Abstract
Reconstruction of the Type II pelvic resection is challenging. Currently available reconstructive options have inherent problems including graft and implant failure, pain, poor function, and high major complication rates. The periacetabular reconstruction (PAR) endoprosthesis was designed to be secured with internal fixation and bone cement to the remaining ilium and support a reconstructed acetabulum. This construct potentially avoids the complications of graft or hardware failure, while maintaining early mobilization, comfort, limb lengths, and function. We retrospectively reviewed 25 patients who underwent Type II pelvic resection and reconstruction with the PAR endoprosthesis, analyzing function, complications, and survivorship. The minimum followup was 13 months (mean, 29.4 months; range, 13 to 108 months). We compared the PAR data with the literature for the Mark II saddle endoprosthesis. The PAR’s average MSTS score was 20.8 (67%), major complications occurred in 14 (56%), and implant survivorship was 84% at 2 years and 60% at 5 years. The rate of failure at the ilium-saddle interface was lower and implant survivorship higher than those in the published literature for the Mark II saddle. We recommend use of the PAR endoprosthesis for reconstruction of large defects following Type II pelvic resection. The modified saddle design provides greater inherent stability, allowing for faster rehabilitation and improved longevity without increased complications and is an improvement over the currently available saddle prostheses.
Level of Evidence: Level III, retrospective case series. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The pelvis is the third most common site for metastatic disease and the site of 10% to 15% of primary sarcomas. Pelvic resection for malignancy can be classified by region, according to the system of Enneking and Dunham [11]. Type II, or periacetabular, lesions are particularly difficult to treat, and their reconstruction results in a higher mechanical complication rate than resections involving the ilium (Type I) or pubis (Type III) alone [7]. The surgical goals for treatment of periacetabular malignancy are primarily aimed toward wide surgical resection in the case of primary sarcomas and the elimination of pain in the case of metastatic disease; however, in both cases, surgeons seek a stable and durable reconstruction, adequate soft tissue reconstruction, preservation or improvement of function, and uneventful wound healing. Many procedures have evolved to help fulfill these goals, including external hemipelvectomy [4, 5, 18], resection without reconstruction (internal hemipelvectomy) [7, 8, 14, 18, 30], arthrodesis [14, 18], cement and screw or pin fixation [25, 29], rotationplasty [19], pure allograft reconstruction [6, 10, 17, 18, 24, 27, 31, 32], allograft-prosthetic-composite reconstruction [17, 18], and autoclaved or irradiated autograft [17, 29]. None of these procedures seems superior, and each comes with its share of disadvantages—with MSTS scores ranging from 45% to 70% of normal, and major complication rates ranging from 30% to 100%.
To address the limitations of these reconstructive options, a variety of endoprostheses have been developed. Standard endoprostheses include custom and modular implants that are cage derivations that anatomically reconstruct and conjoin anterior and posterior columns. These implants experience hip joint reaction forces of up to 5.5 times body weight even with level walking [23], which theoretically may exceed the implant’s minimal fixation; and, in the setting of tumor resection the implants may provide inadequate articular constraint in the setting of compromised soft tissue stabilizers. Subsequently, these cage derivations are associated with complication rates ranging from 39% to 83% and MSTS scores ranging from 37% to 70% [2, 15, 16, 20, 27, 31]. The saddle design consists of a smooth cradle that rides in the ilium for both support and articulation [26]. The Mark I (Link Orthopaedics, Hamburg, Germany) first-generation saddle endoprosthesis offers a durable, stable reconstruction that can replace large defects, but offers no modularity, is rigid, and reportedly has a high incidence of cephalad migration (100%) and a major complication rate of 64% including infection (34%), fracture, loosening, dislocation, instability, and stiffness [26]. The Mark II saddle (Link Orthopaedics, Hamburg, Germany) is a second-generation design that offers improved mobility, improved stability, more anatomic