Abstract
Aims
The purpose of this study was to (i) describe the weight, weight-related perceptions and lifestyle behaviours of hospital-based nurses, and (ii) explore the relationship of demographic, health, weight and job characteristics with lifestyle behaviours.
Background
The obesity epidemic is widely documented. Worksite initiatives have been advocated. Nurses represent an important part of the hospital workforce and serve as role models when caring for patients.
Methods
A sample of 194 nurses from six hospitals participated in anthropometric measurements and self-administered surveys.
Results
The majority of nurses were overweight and obese, and some were not actively involved in weight management behaviours. Self-reported health, diet and physical activity behaviours were low, although variable by gender, age and shift. Reports of co-worker norms supported low levels of healthy behaviours.
Conclusions
Findings reinforce the need to address the hospital environment and culture as well as individual behaviours for obesity control.
Implications for nursing management
Nurse managers have an opportunity to consider interventions that promote a climate favourable to improved health habits by facilitating and supporting healthy lifestyle choices (nutrition and physical activity) and environmental changes. Such efforts have the potential to increase productivity and morale and decrease work-related disabilities and improve quality of life.
Keywords: body mass index, hospital environment, hospital nurses, job satisfaction, nutrition, physical activity
Background
The obesity epidemic in the United States has been widely documented, with an estimated 32% of adults being overweight and 34% obese (Ogden et al. 2006). Maintaining a healthy weight and regular participation in associated dietary and physical activity behaviours are essential elements of good health. Health professionals not only benefit their own health via healthy lifestyles, but can serve as role models for and credible advisors to their patients (Pate et al. 1995). Nurse–patient relationships, which emphasize trust, communication and partnering represent a unique context for health promotion among patients (Rush & Kee 2005). With increased national attention focused on preventing and reducing obesity, the role of nurses as behaviour models is important to patients, families and the community (Rush & Kee 2005). Little is known about the personal eating and exercise patterns or obesity prevalence of the nursing workforce. Several studies have investigated job-related factors, such as nurse’s views of the work environment (Ulrich et al. 2005), stress in the workplace (New York State Education Department Office of the Professions 2003), job satisfaction (Zangaro & Soeken 2007), and shift patterns and their impact on the health of nurses (Wilson 2002). However, investigations of how these factors impact obesity and associated health behaviours in nurses are limited (Overgaard et al. 2004).
The purpose of this study was to: (i) describe the weight, weight-related perceptions and lifestyle behaviour profile of hospital-based nurses, and (ii) explore the relationship of demographic, health, weight and job characteristics with the lifestyle behaviours.
Methods
Setting and subjects
This study was conducted in six hospitals in central Massachusetts as part of a worksite intervention to promote healthy behaviours that prevent or reduce obesity (Zapka et al. 2007). Employees of diverse occupations participated in a baseline survey. Subjects for this report are the 194 nurses who participated. Nurse practitioners, who primarily work in out-patient clinics, were excluded.
Recruitment and data collection
A representative sample of employees from the work-force of the six hospitals was invited to participate. Current employees were identified through human resource records, and included information on gender, age, race/ethnicity and job title. Employees were stratified by gender and minority status within each hospital, and a random sample was selected from each stratum with oversampling of minority and male employees.
In congruence with the institutional review board-approved protocol, the following enrolment procedure was used. Selected employees received an invitation letter between March and December of 2005, signed by the study principal investigator and the hospital president. The letter explained the study and informed the employee they could telephone or email the project coordinator to set up an initial visit, ask questions or refuse participation. Employees who did not actively refuse were offered two alternatives for enrolment: individually scheduled appointments or drop-in sessions. Project staff contacted invitees via work telephone, pager or mail.
Responsive employees were then screened to determine eligibility. Criteria included: (i) age between 18 and 65 years; (ii) work at least 20 hours per week; (iii) work at only one participating hospital; (iv) intention to work for the next 2 years at the hospital; (v) understand and communicate in English or Spanish; and (vi) have no impediment to being weighed and measured (e.g. wheelchair bound).
Baseline data were collected at two time points within 6 months, as part of the longitudinal study design. The three data sources were human resource files, a 30-minute self-administered survey and anthropometric measurements (height, weight) taken using standardized protocols.
Measures
Demographic measures collected from human resource files or survey included age, gender, race/ethnicity, marital status and education. Health-related measures included self-reported smoking status and health (hypertension and high cholesterol) risk factors.
