Abstract
The current review uses a developmental perspective to examine processes that may underlie and partially account for the association between anxiety disorders and disruptive behavior disorders among children and adolescents. We propose that one way to understand development of comorbid anxiety and disruptive behavior disorders is to examine symptoms that are precursors for or part of these syndromes, such as anxious symptoms and reactive aggression. We use a framework that considers these issues first at the syndrome or disorder level (e.g., anxiety disorders, disruptive behavior disorders), then at the symptom level (e.g., anxious symptoms, reactive aggression), and finally at the risk factor level (e.g., factors associated with anxious symptoms and/or reactive aggression). We apply various frameworks that have been put forth for understanding comorbidity of psychological syndromes to the co-occurrence of anxiety and disruptive behavior disorders and to the co-occurrence of reactive aggression and anxious symptoms where possible. We then identify gaps in the literature with regard to anxiety and reactive aggression, as well as anxiety and disruptive behavior disorders more generally. Finally, we provide a conceptual model describing how the relation of anxiety and reactive aggression may develop into clinically identifiable, comorbid anxiety and disruptive behavior disorders.
Comorbidity, or the co-occurrence of psychological disorders, is relatively common among childhood psychological conditions and consequently is a critical area of research inquiry for child and adolescent psychopathology (Angold, Costello, & Erkanli, 1999a; Caron & Rutter, 1991; Kendall & Clarkin, 1992; Klein & Riso, 1993). Consistent with the noted importance of this issue, research to date has examined comorbid externalizing disorders (e.g., attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD)), comorbid internalizing disorders (e.g., generalized anxiety disorder (GAD) and major depressive disorder (MDD)), and comorbid externalizing and internalizing disorders (e.g., conduct disorder (CD) and MDD) (for a review, see Angold et al., 1999a). Nevertheless, there is a relative paucity of research examining the association between anxiety and disruptive behavior disorders, despite the fact that such comorbidity has important clinical and nosological implications (Drabick, Gadow, & Loney, 2008; Flannery-Schroeder, Suveg, Safford, Kendall, & Webb, 2004; Garland & Garland, 2001; Russo & Beidel, 1994).
Reasons for the dearth of literature involving co-occurring anxiety and disruptive behavior disorders are unclear. One possible reason is that positive associations between anxiety and externalizing behaviors seem counterintuitive and are difficult to reconcile conceptually. For instance, earlier conceptualizations of individuals with conduct problems and antisocial behavior included a lack of fearful inhibition (Gray, 1982) and/or absence of anxiety (Cleckley, 1982), which would suggest that anxiety and disruptive behavior disorders would be unlikely to co-occur. Yet numerous studies have noted that ADHD, ODD, and CD significantly co-occur with anxiety disorders (e.g., GAD and separation anxiety disorder (SAD)) among children (American Psychiatric Association, 2000; Fleitlich-Bilyk & Goodman, 2004; Ford, Goodman, & Meltzer, 2003; Marmorstein, 2007). Moreover, such co-occurrence is three times more likely than expected given documented base rates among community-based samples (Angold et al., 1999a). Rates of comorbidity within clinical settings are also high. Among children attending an anxiety disorders clinic, approximately 9% met criteria for ODD and approximately 15% met criteria for ADHD (Kendall, Brady, & Verduin, 2001). Children and adolescents with SAD that persisted over an 18-month period exhibited a higher prevalence of ODD and more impairment associated with ADHD symptoms than children who met criteria for SAD only at the initial wave of data collection (Foley, Pickles, Maes, Silberg, & Eaves, 2004). Similarly, 20%–63% of children with GAD also meet criteria for ODD or CD (Garland & Garland, 2001; Masi et al., 2004). However, research comparing the likelihood that specific disruptive behavior disorders co-occur with anxiety disorders suggests that children with ODD are at greater risk for comorbid anxiety disorders, as compared to those with CD (Maughan, Rowe, Messer, Goodman, & Meltzer, 2004).
To understand why anxiety and disruptive behavior disorders co-occur, we examine comorbid anxiety and disruptive behavior disorders using several lines of inquiry in this review. We propose that one way to understand co-occurring anxiety and disruptive behavior disorders is to examine precursors or earlier manifestations of these conditions, which could provide an important adjunct to research that examines the co-occurrence of diagnostic syndromes. We also suggest that examining the relations between anxiety symptoms and reactive aggression, as well as risk factors that may be associated with both anxiety symptoms and reactive aggression, could be useful for understanding the precursors of comorbid anxiety and disruptive behavior disorders. Among children, reactive aggression (also called affective, defensive, or “hot blooded” aggression) refers to angry, explosive, and often emotionally dysregulated responses to perceived offenses or frustrations (Card & Little, 2006; Dodge, 1991). Reactive aggression can be self- or other-directed, accompanied by anger or fear, and characterized by high levels of arousal (Vitiello & Stoff, 1997). Reactive aggression can be contrasted with proactive aggression, which does not require provocation or anger, and involves deliberate acts directed toward obtaining desired goals (Dodge, 1991).
We focus on anxiety symptoms and reactive aggression for several reasons. First, anxiety symptoms and reactive aggression consistently are related among children (Card & Little, 2006; Marsee, Weems, & Taylor, 2007; Vitaro, Brendgen, & Tremblay, 2002). For instance, reactively aggressive children and adolescents are rated as more anxious than their proactively aggressive and non-aggressive counterparts (Vitaro et al., 2002). Second, reactive aggression is associated with each of the disruptive behavior disorders in childhood (ADHD, ODD, and CD; Dodge, Lochman, Harnish, Bates, & Pettit, 1997; Waschbusch et al., 2002; Waschbusch, Willoughby, & Pelham, 1998), which suggests that reactive aggression may be an important component or correlate of disruptive behavior disorders. Proactive aggression also co-occurs with these disruptive behavior disorders. However, it is less likely that proactive aggression, which is associated with callous and unemotional traits (Frick, Cornell, Barry, Bodin, & Dane, 2003; Frick, Lilienfeld, Ellis, Loney, & Silverthorn, 1999; Marsee & Frick, 2007), is associated with anxiety symptoms, particularly given that callous and unemotional traits are negatively associated with anxiety symptoms (Frick et al., 1999). Third, anxiety symptoms and reactive aggression have similar child-specific correlates, such as difficult temperamental styles (Ortiz & del Barrio Gandara, 2006; Shaw, Keenan, Vondra, Delliquadri, & Giovannelli, 1997); autonomic hyperarousal (Hubbard et al., 2002; van Goozen et al., 1998); and hypervigilance to threatening stimuli (Beck & Emery, 1985; Dodge & Coie, 1987; Ingram & Kendall, 1985). These findings suggest that the child-specific correlates of, or processes underlying, the co-occurrence of anxious symptoms and reactive aggression may partly explain the presence of comorbid anxiety disorders and disruptive behavior disorders among children.
Given the relative paucity of research evaluating co-occurring anxiety and disruptive behavior disorders, we used a more broad and inclusive approach for identifying relevant studies. The following disruptive behavior disorders are included in the current review: ADHD, which is characterized by problems with attention, hyperactivity, and impulsivity; ODD, which is defined by a pattern of negativistic, hostile, and oppositional behaviors toward adults; and CD, which involves a pattern of behavior in which the rights of others and societal norms are violated (APA, 2000). Anxiety conditions central to the current review include GAD, which is characterized by excessive anxiety and worry in multiple domains of the child’s life, and SAD, which involves developmentally inappropriate, excessive, and persistent worry about separation from attachment figures (APA, 2000). Although other anxiety disorders (e.g., social phobia) could have been included in this review, we chose to focus on SAD and GAD for several reasons. First, there is less of a literature explicitly examining the development of social phobia in childhood, relative to SAD and GAD. Second, reviews of previous literature suggest that social phobia may have different developmental underpinnings, as compared to other childhood anxiety disorders (Neal & Edelmann, 2003).
The Current Review
In the current review, we synthesize a variety of literatures (e.g., child clinical psychology, developmental psychology, developmental psychopathology, and psychophysiology) in an effort to develop a conceptual model that links anxiety and disruptive behavior disorders. We included studies that involve both the co-occurrence of syndromes (e.g., anxiety and disruptive behavior disorders) and symptoms (e.g., anxious and aggressive symptoms). We considered studies examining anxious and aggressive symptoms given the fact that few children exhibit prototypical cases of mental disorders (Kaplan, Dewey, Crawford, & Wilson, 2001), as well as suggestions that the development of comorbidity may be better understood from a dimensional (e.g., symptom) as opposed to categorical (e.g., syndrome) framework (Bogenschutz & Nurnberg, 2002). A dimensional framework could be useful for understanding co-occurring syndromes if relatively little is known about etiological processes underlying the comorbid conditions (Klein & Riso, 1993), as is the case with co-occurring anxiety and disruptive behavior disorders. Last, children who exhibit externalizing and anxiety symptoms, but do not meet diagnostic criteria for the associated disorders, often experience significant impairment, even at subthreshold levels (Angold, Costello, Farmer, Burns, & Erkanli, 1999b). Thus, in combination with a categorical approach, a dimensional approach and consideration of symptoms could be fruitful for developing a model for the co-occurrence of disruptive behavior and anxiety disorders.
We also provide a critical examination of potential reasons for the co-occurrence of anxiety symptoms and reactive aggression in the current review. The framework used relies on explanations for the co-occurrence of psychological disorders (Angold et al., 1999a; Caron & Rutter, 1991; Klein & Riso, 1993), which we applied to co-occurring anxiety and disruptive behavior disorders, as well as co-occurring anxiety symptoms and reactive aggression where feasible. Furthermore, we identify gaps in the literature with regard to anxiety and reactive aggression, as well as anxiety and disruptive behavior disorders more generally. We then provide a conceptual model describing how co-occurring anxiety symptoms and reactive aggression may develop into comorbid anxiety and disruptive behavior disorders. Finally, we present clinical implications of the conceptual model and directions for future research.
