Abstract
Extension contracture of the knee is a common complication of femoral lengthening. Knee flexion exercises to stretch the contracture with physical therapy can be effective but take a prolonged amount of time to work and place increased stress across the patellofemoral joint. We developed a minimal-incision limited quadricepsplasty surgical technique to treat knee extension contracture secondary to femoral lengthening and retrospectively reviewed 16 patients treated with this procedure. The mean age of the patients was 23 years. Range of motion of the knee and quadriceps strength were recorded preoperatively, after femur lengthening but before additional surgery, after quadricepsplasty, and at each followup. The mean femoral lengthening performed was 4.4 cm. We compared range of motion and time to regain knee flexion with those of historical controls. The minimum followup after quadricepsplasty was 6 months (mean, 38 months; range, 6–84 months). The mean range of motion was 129° preoperatively, 29° after the distraction phase of femoral lengthening, and 108° after limited quadricepsplasty, and at final followup, the mean knee flexion was 125°. There were no major complications. Limited quadricepsplasty improved knee flexion after a knee extension contracture developed secondary to femoral lengthening. In comparison to historical controls who did not have quadricepsplasty, the patients with limited quadricepsplasty had quicker return of knee flexion, although there was no difference in knee flexion achieved ultimately.
Level of Evidence: Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Quadricepsplasty is a well-known procedure to improve the range of motion (ROM) in patients with knee stiffness [1, 11, 12, 21]. Some causes for the stiffness include scarring after trauma or intraarticular knee surgery and quadriceps tightness after femoral lengthening. Femoral lengthening using distraction osteogenesis and the Ilizarov method is a recognized treatment modality for patients with lower extremity limb length discrepancy (LLD) [5, 19, 20]. However, femoral lengthening requires substantial muscle and tendon stretching, which often leads to knee stiffness and an extension contracture [7, 9, 17].
Numerous methods have been used to treat knee extension contractures associated with lengthening, including the Thompson quadricepsplasty [21], Judet quadricepsplasty [1, 11, 12], and their modifications [6]. These procedures are associated with risks of complications, such as severe extensor mechanism weakness and extensor lag [4, 15, 16] and infection associated with a large exposure [15, 16].
We describe our technique of a minimal-incision limited quadricepsplasty. We determined gains in ROM with this procedure, time to regain flexion, quadriceps strength, and complications. Finally, we compared the ROM of our patients with those from historical controls [7].
Material and Methods
We retrospectively reviewed the charts of 66 patients who underwent femur lengthening procedures from 2000 to 2006. Of these 66 patients, 16 (24%) had an extension contracture of the knee develop (Table 1). These patients were not able to bend their knee greater than 60° despite aggressive physical therapy. We considered these findings indications for a minimal-incision limited quadricepsplasty. There were 10 males and six females. Their mean age was 23 years (range, 4.5–54 years). These patients had various underlying diagnoses (Table 1). The femoral lengthening was performed using the EBI Multi-Axial Correction frame (Biomet/EBI, Parsippany, NJ) in five patients, the EBI rail frame (Biomet/EBI) in nine patients, and the Ilizarov/Taylor spatial frame (Smith and Nephew, Inc, Memphis, TN) in two patients. Fifteen patients (93%) had a distal femur osteotomy and one patient had a midshaft femur osteotomy. One patient (Patient 1) also had tibia lengthening after the femur lengthening. All 16 patients were evaluated during regular followups in the office. None of the 16 patients was to lost followup; none was seen specifically for this study. The minimum followup after quadricepsplasty was 6 months (mean, 38 months; range, 6–84 months). This study was approved by Institutional Review Board of the Hospital for Special Surgery.
Table 1.
