Abstract
Background
Subjective memory complaints (SMC) are common among elderly patients and little is know about the association between SMC and health care utilisation. Thus, the aim of this study was to investigate health care utilisation during a three-year follow-up among elderly patients consulting their general practitioner and reporting subjective memory complaints (SMC).
Methods
This study was conducted as a prospective cohort survey in general practice with three-year follow-up. Selected health care utilisation or costs relative to SMC adjusted for potential confounders were analyzed in a two-part model where the incidence of use of a selected health care service were analyzed separately from the quantity of use for those that use the service. The former analyzed in a Poisson regression approach, the latter in a generalized linear regression model.
Results
A total 758 non-nursing home residents aged 65 years and older consulted their GP in October and November 2002 and participated in the present study. The adjusted probability of nursing home placement was significantly increased in subjects with SMC relative to subjects without SMC (RR = 2.3). More generally, SMC was associated with an increase in the cost of selected health care utilisation of 60% over three years (p = 0.003).
Conclusion
The data of this study indicated that in an elderly primary care population the presence of SMC increased the cost of health care utilisation by 60% over three years. Thus, inquiry into SMC may contribute to a risk profile assessment of elderly patients and may identify patients with an increased use of health care services.
Background
In studies of older patients, the reported prevalence of subjective memory complaints (SMC) shows a huge variation with figures ranging from 10-56% [1,2]. The large variation may be explained by sample selection or by the methods applied for assessing SMC [1]. Studies have consistently associated SMC with depression [2-4], as well as personality traits [5], high age, low education and female gender [1]. A Danish study indicated that these patients rarely share their perception of SMC with their General Practitioner (GP) spontaneously [6], even though SMC may identify frail patients and inquiry into SMC may easily be implemented in a busy GP routine consultation.
In some studies, association has been found between memory complaints and cognitive impairment on testing, even after adjustment for depressive symptoms [7,8]. However, longitudinal studies assessing the value of SMC in predicting dementia or cognitive decline have shown varying results [9-16]. Thus, the nature of SMC is complex [17].
In a study from 1999 among 8775 non-institutionalized persons aged 65 or more, a single question about health strongly predicted subsequent health care utilisation after a year [18]. Other research suggests that patients with mental health conditions use general medical services at a higher rate than those without mental health conditions [19-21]. Furthermore, dementia has been associated with increased health care utilisation in several studies [22,23]. In our recent study, SMC was associated with an increased probability for nursing home placement over 4 years following the assessment [24]. However, we did not identify any other studies addressing the association between the presence of SMC and health care utilisation. Thus, the aim of the present prospective study was to investigate health care utilisation during a three-year follow-up among elderly patients with and without SMC consulting their general practitioner.
Methods
Study Population
All 17 practices comprising a total of 24 GPs in the central district of the municipality of Copenhagen, Denmark, participated in this study. A total of 40.865 patients were listed and 2.934 were 65 or older. Patients' aged 65 and older consulting their GP, regardless of reason for the encounter, were asked to participate in the study and received information both verbally and written. All participants signed an informed consent declaration and were not offered a refund. Patients not able to speak or read Danish, patients living in a nursing home, and patients with severe acute or terminal illness, or specialist-diagnosed patients with dementia were excluded. Non-participants were defined as those who were not excluded because of the exclusion criteria, but refused to participate. The participants were enrolled during October and November 2002.
Outcome
End-point variables were GP related contacts, out-of-hour services, hospitalization and nursing home placement within a three-year period from enrolment, and a cumulated value of these services.
Measurements
In brief, the examination contained:
1) A self-administered participant questionnaire concerning aspects of memory and sociodemographics. Information on SMC was obtained from the following item: "How would you judge your memory?" Theresponse categories were: "excellent", "good", "less good", "poor", or "miserable". Patients rating their memory as "less good", "poor" or "miserable" were classified as patients with SMC, while patients rating their memory as "excellent" or "good" were defined as patients without SMC.
2) A self-administered quality of life assessment. The patients completed the Danish Validated Version of Euro-Qol-5D. Euro-Qol-5D is a standardised instrument for use as a measure of health outcome and measures five dimensions - mobility, self-care, usual activities, pain/discomfort, and anxiety/depression - each by three levels of severity [25]. The anxiety/depression dimension was used as a proxy for depression.