Comorbidity Explanations
Various authors have suggested frameworks for conceptualizing comorbidity of psychological syndromes among children (Angold et al., 1999a; Caron & Rutter, 1991; Klein & Riso, 1993). These explanations include artifactual, methodological, and causal explanations. Little research, however, has examined how the co-occurrence of precursors for, or symptoms associated with, these disorders should be conceptualized. As such, we consider several comorbidity explanations in relation to anxiety and disruptive behavior disorder syndromes, as well as anxiety symptoms and reactive aggression. The artifactual and methodological explanations include possibilities that comorbidity is due to chance, sampling bias, or symptom overlap. Given the nature of these explanations, evidence for artifactual and methodological explanations is best examined from the perspective of the categorical approach to comorbidity. Thus, for the most part, evidence for these explanations involves research evaluating diagnostic categories. However, the “causal” explanations stem from a more developmental framework. These explanations include the possibilities that (a) one disorder (or set of symptoms) confers risk for another (e.g., GAD confers risk for ODD or vice versa), and (b) shared risk processes may account for the co-occurrence of anxiety and disruptive behavior disorders. Given the nature of these explanations, we first review research involving diagnostic categories. We then review research involving symptoms associated with these categories that may serve as precursors for these disorders. Consideration of these explanations at both the syndromal and symptom levels should contribute to a more complete understanding of how such comorbidity develops over time and facilitate identification of gaps in the literature that can be addressed in future work
Artifactual Explanations
The first artifactual explanation is that comorbidity of anxiety and disruptive behavior disorders may be due to chance. That is, if occurrence of two disorders is high, the chance of their co-occurrence would be high as well. However, because DSM-IV anxiety and disruptive behavior disorders co-occur at rates above chance (Angold et al., 1999a; Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Fleitlich-Bilyk & Goodman, 2004; Ford et al., 2003; Marmorstein, 2007), this explanation cannot completely account for the comorbidity of anxiety and disruptive behavior disorders. For instance, a review of comorbid conditions by Angold et al. (1999a) demonstrated that the odds ratio for comorbid anxiety disorders (including GAD and SAD) and ODD or CD was 3.1, and the odds ratio for comorbid anxiety disorders and ADHD was 3.0. Looking at associations among disorders by developmental period, anxiety disorders (including GAD and SAD) are significantly related to ODD among preschool-age children (Egger & Angold, 2006). Considering middle childhood and adolescence, community-based studies report that 8.7% of children 7–14 years of age exhibited comorbid anxiety and disruptive behavior disorders (Fleitlich-Bilyk & Goodman, 2004). In addition, 7.7% of children 9–13 years of age met criteria for any anxiety disorder and ODD, 7.7% met criteria for any anxiety disorder and ADHD, and 3.5 % met criteria for any anxiety disorder and CD (Costello et al., 2003). Last, 7% of children aged 5–15 met criteria for co-occurring anxiety (including GAD and SAD) and disruptive behavior disorders (i.e., ADHD, ODD, CD) (Ford et al., 2003).
Very few published reports permit examination of comorbidity between specific anxiety and disruptive behavior disorders. Similar to the research reviewed already, results from the Methods for the Epidemiology of Child and Adolescent Mental Disorders study indicate that, using DSM-III-R diagnostic criteria, ADHD, ODD, and CD are often comorbid with anxiety disorders (considered as a group) among children and adolescents (Marmorstein, 2007). However, findings also suggest distinct relations among each of the disruptive behavior and anxiety disorders. Specifically, ODD and ADHD were related to both GAD and SAD, whereas CD only was associated with GAD. Odds ratios ranged from 2 to 7, again suggesting greater than chance associations among these disorders (Marmorstein, 2007).
Taken together, epidemiological and community-based studies involving multiple versions of the DSM suggest that anxiety and disruptive behavior disorders co-occur at above chance rates. In addition, ODD and ADHD are more consistently related to anxiety disorders (particularly GAD and SAD) than CD. There are a couple potential reasons for these different patterns of associations. First, avoidance, which is a core feature of several anxiety disorders, may manifest as opposition to complying with developmentally appropriate expectations. Thus, children who engage in avoidance may be more likely to evidence comorbid ODD, as opposed to CD, symptoms (Drabick et al., 2008; Garland & Garland, 2001). Second, reactive aggression is more likely to be associated with ODD and/or ADHD, whereas proactive aggression is more likely to be associated with CD (Card & Little, 2006; Vitaro, Gendreau, Tremblay, & Oligny, 1998). Children with CD who exhibit reactive aggression consequently may be more likely to experience comorbid anxiety symptoms than children with CD who primarily exhibit proactive aggression (Frick et al., 1999). Regardless of the reasons for these different patterns of associations, it is clear that the comorbidity of disruptive behavior and anxiety disorders cannot be attributed to chance, and consideration of alternative explanations is necessary.
A second artifactual reason for the overlap between anxiety and disruptive behavior disorders is sampling bias. Clinic-based samples are more likely to include children and adolescents with comorbid conditions than youth who do not attend a clinic, as the probability of seeking treatment is greater among individuals with more than one disorder (Ferro & Klein, 1997). Clinic samples thus can produce artificially elevated rates of comorbidity (Angold et al., 1999a; Klein & Riso, 1993). It should be noted that disparate rates of comorbidity can be obtained in non-clinical samples as well. For example, in a self-selected or volunteer community sample, information on individuals who choose not to participate is typically unavailable. Therefore, rates of comorbidity may be biased because of the individual’s ability to select into or out of the sample. Nevertheless, as presented above, prevalence rates for co-occurring anxiety and disruptive behavior disorders that exceed chance have been found consistently among epidemiological samples of children and adolescents (Costello et al., 2003; Fleitlich-Bilyk & Goodman, 2004; Ford et al., 2003; Marmorstein, 2007). Thus, sampling biases cannot fully account for the co-occurrence of disruptive behavior and anxiety disorders either.
A third artifactual explanation for comorbidity involves symptom overlap among diagnostic categories (Angold et al., 1999a; Klein & Riso, 1993). Because disorders can be manifested heterogeneously and include symptoms often associated with other disorders, observed comorbidity may be a function of symptom overlap. This explanation is unlikely to account for comorbid anxiety and disruptive behavior disorders, as few symptoms are similar across these diagnostic categories. However, one potential area of overlap that is not readily apparent from these syndromes involves avoidance and oppositional behaviors, which are typically associated with anxiety disorders and ODD, respectively. This area of potential overlap can lead to an artifactual comorbidity, stemming from differences in informant perspectives (De Los Reyes & Kazdin, 2005; Drabick et al., 2008). For instance, refusing to comply with an adult request may be seen as indicative of child oppositionality, or alternatively, this refusal may be attributed to the child’s anxiety about engaging in a task. For a child who evidences anxiety with regard to multiple domains of functioning (and thus manifests oppositional or avoidant behavior in multiple circumstances), it may be difficult to differentiate oppositional from anxious/avoidant behavior (Drabick et al., 2008). Thus, differences in informant attributions may result in labeling the same child behavior (e.g., refusal to do a task) as an example of a symptom that is typically associated with different syndromes (e.g., ODD vs. GAD). A recent study examining this issue with regard to co-occurring ODD and GAD symptoms demonstrated viability of cross-informant, mixed comorbidity (i.e., the child meets criteria for multiple disorders, but informants endorse symptoms that are consistent with different disorders; Drabick et al., 2008). Specifically, approximately 11% of this clinic-based sample met criteria for cross-informant, mixed comorbid ODD and GAD, with 5% meeting criteria for teacher-rated ODD and mother-rated GAD and 6% meeting criteria for teacher-rated GAD and mother-rated ODD. This study thus suggests that co-occurring ODD and GAD, whether considered within or between informants, may partially stem from informants’ interpreting particular symptoms differently. Although this is a potentially important methodological issue to consider in research involving dimensional approaches to comorbidity and multiple informants of child symptoms, it is less likely that this methodological factor affects rates of co-occurring anxiety and disruptive behavior disorders derived from diagnostic interviews.
Taken together, these artifactual explanations are not sufficient to account for co-occurring anxiety and disruptive behavior disorders. Thus, evaluation of alternative explanations is necessary. Three additional explanations that may be relevant for co-occurring anxiety and disruptive behavior disorders include: (1) anxiety disorders confer risk for disruptive behavior disorders, (2) disruptive behavior disorders confer risk for anxiety disorders, and (3) shared risk processes account for their co-occurrence. One of the goals of this review is to examine both syndromes and symptoms; consequently, research involving anxiety and disruptive behavior disorders, as well as anxiety symptoms and reactive aggression that may be components or correlates of these disorders, is considered for each explanation where possible.
Anxiety Precedes Disruptive Behavior
The first explanation, which states that anxiety disorders confer risk for disruptive behavior disorders, is also consistent with the possibility that the presence of an anxiety disorder may lower the threshold for the expression of a disruptive behavior disorder. For example, if a child has subthreshold ODD symptoms, onset of an anxiety disorder may exacerbate oppositional or noncompliant behaviors, leading to a subsequent ODD diagnosis. When considering research that examines these conditions at the level of the disorder, this explanation has received support in clinic-based samples. Among children 8–17 years of age with SAD, Foley et al. (2004) reported that 19% of youth with SAD only at initial interview, and 15% of children with SAD at both the initial and 18-month follow-up interviews, met criteria for ODD at follow-up. In another clinical sample of children aged 5–18 diagnosed with various anxiety disorders, including SAD and overanxious disorder (OAD; DSM-III-R version of GAD), 7.1% of children met criteria for a disruptive behavior disorder (i.e., ADHD, ODD, and CD) at follow up (at least 12 months after initial interview; Last, Perrin, Hersen, & Kazdin, 1996). In addition, in an epidemiological sample of youth aged 9 to 19, Bittner et al. (2007) found that the presence of GAD before age 13 predicted the development of CD subsequent to age 13, and the odds ratio of this co-occurrence was 3.6.
Turning from the syndrome to symptom level, anxiety symptoms reportedly precede reactive aggression. Anxiety symptoms assessed at age 6 are prospectively related to reactive aggression at ages 10 to 12 (Vitaro et al., 2002). Ialongo, Edelsohn, Werthamer-Larsson, and Kellam (1994) also found a positive relation between anxious symptoms in the fall of first grade and aggressive behaviors in the spring of first grade, even after controlling for initial levels of aggression. One possible explanation for why anxiety may confer risk for the development of reactive aggression is the frustration-aggression model (Polman, Orobio de Castro, Koops, van Boxtel, & Merk, 2007). This model proposes that reactive aggression results from frustration. In addition, this frustration and associated negative emotions (e.g., anxiety, anger) stem from blocking of the individual’s goals (e.g., withdrawing from an anxiety-provoking situation). The model also proposes that the level of frustration and aggressive impulses are proportional to the importance of the blocked goal (Dollard, Doob, Miller, Mowrer, & Sears, 1939). That is, the more important the goal (e.g., the greater the desire for withdrawal), the greater the frustration and subsequent aggression if the goal is blocked. In this way, anxiety may lead to reactive aggression, as a result of the individual’s inability to avoid or withdraw from a particular situation.
One line of work that may be relevant for the frustration-aggression model is research examining response times among anxious and/or impulsive adults. After being punished, anxious individuals respond more quickly than impulsive and comparison individuals (Barratt & Patton, 1983; Milich & Kramer, 1984). This notion of “anxious impulsivity” may seem incompatible with the more typical description of anxious individuals as withdrawn and over-inhibited. Nevertheless, the individual’s tendency to withdraw may be overcome by previous experiences or situational constraints that preclude inhibition or withdrawal. For instance, using a laboratory task for which the participant was instructed to trace a circle as slowly as possible without stopping, Wallace and Newman (1990) found that the response times for anxious individuals and for impulsive individuals did not differ when the game involved the risk of punishment (e.g., losing $3.00). However, impulsive individuals exhibited faster response times than anxious individuals when they could obtain a reward (e.g., $3.00; Wallace & Newman, 1990). These findings suggest that in punishment conditions where the individual cannot withdraw, anxious individuals may respond similarly to impulsive individuals. Moreover, this tendency among anxious individuals to respond impulsively in negatively valenced (e.g., punishment) situations may be an over-learned, inflexible response that could stem from difficulty regulating negative emotions (Newman & Wallace, 1993). Consequently, anxious individuals may respond impulsively when they experience heightened levels of negative emotion.
