Abstract
Background
Although numerous studies have examined the association of area socioeconomic status (SES) and cancer screening after controlling for individual SES, findings have been inconsistent. A systematic review of existing studies is timely in order to identify conceptual and methodologic limitations and to provide a basis for future research directions and policy.
Objective
The objectives were to: 1) describe the study designs, constructs, methods, and measures; 2) describe the independent association of area SES and cancer screening; and 3) identify neglected areas of research.
Methods
We searched 6 electronic databases and manually searched cited and citing articles. Eligible studies were published before 2008 in peer-reviewed journals in English, represented primary data on individuals aged ≥18 years from developed countries, and measured the association of area and individual SES with breast, cervical, or colorectal cancer screening.
Results
Of 19 eligible studies, most measured breast cancer screening. Studies varied widely in research design, definitions and measures of SES, cancer screening behaviors, and covariates. Eight employed multilevel logistic regression, the remainder analyzed data with standard single level logistic regression. The majority measured 1 or 2 indicators of area and individual SES; common indicators at both levels were poverty, income, and education. There was no consistent pattern in the association between area SES and cancer screening.
Discussion
The gaps and conceptual and methodologic heterogeneity in the literature to date limit definitive conclusions about an underlying association between area SES and cancer screening. We identify five areas of research deserving greater attention in the literature.
Keywords: Cancer Screening, Neighborhoods, Socioeconomic Status, Multilevel Research
Introduction
Cancer is the second leading cause of death among U.S. adults, accounting for approximately one-fourth of all deaths in recent years (1). Of 1.5 million estimated new cases of cancer in 2009, 24% will be breast, colorectal, and cervical cancers (2), the three cancers for which broad consensus exists for population screening (3, 4). Yet, there remains a gap between actual and ideal rates of routine screening for these cancers in the U.S., particularly for colorectal cancer (CRCS) (5, 6). Low rates are especially troublesome for populations of lower socioeconomic status (SES) because they experience disproportionate cancer incidence and mortality (5, 7, 8).
Socioeconomic status, widely defined as the social and economic standing of an individual within a hierarchically-stratified society, has consistently been associated with cancer screening rates: low-income, less educated and working class populations are less likely to have obtained and maintained cancer screening than their counterparts (6, 8–11). Although widely referred to as “health disparities,” we embrace the principle of distributive justice (12) and its underlying tenet that disparities in health between the advantaged and disadvantaged are unnecessary, unjust, and avoidable (13), by referring to these SES differentials as social inequities in health. The consistent findings regarding cancer inequities have led to numerous programmatic responses, including educational interventions aiming to reduce SES-associated inequities in knowledge and attitudes and publicly-funded programs providing screening to low-income and uninsured individuals (14–17).
SES inequities in cancer incidence, mortality, and screening, have persisted despite decades of research and interventions targeting individuals (7, 18–20). Because cancer screening requires interaction with both healthcare services and the larger environment in which those services exist, those seeking to understand and positively influence these behaviors have increasingly turned to multilevel or contextual frameworks (21–24). These frameworks move beyond the individual and conceptualize health and health behaviors as a product of the dynamic interrelation of multiple levels of influence, including the individual, community, social, and structural. For example, multilevel or “ecosocial” (25) theories, such as neighborhood social disorganization (26) and social capital (27) and those models currently developing in cardiovascular and glycemic disease (28–31) hypothesize about the direct and indirect effects of social and contextual influences as measured by variables such as neighborhood disorder, social cohesiveness, residential mobility, area-level poverty, or the availability of parks and recreational facilities. In contrast, individual-level frameworks conceptualize health behaviors and medical outcomes as products of such individual-level attributes as knowledge, attitudes, or genetics. By facilitating a clearer understanding of the pathways and mechanisms linking geographic areas and health, multilevel frameworks offer the promise of new and innovative interventions and policies to increase cancer screening and reduce cancer-related inequities.
A growing number of studies have used multilevel frameworks to examine the association of area-level SES—the economic, educational, occupational, or class status of a particular area— and cancer screening. Several studies have demonstrated relations between areas characterized as low in SES and a greater likelihood of late- or no- screening, even after controlling for the contribution of individual SES (23, 32–38). Not all of the measured area-based socioeconomic measures (ABSMs) have been significantly associated with screening (23, 33); in other studies, significant associations have become non-significant following adjustment for individual SES (39–41). Moreover, at least one study found no variation in cancer screening at the area-level (42).
Conceptual and methodologic differences in this literature may be responsible for the observed variation in findings. Moreover, these differences may limit comparability across studies, hinder interpretation of observed associations between area-level SES exposures and cancer outcomes, and constrain our ability to develop and test hypotheses about potential mechanisms linking neighborhoods, screening behaviors, and cancer outcomes.
To provide coherence to this emerging and heterogeneous research area, we conducted a systematic review to describe studies of area SES and individual cancer screening behaviors. Specific aims were to: 1) describe the study designs, constructs, methods, and measures; 2) describe the independent association of area socioeconomic status (SES) and cancer screening over and above individual SES; and 3) identify neglected areas of research. While common methodologic practice in the systematic review literature is to pool results from homogenous groups of high quality studies in order to synthesize the literature and draw conclusions regarding the strength of the association of interest using a narrative best evidence synthesis framework (43) or quantitative meta analytic techniques (44) the high degree of observed heterogeneity in these studies precluded our ability to summarize and draw definitive conclusions about the underlying association of interest. We do, however, outline a summary of the tested associations and their outcomes in the literature to date in the results section and leverage both the identified sources of heterogeneity and neglected areas of research as a basis for our discussion, in which we identify the key priority areas needing refinement in the multilevel cancer screening literature.
Methods
Eligibility Criteria
Studies were included if they: 1) were written in English; 2) were published or in-press in a peer-reviewed journal; 3) reported data from a primary study (not a review or editorial); 4) were conducted in developed countries; 5) included participants aged 18 years and older; 6) measured area SES with one or more ABSMs as an independent variable and provided one or more measures of effect; 7) measured cancer screening uptake (cervical, breast, or colorectal) at the individual-level as a dependent variable; and 8) controlled for one or more measures of individual SES in the analysis of ABSM effects. Eligibility criteria were applied hierarchically in the numeric order above. Studies using either multilevel analyses (e.g., hierarchical logistic regression methods that control for the clustering of individuals within geographic areas) or single level analytic methods (e.g., standard logistic regression methods that do not account for the nested structure of the data) were eligible for inclusion.
ABSMs were broadly defined to include compositional (measures of central tendency aggregated from multiple individual-level observations) or contextual (area-level observations) measures of SES within a defined geographic area ranging in size from as large as a state or province to as small as a block group. Individual SES measures were defined as individually-reported characteristics such as social class, occupation, Medicaid status, education, or individual or household income. Cancer screening was defined as tests that are recommended for population-wide screening for breast, cervical, or colorectal cancer (3, 4). Developed countries were those classified as having “high human development” on the United Nations Human Development Index (45).
Citations
We searched six electronic databases that index behavioral and health journals to identify peer-reviewed articles meeting our inclusion criteria published through the year 2007. The databases, the platform, and the dates they began coverage include: Medline (via OVID) 1950, CINAHL (via OVID) 1982, Academic Search Premier (via EBSCO) 1990, Sociological Abstracts (via CSA) 1963, Social Services Abstracts (via CSA) 1980, and PsycINFO (via OVID) 1887.
An informal and brief review of the literature was used to identify preliminary keywords. The keywords fell into 3 broad categories (Appendix A): area (e.g., census tract, metropolitan area), socioeconomic factor (e.g., poverty, deprivation), and cancer screening test (e.g., Pap smear, mammography) and were adapted for each database’s unique thesaurus of subject headings with the assistance of a public health research librarian. The search strategies were pretested and refined in an iterative process in which citations were screened for relevance and for additional keywords and exclusion criteria. The search was modified as necessary to ensure that it captured the sample of eligible articles obtained by the first author through initial literature searches and previous research. The final search strategies include keywords and subject headings specific to each of the electronic databases (Appendix B).
For each eligible article, we searched the article bibliography, entered the citation into the ISI Web of Science database, and contacted first authors to identify additional eligible cited, citing, or new articles. Finally, we searched Proquest Digital Dissertation database and contacted all authors of potentially eligible dissertations to determine whether the dissertation had been recently accepted for publication in a peer reviewed journal.
Screening
We employed a two-step process for screening studies. First, titles and abstracts of all articles were screened by the first author to determine eligibility. Next, for all abstracts meriting further review and for those abstracts in which eligibility was unclear, full texts were reviewed for eligibility. A quality control check was conducted using an independent reviewer (M.S.) who reviewed titles and abstracts of a random sample of 5% (n=38) of the excluded and 50% (n=9) of the included articles. He and the first author disagreed on 2 excluded and 2 included articles. Upon reviewing the full text of these 4 articles, however, the independent reviewer agreed with the first author’s decisions.
Data Extraction and Description
In data extraction, all eligible studies were read and coded by two reviewers: the first author (SLP) and one member of the review panel (the co-authors and an MPH-trained research assistant). A web-based systematic review software program, SRS 4.0 (TrialStat, Ottawa, Canada), was used for data extraction. All codes were checked for interrater reliability by examining the percent agreement (0.92) and kappa statistic (0.82). Discrepancies were resolved by discussion and consensus between the coders.
Consistent with our aims and an earlier review of multilevel studies (46), we identified study characteristics and findings for extraction. For aim 1, we extracted data on the study sample, design, data sources, area-level, method of analysis, and measurement of individual and area SES, cancer screening outcome(s), and covariates. For aim 2, we coded information on the association of ABSMs and cancer screening by extracting data from a maximum of 2 analytic models per dependent variable, including the effect sizes and confidence intervals for the unadjusted (or least adjusted) and the final fully adjusted models, as available. Finally, for aim 3, we evaluate the existing literature and identify neglected areas of research to provide direction and guidance to researchers designing the next generation of multilevel cancer prevention research.