Patient data
| Patient | Age (years) | Starting leg length discrepancy (cm) | Final leg length discrepancy (cm) | Femoral lengthening performed (cm) | Time wearing frame (Month) | Time from end of distraction to quadricepsplasty (days) | Complications | Treatment | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 12 | 4.5 | 0 | 2.5 | 4.77 | 16 | Congenital shortening of the lower extremity | ||
| 2 | 36 | 2.1 | 0 | 2.7 | 5.3 | 24 | Superficial pin tract infection, femoral nerve sensory symptoms | Oral antibiotics conservative treatment | Leg length discrepancy from radiation-induced growth arrest |
| 3 | 9 | 5.5 | 1.1 | 4.8 | 5.1 | −11 | Congenital short femur and tibia | ||
| 4 | 34 | 3.5 | 0.5 | 3 | 6.27 | 6 | Tarsal tunnel syndrome, flexion contractures of toes 2, 3, and 4. | Nerve release and flexor tenotomy | Congenital femoral valgus deformity with leg length discrepancy |
| 5 | 33 | 2 | 0.6 | 2 | 0.97 | 1 | Nonunion of the femur with femur shortening | ||
| 6 | 13 | 3 | 0 | 5.8 | 5.77 | 40 | Subtrochantic fracture of femur proximal to femoral pin | Ilizarov frame application (addition of Ilizarov ring proximally) | Distal femoral growth plate injury with femoral shortening |
| 7 | 54 | 5.2 | 2.7 | 3.5 | 7.77 | 7 | Superficial pin tract infection | Oral antibiotics | Posttraumatic distal femoral growth plate injury with femoral shortening |
| 8 | 25 | 4.3 | 1.5 | 4.5 | 7.07 | 43 | Iliotibial band tethering | Iliotibial band release | Postseptic hip with leg length discrepancy |
| 9 | 25 | 4 | 0.2 | 4.2 | 8.9 | 193 | Femoral valgus deformity with leg length discrepancy | ||
| 10 | 42 | 4 | 0 | 4.1 | 28.93 | 1 | Postsepsis hip with leg length discrepancy | ||
| 11 | 4.5 | 4.1 | 0 | 4 | 4.5 | 30 | Congenital short femur and tibia | ||
| 12 | 16 | 3.3 | −0.7 | 4 | 4 | 72 | Posttraumatic distal femoral growth plate injury | ||
| 13 | 18 | 12 | 1.6 | 12 | 5.6 | 6 | Subcutaneous abscess of the thigh | Incision and drainage, intravenous antibiotics | Segmental defect of the femur, after resection of low grade periosteal osteosarcoma of the femur. |
| 14 | 17 | 5.2 | 0 | 7.5 | 12 | −33 | Congenital dislocation of hip with necrosis and instability. Ilizarov hip reconstruction-proximal femur valgus osteotomy and distal femur osteoplasty for lengthening. | ||
| 15 | 12 | 3 | 0 | 3 | 4 | 37 | Posttraumatic distal femoral growth plate injury | ||
| 16 | 33 | 7 | 3 | 4 | 4.5 | 110 | Postpolio-side weakness with leg length discrepancy |
The mean preoperative LLD, including the femur and tibia, before lengthening was 4.5 cm (range, 2–12 cm). The mean femoral lengthening performed was 4.4 cm (range, 2–12 cm). The mean percentage femur lengthening performed was 11.6% (range, 5.3%–26.8%) of the entire bone length. The average final LLD was 0.6 cm (range, 0.7–3 cm). The mean difference between starting LLD and final LLD was 3.9 ± 2.0 cm (p < 0.001).
ROM of the knee was measured by the senior surgeon (SRR), using a goniometer, before femur lengthening, after femur lengthening, after quadricepsplasty, and at each followup. Watkins et al. [22] mentioned measuring ROM of the knee in the clinical setting is reasonably reliable.
