Abstract
OBJECTIVES
Studies suggest that breastfeeding is protective for later obesity; however, this association has not held among all racial and socioeconomic status groups. Racial and socioeconomic status differences in breastfeeding behavior have also been noted. In this study, we formally test whether breastfeeding mediates the relationship between race and socioeconomic status with adolescent adiposity.
METHODS
Data were analyzed from 739 black and white 10- to 19-year-old adolescents who participated in a large, school-based study. Parents provided information on parental education, used to measure socioeconomic status, and whether the child was breastfed as an infant. BMI was used to measure adolescent adiposity and was analyzed as a continuous measure (BMI z score) using linear regression and categorically (BMI ≥85th and ≥95th percentile) using logistic regression.
RESULTS
Black adolescents and those without a college-educated parent were less likely to have been breastfed for >4 months. Race and parental education were each independent predictors of BMI z score and of having BMI ≥85th percentile or BMI ≥95th percentile. When added to the model, being breastfed for >4 months was also independently associated with lower BMI z score and lower odds of having BMI ≥85th percentile or BMI ≥95th percentile. Inclusion of being breastfed for >4 months resulted in a 25% decrease in racial and parental education differences in adolescent BMI z score, supporting partial mediation.
CONCLUSIONS
Having been breastfed for >4 months was associated with lower adolescent BMI z score and lower odds of having a BMI ≥85th percentile or BMI ≥95th percentile, independent of race or parental education. Furthermore, these analyses suggest that being breastfed for >4 months partially explains the relationship between social disadvantage and increased adiposity. Increasing breastfeeding duration could result in lower adolescent adiposity for all racial and socioeconomic status groups and potentially minimize socioeconomic disparities in adiposity.
Keywords: adolescent obesity, breastfeeding, epidemiology, racial differences, socioeconomic status
Adolescent obesity is a major public health issue that has been increasing in the past 2 decades. This problem disproportionately affects socially disadvantaged groups. Recent national studies have found that >40% of black adolescents aged 12 to 19 are at risk for overweight (eg, BMI ≥85th percentile for age and gender) or are overweight (BMI ≥95th percentile) compared with 26.5% of white teens and that this proportion has been increasing.1,2 In addition, low socioeconomic status (SES) is frequently associated with higher rates of overweight.3–6 Thus, the search for causes and potential interventions to decrease these disparities and reduce the prevalence of overweight is crucial.
Breastfeeding has been reported as being protective against obesity, but this association is somewhat controversial. Whereas several studies found significantly lower obesity rates among those who were breastfed as infants7–11 and a dosage-related effect of breastfeeding,12–17 not all studies supported these findings.18–21 Two large studies suggested that the protective association of breastfeeding may be limited to non-Hispanic white individuals. Others indicated that the protective effect may be confounded by SES.17,22–25 These inconsistencies may reflect the correlation of racial/ethnic minority status with low SES, as well as racial and SES differences in breastfeeding behavior.26–28
Despite these controversies, to date, the literature suggests that breastfeeding has a small but consistent independent protective effect on adiposity, adjusting for underlying racial or SES differences in adiposity.29 However, to our knowledge, no studies have explored the role that breastfeeding may play in the development of racial/ethnic and SES disparities in overweight, including the possibility that breastfeeding may lie in the pathway between social disadvantage and increased adiposity. If this is true, then changing breastfeeding behavior may reduce these underlying adiposity differences by race or SES, providing a useful tool for reducing disparities and decreasing overweight. In this study, we formally test whether breastfeeding mediates the relationship between race and/or SES and adolescent adiposity in a large, economically diverse cohort of black and white adolescents.
METHODS
Study Sample
This study used baseline data from a large, recent, longitudinal, school-based study of youth from the Greater Cincinnati area: the Princeton City School District (PSD) Study.30 Students were recruited from the single public high school (grades 9–12) and junior high school (grades 7–8) in the district. The participants in the PSD Study represent a wide range of household income and parental education.31 Regional breastfeeding rates at the time of the cohort’s birth were 59% for white individuals and 33% for black individuals.32 The study design and recruitment process has been described in detail elsewhere30 but, briefly, included physical measurements and administration of questionnaires to students by trained study personnel in school facilities, as well as mailed questionnaires to parents. All study participants who were older than 18 years and parents provided written informed consent, and participants who were younger than 18 years provided written assent.31,33 The study protocol was approved by the institutional review board of the local children’s hospital and participating university.
Analysis Cohort
All children who were enrolled in the 2001–2002 school year were eligible for inclusion in the PSD Study, but because the district is 95% non-Hispanic black and white, only non-Hispanic black and white youth were included in these analyses. Of the 2161 non-Hispanic black and white PSD Study participants, 1719 (79.4%) had a parent provide information on parental education on a baseline questionnaire. A second parental questionnaire that sought information on breastfeeding, birth weight, and prematurity was mailed during the 2004–2005 school year to families who participated in the study that year (n = 1545; 71.5% of baseline cohort); response rate for this survey was 57.9%. Of those who had a parent return the second survey, 739 (82.7%) had baseline information about parent education. These 739 youth make up the analysis cohort. Those included in the analysis cohort were more likely to be white (70% vs 40%), were younger (mean ± SD: 14.1 ± 2.1 vs 14.7 ± 2.1), and had lower BMI z scores (mean ± SD: 0.64 ± 1.0 vs 0.78 ± 1.0) than those who were excluded because of missing data (all P < .01).