reconstruction, increased modularity, and improved function (MSTS scores, 51%–63%). However, the Mark II requires additional iliac resection, cannot adapt for extra tumor resection, and provides an unstable articulation at ilium, as evidenced by 87% of the 29% to 52% mechanical failures occurring at the ilium-saddle interface [1, 3, 9, 22, 28]. Accordingly, the survival of these implants ranges from 33% to 53% at 3 years [9, 28]. Noting the problems in design, Aboulafia et al. stated, “hopefully, modifications in the design of the prosthesis will help minimize the mechanical complications [1].” To address these problems with Type II pelvic reconstructions, we developed the PAR periacetabular endoprosthesis, which is a modular third-generation saddle endoprosthesis consisting of a wide iliac wing component that is secured to the ilium with three cross bolts and cement, with a constrained bipolar ball and socket joint and a modular standard or endoprosthetic femoral stem. This article represents a continuation of a previous publication [13], which was a preliminary report on the initial PAR patients. In the current study, the number of patients has increased from 21 to 25, and mean followup of all patients (including the deceased) increased from 20.5 months to 29.4 months. In the ten remaining live patients, average follow up was 57.6 months (range (13–108), with all of these live patients having two year minimum followup except one. The previous article looked at early complications and MSTS scores, but offered no survivorship analysis or comparison with historical controls. This article seeks to provide longer followup with more patients regarding functional outcome and complications, as well as to document the PAR’s survivorship and comparison with other modes of reconstruction.
To examine the differences of this modified saddle design in the treatment of a difficult problem with no easy answers, we asked the following questions: (1) What functional outcome can one expect with the PAR? (2) What complications arise as a result of using the PAR endoprosthesis? (3) What is the PAR’s survivorship? (4) How does the PAR compare to the historical published data of earlier generation saddle endoprostheses?
Patients and Methods
We retrospectively reviewed all 25 patients who underwent PAR reconstruction for Type II pelvic resection from July 2000 to July 2009. There were no exclusion criteria. Indications for reconstruction included Type II pelvic resection for malignancy. Contraindications included inability to tolerate an extensive surgical procedure. We also performed an in-depth review of the literature regarding Mark II saddle endoprosthesis, comparing MSTS scores, complications, and survivorship. Of the 25 PAR patients, 12 were men, 13 women, and the average age was 54.6 years (range, 29–81 years). The diagnosis was primary sarcoma in eight and metastatic carcinoma in 17 (Table 1). At the time of the study, 10 patients were still alive, and minimum followup was 13 months (average, 29.4 months; range, 13–108 months). No patients were lost to followup. This study was approved by our institution’s ethical board review.
Table 1.
Diagnosis of PAR cases
| Primary sarcoma (8) | Metastatic carcinoma (17) |
|---|---|
| Chondrosarcoma (6) | Renal CA (7) |
| Ewing’s sarcoma (1) | Breast CA (3) |
| Osteogenic sarcoma (1) | Thyroid CA (1) |
| Lung CA (2) | |
| Bladder CA (1) | |
| Ovarian CA (1) | |
| Uterus CA (1) | |
| Gallbladder CA (1) |
In design, the PAR is a third-generation saddle endoprosthesis with a wide iliac wing component and large surface area that is secured to ilium with three cross bolts and cement, theoretically allowing for more stable iliac fixation and the freedom to perform more aggressive iliac resection (Fig. 1A–B). The PAR has a constrained bipolar ball and socket giving range of motion and stability; it is also highly flexible, with a modular head and attached “elbow,” and a modular femoral stem, which improves stability and limb-length equality (Fig. 1C). In addressing the previous mechanical complications found with earlier generation saddles: loosening, migration, and dissociation are mitigated by secure cross-bolting and cementation; dislocation and instability is tempered by cross-bolting and cementation, a constrained articulation, and by modularity that improves soft tissue tension; stiffness is resolved with the prosthetic ball and socket joint that allows for flexion to 90°; and fracture is addressed by the wide dispersion of contact forces that minimizes stress shielding.