Though speculative, when applied to co-occurring anxiety symptoms and reactive aggression among children, anxious children may be more likely to respond impulsively in contexts that elicit negative emotions (e.g., situations that may lead to punishment). Over time, this response tendency may develop into an inflexible, maladaptive pattern of responding to situations that elicit negative emotions. One example of this type of inflexible responding may be a tendency to engage in reactive aggression. Reactive aggression is thought to be, in part, the result of an over-learned, impulsive style of responding to perceived provocations (Dodge et al., 1997). To illustrate this possibility, if an anxious child is provoked by another child, he or she may experience heightened levels of negative emotions that may be difficult to regulate. If the anxious child is unable to withdraw from the situation because peers block an escape route, the anxious child consequently may engage in reactive aggression, as would be consistent with the frustration-aggression model.
Disruptive Behavior Precedes Anxiety
Evidence from community- and clinic-based samples also supports the second explanation, which states that disruptive behavior disorders confer risk for anxiety disorders. Considering research at the syndrome or disorder level, community-based studies indicated that children with persistent ODD in preschool were at risk for developing comorbid anxiety disorders (e.g., SAD, GAD) in later childhood (Lavigne et al., 2001). Similarly, among a clinic-based sample of boys, Burke, Loeber, Lahey, and Rathouz (2005) found that parent-reported ODD and ADHD in childhood (ages 7–12) predicted OAD in adolescence and adulthood, but OAD in childhood did not predict ODD in adolescence. In another clinic-referred sample of preschool boys, Speltz and colleagues reported that 7.6% of boys diagnosed with ODD, ADHD, or ODD+ADHD at the initial time point had a comorbid anxiety disorder diagnosis at 2-year follow up (Speltz, McCllellan, DeKlyen, & Jones, 1999). Last, in a study that considered both syndrome and symptom levels, externalizing problems (measured by the aggression and delinquency subscales of the CBCL) assessed at ages 4–16 prospectively predicted anxiety disorders (measured by a structured diagnostic interview) approximately 14 years later (Roza, Hofstra, van der Ende, & Verhulst, 2003).
Considering research at the symptom level, support for reactive aggression preceding the onset of anxiety symptoms has yet to be documented in the literature to our knowledge. Such lack of findings may be a function of the limited amount of work concurrently examining reactive aggression and anxiety. In a notable exception, Pihlakoski and colleagues (2006) reported that aggression at age 3 predicted anxious-depressive symptoms at age 12 among Finnish children. In terms of processes that may account for reactive aggression leading to anxiety, Frick and colleagues (1999) hypothesized that engaging in antisocial behaviors may engender recurrent state anxiety. This recurrent state anxiety may become difficult to differentiate from an anxiety disorder over time. A second example of this potential pattern involves peer processes (e.g., peer rejection) as a possible mediator. Specifically, children with externalizing symptoms, including reactive aggression, are often rejected by their peers (Dodge et al., 1997; Little & Garber, 1995). Because peer rejection is associated with anxiety symptoms (Bell-Dolan, Foster, & Christopher, 1995; French, 1990), it is possible that reactive aggression leads to peer rejection, which then may lead to anxiety symptoms.
Interim Summary
In sum, research that considers anxiety and disruptive behavior disorders in both clinic- and community-based samples provides some evidence for the explanations that (a) anxiety disorders confer risk for the development of disruptive behavior disorders and (b) disruptive behavior disorders confer risk for the development of anxiety disorders. Nevertheless, given relatively limited research examining the co-occurrence of anxiety and disruptive behavior disorders and contradictory evidence regarding patterns of their development, it is difficult to draw firm conclusions about which disorders are more likely to precede others. Taken together, findings suggest that ADHD and ODD in early childhood may be more likely to confer risk for anxiety disorders, whereas GAD and SAD in later childhood and adolescence may predict ODD and CD developing in adolescence. Critical examination of these findings raises important questions about the timing of the onset of symptoms and of diagnostic syndromes, however. For example, anxiety symptoms may precede the onset of disruptive behaviors and in turn exacerbate these disruptive behavior problems. This potential series of events could result in the apparent development of a diagnosable disruptive behavior disorder before the development of a diagnosable anxiety disorder. Such possibility suggests that a focus on onset, development, and exacerbation of anxiety and disruptive behavior symptoms, in addition to consideration of the development of anxiety and disruptive behavior disorder syndromes, may help to clarify the circumstances under which these comorbidity explanations apply to comorbid anxiety and disruptive behavior disorders.
Turning from research involving disorders to investigations of anxiety symptoms and reactive aggression, there is relatively greater evidence for a link from anxiety symptoms to reactive aggression than the reverse. However, we know of only one study that examined this relation empirically and the reverse relation, whether reactive aggression predicted anxiety symptoms, was not examined concurrently (Vitaro et al., 2002). Though lack of a predictive relation from reactive aggression to anxiety symptoms is counter to literature examining diagnostic categories, this lack of findings may reflect the paucity of literature examining prospective relations between reactive aggression and anxiety symptoms. Reactive aggression is measured less frequently in studies examining clinical symptoms and disorders, perhaps because reactive aggression does not fit easily into current nosological categories. When more broadly defined symptoms of aggression, including reactive aggression, are examined, a prospective relation between aggression and anxiety symptoms has been found. Nonetheless, it is possible that reactive aggression does not predict anxiety symptoms prospectively. Instead, anxiety symptoms may exacerbate subclinical behavior problems, which may contribute to the presence of reactive aggression and diagnosable disruptive behavior disorders. An empirical examination of whether anxiety symptoms are more likely to precede reactive aggression or vice versa is needed to address this issue.
Another potential confounding issue for which disorder precedes others involves typical developmental processes and age of onset of disorders. For example, behavior problems, particularly physical aggression, peak during the toddler to early childhood years (Broidy et al., 2003; Tremblay & Nagin, 2005). Moreover, given the purported requisite cognitive processes for engaging in worry and potentially other anxious cognitions, GAD may be more likely to follow disruptive behavior disorders. Indeed, children have difficulty reasoning about future possibilities, considering multiple threatening outcomes, and elaborating potential negative consequences before the age of 8 (Vasey, 1993). Given these issues, ADHD and ODD may be more likely to precede anxiety disorders in early childhood, which is consistent with the younger age of onset for ADHD and ODD relative to most anxiety disorders (APA, 2000). Therefore, whether anxiety confers risk for disruptive behavior disorders or disruptive behavior disorders confer risk for anxiety disorders likely depends on the symptoms and diagnostic categories under question. As a result, future examinations of development of co-occurring anxiety and disruptive behavior disorders should consider the roles of normative developmental processes and evaluate associations among specific diagnostic categories rather than broader, more heterogeneous outcomes.
Potential Shared Risk Factors
The third explanation suggests that anxiety and disruptive behavior disorders are associated with shared and distinct risk factors, and their co-occurrence may stem from shared risk factors (i.e., biological, psychological, and/or social factors that are shared by or common to both anxiety and disruptive behavior disorders; Angold et al., 1999a; Caron & Rutter, 1991; Klein & Riso, 1993). Because few studies have examined co-occurring anxiety and disruptive behavior disorders, there is an absence of literature considering potential overlapping and/or unique risk factors for anxiety and disruptive behavior disorders. In an effort to present findings that could support this potential explanation, we focus on research that has identified potential shared risk processes, as opposed to processes that are specific to, anxiety and disruptive behavior disorders in the present review. Studies that have examined this issue suggest a role for both child-specific (e.g., biological) and environmental factors in the association between anxiety and disruptive behavior disorders (e.g., Gregory, Eley, & Plomin, 2004).
With regard to child-specific factors, genes involved in some aspects of dopaminergic and serotonergic function have been implicated in the association between anxiety and disruptive behavior disorders (Gregory et al., 2004). At this point, there is mixed evidence for associations between childhood anxiety and serotonin alleles (i.e., short versus long; Gregory & Eley, 2007; Young, Smolen, Sallings, Corley, & Hewitt, 2003) and dopamine receptors (e.g., DRD4 alleles; Gregory & Eley, 2007; Lakatos et al., 2003). Several measures of serotonin and dopamine activity also have been implicated in childhood disruptive behavior disorders (Lee et al., 2007; van Goozen, Fairchild, Snoek, & Harold, 2007), suggesting potential shared processes at the molecular genetic level.
In terms of shared environmental factors, it is likely that parent-child interactions increase risk for anxiety and disruptive behavior disorders. Indeed, some parent-child interaction styles are similar among families of children with anxiety and disruptive behavior disorders. For instance, parents of anxious or aggressive children are less likely to agree with their children and are less likely to acknowledge positive consequences of situations, as compared to parents of non-clinical children (Barrett, Rapee, Dadds, & Ryan, 1996; Dadds, Barrett, Rapee, & Ryan, 1996). In addition, mothers of children with anxiety or disruptive behaviors tend to display greater and more intrusive involvement than mothers of non-clinical children (Hudson & Rapee, 2001). Because of these parental responses, children may learn dysfunctional ways of reacting to their environment, which place them at risk for anxiety and/or disruptive behavior disorders. It is possible that these parenting behaviors interact with genetic risk to increase risk for anxiety and/or disruptive behavior disorders, though future research will be necessary to clarify whether these gene × environment interactions reliably predict co-occurring anxiety and disruptive behavior disorders.
Another environmental factor that may serve as a shared risk process is exposure to neighborhood violence, which is associated with both anxiety and disruptive behavior disorders (Attar, Guerra, & Tolan, 1994; Gorman-Smith & Tolan, 1998; Guerra, Huesmann, & Spinder, 2003; Martinez & Richters, 1993; Singer, Anglin, Song, & Lunghofer, 1995; Youngstrom, Weist, & Albus, 2003). Children exposed to neighborhood violence may model aggressive behavior, which leads to positive outcome and efficacy beliefs for aggression and the perception that aggression is an appropriate response to ambiguous peer provocation (Schwartz & Proctor, 2000). Thus, exposure to neighborhood violence may confer risk for disruptive behavior disorders. In contrast, anxiety disorders may result from exposure to neighborhood violence if the neighborhood violence is perceived as uncontrollable, which consequently induces greater fear (Chorpita & Barlow, 1998). Regardless of the mechanism, however, it likely that a child’s perception of neighborhood danger confers risk for both anxiety and disruptive behavior disorders.
Given our proposal that the association between anxiety symptoms and reactive aggression may help to explain the co-occurrence of anxiety and disruptive behavior disorders, we also consider potential risk factors that may underlie co-occurring anxiety symptoms and reactive aggression. At this point in time, we are not aware of any studies that have explicitly evaluated shared risk factors for anxiety symptoms and reactive aggression. However, when examined independently, there are several factors that have been associated with both anxiety symptoms and reactive aggression. Although there is a number of potential shared risk processes that could be considered, we focus on a few child-specific factors, namely difficult temperament, information processing biases, and autonomic functioning, as they seem to have the greatest amount of support in the literature and best illustrate our conceptual model.
First, difficult temperamental styles have been linked to both anxiety and aggression, and in particular, reactive aggression (Ortiz & del Barrio Gandara, 2006; Shaw et al., 1997). For example, high temperamental difficulty at age 2 predicted increased depression/anxiety scores on the Child Behavior Checklist (CBCL; Achenbach, 1992) at age 3 (Shaw et al., 1997). In addition, aspects of difficult temperament, such as negative emotionality, irritability, and low frustration tolerance, have been linked to reactive aggression (Merk, 2005; Vitaro, Barker, Boivin, Brendgen, & Tremblay, 2006; Vitaro et al., 2002). Because a difficult temperament and negative emotionality are partly heritable, associations among temperament, anxiety, and reactive aggression also may be partly under genetic influences (Goldsmith, Buss, & Lemery, 1997; Vitaro et al., 2002), suggesting presence of shared biological risk factors for anxiety and reactive aggression.