3) A GP- or nurse- administered Mini Mental State Exermination (MMSE). The MMSE, a widely distributed test recommended in GP guidelines as a cognitive screening test, was completed after the completion of the GP questionnaire [26]. The MMSE score ranges from 0-30; a score lower than 24 was taken as indicative of cognitive impairment.
Registry data
In Denmark, much health information is collected in national registers based on a unique personal identification number allocated to each inhabitant [27]. Information concerning incident deaths, hospital contacts and GP consultations were retrieved from the central national databases by the statistical department of the Danish National Board of Health at the end of 2007. The municipality of Copenhagen provided information concerning nursing home placement at the end of 2006.
In this study the following outcomes were investigated in the three-year period from January 1st 2003 until 31st December 2005:
1) Practice consultations (number of consultations)
2) Home visit consultations by GP (number of visits)
3) GP out-of-hours contacts (number of contacts)
4) Hospital admission (days in hospital, not as out-patient)
5) Out-patient stay (days in outpatient clinic)
6) Emergency room consultations (number of visits)
7) Nursing home placement (days in institution).
Health care utilisation was defined as the sum of the number of services or time (days) of stay over the three-year follow-up period; or a valuation based on the prices in Table 1. For those, who had died (and thereby did not use health care services during all three years), the nominal outcome was multiplied with the inverse of the proportion of the three years the subject was alive. Annualized outcomes were constructed by dividing the three-year outcomes by three.
Table 1.
Valuation of selected health care services
| Service | Unit | Value1 | Source |
| Practice consultations | 1 consultation | € 14,39 | Danish health insurance register (SSR) |
| Visits by GP | 1 visit | € 23,81 | Danish health insurance register (SSR) |
| Hospital stay (not as outpatient) | 1 admission day | € 470,84 | Journal of the Danish Medical Association 2005; 167 (07): 807 |
| Outpatient stay | 1 admission day | € 187,39 | The National Board of Health (drg.dk) |
| Out-of-hours contacts | 1 contact | € 14,66 | Danish health insurance register (SSR) |
| Emergency | 1 visit | € 105,74 | The National Board of Health (drg.dk) |
| Nursing home | 1 admission day | € 127,80 | Journal of the Danish Medical Association 2005; 167 (07): 807 |
12004 prices in DKK converted to EUR using the july 1st 2004 spot rate DKK743.35 = EUR100 (source: Danish national bank http://www.nationalbanken.dk)
Statistical analysis
Differences in characteristics and health care utilisation between participants with and without SMC were tested by chi-squared tests. A total cost for the health care utilisation was calculated using the valuation in Table 1; the difference in this cost between participants with and without SMC was analyzed with a Kruskal-Wallis non-parametric test. Differences in total cost between subgroups of the participants were tested by the F-test of the regression parameter(s) corresponding to the characteristic classifying the subgroups in a linear regression on total cost, additionally adjusted for SMC. These tests evaluated the effect of the characteristic on the total cost beyond the part of the effect that was mediated by SMC.
Multivariate analysis of health care utilisation followed a two-part model where the incidence of use (ever used) of a selected health care service was analyzed separately from the quantity of use for those that use the service [28]. The incidence was analyzed in a Poisson regression approach [29] so that the regression parameters were equivalent to the log of the relative risk (RR) of using the service ever in the study period. For the participants that use the service (or have cost>0) the quantity of use was analyzed in a generalized linear model using a Gamma distribution and a logarithmic link function; the parameters from this model were interpreted as the log of a (multiplicative) factor how much more the service was used compared to a baseline class. A combined (multiplicative) effect of having SMC compared to not having SMC was straightforwardly calculated by multiplying the RR from the first part and the factor from the second part. Statistical significance was assessed at a 5% level. We adjusted for multiple testing by the method of Benjamini-Hochberg in the final multivariate analysis [30].
Ethics
The Scientific Ethical Committee for Copenhagen and Frederiksberg Municipalities evaluated the project. The Danish Data Protection Agency, the Danish College of General Practitioners Study Committee as well as The National Board of Health approved the project.
