Abstract
Objectives
To measure trends and characteristics of first-time nursing home admissions for individuals with mental illness, dementia or both from 1999–2005.
Methods
The Minimum Data Set was used to estimate the number and percent of elderly residents newly admitted to nursing homes who had mental illness (schizophrenia, bipolar disorder, depression or anxiety), dementia, or both from 1999–2005. In 2005, demographic factors, comorbidities, and treatments by mental illness status were compared.
Results
The number of individuals admitted with mental illness increased from 168,721 in 1999 to 187,478 in 2005 and currently exceeds by 50% the number admitted with dementia only (118,290 in 2005). This increase in mental illness is driven by depression, which increased from 128,566 to 154,262. Residents admitted with depression exhibited higher rates of comorbidities, high rates of antidepressant treatment, and high rates of receiving training in skills required to return to the community.
Conclusions
Over the past decade, the number of nursing home admissions for mental illness, in particular depression, has overtaken the number for dementia. These changes may be related to increased recognition of depression, changes in the availability of nursing home substitutes for residents with dementia, and the increased specialization of nursing homes in the care of post-acute, rehabilitation residents. In recognition of these changes, improving the resources of nursing homes to adequately treat residents with mental illness is critical to help facilitate reintegration into the community.
Background
Mental illness is common among nursing home residents. The high prevalence of residents with dementia is known, but major mental illness other than dementia is also common; indeed, the 560,000 nursing home residents with a mental illness other than dementia dwarf the 51,000 [1] individuals in beds at psychiatric hospitals. Mental illness is one, and sometimes the decisive, factor contributing to placement in nursing homes [2]. Addressing the needs of nursing home residents with behavioral symptoms associated with dementia has been a principal focus of research in nursing homes [3, 4]. However, less is known about individuals in nursing homes who have major mental illness.
Estimates from the literature of the rate of significant depressive symptoms among nursing home residents range from 10–44% [5–7]. Estimates of the prevalence of schizophrenia in nursing homes range from 4–13% [8, 9]. Among individuals with mental illness, a diagnosis of schizophrenia or bipolar disorder is associated with a greater likelihood of admission to a nursing home over a three-year period [10] and depression increases the risk of nursing home admission both from the community and after acute hospitalizations [11–13]. Depression and behavioral symptoms in nursing home residents are associated with high rates of functional impairment, disability, worse health outcomes, increased rates of hospitalization and mortality, and greater emergency service use [14–18]. High rates of medical comorbidities, deficits in activities of daily living and instrumental activities of daily living, cognitive impairment, and lack of available family members predict nursing home residence for older adults with mental illness [19, 20].
The nursing home sector has undergone a remarkable transformation over the past two decades with respect to payers and patient mix. Up to the early 1980s, nursing homes largely provided custodial care to long-stay residents. The short-stay, post-acute side of the nursing home market was negligible. Medicare, the primary payer for these services, accounted for only 1.6% of total nursing home expenditures in 1980 [21]. A series of policy changes, however, expanded the post-acute side of the market. Medicare now accounts for 15.7% of all nursing home expenditures. Further, federal standards for Medicaid reimbursement were repealed and social work services were bundled into the nursing home's per diem rate. Growth in short-stay nursing home residents and decreased reimbursement for social work may imply important changes in the relative proportions of nursing home residents admitted with mental illness and dementia.
Little is known about recent trends of admissions of individuals with mental illness to nursing homes. This observational study uses longitudinal data on the census of new nursing home admissions to describe trends in mental illness. We regard this as a first step in directing research and policy attention to the largest population of vulnerable persons with mental illness in institutionalized settings. More specifically, we examine admissions to nursing homes of individuals diagnosed with mental illness, dementia or both from 1999–2005. We compare the demographics, comorbidities, and treatment of individuals with and without mental illness.
Methods
Data
We used the CMS national registry of nursing home resident assessments from the Minimum Data Set (MDS) to examine the prevalence of mental illness in new nursing home admissions. The MDS resident assessment instrument contains nearly 400 data elements, including cognitive functioning, physical functioning, psychosocial well-being, diagnoses, and treatment variables. In describing annual trends, we examined all first-time admissions (N=7,364,470) from 1999–2005 and short-stay and long-stay admissions from 1999–2004. We used the 2005 data (n=996,311) to examine demographics, comorbidities, and treatment variables. Institutional Review Board permission was obtained for this study.