All 66 patients who had femoral lengthening underwent physical therapy during active lengthening to maintain ROM. Therapy consisted of passive, active-assisted, and active ROM knee stretching exercises, bicycle, quadriceps electrical stimulation or ultrasound, patellar mobilization, and weightbearing as tolerated ambulation. Therapy began Postoperative Day 1 and continued for two to three times per week. For patients identified as having an early knee extension contracture, therapy was increased to three to five times per week with a therapist and a daily home program. They were allowed to ambulate with weightbearing as tolerated with an assistive device the next day.
Patients who had less than 60° flexion and showed no improvement despite aggressive therapy were considered for surgery. ROM results were categorized into functional groups according to Judet et al. [11] as knee flexion greater than 100°, flexion between 80° and 100°, and flexion less than 80°.
The mean knee flexion after lengthening and before limited quadricepsplasty was 29° (range, 10°–60°). The average time from the end of distraction for lengthening to limited quadricepsplasty was 35 days (range, −3–193 days). (A negative number indicates the quadricepsplasty was performed before the end of distraction.) The mean time wearing the frame was 7.2 months (range, 0.9–28 months). We compared our series with an historical control. Herzenberg et al. [7] reported results of knee ROM over time in a series of patients who underwent femoral lengthening. They did not use quadricepsplasty.
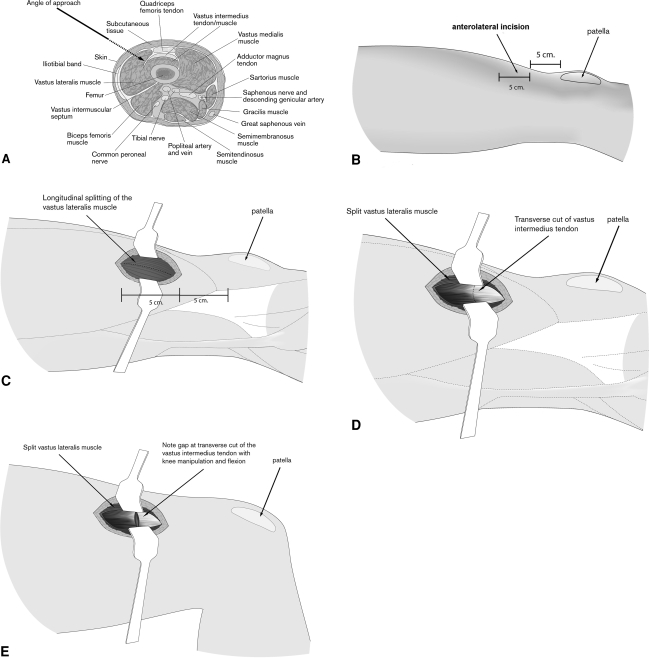
We used epidural anesthesia with intravenous sedation for all procedures. The external fixator was prepped in the field, and pin sites were wrapped with Betadine®-soaked (Purdue Frederick, Norwalk, CT) sponges. We did not use a tourniquet for any procedures. A 5-cm anterolateral skin incision was made beginning from the superolateral aspect of the patella and extended 5 cm proximally (Fig. 1). Dissection was carried down to the fascia. We incised the fascia in line with the fibers of the iliotibial band. A transverse fasciotomy was performed to release the iliotibial band and the anterior fascia of the thigh. The vastus lateralis then was exposed and split longitudinally. This exposed the vastus intermedius muscle and overlying fascia. The rectus femoris muscle and fascia were retracted anteriorly with a right-angled retractor and protected from the field. The vastus lateralis was retracted posteriorly. This exposed the entire vastus intermedius. The anterior fascia then was released with a transverse cut across its fibers. We took care not to incise any of the muscle tissue. The tight bands of the vastus intermedius were most apparent with the knee in maximum flexion. After releasing these fascial bands, we performed gentle manipulation to obtain maximum knee flexion. The hip was flexed during the manipulation to avoid excessive stretching of the femoral nerve. The wound was irrigated copiously and a drain was placed. The fascia was not repaired. We closed the skin in layers. We did not find the need to release the iliotibial band proximally around the distal femur pins.