Variables of Interest
Independent Variables
Race/ethnicity was determined from school records. Although the baseline parental SES survey included information on both parent education and household income, parent education was chosen as a measure of SES because it was likely a better proxy for the adolescent’s SES at birth than current family income and was unlikely to change during a teen’s life. Highest level of parental (either maternal or paternal) education was originally analyzed in 4 groups—high school diploma or less, some college, college degree, and more than a college degree—however, analyses suggested the greatest adiposity difference between adolescents whose parents had a college degree compared with those whose parents did not have a college degree, so for simplicity and sample size considerations, parental education was dichotomized (less than college versus college or more). The latter was used as the reference group in analyses. Results of analyses with the 4-level parent education variable were essentially identical to those reported here with the 2-level variable (data available on request).
Mediator
Breastfeeding was ascertained using 2 questions: (1) “Was your child breastfed (nursed) as a baby?” (2) “If yes, how long was your child breastfed?” For this analysis, breastfeeding was classified as “ever breastfed” when the parent indicated any attempt at breastfeeding (“yes” to question 1), even when the specific duration was not reported in question 2. For those who responded “yes” to question 1, breastfeeding duration (question 2) of “less than 1 month” or “don’t know” was classified as 0.5 months (2 weeks). Breastfeeding duration was initially analyzed as an ordinal variable (never breastfed [reference category], breastfed 0.5–4 months, or breastfed >4 months); however, adiposity for adolescents who were breastfed 0.5 to 4 months was not significantly different from those who were never breastfed in any analysis (data not shown). Therefore, breastfeeding was dichotomized, with all presented analyses comparing those who were breastfed >4 months with all others (eg, combining never breastfed and breastfed 0.5–4 months to create a single category of breastfed 0–4 months).
Dependent Variables
Adiposity was assessed by BMI (kg/m2), calculated using measured height and weight. The Centers for Disease Control and Prevention 2000 growth charts were used to determine gender- and age-specific BMI z scores and percentiles.34,35 Two categories of BMI (BMI ≥85th percentile and BMI ≥95th percentile) were also analyzed.
Covariates
School records provided participants’ date of birth (used to calculate age) and gender. Pubertal stage was determined as described previously30 but, briefly, using a validated algorithm including sex hormone levels and attainment of objective developmental milestones. The second parental questionnaire was used to assess birth weight and prematurity. The question, “What was your child’s birth weight?” was used to assess birth weight. The question, “Was your child’s birth premature (<36 weeks of pregnancy)?” was used to assess prematurity. Previous research has established high maternal recall of prematurity/gestational age (r = 0.82–0.86) and birth weight (r = 0.94–0.99), even several years later.36–38
Statistical Analysis
Analyses were conducted using SAS 9.1 (SAS Institute, Cary, NC). Univariate differences in variables by group were tested using t tests for continuous variables and χ2 tests for categorical variables. Linear regression models were developed with BMI z score as the dependent variable, with β± SE reported. Logistic regression was used to model the risk for BMI ≥85th percentile or BMI ≥95th percentile compared with BMI <85th percentile, with adjusted odds ratios (aORs) and 95% confidence intervals (95% CIs) reported. All relationships were modeled both unadjusted and adjusted for gender, age, pubertal stage, birth weight, and prematurity. Because unadjusted and adjusted results were similar (data not shown), only adjusted relationships are reported.
Stratified models by race and parental education were considered to determine whether effects of breastfeeding were similar by stratum, and interactions between race or parental education and breastfeeding were tested in the full cohort. Adjusted differences between racial and socioeconomic subgroups were assessed using adjusted least square means from general linear modeling, and least square means ± SE are presented. P ≤ .05 was considered significant for all analyses.
Mediation Analysis
Mediation refers to a situation in which a mediator variable lies within a pathway between and fully or partially accounts for the relationship between a predictor and the outcome. Multivariable statistical modeling is used to determine whether mediation exists. The same modeling is used to determine confounding. The difference between a confounding explanation and a mediational one lies in the hypothesized relationships between the independent variable (race/SES in this case) and the mediator (breastfeeding). In confounding, there is an association between the independent variable and the mediator, but this relationship is considered incidental and often a nuisance. By contrast, in mediation, the independent variable is hypothesized to have a causal relationship with the mediator.