Measures
Mental Illness Diagnosis
We defined admission behavioral health diagnosis based upon the MDS full assessment form. We grouped individuals into four overall categories: individuals diagnosed with mental illness only (Section I1dd, I1ee, I1ff, or I1gg indicated on admission MDS), dementia (including Alzheimer's and other dementia) only (Section I1q or I1u indicated), both mental illness and dementia, and neither. The “mental illness only” category was further categorized into schizophrenia, bipolar disorder, depression and anxiety. These categories were hierarchically assigned in the above order. For example, an individual indicating both schizophrenia and anxiety was assigned to the schizophrenia group. The MDS does not include the primary reason for admission and thus a mental illness diagnosis can represent either the primary reason for admission or a comorbid condition.
Demographics, Comorbidity, and Mental Health Treatment
Age, sex, race, marital status, and educational status are documented on the MDS full assessment form. We categorized race as white, black, Hispanic, and other (American Indian/Alaskan Native and Asian/Pacific Islander). Marital status was classified as never married, married, widowed, and separated/divorced. Educational status was categorized as less than high school (including no schooling, 8th grade or less, and 9–11 grades), graduated high school (including high school, technical or trade school, some college), graduated college, graduate degree, or unknown (not reported). We identified the following comorbid conditions: diabetes, other endocrine, cardiovascular, musculoskeletal, neurological excluding dementia, pulmonary, sensory, and other diseases. Limitations with activities of daily living were calculated based on a scale ranging from zero to twenty-eight, with higher values implying greater disability. We used CMS's definition of cognitive impairment as those with impaired short-term memory (MDS item B2a=1) and non-independent in regards to daily decision making (MDS item B4>0). Treatment variables included both pharmaceutical and non-pharmaceutical treatment provided within the past 7 or 14 days. Pharmaceutical treatment variables included average number of medications and any receipt of antipsychotics, antidepressants, or anxiolytics/hypnotics within the past 7 days. Other treatments consisted of residence in an Alzheimer's/dementia special care unit (in the last 14 days); receipt of training skills to return to the community (in the last 14 days); evaluation/treatment by mental health specialist (in the last 7 days); and use of restraints (in the last 7 days).
Short-stay vs, Long-stay
Following Mor et. al. (2007), if a resident was discharged within 90 days, he or she was categorized as a short-stay resident. If a resident remained in the nursing home at least 90 days, he or she was termed a long-stay resident [22].
Analysis
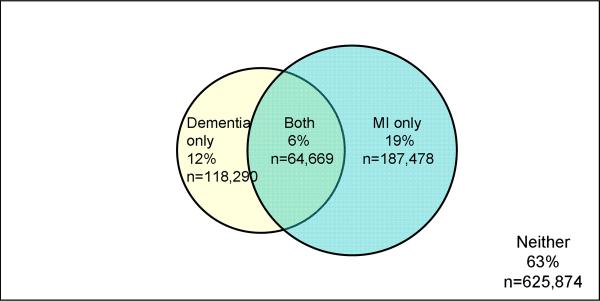
A Venn diagram displays the prevalence of individuals admitted to nursing homes with mental illness only, dementia only, both mental illness and dementia, and neither condition in 2005. We examined overall trends in these conditions as well as in short-stay and long-stay populations. We calculated the overall prevalence of the psychiatric illnesses listed above in individuals admitted to nursing homes from 1999–2005. We describe the demographics, co-morbidities and treatments by mental illness category in 2005. Statistical comparisons for categorical variables were made using an overall chi-square test.
Results
In 2005, the MDS data indicate that the number of new nursing home admissions with a mental illness exceeded the number with dementia (see Figure 1). Of the 996,311 new nursing home admissions across the U.S., 24% had a mental illness as defined by schizophrenia, bipolar disorder, depression, and anxiety disorders, while 18% had Alzheimer's Disease or other dementias. There is some overlap with 6% of all residents admitted having both mental illness and dementia. The remaining 63% of new nursing home admits had no mental illness or dementia diagnoses.
Figure 1.
Venn Diagram of the Prevalence of Dementia and Mental Illness in Nursing Homes among New Admissions, 2005
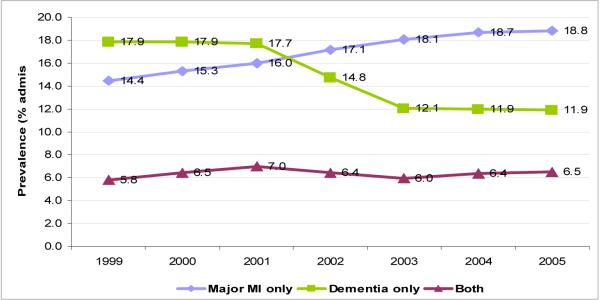
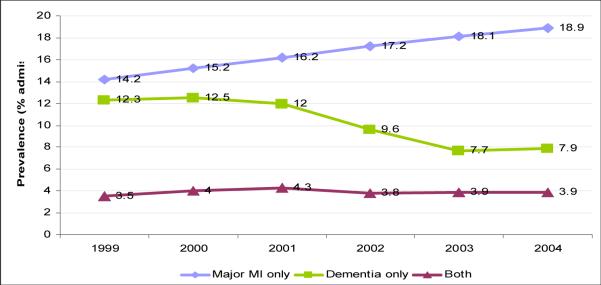
The relative proportion as well as the absolute number of new nursing home admits with mental illness and dementia reflects important changes over recent years (see Figure 2A–2C). In 1999, the number of new admissions with dementia exceeded the number with mental illness. By 2005, the number with mental illness exceeded the number with dementia. Residents admitted with mental illness increased from 168,721 to 187,478 and the number of residents admitted with dementia fell from 208,505 to 118,290. The percent of individuals admitted with both mental illness and dementia was roughly constant.