Fig. 1A–E.
The schematic diagrams show the surgical steps for limited quadricepsplasty. The (A) anatomy of the distal thigh, (B) location of the incision, (C) splitting of the vastus lateralis muscle, (D) exposure and incision of the vastus intermedius tendon/fascia, and (E) the separated vastus intermedius tendon/fascia are shown.
Postoperative pain control typically was achieved with epidural patient-controlled analgesia. Patients were started on a continuous passive movement machine in the recovery room with ROM of 0° to 40° and were advanced as tolerated. The drain was removed the morning after surgery. Physical therapy was started on the first postoperative day with weightbearing as tolerated ambulation and knee ROM. Active-assisted knee flexion, passive flexion, active and passive extension, and isometric quadriceps exercises were encouraged immediately after the surgery. Physical therapy was supervised during the hospital stay and after discharge for 4 weeks by a physical therapist. After approximately 5 to 6 weeks of outpatient physical therapy, unsupervised therapy was recommended.
Differences (mean ± standard deviation [SD]) and comparisons were calculated between: ROM before quadricepsplasty and after quadricepsplasty; ROM before femoral lengthening and at final followup; ROM before quadricepsplasty and at final followup, intraoperative ROM, and ROM at last followup. All comparisons were performed using a paired t test. P values were Bonferroni corrected for the above four comparisons. The statistical program used was SYSTAT® Version 10 (Systat Software Inc, Richmond, CA).
Results
The mean maximum knee flexion before lengthening was 129° (range, 80°–140°) (Table 2). The mean knee flexion at the end of distraction was 29° (range, 10°–60°). The mean knee flexion obtained immediately after limited quadricepsplasty improved (p < 0.001) to 108° (range, 80°–120°). At final followup, the mean knee flexion further improved (p < 0.001) to 125° (range, 90°–140°) (Table 2). Fourteen of the 16 patients regained their preoperative ROM by the final followup. We observed no difference (9° ± 30°; p = 1.0) between mean preoperative flexion and final flexion (Table 3), suggesting patients tended to regain preoperative ROM after limited quadricepsplasty. Fourteen of the 16 patients had knee flexion greater than 100° and two of 16 had knee flexion between 80° and 100° according to the criteria of Judet et al. [11]. None of our patients had knee flexion less than 80° at final followup.
Table 2.
Knee ROM during course of treatment
| Patient | ROM (degrees) | |||
|---|---|---|---|---|
| Before treatment | Before quadricepsplasty | Achieved during quadricepsplasty | At last followup | |
| 1 | 130 | 30 | 110 | 130 |
| 2 | 140 | 60 | 110 | 130 |
| 3 | 135 | 25 | 120 | 130 |
| 4 | 130 | 40 | 120 | 130 |
| 5 | 135 | 30 | 120 | 130 |
| 6 | 130 | 40 | 120 | 140 |
| 7 | 130 | 20 | 120 | 130 |
| 8 | 135 | 35 | 80 | 120 |
| 9 | 140 | 15 | 110 | 130 |
| 10 | 130 | 25 | 110 | 130 |
| 11 | 130 | 15 | 115 | 130 |
| 12 | 130 | 30 | 115 | 135 |
| 13 | 130 | 10 | 115 | 90 |
| 14 | 80 | 30 | 90 | 130 |
| 15 | 130 | 40 | 100 | 130 |
| 16 | 130 | 20 | 90 | 90 |
| Mean | 129 (80–140) | 29 (10–60) | 108 (80–120) | 125 (90–140) |
ROM = range of motion.
Table 3.