Results
The final cohort consisted of 775 non-nursing home residents of which 758 filled out the SMC item. Figure 1 shows the trial flow. The average age of participants at baseline was 74.8 of whom 38.6% were males; average MMSE was 28.2 (range: 16-30). According to our definition 177 (23%) had SMC at baseline. Non-participants were more likely to be males (OR = 1.4) and were, according to the GP, less likely to complain about memory problems, (OR = 1.8). All participants were followed up until the end of 2005 and none were lost to follow-up.
Figure 1.
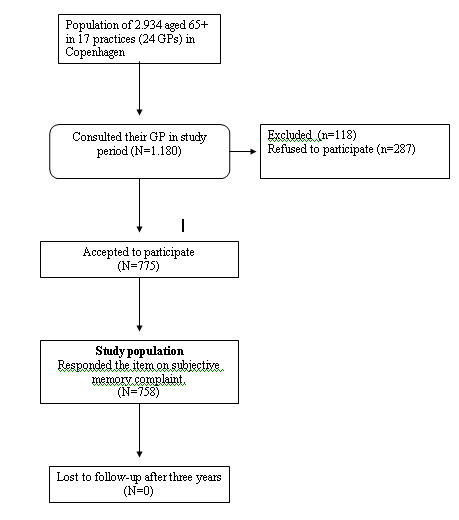
Flowchart of Study population.
During the study period 88 (11.6%) died and 50 (6.6%) were admitted to nursing homes. A total of 701 (92.5%) had at least one GP consultation and 432 (60.0%) have at least one hospital admission during the study period. Furthermore, SMC is not seen to correlate with MMSE (Table 2). Valuations of selected health care services are shown in Table 1.
Table 2.
Baseline characteristics and health care utilisation of the study participants (n = 758) by Subjective Memory Complaints (SMC)
| SMC | |||||||
|
No (n = 581) |
Yes (n = 177) |
||||||
| n | % | n | % | Sign. | Missing | ||
| Death | no | 517 | 89,0 | 153 | 86,4 | ||
| yes | 64 | 11,0 | 24 | 13,6 | |||
| MMSE | ≥ 24 | 555 | 95,5 | 165 | 93,2 | ||
| < 24 | 26 | 4,5 | 12 | 6,8 | |||
| Age | 60 - 74 | 318 | 54,7 | 86 | 48,6 | ||
| 75 - 84 | 207 | 35,6 | 68 | 38,4 | |||
| 85+ | 56 | 9,6 | 23 | 13,0 | |||
| Sex | male | 233 | 40,1 | 61 | 34,5 | ||
| female | 348 | 59,9 | 116 | 65,5 | |||
| Living without partner | no | 240 | 41,4 | 60 | 34,3 | 3 | |
| yes | 340 | 58,6 | 115 | 65,7 | |||
| Education | < 8 years | 226 | 38,9 | 69 | 39,0 | ||
| > 8 years | 355 | 61,1 | 108 | 61,0 | |||
| Home care | no | 473 | 81,7 | 126 | 72,0 | *** | 4 |
| yes | 106 | 18,3 | 49 | 28,0 | |||
| Mobility1 | no problems | 384 | 67,3 | 90 | 52,0 | *** | 14 |
| some problems | 187 | 32,7 | 83 | 48,0 | |||
| Self-care1 | no problems | 539 | 94,7 | 158 | 90,8 | 15 | |
| some problems | 30 | 5,3 | 16 | 9,2 | |||
| Usual activities1 | no problems | 412 | 72,5 | 84 | 48,6 | ||
| some problems | 145 | 25,5 | 84 | 48,6 | *** | 17 | |
| severe problems | 11 | 1,9 | 5 | 2,9 | |||
| Pain/discomfort1 | no | 216 | 38,4 | 45 | 25,9 | ||
| moderate | 323 | 57,4 | 111 | 63,8 | *** | 21 | |
| extreme | 24 | 4,3 | 18 | 10,3 | |||
| Anxiety/depression1 | no | 442 | 77,8 | 98 | 57,0 | ||
| moderate | 115 | 20,2 | 71 | 41,3 | *** | 18 | |
| extreme | 11 | 1,9 | 3 | 1,7 | |||
| Health Care Utilization | |||||||
| Practice consultations2 | no | 41 | 7,1 | 16 | 9,0 | ||
| yes | 540 | 92,9 | 161 | 91,0 | |||
| Visits by GP2 | no | 422 | 72,6 | 117 | 66,1 | ||
| yes | 159 | 27,4 | 60 | 33,9 | |||
| Hospital stay (no outpatient)2 | no | 259 | 44,6 | 67 | 37,9 | ||
| yes | 322 | 55,4 | 110 | 62,1 | |||
| Outpatient stay2 | no | 165 | 28,4 | 34 | 19,2 | * | |
| yes | 416 | 71,6 | 143 | 80,8 | |||
| Out-of-hours contact2 | no | 548 | 94,3 | 170 | 96,0 | ||
| yes | 33 | 5,7 | 7 | 4,0 | |||
| Emergency2 | no | 345 | 59,4 | 82 | 46,3 | ** | |
| yes | 236 | 40,6 | 95 | 53,7 | |||
| Nursing home2 | no | 554 | 95,4 | 154 | 87,0 | *** | |
| yes | 27 | 4,6 | 23 | 13,0 | |||
* significant at 5% level ** significant at 1% level *** significant at 0.1% level, 1based on Euro-Qol-5D, for mobility and self-care the third category did not appear because of the method of data collection, 2incidence in the period 2003-2005.