Results
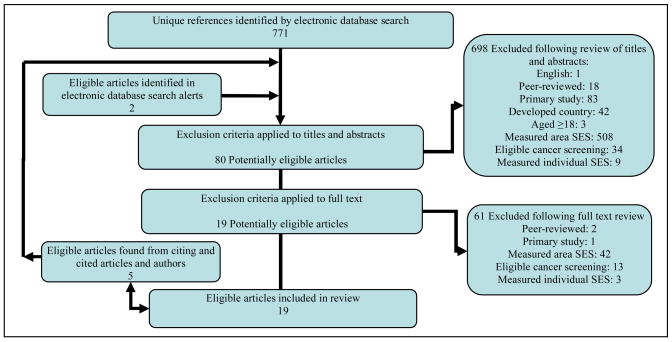
The database search identified 771 potentially relevant unique citations, of which 12 (1.6%) met our inclusion criteria. The additional steps in the search led to the identification of another 7 eligible articles, for a total of 19 (Figure 1). The majority (n=13) of the studies measured breast cancer screening, including mammography, clinical breast exam, and breast self-exam (21, 32–36, 38–40, 47–50) (Table 1). Publication dates ranged from 1998–2007, and the majority of studies were conducted in the U.S. (21, 23, 33–35, 37–40, 42, 47, 48, 50–52). Fifteen studies employed cross-sectional analyses (21, 23, 32, 33, 36–38, 40–42, 47, 49–52). The majority (n=11) analyzed data at a single level using the standard analytic technique of logistic regression (21, 34–38, 41, 47, 48, 50, 51); the remaining 8 articles employed 2-level multilevel logistic regression models (23, 32, 33, 39, 40, 42, 49, 52), with one of these studies also estimating a 3-level model (52) (Table 1).
Figure 1.
Search results and application of eligibility criteria
Table 1.
Summary of eligible studies
| Author, year (Location) | Individual data source (Area data source) | Sample n and description | Definition of positive outcome measure | Area, Level of analysis | Area SES Measures (Measurement) |
|---|---|---|---|---|---|
| Baker, 2004 (US) | 1996 Medical Expenditure Panel Survey; (Area Resource File; year=nr) | Female residents of MSAs, 18–65 (Pap, n=4,600) or 40–75 (mamm n=2,482; CBE n=2,759); no history of breast or cervical cancer; never-screeners ineligible | Recent mamm (≤2 yrs. vs. >2 yrs); Recent CBE (≤2 yrs. vs. >2 yrs); Recent Pap (≤2 yrs. vs. >2 yrs) |
MSA, single | Percent high school graduate (continuous) |
| Benjamins, 2004 (US) | 1996, 1997, 1998 Medical Expenditure Panel Surveys; (Area Resource File; year=nr) | White, black, or Hispanic females (Pap: 18–65, n=13,722) or (Mamm: ≥ 40, n=9325) | Recent mamm (≤2 yrs.); Recent Pap (≤3 yrs.) |
County, single | Percent living in poverty (tertiles) |
| Coughlin, 2006 (US) | 2000, 2002 BRFSS; (2000 Census) | Female ≥18, no hysterectomy; in MSAs with 2000 pop≥1.5 million; n=49,231 | Recent Pap (≤3 yrs.) | County, single | Percent living in poverty (4 cats: 0–4.9; 5–9.9; 10–19.9; ≥ 20); Percent with low education (3 cats: 0–14.9; 15–24.9; ≥25) |
| * Dailey, 2007 (5 cities, Connecticut, US) | 1996–1998 Women presenting for screening mammogram at participating facilities; (1990 Census) | Black and white females 40–79; asymptomatic, no history of breast malignancy, cyst aspiration, or biopsy; n=1,229 | Repeat mamm adherence (women age 40–49: ≥1 repeat mamm ≤ 2 years and 2 months or age ≥ 50 years: ≥ 2 repeat mamms ≤ 2 years and 2 months) | Census tract, single (no 2-level effects found) | Percent in working class jobs; Percent unemployed; Median income; Percent living in poverty; Wealth--percent homes valued ≥ $300K; Percent adults without high school education; Percent persons living in crowded conditions >1 person/room; Percent households without a car; Percent housing units boarded up; Composite SES Index (measuring median household income and percent: working class, below poverty, low education, expensive homes, unemployment) (All measured in race-specific quartiles) |
| Datta, 2006 (US) | 1995 Black Women’s Health Study; (1990 Census) | Black females 21–64; complete data; no hysterectomy, no history of cervical cancer; n=40,009 | Recent Pap (≤2 yrs.) | Census tract and state, 2- & 3-level | Percent living in poverty (4 cats: <5%; 5–9.9%; 10–19.9%; ≥20%) |
| Fukuda, 2005 (Tokyo, Japan) | 2001 Comprehensive Survey of the Living Conditions of People on Health and Welfare; (aggregated responses to survey) | Females 40–64; n=15,224 | Recent breast screen (≤1year; type not specified--CBE is most common in Japan); Recent cervical cancer screen (≤1year; type not specified--Pap is most common in Japan); Recent colorectal screen (≤1year; FOBT is most common in Japan) |
Prefecture, 2-level | Per capita income (continuous, modeled increase of 1 million yen) |
| Koroukian, 2006 (US) | 1999 Medicare Denominator file, Outpatient Standard Analytic File, Part B Physician Supplier File; (1998 Area Resource File) | Medicare beneficiaries for entire year≥65; included only residents of counties with ≥1,000 beneficiaries or 10,000 FFS months of enrolment; n=22,666,112 | Screening FOBT in 1999; Screening sig in 1999; Screening col in 1999; Screening sig or col in 1999 |
County, 2-level | Proportion aged ≥ 65 below poverty level (continuous, models 5 point increase); Proportion adults with high school diploma (continuous, models 5 point increase) |
| Kothari, 2004 (Ontario, Canada) | 1996 National Population Health Survey; (1996 Canadian Census) | Females 50–69; n=4,773 | Ever mamm | Public health agency boundaries, 2-level | Employment-population ratio (continuous); Percent adults without secondary school graduation certificate (continuous) |
| Litaker, 2007 (Ohio, US) | 1998 Ohio Family Health Survey; (1990 Census; Area Resource File, year=nr) | Females 50–69; n=2,231 | Recent mamm (≤1 yr.) | County, 2-level | Proportion below poverty level (continuous, models 5% increase); Proportion female headed households; (continuous, models 5% increase); County located within Appalachia (a federally designated region with concentrated social economic need; dichtomous) |
| O’Malley, 2005 (US) | 2000 Medicare Current Beneficiary Survey and linked claims; (Area Resource File, year=nr) | Black and white uninstutionalized Medicare beneficiaries with usual source of care and physician; ≥65; no end-stage renal disease; no prior colorectal cancer or gastrointestinal symptoms; n=9,985 | CRCS adherence (FOBT ≤ 1 yr. and/or Sig≤5 yrs. and/or Col≤5 yrs.) | County, 2-level | Percent population in poverty (nr) Per capita income (nr) Median family income (nr) |
| Parker, 1998 (California, US) | 1993, 1994 Health Care Financing Administration claims data; (1990 Census) | Female Medicare beneficiaries ≥ 65; n=837,413 | Recent mamm (mamm in 1993 or 1994) | Zip code, single | Percent population ≥ 25 years with college degrees (quintiles) |
| * Rahman, 2003 (Denver Metropolitan Area, Colorado, US) | 1994–1998 prospective mammography facilities and shared with CMAP; (1990 U.S. Census) | Females ≥40; with asymptomatic mammogram at baseline; n=27,778 | Repeat mamm adherence (1. women age ≥ 50 or 40–49 w/family history of breast cancer: ≥ 2 mamms within 1 yr. interval or 2. age 40–49 w/no history: ≥ 2 mamms within 2 yr. interval) | Zip code, single | Median income (6 cats: <$15,000; 15–24,999; 25–34,999; 35–44,999; 45–54,999; ≥ 55,000) |
| * Rosenberg, 2005 (US) | 1995–2001 prospective Black Women’s Health Survey; (2000 U.S. Census) | Black females ≥ 40; cancer free at baseline; completed all 3 follow-ups; n=14,706 | Repeat mamm (mamm use in all in 32 yr. follow-up time periods of study) | Block group, 2-level | Neighborhood SES Index (measuring percent completing college and percent with nonsalary income) (quartiles) |
| * Sabogal, 2001 (California, US) | 1992–1998 retrospective CMS enrollment data base and Medicare Part B billing data; (1990 U.S. Census) | Females ≥ 65, Medicare beneficiaries with continuous coverage; n=515,746 | Repeat mamm 92–98; Regular repeat mamm 92–98 (women who had ≥ 1 mamm and had not skipped 2 years in a row) | Zip code, single | Median household income (quintiles) |
| Schootman, 2005 (US) | 2002 BRFSS; (Area: aggregated data) | ≥50 (CRCS); females ≥40 (CBE and mamm) ≥18 (Pap); N=118,637; MMSAs with ≥ 500 respondents aged ≥ 18+ | Ever mamm; Ever CBE; Ever Pap; Ever FOBT; Ever Col and/or Sig |
MSA/MMSA, 2-level | Percentage living below poverty (continuous; models 5% increase) |
| Siahpush, 2002a (Australia) | 1995 National Health Survey; (1991 Population Census of Australia) | Females ≥40; n=10,179 | Ever mamm; Recent mamm (≤2 yrs. (aged 40–49) or ≤ 1 yr. (aged ≥50)); Ever CBE; Regular CBE (self report “regular” CBE); Regular BSE (self report “regular” BSE) |
Collection district, single | Index of Relative Socioeconomic Disadvantage (IRSD) contains 16 weighted variables: income, education, unemployment, housing characteristics, family structure, occupation, and others; (quintiles) |
| Siahpush, 2002b (Australia) | 1995 National Health Survey; (1991 Population Census of Australia) | Females 18–69; no hysterectomy; n=7,572 | Ever Pap (Ever vs. never); Recent Pap (Pap≤2 yrs.) |
Collection district, single | Index of Relative Socioeconomic Disadvantage (IRSD) contains 16 weighted variables: income, education, unemployment, housing characteristics, family structure, occupation, and others; (quintiles) |
| Thorpe, 2003 (NYC, NY, US) | 2003 New York City Community Health Survey; (area nr) | Uninstitutionalized residents ≥ 50; n=3,606 |
CRCS adherence (FOBT ≤ 1 yr./Sig≤5 yrs./Col ≤10 yrs.); Colonoscopy adherence (Col≤10 yrs.) |
Administratively defined areas, single | Percentage of families ≤200% poverty level (3 cats: low income: ≥ 45%; income: 30–45%; high income: ≤30%) |
| Wells, 1998 (US) | 1990 National Health Interview Survey--NHIS; (1989–1991 aggregated NHIS) | Females: 18–64 (Pap), 35–64 (Mamm, CBE); n=nr |
Ever Mamm; Ever CBE; Ever Pap; |
VSA, single | Median income (4 cats: <$10,000; 10–19,999; 20–29,999; ≥30,000); Percent below poverty (4 cats: 0%; 1–9%; 10–39%; 40–100%); Median education age 25+ (4 cats: <12 y; 12 y; 12–15y; >15 y); Percent unemployed in last 2 weeks (3 cats: <10%; 10–19%; 20–100%) |
All outcome measures are stated in the same direction in the tables for the purpose of consistency; for example, both “recent” and “non-recent” screening outcomes are described as recent screening.