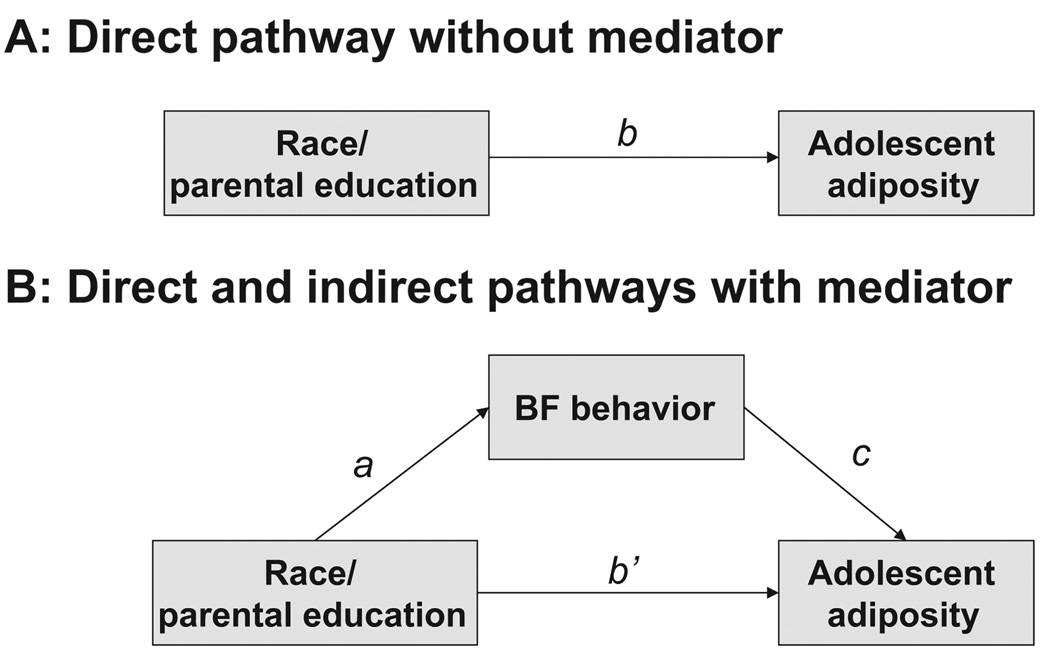
Baron and Kenny’s criteria39 were used to assess whether breastfeeding behaviors partially mediated the relationship between race or parental education and adolescent BMI. By these criteria, breastfeeding behavior can be considered a mediator when all of the following relationships are significant (presented in Fig 2): (1) race and/or parental education predicts breastfeeding behavior (pathway a in Fig 2B); (2) race and/or parental education predicts adolescent BMI (pathway b in Fig 2A and pathway b′ in Fig 2B); and (3) breastfeeding behavior significantly predicts adolescent BMI, adjusting for race and/or parental education (pathway c in Fig 2B). For each of the 3 measures of BMI, an identical modeling strategy was developed. Model 1 assessed the association of black race adjusting for the covariates gender, age, puberty stage, prematurity, and birth weight. Model 2 assessed the relationship between lower parental education and BMI adjusting for covariates. Model 3 assessed the independent relationships between black race and lower parent education variables when adjusted for each other and covariates. Thus, Model 3 tests pathway b in Fig 2A. Model 4 adds the variable breastfeeding for >4 months, the proposed mediator, to model 3 to test pathways b′ and c in Fig 2B. The Sobel test for mediation was conducted for BMI z score. The Sobel test is the gold standard for formally testing the significance of a proposed mediation pathway, in this case between race/parental education and adolescent BMI z score via breastfeeding behavior.39,40 We performed the Sobel test using 1000 bootstrap resamples in SAS41 to determine whether the indirect pathway via breastfeeding behavior was significantly different from 0 (Ho: a*c = 0). Bootstrap resampling was used to obtain a more accurate estimate of the indirect effect and its SE because a normal distribution of the statistic could not be assumed.
FIGURE 2.
Proposed mediation pathways to be tested. A, Adjusted direct effect (pathway b), not including mediator. B, Adjusted direct (pathway b′) and indirect effects (pathways a and c), including potential mediation by breastfeeding.
RESULTS
Table 1 presents descriptive data on the cohort and subsets defined by race and parental education. Black individuals were more likely to have been premature and to have lower birth weight and parental education than white individuals. Adolescents with lower educated parents were more likely to be black and were younger than those with parents with at least a college degree. Fifty-six percent of the adolescent cohort was ever breastfed, and more than one third (36%) had a BMI ≥85th percentile.
TABLE 1.
Cohort Description by Race and Parental Education
| Parameter | All | Black | White | Less Than College |
College or More |
|---|---|---|---|---|---|
| n | 739 | 225 | 514 | 299 | 440 |
| Male, n (%) | 345 (47) | 104 (46) | 241 (47) | 139 (46) | 206 (47) |
| Age, mean ± SD, y | 14.1 ± 2.1 | 13.9 ± 2.1 | 14.2 ± 2.1 | 13.9 ± 2.1 | 14.3 ± 2.1a |
| Puberty, n (%) | |||||
| Prepubertal | 95 (13) | 25 (11) | 70 (14) | 48 (16) | 47 (11) |
| Pubertal | 304 (41) | 90 (40) | 214 (42) | 124 (42) | 180 (41) |
| Postpubertal | 338 (46) | 109 (49) | 229 (45) | 126 (42) | 212 (48) |
| Premature, n (%) | 59 (8) | 30 (13) | 29 (6)b | 25 (8) | 34 (8) |
| Birth weight, mean ± SD, kg | 3.4 ± 0.6 | 3.2 ± 0.6 | 3.5 ± 0.5b | 3.4 ± 0.6 | 3.4 ± 0.5 |
| Black, n (%) | 225 (30) | — | — | 132 (44) | 93 (21)b |
| Parental Education, n (%) | |||||
| Less than college degree | 299 (40) | 142 (59) | 167 (32)b | — | — |
| College degree or more | 440 (60) | 93 (41) | 347 (68) | — | — |
| Breastfeeding behavior, n (%) | |||||
| Never or≤4 mo | 508 (69) | 201 (89) | 307 (60)b | 245 (82) | 263 (60)b |
| >4 mo | 231 (31) | 24 (11) | 207 (40) | 54 (18) | 177 (40) |
| Adolescent adiposity | |||||
| BMI≥85th percentile, n (%) | 269 (36) | 109 (48) | 160 (31)b | 141 (47) | 128 (29)b |
| BMI≥95th percentile, n (%) | 123 (17) | 58 (26) | 65 (13)b | 75 (25) | 48 (11)b |
| BMI z score (mean ± SD) | 0.64 ± 1.00 | 0.95 ± 1.00 | 0.51 ± 1.00b | 0.85 ± 1.10 | 0.51 ± 0.90b |
P<.05 by t test.
P<.001 by χ2 test.