Second, co-occurrence of anxiety and reactive aggression may be explained by information processing models, which suggest that anxious and reactively aggressive children perceive their environments in similar ways. One of the primary cognitive processes examined in relation to anxiety is hypervigilance to threat, which is a common feature of cognitive theories for the development of anxiety among children and adults (Beck & Emery, 1985; Ingram & Kendall, 1985). Anxious children show an attentional bias to emotionally threatening stimuli (Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & van Ijzendoorn, 2007; Puliafuco & Kendall, 2006; Taghavi, Neshat-Doost, Moradi, Yule, & Dalgleish, 1999; Vasey, Daleidan, Williams, & Brown, 1995). Furthermore, anxious children tend to make threatening interpretations when presented with ambiguous information and to attribute hostile intent to others’ actions (Barrett, et al., 1996; Bell-Dolan, 1995; Bogels & Zitgerman, 2000; Muris et al., 2000a; Muris, Luermans, Merckelbach, & Mayer, 2000b). Nevertheless, these information-processing biases are not specific to a particular anxiety disorder (e.g., SAD or GAD), suggesting that such information-processing biases may be characteristic of anxiety symptoms more generally.
Aggressive children also exhibit information-processing biases (Crick & Dodge, 1994). In comparison with their non-aggressive peers, aggressive children encode ambiguous cues as hostile and/or neglect to encode nonhostile cues (Dodge, Bates, & Pettit, 1990a); display a bias toward making hostile attributions of intent (Dodge et al., 1990a; Dodge, Price, Bachorowski, & Newman, 1990b; Orobio de castro, Veerman, Koops, Bosch, & Monshouwer, 2002); and select dominance- and revenge-related goals (Hughes, Meehan, & Cavell, 2004). Subsequently, aggressive children generate more maladaptive responses, are more confident in their ability to enact those maladaptive responses, and are more likely to expect their aggressive behavior to result in a desirable outcome (e.g., obtaining rewards, decreasing aversive treatment from others, and/or facilitating more positive self-evaluations; Asarnow & Callan, 1985; Crick & Ladd, 1990; Dodge & Frame, 1982; Dodge & Newman, 1981).
Studies comparing cognitive biases among anxious vs. aggressive children indicate that anxiety and aggression are associated with biases across multiple stages of information processing, including hypervigilance for threat-related cues, negative interpretations of social situations, and hostile attributions (e.g., Reid, Salmon, & Lovibond, 2006). In addition, research comparing information-processing biases associated with reactive vs. proactive aggression indicates that biases exhibited by reactively aggressive children are similar to biases observed among anxious children. For instance, reactively aggressive children tend to interpret peers’ behaviors as more hostile and to react with aggression more frequently when faced with ambiguous provocations compared to proactively aggressive children (Dodge & Coie, 1987).
Third, autonomic hyperarousal (indexed by increased sympathetic nervous system activity) in stressful situations is a shared correlate of both reactive aggression and anxiety (Hubbard et al., 2002; Tyson, 1998) and may explain their co-occurrence. Generally speaking, the sympathetic nervous system regulates involuntary reactions to stress (e.g., increased heart and breathing rates) and prepares the body for action in the context of stressors (Beauchaine, 2001). Given that the ability to regulate emotional and physiological arousal influences what a child notices and processes about a social situation (Lemerise & Arsenio, 2000), this autonomic hyperarousal may lead reactively aggressive and/or anxious children to become overly focused on their heightened physiological arousal in social situations. As a result, children who are autonomically hyperaroused may be more likely to make hostile interpretations of social situations because their self-focus interferes with their ability to identify social and emotional cues in others. Thus, autonomic hyperarousal and subsequent hostile interpretations of social situations may confer risk for reactive aggression and/or anxiety.
Although associations between increased autonomic arousal and reactive aggression have been demonstrated, these findings are incongruent with most research examining the autonomic profiles of children with disruptive behavior disorders. For example, Beauchaine and colleagues have shown that children who meet diagnostic criteria for ODD or CD exhibit attenuated sympathetic activity while resting and during a task, and children with comorbid ADHD and CD exhibit attenuated parasympathetic activity at baseline and during a task (Beauchaine, Katkin, Strassberg, & Snarr, 2001; Crowell et al., 2006). These discrepancies among autonomic profiles for children with reactive aggression vs. children with disruptive behavior disorders are notable given that children with disruptive behavior disorders often exhibit high levels of reactive aggression (Kempes, Matthys, Maassen, van Goozen, & van Engeland, 2006). Unfortunately, limited research explicitly examines the inconsistent findings among autonomic activity, reactive aggression, and disruptive behavior disorders. As a result, models developed to account for the physiological underpinnings of both reactive aggression and disruptive behavior disorders hold less weight than they would if the contradictions were incorporated into theoretical explanations. One explanation for this contradiction is that children who evidence high levels of reactive, as opposed to proactive, aggression also may exhibit elevated rates of anxiety symptoms. As such, these children also may experience greater autonomic hyperarousal than children with predominantly externalizing symptoms (including both proactive and reactive aggression). In support of this possibility, van Goozen and colleagues (1998) reported that boys with co-occurring ODD and anxiety symptoms had stronger autonomic responses to a frustration induction task than boys with only ODD. Future research will be necessary to determine whether this explanation can partly account for the discrepant findings between disruptive behavior disorders (syndrome level) and reactive aggression (symptom level).
Taken together, there are several possible shared factors that may account for the co-occurrence of anxiety and disruptive behavior disorders, as well as anxiety symptoms and reactive aggression. When examining anxiety and disruptive behavior disorders, studies have implicated both genetic and shared environmental influences (e.g., parent-child interactions, exposure to neighborhood violence). When considering anxiety symptoms or reactive aggression, studies have suggested that a difficult temperamental style, a tendency to perceive situations as threatening and to make hostile attributions, and heightened autonomic arousal in stressful social situations may place a child at increased risk for both anxiety symptoms and reactive aggression. Although this possibility remains to be tested, we hypothesize that, over time, these shared processes may contribute to and exacerbate symptoms of anxiety and reactive aggression and consequently lead to clinically identifiable comorbid anxiety and disruptive behavior disorders among children. It is also likely that these shared processes interact with contextual factors to increase a child’s risk for or buffer against the development anxiety and reactive aggression.
Unfortunately, usefulness of these purported shared risk factors for understanding co-occurring anxiety and disruptive behavior disorders, as well as co-occurring anxious symptoms and reactive aggression, is limited. First, these risk factors are not specific to these childhood symptoms or disorders, which limits their usefulness for etiological and intervention models for comorbid anxiety and disruptive behavior disorders (Steinberg & Avenevoli, 2000). Thus, future research is required to determine whether these risk processes exhibit more distal associations with disruptive behavior and anxiety disorders, or whether they are more specifically associated with anxiety symptoms and reactive aggression. Second, presuming these are “shared” risk factors is arbitrary in that these factors have not been effectively tested in other viable roles, such as mediators or moderators. For example, hostile attribution biases may mediate or moderate the effects of anxiety symptoms on reactive aggression, or the effects of ODD on GAD. It also is plausible that these factors each play a role in the development of co-occurring symptoms or disorders, but their effects differ depending on when they are experienced. Research that permits comparisons of multiple roles (e.g., shared process, mediator, moderator) within the same sample could provide a greater understanding of the effects of these processes on co-occurring anxiety and disruptive behavior disorders, and thus inform etiological and intervention models.
Gaps in the Literature
Given the relatively small body of literature examining the co-occurrence of anxiety and disruptive behavior disorders, there are several gaps that limit the understanding of these comorbid conditions. First, there is limited knowledge as to developmental pathways of co-occurring anxiety and disruptive behavior disorders. In terms of age, anxiety and disruptive behavior disorders tend to be more strongly associated among younger, as compared to older, youth in both community- and clinic-based samples (Bird, Gould, & Staghezza, 1993; Card & Little, 2006; Russo & Beidel, 1994). Given this age effect, future research should examine reasons for decreased associations between anxiety and disruptive behavior disorders over time. One possibility is that younger children may be more likely to express their anxiety by refusing to comply with commands or by acting oppositionally, whereas older children may be able to express their anxiety more directly or cope with their anxiety in a more socially acceptable way. This possibility is supported by evidence that language and verbal abilities develop as children age, and these abilities may facilitate anxiety expression and emotion regulation strategies (Wellman, Harris, Banerjee, & Sinclair, 1995).
Another critical gap is limited knowledge regarding how sex differences in prevalence rates for anxiety and disruptive behavior disorders affect their comorbidity. Anxiety disorders are generally more common among girls, whereas disruptive behavior disorders are more common among boys (Costello, Egger, & Angold, 2005; Simonoff et al., 1997). However, at the level of individual anxiety diagnoses, sex differences in prevalence rates are generally small (Costello et al., 2005). Recent studies suggest that, compared to boys, girls who meet criteria for a psychological disorder in childhood are more likely to develop a second, distinct condition in addition to their index condition (Costello et al., 2003), which suggests that girls may be more likely to develop co-occurring anxiety and disruptive behavior disorders. Nevertheless, in terms of ADHD, compared to girls, boys who met diagnostic criteria for DSM-III-R attention deficit disorder with hyperactivity were more likely to receive a co-diagnosis of anxiety (Livingston, Dykman, & Ackerman, 1990), and boys with ADHD were more likely to meet criteria for comorbid anxiety disorders as they age (Brown, Maden-Swain, & Baldwin, 1991). Given that boys exhibit higher levels of ADHD symptoms in childhood (APA, 2000; Gaub & Carlson, 1997), this sex difference in co-occurring ADHD and anxiety may be a result of higher base rates of ADHD among boys (APA, 1994, 2000).
Using similar reasoning, because adolescent girls are more likely to demonstrate anxiety disorders than boys, girls may experience greater risk for the comorbidity of anxiety with ODD and anxiety with CD than boys. In support of this possibility, Loeber and Keenan (1994) reported results from the Ontario Child Health Study in which 31.3% of 4–11 year old girls and 48.1% of 12–16 year old girls with CD met criteria for “neurosis” (i.e., OAD, SAD, and/or obsessive compulsive disorder), whereas less than 20% of 4–16 year old boys exhibited comorbid anxiety and CD. Moreover, Maughan et al. (2004) indicated that ODD independently contributed to the prediction of anxiety among girls, but not boys. Last, Foley et al. (2004) demonstrated that girls with SAD evidenced higher levels of ODD symptoms at a later time point than boys with SAD. Thus, these results suggest greater risk among boys for the comorbidity of anxiety and ADHD, and among girls for the comorbidity of anxiety with ODD and anxiety with CD. We know of only one study that has explicitly examined sex differences in multiple disruptive behavior and anxiety disorders. Marmorstein (2007) reported that among 9–17 year old youth, DSM-III-R disruptive behavior disorders (i.e., ADHD, ODD, and CD) were associated with a range of anxiety disorders, including GAD and SAD, among boys. In contrast, among girls, disruptive behavior disorders were primarily associated with GAD. Differences in the results of Marmorstein (2007), compared to Maughan et al. (2004) and Foley et al. (2004), could be related to the use of different DSM criteria, as well as differences in sampling methods. As a result, studies using the most recent DSM criteria and including both sexes may be more likely to report sex differences among children with co-occurring anxiety and disruptive behavior disorders.