Individual-level data collected via retrospective or prospective study design.
Abbreviations: Nr=not reported; Mamm=mammography; CBE= clinical breast exam; BSE=breast self exam; FOBT=fecal occult blood test; Sig=flexible sigmoidoscopy; Col=colonscopy; CRCS=colorectal cancer screening; Cats=categories; FSS=fee for service; VSA=very small area; MSA= metropolitan statistical area; MMSA=micropolitan or metropolitan statistical area
Data Sources
Eight studies linked self-report individual-level data obtained from surveys to separate administrative sources of area-level data such as the U.S. census (21, 36, 39, 41, 42, 47, 51, 52). Three studies used the same data source for both individual- and area-level data, using aggregated individual-level data to represent area-level exposure (32, 38, 40). Four studies provided details about the geocoding procedures used to link individual- and area- level data such as rates of address matching (35, 39, 48, 52). Eleven included national samples (21, 23, 36, 38–42, 47, 51, 52). In eight of twelve studies reporting racial/ethnic composition, populations consisted of 75% or more non-Hispanic whites (21, 23, 33–35, 40, 42, 50). Although a few studies reported including large (≥25%) (48) or entirely African American populations (39, 52), no studies reported including significant populations (≥25%) of Hispanics.
While inclusion criteria varied, all studies had some age requirement and several (n=4) restricted the sample to individuals with no personal history of cancer (21, 42, 48, 52) or no current cancer or symptomatic screening tests (34, 39). A few studies (n=4) also applied inclusion/exclusion criteria to the area-levels of interest (21, 23, 40, 51) for example, limiting study inclusion to residents living in areas with a population ≥1.5 million.
The dates of data collection for individual- and area-level data were not consistently or clearly reported in five studies (21, 33, 37, 42, 47). Exposure (area-level) data were measured between 1 and 8 years prior to outcomes in 9 studies (23, 33, 34, 36, 41, 48, 50–52) and at the same or approximately the same time as individual outcomes in 6 studies (32, 35, 38–40, 49).
Area-level Data
All studies defined geographic “areas” using some form of country-specific administrative boundaries (e.g., metropolitan statistical areas (MSAs), counties, census tracts, collection districts) or best approximations of administrative areas (38) rather than resident-defined “neighborhoods” or places delineated by other spatial criteria, such as the radius around a respondent’s home. The primary source of area-level data in U.S. studies was the U.S. Census (n=8) (33–35, 39, 48, 50–52) and most U.S. studies analyzed data aggregated within relatively large areas, including MSAs (n=2) (21, 40), counties (n=5) (23, 33, 42, 47, 51), and zip codes (n=3) (34, 35, 50). Fewer studies analyzed data at the census tract level (n=2) (48, 52) (population range: 1500–8000) or block groups level (n=1) (39) (population range: 600–3000).
Area-based Socioeconomic Measures
We identified and coded multiple ABSMs used in these 19 studies, described in detail in Table 1. Most studies used just one (n=12) (21, 32, 34–37, 39–41, 47, 50, 52) or two measures (n=3) (23, 49, 51). The majority of studies (n=12 of 18 reporting) modeled ABSMs as categorical variables (34–39, 41, 47, 48, 50–52). Most studies measured at least one indicator of percent living in poverty (n=10) (23, 33, 37, 38, 40, 42, 47, 48, 51, 52), area income (n=6) (32, 34, 35, 38, 42, 48), or area education (n=7) (21, 23, 38, 48–51). Fewer articles measured unemployment or occupation (n=3) (38, 48, 49), SES indices (n=4) (36, 39, 41, 48), or other SES indicators (n=2) (33, 48). Poverty was defined following U.S. government standards in which total family earnings are compared to the U.S. poverty thresholds, standards set for families of certain ages and sizes. Families under the threshold are considered to live in poverty (53). Most measures of income captured median household, family, or per capita income, representing measures of area central tendency rather than measures of income distribution. Whereas income was measured as an absolute phenomenon, education was typically measured as a relative phenomenon, with the percent of individuals above or below a certain level (e.g., percent of population with high school education or above). A few studies (n=4) measured indices comprised of multiple SES indicators including education, income, and unemployment (36, 39, 41, 48). No studies measured socioeconomic inequities—unequal distributions of economic assets, income, or education—using measures such as the Gini coefficient.
Individual-level Socioeconomic Status
Individual SES was controlled for using 1 to 4 measures. Table 2 displays the individual SES measures used and the number of categories for each measure. The most commonly used indicators were education (n=15) (21, 33, 34, 36–42, 47–49, 51, 52) and income (n=9) (21, 32, 37–40, 42, 48, 51); three studies calculated federal poverty levels using household income and the standard methods described above (33, 38, 47). Income was measured with annual family or household income and only one study controlled for family size or the number of people supported by that income (51). Education was typically defined as the highest level of education obtained. Three studies of Medicare beneficiaries used dual enrollment in Medicare and Medicaid as a proxy measure of individual low-income status, presumably due to a lack of other available SES indicators (23, 35, 50). Other individual SES measures included employment status (e.g., unemployed vs. employed) and occupation (e.g., professional vs. nonprofessional).
Table 2.
Summary of associations between area SES and cancer screening.
| Author, year | Outcome | Area Socioeconomic Status Indicators | Model Covariates
|
|||||
|---|---|---|---|---|---|---|---|---|
| Income | Poverty | Education | Employment | Indices | Other | |||
| Breast cancer screening | ||||||||
| Single level studies | ||||||||
| MSA | ||||||||
| Baker, 2004 | Recent mamm | ns |
|
|||||
| Recent CBE | ns | |||||||
| Zip Code | ||||||||
| * Sabogal, 2001 | Repeat mamm (vs. no repeat) | + |
|
|||||
| Regular repeat mamm (vs. irregular repeat mamm) | + | |||||||
| Parker, 1998 | Recent mamm | + | Unadjusted | |||||
| + |
|
|||||||
| Stratified: Medicare only |
|
|||||||
| + | ||||||||
| Stratified: Medicare + Medicaid | ||||||||
| ns | ||||||||
| * Rahman, 2003 | Repeat mamm adherence | +§ | Unadjusted | |||||
| +§ |
|
|||||||
| County | ||||||||
| Benjamins, 2004 | Recent mamm | ns | ||||||
| Census tract | ||||||||
| * Dailey, 2007 | Repeat mamm adherence | African American |
|
|||||
| + | + | + | + | + | ns1, +2, ns3, +4, +5 | |||
| White | ||||||||
| ns | + | + | + | ns | +1, ns2, +3, +4, ns5 | |||
| African American |
|
|||||||
| ns | ns | + | ns | + | ns1, +2, ns3, ns4, ns5 | |||
| White | ||||||||
| ns | ns | ns | ns | ns | +1, ns2, +3, ns4, ns5 | |||
| Other | ||||||||
| Siahpush, 2002 | Ever mamm | + |
|
|||||
| + |
|
|||||||
| Recent mamm | + |
|
||||||
| + |
|
|||||||
| Ever CBE | + |
|
||||||
| + |
|
|||||||
| Regular CBE | + |
|
||||||
| + |
|
|||||||
| Regular BSE | ns |
|
||||||
| ns |
|
|||||||
| Wells, 1998 | Ever mamm | + | + | + | ns | Unadjusted | ||
| + | + | + | ns |
|
||||
| Ever CBE | + | + | + | + | Unadjusted | |||
| + | + | ns | ns |
|
||||
| Multilevel studies | ||||||||
| MSA | ||||||||
| Schootman, 2005 | Ever mamm | + | Unadjusted | |||||
| + |
|
|||||||
| Ever CBE | + | Unadjusted | ||||||
| + |
|
|||||||
| County | ||||||||
| Litaker, 2007┼ | Recent mamm | ns | +6, ns7 |
|
||||
| ns | +6, ns7 |
|
||||||
| Block group | ||||||||
| * Rosenberg, 2005 | Repeat mammography in 3 time periods | + |
|
|||||
| ns |
|
|||||||
| Other | ||||||||
| Fukuda, 2005 | Recent breast screen | − | Unadjusted | |||||
| − |
|
|||||||
| Kothari, 2004 | Ever mamm | Int. | ns |
|
||||
| Cervical Screening | ||||||||
| Single level studies | ||||||||
| MSA | ||||||||
| Baker, 2004 | Recent Pap | ns |
|
|||||
| County | ||||||||
| Benjamins, 2004 | Recent Pap | ns | ||||||
| Coughlin, 2006┼ | Recent Pap | − | Int. |
|
||||
| Other | ||||||||
| Wells, 1998 | Ever Pap | + | + | ns | + | Unadjusted | ||
| + | + | ns | ns |
|
||||
| Siahpush, 2002b | Ever Pap | ns | Unadjusted | |||||
| ns |
|
|||||||
| Recent Pap | + | Unadjusted | ||||||
| ns |
|
|||||||
| Multilevel studies | ||||||||
| MSA | ||||||||
| Schootman, 2005 | Ever Pap | + | Unadjusted | |||||
| ns |
|
|||||||
| Census tract | ||||||||
| Datta, 2006 | Recent Pap | + |
|
|||||
| + |
|
|||||||
| Other | ||||||||
| Fukuda, 2005 | Recent Pap | − | Unadjusted | |||||
| − |
|
|||||||
| CRCS screening | ||||||||
| Single level studies | ||||||||
| Other | ||||||||
| Thorpe, 2003 | CRCS adherence | + |
|
|||||
| Col adherence | + | |||||||
| Multilevel studies | ||||||||
| MSA | ||||||||
| Schootman, 2005 | Ever FOBT | + | Unadjusted | |||||
| + |
|
|||||||
| Ever Col/Sig | + | Unadjusted | ||||||
| + |
|
|||||||
| County | ||||||||
| O’Malley, 2005 | CRCS Adherence | ns8, ns9 | ns |
|
||||
| Koroukian, 2006┼ | Recent FOBT | ns | + |
|
||||
| Recent SIG | ns | + | ||||||
| Recent Col/Sig | ns | ns | ||||||
| Recent Col | ns | ns | ||||||
| Other | ||||||||
| Fukuda, 2005 | Recent CRCS | ns | Unadjusted | |||||
| − |
|
|||||||
Shaded boxes indicate that ≥ 1 indicators of the specific area SES categories were measured in the study. + indicates that the main effect of the indicator was significantly and positively associated with the outcome, signifying that higher SES (i.e. higher income and education, lower poverty rates and unemployment) was associated with greater likelihood of cancer screening; − indicates a statistically significant negative association; ns indicates the association was not statistically significant; Int. indicates that there was a statistically significant interaction.