Annualized cost (in EUR) of health care utilisation by SMC and participant characteristics is shown in Table 3. Lower MMSE scores, increased age, lower education, home care and lower physical activity increased the cost of health care utilisation. The differences in health care utilisation and costs attributable to SMC, i.e. adjusted for the characteristics listed in Table 3, are shown in Table 4. The presence of SMC significantly increased the probability of nursing home placement (RR = 2.3). More generally, SMC was significantly associated with an increase in health care costs for the combined selected services over the three years of follow-up by 60%. When the cost of nursing home admission is omitted from the total cost analysis, SMC is associated only with a non-significant 23% increase
Table 3.
Annualised cost (EUR) of health care utilisation by Subjective Memory Complaints (SMC) and participant characteristics
| SMC | ||||||||
| No (n = 581) | Yes (n = 177) | |||||||
| Median | IQR | Median | IQR | Sign.1 | ||||
| Total cost (EUR) | 838 | 192 | 3389 | 1577 | 597 | 9894 | ***2 | |
| MMSE | ≥24 | 831 | 192 | 3209 | 1457 | 548 | 7620 | ** |
| < 24 | 4572 | 183 | 13033 | 9888 | 2597 | 22082 | ||
| Age | 60 - 74 | 566 | 178 | 2170 | 993 | 274 | 1659 | |
| 75 - 84 | 1143 | 226 | 4438 | 3321 | 1076 | 14743 | *** | |
| 85+ | 3277 | 494 | 24366 | 14609 | 1713 | 27545 | ||
| Sex | male | 1036 | 202 | 3637 | 1190 | 322 | 3302 | |
| female | 794 | 187 | 3360 | 2187 | 733 | 13738 | ||
| Living without partner | no | 815 | 154 | 2601 | 1225 | 541 | 4135 | |
| yes | 842 | 219 | 3931 | 2125 | 695 | 14770 | ||
| Education | < 8 years | 944 | 185 | 4151 | 2998 | 528 | 17280 | * |
| > 8 years | 831 | 197 | 2750 | 1383 | 612 | 6291 | ||
| Home care | no | 660 | 182 | 2551 | 1069 | 307 | 2998 | *** |
| yes | 2642 | 682 | 9065 | 14609 | 3329 | 23801 | ||
| Mobility | no problems | 613 | 163 | 2327 | 1177 | 280 | 4985 | *** |
| some problems | 1778 | 313 | 8509 | 2883 | 958 | 14770 | ||
| Self-care | no problems | 832 | 192 | 3294 | 1431 | 548 | 6755 | ** |
| some problems | 2027 | 288 | 8896 | 13416 | 2788 | 20493 | ||
| Usual activities | no problems | 605 | 163 | 2380 | 1194 | 301 | 4160 | |
| some problems | 1891 | 433 | 6497 | 2556 | 767 | 13791 | ||
| severe problems | 1531 | 178 | 14788 | 3615 | 3248 | 23152 | *** | |
| Pain/discomfort | no | 594 | 133 | 2227 | 1811 | 695 | 14609 | |
| moderate | 1063 | 222 | 4266 | 1510 | 543 | 6161 | ||
| extreme | 1877 | 324 | 6137 | 2669 | 1050 | 12867 | ||
| Anxiety/depression | no | 794 | 187 | 3182 | 1494 | 548 | 8905 | |
| moderate | 1036 | 226 | 3595 | 1577 | 682 | 9894 | ||
| extreme | 13606 | 887 | 17944 | 12512 | 7620 | 30547 | ||
*significant at 5% level ** significant at 1% level *** significant at 0.1% level
1Significance of the regression parameter of the corresponding participant characteristic in a linear regression on total cost, adjusted for SMC
2Wilcoxon non-parametric test
Table 4.
