follow-up. Non-Blacks, however, were associated with less club drug use during follow-up. These variables were included as covariates in subsequent analyses.
The test of main effects for condition was statistically significant (B = .284; z = 2.27, p < .02) indicating that participants assigned to the control condition, on average, were using more club drugs than those assigned to the MI condition during follow-up. In addition, time was significant in the model. Comparisons across the 3-month follow-up period (B = .378; z = 2.55, p < .01), 6-month follow-up period (B = .357; z = 2.47, p < .01), and the 9-month follow-up period (B = .285; z = 2.27, p < .02) indicated that participants reduced their club drug use across the course of the follow-up period up to 12-month follow-up. The condition X time (p > .38) interaction, however, was not significant indicating that condition differences did not vary across follow-up periods. Thus, the condition X time variable was removed from further models.
In our final model, there was a significant condition X drug dependence interaction (B = .065; z = −2.42, p < .02). See Table 2 for parameter estimates of the final model. The following variables remained significant in the model: HIV status, baseline club drug use, condition, drug dependence severity, and time. We then solved the regression equation to generate intercept and slope values for each condition1. The slope in the education condition was flat indicating days of club drug use did not vary much based on severity. By contrast the slope was positive in the MI condition indicating days of club drug use increased as dependence severity increased.
Table 2.
Parameter estimates for final GEE analysis modeling days of any club drug use
| Estimate | S.E. | 95% C.I.s | Z-score | p-value | ||
|---|---|---|---|---|---|---|
| Ethnicity | .211 | .149 | −.504 | .082 | −1.41 | .158 |
| HIV status | .348 | .151 | .053 | .644 | 2.31 | .021 |
| Baseline drug use | .035 | .004 | .028 | .043 | 9.60 | .0001 |
| Drug use severity | .058 | .019 | .203 | .095 | 3.02 | .003 |
| Condition | .610 | .196 | .225 | .995 | 3.11 | .002 |
| Time* | ||||||
| 90-day follow-up | .394 | .121 | .156 | .631 | 3.24 | .001 |
| 180-day follow-up | .304 | .111 | .088 | .521 | 2.75 | .010 |
| 270-day follow-up | .205 | .095 | .018 | .391 | 2.15 | .031 |
| Drug use severity X Condition | −.065 | .027 | −.118 | −.012 | −2.42 | .020 |
Note: The main effects analysis for time was based on comparisons between each time point and the 12-month time point.
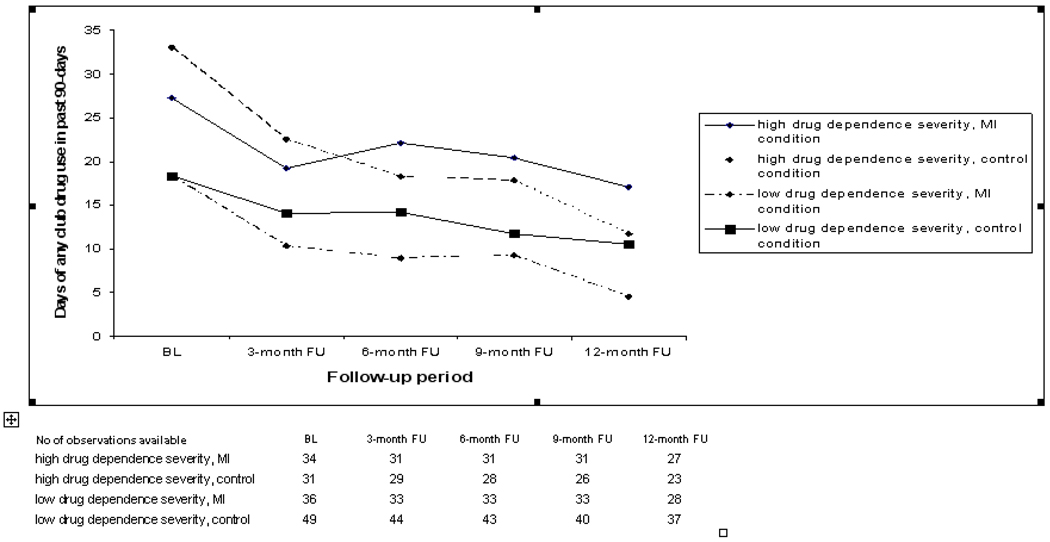
To further understand the condition X drug dependence severity interaction, we dichotomized the drug dependence variable into separate groups based on a mean split (M = 5.44). Individuals were categorized into either one of two groups: 1) low severity group; or 2) high severity group. Those whose drug severity scores were above the overall mean were placed into the high severity group and individuals below the overall mean were placed into the low severity group. Then, the drug severity group variable was combined with the condition variable to create four groups (e.g., high drug dependence severity, MI condition).