Note: All outcomes are stated in the positive direction for consistency. Results from unadjusted area SES-cancer screening models that provided effect sizes and final, fully adjusted models are provided. If only one model was provided in a study, results are presented from that model. If a study did not provide results from unadjusted analyses, data from the least adjusted models were extracted for presentation in the table.
Prospective or retrospective study design at the individual-level
Different categories of the same ABSM indicated both negative and positive associations; positive associations were more prevalent
Multiple areas-level SES measures included in the same models
% Crowding
% Working class
% Homes valued $300,000
% Without a car
% Homes boarded up
% Female headed households
Residence in Appalachia
Median family income
Per capita income
Covariates
Individual-level covariates included sociodemographic characteristics such as age, race/ethnicity, gender, and health insurance status. Behavioral or psychosocial covariates were rarely measured. Nine studies measured area-level covariates (21, 23, 32, 33, 35, 47, 48, 50, 52) such as racial/ethnic composition, area medical services, or urbanity. Area racial/ethnic composition was conceptualized as the percent of population that was non-white, non-Hispanic white, Mexican, Asian, or black. Measures of area-level medical characteristics included HMO market share, the number of generalists or specialty physicians in an area, or medically-underserved areas.
Cancer Screening
Studies measured multiple dichotomous dependent variables encompassing 7 types of cancer screening (mammography, clinical breast exam, breast self exam, fecal occult blood test, sigmoidoscopy, colonoscopy, and Pap smear) for breast, cervical, and colorectal cancer. Cancer screening uptake was measured by self-report in most studies or by clinic, administrative, or claims data in 5 studies (23, 34, 35, 48, 50); no studies used both methods. One study reported excluding testing done for diagnostic reasons or symptoms (23). The majority of dependent variables in the cross-sectional studies measured recent or adherent screening (within previous 1–2 years for breast cancer screening, 1–3 years for cervical cancer screening and 1–10 years for colorectal cancer screening) (21, 23, 32, 33, 36, 37, 41, 42, 47, 50–52). Three studies measured lifetime screening only (38, 40, 49). The 3 prospective studies (34, 39, 48) and 1 retrospective study (a study measuring screening retrospectively over time using claims data) (35), all of which measured breast cancer screening, measured repeat screening.
Associations between Area Socioeconomic Status and Cancer Screening
In all, 132 unadjusted and adjusted associations between ABSMs and cancer screening were tested (Table 2). Seventy-one (53.8%) associations were statistically significant and positive, indicating that as SES increased (i.e., increasing income and education, decreasing poverty and unemployment), the odds of cancer screening increased. Only 6 (4.5%) were negative associations and 55 (41.7%) were not statistically significant. Of 54 tested associations from models that did not control for individual SES, 38 (70.4%) were positive, 2 (3.7%) were negative, and 14 (25.9%) were not statistically significant. After controlling for individual level SES and other covariates in fully adjusted models, 32 (41.0%) of 78 tested associations were positive, 4 (5.1%) were negative, and 42 (53.9%) were not statistically significant. Fewer associations were statistically significant and positive in multilevel models (n=17, 43.6%) versus single level models that did not account for the clustering of individuals in areas (n=53, 57.0%).
Notably, while there are many positive and nonsignificant results, there are far fewer negative associations, with the majority of those attributable to one study. In this Japanese study, the authors suggest that the unexpected direction of effect may reflect a lower likelihood of screening in urban areas resulting from the use of an imprecise indicator of urbanity and/or the very strong correlation between urbanization and higher regional indicators of income and education in Japan (32).
Breast Cancer Screening
In all, 13 studies measured breast cancer screening; 4 employed prospective or retrospective study designs (34, 35, 39, 48) and 5 provided results of multilevel analyses (32, 33, 39, 40, 49). Of all studies, 2 demonstrated only nonsignificant results (21, 47), 1 demonstrated only negative associations (32), 2 demonstrated significant interactive effects (49, 50), and the remaining 8 studies (including the 4 prospective or retrospective studies) demonstrated at least one significant positive association, although in a prospective study, one of these was no longer significant after adjustment for household income (39) and another prospective study demonstrated both positive and negative associations between categories of zip code median income and mammography adherence (34).
Of the 2 studies demonstrating interactive effects, a Canadian study demonstrated a significant cross level interaction between regional education and social involvement, demonstrating that the influence of increased participation in volunteer activities and religious services modified the negative influence of low regional education level on mammography uptake (6). In a study of U.S. Medicare beneficiaries, compared to those living in zip codes in the highest quintile of college education rates, Medicare-only women living in the lowest quintiles were less likely (OR: 0.73; 95% CI: 0.72–0.74) and Medicare-Medicaid women were equally as likely (OR: 0.98; 95% CI: 0.94–1.02) to have had a recent mammography (41).
Several breast cancer screening studies measured multiple associations, encompassing multiple ABSMs and/or dependant variables (33, 38, 41, 48). One study measured a total of 40 associations including both unadjusted and adjusted associations between a single dependent variable and 10 ABSMs separately for African American and white women. In this single level prospective study, different ABSMs predicted nonadherence to mammography for blacks and whites. In the fully adjusted models of 10 ABSMs, 5 demonstrated statistically significant positive associations with mammography: 3 among blacks (% working class, % adults without high school education, and the SES Index) and 2 (% living in crowded conditions, % of homes valued ≥$300,000) among whites (48).
Of the 3 cancer screening modalities included in this review, breast cancer screening is the best developed and most frequently studied. The findings of these studies, while mixed, demonstrate predominantly positive associations. Several studies demonstrated that the associations between area SES and breast cancer screening may differ by individual or area characteristics or by ABSM (33, 38, 48–50) and several studies demonstrated attenuation of effects after control for covariates (38, 39, 48). Overall, these results indicate that associations between area SES and breast cancer screening may be more complex than previously acknowledged and suggest a need for further research in ABSM measurement and both moderating and mediating pathways in the breast cancer literature.
Cervical Cancer Screening
Eight cross-sectional studies examined cervical cancer screening (21, 32, 38, 40, 41, 47, 51, 52). These studies typically controlled for few individual or area covariates, 5 measured only a single ABSM (21, 32, 40, 41, 47, 52), and only 3 employed multilevel analyses (40, 52, 54). Two studies examined only lifetime use of a Pap smear (38, 40) and the others examined Pap screening in the last 1–3 years. One of the U.S. studies was conducted at the census tract level (52); no studies were conducted at the block group level.
In the 4 studies presenting unadjusted associations, 1 found only negative associations (32) and 3 found at least one significant positive association between lower area SES and lifetime receipt of Pap screening (38, 40, 41). In models that controlled for individual SES, only 2 of 8 studies demonstrated at least one significant positive association between low area SES and Pap screening and 1 study demonstrated 1 negative and 1 significant interactive effect. After controlling for all individual covariates and state level poverty, a multilevel study of black women found that compared to those living in census tracts with <5% poverty, women living in high poverty areas (≥20% poverty) were 1.2 times more likely (95% CI: 1.1–1.4) to have not had a Pap smear in the 2 years (52). The other study with positive adjusted associations found larger effects between area median income, percent living in poverty, and lifetime receipt of Pap smear but controlled for fewer covariates (38). A single level study found a negative association between area poverty and Pap smear in the last 3 years, a non-significant interaction between individual income and county-level poverty and a significant interaction between individual and area-level education, with less educated women living in better educated counties less likely to undergo Pap screening than the same women living in less educated counties (51). One additional study reported the results of testing for interactions and found a non-significant interaction of census tract poverty rate and individual education(52).
Overall, the findings for cervical cancer screening were mixed and demonstrated positive, negative, nonsignificant, and interactive associations. Compared to the breast cancer literature, the cervical cancer literature is sparse and includes few studies conducted at smaller, more homogenous geographic levels and few multilevel studies.
Colorectal Cancer Screening
Five cross-sectional studies measured CRCS (23, 32, 37, 40, 42), 4 of which employed multilevel analyses (23, 32, 40, 42). All but one of the CRCS studies (32) were conducted in the U.S., none examined census tracts or block groups, 1 measured lifetime use of screening (40), 2 measured recent or adherent screening within the last 1–10 years, with the time interval contingent on test modality (37, 42) and 2 measured testing within the last year regardless of test modality (23, 32).
In all, 3 studies demonstrated at least 1 significant positive association between area SES and CRCS, 1 study demonstrated a significant negative association, and 1 study found only nonsignificant associations. In the 2 studies that controlled for the most comprehensive sets of individual- and county-level covariates such as use of and local availability of healthcare services (23, 42), 1 study tested 8 associations and found 2 positive associations, with a higher county-level percent of adults with high school diplomas associated with greater likelihood of FOBT (OR: 1.06, 95% CI: 1.00–1.12) and SIG (OR: 1.14 95% CI: 1.08–1.20) in the last year. In the same models, poverty was not significant; and neither ABSM was associated with colonoscopy alone or a combined variable of either sigmoidoscopy or colonoscopy (23). The other study did not present data but reported no significant random variation at the county level and reported that none of the county-level variables (percentage of population in poverty, median family income, and per capital income) were associated with any type of CRCS adherence in the multivariate models (42). Of the remaining 3 CRCS studies, the Japanese study reported a negative adjusted association (32) and the other 2 U.S. studies found that all 6 of the tested associations between MSA- and neighborhood-level poverty and lifetime (40) and adherent screening (37) were positive.