Selected health care utilisation and costs in subjects with Subjective Memory Complaints (SMC) relative to patients without SMC1
| The RR of any use of the corresponding service at all | Factor how much more people with SMC use the service | Combined effect | |||||||
| Service | RR | 95% CI | p-value2 | Factor | 95% CI | p-value2 | |||
| GP contacts | |||||||||
| Practice consultations | 0,976 | 0,922 | 1,032 | 0,3924 | 0,988 | 0,866 | 1,126 | 0,8559 | 0,964 |
| Visits by GP | 1,116 | 0,876 | 1,421 | 0,3863 | 0,967 | 0,717 | 1,304 | 0,8255 | 1,079 |
| GP contacts (cost) | 0,970 | 0,920 | 1,023 | 0,2610 | 1,001 | 0,883 | 1,135 | 0,9830 | 0,972 |
| Hospital stay | |||||||||
| Hospital stay (not as outpatient, days) | 1,052 | 0,911 | 1,216 | 0,4953 | 1,189 | 0,895 | 1,582 | 0,2282 | 1,252 |
| Outpatient stay (days) | 1,111 | 1,010 | 1,221 | 0,0344 | 1,082 | 0,875 | 1,338 | 0,4663 | 1,202 |
| Hospital stay (cost) | 1,061 | 0,978 | 1,151 | 0,1611 | 1,178 | 0,920 | 1,509 | 0,1896 | 1,250 |
| Out-of-hours services | |||||||||
| Out-of-hours GP contacts | 0,575 | 0,237 | 1,398 | 0,1686 | 1,437 | 1,092 | 1,891 | 0,0116 | 0,827 |
| Emergency (visits) | 1,209 | 1,007 | 1,452 | 0,0512 | 1,073 | 0,916 | 1,256 | 0,3828 | 1,297 |
| Out-of-hours services (cost) | 1,121 | 0,939 | 1,340 | 0,2183 | 1,172 | 0,977 | 1,405 | 0,0858 | 1,314 |
| Nursing home | |||||||||
| Nursing home (days) | 2,296 | 1,357 | 3,886 | 0,0075 | 0,922 | 0,686 | 1,238 | 0,5900 | 2,117 |
| Nursing home (cost) | 2,296 | 1,357 | 3,886 | 0,0075 | 0,922 | 0,686 | 1,238 | 0,5900 | 2,117 |
| The above combined (cost) | 0,990 | 0,961 | 1,020 | 0,5070 | 1,615 | 1,234 | 2,114 | 0,0003 | 1,599 |
1All analyses adjusted for the participant characteristics presented in Table 3
2Due to multiple testing the level of significance is set to 0.0081
Discussion
To our knowledge, this is the first study to demonstrate that in elderly patients SMC was attributable to an increase in cost by 60% over three years for selected health care services. Specifically, SMC increased the probability of nursing home placement. Much of the excess cost in the SMC group seems to be explained by the higher frequency of nursing home admission.
SMC is a commonly reported symptom in the elderly [1,2]. In this study we adjusted for commonly known confounders e.g. depression and cognitive performance, and the result indicated that the increase in health care utilisation attributed to SMC was substantial. The tendency, that nursing home placement was increased has been reported previously using data from this study. The increased health care utilisation may not solely be explained by nursing home admission. Tendencies of increased use of out-patient clinic admissions and out-of-hour services can be observed. In contrast, the use of GP daytime consultations and acute hospital admittance were not increased.