Figure 2 depicts overall club drug use means across the study period (i.e., baseline to 12-month follow-up) for the combined four groups. Overall, each group reduced their club drug use across time. Among those with low drug dependence severity, the MI condition reduced drug use more at each time point in comparison to the control condition. In order to further understand the magnitude of these differences, we computed effect size estimates using Cohen’s d (Cohen, 1988) at each time point between these two groups. Overall, the effect sizes were in the small to moderate range and were as follows: 3-month d = .23 (95% C.I. −.22 to .68), 6-month d = .37 (95% C.I. −.10 to .81), 9-month d = .17 (95% C.I. −.29 to .63) and 12-month d = .61 (95% C.I. .10 to 1.11). Among those with high drug dependence severity, MI condition appears to do better at 3-month follow-up. However, at later time points the direction of the effects were reversed with participants in the control condition reducing their club drug use more than those in MI
Figure 2.
Plot of interaction between treatment condition and club drug dependence severity status for days of any club drug use across the study period.
Primary Sex Behavior Outcomes
For the primary sex outcome analyses, the following covariates were significant in the model: baseline unsafe sex acts (B = .048; z = 5.44, p < .001) and drug dependence severity (B = −.055; z = −2.19, p < .03). These findings indicate that individuals who engage in greater number of unsafe sex acts at baseline were more likely to engage in unsafe sex acts during follow-up. In addition, greater drug dependence severity at baseline was associated with less unsafe sex during follow-up.
In contrast to the drug outcome analyses, the main effects analysis for condition was not significant (p > .75). In addition, both time (p > .50) and the time X condition interaction (p’s > .25) were not significant in the model. Since time was not significant, we examined if changes in unsafe sex acts occurred from baseline through follow-up. There were no significant changes in the number of unsafe sex acts across the study period. Further, since we found a significant condition X drug dependence interaction in the drug outcome analyses, we tested for this interaction which was not significant (p > .65).
Post-hoc Analyses of Sex Behavior Outcomes
Given that there were no changes in the number of unsafe sex acts during follow-up, we conducted three sets of post-hoc analyses. First, we examined two secondary sex behavior outcome variables: 1) number of highest-risk unsafe sex acts, as defined above and 2) the number of non-primary or casual sex partners. Highest risk unsafe sex acts was chosen because current social norms in the gay community indicate that MSM may engage in harm reduction strategies such as sero-sorting, but the community norm acknowledges highest risk unsafe sex acts as problematic. We first examined the frequency of highest risk unsafe sex acts across time, which was not frequent, and therefore determined that a GEE analysis would not be appropriate. Then, we aggregated frequency of highest risk sex acts across all follow-up points and used multiple regression techniques and a similar model building strategy to test for effects. Condition did not significantly predict outcome (p > .30).
Next we examined number of casual sex partners using the data analytic approach described above for the primary outcome analyses. There were no significant condition effects (all ps > .20) in any of the analyses. We also examined whether there was a significant reduction in number of casual sex partners from baseline through the 12 month outcome. Analyses showed a significant effect for time (p<.001) indicating that there was a reduction in number of casual sex partners. Examination of the means at baseline (M=6.91 SD=8.33) and 12 month outcome (M=2.67, SD=4.2) showed an effect size of d = .64.