Turning from research involving syndromes to a consideration of symptoms, similar rates of reactive aggression among boys and girls have been found in clinic-based samples (Connor, Steingard, Anderson, & Melloni, 2003). However, correlates related to reactive aggression may differ by sex. For instance, reactive aggression was related to increased levels of hyperactive/impulsive symptoms among clinic-referred boys (Connor et al., 2003), which may partially explain why ADHD and anxiety are more consistently associated among boys than girls. In comparison, community-based studies have found that boys exhibit higher rates of reactive aggression than girls (Salmivalli & Nieminen, 2002). Despite the difference in rates of reactive aggression, there is a significant relation between reactive aggression and anxiety among both boys and girls in non-referred samples (Marsee et al., 2007), suggesting that differences in base rates of reactive aggression may not impact rates of co-occurring symptoms among boys and girls. In sum, there appear to be sex differences among children with co-occurring anxiety and disruptive behavior disorders; though, sex differences depend on the age of the child. In contrast, there is less evidence for sex differences among children exhibiting anxiety symptoms and reactive aggression. Future research should more specifically consider the role of sex differences in this comorbid condition.
Conceptual Model
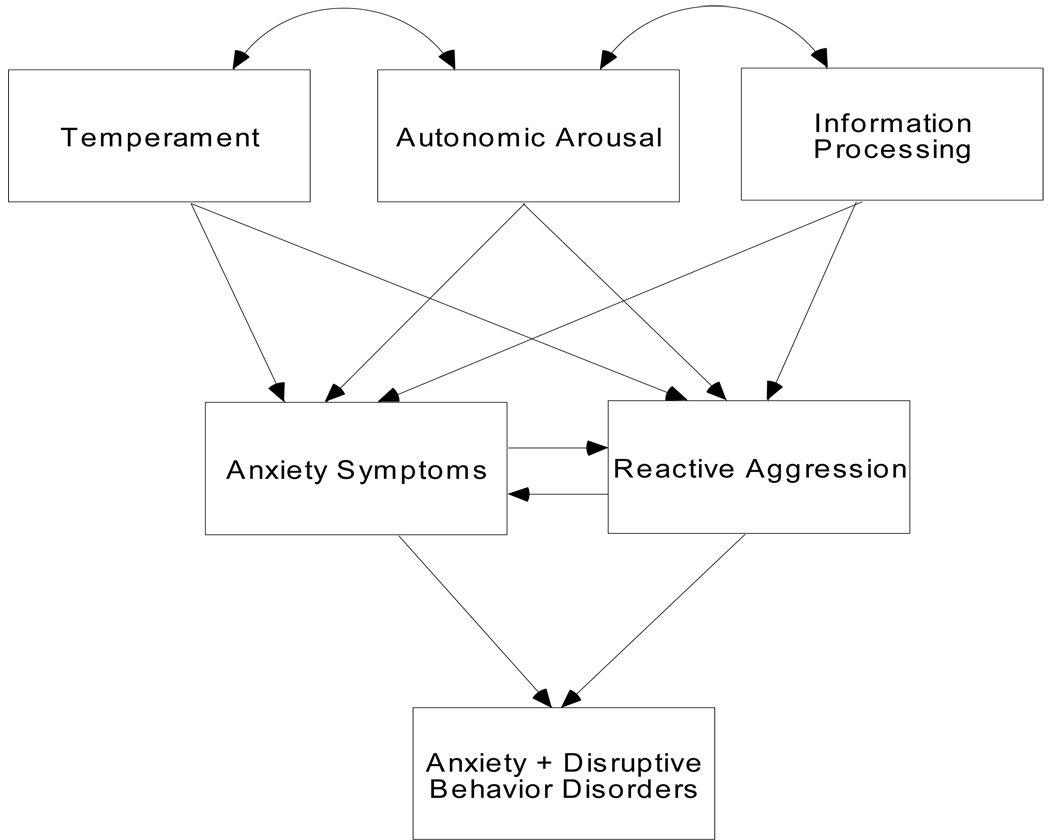
Combining literature for reactive aggression and anxiety symptoms, we developed a potential conceptual model for the co-occurrence of anxiety and disruptive behavior disorders (Figure 1). Specific risk factors, such as the child’s temperament (e.g., presence of negative emotionality, irritability, and low frustration tolerance), tendency for autonomic hyperarousal, hypervigilance to threat, and hostile interpretations of situations, may predispose the child to experience negative emotional responses (e.g., anxiety and fear) more frequently and in more situations than an individual without these characteristics. In situations that engender negative emotions, children who are anxious and/or fearful may manifest an impulsive response style that over time may become more frequent and automatic. When this relatively inflexible response pattern is coupled with situational constraints such as not being able to avoid feared or threatening experiences, the child may be more likely to exhibit significant anxiety symptoms and/or reactive aggression. For example, in the case of SAD, the child attempts to avoid separation from his or her caregiver. Given that even the thought of separation from the caregiver can lead to significant anxiety, the child could become argumentative and defiant when separation from the caregiver is expected. The child’s use of defiant behavior could become a more frequent and consistent pattern, and over time, the child may engage in defiant behavior even when separation is not imminent.
Figure 1.
Model for the development of comorbid anxiety and disruptive behavior disorders.
At this point, it is unclear whether anxiety symptoms and reactive aggression develop concurrently or whether one precedes the other. In terms of the latter possibility, an anxious child may perceive his or her environment and others as threatening, which may lead the child to act in a hostile or reactively aggressive way when provoked. Alternatively, a reactively aggressive child who is rejected by peers may develop a fear or concern of future rejections. This fear of rejection may manifest as anxiety and generalize to multiple situations and contexts. Nevertheless, although these underlying symptoms and potential mechanisms (e.g., social information processing biases, peer rejection) require further examination, it is hypothesized that once anxiety and reactive aggression co-occur, the risk of developing clinically identifiable comorbid anxiety and disruptive behavior disorders increases substantially. Future research will be necessary to evaluate this conceptual model and to determine whether associated factors act as mechanisms, risk factors, correlates, or sequelae for these symptoms and disorders. Future investigations also will be necessary to determine whether and/or how contextual factors interact with specific risk factors to either increase risk for or buffer against the development of these co-occurring symptoms and disorders.
Clinical Implications
Despite possible assumptions that rates of overlap may be relatively low, it is important for clinicians to assess for both disruptive behavior and anxiety disorders, as well as for anxiety symptoms and reactive aggression, among children and adolescents. A comprehensive conceptualization of the processes underlying and maintaining a child’s behaviors must also consider the interplay among different sets of problems. For example, a child’s oppositional behavior may be due to avoidance associated with separation anxiety. Thus, including functional analysis when assessing a child’s externalizing and anxiety symptoms would be useful to determine the antecedents and consequences of particular behaviors, in addition to possible maintaining or exacerbating roles of the co-occurring symptoms. Evaluating information from multiple informants who can speak to the child’s behavior in various settings is also important.
From a prevention perspective, identification of co-occurring anxiety symptoms and reactive aggression among young children may enable clinicians to target children who are at significant risk for developing comorbid anxiety and disruptive behavior disorder diagnoses. Early identification of these risk factors and symptom correlates may facilitate recognition of children who could benefit from early intervention, potentially preclude or mitigate these syndromes and co-occurring conditions, minimize the significant impairment that is often associated with comorbid disorders, and aid clinicians in selecting treatment strategies and targets for intervention (Kendall et al., 2001).
In terms of treatment of youth with comorbid anxiety and disruptive behavior disorders, intervention studies involving children with primary anxiety or primary disruptive behavior disorders suggest several possible strategies. First, cognitive-behavioral approaches for the treatment of anxiety, in which youth are taught ways to deal with their anxiety and are exposed to feared cues, have resulted in significant improvements (Kendall, 1994; Kendall et al., 1997, 2001). Similarly, treatments for externalizing problems, such as parent-child interaction therapy, parent management training, and the Incredible Years series, also are associated with significant improvements in externalizing behaviors (Brestan & Eyberg, 1998; DeGarmo, Patterson, & Forgatch, 2004; Farmer, Compton, Burns, & Robertson, 2002; Webster-Stratton & Hammond, 1997; Webster-Stratton, Hollinsworth, & Kolpacoff, 1989). Nevertheless, few studies have examined the impact of comorbid anxiety or disruptive behavior disorders on treatment outcome. It has been suggested that the presence of comorbid conditions reduces the effectiveness of a specific treatment on a primary disorder because comorbid diagnoses are associated with greater impairment and severity of symptoms and may interfere with the effectiveness of the treatment on the primary condition. However, several studies have examined treatments for youth with comorbid anxiety and disruptive behavior disorders (Chase & Eyberg, 2008; Flannery-Schroeder et al., 2004; Kendall et al., 2001; Levy, Hunt, & Heriot, 2007; Rapee, 2003). Flannery-Schroeder et al. (2004), Kendall et al. (2001), and Rapee (2003) all documented significant improvements as a result of participation in anxiety-based treatments among anxious children with and without comorbid disruptive behavior disorders. In addition, Kendall et al. (2001) noted that the rate of ODD post-treatment was 1.8% (reduced from 9.2%). Similarly, Chase and Eyberg (2008) reported that among children with comorbid ODD and SAD, parent-child interaction therapy led to significant declines in both ODD and SAD symptoms following intervention. Levy et al. (2007) explicitly examined a treatment designed to address both anxiety and externalizing behaviors. In this study, strategies targeting anger and aggression were added to the “Cool Kids” anxiety treatment program (Rapee, Wignall, Hudson, & Schniering, 2000). Comparisons involved the original Cool Kids program with the combined Cool Kids + anger/aggression program. Strategies for anger and aggression included self-management, self-reflection, and self-monitoring skills. Both programs led to significant improvements (symptom decrements) on measures of child internalizing symptoms and parent-reported externalizing problems, indicating that children’s internalizing and externalizing problems decreased even when they received a treatment program targeting anxiety only (Levy et al., 2007).
Taken together, these findings suggest that treatments for anxiety disorders can be successful in reducing co-occurring externalizing symptoms among children and, similarly, treatments for externalizing or disruptive behavior disorders can reduce the frequency of co-occurring anxiety symptoms. Furthermore, these results suggest that the processes underlying anxiety may play a role in the onset and/or maintenance of externalizing behaviors, and that processes underlying externalizing symptoms also may play a role in the onset and/or maintenance of anxiety symptoms. It will be beneficial for future research to examine the components of treatment that lead to change in both anxiety and externalizing symptoms among children to identify factors associated with successful treatment of these comorbid conditions.