The reported effect of SMC was beyond various other potential confounders. It is well-known that the presence of dementia in general is associated with an increased health care utilisation [31]. This is in accordance with this study, where our item indicating that significant cognitive impairment (defined as MMSE less than 24) was an independent predictor for nursing home placement. Also, depression in old age has also consistently been associated with an increased health care costs, even after controlling for chronic medical co-morbidity [32]. Our study found that age, but not depressive symptoms were associated with an increased health care utilisation. Furthermore, low education increased health care utilisation. The absence of correlation between SMC and cognitive functioning (MMSE) stresses their different psychometric properties. We assume that SMC measures a global functioning in elderly patients. In Table 2 it can be seen that there is no notable difference in mortality between the subjects with and without SMC. Hence, the difference in health care utilisation and costs cannot be attributed to the high end-of-life utilisation and costs that are generally observed.
The mechanism by which SMC leads to increased health care utilisation is, in our view, not a direct causative relation. However, we see a statistical association between SMC and health care utilisation as residual confounding, i.e. there are certain factors - possibly unknown or immeasurable - beyond the covariates that are used in the analyses, that cause the subject to have memory complaints and cause increased health care utilisation.
The sampling of the participants reflects the population in which the GP has an opportunity to ask questions about SMC. Thus, we deliberately designed the study to include a patient sample, which reflects daily clinical practice. The nation-wide databases used in order to evaluate our main outcomes are regarded as highly valid. Thus, we believe that our findings are valid.
The statistical analysis was done in a two-part model according to recommendations [28]. Data tend to conform to the analytic assumptions for these models, and the models can be used to gain insight in the process of health care utilisation. The decision to have any use at all of a certain service is most likely made by the person and so is related primarily to personal characteristics, while the cost and frequency per user may be more related to characteristics of the health care system.
Several limitations must be addressed. This study had some selection biases at baseline, which may decrease generalizability. Only elderly persons who consulted their GP for whatever reason were included, and they may be more vulnerable than elderly persons in the general population. We did not have access to databases regarding medication, which would have been relevant to evaluate. Likewise, we did not obtain information about medical diagnosis in the participants, as diagnostic criteria are not systematically implemented in general practice in Denmark, and we wanted the study to reflect current standards. Participants who had already been diagnosed with dementia by a specialist were excluded from the study, which is reflected by the high average MMSE in our study population. A MMSE score less than 24 has been widely used as an indication of the presence of cognitive impairment in population based studies [33]. However, epidemiological research has shown that MMSE scores are affected by age, education, and cultural background [33] and MMSE is not sufficient to diagnose dementia. In our study we used the depression item in the Euro-Qol-5D to identify patients with self reported anxiety and depression. These patients may not fulfill international criteria for anxiety and depression. However, this item may serve as indicator for affective symptoms.
There is a lack of consensus concerning the assessment of SMC. Some studies have assessed the presence of SMC by a single item, others by several items. In this study, a single item was used to assess SMC. This item did not allow us to know whether the patient was calibrating the response by comparing to former functioning or to the functioning of others. Notably, our SMC item did not distinguish between short-term and long-term memory loss. We recommend that future studies give more attention to this specific aspect and also include informant reports on memory.
Conclusion
The data suggest that in an elderly primary care population SMC is associated with an increased health care utilisation by 60%, primarily because of increased nursing home placement. Therefore, the result of this study indicates that GPs may identify elderly patients with an increased probability of subsequent health care utilisation by routinely inquiring about memory problems.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
FBW conceived the study concept, design, funding, data analysis, interpretation, and wrote the first draft of the manuscript. VS participated in the data analysis, interpretation, and manuscript preparation. GW participated in the study concept, design, data analysis, interpretation, and manuscript preparation. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
This work was supported by a General Practitioners' Foundation for Education and Development Grant (Grant nr: R56-A369-B186). The sponsor did not contribute to any part of the study or the preparation of the manuscript.
Contributor Information
Frans Boch Waldorff, Email: fbw@gpmed.ku.dk.
Volkert Siersma, Email: siersma@sund.ku.dk.
Gunhild Waldemar, Email: gunhild.waldemar@rh.regionh.dk.