In a third set of analyses, we examined the relationship between club drug use and unsafe sex acts (our primary sex behavior outcome measure) and number of casual partners (a secondary outcome measure) via time-lagged analysis of their relationship using GEE techniques. An underlying assumption was that MI would work to reduce risky sex by reducing club drug use. Club drug use was significantly related to unsafe sex acts at baseline (r =.26, p <.002). However, there were no significant relationships (all p’s > .20) that emerged as a part of this analysis during the outcome period. Club drug use was significantly related to number of casual partners at baseline (r =.20, p < .05). In addition, club drug use during the prior outcome period significantly predicted number of casual partners (p<.0001) in the subsequent outcome period, even after controlling for baseline risk behaviors and other baseline covariates. Overall, the absence of a condition effect on unsafe sex behaviors appeared consistent across three different outcome measures. However, the relationship between club drug use and risky sex differed depending on the outcome measure.
Secondary Analyses
In order to elucidate findings further, we examined whether dichotomizing the sample at the mean appeared to divide the sample into clinically meaningful low and high severity groups. Overall, among the low severity group (n=85), only two participants met five dependence criteria and about 75% met 1–4 dependence criteria for any one of the five drug classes. About 30.6 % met DSM-IV criteria for at least one club drug dependence diagnosis and 90.6% reported experiencing at least one major negative consequence of drug use in the last 90 days. By contrast, about 80% of the high severity group met 5 or more dependence criteria and about 50% met 6 or 7 criteria for a single club drug class. In addition, 50.7% of the high severity group met criteria for two or more club drug dependence diagnoses, whereas in the low severity group less than 2% (n=1) did so.
In addition, we examined whether those who attended more treatment had better outcomes and whether there was a significant treatment condition by treatment attendance interaction in favor of MI. Analyses were conducted using a similar analytic approach described above. Attendance did not predict either primary outcome nor were there any significant attendance by treatment condition interactions (all ps>.30). Thus, there were no significant effects of greater treatment attendance on outcome in either condition.
Contrary to prediction, Figure 2 indicates among the high severity group, participants in the control condition had less club drug use than those in MI at 6, 9, and especially at the 12 month follow-up. We examined whether results might be related to greater exposure to education versus MI or greater help seeking during follow-up. However, there were no significant differences in the high severity (or low severity) group on study treatment attendance nor attendance in SUD treatment at follow-up (all ps >.4). In addition, exposure to any formal SUD treatment during follow-up was low among all participants, with only 4% to 11% reporting even one SUD session during a 90 day follow-up period. Finally, because differences in favor of the control were most pronounced at 12 months, we examined the data for influential outliers. Although we did not find outliers, we did find that groups were especially small at the 12 month follow-up (high severity MI n=27, ED, n=23) because we did not have resources to follow 19 participants at 12 months and because there was more attrition among the high severity clients at this follow-up. In groups this small, the absence of a few high use clients could skew the results.
Discussion
Over the last three decades research on brief interventions, especially MI, has established the efficacy of secondary prevention for problem drinkers, even among those with mild-to-moderate alcohol dependence (Morgenstern et al., 2007). This research has helped broaden the base of alcohol treatment. Much less is known about the efficacy of brief interventions for problem drug use and drug use disorders. Even intervention studies of marijuana dependence have recruited people who wanted to quit rather than simply reduce their drug use (Stephens et al., 2000; Babor & The Marijuana Treatment Research Group, 2004). Thus, even with regard to marijuana little is known about whether brief interventions for individuals seeking to moderate use would be effective.
The current study is the first to demonstrate that MI is an effective stand-alone treatment for at-risk to mildly dependent club drug users, including individuals who were actively using cocaine and methamphetamines. In addition, the effects of MI were sustained across the 12 month follow-up period suggesting that even a brief intervention can have longer-term effects. A number of study features strengthen the internal validity of findings including random assignment, good treatment fidelity for MI, use of an apparently credible control condition that was as well attended as the MI treatment, a 12 month follow-up, and biological confirmation of self-reported drug use and HIV status. In addition, the sample was socio-demographically diverse, not restricted to MSM in any single neighborhood in New York, and those participating in the study did not differ significantly on demographics and problem severity from those who refused to participate. These sample features strengthen study external validity, although as noted below, it is unclear how representative the sample is of the target population of at-risk MSM in New York.