Figure 2A.
New admission trends for dementia, mental illness, or both, 1999–2005
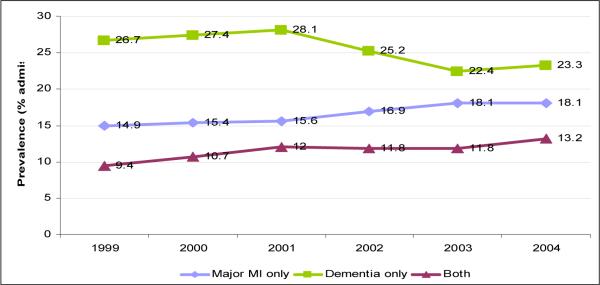
Figure 2C.
New Admission trends for dementia, mental illness, or both 1999–2004 in long-stay residents
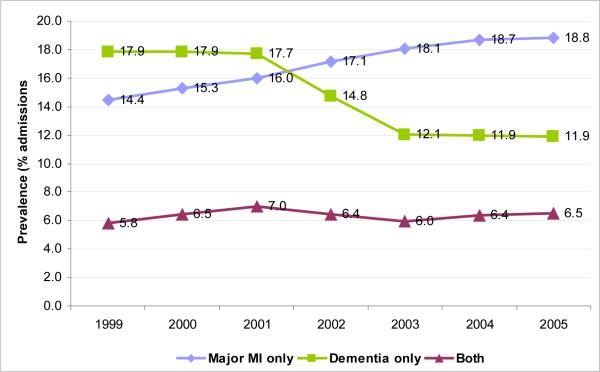
In 1999, long-stay admissions accounted for 38.5% of admissions. By 2005, this proportion was 25.3%. Similar trends to those above are seen in short-stay and long-stay residents. As expected, the absolute percentage of dementia only residents is higher in the long-stay population. From 1999–2004, the proportion of residents admitted with dementia decreased in both the short-stay (by 4.4 percentage points) and long-stay (by 3.4 percentage points) populations. Alternatively, the proportion of residents admitted with mental illness increased in both the short-stay (by 4.7 percentage points) and long-stay residents (by 3.2 percentage points). In both cases, the trends are stronger in the short-stay population. Finally, the proportion of residents admitted with both dementia and mental illness increased in the long-stay population (by 3.4 percentage points).
The number of individuals admitted with depression increased four percentage points from 11.0% (N=128,566) to 15.5% (N=154,262) between 1999 and 2005 (Figure 3). There was a one tenth of one percentage point increase in bipolar disorder admissions (from 0.4% (N=4,597) to 0.5% (N=5,299)), a two tenths of one percentage point decline in anxiety admissions (from 2.5% (N=29,221) to 2.3% (N=22,513)), and the percent of schizophrenia admissions remained roughly constant at 0.5%. Thus, the large increase in mental illness admissions over 1999–2005 was primarily due to the increase in residents with a depression diagnosis.
Figure 3.
New admission trends for mental illness excluding dementia, 1999–2005
Individuals admitted with mental illness or dementia differed from other nursing home residents (and one another) in their demographics, co-morbidities and treatments received (see Table 1). Relative to new admits without mental illness or dementia, individuals with a mental illness were generally younger and white (excluding those with schizophrenia). Those admitted with schizophrenia, anxiety, or dementia were more poorly educated and those with schizophrenia or bipolar were less likely to have been married. Admissions with schizophrenia or bipolar disorder had relatively lower activities of daily living scores and higher levels of cognitive impairment than individuals with depression, anxiety, or neither mental illness nor dementia. Individuals with anxiety, depression, or dementia were more likely to have cardiovascular, musculoskeletal, or neurological comorbidities. Those with any mental illness were more likely to have pulmonary disease. Individuals with schizophrenia or dementia were on fewer medications. As expected, individuals with depression had higher rates of antidepressant treatment, individuals with schizophrenia; bipolar disorder, and to a lesser extent dementia, had higher rates of anti-psychotic use; and individuals with anxiety had higher rates of anxiolytic/hypnotic use. Those with schizophrenia and dementia were less likely to receive training in skills required to return to the community and more likely to be physically or chemically restrained than those with bipolar, depression, anxiety, or without mental illness or dementia. Finally, those with mental illness or dementia were more likely to receive evaluation or therapy by a licensed mental health professional. Given the large numbers involved, all overall differences were statistically significant at a p<0.001 level.