Fig. 1A–C.
These figures demonstrate (A) a fully assembled periacetabular endoprosthesis (PAR); (B) the iliac cross-bolting mechanism of the PAR that differentiates it from earlier generation saddle endoprostheses; and (C) the modular components of the PAR that improve reconstructive options.
Surgical technique begins with the patient placed in the supine position with a bump under the involved hip and both extremities prepped in the surgical field. This positioning facilitates fluoroscopic imaging and clinical evaluation of limb lengths. The surgical approach is extended iliofemoral and the Type II pelvic resection is performed in the manner indicated by the disease, though a horizontal iliac osteotomy must be made. A central notch is made at the iliac osteotomy with a high-speed burr, the iliac component is placed as far posteriorly and medially as possible on the remaining ilium, and three cross-locking bolts are drilled from the outer plate of the implant through to the inner plate in order to provide stable fixation to the remaining bone.
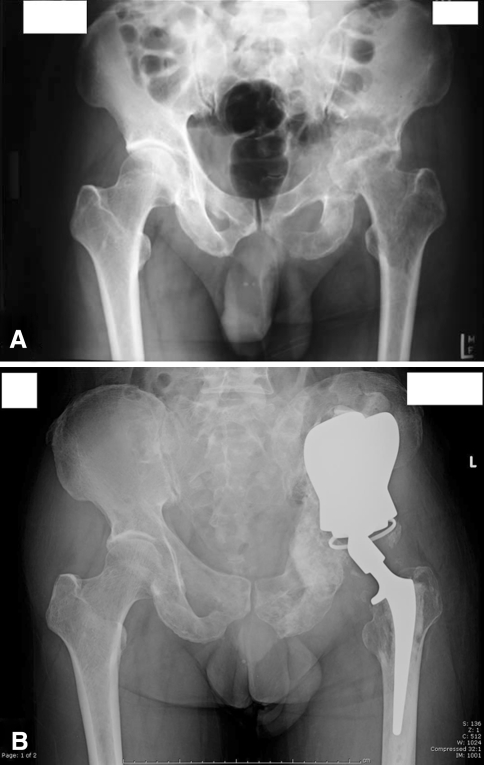
Polymethylmethacrylate cement is applied to the spaces between the wing plates and the ilium on both sides for additional fixation. Trial components are then inserted and tested for stability, soft tissue tension, and limb-length equality, and the final components implanted—with the femoral stem and the modular “head-elbow” providing modularity (Fig. 1C). Preoperative radiographs of the disease (Fig. 2A) and postoperative radiographs of the PAR reconstruction (Fig. 2B) are shown.
Fig. 2A–B.
These figures illustrate the case of a 46-year-old male with metastatic bronchogenic carcinoma to the left acetabulum, requiring type II pelvic resection and PAR reconstruction for pain control and functional improvement, showing the (A) preoperative AP radiograph revealing periacetabular disease; and the (B) postoperative AP radiograph demonstrating a secure iliac interface (through cross-bolting and cement) and an anatomic reconstruction.
Postoperatively, we immediately mobilized the patients and allowed weight bearing with walking assists as tolerated. Physical therapy was initiated on postoperative day 1, using a front wheel walker for ambulation, which was converted to crutches followed by a cane in the opposite hand at a time deemed appropriate by the therapist.
We used the 1993 MSTS lower extremity scores to measure function [12]. This scoring system is a validated and reliable measure [12] that accounts for pain, function, emotional acceptance, need for supports, walking ability, and gait. MSTS scores were measured at the time of latest followup (even in patients who had implants removed). Complications were defined as adverse events causing morbidity. Implant survivorship was defined as number of live patients who retained implants.