Dichotomizing the measure of dependence severity and plotting the arithmetic means of the four groups over time (Figure 2) helps to illustrate these findings. For example, among the low severity subgroup of participants those in MI experienced a threefold decrease in the frequency of club drug use from baseline to the 12 month follow-up (d=1.1). Effect size estimates for MI relative to the control condition are small-to-medium, similar to prior stand-alone studies of MI for alcohol (Hettema et al., 2005).
Equally important, MI’s positive effects relative to a control were attenuated as drug dependence increased. Figure 2 illustrates that among clients meeting greater than 5 DSM-IV dependence criteria, MI was not more effective than the control. The overall effect size of the reduction of frequency of drug use from baseline to 12 months for the high severity group was d=.61 or about half the reduction for the low severity group. Lower reduction in drug use in the high severity group when compared to the lower severity group would be consistent with the assumption that brief, self-management therapies are not effective, at least as a stand alone treatment, for clients with moderate to severe drug dependence.
HIV Risk Behavior Outcomes
Contrary to prediction, MI was not more effective than control in reducing unsafe sex behaviors. Previous efforts to reduce sexual risk behaviors among drug-using MSM using MI have yielded mixed results. For example, Naar-King and colleagues (2006) found that, compared to a wait-list control, a four session MI intervention targeting substance use, unprotected sex, and medication adherence among HIV+ youth (including MSM) significantly reduced unprotected sexual acts at three-months. However, no effects were found at later follow-ups (Naar-King et al., 2007). Mausbach, Semple, Strathdee, Zians, and Patterson (2007), in their 8-session MI-based intervention for HIV+ MSM methamphetamine users, found significant reductions in unprotected sex acts, but not on methamphetamine use. Although findings from Shoptaw and colleagues (2005) indicate a reduction in both drug use and risky sex among methamphetamine-dependent MSM, all participants were treatment seeking and the intervention was significantly more intensive and occurred in a different context – patients already engaged in a specialized SUD treatment program.
It is possible that the lack of impact on sexual risk with a four session intervention aimed at motivation may stem from the absence of significant intervention content aimed at skills building around safer sex and sexual risk reduction. The Information-Motivation-Behavioral Skills (IMB) model (Fisher & Fisher, 1993) suggests that information and motivation must be supplemented with skills-building activities in order to effectively promote behavior change. A recent meta-analysis of HIV prevention interventions for MSM (Johnson et al., 2008) found those behavioral interventions that included skills building appeared to be somewhat more effective for this population. In addition, it is important to note that popular theoretical models focused on HIV risk reduction (e.g., IMB, theory of planned behavior) often focus on peer norms as a critical factor related to behavior change. Peer norms regarding sexual risk reduction in MSM communities are complicated by the many harm reduction techniques – such as serosorting, strategic positioning, and withdrawal - currently practiced (Grov et al., 2007; Parsons et al., 2005). As a result, the inconsistency of peer norms within the various MSM communities suggests that new, or at least modified, theoretical approaches be considered.
Relationship between Club Drug Use and Risky Sex
One underlying hypothesis that guided this study was that use of club drugs reduces inhibitions and thus is a factor in facilitating unsafe sex among MSM. Thus, reduction of club drug use should result in a reduction of risky sex. Interestingly, the relationship between club drug use and risky sex during the outcome period differed across two measures of risky sex. Unsafe sex acts, our primary outcome measure, showed no significant reduction and was not related to reduction in club drub use. By contrast, number of casual partners was reduced and this reduction was significantly associated with a reduction in club drug use. One possible explanation is that a reduction in club drug use, primarily stimulant drugs in our sample, led to a reduction in casual sex encounters. However, use of condoms was not affected by level of club drug use.
The relationship between club drug use and HIV sexual risk behaviors may be more complex than originally hypothesized. For example, it has been shown recently that despite the emphasis on methamphetamine as driving sexual risk behaviors among MSM. many MSM methamphetamine users are able to engage in safer sex, and the majority of MSM in New York City who report unprotected anal sex are not methamphetamine users (Grov, Parsons, & Bimbi, 2008). Clearly, more research needs to be conducted to better understand the nature of the relationship between club drugs and risky sex among MSM.