Overall, with only 5 studies, the CRCS literature is the most limited domain of the 3 cancer screening modalities reviewed here. The findings are mixed and while the majority of studies use multilevel analyses, no studies measured SES at the census tract or block group level, and only 2 studies measured multiple ABSMs.
Discussion
Overall, we found a high degree of heterogeneity in study design, statistical methods, and definitions and measures of area and individual SES, screening tests, and covariates. Given the limited sets of conceptually and methodologically similar studies in which to compare and contrast findings, and a lack of clear patterns in the associations by outcomes, study design, and methods, we were unable to provide a definitive evidence synthesis or draw conclusions about the strength of the evidence either for or against an area SES-cancer screening association over and above individual SES.
The broader area and health research literature has seen significant debate and discussion regarding current methodologic practices (55–66) and previous reviews and critiques have outlined multiple weaknesses in the literature (46, 67–70). Building on these critiques and incorporating the identified sources of heterogeneity and weaknesses in the studies reviewed here, we identify 5 key priority areas of research and set 6 immediate research targets for the multilevel cancer screening literature.
Priority Area 1: Theory and Conceptualization
This literature is currently dominated by either atheoretical studies or individual-level behavior change models and is limited by a lack of understanding regarding the mechanisms linking areas and behavior. Only a handful of studies cited theory or conceptual models as justification for their selection of variables or analytic methods (33, 34, 40, 47, 48). Cited models include the Health Belief Model and Andersen’s Behavioral Model of Health Services Use. Many individual-level psychosocial and behavioral correlates and predictors of cancer screening behavior have been identified (71), including receiving a screening recommendation from a doctor and perceived risk of cancer; however, these variables were rarely included in the reviewed studies. Thus, while we have some understanding regarding the mechanisms linking individual SES and health behavior and outcomes (72), we know little about the pathways through which area SES influences health and screening behaviors. Several studies discussed possible mechanisms linking area characteristics and cancer screening by suggesting that access to material resources such as medical facilities was a primary driver of observed associations. Other studies suggested social influences and resources as possible mechanisms linking area characteristics to individual behavior. Suggested social mechanisms included social support, social cohesion, collective efficacy, social capital, social norms, values and attitudes about healthcare, social and economic pressures shaping the quality of healthcare options, and overall variability of opportunities for choices about healthcare behaviors in different areas. Many of these mechanisms, well-established in other fields, deserve hypothesis development and testing in the cancer screening literature. While some of the reviewed studies suggested that area characteristics may shape individual behavior by influencing individual income, education, and employment opportunities, few explored cross-level ABSM interaction terms and no studies tested for mediation.
Although several conceptual models have been developed, no comprehensive and testable theory is available that offers an adequate explanation of the mechanisms linking area-level factors to a diversity of health outcomes (69, 73, 74). The challenge for the cancer screening literature is to begin to integrate our established individual-level models and constructs with perspectives capturing higher-level structural inequities. Similar efforts at conceptual integration are already underway in other fields where researchers are mapping the links between areas and cardiovascular and glycemic disease (28–31). It is important for all prevention sciences to move beyond models identifying individual-level predictors of health outcomes to modeling the pathways linking areas and individual health behaviors.
Acknowledging the influence of different intra- and inter-national cultural contexts, rather than assuming homogeneity of area-level effects across populations and societies, will be of critical importance. In this review, for example, unexpected negative associations were seen in the one reviewed Japanese study (32), possibly the result of a different cultural context. And a recent cancer screening study demonstrated three-way interactions between area-level SES, gender, and race (75), suggesting differential effects of area-level factors by population subgroup.
The current lack of cross-level conceptual integration limits our ability to develop and test creative and appropriate hypotheses regarding mediating and moderating pathways. By incorporating hypothesized multilevel pathways and mechanisms, newer models will provide a useful guide for researchers, policy-makers and health promoters seeking to understand and influence the multilevel context of cancer screening in order to prevent cancer-related inequities.
Priority Area 2: Temporality and Causality
Many of the studies in this review demonstrated some significant associations between ABSMs and cancer screening; however, most were cross-sectional and thus unable to establish causality. While cancer screening researchers have been encouraged to use consistent measures of consecutive or repeat on-schedule screening (76–79) due to the high prevalence of lifetime screening, particularly for breast and cervical cancer, several studies measured only lifetime screening, further obscuring any potential temporal associations. Even studies with retrospective and prospective designs did not fully capture the temporal associations between areas and individuals. For example, while a few studies may have carefully and prospectively measured individual adherence to screening, the exposure of interest, area SES, may have been measured several years earlier or even concurrently with individual-level covariates and outcomes.
Although the majority of cross-sectional multilevel studies, including most of those in this review, do not include individual and area data drawn from the same time period, partly due to feasibility issues such as the infrequent collection of area-level data (55), they still treat the data as cross-sectional. By ignoring the need for a time-lag for many exposures and the possibility of change at the area-level, such as gentrification, and at the individual-level, with individuals migrating in and out of areas over time, these studies miss important opportunities to model potential causal relations between areas and health. Collecting exposure and outcome data at the same time implies a zero time lag between area exposures and individual outcomes, an implausible scenario unless the area exposure is assumed to be stable over time (80). Three studies collected exposure and outcome data from the same time periods by using the same data source for both levels, with areas comprised solely of aggregated responses to the individual survey. In addition to assuming a zero time lag, this approach can result in same source bias—a spurious association related to the use of the same individuals’ self report assessments of both exposure and outcome (81). Moreover, unless compositional effects tests are conducted, it is not known whether modeling an aggregated variable at a higher level of analysis provides increased explanatory power as compared to modeling the original variable at the individual-level.
The preponderance of cross-sectional designs, lack of temporally matched data, and lack of appropriately time-lagged study designs in this literature clouds an already unclear etiologic picture between area SES and cancer screening. At a minimum, assumptions of area stability or change over time should be theoretically justified; for example, while immediate changes in transportation infrastructure are unlikely, very rapid socio-cultural changes may result from area gentrification or area decline. Going further, these assumptions may be tested by examining the stability of population composition over time. Future research should employ prospective designs that incorporate aspects of lifecourse and choice theories and should control for the effect of individuals moving into and out of geographic areas.
Priority 3: Defining Area Units
Studies primarily relied on larger area units defined for political or administrative purposes. Decisions about the most appropriate geographic levels for analysis are often driven by considerations of data availability, sample size, and area homogeneity, with larger areas such as zip codes and counties considered more heterogeneous than smaller areas such as census tract and block groups. Extreme within-cluster heterogeneity may limit the utility of central tendency measures such as median household income while total homogeneity within an area may preclude studies of area effects (46). Although debate exists about appropriate geographic levels of analysis (61, 63, 66), previous U.S. research has indicated that smaller units such as census tracts or block groups model socioeconomic gradients in some health outcomes more consistently than larger geographic units (82–85). Research in Australia has also supported the use of smaller geographic units known as collector’s districts rather than larger postcodes (86). Studies using smaller, more homogeneous geographic units such as census tracts and block groups are underrepresented in the U.S. literature, including the cancer screening literature reviewed here, and deserve more attention. Future research should explore the validity and reliability of various ABSMs across geographic units in studies controlling for individual SES or in studies examining cancer prevention behavior outcomes. Cancer prevention researchers should also begin to incorporate approaches such as conditional autoregressive models (87) and hierarchical geostatistical models (88, 89) as methods to help guard against the modifiable areal unit problem, in which aggregation of continuous spatial phenomena to administrative areas of arbitrary sizes and shapes may introduce bias.
Ideally, researchers should specify the hypothesized mechanisms underlying the association of interest and select areas that best capture those pathways of influence. For example, studies have shown that the effects of socioeconomic inequity on health using measures such as the Gini coefficient are best captured with the use of larger areas encompassing larger populations and greater heterogeneity (90, 91). If area effects are hypothesized to influence outcomes via characteristics of inter-personal mechanisms such as social support, capital, or norms, community-defined and natural neighborhood boundaries or administrative areas of smaller sizes may be the most appropriate choice of area-level. Alternatively, because social service, housing, and medical services are typically delivered at county or other administratively-defined levels, researchers hypothesizing about these mechanisms should consider using the relevant administrative boundaries.
Priority Area 4: Area-based Socioeconomic Measures
There are multiple weaknesses in the measurement of area-level SES in this literature including the use of a limited set of ABSMs, potential residual confounding from individual SES, the exclusive use of compositional ABSMs, and the unknown effects of categorizing ABSMs.
Limited Set of ABSMs
While multiple ABSMs were used in these studies, the majority were indicators of poverty, income, and education; fewer measures captured area distributions of employment, occupation, resources, or wealth. A much wider array of ABSMs and other area-level indicators have been employed in sociology and in the wider public health literature (46, 70, 92). Some examples of these variables include: availability of health services, measures of medical underservice, distance to medical facilities, neighborhood social and physical disorder, residential mobility, wealth as measured by assets or non-salary income, social class, community socialization and involvement, social trust and cohesion, norms, collective efficacy, compositional demographics, family structure, and subjective and perceived area SES (46, 70, 92–94).
Residual Confounding
Several studies in this review controlled for only a single individual SES variable and many variables were measured with only 2 or 3 categories. A few used a measure of dual enrollment in Medicare and Medicaid as the only individual SES measure. While this measure is thought to “reflect on the individual’s low income status” (23), not all eligible low-income individuals are Medicaid beneficiaries and dually-eligible individuals may differ from Medicare-only enrollees; for example, they are more likely to be institutionalized and face greater health concerns (95). With limited or inaccurate control of individual-level SES, ABSMs may be more likely to capture the unmeasured aspects of individual SES. However, if individual variables are mediators on the causal pathway between area SES and individual outcomes, controlling for multiple indicators of individual SES may result in an underestimation of the true independent effects of area-level characteristics (57).
Compositional ABSMs
All ABSMs in these studies were compositional variables. Such aggregated variables are assumed to represent contextual characteristics of neighborhoods. Contextual variables measured at the area-level, such as observation of the number of broken windows in a neighborhood, have been recommended by some to better capture area characteristics (96) and others have argued for triangulation with the use of multiple methods of ABSM ascertainment (81, 97). However, the lack of data about the reliability and validity of various area characteristics combined with a lack of standardized national data of contextual area characteristics has limited the applicability of such measures for large-scale U.S. studies. Ideally, the decision between compositional and contextual variables should be driven by theory. A classic example of a theory-driven compositional variable is social norms, demonstrated in statistical analyses to have predictive power beyond that explained by individually reported norms alone (98).