All data were entered into an Excel (Microsoft Corporation, Redmond, WA) spreadsheet for analysis. The proportions regarding MSTS scores and complications of the Mark II literature and the PAR patients in our study were then compared by the chi square test to determine statistical differences between them. We performed Kaplan-Meier survivorship analysis from the date of operation to the endpoints of loss of implants and survival, set to a 95% confidence interval. Statistical tests were two-sided and MedCalc (MedCalc Software, Broekstraat 52, Belgium) statistical software was used for the data analysis.
Results
The mean MSTS score was 21 (range 11 to 27), which was 67% of normal. The highest mean scores were seen with emotional acceptance (4.3), pain (4.1), and function (4.0). The lowest mean scores obtained were in patients with persistent infection that required resection of implants. All of these resected patients were ambulatory but required the use of assistive devices (cane, walker, crutches) and all had persistent limp. All patients achieved at least 90° of hip flexion, with mean hip abduction of 12°, and hip external rotation of 16°.
Fourteen of 25 patients (56%) had at least one major complication. The most notable complications consisted of deep infections in six, local recurrence in five, dislocation in three, and fracture in two (Table 2). Of the six deep infections, five underwent resection arthroplasty, and one retained the implants after irrigation and débridement (I&D) and suppressive antibiotics. The two superficial infections resolved with incision and drainage and short-term antibiotics. The single case of skin necrosis was treated successfully with skin grafting. Two of the patients with chondrosarcoma and three of the patients with metastatic disease experienced local recurrence. Two of these patients experienced pathologic fracture related to their recurrence and underwent revision accordingly. There were three dislocations, two of which occurred after falls resulting in dislocations through the constrained acetabular liner. Both underwent successful revision with a new constrained liner. One patient dislocated at the Morse taper between the femoral stem and the “head-elbow” piece. Other complications included a rotational deformity that was treated successfully with rotational osteotomy, one case of severe heterotopic ossification resulting in no clinical impairment (Fig. 3), a case of DIC resulting in intraoperative mortality, and a case of cardiac arrest.
Table 2.
Complications of PAR cases
| Complication | Number (%) |
|---|---|
| Deep infections | 6 (24%) |
| Superficial infections | 2 (8%) |
| Wound complication | 1 (4%) |
| Local recurrence | 5 (20%) |
| Fracture | 2 (8%) |
| Dislocations | 3 (12%) |
| Rotational deformity | 1 (4%) |
| Intraoperative mortality | 1 (4%) |
Fig. 3.
This radiograph is an example of extensive heterotopic ossification, one of the PAR’s major complications.
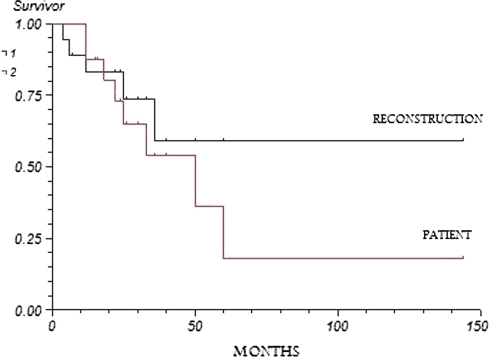
The PAR patients had 84% implant survival and 65% patient survival at 2 years, a 72% implant survival and 54% patient survival at 3 years, and a 60% implant survival and 15% patient survival at 5 years (Fig. 4).
Fig. 4.
This figure shows the Kaplan-Meier survival curves of PAR patients in regard to survivorship of implants (reconstruction [95% CI of 52.2 to 135.5]) and the survivorship of life (patient [95% CI of 22.4 to 89.1]) from the time of surgery.
Discussion
Type II pelvic resections are particularly problematic from the standpoint of reconstruction. Many reconstructive procedures have evolved, each with their disadvantages. Early generation saddle endoprostheses were developed to be an answer to this reconstructive problem, but their design results in an unacceptably high rate (29% to 52%) of mechanical complications [1, 3, 9, 22, 28]. Therefore, we developed a new third-generation saddle design. We performed this study to evaluate this new endoprosthesis in terms of function, complications, and survivorship, and to compare these outcomes to the current saddle endoprosthesis.