Associations of Race and Parental Education With Breastfeeding
Both black race (aOR: 0.29; 95% CI: 0.14–0.37) and lower parent education (aOR: 0.42; 95% CI: 0.29–0.60) were associated with decreased likelihood of being breastfed for >4 months, adjusting for covariates (pathway a in Fig 2B). Importantly, prematurity and birth weight were not significant predictors of being breastfed for >4 months in these multivariable models, and there was no interaction between race and parental education.
Direct and Indirect Pathways Between Race or Parental Education and Adolescent BMI
Table 2 presents results from multivariable regression analyses that tested the pathways presented in Fig 2 for all 3 measures of BMI. When BMI was modeled as a continuous measure, black adolescents (model 1) and adolescents with less educated parents (model 2) had higher mean BMI z scores than white individuals or adolescents with at least 1 college-educated parent, and both variables remained highly significant when included in the same model (model 3). When being breastfed for >4 months was added to the model (model 4), it was significantly associated with lower adolescent BMI z score, whereas both race and parental education differences in BMI z score were significantly attenuated (~25% attenuation of β estimate). The Sobel test for mediation was highly significant (P < .0001), supporting a role for breastfeeding behavior’s partially accounting for race and parental education differences in adolescent BMI z score.
TABLE 2.
Adjusted Linear and Logistic Regression Estimates to Test Mediation Pathways
| Dependent Variables | Independent Variablesa | Mediator | |
|---|---|---|---|
| Black | Less Than College |
Breastfeeding for >4mob |
|
| BMI z score | β ± SE | β ± SE | β ± SE |
| Model 1 | 0.47 ± 0.08d | ||
| Model 2 | 0.37 ± 0.07d | ||
| Model 3 | 0.40 ± 0.08d | 0.28 ± 0.07d | |
| Model 4 | 0.32 ± 0.08d | 0.23 ± 0.08e | −0.33 ± 0.08d |
| BMI≥85th percentilec | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) |
| Model 1 | 2.28 (1.62–3.22)d | ||
| Model 2 | 2.25 (1.65–3.08)d | ||
| Model 3 | 1.94 (1.36–2.77)d | 1.98 (1.44–2.73)d | |
| Model 4 | 1.67 (1.16–2.41)e | 1.80 (1.30–2.49)d | 0.49 (0.33–0.72)d |
| BMI≥95th percentilec | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) |
| Model 1 | 3.06 (1.96–4.78)d | ||
| Model 2 | 3.32 (2.18–5.05)d | ||
| Model 3 | 2.43 (1.53–3.86)d | 2.80 (1.81–4.31)d | |
| Model 4 | 2.14 (1.33–3.44)e | 2.61 (1.68–4.04)d | 0.58 (0.34–0.99)f |
Model 1 includes race + covariates (gender, age, puberty stage, prematurity, and birth weight). Model 2 includes parent education + covariates. Model 3 includes both race and parent education + covariates. Model 4 adds breastfeeding for >4 months, the proposed mediator, to model 3.
Referent categories are white and college degree or more.
Referent category is breastfeeding for 0 to 4 months.
Compared with BMI<85th percentile.
P≤.001.
P≤.01.
P≤.05.
Findings were similar when BMI was modeled categorically. Black adolescents or adolescents with less educated parents were twice as likely to have a BMI ≥85th percentile and were nearly 3 times as likely to have a BMI ≥95th percentile as white individuals or those with higher educated parents, even when included in the same model (model 3). When breastfeeding for >4 months was added to the model (model 4), it was independently associated with ~50% lower odds having a BMI ≥85th percentile and a 42% lower odds of having BMI ≥95th percentile. For both categorical outcomes, the effects of race and parental education were attenuated in model 4, although formal testing for mediation could not be conducted with categorical outcomes.
Consistency of Breastfeeding Effects by Race and Parental Education
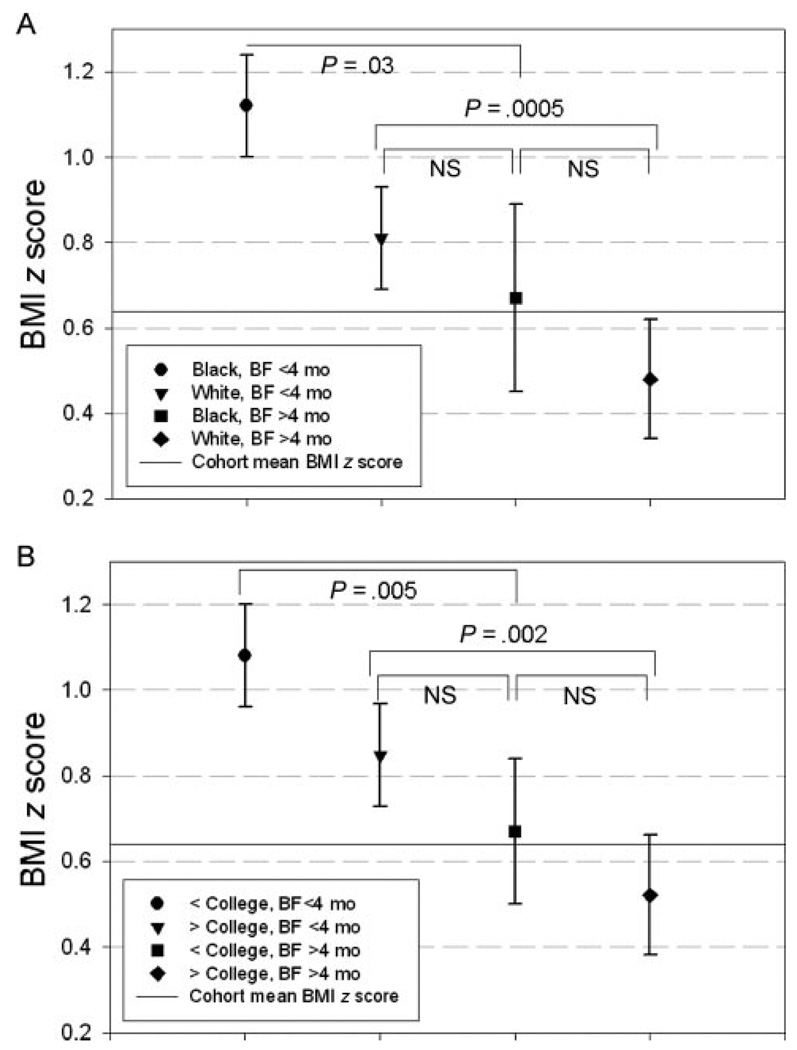
In stratified analyses, the associations of breastfeeding for >4 months with adolescent BMI z score were consistent in black individuals (β± SE: −0.38 ± 0.21; P = .07) and white individuals (−0.31 ± 0.09; P = .0005) and in lower (−0.39 ± 0.16; P = .01) and higher educated families (−0.30 ± 0.09; P = .001). The same was true when BMI was modeled as a categorical variable. The odds of adolescents’ having a BMI ≥85th percentile when breastfed >4 months were similar in black individuals (aOR: 0.50; 95% CI: 0.20–1.27) and white individuals (aOR: 0.48; 95% CI: 0.32–0.74) and in lower (aOR: 0.57; 95% CI: 0.30–1.08) and higher educated families (aOR: 0.45; 95% CI: 0.28–0.72). For BMI ≥95th percentile, breastfeeding for >4 months seemed to have a stronger protective effect among black individuals (black: aOR: 0.35 [95% CI: 0.09–1.32]; white: aOR: 0.67 [95% CI: 0.37–1.23]) and those who had a college-educated parent (less than college: aOR: 0.80 [95% CI: 0.37–1.73]; college or more: aOR: 0.45 [95% CI: 0.21–0.95]). However, the CIs were highly overlapping, suggesting that the effect of breastfeeding was similar across these racial and socioeconomic groups, and interactions in the full model were not significant. In addition, the CIs included 1.0 for all subgroups but those who had a college-educated parent, suggesting insufficient power to detect significance in all groups.