Table 1.
Demographic and treatment variables for new nursing home admissions in 2005
| Major Mental Illness Only |
Dementia Only | Both | Neither | Total | ||||
|---|---|---|---|---|---|---|---|---|
| Schizophrenia | Manic Depression | Depression | Anxiety | |||||
| N | 5,404 | 5,299 | 154,262 | 22,513 | 118,290 | 64,669 | 625,874 | 996,311 |
| Average Age* | 74.2 | 75.2 | 79.4 | 80.1 | 83.9 | 82.5 | 80.7 | 80.9 |
| Female | 66.4 | 67.6 | 68.6 | 74.3 | 63.1 | 69.1 | 62.6 | 64.3 |
| Race | ||||||||
| White | 76.3 | 92.6 | 91.2 | 91.8 | 83.2 | 89.6 | 85.7 | 86.6 |
| Black | 17.1 | 4.3 | 4.5 | 4.0 | 11.5 | 6.0 | 8.9 | 8.2 |
| Hispanic | 4.9 | 2.4 | 3.2 | 3.3 | 3.3 | 3.2 | 3.5 | 3.4 |
| Other | 1.8 | 0.8 | 1.1 | 0.8 | 2.0 | 1.2 | 2.0 | 1.7 |
| Education | ||||||||
| <High School | 29.7 | 15.3 | 18.8 | 30.2 | 33.4 | 30.7 | 19.2 | 21.8 |
| Graduated High School | 40.3 | 44.9 | 45.5 | 59.5 | 54.5 | 57.4 | 41.8 | 45.2 |
| Graduated College | 3.7 | 7.2 | 5.4 | 5.8 | 6.3 | 6.6 | 5.2 | 5.4 |
| Graduate Degree | 1.5 | 4.9 | 2.8 | 2.8 | 3.3 | 3.3 | 2.7 | 2.8 |
| Unknown (missing) | 24.8 | 27.6 | 27.5 | 1.7 | 2.6 | 2.1 | 31.2 | 24.6 |
| Marital status | ||||||||
| Never Married | 32.2 | 11.6 | 5.8 | 6.8 | 6.8 | 5.8 | 7.7 | 7.3 |
| Married | 15.5 | 33.4 | 35.2 | 31.4 | 33.3 | 31.7 | 36.2 | 35.2 |
| Widowed | 30.9 | 36.3 | 50.2 | 53.0 | 53.6 | 55.2 | 48.4 | 49.7 |
| Separated/Divorced | 21.3 | 18.6 | 8.8 | 8.9 | 6.4 | 7.3 | 7.7 | 7.8 |
| Functional Status | ||||||||
| Average ADL score (0–28)* | 13.3 | 13.9 | 15.2 | 14.7 | 16.0 | 15.4 | 14.9 | 15.1 |
| Cognitive impairment* | 55.3 | 44.2 | 37.1 | 31.0 | 87.3 | 85.7 | 31.7 | 42.8 |
| Diseases | ||||||||
| Diabetes | 31.5 | 28.0 | 30.3 | 24.9 | 22.3 | 21.8 | 28.4 | 27.5 |
| Endocrine excluding diabetes | 10.6 | 15.9 | 12.1 | 18.8 | 15.9 | 20.1 | 8.2 | 10.8 |
| Cardiovascular | 55.5 | 56.1 | 64.3 | 84.9 | 77.8 | 79.7 | 58.7 | 63.7 |
| Musculoskeletal | 22.0 | 26.4 | 30.6 | 48.1 | 38.1 | 44.6 | 26.4 | 30.1 |
| Neurological excluding dementia | 11.2 | 10.3 | 15.6 | 11.2 | 15.6 | 15.4 | 13.2 | 13.9 |
| Pulmonary | 26.0 | 25.5 | 25.2 | 31.6 | 13.7 | 16.8 | 19.9 | 20.1 |
| Sensory | 5.2 | 5.2 | 7.3 | 12.7 | 11.6 | 13.8 | 5.9 | 7.4 |
| Other | 29.3 | 32.4 | 34.4 | 60.3 | 43.2 | 47.8 | 28.1 | 32.9 |
| Medications | ||||||||
| Average # medications* | 10.0 | 11.5 | 12.2 | 11.5 | 8.5 | 10.2 | 10.3 | 10.4 |
| Antipsychotics | 78.2 | 53.7 | 11.0 | 7.5 | 27.3 | 37.6 | 5.5 | 11.7 |
| Antidepressants | 36.1 | 54.3 | 81.8 | 18.0 | 14.4 | 70.4 | 10.8 | 26.6 |
| Anxiolytics/hypnotics | 24.4 | 35.5 | 34.0 | 69.6 | 16.8 | 32.1 | 20.7 | 24.2 |
| Other treatments | ||||||||
| Alzheimer's/dementia special care unit | 3.4 | 1.9 | 0.8 | 0.4 | 10.3 | 11.6 | 0.6 | 2.5 |
| Skills training to return to community | 35.6 | 54.0 | 58.7 | 55.1 | 34.5 | 34.4 | 59.8 | 54.7 |
| Evaluation or therapy by licensed mental health professional | 19.1 | 15.2 | 5.4 | 3.6 | 8.2 | 16.8 | 1.1 | 3.8 |
| Restraints excluding bed rails | 2.2 | 1.8 | 1.3 | 1.5 | 5.4 | 5.5 | 1.3 | 2.1 |
Notes: ADL=activities of daily living
Because of the substantial increase in individuals admitted with depression over time, we examined the demographic, clinical, and treatment variables above for 1999 as well as 2005. Age, gender and racial make up were largely the same. We saw an increase in depressed individuals who were married (31.7 to 35.2) and decrease in those who were widowed (55.1 to 50.2). Functional status was similar. With the exception of diabetes and lung disease both of which increased, all other comorbidities decreased from 1999 to 2005. Treatment variables showed that in 2005 individuals were on more medications (12.2 versus 10.4 in 1999), used more psychotropics (antipsychotics: 11.0% in 2005 versus 8.3% in 1999; antidepressants: 81.8% versus 77.8%; and anxiolytics: 34% versus 32.5%) and required fewer restraints (1.3 in 2005 versus 2.4 in 1999). Finally, a higher percentage of depressed residents received skills training to return to the community in 2005 (58.7% versus 41.8%) and fewer were evaluated by a mental health professional (5.4% versus 10.4%).