The limitations of this study begin with numbers. Because of the relatively low numbers of Type II pelvic resections performed, we do not have the sample size of traditional arthroplasty studies. These limited numbers do not allow us to perform subcohort analyses or to analyze factors influencing survival or other outcomes. The limited numbers likely precluded us from identifying some differences in outcomes. However, our data compare with other published data regarding periacetabular reconstruction, and even with small numbers we are still able to show differences in regard to mechanical failure. Second, the retrospective nature of the study does not allow us to control for confounding variables; however, in the case of complex oncologic cases, it is unlikely that these variables could ever be controlled even prospectively. Though not fully controlled (for diagnosis, medical comorbidities, etc.), the data give an accurate general reflection of the type of patients who would undergo such a procedure.
Our average MSTS score of 67% compares favorably with other periacetabular reconstructions (Table 3). Our major complication rate of 56% also compares favorably with the literature (Table 4). Our implant survivorship of 78% at 2 years and 65% at 3 years is higher than that of the Mark II and also compares with the data regarding survivorship of other periacetabular reconstructions (Table 5). In comparison with the Mark II saddle historical data, no differences were seen with the average MSTS scores. The Mark II saddles had a major complication rate of 31% and higher, with mechanical failure occurring in 29% to 52% of cases [1, 3, 9, 22, 28]. In 87% of these cases, the failure occurred at the ilium-saddle interface. This overall incidence of 33% failure at the ilium-saddle interface was higher (p < 0.0001) than that of the PAR’s (0%). The PAR’s 72% survivorship at 3 years was also higher than the saddle’s published survivorship of 33% (p = 0.029) and 53% at 3 years (p = 0.38) [9, 28].
Table 3.
MSTS scores of alternative reconstructions
Table 4.
Complications of alternative reconstructions
| Reconstructive method | % Complications |
|---|---|
| Hemipelvectomy [4, 5] | 29–80% |
| Resection alone [8, 14, 18, 30] | 30–55% |
| Arthrodesis [14, 18] | 25% |
| Cement and screws/pins [25, 29] | 33% |
| Graft reconstruction [6, 10, 17, 21, 24, 32] | 36–89% |
| Custom endoprosthesis [2, 15, 16, 20, 27, 31] | 39–83% |
| Saddle endoprosthesis [1, 3, 9, 22, 26, 28] | 31–100% |
Table 5.
Survivorship of alternative reconstructions
Though difficult to ascertain with the limited numbers in the literature, the question arises to whether the PAR is superior to no reconstruction at all, eg, resection arthroplasty or iliofemoral fusion. The outcomes (Table 3) and complications (Table 4) are comparable; however, these procedures often require prolonged postoperative immobilization or activity restriction, which may be problematic in medically compromised individuals. Conversely, the PAR allows for postoperative weight bearing as tolerated; furthermore, in our experience, it allows for immediate, relatively painless, and unrestricted ambulation with equal limb lengths. We feel that this ability to mobilize early and comfortably improves the overall medical state of the patient.
In conclusion, the PAR endoprosthesis provides pain relief, function, and ambulatory ability with rates of complications similar to other reconstructive options. The PAR results in decreased mechanical failure at the ilium prosthetic interface compared to the standard saddle prostheses; and the survivorship of the PAR is higher than that of second-generation saddles at equivalent duration. In patients with tumors of the pelvis requiring Type II pelvic resection, we believe the PAR is an acceptable reconstructive option that offers advantages of early patient mobilization, stability, flexibility, and durability.
Acknowledgments
We thank the faculty and staff of the University of Southern California Medical Center, who are our partners in patient care and our search for medical knowledge and improvement.
Footnotes
The lead author (LRM) is a consultant for Stryker, has patents on the device reported, and certifies that he has or may receive payments or benefits from a commercial entity related to this work.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
The study was performed at University of Southern California + Los Angeles County Medical Center, Los Angeles, CA.