Figure 1 shows the estimated mean BMI z score in subgroups stratified by breastfeeding for >4 months and race (Fig 1A) and stratified by breastfeeding for >4 months and parent education (Fig 1B). Looking across these 2 panels, the protective effect of breastfeeding for >4 months is clear. Also of note is the similarity in the effects of race and parent education.
FIGURE 1.
Adjusted least square mean BMI z score ± SE by breastfeeding (BF;>4 months versus all others) and race (A) or parental education (B), from general linear modeling. Both models included race, parental education, breastfeeding for >4 months, gender, age, puberty stage, prematurity, and birth weight. Nonsignificant interactions of race by breastfeeding for >4 months (A) or parent education by breastfeeding for >4 months (B) were included in the model to estimate group-specific least square means.
DISCUSSION
This study examined in detail the interrelationships among race, parental education, and breastfeeding with adolescent adiposity, measured as BMI. We report that race, parental education, and breastfeeding are independently associated with adolescent BMI z scores. Mediation testing identified that ~25% of the race or parental education differences seen in adolescent BMI z scores are attributable to lower prevalence of breastfeeding for >4 months in disadvantaged groups. Furthermore, our data demonstrate that the magnitude of the relationship between breastfeeding for >4 months and lower BMI z score or risk for BMI ≥85th percentile or BMI ≥95th percentile is similar for groups defined by either race or parental education, suggesting that breastfeeding for >4 months may be similarly advantageous across race and SES groups.
The diversity of this cohort allowed us to distinguish effects of race, parent education, and breastfeeding and estimate a mediation effect. It is possible that previous studies with greater homogeneity among these factors might not have had the power to determine separate breastfeeding, race, and SES effects,12,42 resulting in the interpretation that breastfeeding does not have an independent relationship with adiposity.
Through formal mediational testing, we demonstrated that breastfeeding behaviors accounted for ~25% of the racial or SES disparities in adolescent BMI z score. This interpretation of the regression analyses contrasts with previous reports that treated the relationship of breastfeeding to adolescent BMI as confounded by race or SES, rather than viewing breastfeeding as a mediator between race or SES and adiposity.12,17,24,25,42 We consider the argument for a mediational model to be the more compelling, given that race and parental education are powerful social factors that exist before childbirth and are known to have an impact on the decision to breastfeed. Indeed, other studies that showed attenuation of the breastfeeding effect with the inclusion of race or SES may be interpreted to support the concept of partial mediation without having directly tested it.7,9,13,16,24
This study also explored how different definitions of adolescent adiposity may affect a study’s conclusions. Adolescent BMI can be operationalized as either a continuous variable (BMI z score) or a categorical variable that either models the extreme upper end of the BMI distribution (BMI ≥95th percentile) or includes a relatively large proportion of the population (BMI ≥85th percentile). In this study, we explored whether the effect of breastfeeding changed depending on the definition of BMI. For all 3 of the definitions used, we found that breastfeeding for >4 months was significantly associated with lower adolescent BMI; we noted that the effect of breastfeeding for >4 months had a similar reduction in odds for BMI ≥85th percentile and BMI ≥95th percentile. From this information, it seems that breastfeeding for >4 months may influence adolescent BMI z scores across the physiologic range, not only at the extremes of the BMI distribution.