Discussion
Over the past decade, admissions to nursing homes for individuals with dementia decreased and admissions for residents with non-dementia mental illness, primarily depression, increased. As expected, individuals admitted with a major mental illness or dementia differ from one another and other nursing home residents in terms of their demographics, co-morbidities and treatments received.
These findings raise two important questions. First, what explains the change in mix of admissions? And second, what does this new mix of patients imply for nursing homes and the treatment of persons with mental illness?
One explanation for the decrease in dementia admissions (and the increase in depression admissions) is the growth of post-acute, short-stay nursing home residents. Individuals with dementia are more likely to be admitted for long-stay placement and nursing homes have increasingly shifted away from the long-stay population. Higher payments for post-acute stays by Medicare in contrast to lower payments by Medicaid for long-term care contribute to this shift. A second factor is the increased development of alternatives to nursing homes for individuals with dementia. In particular, assisted living facilities and increased home support for individuals with dementia have attracted some away from nursing homes [23, 24].
Individuals admitted with depression (either primary or secondary diagnosis) increased markedly from 1999–2005. Depression studies in the elderly have shown increases in the diagnosis of depression in community dwelling elderly during the 1990s. Crystal and colleagues found that the percent of elderly Medicare beneficiaries diagnosed with depression increased from 2.8% in 1992 to 5.8% in 1998 [25]. Follow-up studies found that this increase was consistent with the utilization of new treatment modalities such as the selective serotonin reuptake inhibitors [25–27]. Increases in either recognition or prevalence could explain observed increases in admissions with depression.
The numbers of individuals with severe mental illnesses such as schizophrenia or bipolar disorder has remained roughly constant. Medicaid waivers for developing home and community based services for individuals with mental illness have been negligible [28]. Past studies have shown that cognitive impairment, limited activities of daily living, and social isolation place individuals at risk both of nursing home admission and becoming long stay residents [29–32]. We have shown that individuals with schizophrenia and bipolar disorder have high rates of cognitive impairment and social isolation placing them at greater risk of nursing home admission.
Turning to the second question, nursing homes are coping with a large influx of post-acute patients with comorbid depression. The ramifications of depression on nursing home use, hospital readmission, and reintegration into the community remain questions only beginning to be explored. Studies have shown that depression places elderly individuals hospitalized for stroke at a higher risk of nursing home placement; depression prolongs nursing home care and increases costs in acute and rehabilitation services; and depression increases the risk of rehospitalization [33–35]. In addition, the increased morbidity often associated with depression such as poor medication compliance, poor self care, and increased mortality places individuals with depression at greater risk of requiring nursing home care [12, 13]. Whether or not more intensive treatment of depression can improve outcomes for these individuals is unknown.
