DR Jette has challenged the gerontological research community to adopt the language of the World Health Organization's International Classification of Functioning, Disability and Health (ICF) for the study of late-life disability (1). I agree that having an internationally agreed-upon language to advance the study of disability, one that can be used across nations and age groups, is extremely appealing. The field will surely benefit from discourse that is broadly understood. At the same time, two very practical challenges seem to be hindering the speedy embrace of the ICF language by the gerontological community.
First, the lack of precision in the crosswalk between the ICF language and the existing measures of late-life functioning can leave a gerontologist who wants to embrace the new language understandably dissatisfied. The widely used measures of functional limitations, activities of daily living (ADLs), and instrumental activities of daily living (IADLs) that most existing surveys and studies of older adults include do not map precisely into the ICF categories as they now stand. Nor at first glance does the ICF language explicitly recognize that performance-based measures of lower extremity functioning, such as the short physical performance battery (2), convey information that is distinctive from—and indeed predictive of—the onset of activity limitations. Subsuming under the rubric of “activities”, functional limitations as well as ADLs and IADLs, ignores critical conceptual distinctions between the building blocks of activities—mobility, upper and lower body movements, sensory and cognitive capabilities—and the activities themselves. As Dr Jette points out, clarifying how the subdomains of activity limitations and participation fit together is an important next step in the development of the ICF that will surely counter some of the inertia.
An additional challenge for purposes of studying disablement is that the ICF is not intended to be a dynamic model. In Dr Jette's words, it is a “framework to code information about health and to equip the international community with a standard language.” The Institute of Medicine's (IOM) Committee on the Future of Disability in America (3) went further, noting:
[T]he ICF is a classification scheme. Unlike the Nagi and 1991 and 1997 IOM frameworks, it does not present a model of disability—or enablement/disablement—as a dynamic process. In this respect, even if a definitional “crosswalk” between these models and ICF concepts is required, process models and their elaborations remain important (see, e.g., Verbrugge and Jette [1994], Fougeyrollas et al. [1998], and Jette and Badley [2002]). Such models help focus research on identifying and understanding interactions among health conditions, other personal characteristics, and environmental factors that contribute to the movement of individuals from one health or disability state to another. (p. 47).
Understandably, some researchers—even those eager to embrace more widely accepted and broadly conceived language—may be uncomfortable parting from a dynamic model with clear concepts, a set of prespecified testable relationships, and validated measures, for a new language not yet fully formulated.
Nevertheless, I believe that if the field can meld the benefits that each approach has to offer, the gerontological community will, in time, adopt the language of the ICF. Over the past year, I have had the unique opportunity to work on this very challenge with a consortium of colleagues who are developing, testing, and fielding a state-of-the-art disability instrument for the National Health and Aging Trends Study (NHATS). Funded by the National Institute on Aging as the successor to the National Long Term Care Survey, NHATS will support studies of disability trends and trajectories in later life. A centerpiece of the study will be a new instrument to measure disability using both performance-based and self-reported measures. It is undeniably a tall order, and we are both excited and humbled by the opportunity.
Our experience to date may be instructive. The group began with the premise that adopting the language of the ICF would indeed be useful. Beyond its broad acceptance and the potential for universal interpretation, the ICF also offers some new language for those interested in expanding the scope of study related to the disablement process. In particular, the addition of the term “participation” to our vocabulary brings into the dialogue concepts of participating in productive, generative, community, social, and civic life. Notably, Fried and colleagues (4) have already moved in this direction with their study of older adults’ participation in a volunteer school-based program, which suggested positive effects of such a program on physical, cognitive, and social activity. A second advantage is the explicit and broadly defined role for the environment, both physical and social, as well as more macro policies and systems. In this regard, explicit recognition that the environment plays a role at every stage of the disablement process is an important advancement, one ripe for hypothesis testing (5). Third, the availability of positive analogues for concepts that have traditionally been expressed in terms of loss is an advancement that allows researchers to bring into focus questions about how best to maximize functioning of older adults, irrespective of their stage in the disablement process (6). Finally, the distinction between capacity to perform and actual performance of a range of activities (7) opens up the possibility of studying how accommodations such as assistive devices and changes to the environment might bridge the gap between an individual's underlying capacity and actual performance of activities (8).