Limitations
Findings are limited to an urban sample of MSM not seeking help nor being coerced by the criminal justice or other social service systems. Studies have found that MI when added to intensive treatment is effective, even for moderate to severely dependent drug users seeking help (Hettema et al., 2005). In addition, sampling strategies were not designed to recruit a representative sample of at-risk MSM. Although the recruitment approach did engage in active recruitment strategies and identified a diverse sample, it is unclear how representative this sample is of the target population. In addition, by design we examined a sample of mixed drug users. Although the primary drug of choice was some form of stimulant, either cocaine or methamphetamine, caution is needed in generalizing to other samples. Finally, it should be noted that our approach to illustrating the GEE results (e.g., Figure 2) is imprecise. For example, arithmetic means of raw data rather than negative binomial distributions are represented. Thus, effect size estimates are presented for illustrative purposes only and should be interpreted with caution. Similarly, it should be noted that Figure 2 provides an illustration of the treatment condition by severity interaction and should not be interpreted as providing a precise threshold beyond which MI is or is not effective. Currently, it appears that MI is likely to be effective for at-risk users and those with mild dependence, but not moderate or severe dependence. More research is needed to identify a precise severity threshold.
Implication for Research and Health Care Policy
This study adds to a large body of research indicating stand-alone motivational interviewing and other low threshold self-management interventions (Baer, Kivlahan, Blume, McKnight, & Marlatt, 2001) can be effective in treating SUDs among individuals at risk to develop chronic substance dependence disorders. We now know that the least expensive and most effective way to treat chronic disorders is to prevent the problem from crossing the threshold to chronic illness (Wagner, Austin & Van Korff, 1996). More research is needed to improve access and effectiveness of early or secondary prevention interventions for drug use disorders. Among the most important research questions is understanding the limits of effectiveness of brief interventions among those with drug dependence. More research is also needed to understand factors that promote individuals in early stages of drug use disorders to seek help. For example, it is important to note that in this and our earlier study (Morgenstern et al., 2007), the majority of MSM with SUD who contacted the study declined to engage in the no cost, low threshold intervention.
Substantially more rigorous research is also needed to test the efficacy of interventions to reduce HIV risk among alcohol and drug users, especially MSM. Given the public health importance of HIV prevention and its relation to substance use, it is surprising how few trials have reported findings among MSM populations. The Shoptaw et al. findings (2005) suggest that an intensive intervention delivered to a population motivated to abstain can be effective in reducing drug use and risky sex among MSM. However, results from the current study suggest those findings may not generalize to broader public health contexts beyond those seeking intensive drug abuse treatment and that interventions that simply reduce drug use may not reduce HIV risk behaviors.
Conclusion
Motivational interviewing significantly reduced club drug use among at-risk and mildly dependent club drug users when compared to an education control. Treatment effects were sustained across a 12 month follow-up. MI was not effective in reducing use among individuals with moderate to severe drug dependence. Contrary to the study hypothesis, MI was not effective in reducing HIV risk behaviors relative to an education control.