Differences in knee ROM at different times during course of treatment
| Comparison times | Difference in ROM (degrees)* | p Value | |
|---|---|---|---|
| Before treatment | Before quadricepsplasty | 99 ± 19 | < 0.0001 |
| Before treatment | During quadricepsplasty | 20 ± 15 | < 0.0001 |
| Before quadricepsplasty | During quadricepsplasty | −79 + 20 | < 0.0001 |
| Before treatment | At last followup | 9 ± 30 | 1.0 |
| Before quadricepsplasty | At last followup | −90 + 26 | < 0.0001 |
| Intraoperative | At last followup | −11 + 29 | 0.1 |
* Values are expressed as mean ± standard deviation; ROM = range of motion.
Two patients (Patients 13 and 16) did not regain their preoperative ROM. Patient 13 had extension contracture develop during femoral bone transport after segmental resection of the femur for periosteal osteosarcoma. In this patient, lengthening was continued after quadricepsplasty, and ultimately, a 12-cm bone transport was accomplished. Other complications included nonunion of his femur docking site, which required exchange femoral nailing twice. Patient 16 had postpolio residual paralysis with quadriceps weakness. This patient underwent the quadricepsplasty during active femur lengthening. Based on these two patients, we do not think quadricepsplasty should be performed during active lengthening; it seems better to continue the lengthening or the bone transport and then perform the quadricepsplasty after the distraction phase.
Quadriceps muscle power was graded as 5/5 in all but one patient (Patient 14) who was graded 4/5. A 10° extensor lag was seen in one patient (Patient 16). This patient had postpolio residual paralysis with quadriceps weakness in which extensor lag was present even before the femoral lengthening.
During femoral lengthening, two patients (Patients 2 and 7) had superficial pin tract infections, which were treated successfully with local wound care and oral antibiotics (Table 1). Femoral nerve sensory symptoms were seen in one patient during lengthening (Patient 2), which resolved but slowed down the rate of distraction. A subcutaneous abscess of the thigh was seen in one patient (Patient 13), who was treated with incision and drainage under anesthesia and intravenous antibiotics. None had skin necrosis or wound dehiscence.
Discussion
Femoral lengthening can lead to knee stiffness and an extension contracture. The Thompson quadricepsplasty, the Judet quadricepsplasty, and their modifications are associated with increased risks of complications. We describe a minimal-incision limited quadricepsplasty for extension contracture of the knee. We analyzed the gain in ROM of the knee, time to regain flexion, quadriceps strength, and complications. We compared ROM of our patients and time to regain knee flexion with those from historical controls.
The major limitation in our study is the heterogeneity of case series. Patients were of different age groups, and femoral lengthening was done for leg length discrepancy attributable to multiple reasons, for example congenital, posttraumatic, postirradiation growth arrest or postseptic joint. Another limitation was the different method of fixation during femoral lengthening. These included application of a monolateral external fixator, a ring fixator, or lengthening over a nail. We think these limitations do not jeopardize our conclusions. Our patient group is different in that their contractures were acute and were related specifically to femur lengthening. These patients tend not to have arthrofibrosis, patellar tendon scarring, and patellar retinacular contraction often seen in posttraumatic or postsurgical generated knee extension contractures. We do not recommend limited quadricepsplasty for a chronic knee extension contracture from nonlengthening-related etiologies. Our technique is effective for extension contracture in the context of femoral lengthening and although we have no data, we believe it works best if performed soon after the distraction phase. We have not found the pins to mechanically block ROM of the knee. We also did not find the need to release the iliotibial band around the distal femur pins.