Categorizing ABSMs
SES is often conceptualized as a relative phenomena (99, 100) and categorizing either area- or individual-level SES may obscure the full gradient of SES inequities (101). However, the majority of studies in this review employed categorical ABSMs and in many studies, only a few of the measured categories were significantly associated with the outcome. Whether these findings are indicative of non-linear associations, threshold effects, or are artifacts of sample size in each of the categories or the size and homogeneity of each category, is unclear. To begin to address these unanswered questions, researchers should be clear about their theoretical or methodologic reasons for employing categorized or continuous ABSMs and make explicit their reasons for their decisions.
Improving ABSMs
The limitations of the current practices involving ABSMs combined with a lack of reporting about the psychometric and distributional properties of these variables hamper definitive conclusions about the validity of these measures across or within cancer screening behaviors. Future cancer prevention research should explore a broader range of ABSMs than previously explored, should acknowledge the well-known drawbacks resulting from the use of SES indices (46, 83–85), should begin introducing contextual variables, and should explore and report the effects of categorization. In particular, smaller, in-depth pilot and qualitative primary data collection studies are needed in the cancer prevention literature to introduce and explore subjective measures of area context as perceived by neighborhood residents as well as systematic social observations made by outsiders (non-residents) (81, 93, 94, 102). And while this first generation of research has taken advantage of existing available data, future decisions about ABSMs should be guided by theory when possible.
Priority Area 5: Analytic Challenges in Multilevel Modeling
We restricted our review to studies that are inherently hierarchical, with individuals living nested within areas and studies measuring both individual- and area-level SES. However, over half of the studies used standard single level logistic regression analyses that did not account for this clustering. It should be noted that one study presented single level analyses after testing for and finding no significant random effects at area-level (48), an intuitively appropriate but debatable strategy given the power and estimation difficulties related to variance component tests in multilevel logistic models (103). Failure to test for multilevel nesting and subsequently account for the hierarchical nature of data using multilevel analyses leads to negatively biased standard errors potentially resulting in spuriously statistically significant results (103). Multilevel analyses, on the other hand, account for clustering (non-independence) of individuals within areas and allow for the simultaneous modeling of the association of group and individual characteristics and any interaction between the two on outcomes.
Multilevel analyses have their own methodologic challenges previously described in earlier methodologic papers (57, 59, 65, 80, 104, 105). One of the critical challenges in the multilevel literature that was poorly addressed in these studies is the decomposition of variance in the outcome into within and between area components. The relative influence and importance of area vs. individual attributes on individual outcomes is an unresolved debate. We cannot shed much additional light on this topic, in part because most studies reviewed here based their claims about the relative importance of multiple levels on an examination of effect sizes and associated p-values of area- and individual- fixed effects, an inappropriate strategy. An alternative method for drawing conclusions about the relative importance of multiple levels of influence is the intraclass correlation coefficient (ICC), a measure expressing the proportion of the totalvariance in the individual outcome resulting from the influence of the area-level. However, while widely used and appropriate for use in multilevel linear models, debate exists about the appropriateness of the ICC in multilevel logistic regression models. Few studies in this review (32, 40, 48, 52) presented ICCs or other partitioned variance estimates. Alternative measures such as median and interval odds ratios that capture area variance have been suggested (64, 106–108) and while appropriate for dichotomous outcomes, are not yet widely used and should be adopted in this literature.
Cancer screening researchers should take advantage of recent technological innovations in Bayesian and spatial analytic methods (87, 89, 109, 110) that can incorporate temporal and spatial dimensions such as spatial adjacency and decay functions and dynamic agent-based models, computer representations of the multiple feedback loops between people and places that lead to spatial patterning of individual-level outcomes (111). Further development and use of multilevel structural equation modeling, methods allowing for more sophisticated testing of moderating and mediating pathways, is also needed.
Immediate Research Targets
We have offered multiple suggestions for improvement within our 5 identified priority areas of research and while all are important, we acknowledge that to some extent, our suggestions represent an ambitious wish-list of ideals. Given the emerging nature of this research, the limitations of existing area-level data, and the developmental stage of our more advanced analytic methods, we acknowledge the importance of identifying realistic and immediate next steps of this research. That said, we recommend the following 6 more immediate research goals: 1) Infuse more theory into the literature by applying existing theories and developing and testing new conceptual models. 2) Conduct prospective studies and embrace natural experiments when possible. 3) Move beyond poverty by comparing contrasting multiple ABSMs within studies. 4) Conduct qualitative and pilot studies to capture unique social and physical characteristics at the area-level and to explore areal units that go beyond aggregated administrative data and administrative boundaries. 5) Accept complexity by testing for cross-level interactions and population subgroup effects. And lastly, 6) Continue to develop and implement alternative analytic technologies and when using multilevel logistic models, expand reporting of model statistics, and when possible, measures of area-level variance and median and interval odds ratios.
Conclusion
Among the 3 cancer screening behaviors in this review, the breast cancer screening literature is the most extensive and the only literature that has employed prospective designs. Greater attention to cervical and colorectal cancer screening and prospective designs is needed, particularly among African American and Hispanic populations that have been largely overlooked in this literature.
Limitations of this review include that it was limited to published, peer-reviewed, English-language articles and to studies measuring at least one indicator of area SES. We may have excluded studies measuring other important area-level factors such as medical underservice or area racial/ethnic composition. Despite these limitations, this is the first attempt to systematically review the literature in this emergent area of cancer prevention research.
Early efforts to monitor and promote cancer screening focused on individual determinants. In recent years, the cancer screening literature has witnessed an increasing number of calls to increase and improve research into the multilevel context in which health behavior occurs (78, 112, 113). Although conceptual and methodologic heterogeneity and weaknesses limited our ability to draw definitive conclusions about the underlying relations between area SES and cancer screening, we believe that awareness of these limitations will lead to better decisions regarding conceptualization, measurement, and analysis of area SES factors associated with cancer screening. Addressing these issues will allow future researchers to develop and test more sophisticated hypotheses about the complex interrelations between the multiple levels of influence and effective methods of cancer prevention and control.
Acknowledgments
Funding: This work was supported by: the predoctoral fellowship of SLP while at University of Texas School of Public Health (UTSPH Cancer Education and Career Development Program, National Institutes of Health, National Cancer Institute R25 CA05771) and the postdoctoral fellowship of SLP at WU (Barnes Jewish Hospital Foundation, Siteman Cancer Center Prevention and Control Program) and grant support of SWV’s time (National Institutes of Health, National Cancer Institute, RO1 CA97263 and RO1 CA112223). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
The authors acknowledge Margaret Anderson for her assistance with identifying subject headings appropriate for the electronic database search and Stephanie Wuelling Russell for her help with data extraction.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer Facts and Figures. 2009 [Accessed on 5–6–2009]; Available from: http://www.cancer.org/docroot/STT/STT_0.asp.
- 3.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer, 2006. CA Cancer J Clin. 2006;56:11–25. doi: 10.3322/canjclin.56.1.11. [DOI] [PubMed] [Google Scholar]
- 4.U. S. Preventive Services Task Force. Guide to clinical preventive services, 2007: Recommendations of the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality, 2007; 20080311. Report No.: AHRQ Publication No. 07–05100. [Google Scholar]
- 5.Meissner HI, Breen N, Klabunde CN, Vernon SW. Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2006;15:389–94. doi: 10.1158/1055-9965.EPI-05-0678. [DOI] [PubMed] [Google Scholar]
- 6.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–40. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 7.Singh GK, Miller BA, Hankey BF, Edwards BK. Area socioeconomic variations in U.S. cancer incidence, mortality, stage, treatment, and survival, 1975–1999. Bethesda, MD: National Cancer Institute; 2003. NIH Publication No. 03–0000. [Google Scholar]