References
- 1.Aboulafia AJ, Buch R, Mathews J, Li W, Malawer MM. Reconstruction using the saddle prosthesis following excision of primary and metastatic periacetabular tumors. Clin Orthop Relat Res. 1995;314:203–213. [PubMed]
- 2.Abudu A, Grimer RJ, Cannon SR, Carter SR, Sneath RS. Reconstruction of the hemipelvis after the excision of malignant tumours. Complications and functional outcome of prostheses. J Bone Joint Surg Br. 1997;79:773–779. [DOI] [PubMed]
- 3.Aljassir F, Beadel GP, Turcotte RE, Griffin AM, Bell RS, Wunder JS, Isler MH. Outcome after pelvic sarcoma resection reconstructed with saddle prosthesis. Clin Orthop Relat Res. 2005;438:36–41. [DOI] [PubMed]
- 4.Apffelstaedt JP, Driscoll DL, Spellman JE, Velez AF, Gibbs JF, Karakousis CP. Complications and outcome of external hemipelvectomy in the management of pelvic tumors. Ann Surg Oncol. 1996;3:304–309. [DOI] [PubMed]
- 5.Beck LA, Einertson MJ, Winemiller MH, DePompolo RW, Hoppe KM, Sim FF. Functional outcomes and quality of life after tumor-related hemipelvectomy. Phys Ther. 2008;88:916–927. [DOI] [PubMed]
- 6.Bell RS, Davis AM, Wunder JS, Buconjic T, McGoveran B, Gross AE. Allograft reconstruction of the acetabulum after resection of stage-IIB sarcoma. Intermediate-term results. J Bone Joint Surg Am. 1997;79:1663–1674. [DOI] [PubMed]
- 7.Campanacci M, Capanna R. Pelvic resections: the Rizzoli Institute experience. Orthop Clin North Am. 1991;22:65–86. [PubMed]
- 8.Capanna R, Manfrini M, Pignatti G, Martelli C, Gamberini G, Campanacci M. Hemipelvectomy in malignant neoplasms of the hip region. Ital J Orthop Traumatol. 1990;16:425–437. [PubMed]
- 9.Cottias P, Jeanrot C, Vinh TS, Tomeno B, Anract P. Complications and functional evaluation of 17 saddle prostheses for resection of periacetabular tumors. J Surg Oncol. 2001;78:90–100. [DOI] [PubMed]
- 10.Delloye C, Banse X, Brichard B, Docquier PL, Cornu O. Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. J Bone Joint Surg Am. 2007;89:579–587. [DOI] [PubMed]
- 11.Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am. 1978;60:731–746. [PubMed]
- 12.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246. [PubMed]
- 13.Falkinstein Y, Ahlmann ER, Menendez LR. Reconstruction of type II pelvic resection with a new peri-acetabular reconstruction endoprosthesis. J Bone Joint Surg Br. 2008;90:371–376. [DOI] [PubMed]
- 14.Fuchs B, O’Connor MI, Kaufman KR, Padgett DJ, Sim FH. Iliofemoral arthrodesis and pseudarthrosis: a long-term functional outcome evaluation. Clin Orthop Relat Res. 2002;397:29–35. [DOI] [PubMed]
- 15.Gradinger R, Rechl H, Ascherl R, Plötz W, Hipp E. Partial endoprosthetic reconstruction of the pelvis in malignant tumors. Orthopade. 1993;22:167–173. [PubMed]
- 16.Guo W, Li D, Tang X, Yang Y, Ji T. Reconstruction with modular hemipelvic prostheses for periacetabular tumor. Clin Orthop Relat Res. 2007;461:180–188. [DOI] [PubMed]
- 17.Harrington KD. The use of hemipelvic allografts or autoclaved grafts for reconstruction after wide resections of malignant tumors of the pelvis. J Bone Joint Surg Am. 1992;74:331–341. [PubMed]