References
- Jonker C, Geerlings MI, Schmand B. Are memory complaints predictive for dementia? A review of clinical and population-based studies. Int J Geriatr Psychiatry. 2000;15:983–991. doi: 10.1002/1099-1166(200011)15:11<983::AID-GPS238>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- Jungwirth S, Fischer P, Weissgram S, Kirchmeyr W, Bauer P, Tragl KH. Subjective memory complaints and objective memory impairment in the Vienna-Transdanube aging community. J Am Geriatr Soc. 2004;52:263–268. doi: 10.1111/j.1532-5415.2004.52066.x. [DOI] [PubMed] [Google Scholar]
- Bassett SS, Folstein MF. Memory complaint, memory performance, and psychiatric diagnosis: a community study. J Geriatr Psychiatry Neurol. 1993;6:105–111. doi: 10.1177/089198879300600207. [DOI] [PubMed] [Google Scholar]
- Kahn RL, Zarit SH, Hilbert NM, Niederehe G. Memory complaint and impairment in the aged. The effect of depression and altered brain function. Arch Gen Psychiatry. 1975;32:1569–1573. doi: 10.1001/archpsyc.1975.01760300107009. [DOI] [PubMed] [Google Scholar]
- Hanninen T, Reinikainen KJ, Helkala EL, Koivisto K, Mykkanen L, Laakso M, Pyorala K, Riekkinen PJ. Subjective memory complaints and personality traits in normal elderly subjects. J Am Geriatr Soc. 1994;42:1–4. doi: 10.1111/j.1532-5415.1994.tb06064.x. [DOI] [PubMed] [Google Scholar]
- Waldorff FB, Rishoj S, Waldemar G. If you don't ask (about memory), they probably won't tell. J Fam Pract. 2008;57:41–44. [PubMed] [Google Scholar]
- Gagnon M, Dartigues JF, Mazaux JM, Dequae L, Letenneur L, Giroire JM, Barberger-Gateau P. Self-reported memory complaints and memory performance in elderly French community residents: results of the PAQUID Research Program. Neuroepidemiology. 1994;13:145–154. doi: 10.1159/000110373. [DOI] [PubMed] [Google Scholar]
- Jonker C, Launer LJ, Hooijer C, Lindeboom J. Memory complaints and memory impairment in older individuals. J Am Geriatr Soc. 1996;44:44–49. doi: 10.1111/j.1532-5415.1996.tb05636.x. [DOI] [PubMed] [Google Scholar]
- Schmand B, Jonker C, Geerlings MI, Lindeboom J. Subjective memory complaints in the elderly: depressive symptoms and future dementia. Br J Psychiatry. 1997;171:373–376. doi: 10.1192/bjp.171.4.373. [DOI] [PubMed] [Google Scholar]
- Schofield PW, Marder K, Dooneief G, Jacobs DM, Sano M, Stern Y. Association of subjective memory complaints with subsequent cognitive decline in community-dwelling elderly individuals with baseline cognitive impairment. Am J Psychiatry. 1997;154:609–615. doi: 10.1176/ajp.154.5.609. [DOI] [PubMed] [Google Scholar]
- Wang L, van BG, Crane PK, Kukull WA, Bowen JD, McCormick WC, Larson EB. Subjective memory deterioration and future dementia in people aged 65 and older. J Am Geriatr Soc. 2004;52:2045–2051. doi: 10.1111/j.1532-5415.2004.52568.x. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Christensen H, Korten AE, Jacomb PA, Henderson AS. Memory complaints as a precursor of memory impairment in older people: a longitudinal analysis over 7-8 years. Psychol Med. 2001;31:441–449. [PubMed] [Google Scholar]
- Smith GE, Petersen RC, Ivnik RJ, Malec JF, Tangalos EG. Subjective memory complaints, psychological distress, and longitudinal change in objective memory performance. Psychol Aging. 1996;11:272–279. doi: 10.1037/0882-7974.11.2.272. [DOI] [PubMed] [Google Scholar]
- Wang PN, Wang SJ, Fuh JL, Teng EL, Liu CY, Lin CH, Shyu HY, Lu SR, Chen CC, Liu HC. Subjective memory complaint in relation to cognitive performance and depression: a longitudinal study of a rural Chinese population. J Am Geriatr Soc. 2000;48:295–299. doi: 10.1111/j.1532-5415.2000.tb02649.x. [DOI] [PubMed] [Google Scholar]