- 8.Ward E, Jemal A, Cokkinides V, et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54:78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 9.Katz SJ, Hofer TP. Socioeconomic disparities in preventive care persist despite universal coverage. Breast and cervical cancer screening in Ontario and the United States. JAMA. 1994;272:530–4. [PubMed] [Google Scholar]
- 10.Nelson DE, Bolen J, Marcus S, Wells HE, Meissner H. Cancer screening estimates for U.S. metropolitan areas. Am J Prev Med. 2003;24:301–9. doi: 10.1016/s0749-3797(03)00024-2. [DOI] [PubMed] [Google Scholar]
- 11.Phillips KA, Liang SY, Ladabaum U, et al. Trends in Colonoscopy for Colorectal Cancer Screening. Med Care. 2007;45:160–7. doi: 10.1097/01.mlr.0000246612.35245.21. [DOI] [PubMed] [Google Scholar]
- 12.Braveman P, Gruskin S. Defining equity in health. J Epidemiol Community Health. 2003 Apr;57:254–8. doi: 10.1136/jech.57.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whitehead M. The concepts and principles of equity and health. Int J Health Serv. 1992;22:429–45. doi: 10.2190/986L-LHQ6-2VTE-YRRN. [DOI] [PubMed] [Google Scholar]
- 14.Benard VB, Eheman CR, Lawson HW, et al. Cervical screening in the National Breast and Cervical Cancer Early Detection Program, 1995–2001. Obstet Gynecol. 2004 Mar;103:564–71. doi: 10.1097/01.AOG.0000115510.81613.f0. [DOI] [PubMed] [Google Scholar]
- 15.DeGroff A, Holden D, Goode Green S, Boehm J, Seeff LC, Tangka F. Start-up of the colorectal cancer screening demonstration program. Prev Chronic Dis. 2008 Apr;5:A38. [PMC free article] [PubMed] [Google Scholar]
- 16.Eheman CR, Benard VB, Blackman D, et al. Breast cancer screening among low-income or uninsured women: results from the National Breast and Cervical Cancer Early Detection Program, July 1995 to March 2002 (United States) Cancer Causes Control. 2006 Feb;17:29–38. doi: 10.1007/s10552-005-4558-y. [DOI] [PubMed] [Google Scholar]
- 17.Seeff LC, DeGroff A, Tangka F, et al. Development of a federally funded demonstration colorectal cancer screening program. Prev Chronic Dis. 2008 Apr;5:A64. [PMC free article] [PubMed] [Google Scholar]
- 18.Bigby J, Holmes MD. Disparities across the breast cancer continuum. Cancer Causes Control. 2005;16:35–44. doi: 10.1007/s10552-004-1263-1. [DOI] [PubMed] [Google Scholar]
- 19.Newmann SJ, Garner EO. Social inequities along the cervical cancer continuum: a structured review. Cancer Causes Control. 2005;16:63–70. doi: 10.1007/s10552-004-1290-y. [DOI] [PubMed] [Google Scholar]
- 20.Palmer RC, Schneider EC. Social disparities across the continuum of colorectal cancer: a systematic review. Cancer Causes Control. 2005;16:55–61. doi: 10.1007/s10552-004-1253-3. [DOI] [PubMed] [Google Scholar]
- 21.Baker LC, Phillips KA, Haas JS, Liang SY, Sonneborn D. The effect of area HMO market share on cancer screening. Health Serv Res. 2004;39:1751–72. doi: 10.1111/j.1475-6773.2004.00316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coughlin SS, Leadbetter S, Richards T, Sabatino SA. Contextual analysis of breast and cervical cancer screening and factors associated with health care access among United States women, 2002. Soc Sci Med. 2008 Jan;66:260–75. doi: 10.1016/j.socscimed.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 23.Koroukian SM, Xu F, Dor A, Cooper GS. Colorectal cancer screening in the elderly population: disparities by dual Medicare-Medicaid enrollment status. Health Serv Res. 2006;41:2136–54. doi: 10.1111/j.1475-6773.2006.00585.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schootman M, Walker MS, Jeffe DB, Rohrer JE, Baker EA. Breast cancer screening and incidence in communities with a high proportion of uninsured. Am J Prev Med. 2007 Nov;33:379–86. doi: 10.1016/j.amepre.2007.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med. 1994 Oct;39:887–903. doi: 10.1016/0277-9536(94)90202-x. [DOI] [PubMed] [Google Scholar]
- 26.Shaw CR, McKay HD. Juvenile delinquency in urban areas. Chicago: University of Chicago Press; 1942. [Google Scholar]
- 27.Putnam R. The prosperous community: Social capital and community life. American Prospect. 1993:4. [Google Scholar]
- 28.Daniel M, Moore S, Kestens Y. Framing the biosocial pathways underlying associations between place and cardiometabolic disease. Health Place. 2008 Jun;14:117–32. doi: 10.1016/j.healthplace.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003 Dec;80:569–89. doi: 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Homer J, Milstein B, Wile K, Pratibhu P, Farris R, Orenstein DR. Modeling the local dynamics of cardiovascular health: risk factors, context, and capacity. Prev Chronic Dis. 2008 Apr;5:A63. [PMC free article] [PubMed] [Google Scholar]
- 31.Schulz AJ, Kannan S, Dvonch JT, et al. Social and physical environments and disparities in risk for cardiovascular disease: The Healthy Environments Partnership conceptual model. Environmental Health Perspectives. 2005 Dec;113:1817–25. doi: 10.1289/ehp.7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fukuda Y, Nakamura K, Takano T. Reduced likelihood of cancer screening among women in urban areas and with low socio-economic status: a multilevel analysis in Japan. Public Health. 2005;119:875–84. doi: 10.1016/j.puhe.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 33.Litaker D, Tomolo A. Association of contextual factors and breast cancer screening: finding new targets to promote early detection. J Womens Health (Larchmt) 2007;16:36–45. doi: 10.1089/jwh.2006.0090. [DOI] [PubMed] [Google Scholar]
- 34.Rahman SM, Dignan MB, Shelton BJ. Factors influencing adherence to guidelines for screening mammography among women aged 40 years and older. Ethn Dis. 2003;13:477–84. [PMC free article] [PubMed] [Google Scholar]
- 35.Sabogal F, Merrill SS, Packel L. Mammography rescreening among older California women. Health Care FinancRev. 2001;22:63–75. [PMC free article] [PubMed] [Google Scholar]
- 36.Siahpush M, Singh GK. Sociodemographic variations in breast cancer screening behavior among Australian women: results from the 1995 National Health Survey. Prev Med. 2002;35:174–80. doi: 10.1006/pmed.2002.1063. [DOI] [PubMed] [Google Scholar]
- 37.Thorpe LE, Mostashari F, Hajat A, et al. Colon cancer screening practices in New York City, 2003: results of a large random-digit dialed telephone survey. Cancer. 2005;104:1075–82. doi: 10.1002/cncr.21274. [DOI] [PubMed] [Google Scholar]
- 38.Wells BL, Horm JW. Targeting the underserved for breast and cervical cancer screening: the utility of ecological analysis using the National Health Interview Survey. Am J Public Health. 1998;88:1484–9. doi: 10.2105/ajph.88.10.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenberg L, Wise LA, Palmer JR, Horton NJ, Adams-Campbell LL. A multilevel study of socioeconomic predictors of regular mammography use among African-American women. Cancer Epidemiol Biomarkers Prev. 2005;14:2628–33. doi: 10.1158/1055-9965.EPI-05-0441. [DOI] [PubMed] [Google Scholar]
- 40.Schootman M, Jeffe DB, Baker EA, Walker MS. Effect of area poverty rate on cancer screening across US communities. Journal of Epidemiology and Community Health. 2006;60:202–7. doi: 10.1136/jech.2005.041020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Siahpush M, Singh GK. Sociodemographic predictors of pap test receipt, currency and knowledge among Australian women. Prev Med. 2002;35:362–8. doi: 10.1006/pmed.2002.1086. [DOI] [PubMed] [Google Scholar]
- 42.O’Malley AS, Forrest CB, Feng S, Mandelblatt J. Disparities despite coverage: gaps in colorectal cancer screening among Medicare beneficiaries. Arch Intern Med. 2005;165:2129–35. doi: 10.1001/archinte.165.18.2129. [DOI] [PubMed] [Google Scholar]
- 43.Slavin RE. Best evidence synthesis: an intelligent alternative to meta-analysis. J Clin Epidemiol. 1995 Jan;48:9–18. doi: 10.1016/0895-4356(94)00097-a. [DOI] [PubMed] [Google Scholar]
- 44.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000 Apr 19;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 45.United Nations Development P. Human development report 2007/2008: 2007 [updated 2008/02/27/].
- 46.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. Journal of Epidemiology and Community Health. 2001;55:111–22. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Benjamins MR, Kirby JB, Bond Huie SA. County characteristics and racial and ethnic disparities in the use of preventive services. Prev Med. 2004;39:704–12. doi: 10.1016/j.ypmed.2004.02.039. [DOI] [PubMed] [Google Scholar]
- 48.Dailey AB, Kasl SV, Holford TR, Calvocoressi L, Jones BA. Neighborhood-level socioeconomic predictors of nonadherence to mammography screening guidelines. Cancer Epidemiol Biomarkers Prev. 2007;16:2293–303. doi: 10.1158/1055-9965.EPI-06-1076. [DOI] [PubMed] [Google Scholar]
- 49.Kothari AR, Birch S. Individual and regional determinants of mammography uptake. Can J Public Health. 2004;95:290–4. doi: 10.1007/BF03405134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parker J, Gebretsadik T, Sabogal F, Newman J, Lawson HW. Mammography screening among California Medicare beneficiaries: 1993–1994. Am J Prev Med. 1998;15:198–205. doi: 10.1016/s0749-3797(98)00045-2. [DOI] [PubMed] [Google Scholar]
- 51.Coughlin SS, King J, Richards TB, Ekwueme DU. Cervical cancer screening among women in metropolitan areas of the United States by individual-level and area-based measures of socioeconomic status, 2000 to 2002. Cancer Epidemiol Biomarkers Prev. 2006;15:2154–9. doi: 10.1158/1055-9965.EPI-05-0914. [DOI] [PubMed] [Google Scholar]
- 52.Datta GD, Colditz GA, Kawachi I, Subramanian SV, Palmer JR, Rosenberg L. Individual-, neighborhood-, and state-level socioeconomic predictors of cervical carcinoma screening among U.S. black women: a multilevel analysis. Cancer. 2006;106:664–9. doi: 10.1002/cncr.21660. [DOI] [PubMed] [Google Scholar]
- 53.U.S. Census Bureau. How the Census Bureau measures poverty (official measure) [1- 26–09]; Available from: http://www.census.gov/hhes/www/poverty/povdef.html.