Given these issues, a key concern moving forward is the quality of care received by individuals with a mental illness in nursing homes. The Omnibus Budget Reconciliation Act (OBRA) of 1987 was the most recent major policy reform directly addressing the need for appropriate mental health services in nursing homes. These regulations mandated a Pre-Admission Screening and Annual Resident Review (PASARR) to identify nursing home residents with a history of mental illness. However, studies report low rates of compliance with the implementation of recommended mental health services [36, 37]. Only 35% of preadmission screening recommendations for new mental health services are followed [38]. Among nursing home residents with an identified, known psychiatric diagnosis, less than two-fifths (36%) receive a mental health visit during a year [39]. Approximately one-fifth of all nursing homes receive a deficiency citation each year for mental health care as part of the federal survey and certification process [40, 41].
The MDS data have limitations. The MDS depends on assessment nurses accurately recording the information including diagnoses. Studies have generally confirmed the reliability and validity of these data, with some variability across nursing homes [42]. A recent examination shows that rates of diagnosis of mental illness are slightly higher in the MDS (46%) than the National Nursing Home Survey (33.1%) in a cross-sectional analysis[43]. The recorded diagnosis is not a validated method and this may lead to individuals being misclassified as having or not having depression. Both diagnostic biases should be systematic over time; however, it is possible that the trends reported result from an increase in these biases over time. Further, we were not able to verify diagnosis, treatment, or functional measures from outside sources. The linkage of the MDS to other potential data sources (e.g., claims data) would help to address this limitation. However, the fact that the medication patterns largely supported the disease classifications is reassuring. Finally, we constructed our sample based on first-time nursing home admissions rather than a single cross-section of residents at a given time point each year. As such, our data examines the flow of residents into nursing homes but not how they accumulate in nursing homes.
Conclusions
Over the past decade, the composition of mental illness and dementia in nursing homes has evolved. The number of admissions for dementia patients has fallen dramatically and mental illness, in particular depression, has increased. Given the high rates of comorbidity and the mixed treatment success in nursing homes, increased focus should be placed on understanding the contribution mental illness plays in nursing home placement and subsequent quality and cost of care. In particular, research focused on understanding the impact of depression as well as interventions aimed at treating depression on nursing home costs, community reintegration, and hospital readmissions will be particularly important as the rates of depression in post-acute care nursing homes increase.
Figure 2B.
New admission trends for dementia, mental illness, or both 1999–2004 in short-stay residents
Acknowledgements
Dr. Fullerton was supported in part by grant 5T32-MH019733 from the National Institute of Mental Health (NIMH). Dr. McGuire was supported by grant P60-MD002261 from the National Center for Minority Health and Health Disparities and NIMH grant P50 MH073469. Dr. Feng and Dr. Mor were supported in part by grant R01-AG26465 from the National Institute on Aging (NIA), which also supported the data use agreement for this work (DUA 15293). Dr. Grabowski was supported in part by NIA career development award K01-AG024403.
Footnotes
Disclosures: None for any author.
References
- 1.Frank RG, Glied SA. Better but not Well: Mental Health Policy in the United States since 1950. Johns Hopkins University Press; Baltimore: 2006. [Google Scholar]
- 2.Black BS, Rabins PV, German PS. Predictors of nursing home placement among elderly public housing residents. Gerontologist. 1999;39:559–568. doi: 10.1093/geront/39.5.559. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell SL, Kiely DK, Hamel MB, et al. Estimating prognosis for nursing home residents with advanced dementia. Journal of the American Medical Association. 2004;291:2734–2740. doi: 10.1001/jama.291.22.2734. [DOI] [PubMed] [Google Scholar]