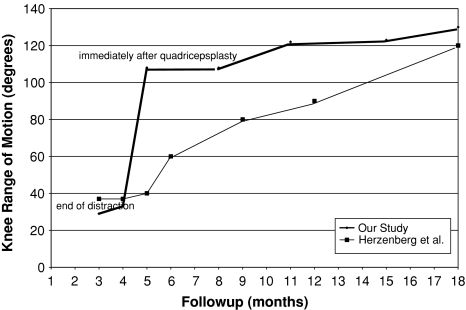
Herzenberg et al. [7] reported followup ROM of 25 patients with extension contractures after femoral lengthening treated nonoperatively. The mean age of their patients was 20.2 years. Fifteen patients underwent femoral lengthening for atraumatic (congenital or developmental) and 10 for posttraumatic shortening. The mean femoral lengthening was 6 cm (range, 3–15 cm). ROM decreased from 127° ± 16° to 37° ± 15° after femoral lengthening. All patients underwent daily aggressive physiotherapy. All but one patient achieved 90° knee flexion by 6 months after frame removal and full recovery was seen during the course of 1 year after frame removal. Patients required very aggressive physical therapy during the course of 1 year to recover ROM of the knee. At final followup, knee flexion was 122° ± 23°. A comparison of ROM of our patients with the historical series of Herzenberg et al. [7] is shown in Fig. 2. We did not have access to the raw data of Herzenberg et al. [7]. For this reason, we could not establish matching patient groups, and we also could not statistically compare ROMs of the two groups. Our patient group had greater than 90° of knee flexion immediately after quadricepsplasty which led to a much more rapid return of knee flexion compared with the patients of Herzenberg et al. [7]. Their patients were young with short-term followup; it is not known whether they are at increased risk for patellofemoral arthritis secondary to the increased joint surface contact pressures required to nonsurgically release these contracted tissues. Others have observed the flexing of knees with extension contractures treated with a combination of surgical releases and therapy has led to a substantial increase in patellofemoral arthritis [3, 14]. Intuitively, one could reason, without the surgical releases, the even tighter joint may suffer even greater compression with flexion, but to our knowledge, this has not been proven. A more rapid recovery of motion may be advantageous.
Fig. 2.
A comparison of ROM of our patients with ROM of the patients of Herzenberg et al. [7] is shown.
Merchan and Myong [13] reported results of 21 Judet quadricepsplasties for posttraumatic stiffness: 9.5% had knee flexion greater than 100°, 57.1% had knee flexion between 80° and 100°, and 33.3% had flexion between 50° and 80° according to the criteria of Judet et al. [11]. Nicoll [16] reported 33% of his patients had knee flexion greater than 80° after Judet quadricepsplasty. Ali et al. [1] reported the results of 10 patients treated with Judet quadricepsplasty for severe extension contracture of the knee after femoral fracture with an external fixator. Their results showed an improvement from 33° preoperatively to 88° at an average of 24 months’ final followup. Bellemans et al. [2] reported the results of 16 patients who had Judet quadricepsplasties with a mean followup of 22 months. The mean gain in knee flexion was 68°, with maximum movement as much as 90° [2]. Masse et al. [12] studied the clinical outcomes of 21 patients who had Judet quadricepsplasties after an average followup of 101 months. Knee flexion was greater than 100° in eight patients (38.10%), greater than 80° and less than 90° in nine (42.86%), and between 50° and 80° in four (19.05%), with no patients with knee flexion less than 50° [12]. Judet et al. [11] reported active flexion greater than 100° in most of their patients and extensor lag in 11% of patients. The complications associated with the Thompson procedure were severe quadriceps muscle weakness and extensor lag [1, 4, 7–10]. Moore et al. [15] and Pick [18] observed extensor lag after the Thompson quadricepsplasty of 33% and 66% respectively. Patient 14 had some relative weakness of the quadriceps compared with the opposite side at latest followup. Patient 16 showed no change from preoperative regarding quadriceps weakness.
The minimal incision limited quadricepsplasty was effective for treating knee extension contractures after femoral lengthening. In comparison to historical controls, it was easier and quicker for patients to achieve maximum knee flexion.