Appendix
|
PAPER SECTION And topic |
Item | Descriptor | Reported On Page # |
|---|---|---|---|
| TITLE & ABSTRACT | 1 | How participants were allocated to interventions (e.g., "random allocation", "randomized", or "randomly assigned"). | 1–2 |
|
INTRODUCTION Background |
2 | Scientific background and explanation of rationale. | 3–7 |
|
METHODS Participants |
3 | Eligibility criteria for participants and the settings and locations where the data were collected. | 7, 14 |
| Interventions | 4 | Precise details of the interventions intended for each group and how and when they were actually administered. | 10–12 |
| Objectives | 5 | Specific objectives and hypotheses. | 7 |
| Outcomes | 6 | Clearly defined primary and secondary outcome measures and, when applicable, any methods used to enhance the quality measurements (e.g., multiple observations, training of assessors). | 9–10 |
| Sample size | 7 | How sample size was determined and, when applicable, explanation of any interim analyses and stopping rules. | 7 |
| Randomization-- Sequence generation |
8 | Method used to generate the random allocation sequence, including details of any restrictions (e.g., blocking, stratification) | 13 |
| Randomization -- Allocation concealment |
9 | Method used to implement the random allocation sequence (e.g., numbered containers or central telephone), clarifying whether the sequence was concealed until interventions were assigned. | 13 |
| Randomization -- Implementation |
10 | Who generated the allocation sequence, who enrolled participants, and who assigned participants to their groups. | 12–13 |
| Blinding (masking) | 11 | Whether or not participants, those administering the interventions, and those assessing the outcomes were blinded to group assignment. If done, how the success of blinding was evaluated. | 12–14 |
| Statistical methods |
12 | Statistical methods used to compare groups for primary outcome(s); Methods for additional analyses, such as subgroup analyses and adjusted analyses. | 15–16 |
|
RESULTS Participant flow |
13 | Flow of participants through each stage (a diagram is strongly recommended). Specifically, for each group report the numbers of participants randomly assigned, receiving intended treatment, completing the study protocol, and analyzed for the primary outcome. Describe protocol deviations from study as planned, together with reasons. | 9 & Figure 1 |
| Recruitment | 14 | Dates defining the periods of recruitment and follow-up. | 9 |
| Baseline data |
15 | Baseline demographic and clinical characteristics of each group. | 8 & Table 1 |
| Numbers analyzed |
16 | Number of participants (denominator) in each group included in each analysis and whether the analysis was by "intention-to-treat". State the results in absolute numbers when feasible (e.g., 10/20, not 50%). | 14 |
| Outcomes and estimation |
17 | For each primary and secondary outcome, a summary of results for each group, and the estimated effect size and its precision (e.g., 95% confidence interval). | 17–23 |
| Ancillary analyses |
18 | Address multiplicity by reporting any other analyses performed, including subgroup analyses and adjusted analyses, indicating those pre-specified and those exploratory. | 21–23 |
| Adverse events |
19 | All important adverse events or side effects in each intervention group. | n/a |
|
DISCUSSION Interpretation |
20 | Interpretation of the results, taking into account study hypotheses, sources of potential bias or imprecision and the dangers associated with multiplicity of analyses and outcomes. | 21–25 |
| Generalizability | 21 | Generalizability (external validity) of the trial findings. | 23–29 |
| Overall evidence |
22 | General interpretation of the results in the context of current evidence. | 23–29 |
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/ccp.
Because the outcome was modeled as a negative binomial we determined a graph of X and Y would not be informative. The regression equations for each condition are: ED: Y=1.6 + −.01X and MI: Y=.96 + .06X.
Contributor Information
Jon Morgenstern, Research Foundation for Mental Hygiene & Columbia University College of Physicians & Surgeons.
Donald A. Bux, Jr., Research Foundation for Mental Hygiene & Columbia University College of Physicians & Surgeons
Jeffrey Parsons, Hunter College, City University of New York.
Brett T. Hagman, Research Foundation for Mental Hygiene & Columbia University College of Physicians & Surgeons
Milton Wainberg, Research Foundation for Mental Hygiene & Columbia University College of Physicians & Surgeons.
Thomas Irwin, Research Foundation for Mental Hygiene & Columbia University College of Physicians & Surgeons.