- 4.Phillips CD, Spry KM, Sloane PD, et al. Use of physical restraints and psychotropic medications in Alzheimer special care units in nursing homes. American Journal of Public Health. 2000;90:92–96. doi: 10.2105/ajph.90.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devanand DP, Jacobs DM, Tang MX, et al. The course of psychopathologic features in mild to moderate Alzheimer disease. Archives of General Psychiatry. 1997;54:257–263. doi: 10.1001/archpsyc.1997.01830150083012. [DOI] [PubMed] [Google Scholar]
- 6.Burrows AB, Satlin A, Salzman C, et al. Depression in a long-term care facility: Clinical features and discordance between nursing assessment and patient interviews. Journal of the American Geriatrics Society. 1995;43:1118–1122. doi: 10.1111/j.1532-5415.1995.tb07011.x. [DOI] [PubMed] [Google Scholar]
- 7.Lyketsos CG, Steinberg M, Tschanz JT, et al. Mental and behavioral disturbances in dementia: Findings from the Cache County study on memory in ageing. American Journal of Psychiatry. 2000;157:708–714. doi: 10.1176/appi.ajp.157.5.708. [DOI] [PubMed] [Google Scholar]
- 8.Mechanic D, McAlpine DD. Use of nursing homes in the care of persons with severe mental illness: 1985–1995. Psychiatric Services. 2000;51:354–358. doi: 10.1176/appi.ps.51.3.354. [DOI] [PubMed] [Google Scholar]
- 9.McCarthy JF, Blow FC, Kales HC. Disruptive behaviors in veterans affairs nursing home residents: How different are residents with serious mental illness? Journal of the American Geriatrics Society. 2004;52:2031–2038. doi: 10.1111/j.1532-5415.2004.52559.x. [DOI] [PubMed] [Google Scholar]
- 10.Miller EA, Rosenheck RA. Risk of nursing home admission in association with mental illness nationally in the Department of Veterans Affairs. Medical Care. 2006;44:343–351. doi: 10.1097/01.mlr.0000204008.83633.ed. [DOI] [PubMed] [Google Scholar]
- 11.Onder G, Liperoti R, Soldato M, et al. Depression and risk of nursing home admission among older adults in home care in Europe: Results from the Aged in Home Care (AdHOC) study. Journal of Clinical Psychiatry. 2007;68:1392–1398. doi: 10.4088/jcp.v68n0910. [DOI] [PubMed] [Google Scholar]
- 12.Harris Y. Depression as a risk factor for nursing home admission among older individuals. Journal of the American Medical Directors Association. 2007;8:271. doi: 10.1016/j.jamda.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 13.Harris Y, Cooper JK. Depressive symptoms in older people predict nursing home admission. Journal of the American Geriatrics Society. 2006;54:593–597. doi: 10.1111/j.1532-5415.2006.00687.x. [DOI] [PubMed] [Google Scholar]
- 14.Gates DM, Fitzwater E, Meyer U. Violence against caregivers in nursing homes - expected, tolerated, and accepted. Journal of Gerontological Nursing. 1999;25:12–22. doi: 10.3928/0098-9134-19990401-05. [DOI] [PubMed] [Google Scholar]
- 15.Forsell Y, Winblad B. Major depression in a population of demented and nondemented older people: Prevalence and correlates. Journal of the American Geriatrics Society. 1998;46:27–30. doi: 10.1111/j.1532-5415.1998.tb01009.x. [DOI] [PubMed] [Google Scholar]
- 16.Kales HC, Blow FC, Copeland LA, et al. Health care utilization by older patients with coexisting dementia and depression. American Journal of Psychiatry. 1999;156:550–556. doi: 10.1176/ajp.156.4.550. [DOI] [PubMed] [Google Scholar]
- 17.Clyburn LD, Stones MJ, Hadjistavropoulos T, et al. Predicting caregiver burden and depression in Alzheimer's disease. Journal of Gerontology: B: Psychological Science and Social Science. 2000;55:S2–13. doi: 10.1093/geronb/55.1.s2. [DOI] [PubMed] [Google Scholar]
- 18.Bartels SJ, Horn SD, Smouth RJ, et al. Agitation and depression in frail nursing home elderly patients with dementia: Treatment characteristics and service use. American Journal of Geriatric Psychiatry. 2003;11:231–238. [PubMed] [Google Scholar]
- 19.Bartels SJ, Mueser KT, Miles KM. A comparative study of elderly patients with schizophrenia and bipolar disorder in nursing homes and the community. Schizophrenia Research. 1997;27:181–190. doi: 10.1016/S0920-9964(97)00080-7. [DOI] [PubMed] [Google Scholar]
- 20.Kilbourne AM, Cornelius JR, Han X, et al. General-medical conditions in older patients with serious mental illness. American Journal of Geriatric Psychiatry. 2005;13:250–254. doi: 10.1176/appi.ajgp.13.3.250. [DOI] [PubMed] [Google Scholar]
- 21.National Center for Health Statistics . Health, United States, 2007 With Chartbook on Trends in the Health of Americans. Hyattsville, MD: 2007. [PubMed] [Google Scholar]
- 22.Mor V, Zinn J, Gozalo P, et al. Prospects for transferring nursing home residents to the communtiy. Health Affairs. 2007;26:1762–1771. doi: 10.1377/hlthaff.26.6.1762. [DOI] [PubMed] [Google Scholar]