Acknowledgments
We thank Cynthia Bugwadia and Kira Segal for research assistance.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Ali AM, Villafuerte J, Hashmi M, Saleh M. Judet’s quadricepsplasty, surgical technique, and results in limb reconstruction. Clin Orthop Relat Res. 2003;415:214–220. [DOI] [PubMed]
- 2.Bellemans J, Steenwerckx A, Brabants K, Victor J, Lammens J, Fabry G. The Judet quadricepsplasty: a retrospective analysis of 16 cases. Acta Orthop Belg. 1996;62:79–82. [PubMed]
- 3.Cosgarea AJ, DeHaven KE, Lovelock JE. The surgical treatment of arthrofibrosis of the knee. Am J Sports Med. 1994;22:184–191. [DOI] [PubMed]
- 4.Ebraheim NA, DeTroye RJ, Saddemi SR. Results of Judet quadricepsplasty. J Orthop Trauma. 1993;7:327–330. [DOI] [PubMed]
- 5.Grill F, Dungl P. Lengthening for congenital short femur: results of different methods. J Bone Joint Surg Br. 1991;73:439–447. [DOI] [PubMed]
- 6.Hahn SB, Lee WS, Han DY. A modified Thompson quadricepsplasty for the stiff knee. J Bone Joint Surg Br. 2000;82:992–995. [DOI] [PubMed]
- 7.Herzenberg JE, Scheufele LL, Paley D, Bechtel R, Tepper S. Knee range of motion in isolated femoral lengthening. Clin Orthop Relat Res. 1994;301:49–54. [PubMed]
- 8.Hesketh KT. Experiences with the Thompson quadricepsplasty. J Bone Joint Surg Br. 1963;45:491–495. [PubMed]
- 9.Hosalkar HS, Jones S, Chowdhury M, Hartley J, Hill RA. Quadricepsplasty for knee stiffness after femoral lengthening in congenital short femur. J Bone Joint Surg Br. 2003;85:261–264. [DOI] [PubMed]
- 10.Ikpeme JO. Quadricepsplasty following femoral shaft fractures. Injury. 1993;24:104–108. [DOI] [PubMed]
- 11.Judet R, Judet J, LaGrange J. [Not available][in French]. Mem Acad Chir (Paris). 1956;82:402–405; discussion, 405–407. [PubMed]
- 12.Masse A, Biasibetti A, Demangos J, Dutto E, Pazzano S, Gallinaro P. The Judet quadricepsplasty: long-term outcome of 21 cases. J Trauma. 2006;61:358–362. [DOI] [PubMed]
- 13.Merchan EC, Myong C. Quadricepsplasty: the Judet technique and results of 21 posttraumatic cases. Orthopedics. 1992;15:1081–1085. [DOI] [PubMed]
- 14.Millett PJ, Williams RJ 3rd, Wickiewicz TL. Open debridement and soft tissue release as a salvage procedure for the severely arthrofibrotic knee. Am J Sports Med. 1999;27:552–561. [DOI] [PubMed]
- 15.Moore TJ, Harwin C, Green SA, Garland DE, Chandler RW. The results of quadricepsplasty on knee motion following femoral fractures. J Trauma. 1987;27:49–51. [DOI] [PubMed]
- 16.Nicoll EA. Quadricepsplasty. J Bone Joint Surg Br. 1963;45:483–490. [PubMed]
- 17.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed]
- 18.Pick RY. Quadricepsplasty: a review, case presentations, and discussion. Clin Orthop Relat Res. 1976;120:138–142. [PubMed]
- 19.Rose RE. Femoral lengthening using the Ilizarov technique. West Indian Med J. 2006;55:420–424. [DOI] [PubMed]
- 20.Sangkaew C. Distraction osteogenesis of the femur using conventional monolateral external fixator. Arch Orthop Trauma Surg. 2008;128:889–899. [DOI] [PubMed]
- 21.Thompson TC. Quadricepsplasty. Ann Surg. 1945;121:751–754. [DOI] [PMC free article] [PubMed]
- 22.Watkins MA, Riddle DL, Lamb RL, Personius WJ. Reliability of goniometric measurements and visual estimates of knee range of motion obtained in a clinical setting. Phys Ther. 1991;71:90–96; discussion 96–97. [DOI] [PubMed]