References
- The Marijuana Treatment Research Group. Babor TF. Brief treatments for cannabis dependence: Findings from a randomized multisite trial. Journal of Consulting and Clinical Psychology. 2004;72(3):455–466. doi: 10.1037/0022-006X.72.3.455. [DOI] [PubMed] [Google Scholar]
- Baer JS, Kivlahan DR, Blume AW, McKnight GA, Marlatt A. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. American Journal of Public Health. 2001;97(8):1310–1316. doi: 10.2105/ajph.91.8.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker A, Lee NK, Claire M, Lewin TJ, Grant T, Pohlman S, et al. Brief cognitive behavioural interventions for regular amphetamine users: A step in the right direction. Addiction. 2005;100(3):367–378. doi: 10.1111/j.1360-0443.2005.01002.x. [DOI] [PubMed] [Google Scholar]
- Bernstein J, Bernstein E, Tassiopoulos K, Heeren T, Levenson S, Hingson R. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug and Alcohol Dependence. 2005;77(1):49–59. doi: 10.1016/j.drugalcdep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: A review. Addiction. 1993;88(3):315–335. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- Blanchard KA, Morgenstern J, Labouvie E, Morgan T, Bux DA. Assessing consequences of substance use: Psychometric properties of the inventory of drug use consequences (InDUC-2R) Psychology of Addictive Behaviors. 2003;17:328–331. doi: 10.1037/0893-164X.17.4.328. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Onken LS. Behavioral therapies for drug abuse. American Journal of Psychiatry. 2005;162(8):1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Ackerman D, Mays VM, Ross MW. Prevalence of non-medical drug use and dependence among homosexually active men and women in the US population. Addiction. 2004;99:989–998. doi: 10.1111/j.1360-0443.2004.00759.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin BA, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrate), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. Journal of Urban Health. 2005;82:62–70. doi: 10.1093/jurban/jti025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colfax G, Shoptaw S. The methamphetamine epidemic: implications for HIV prevention and treatment. Current HIV/AIDS report. 2005;2(4):194–199. doi: 10.1007/s11904-005-0016-4. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Rosengren DB, Downey L, Cox GB, Sloan KL. Attrition prevention with individuals awaiting publicly funded drug treatment. Addiction. 2001;96(8):1149–1160. doi: 10.1046/j.1360-0443.2001.96811498.x. [DOI] [PubMed] [Google Scholar]
- The EXPLORE Study Team. Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: The EXPLORE randomized controlled study. Lancet. 2004;364:41–50. doi: 10.1016/S0140-6736(04)16588-4. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, Research version, Patent edition with psychotic screen (SCID-I/PW/PSY SCREEN) New York: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- Fisher WA, Fisher JD. A general social psychological model for changing AIDS risk behavior. In: Pryor J, Reeder G, editors. The social psychology of HIV infection. Hillsdale, NJ: Erlbaum; 1993. pp. 127–153. [Google Scholar]
- Fleiss JL, Shrout PE. Approximate interval estimation for a certain intraclass correlation coefficient. Psychometrika. 1978;43(2):259–262. [Google Scholar]
- Grov C, Parsons JT, Bimbi DS. In the shadows of a prevention campaign: Sexual risks in the absence of crystal methamphetamine. AIDS Education and Prevention. 2008;20:42–55. doi: 10.1521/aeap.2008.20.1.42. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT. Recreational drug use and HIV-risk sexual behavior among men frequenting gay social venues. Journal of Gay & Lesbian Social Services: Issues in Practice, Policy & Research. 2002;14(4):19–38. [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Tucker JA. Toward more responsive and effective intervention systems for alcohol-related problems. Addiction. 2002;97:126–132. doi: 10.1046/j.1360-0443.2002.00004.x. [DOI] [PubMed] [Google Scholar]
- Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, Malow R, McClellan WM. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database of Systematic Reviews. 2008;(Issue 3) doi: 10.1002/14651858.CD001230.pub2. Art. No.: CD001230. [DOI] [PubMed] [Google Scholar]
- Kalivas PW, Volkow ND. The neural basis of addiction: A pathology of motivation and choice. American Journal of Psychiatry. 2005;162(8):1403–1413. doi: 10.1176/appi.ajp.162.8.1403. [DOI] [PubMed] [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, et al. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20(5):731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Mausbach BT, Semple SJ, Strathdee SA, Zians J, Patterson TL. Efficacy of a behavioral intervention for increasing safer sex behaviors in HIV-negative, heterosexual methamphetamine users: Results from the Fast-Lane Study. Annals of Behavioral Medicine. 2007;34(3):263–274. doi: 10.1007/BF02874551. [DOI] [PubMed] [Google Scholar]