- 23.Leon J, Moyer D. Potential cost savings in residential care for Alzheimer's disease patients. Gerontologist. 1999;39:440–449. doi: 10.1093/geront/39.4.440. [DOI] [PubMed] [Google Scholar]
- 24.Kopetz S, Steele CD, Brandt J, et al. Characteristics and outcomes of dementia residents in an assisted living facility. International Journal of Geriatric Psychiatry. 2000;15:586–593. doi: 10.1002/1099-1166(200007)15:7<586::aid-gps148>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 25.Crystal S, Sambamoorthi U, Walkup JT, et al. Diagnosis and treatment of depression in the elderly Medicare population: Predictors, disparities, and trends. Journal of the American Geriatrics Society. 2003;51:1718–1728. doi: 10.1046/j.1532-5415.2003.51555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olfson M, Marcus SC, Druss B, et al. National trends in the outpatient treatment of depression. JAMA. 2002;287:203–209. doi: 10.1001/jama.287.2.203. [DOI] [PubMed] [Google Scholar]
- 27.Sambamoorthi U, Olfson M, Walkup JT, et al. Diffusion of new generation antidepressant treatment among elderly diagnosed with depression. Medical Care. 2003;41:180–194. doi: 10.1097/00005650-200301000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Shirk C. Rebalancing long-term care: The role of the Medicaid HCBS waiver program. National Health Policy Forum; Washington DC: 2006. [Google Scholar]
- 29.Reschovsky JD. The demand for post-acute and chronic care nursing in nursing homes. Medical Care. 1998;36:475–490. doi: 10.1097/00005650-199804000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Coughlin TA, McBride TD, Liu K. Determinants of transitory and permanent nursing home admissions. Medical Care. 1990;28:616–631. doi: 10.1097/00005650-199007000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Liu K, McBride TD, Coughlin TA. Risk of entering nursing homes for long versus short stays. Medical Care. 1994;32:315–327. doi: 10.1097/00005650-199404000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Greene V, Ondrich J. Risk factors for nursing home admissions and exits: a discrete-time hazard function approach. J Gerontol. 1990;45:S250–258. doi: 10.1093/geronj/45.6.s250. [DOI] [PubMed] [Google Scholar]
- 33.Nuyen J, Spreeuwenberg PM, Groenewegen PP, et al. Impact of preexisting depression on length of stay and discharge destination among patients hospitalized for acute stroke: linked register-based study. Stroke. 2008;39:132–138. doi: 10.1161/STROKEAHA.107.490565. [DOI] [PubMed] [Google Scholar]
- 34.Bula CJ, Wietlisbach V, Burnand B, et al. Depressive symptoms as a predictor of 6-month outcomes and services utilization in elderly medical inpatients. Archives of Internal Medicine. 2001;161:2609–2615. doi: 10.1001/archinte.161.21.2609. [DOI] [PubMed] [Google Scholar]
- 35.Webber AP, Martin JL, Harker JO, et al. Depression in older patients admitted for postacute nursing home rehabilitation. Journal of the American Geriatrics Society. 2005;53:1017–1022. doi: 10.1111/j.1532-5415.2005.53322.x. [DOI] [PubMed] [Google Scholar]
- 36.Borson S, Loebel P, Kitchell M, et al. Psychiatric assessments of nursing home residents under OBRA-87: Should PASARR be reformed? Journal of the American Geriatrics Society. 1997;45:1173–1181. doi: 10.1111/j.1532-5415.1997.tb03766.x. [DOI] [PubMed] [Google Scholar]
- 37.Bazelon Center . The Impact of PASSAR. Bazelon Center for Mental Health Law; Washington, D.C.: 1996. [Google Scholar]
- 38.Snowden M, Roy-Byrne P. Mental illness and nursing home reform: OBRA-87 ten years later. Psychiatric Services. 1998;49:229–233. doi: 10.1176/ps.49.2.229. [DOI] [PubMed] [Google Scholar]
- 39.Shea D, Russo PA, Smyer MA. Use of mental health services by persons with a mental illness in nursing facilities: Initial impacts of OBRA87. Journal of Ageing and Health. 2000;12:560–578. doi: 10.1177/089826430001200406. [DOI] [PubMed] [Google Scholar]
- 40.Castle NG. Deficiency citations for mental health care in nursing homes. Administration and Policy in Mental Health. 2001;29:157–171. doi: 10.1023/a:1014340731399. [DOI] [PubMed] [Google Scholar]
- 41.Castle NG, Myers S. Mental health care deficiency citations in nursing homes and caregiver staffing. Administration and Policy in Mental Health. 2006;33:215–225. doi: 10.1007/s10488-006-0038-2. [DOI] [PubMed] [Google Scholar]
- 42.Mor V, Angelilli J, Jones RN, et al. Inter-rater reliability of nursing home quality indicators in the U.S. BMC Health Services Research. 2003;3 doi: 10.1186/1472-6963-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bagchi A, Verdier J, Simon SE. Academy Health Annual Research Meeting. Washington, D.C.: 2008. How many nursing home residents live with a mental illness? [DOI] [PubMed] [Google Scholar]