Conclusions and Directions for Future Research
Despite apparent topographic differences, anxiety and disruptive behavior disorders co-occur at above chance rates among children and adolescents according to epidemiological and community-based studies (Angold et al., 1999a; Costello et al., 2003; Ford et al., 2003). Nevertheless, there is limited literature examining why these disorders co-occur. Although there may be some support for methodological explanations of comorbid anxiety and disruptive behavior disorders, methodological explanations are not sufficient to account for these comorbidities. Support for alternative explanations (e.g., one disorder confers risk for another, shared risk processes account for disorder co-occurrence) varies based on developmental period, sample characteristics (e.g., sex, type of sample), and specific disorders examined. Though the research is limited, evidence involving diagnostic categories suggests that (a) ADHD and ODD in early childhood confer risk for the development of anxiety disorders, and (b) SAD and GAD in later childhood confer risk for the development of ODD and CD in adolescence. This ordering may partly reflect developmental processes and the typical age of onset of these disorders, with disorders with earlier onsets being more likely to precede disorders with later onsets. We also found support for the possibility that shared risk factors (e.g., genetics, parental behaviors, neighborhood violence) underlie anxiety and disruptive disorder co-occurrence. However, these factors have not been tested in other viable roles (e.g., mediators, moderators, sequelae). Thus, future research examining these diagnostic categories should consider each of these explanations concurrently, as well as multiple roles for potential shared processes. Such research could speak to the circumstances for which each explanation receives support and the effect of these variables on the development of comorbid conditions. In this review, we presented a relatively limited set of potential shared risk factors in an effort to illustrate applicability of this explanation. Future investigations that consider not only shared, but also unique or specific, processes associated with anxiety and disruptive behavior disorders are necessary to determine whether some processes are associated with one vs. multiple conditions, and how these processes may operate in the development of disruptive behavior and/or anxiety disorders. Given that we did not include discussions of social anxiety in the present review, it also will be important for future research to examine alternative explanations for the co-occurrence of social anxiety and disruptive behavior disorders.
Taking a more dimensional or symptom-based approach, we propose that consideration of potential earlier precursors or symptoms of anxiety and disruptive behavior disorders (i.e., anxious symptoms and reactive aggression) also may be fruitful for understanding the development of these comorbid diagnostic categories. Given that shared processes likely underlie anxious and reactive aggression symptoms, using a developmental perspective to identify factors that confer risk for, maintain, and/or buffer against anxiety and externalizing symptoms can be useful for charting heterogeneous trajectories associated with these comorbidities. More specifically, anxiety symptoms and reactive aggression may co-occur as a result of specific shared risk factors (e.g., child temperament, autonomic arousal, and information processing style), each of which has been associated with anxiety symptoms and reactive aggression in early childhood. Furthermore, examination of these risk factors in early and middle childhood may be particularly important, as this developmental period corresponds to the period when disruptive behavior and anxiety disorders are most likely to co-occur (Russo & Beidel, 1994). The viability of these processes as shared risk factors has yet to be evaluated. Thus, future research is necessary to determine whether these potential shared processes can account for co-occurring anxiety and reactive aggression symptoms.
It also is unclear whether anxiety symptoms and reactive aggression develop concurrently or if one precedes the other. Thus, similar to the suggestion in the context of diagnostic syndromes, future research could evaluate whether one set of symptoms precedes, maintains, or exacerbates the other, and whether shared risk processes underlie symptom co-occurrence. This has important implications for developmental and intervention models for co-occurring anxiety and disruptive behavior disorders. Specifically, we hypothesize that if anxiety symptoms and reactive aggression do co-occur, the child will be at risk for the development of comorbid anxiety and disruptive behavior disorders; consequently, identification of these symptoms could aid early intervention efforts.
Combining categorical and dimensional approaches could facilitate disentangling which comorbidity explanation is most useful. For example, anxious symptoms in early childhood may precede and later exacerbate disruptive behaviors, eventually leading to a diagnosable disruptive behavior disorder. This disruptive behavior disorder in turn could exacerbate anxiety symptoms, leading to an apparent co-occurring anxiety disorder. Consideration of these processes at the syndrome level consequently would suggest a different temporal ordering than would be suggested at the symptom level, though subclinical symptoms obviously underlie these associations. Consideration of symptoms is important, given that little is known about the etiology of co-occurring anxiety and disruptive behavior disorders (Klein & Riso, 1993) and that children exhibiting anxiety and externalizing symptoms without meeting diagnostic criteria exhibit significant impairment (Angold et al., 1999b). Furthermore, as current findings regarding sex differences are inconsistent, it would be beneficial to evaluate whether these inconsistencies are due to changes in DSM criteria, sampling methods, or other substantive reasons. Though no small endeavor, research examining the developmental pathways of comorbid anxiety and disruptive behavior disorders could inform both etiological and intervention models, and thus improve our efforts to intervene and mitigate the negative correlates and sequelae associated with these co-occurring conditions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Manual for the Child Behavior Checklist 2/3 and 1992 profile. Burlington, VT: University of Vermont Department of Psychiatry; 1992. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, Fourth edition (DSM-IV) Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, Fourth edition-Text revision (DSM-IV-TR) Washington, DC: Author; 2000. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999a;40:57–87. [PubMed] [Google Scholar]
- Angold A, Costello EJ, Farmer EMZ, Burns BJ, Erkanli A. Impaired but undiagnosed. Journal of the American Academy of Child and Adolescent Psychiatry. 1999b;38:129–137. doi: 10.1097/00004583-199902000-00011. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Callan JW. Boys with peer adjustment problems: Social cognitive processes. Journal of Consulting and Clinical Psychology. 1985;53:80–87. doi: 10.1037//0022-006x.53.1.80. [DOI] [PubMed] [Google Scholar]
- Attar BK, Guerra NG, Tolan PH. Neighborhood disadvantage, stressful life events, and adjustment in urban elementary-school children. Journal of Clinical Child Psychology. 1994;23:391–400. [Google Scholar]
- Bar-Haim Y, Lamy D, Pergman L, Bakermans-Kranenburg MJ, van Ijzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin. 2007;133:1–24. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- Barratt ES, Patton JH. Impulsivity: Cognitive, behavioral, and psychophysiological correlates. In: Zuckerman M, editor. The biological bases of sensation seeking, impulsivity, and anxiety. Hillsdale, NJ: Erlbaum; 1983. pp. 71–117. [Google Scholar]
- Barrett PM, Rapee RM, Dadds MR, Ryan SM. Family enhancement of cognitive style in anxious and aggressive children: Threat bias and the FEAR effect. Journal of Abnormal Child Psychology. 1996;24:187–203. doi: 10.1007/BF01441484. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP. Vagal tone, development, and Gray’s motivational theory: Toward an integrated model of autonomic nervous system functioning in psychopathology. Development and Psychopathology. 2001;13:183–214. doi: 10.1017/s0954579401002012. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Katkin ES, Strassberg Z, Snarr J. Disinhibitory psychopathology in male adolescents: Discriminating conduct disorder from attention-deficit/ hyperactivity disorder through concurrent assessment of multiple autonomic states. Journal of Abnormal Psychology. 2001;110:610–624. doi: 10.1037//0021-843x.110.4.610. [DOI] [PubMed] [Google Scholar]
- Beck AT, Emery G. Anxiety disorders and phobias: A cognitive perspective. New York: Basic Books; 1985. [Google Scholar]
- Bell-Dolan DJ. Social cue interpretation of anxious children. Journal of Clinical Child Psychology. 1995;24:1–10. [Google Scholar]
- Bell-Dolan DJ, Foster SL, Christopher JS. Girls’ peer relations and internalizing problems: Are socially neglected, rejected, and withdrawn girls at risk? Journal of Clinical Child Psychology. 1995;24:463–473. [Google Scholar]
- Bird HR, Gould MS, Staghezza BM. Patterns of diagnostic comorbidity in a community sample of children aged 9 through 16 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:361–368. doi: 10.1097/00004583-199303000-00018. [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Costello EJ, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry. 2007;48:1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- Bogels SM, Zigterman D. Dysfunctional cognitions in children with social phobia, separation anxiety disorder and generalized anxiety disorder. Journal of Abnormal Child Psychology. 2000;28:205–211. doi: 10.1023/a:1005179032470. [DOI] [PubMed] [Google Scholar]
- Bogenschutz MP, Nurnberg HG. Theoretical and methodological issues in psychiatric comorbidity. Harvard Review of Psychiatry. 2000;8:18–24. [PubMed] [Google Scholar]
- Brestan EV, Eyberg SM. Effective psychosocial treatments of conduct-disordered children and adolescences: 29 years, 82 studies, and 5, 272 kids. Journal of Clinical Child Psychology. 1998;27:180–189. doi: 10.1207/s15374424jccp2702_5. [DOI] [PubMed] [Google Scholar]
- Broidy LM, Nagin DS, Tremblay RW, Bates JE, Brame B, Dodge KA, et al. Developmental trajectories of childhood disruptive behaviors and adolescent delinquency: A six-site, cross-national study. Developmental Psychology. 2003;39:222–245. doi: 10.1037//0012-1649.39.2.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RT, Maden-Swain A, Baldwin K. Gender differences in a clinic referred sample of attention-deficit-disordered children. Child Psychiatry and Human Development. 1991;22:111–128. doi: 10.1007/BF00707789. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46:1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Card NA, Little TD. Proactive and reactive aggression in childhood and adolescence: A meta-analysis of differential relations with psychosocial adjustment. International Journal of Behavioral Development. 2006;30:466–480. [Google Scholar]
- Caron C, Rutter M. Comorbidity in child psychopathology: Concepts, issues, and research strategies. Journal of Child Psychology and Psychiatry. 1991;32:1063–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- Chase RM, Eyberg SM. Clinical presentation and treatment outcome for children with comorbid externalizing and internalizing symptoms. Anxiety Disorders. 2008;22:273–282. doi: 10.1016/j.janxdis.2007.03.006. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Barlow DH. The development of anxiety: The role of control in the early environment. Psychological Bulletin. 1998;124:3–21. doi: 10.1037/0033-2909.124.1.3. [DOI] [PubMed] [Google Scholar]