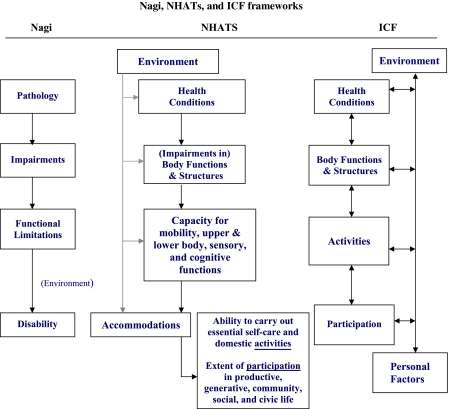
During the design phase of NHATS, we have drawn upon this new language, as well as our highly valued Nagi roots. Four points regarding the middle panel of Figure 1—our current NHATS conceptualization—are noteworthy:
We highlight the ICF term “capacity” to refer to an individual's physiological, cognitive, and sensory capabilities to carry out the building blocks of activities (e.g., mobility and other physical movements, learning, remembering, seeing, hearing, and communicating). Such measures are frequently subsumed in Nagi's “functional limitations,” whereas the ICF considers these for the most part subdomains of both “activities” and “participation.” We envision assessing these domains mainly through performance measures.
We add a new domain—“accommodations”—that does not appear explicitly in either the Nagi model or the ICF framework. We define accommodations as behavioral responses to changes in capacity and include in this domain the receipt of help, take-up of assistive technology, changes to the environment, and other compensatory strategies (9) such as doing an activity less frequently, more slowly, or differently.
The final “box” in the framework specifies two distinct concepts: the ability to carry out self-care (ADL-like) and domestic life (IADL-like) activities and the extent of participation in productive, generative, community, social, and civic life. The former reflects what is typically assessed as “disability” under the Nagi model. The latter explicitly captures elective but valued activities that represent an important extension of concerns about quality of life beyond the basics of self-care and domestic life. The work of Jette and colleagues (10,11) offers important foundations for empirically characterizing such distinctions.
We recognize, as does the ICF, that the environment may influence the entire disablement process, and we envision measuring not only the physical but also the social and technological environments in which older adults carry out activities.
Figure 1.
Nagi, NHATs, and ICF frameworks.
NHATS workgroups are currently operationalizing these concepts. It is early in the development process, with much testing yet to do before the new measures are deemed valid, and even more importantly, proven useful. But I hope—as in “A Field of Dreams”—if we build, validate, and disseminate such measures, gerontologists will surely come.
FUNDING
Funding was provided by the National Institute on Aging at the National Institutes of Health (U01-AG032947).
Acknowledgments
I gratefully acknowledge the helpful comments of Judith Kasper (Principal Investigator, NHATS, Johns Hopkins Bloomberg School of Public Health) and the contributions of the NHATS team members to the framework development. The views expressed are those of the author alone and do not reflect the University of Medicine and Dentistry of New Jersey or funding agency.
References
- 1.Jette AM. J Gerontol A Biol Sci Med Sci. 2009. Toward a common language of disablement. doi:10.1093/gerona/glp093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine. The Future of Disability in America. Washington, DC: The National Academies Press; 2007. [PubMed] [Google Scholar]
- 4.Fried LP, Carlson MC, Freedman M, et al. A social model for health promotion for an aging population: initial evidence on the Experience Corps model. J Urban Health. 2004;81(1):64–78. doi: 10.1093/jurban/jth094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keysor J. How does the environment influence disability? Examining the evidence. In: Field MJ, Jette AM, Martin LG, editors. Workshop on Disability in America: A New Look. Washington, DC: National Academies Press; 2006. pp. 88–100. [Google Scholar]
- 6.Albert SM. Public Health and Aging: An Introduction to Maximizing Function and Well-Being. New York, NY: Springer Publishing Company; 2004. [Google Scholar]
- 7.World Health Organization. Towards a Common Language For Functioning, Disability and Health ICF. The International Classification of Functioning, Disability and Health. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 8.Agree EM, Freedman VA. A comparison of assistive technology and personal care in alleviating disability and unmet need. Gerontologist. 2003;43(3):142–151. doi: 10.1093/geront/43.3.335. [DOI] [PubMed] [Google Scholar]
- 9.Weiss CO, Hoenig HM, Fried LP. Compensatory strategies used by older adults facing mobility disability. Arch Phys Med Rehabil. 2007;88(9):1217–1220. doi: 10.1016/j.apmr.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Jette AM, Haley SM, Kooyoomjian JT. Are the ICF activity and participation dimensions distinct? J Rehabil Med. 2003;35:145–149. doi: 10.1080/16501970310010501. [DOI] [PubMed] [Google Scholar]
- 11.Jette AM, Tao W, Haley S. Blending activity and participation sub-domains of the ICF. Disabil Rehabil. 2007;29(22):1742–1750. doi: 10.1080/09638280601164790. [DOI] [PubMed] [Google Scholar]