There are some limitations that should be noted. The analysis cohort included a lower proportion of black adolescents than the baseline cohort, as a result of lower response rates in this group for the second parental questionnaire used to assess breastfeeding. Thus, there may be selection bias; however, >30% of our cohort was black, which exceeds the proportion in many other large studies7,19 and is similar to data from low-income populations.12 In addition, the breastfeeding rates in our analysis cohort are nearly identical to regional breastfeeding rates at the time of the cohort’s birth, suggesting that the effect of selection may be limited.
Our breastfeeding data also relied on parental recall and did not capture information about breastfeeding exclusivity. Although this may introduce some misclassification, previous studies demonstrated that maternal recall of pregnancy-related events including breastfeeding is valid over long durations36,43–45 and does not differ by race46 or education.44 Furthermore, our methods did not differ substantially from other large-scale epidemiologic studies, including the Centers for Disease Control and Prevention’s National Immunization Survey, which is used to estimate national breastfeeding prevalence.7,47
In addition, our proxy for SES was the higher of either maternal or paternal education, rather than maternal education only. Studies have shown that maternal education is an important factor in the decision to breastfeed,27,28,32,48 although highest household and paternal education are often independent predictors as well.26,49–51 Because previous research demonstrated that our primary outcome, BMI, is associated with parental education regardless of the parent considered,52 we used highest parental education in this study. A reanalysis of this study cohort using only maternal education revealed strong correlations (r = 0.75) between maternal and highest parental education and very similar results (data not shown).
We also noted that the decision to explore 4-month duration of breastfeeding was based on several factors, including previous studies that examined this duration, 9,12,13,15,22,53 the past and current American Academy of Pediatrics breastfeeding recommendations, which discourage introduction of solid foods before 4 months,54 and the desire to have sufficient sample size in all subgroups. We found significant effects for all measures of adolescent BMI among adolescents who had been breastfed for >4 months; however, this does not rule out increased protection with longer durations of breastfeeding, as has been reported elsewhere.13,16
CONCLUSIONS
In this study of black and white adolescents from a mixed-SES school district, breastfeeding for >4 months was associated with lower adolescent BMI z score and lower odds for having a BMI ≥85th percentile or BMI ≥95th percentile, independent of race or parental education level. In addition, analyses showed that breastfeeding was a partial mediator of the racial and educational disparities in adolescent BMI, lending support to the idea that these factors are markers of social disadvantage and are powerful in shaping behaviors and biology. These results suggest that efforts to increase the duration of breastfeeding could result in lower adolescent adiposity for all racial and SES groups. Interventions targeted toward socially disadvantaged groups may also decrease social inequalities in overweight and future cardiovascular disease.
ACKNOWLEDGMENTS
This study was supported by National Institutes of Health grants R01-DK59183 (Dr Dolan), R01-HD41527 (Dr Goodman), R21-HD054029 (Dr Woo), and P01-HD13021 (Dr Morrow) and the American Diabetes Association (7-03-CD-06; Dr Woo).
We gratefully acknowledge the participants, families, and schools involved in the PSD Study, as well as the PSD Study team: Tara Schafer-Kalkhoff, Tara Foltz, RN, Amy Cline, RN, Sang Sam, Michelle Hull, and Julie Schwarber.
Abbreviations
- SES
socioeconomic status
- PSD
Princeton School District
- aOR
adjusted odds ratio
- CI
confidence interval
Footnotes
The authors have indicated they have no financial relationships relevant to this article to disclose.
Reprints Information about ordering reprints can be found online: http://www.pediatrics.org/misc/reprints.shtml
REFERENCES
- 1.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity (Silver Spring) 2006;14(2):301–308. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288(14):1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 3.Kinra S, Nelder RP, Lewendon GJ. Deprivation and childhood obesity: a cross sectional study of 20,973 children in Plymouth, United Kingdom. J Epidemiol Community Health. 2000;54(6):456–460. doi: 10.1136/jech.54.6.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinra S, Baumer JH, Davey Smith G. Early growth and childhood obesity: a historical cohort study. Arch Dis Child. 2005;90(11):1122–1127. doi: 10.1136/adc.2004.066712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wardle J, Brodersen NH, Cole TJ, Jarvis MJ, Boniface DR. Development of adiposity in adolescence: five year longitudinal study of an ethnically and socioeconomically diverse sample of young people in Britain. BMJ. 2006;332(7550):1130–1135. doi: 10.1136/bmj.38807.594792.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moore DB, Howell PB, Treiber FA. Changes in overweight in youth over a period of 7 years: impact of ethnicity, gender and socioeconomic status. Ethn Dis. 2002;12(1):S1–83–S1–86. [PubMed] [Google Scholar]
- 7.Gillman MW, Rifas-Shiman SL, Camargo CA, Jr, et al. Risk of overweight among adolescents who were breastfed as infants. JAMA. 2001;285(19):2461–2467. doi: 10.1001/jama.285.19.2461. [DOI] [PubMed] [Google Scholar]
- 8.Arenz S, Ruckerl R, Koletzko B, von Kries R. Breast-feeding and childhood obesity: a systematic review. Int J Obes Relat Metab Disord. 2004;28(10):1247–1256. doi: 10.1038/sj.ijo.0802758. [DOI] [PubMed] [Google Scholar]