- 18.Hillmann A, Hoffmann C, Gosheger G, Rödl R, Winkelmann W, Ozaki T. Tumors of the pelvis: complications after reconstruction. Arch Orthop Trauma Surg. 2003;123:340–344. [DOI] [PubMed]
- 19.Hillmann A, Rosenbaum D, Gosheger G, Hoffmann C, Rödl R, Winkelmann W. Rotationplasty Type B IIIa According to Winkelmann: Electromyography and Gait Analysis. Clin Orthop Relat Res. 2001;384:224–231. [DOI] [PubMed]
- 20.Jaiswal PK, Aston WJ, Grimer RJ, Abudu A, Carter S, Blunn G, Briggs TW, Cannon S. Peri-acetabular resection and endoprosthetic reconstruction for tumours of the acetabulum. J Bone Joint Surg Br. 2008;90:1222–1227. [DOI] [PubMed]
- 21.Kim HS, Kim KJ, Han I, Oh JH, Lee SH. The use of pasteurized autologous grafts for periacetabular reconstruction. Clin Orthop Relat Res. 2007;464:217–223. [DOI] [PubMed]
- 22.Kitagawa Y, Ek ET, Choong PF. Pelvic reconstruction using saddle prosthesis following limb salvage operation for periacetabular tumour. J Orthop Surg (Hong Kong). 2006;14:155–162. [DOI] [PubMed]
- 23.Kotzar GM, Davy DT, Goldberg VM, Heiple KG, Berilla J, Heiple KG Jr, Brown RH, Burstein AH. Telemeterized in vivo hip joint force data: a report on two patients after total hip surgery. JOrthop Res. 1991;9:621–633. [DOI] [PubMed]
- 24.Langlais F, Lambotte JC, Thomazeau H. Long-term results of hemipelvis reconstruction with allografts. Clin Orthop Relat Res. 2001;388:178–186. [DOI] [PubMed]
- 25.Marco RA, Sheth DS, Boland PJ, Wunder JS, Siegel JA, Healey JH. Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease. J Bone Joint Surg Am. 2000;82:642–651. [DOI] [PubMed]
- 26.Nieder E, Elson RA, Engelbrecht E, Kasselt MR, Keller A, Steinbrink K. The saddle prosthesis for salvage of the destroyed acetabulum. J Bone Joint Surg Br. 1990;72:1014–1022. [DOI] [PubMed]
- 27.Ozaki T, Hoffmann C, Hillmann A, Gosheger G, Lindner N, Winkelmann W. Implantation of hemipelvic prosthesis after resection of sarcoma. Clin Orthop Relat Res. 2002;396:197–205. [DOI] [PubMed]
- 28.Renard AJ, Veth RP, Schreuder HW, Pruszczynski M, Keller A, van Hoesel Q, Bökkerink JP. The saddle prosthesis in pelvic primary and secondary musculoskeletal tumors: functional results at several postoperative intervals. Arch Orthop Trauma Surg. 2000;120:188–194. [DOI] [PubMed]
- 29.Satcher RL Jr, O’Donnell RJ, Johnston JO. Reconstruction of the pelvis after resection of tumors about the acetabulum. Clin Orthop Relat Res. 2003;409:209–217. [DOI] [PubMed]
- 30.Takami M, Ieguchi M, Takamatsu K, Kitano T, Aono M, Ishida T, Yamano Y. Functional evaluation of flail hip joint after periacetabular resection of the pelvis. Osaka City Med J. 1997;43:173–183. [PubMed]
- 31.Windhager R, Karner J, Kutschera HP, Polterauer P, Salzer-Kuntschik M, Kotz R. Limb salvage in periacetabular sarcomas: review of 21 consecutive cases. Clin Orthop Relat Res. 1996;331:265–276. [DOI] [PubMed]
- 32.Yoshida Y, Osaka S, Mankin HJ. Hemipelvic allograft reconstruction after periacetabular bone tumor resection. J Orthop Sci. 2000;5:198–204. [DOI] [PubMed]