- McVinney LD. Harm reduction, crystal methamphetamine, and gay men. Journal of Gay & Lesbian Psychotherapy. 2006;10:159–169. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York, NY: Guilford Press; 1991. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. (Project MATCH Monograph Series, Vol. 4) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse. Test manual. [Google Scholar]
- Miller WR, Yahne CE, Tonigan JS. Motivational interviewing in drug abuse services: A randomized trial. Journal of Consulting and Clinical Psychology. 2003;71:754–763. doi: 10.1037/0022-006x.71.4.754. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Project MATCH monograph series, Volume 2 (DHHS Publication No, 94-3723) Rockville, MD: NIAAA; 1994. Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. [Google Scholar]
- Morgenstern J, Irwin TW, Wainberg ML, Parsons JT, Muench F, Bux DA, Jr, et al. A Randomized Controlled Trial of Goal Choice Interventions for Alcohol Use Disorders Among Men Who Have Sex With Men. Journal of Consulting and Clinical Psychology. 2007;75(1):72–84. doi: 10.1037/0022-006X.75.1.72. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28(1):19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Revised Global Scales: Motivational Interviewing Treatment Integrity 3.0 (MITI 3.0) Albuquerque, NM: University of New Mexico, Center on Alcoholism, Substance Abuse, and Addictions (CASAA); 2007. [Google Scholar]
- Naar-King S, Green M, Wright K, Outlaw A, Wang B, Liu H. Ancillary services and retention of youth in HIV care. AIDS Care. 2007;19(2):248–251. doi: 10.1080/09540120600726958. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Wright K, Parsons JT, Frey M, Templin T, Lam P, et al. Healthy choices: Motivational enhancement therapy for health risk behaviors in HIV-positive youth. AIDS Education and Prevention. 2006;18(1):1–11. doi: 10.1521/aeap.2006.18.1.1. [DOI] [PubMed] [Google Scholar]
- Office of National Drug Control Policy. (Publication No. NCJ-190636) Washington, D.C: Executive Office of the President; 2001. The Economic Costs of Drug Abuse in the United States, 1992-1998. [Google Scholar]
- Parsons JT, Halkitis PN, Bimbi DS. Club Drug Use Among Young Adults Frequenting Dance Clubs and Other Social Venues in New York City. Journal of Child & Adolescent Substance Abuse. 2006;15(3):1–14. [Google Scholar]
- Parsons JT, Schrimshaw EW, Wolitski RJ, Halkitis PN, Purcell DW, Hoff CC, Gomez C. Sexual harm reduction practices of HIV seropositive gay and bisexual men: Serosorting, strategic positioning, and withdrawal before ejaculation. AIDS. 2005;19(S1):13–26. doi: 10.1097/01.aids.0000167348.15750.9a. [DOI] [PubMed] [Google Scholar]
- Saunders B, Wilkinson C, Phillips M. The impact of a brief motivational intervention with opiate users attending a methadone programme. Addiction. 1995;90(3):415–424. doi: 10.1046/j.1360-0443.1995.90341510.x. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Reback CJ, Peck JA, Yang X, Rotheram-Fuller E, Larkins S, et al. Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug and Alcohol Dependence. 2005;78(2):125–134. doi: 10.1016/j.drugalcdep.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-Back User's Guide: A Calendar Method for Assessing Alcohol and Drug Use. Toronto, Canada: Addition Research Foundation; 1996. [Google Scholar]
- Stephens R, Roffman R, Curtin L. Comparison of extended versus brief treatment for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68(5):898–908. [PubMed] [Google Scholar]
- Stotts AL, Schmitz JM, Rhoades HM, Grabowski HG. Motivational interviewing with cocaine-dependent patients: A pilot study. Journal of Consulting and Clinical Psychology. 2001;69:858–862. doi: 10.1037//0022-006x.69.5.858. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (NSDUH Series H-32, DHHS Publication No. SMA 07-4293) Rockville, MD: Office of Applied Studies, NSDUH Series; 2007. Results from the 2006 national survey on drug use and health: National findings. [Google Scholar]
- Tourangeau R, Smith T. Asking sensitive questions: The impact of data collection mode, question format, and question content. Public Opinion Quarterly. 1996;60(2):275–304. [Google Scholar]
- Vittinghoff E, Douglas J, Judson F, McKirnan D, MacQueen K, Buchbinder S. Per-contact risk of human immunodeficiency virus transmission between male sexual partners. American Journal of Epidemiology. 1999;150:427–431. doi: 10.1093/oxfordjournals.aje.a010003. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. The Milbank Quarterly. 1996;74:511–544. [PubMed] [Google Scholar]