- Cleckley H. The mask of sanity. St. Louis, MO: Mosby; 1982. [Google Scholar]
- Connor D, Steingard RJ, Anderson JJ, Melloni RH. Gender differences in reactive and proactive aggression. Child Psychiatry and Human Development. 2003;33:279–294. doi: 10.1023/a:1023084112561. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child and Adolescent Psychiatric Clinics of North America. 2005;14:631–648. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Crick N, Dodge KA. A review and reformulation of social information processing mechanisms in children’s social adjustment. Psychological Bulletin. 1994;115:74–101. [Google Scholar]
- Crick NR, Ladd GW. Children’s perceptions of the outcomes of aggressive strategies: Do the ends justify being mean? Developmental Psychology. 1990;26:612–620. [Google Scholar]
- Crowell SE, Beauchaine TP, Gatzke-Kopp L, Sylvers P, Mead H, Chipman-Chacon J. Autonomic correlates of attention-deficit/hyperactivity disorder and oppositional defiant disorder in preschool children. Journal of Abnormal Psychology. 2006;115:174–178. doi: 10.1037/0021-843X.115.1.174. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Barrett PM, Rapee RM, Ryan S. Family process and child anxiety and aggression: An observational analysis. Journal of Abnormal Child Psychology. 1996;24:715–734. doi: 10.1007/BF01664736. [DOI] [PubMed] [Google Scholar]
- DeGarmo DS, Patterson GR, Forgatch MS. How do outcomes in a specified parent training intervention maintain or wane over time? Prevention Science. 2004;5:73–89. doi: 10.1023/b:prev.0000023078.30191.e0. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:493–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Dodge KA. The structure and function of reactive and proactive aggression. In: Pepler DJ, Rubin KH, editors. The development and treatment of childhood aggression. Hillsdale, NJ: Erlbaum; 1994. pp. 201–218. [Google Scholar]
- Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science. 1990a;250:1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Coie J. Social information processing factors in reactive and proactive aggression in children’s peer groups. Journal of Personality and Social Psychology. 1987;53:1146–1158. doi: 10.1037//0022-3514.53.6.1146. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Frame CL. Social cognitive biases and deficits in aggressive boys. Child Development. 1982;53:620–635. [PubMed] [Google Scholar]
- Dodge KA, Lochman JE, Harnish JD, Bates JE, Pettit GS. Reactive and proactive aggression in school children and psychiatrically impaired chronically assaultive youth. Journal of Abnormal Psychology. 1997;106:37–51. doi: 10.1037//0021-843x.106.1.37. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Newman JP. Biased decision-making processes in aggressive boys. Journal of Abnormal Psychology. 1981;106:37–51. doi: 10.1037//0021-843x.90.4.375. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Price J, Bachorowski J, Newman J. Hostile attributional biases in severely aggressive adolescents. Journal of Abnormal Psychology. 1990b;99:385–392. doi: 10.1037//0021-843x.99.4.385. [DOI] [PubMed] [Google Scholar]
- Dollard J, Doob LW, Miller NE, Mowrer OH, Sears RR. Frustration and aggression. New Haven, CT: Yale University Press; 1939. [Google Scholar]
- Drabick DA, Gadow KD, Loney J. Co-occurring ODD and GAD symptom groups: Source-specific syndromes and cross-informant comorbidity. Journal of Clinical Child and Adolescent Psychology. 2008;37:314–326. doi: 10.1080/15374410801955862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Farmer EMZ, Compton SN, Burns BJ, Robertson E. Review of the evidence base for treatment of childhood psychopathology: Externalizing disorders. Journal of Consulting and Clinical Psychology. 2002;70:1267–1302. doi: 10.1037//0022-006x.70.6.1267. [DOI] [PubMed] [Google Scholar]
- Ferro T, Klein DN. Assessment of comorbidity. In: Wetzler S, Sanderson WC, editors. Treatment strategies for patients with psychiatric comorbidity. Hoboken, NJ: Wiley; 1997. pp. 49–71. [Google Scholar]
- Flannery-Schroeder E, Suveg C, Safford S, Kendall PC, Webb A. Comorbid externalising disorders and child anxiety treatment outcomes. Behaviour Change. 2004;21:14–25. [Google Scholar]
- Fleitlich-Bilyk B, Goodman R. Prevalence of child and adolescent psychiatric disorders in southeast Brazil. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:727–734. doi: 10.1097/01.chi.0000120021.14101.ca. [DOI] [PubMed] [Google Scholar]
- Foley DL, Pickles A, Maes HM, Silberg JL, Eaves LJ. Course and short-term outcomes of separation anxiety disorder in a community sample of twins. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:1107–1114. doi: 10.1097/01.chi.0000131138.16734.f4. [DOI] [PubMed] [Google Scholar]
- Ford T, Goodman R, Meltzer H. The British child and adolescent mental health survey 1999: The prevalence of DSM-IV disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- French DC. Heterogeneity of peer rejected girls. Child Development. 1990;61:2028–2031. doi: 10.1111/j.1467-8624.1988.tb03250.x. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Cornell AH, Barry CT, Bodin SD, Dane HE. Callous-unemotional traits and conduct problems in the prediction of conduct problem severity, aggression, and self-report of delinquency. Journal of Abnormal Child Psychology. 2003;31:457–470. doi: 10.1023/a:1023899703866. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Lilienfeld SO, Ellis M, Loney B, Silverthorn P. The association between anxiety and psychopathy dimensions in children. Journal of Abnormal Child Psychology. 1999;27:383–392. doi: 10.1023/a:1021928018403. [DOI] [PubMed] [Google Scholar]
- Garland EJ, Garland OM. Correlation between anxiety and oppositionality in a children’s mood and anxiety disorder clinic. Canadian Journal of Psychiatry. 2001;46:953–958. doi: 10.1177/070674370104601008. [DOI] [PubMed] [Google Scholar]
- Gaub M, Carlson CL. Gender differences in ADHD: A meta-analysis and critical review. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1036–1045. doi: 10.1097/00004583-199708000-00011. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Buss KA, Lemery KS. Toddler and childhood temperament: Expanded content, stronger genetic evidence, new evidence for the importance of environment. Developmental Psychology. 1997;33:891–905. doi: 10.1037//0012-1649.33.6.891. [DOI] [PubMed] [Google Scholar]
- Gorman-Smith D, Tolan P. The role of exposure to community violence and developmental problems among inner-city youth. Development and Psychopathology. 1998;10:101–116. doi: 10.1017/s0954579498001539. [DOI] [PubMed] [Google Scholar]
- Gray JA. The neuropsychology of anxiety: An enquiry into the functions of the septo-hippocampal system. Oxford: Oxford University Press; 1982. [Google Scholar]
- Gregory AM, Eley TC. Genetic influences on anxiety in children: What we’ve learned and where we’re heading. Clinical Child and Family Psychology. 2007;10:199–212. doi: 10.1007/s10567-007-0022-8. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Eley TC, Plomin R. Exploring the association between anxiety and conduct problems in a large sample of twins aged 2–4. Journal of Abnormal Child Psychology. 2004;32:111–122. doi: 10.1023/b:jacp.0000019765.29768.1c. [DOI] [PubMed] [Google Scholar]
- Guerra NG, Huesmann LR, Spindler A. Community violence exposure, social cognition, and aggression among urban elementary school children. Child Development. 2003;74:1561–1576. doi: 10.1111/1467-8624.00623. [DOI] [PubMed] [Google Scholar]
- Hubbard JA, Smithmyer CM, Ramsden SR, Parker EH, Flanagan KD, Dearing KF, et al. Observational, physiological, and self-report measures of children’s anger: Relations to reactive versus proactive aggression. Child Development. 2002;73:1101–1118. doi: 10.1111/1467-8624.00460. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Rapee RM. Parent-child interactions and the anxiety disorders: An observational analysis. Behaviour Research and Therapy. 2001;39:1411–1427. doi: 10.1016/s0005-7967(00)00107-8. [DOI] [PubMed] [Google Scholar]
- Hughes JN, Meehan BT, Cavell TA. Development and validation of a gender-balanced measure of aggression-relevant social cognition. Journal of Clinical Child and Adolescent Psychology. 2004;33:292–302. doi: 10.1207/s15374424jccp3302_11. [DOI] [PubMed] [Google Scholar]
- Ialongo N, Edelsohn G, Werthamer-Larsson L, Kellam S. The significance of self-reported anxious symptoms in first grade children. Journal of Abnormal Child Psychology. 1994;22:441–456. doi: 10.1007/BF02168084. [DOI] [PubMed] [Google Scholar]
- Ingram RE, Kendall PC. The cognitive side of anxiety. Cognitive Therapy and Research. 1987;11:523–536. [Google Scholar]
- Kaplan BJ, Dewey DM, Crawford SG, Wilson BN. The term comorbidity is of questionable value in reference to developmental disorders: Data and theory. Journal of Learning Disabilities. 2001;34:555–565. doi: 10.1177/002221940103400608. [DOI] [PubMed] [Google Scholar]
- Kempes M, Matthys W, Maassen G, van Goozen S, van Engeland H. A parent questionnaire for distinguishing between reactive and proactive aggression in children. European Child and Adolescent Psychiatry. 2006;15:38–45. doi: 10.1007/s00787-006-0502-2. [DOI] [PubMed] [Google Scholar]
- Kendall PC. Treating anxiety disorders in children: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 1994;62:100–110. doi: 10.1037//0022-006x.62.1.100. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Brady EU, Verduin TL. Comorbidity in childhood anxiety disorders and treatment outcome. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:787–794. doi: 10.1097/00004583-200107000-00013. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Clarkin JF. Introduction to Special Section: Comorbidity and treatment implications. Journal of Clinical and Consulting Psychology. 1992;60:833–834. [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:366–380. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- Klein DN, Riso LP. Psychiatric disorders: Problems of boundaries and comorbidity. In: Costello CG, editor. Basic issues in psychopathology. New York: Guilford; 1993. pp. 19–26. [Google Scholar]
- Lakatos K, Nemoda Z, Birkas E, Ronai Z, Kovacs E, Ney K, et al. Association of D4 dopamine receptor gene and serotonin transporter promoter polymorphisms with infants’ response to novelty. Molecular Psychiatry. 2003;8:90–97. doi: 10.1038/sj.mp.4001212. [DOI] [PubMed] [Google Scholar]
- Last C, Perrin S, Hersen M, Kazdin AE. A prospective study of childhood anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1502–1510. doi: 10.1097/00004583-199611000-00019. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Cicchetti C, Gibbons RD, Binns HJ, Larsen L, DeVito C. Oppositional defiant disorder with onset in preschool years: Longitudinal stability and pathways to other disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1393–1400. doi: 10.1097/00004583-200112000-00009. [DOI] [PubMed] [Google Scholar]
- Lee SS, Lahey BB, Waldman I, Van Hulle CA, Rathouz P, Pelham WE, et al. Association of dopamine transporter genotype with disruptive behavior disorders in an eight year longitudinal study of children and adolescents. American Journal of Medical Genetics: Part B, Neuropsychiatric Genetics. 2007;144:310–317. doi: 10.1002/ajmg.b.30447. [DOI] [PubMed] [Google Scholar]
- Lemerise EA, Arsenio WF. An integrated model of emotion processes and cognition in social information processing. Child Development. 2000;71:107–118. doi: 10.1111/1467-8624.00124. [DOI] [PubMed] [Google Scholar]
- Levy K, Hunt C, Heriot S. Treating comorbid anxiety and aggression in children. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1111–1118. doi: 10.1097/chi.0b013e318074eb32. [DOI] [PubMed] [Google Scholar]
- Little SA, Garber J. Aggression, depression, and stressful life events predicting peer rejection in children. Development and Psychopathology. 1995;7:845–856. [Google Scholar]