- 9.Li C, Kaur H, Choi WS, Huang TT, Lee RE, Ahluwalia JS. Additive interactions of maternal prepregnancy BMI and breast-feeding on childhood overweight. Obes Res. 2005;13(2):362–371. doi: 10.1038/oby.2005.48. [DOI] [PubMed] [Google Scholar]
- 10.Toschke AM, Vignerova J, Lhotska L, Osancova K, Koletzko B, Von Kries R. Overweight and obesity in 6- to 14-year-old Czech children in 1991: protective effect of breast-feeding. J Pediatr. 2002;141(6):764–769. doi: 10.1067/mpd.2002.128890. [DOI] [PubMed] [Google Scholar]
- 11.Dewey KG. Is breastfeeding protective against child obesity? J Hum Lact. 2003;19(1):9–18. doi: 10.1177/0890334402239730. [DOI] [PubMed] [Google Scholar]
- 12.Grummer-Strawn LM, Mei Z. Does breastfeeding protect against pediatric overweight? Analysis of longitudinal data from the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System. Pediatrics. 2004;113(2) doi: 10.1542/peds.113.2.e81. Available at www.pediatrics.org/cgi/content/full/113/2/e81. [DOI] [PubMed] [Google Scholar]
- 13.von Kries R, Koletzko B, Sauerwald T, et al. Breast feeding and obesity: cross sectional study. BMJ. 1999;319(7203):147–150. doi: 10.1136/bmj.319.7203.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.von Kries R, Koletzko B, Sauerwald T, von Mutius E. Does breast-feeding protect against childhood obesity? Adv Exp Med Biol. 2000;478:29–39. doi: 10.1007/0-306-46830-1_3. [DOI] [PubMed] [Google Scholar]
- 15.Shields L, O’Callaghan M, Williams GM, Najman JM, Bor W. Breastfeeding and obesity at 14 years: a cohort study. J Paediatr Child Health. 2006;42(5):289–296. doi: 10.1111/j.1440-1754.2006.00864.x. [DOI] [PubMed] [Google Scholar]
- 16.Liese AD, Hirsch T, von Mutius E, Keil U, Leupold W, Weiland SK. Inverse association of overweight and breast feeding in 9 to 10-y-old children in Germany. Int J Obes Relat Metab Disord. 2001;25(11):1644–1650. doi: 10.1038/sj.ijo.0801800. [DOI] [PubMed] [Google Scholar]
- 17.Nelson MC, Gordon-Larsen P, Adair LS. Are adolescents who were breast-fed less likely to be overweight? Analyses of sibling pairs to reduce confounding. Epidemiology. 2005;16(2):247–253. doi: 10.1097/01.ede.0000152900.81355.00. [DOI] [PubMed] [Google Scholar]
- 18.Hediger ML, Overpeck MD, Ruan WJ, Troendle JF. Early infant feeding and growth status of US-born infants and children aged 4–71 mo: analyses from the third National Health and Nutrition Examination Survey, 1988–1994. Am J Clin Nutr. 2000;72(1):159–167. doi: 10.1093/ajcn/72.1.159. [DOI] [PubMed] [Google Scholar]
- 19.Michels KB, Willett WC, Graubard BI, et al. A longitudinal study of infant feeding and obesity throughout life course. Int J Obes (Lond) 2007;31(7):1078–1085. doi: 10.1038/sj.ijo.0803622. [DOI] [PubMed] [Google Scholar]
- 20.Burdette HL, Whitaker RC, Hall WC, Daniels SR. Breastfeeding, introduction of complementary foods, and adiposity at 5 y of age. Am J Clin Nutr. 2006;83(3):550–558. doi: 10.1093/ajcn.83.3.550. [DOI] [PubMed] [Google Scholar]
- 21.Victora CG, Barros F, Lima RC, Horta BL, Wells J. Anthropometry and body composition of 18 year old men according to duration of breast feeding: birth cohort study from Brazil. BMJ. 2003;327(7420):901. doi: 10.1136/bmj.327.7420.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li C, Goran MI, Kaur H, Nollen N, Ahluwalia JS. Developmental trajectories of overweight during childhood: role of early life factors. Obesity (Silver Spring) 2007;15(3):760–771. doi: 10.1038/oby.2007.585. [DOI] [PubMed] [Google Scholar]
- 23.Parsons TJ, Power C, Manor O. Infant feeding and obesity through the lifecourse. Arch Dis Child. 2003;88(9):793–794. doi: 10.1136/adc.88.9.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics. 2005;115(5):1367–1377. doi: 10.1542/peds.2004-1176. [DOI] [PubMed] [Google Scholar]
- 25.Owen CG, Martin RM, Whincup PH, Davey-Smith G, Gillman MW, Cook DG. The effect of breastfeeding on mean body mass index throughout life: a quantitative review of published and unpublished observational evidence. Am J Clin Nutr. 2005;82(6):1298–1307. doi: 10.1093/ajcn/82.6.1298. [DOI] [PubMed] [Google Scholar]
- 26.Heck KE, Braveman P, Cubbin C, Chavez GF, Kiely JL. Socioeconomic status and breastfeeding initiation among California mothers. Public Health Rep. 2006;121(1):51–59. doi: 10.1177/003335490612100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forste R, Weiss J, Lippincott E. The decision to breastfeed in the United States: does race matter? Pediatrics. 2001;108(2):291–296. doi: 10.1542/peds.108.2.291. [DOI] [PubMed] [Google Scholar]
- 28.Kurinij N, Shiono PH, Rhoads GG. Breast-feeding incidence and duration in black and white women. Pediatrics. 1988;81(3):365–371. [PubMed] [Google Scholar]
- 29.Ip S, Chung M, Raman G, et al. Rockville, MD: Agency for Healthcare Research and Quality; Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries. Evidence Report/Technology Assessment No. 153. 2007 April; AHRQ Publication No. 07-E007 (Prepared by Tufts-New England Medical Center Evidence-based Practice Center, under Contract No. 290-02-0022)
- 30.Dolan LM, Bean J, D’Alessio DD, et al. The frequency of abnormal carbohydrate intolerance and diabetes in a population based screening of adolescents. J Pediatr. 2005;146(6):751–758. doi: 10.1016/j.jpeds.2005.01.045. [DOI] [PubMed] [Google Scholar]
- 31.Goodman E, Adler NE, Daniels SR, Morrison JA, Slap GB, Dolan LM. Impact of objective and subjective social status on obesity in a biracial cohort of adolescents. Obes Res. 2003;11(8):1018–1026. doi: 10.1038/oby.2003.140. [DOI] [PubMed] [Google Scholar]
- 32.Ryan AS. The resurgence of breastfeeding in the United States. Pediatrics. 1997;99(4) doi: 10.1542/peds.99.4.e12. Available at: www.pediatrics.org/cgi/content/full/99/4/e12. [DOI] [PubMed] [Google Scholar]
- 33.Cline A, Schafer-Kalkhoff T, Strickland E, Hamann T. Recruitment strategies for the Princeton (Ohio) city school district epidemiologic study. J Sch Health. 2005;57:189–191. [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. [Accessed December 3, 2002];A SAS Program for the CDC Growth Charts. Available at: www.cdc.gov/nccdphp/dnpa/growthcharts/sas.htm.