- Palmer K, Backman L, Winblad B, Fratiglioni L. Detection of Alzheimer's disease and dementia in the preclinical phase: population based cohort study. BMJ. 2003;326:245. doi: 10.1136/bmj.326.7383.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glodzik-Sobanska L, Reisberg B, De SS, Babb JS, Pirraglia E, Rich KE, Brys M, de Leon MJ. Subjective memory complaints: presence, severity and future outcome in normal older subjects. Dement Geriatr Cogn Disord. 2007;24:177–184. doi: 10.1159/000105604. [DOI] [PubMed] [Google Scholar]
- Reid LM, Maclullich AM. Subjective memory complaints and cognitive impairment in older people. Dement Geriatr Cogn Disord. 2006;22:471–485. doi: 10.1159/000096295. [DOI] [PubMed] [Google Scholar]
- Bierman AS, Bubolz TA, Fisher ES, Wasson JH. How well does a single question about health predict the financial health of Medicare managed care plans? Eff Clin Pract. 1999;2:56–62. [PubMed] [Google Scholar]
- Fogarty CT, Sharma S, Chetty VK, Culpepper L. Mental health conditions are associated with increased health care utilization among urban family medicine patients. J Am Board Fam Med. 2008;21:398–407. doi: 10.3122/jabfm.2008.05.070082. [DOI] [PubMed] [Google Scholar]
- Thomas MR, Waxmonsky JA, Gabow PA, Flanders-McGinnis G, Socherman R, Rost K. Prevalence of psychiatric disorders and costs of care among adult enrollees in a Medicaid HMO. Psychiatr Serv. 2005;56:1394–1401. doi: 10.1176/appi.ps.56.11.1394. [DOI] [PubMed] [Google Scholar]
- Salsberry PJ, Chipps E, Kennedy C. Use of general medical services among Medicaid patients with severe and persistent mental illness. Psychiatr Serv. 2005;56:458–462. doi: 10.1176/appi.ps.56.4.458. [DOI] [PubMed] [Google Scholar]
- Hill JW, Futterman R, Duttagupta S, Mastey V, Lloyd JR, Fillit H. Alzheimer's disease and related dementias increase costs of comorbidities in managed Medicare. Neurology. 2002;58:62–70. doi: 10.1212/wnl.58.1.62. [DOI] [PubMed] [Google Scholar]
- Fillit H, Hill JW, Futterman R. Health care utilization and costs of Alzheimer's disease: the role of co-morbid conditions, disease stage, and pharmacotherapy. Fam Med. 2002;34:528–535. [PubMed] [Google Scholar]
- Waldorff FB, Siersma V, Waldemar G. Association between subjective memory complaints and nursing home placement: a four-year follow-up. Int J Geriatr Psychiatry. 2009;24:602–609. doi: 10.1002/gps.2163. [DOI] [PubMed] [Google Scholar]
- Rabin R, de CF. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Olivarius NF, Hollnagel H, Krasnik A, Pedersen PA, Thorsen H. The Danish National Health Service Register. A tool for primary health care research. Dan Med Bull. 1997;44:449–453. [PubMed] [Google Scholar]
- Diehr P, Yanez D, Ash A, Hornbrook M, Lin DY. Methods for analyzing health care utilization and costs. Annu Rev Public Health. 1999;20:125–144. doi: 10.1146/annurev.publhealth.20.1.125. [DOI] [PubMed] [Google Scholar]
- Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling for the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B. 1995;57:289–300. [Google Scholar]
- Kronborg AC, Sogaard J, Hansen E, Kragh-Sorensen A, Hastrup L, Andersen J, Andersen K, Lolk A, Nielsen H, Kragh-Sorensen P. The cost of dementia in Denmark: the Odense Study. Dement Geriatr Cogn Disord. 1999;10:295–304. doi: 10.1159/000017135. [DOI] [PubMed] [Google Scholar]
- Luppa M, Heinrich S, Matschinger H, Sandholzer H, Angermeyer MC, Konig HH, Riedel-Heller SG. Direct costs associated with depression in old age in Germany. J Affect Disord. 2008;105:195–204. doi: 10.1016/j.jad.2007.05.008. [DOI] [PubMed] [Google Scholar]
- Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]