- Livingston RL, Dykman RA, Ackerman PT. The frequency and significance of self-reported psychiatric diagnoses in children with attention deficit disorder. Journal of Abnormal Child Psychology. 1990;18:465–478. doi: 10.1007/BF00911102. [DOI] [PubMed] [Google Scholar]
- Loeber R, Keenan K. Interaction between conduct disorder and its comorbid conditions: Effects of age and gender. Clinical Psychology Review. 1994;14:497–523. [Google Scholar]
- Marmorstein N. Relationships between anxiety and externalizing disorders in youth: The influences of age and gender. Journal of Anxiety Disorders. 2007;21:420–432. doi: 10.1016/j.janxdis.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Marsee MA, Frick PJ. Exploring the cognitive and emotional correlates to proactive and reactive aggression in a sample of detained girls. Journal of Abnormal Child Psychology. 2007;35:969–981. doi: 10.1007/s10802-007-9147-y. [DOI] [PubMed] [Google Scholar]
- Marsee MA, Weems CF, Taylor LK. Exploring the association between aggression and anxiety in youth: A look at aggressive subtypes, gender, and social cognition. Journal of Child and Family Studies. 2008;17:154–168. [Google Scholar]
- Martinez P, Richters JE. The NIMH community violence project: II. Children’s distress symptoms associated with violence exposure. Psychiatry. 1993;56:22–35. doi: 10.1080/00332747.1993.11024618. [DOI] [PubMed] [Google Scholar]
- Masi G, Millepiedi S, Mucci M, Poli P, Bertini N, Milantoni L. Generalized anxiety disorder in referred children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:752–760. doi: 10.1097/01.chi.0000121065.29744.d3. [DOI] [PubMed] [Google Scholar]
- Maughan B, Rowe R, Messer J, Goodman R, Meltzer H. Conduct disorder and oppositional defiant disorder in a national sample: Developmental epidemiology. Journal of Child Psychology and Psychiatry. 2004;45:609–621. doi: 10.1111/j.1469-7610.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- Merk W. Development of reactive and proactive aggression in boys. Enschede, Netherlands: Print Partners Ipskamp; 2005. [Google Scholar]
- Milich R, Kramer J. Reflections on impulsivity: An empirical investigation of impulsivity as a construct. In: Gadow KD, editor. Advances in learning and behavioral disabilities. Vol. 3. Greenwich, CT: JAI Press; 1984. pp. 57–94. [Google Scholar]
- Muris P, Kindt M, Bogels SM, Merckelbach H, Gadet B, Moulaert V. Anxiety and threat perception abnormalities in normal children. Journal of Psychopathology and Behavioral Assessment. 2000a;22:183–199. [Google Scholar]
- Muris P, Luermans J, Merkelbach H, Mayer B. Danger is lurking everywhere: The relationship between anxiety and threat perception abnormalities in normal children. Therapy and Experimental Psychiatry. 2000b;31:123–136. doi: 10.1016/s0005-7916(00)00016-1. [DOI] [PubMed] [Google Scholar]
- Neal JA, Edelmann RJ. The etiology of social phobia: Toward a developmental profile. Clinical Psychology Review. 2003;23:761–786. doi: 10.1016/s0272-7358(03)00076-x. [DOI] [PubMed] [Google Scholar]
- Newman JP, Wallace JF. Diverse pathways to deficient self regulation: Implications for disinhibitory psychopathology in children. Clinical Psychology Review. 1993;13:699–720. [Google Scholar]
- Orobio de Casto B, Veerman JW, Koops W, Bosch JD, Monshouwer HJ. Hostile attribution of intent and aggressive behavior: A meta-analysis. Child Development. 2002;73:916–934. doi: 10.1111/1467-8624.00447. [DOI] [PubMed] [Google Scholar]
- Ortiz MAC, del Barrio Gandara V. Study on the relations between temperament, aggression, and anger in children. Aggressive Behavior. 2006;32:207–215. [Google Scholar]
- Pihlakoski L, Sourander A, Aromaa M, Rautava P, Helenius H, Silanpaa M. The continuity of psychopathology from early childhood to preadolescence: A prospective cohort study of 3–12 year old children. European Child and Adolescent Psychiatry. 2006;15:409–417. doi: 10.1007/s00787-006-0548-1. [DOI] [PubMed] [Google Scholar]
- Polman H, Orobio de Castro B, Koops W, van Boxtel HW, Merk WW. A meta-analysis of the distinction between reactive and proactive aggression in children and adolescents. Journal of Abnormal Child Psychology. 2007;35:522–535. doi: 10.1007/s10802-007-9109-4. [DOI] [PubMed] [Google Scholar]
- Puliafico AC, Kendall PC. Threat-related attentional bias in anxious youth: A review. Clinical Child and Family Psychology Review. 2006;9:162–180. doi: 10.1007/s10567-006-0009-x. [DOI] [PubMed] [Google Scholar]
- Rapee R. The influence of comorbidity on treatment outcome for children and adolescents with anxiety disorders. Behavioral Research and Therapy. 2003;41:105–112. doi: 10.1016/s0005-7967(02)00049-9. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Wignall A, Hudson JL, Schneiring CA. Treating anxious children and adolescents: An evidence-based approach. Oakland, CA: New Harbinger; 2000. [Google Scholar]
- Reid SC, Salmon K, Lovibond PF. Cognitive biases in childhood anxiety, depression, and aggression: Are they pervasive or specific? Cognitive Therapy Research. 2006;30:531–549. [Google Scholar]
- Roza SJ, Hofstra MB, van der Ende J, Verhulst FC. Stable prediction of mood and anxiety disorders based on behavioral and emotional problems in childhood: A 14-year follow-up during childhood, adolescence, and young adulthood. American Journal of Psychiatry. 2003;160:2116–2121. doi: 10.1176/appi.ajp.160.12.2116. [DOI] [PubMed] [Google Scholar]
- Russo MF, Beidel DC. Comorbidity of childhood anxiety and externalizing disorders: Prevalence, associated characteristics, and validation issues. Clinical Psychology Review. 1994;14:199–221. [Google Scholar]
- Salmivalli C, Nieminen E. Proactive and reactive aggression among school bullies, victims, and bully-victims. Aggressive Behavior. 2002;28:30–44. [Google Scholar]
- Schwartz D, Proctor LJ. Community violence exposure and children’s social adjustment in the school peer group: The mediating roles of emotion regulation and social cognition. Journal of Consulting and Clinical Psychology. 2000;68:670–683. [PubMed] [Google Scholar]
- Shaw DS, Keenan K, Vondra JI, Delliquadri E, Giovannelli J. Antecedents of preschool children’s internalizing problems: A longitudinal study of low-income families. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1760–1767. [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Meyer JM, Silberg JL, Maes HH, Loeber R, et al. The Virginia twin study of adolescent behavioral development: Influences of age, gender and impairment on rates of disorder. Archives of General Psychiatry. 1997;54:801–808. doi: 10.1001/archpsyc.1997.01830210039004. [DOI] [PubMed] [Google Scholar]
- Singer MI, Anglin TM, Song LY, Longhofer L. Adolescents’ exposure to violence and associated symptoms of psychological trauma. Journal of the American Medical Association. 1995;273:477–482. [PubMed] [Google Scholar]
- Speltz ML, McClellan J, DeKlyen M, Jones K. Preschool boys with oppositional defiant disorder: Clinical presentation and diagnostic change. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:838–845. doi: 10.1097/00004583-199907000-00013. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Avenevoli S. The role of context in the development of psychopathology: A conceptual framework and some speculative propositions. Child Development. 2000;71:66–74. doi: 10.1111/1467-8624.00119. [DOI] [PubMed] [Google Scholar]
- Taghavi MR, Moradi AR, Doost HTN, Yule W, Dalgleish T. Interpretation of ambiguous emotional information in clinically anxious children and adolescents. Cognition and Emotion. 2000;14:809–822. [Google Scholar]
- Tremblay RE, Nagin DS. The developmental origins of physical aggression in humans. In: Tremblay RE, Hartup WW, Archer J, editors. Developmental origins of aggression. New York: Guilford; 2005. pp. 83–106. [Google Scholar]
- Tyson PD. Physiological arousal, reactive aggression, and the induction of an incompatible relaxation response. Aggression and Violent Behavior. 1998;3:143–158. [Google Scholar]
- van Goozen SHM, Fairchild G, Snoek H, Harold GT. The evidence for a neurobiological model of childhood antisocial behavior. Psychological Bulletin. 2007;133:149–182. doi: 10.1037/0033-2909.133.1.149. [DOI] [PubMed] [Google Scholar]
- van Goozen SHM, Matthys W, Cohen-Kettenis PT, Gispen-de Wied C, Wiegent VM, van England H. Salivary cortisol and cardiovascular activity during stress in oppositional-defiant disorder boys and normal controls. Society of Biological Psychology. 1998;43:531–539. doi: 10.1016/S0006-3223(97)00253-9. [DOI] [PubMed] [Google Scholar]
- Vasey MW. Development and cognition in childhood anxiety: The example of worry. Advances in Clinical Child Psychology. 1993;15:1–39. [Google Scholar]
- Vasey MW, Daleiden EL, Williams LL, Brown LM. Biased attention in childhood anxiety disorders: A preliminary study. Journal of Abnormal Child Psychology. 1995;23:267–279. doi: 10.1007/BF01447092. [DOI] [PubMed] [Google Scholar]
- Vitaro F, Barker ED, Boivin M, Brendgen M, Tremblay RE. Do early difficult temperament and harsh parenting differentially predict reactive and proactive aggression? Journal of Abnormal Child Psychology. 2006;34:685–695. doi: 10.1007/s10802-006-9055-6. [DOI] [PubMed] [Google Scholar]
- Vitaro F, Brendgen M, Tremblay RE. Reactively and proactively aggressive children: Antecedent and subsequent characteristics. Journal of Child Psychology and Psychiatry. 2002;43:495–505. doi: 10.1111/1469-7610.00040. [DOI] [PubMed] [Google Scholar]
- Vitaro F, Gendreau PL, Tremblay RE, Oligny P. Reactive and proactive aggression differentially predict later conduct problems. Journal of Child Psychology and Psychiatry. 1998;39:377–385. [PubMed] [Google Scholar]
- Vitiello B, Stoff DM. Subtypes of aggression and their relevance to child psychiatry. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:307–315. doi: 10.1097/00004583-199703000-00008. [DOI] [PubMed] [Google Scholar]
- Wallace JF, Newman JP. Differential effects of reward and punishment cues on response speed in anxious and impulsive individuals. Personality and Individual Differences. 1990;11:999–1009. [Google Scholar]
- Waschbusch DA, Pelham WE, Jennings JR, Greiner AR, Tarter RE, Moss HB. Reactive aggression in boys with disruptive behavior disorders: Behavior, physiology, and affect. Journal of Abnormal Child Psychology. 2002;30:641–656. doi: 10.1023/a:1020867831811. [DOI] [PubMed] [Google Scholar]
- Waschbusch DA, Willoughby MT, Pelham WE. Criterion validity and the utility of reactive and proactive aggression: Comparisons to attention deficit hyperactivity disorder, oppositional defiant disorder, conduct disorder, and other measures of functioning. Journal of Clinical Child Psychology. 1998;27:396–405. doi: 10.1207/s15374424jccp2704_3. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Hammond M. Treating children with early-onset conduct problems: A comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology. 1997;65:93–109. doi: 10.1037//0022-006x.65.1.93. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Hollinsworth T, Kolpacoff M. The long-term effectiveness and clinical significance of three cost-effective training programs for families with conduct-problem children. Journal of Consulting and Clinical Psychology. 1989;57 doi: 10.1037//0022-006x.57.4.550. 550-533. [DOI] [PubMed] [Google Scholar]
- Wellman HM, Harris PL, Banerjee M, Sinclair A. Early understanding of emotion: Evidence from natural language. Cognition and Emotion. 1995;9:117–149. [Google Scholar]
- Young SE, Smolen A, Stallings MC, Corley RP, Hewitt JK. Sibling based association analyses of the serotonin transporter polymorphism and internalizing behavior problems in children. Journal of Child Psychology and Psychiatry. 2003;44:961–967. doi: 10.1111/1469-7610.00180. [DOI] [PubMed] [Google Scholar]
- Youngstrom E, Weist MD, Albus KE. Exploring violence exposure, stress, protective factors, and behavioral problems among inner-city youth. American Journal of Community Psychology. 2003;32:115–129. doi: 10.1023/a:1025607226122. [DOI] [PubMed] [Google Scholar]