- 35.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. Advanced data from vital health and statistics; no. 314. Hyattsville, MD: National Center for Health Statistics; 2000. CDC Growth Charts: United States. [PubMed] [Google Scholar]
- 36.Tomeo CA, Rich-Edwards JW, Michels KB, et al. Reproducibility and validity of maternal recall of pregnancy-related events. Epidemiology. 1999;10(6):774–777. [PubMed] [Google Scholar]
- 37.Yawn BP, Suman VJ, Jacobsen SJ. Maternal recall of distant pregnancy events. J Clin Epidemiol. 1998;51(5):399–405. doi: 10.1016/s0895-4356(97)00304-1. [DOI] [PubMed] [Google Scholar]
- 38.Olson JE, Shu XO, Ross JA, Pendergrass T, Robison LL. Medical record validation of maternally reported birth characteristics and pregnancy-related events: a report from the Children’s Cancer Group. Am J Epidemiol. 1997;145(1):58–67. doi: 10.1093/oxfordjournals.aje.a009032. [DOI] [PubMed] [Google Scholar]
- 39.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 40.Sobel M. Asymptotic confidence intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological Methodology. San Francisco, CA: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- 41.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 42.Bogen DL, Hanusa BH, Whitaker RC. The effect of breastfeeding with and without formula use on the risk of obesity at 4 years of age. Obes Res. 2004;12(9):1527–1535. doi: 10.1038/oby.2004.190. [DOI] [PubMed] [Google Scholar]
- 43.Launer LJ, Forman MR, Hundt GL, et al. Maternal recall of infant feeding events is accurate. J Epidemiol Community Health. 1992;46(3):203–206. doi: 10.1136/jech.46.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eaton-Evans J, Dugdale AE. Recall by mothers of the birth weights and feeding of their children. Hum Nutr Appl Nutr. 1986;40(3):171–175. [PubMed] [Google Scholar]
- 45.Tienboon P, IHE R, Wahlqvist M. Maternal recall of infant feeding practices after an interval of 14 to 15 years. Aust J Nutr Diet. 1994;40(3):171–175. [Google Scholar]
- 46.Troy LM, Michels KB, Hunter DJ, et al. Self-reported birth-weight and history of having been breastfed among younger women: an assessment of validity. Int J Epidemiol. 1996;25(1):122–127. doi: 10.1093/ije/25.1.122. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention. Racial and socioeconomic disparities in breastfeeding—United States, 2004. MMWR Morb Mortal Wkly Rep. 2006;55(12):335–339. [PubMed] [Google Scholar]
- 48.Flacking R, Wallin L, Ewald U. Perinatal and socioeconomic determinants of breastfeeding duration in very preterm infants. Acta Paediatr. 2007;96(8):1126–1130. doi: 10.1111/j.1651-2227.2007.00386.x. [DOI] [PubMed] [Google Scholar]
- 49.Li R, Grummer-Strawn L. Racial and ethnic disparities in breastfeeding among United States infants: Third National Health and Nutrition Examination Survey, 1988–1994. Birth. 2002;29(4):251–257. doi: 10.1046/j.1523-536x.2002.00199.x. [DOI] [PubMed] [Google Scholar]
- 50.Ludvigsson JF, Ludvigsson J. Socio-economic determinants, maternal smoking and coffee consumption, and exclusive breastfeeding in 10205 children. Acta Paediatr. 2005;94(9):1310–1319. doi: 10.1111/j.1651-2227.2005.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 51.Noble L, Hand I, Haynes D, McVeigh T, Kim M, Yoon JJ. Factors influencing initiation of breast-feeding among urban women. Am J Perinatol. 2003;20(8):477–483. doi: 10.1055/s-2003-814732. [DOI] [PubMed] [Google Scholar]
- 52.Goodman E. The role of socioeconomic status gradients in explaining differences in US adolescents’ health. Am J Public Health. 1999;89(10):1522–1528. doi: 10.2105/ajph.89.10.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hediger ML, Overpeck MD, Kuczmarski RJ, Ruan WJ. Association between infant breastfeeding and overweight in young children. JAMA. 2001;285(19):2453–2460. doi: 10.1001/jama.285.19.2453. [DOI] [PubMed] [Google Scholar]
- 54.Gartner L, Morton J, Lawrence R, et al. Breastfeeding and the use of human milk. Pediatrics. 2005;115(2):496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]