- 54.Fukuda Y, Nakamura K, Takano T. Accumulation of health risk behaviours is associated with lower socioeconomic status and women’s urban residence: a multilevel analysis in Japan. BMC Public Health. 2005;5:53. doi: 10.1186/1471-2458-5-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Buzzelli M, Su J. Multi-level modelling in health research: a caution and rejoinder on temporally mismatched data. Soc Sci Med. 2006;62:1215–8. doi: 10.1016/j.socscimed.2005.06.056. [DOI] [PubMed] [Google Scholar]
- 56.Cummins S. Commentary: investigating neighbourhood effects on health--avoiding the ‘local trap’. Int J Epidemiol. 2007;36:355–7. doi: 10.1093/ije/dym033. [DOI] [PubMed] [Google Scholar]
- 57.Diez Roux AV. Estimating neighborhood health effects: the challenges of causal inference in a complex world. Soc Sci Med. 2004;58:1953–60. doi: 10.1016/S0277-9536(03)00414-3. [DOI] [PubMed] [Google Scholar]
- 58.Diez Roux AV. Commentary: estimating and understanding area health effects. Int J Epidemiol. 2005;34:284–5. doi: 10.1093/ije/dyi020. [DOI] [PubMed] [Google Scholar]
- 59.Diez-Roux AV. Bringing context back into epidemiology: variables and fallacies in multilevel analysis. Am J Public Health. 1998;88:216–22. doi: 10.2105/ajph.88.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21:171–92. doi: 10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed] [Google Scholar]
- 61.Geronimus AT, Bound J. Use of census-based aggregate variables to proxy for socioeconomic group: Evidence from national samples. American Journal of Epidemiology. 1998;148:475–86. doi: 10.1093/oxfordjournals.aje.a009673. [DOI] [PubMed] [Google Scholar]
- 62.Kaufman JS. Re: “Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression”. Am J Epidemiol. 2005;162:602–3. doi: 10.1093/aje/kwi251. [DOI] [PubMed] [Google Scholar]
- 63.Krieger N, Gordon D. Re: “Use of census-based aggregate variables to proxy for socioeconomic group: evidence from national samples”. Am J Epidemiol. 1999;150:892–6. doi: 10.1093/oxfordjournals.aje.a010095. [DOI] [PubMed] [Google Scholar]
- 64.Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol. 2005;161:81–8. doi: 10.1093/aje/kwi017. [DOI] [PubMed] [Google Scholar]
- 65.Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58:1929–52. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 66.Smith GD, Hart C. Re: “Use of census-based aggregate variables to proxy for socioeconomic group: evidence from national samples”SMITH1999. Am J Epidemiol. 1999;150:996–7. doi: 10.1093/oxfordjournals.aje.a010109. [DOI] [PubMed] [Google Scholar]
- 67.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91:1783–9. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55:125–39. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- 69.Robert SA. Socioeconomic position and health: The independent contribution of community socioeconomic context. Ann Rev Sociol. 1999;25:489–516. [Google Scholar]
- 70.Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “neighborhood effects”: Social processes and new directions in research. Annual Review of Sociology. 2002;28:443–78. [Google Scholar]
- 71.Zapka JG, Lemon SC. Interventions for patients, providers, and health care organizations. Cancer. 2004 Sep 1;101:1165–87. doi: 10.1002/cncr.20504. [DOI] [PubMed] [Google Scholar]
- 72.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff(Millwood) 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 73.Curtis S, Rees Jones I. Is there a place for geography in the analysis of health inequality? Sociology of Health and Illness. 1998;20:645–72. [Google Scholar]
- 74.O’Campo P. Invited commentary: Advancing theory and methods for multilevel models of residential neighborhoods and health. Am J Epidemiol. 2003;157:9–13. doi: 10.1093/aje/kwf171. [DOI] [PubMed] [Google Scholar]
- 75.Ananthakrishnan AN, Schellhase KG, Sparapani RA, Laud PW, Neuner JM. Disparities in colon cancer screening in the Medicare population. Arch Intern Med. 2007;167:258–64. doi: 10.1001/archinte.167.3.258. [DOI] [PubMed] [Google Scholar]
- 76.Hiatt RA. Behavioral research contributions and needs in cancer prevention and control: adherence to cancer screening advice. Prev Med. 1997 Sep-Oct;26:S11–8. doi: 10.1006/pmed.1997.0205. [DOI] [PubMed] [Google Scholar]
- 77.Meissner HI, Breen N, Coyne C, Legler JM, Green DT, Edwards BK. Breast and cervical cancer screening interventions: an assessment of the literature. Cancer Epidemiol Biomarkers Prev. 1998 Oct;7:951–61. [PubMed] [Google Scholar]
- 78.Rakowski W, Breslau ES. Perspectives on behavioral and social science research on cancer screening. Cancer. 2004 Sep 1;101:1118–30. doi: 10.1002/cncr.20503. [DOI] [PubMed] [Google Scholar]
- 79.Vernon SW, Briss PA, Tiro JA, Warnecke RB. Some methodologic lessons learned from cancer screening research. Cancer. 2004 Sep 1;101:1131–45. doi: 10.1002/cncr.20513. [DOI] [PubMed] [Google Scholar]
- 80.Blakely T, Subramanian SV, Oakes JM, Kaufman JS. Methods in social epidemiology. San Francisco, CA: Jossey-Bass; 2006. Multilevel studies; pp. 316–40. [Google Scholar]
- 81.Raudenbush SW, Sampson RJ. Ecometrics: Toward a science of assessing ecological settings, with application to the systematic social observation of neighborhoods. Sociological Methodology. 1999;29:1–41. [Google Scholar]
- 82.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures--the public health disparities geocoding project. Am J Public Health. 2003;93:1655–71. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156:471–82. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 84.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US) Journal of Epidemiology and Community Health. 2003;57:186–99. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures--the public health disparities geocoding project (US) Public Health Rep. 2003;118:240–60. doi: 10.1093/phr/118.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hyndman JC, Holman CD, Hockey RL, Donovan RJ, Corti B, Rivera J. Misclassification of social disadvantage based on geographical areas: comparison of postcode and collector’s district analyses. Int J Epidemiol. 1995;24:165–76. doi: 10.1093/ije/24.1.165. [DOI] [PubMed] [Google Scholar]
- 87.Lawson AB. Bayesian disease mapping: Hierarchical modeling in spatial epidemiology. Boca Raton, FL: CRC Press, Taylor & Francis Group; 2009. [Google Scholar]
- 88.Chaix B, Leyland AH, Sabel CE, et al. Spatial clustering of mental disorders and associated characteristics of the neighbourhood context in Malmo, Sweden, in 2001. Journal of Epidemiology and Community Health. 2006;60:427–35. doi: 10.1136/jech.2005.040360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chaix B, Merlo J, Chauvin P. Comparison of a spatial approach with the multilevel approach for investigating place effects on health: the example of healthcare utilisation in France. Journal of Epidemiology and Community Health. 2005;59:517–26. doi: 10.1136/jech.2004.025478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Franzini L, Ribble J, Spears W. The effects of income inequality and income level on mortality vary by population size in Texas counties. J Health Soc Behav. 2001;42:373–87. [PubMed] [Google Scholar]
- 91.Subramanian SV, Kawachi I. Income inequality and health: What have we learned so far? Epidemiologic Reviews. 2004;26:78–91. doi: 10.1093/epirev/mxh003. [DOI] [PubMed] [Google Scholar]
- 92.Rajaratnam JK, Burke JG, O’Campo P. Maternal and child health and neighborhood context: the selection and construction of area-level variables. Health Place. 2006;12:547–56. doi: 10.1016/j.healthplace.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 93.Feldman PJ, Steptoe A. How neighborhoods and physical functioning are related: the roles of neighborhood socioeconomic status, perceived neighborhood strain, and individual health risk factors. Ann Behav Med. 2004 Apr;27:91–9. doi: 10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- 94.Weden MM, Carpiano RM, Robert SA. Subjective and objective neighborhood characteristics and adult health. Soc Sci Med. 2008 Mar;66:1256–70. doi: 10.1016/j.socscimed.2007.11.041. [DOI] [PubMed] [Google Scholar]
- 95.Murray LA, Shatto AE. Dually eligible Medicare beneficiaries. Health Care Financing Review. 1998;20:131–40. [PMC free article] [PubMed] [Google Scholar]
- 96.Macintyre S, Maciver S, Sooman A. Area, Class and Health - Should We be Focusing on Places Or People. Journal of Social Policy. 1993;22:213–34. [Google Scholar]
- 97.Messer LC. Invited commentary: Beyond the metrics for measuring neighborhood effects. Am J Epidemiol. 2007;165:868–71. doi: 10.1093/aje/kwm038. [DOI] [PubMed] [Google Scholar]
- 98.Barrientos-Gutierrez T, Gimeno D, Mangione TW, Harrist RB, Amick BC. Drinking social norms and drinking behaviours: a multilevel analysis of 137 workgroups in 16 worksites. Occup Environ Med. 2007 Sep;64:602–8. doi: 10.1136/oem.2006.031765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Adler NE, Boyce T, Chesney MA, et al. Socioeconomic-Status and Health - the Challenge of the Gradient. American Psychologist. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- 100.Marmot MG, Shipley MJ, Rose G. Inequalities in death--specific explanations of a general pattern? Lancet. 1984 May 5;1:1003–6. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- 101.Hauser RM, Carr D. Measuring poverty and socioeconomic status in studies of health and well-being. Madison, WI: 1995. [Google Scholar]
- 102.Sampson RJ, Raudenbush SW. Seeing disorder: Neighborhood stigma and the social construction of “broken windows”. Social Psychology Quarterly. 2004 Dec;67:319–42. [Google Scholar]
- 103.Snijders TAB, Bosker R. An introduction to basic and advanced multilevel modeling. Thousand Oaks, CA: Sage; 1999. Multilevel analysis. [Google Scholar]
- 104.Blakely TA, Woodward AJ. Ecological effects in multi-level studies. Journal of Epidemiology and Community Health. 2000;54:367–74. doi: 10.1136/jech.54.5.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Subramanian SV. The relevance of multilevel statistical methods for identifying causal neighborhood effects - Commentary. Social Science & Medicine. 2004;58:1961–7. doi: 10.1016/S0277-9536(03)00415-5. [DOI] [PubMed] [Google Scholar]
- 106.Larsen K, Petersen JH, Budtz-Jorgensen E, Endahl L. Interpreting parameters in the logistic regression model with random effects. Biometrics. 2000;56:909–14. doi: 10.1111/j.0006-341x.2000.00909.x. [DOI] [PubMed] [Google Scholar]
- 107.Merlo J. Multilevel analytical approaches in social epidemiology: measures of health variation compared with traditional measures of association. Journal of Epidemiology and Community Health. 2003;57:550–2. doi: 10.1136/jech.57.8.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. Journal of Epidemiology and Community Health. 2006;60:290–7. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chaix B, Merlo J, Subramanian SV, Lynch J, Chauvin P. Comparison of a spatial perspective with the multilevel analytical approach in neighborhood studies: the case of mental and behavioral disorders due to psychoactive substance use in Malmo, Sweden, 2001. Am J Epidemiol. 2005;162:171–82. doi: 10.1093/aje/kwi175. [DOI] [PubMed] [Google Scholar]
- 110.Schootman M, Jeff DB, Gillanders WE, Yan Y, Jenkins B, Aft R. Geographic clustering of adequate diagnostic follow-up after abnormal screening results for breast cancer among low-income women in Missouri. Ann Epidemiol. 2007 Sep;17:704–12. doi: 10.1016/j.annepidem.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 111.Auchincloss AH, Diez Roux AV. A new tool for epidemiology: the usefulness of dynamic-agent models in understanding place effects on health. Am J Epidemiol. 2008 Jul 1;168:1–8. doi: 10.1093/aje/kwn118. [DOI] [PubMed] [Google Scholar]
- 112.Hiatt RA, Rimer BK. A new strategy for cancer control research. Cancer Epidemiol Biomarkers Prev. 1999 Nov;8:957–64. [PubMed] [Google Scholar]
- 113.Meissner HI, Smith RA, Rimer BK, et al. Promoting cancer screening: Learning from experience. Cancer. 2004;101:1107–17. doi: 10.1002/cncr.20507. [DOI] [PubMed] [Google Scholar]