Weight-related measures included objective measurements and self-reported perceptions, receipt of advice and efforts. Body mass index (BMI) was calculated from measured height and weight obtained by trained research staff. For analysis, BMI is categorized according to the standard classification of normal (BMI < 25.0 kg/m2), overweight (BMI = 25.0 kg/m2–29.9 kg/m2) and obese (BMI ≥ 30.0 kg/m2). Participants were asked about their perception of their weight (underweight, just right, a little overweight, moderately overweight and very overweight). Additionally, they reported whether a health care provider had recommended they lose weight (yes/no) and whether they were currently trying to lose weight (yes/no).
Job characteristics included number of years at the hospital, hours worked per week, working a second job, shift (Wilson 2002), perceived stress of the job and the hospital environment, and overall job satisfaction.
Perception of worksite norms were measured in the survey using two summated scales (Lemon & Zapka 2007, Lemon et al. in press) adapted from the Worksite Health Climate Scale (Ribisl & Reischl 1993). Perception of organizational commitment to employee health was measured using four items, answered on a five-point scale (1–5) ranging from strongly disagree to strongly agree. Possible summated scores range from 4 to 20 on this scale. The second scale had two subscales related to employee perceptions of the eating (five items) and physical activity (four items) behaviours of co-workers. Items such as ‘how many co-workers regularly eat potato chips or candy bars for snacks’ had a 7 category response from ‘none’ to ‘all’. Possible summated scores ranged from 0 to 30 on the eating subscale and from 0 to 24 on the physical activity subscale.
Physical activity was assessed by the self-administered form of the work domain of the International Physical Activity Questionnaire (IPAQ) (Hallal & Victora 2004). The IPAQ, developed by the World Health Organization, has demonstrated reasonable psychometric properties in comparison to other self-reported physical activity measures. We report the work sub-score as the number of kilocalories per week. Other physical activity measures included number of flights of stairs walked up or down per day at work, and days per week that participants walked on break.
Measures for diet habits included fruit and vegetable and saturated fat consumption, measured by the Block Screeners (Block et al. 2000). These are brief food-frequency type measures that assess commonly eaten foods. Seven items ask about fruits and vegetables and 15 items about foods high in fat. Measures are reported in number of servings of fruits and vegetables per day and per cent calories from fat per day.
Data management and analyses
Analyses were weighted by the inverse of the stratum-specific sampling probability to account for the sampling design. To describe the population, frequency distributions were computed for categorical variables, and mean, standard deviation and quartile values were computed for continuous variables. For categorical variables, Pearson’s chi-square test was used to assess the level of association (Rosner 2006). Unadjusted relationships between demographic, health-, weight-and job-related variables and behaviour (diet and physical activity) were assessed, with behaviours being the dependent variables in single-variable regression models. The physical activity score was log transformed to approximate a normal distribution. Fruit and vegetable servings, percent fat and log of physical activity score were then assessed using linear regression. ‘Flights up per week’ and ‘flights down per week’ were modelled using Poisson’s regression because of the count nature of these data. ‘Days walking on break per week’ and ‘days parking farther away per week’ were categorized as either ‘0’or ‘1 or more’ and analysed using logistic regression. Data were analysed using Stata SE 9.1 software (Stata Corp, College Station, TX, USA).
Results
A total of 405 nurse employees were contacted to participate. Of these, 49 were judged ineligible, with the most frequent reasons being they were no longer employed, on extended leave, or worked fewer than 20 hours. Of the 356 eligible nurses, 194 (54.5%) consented to participate. Primary reasons offered for refusal included ‘not interested’, ‘no time’ or ‘conflicting demands’. Of the 194 who consented and completed baseline, 187 (97%) completed baseline part two.
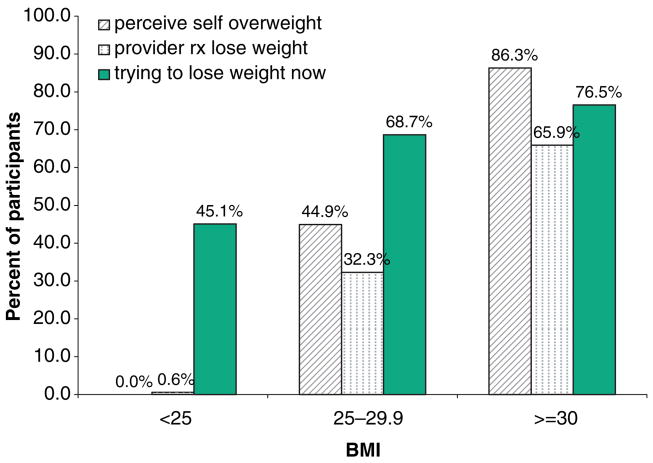
Table 1 reports the participants’ demographic characteristics. The range of educational status reflects the various types of nurses employed, such as licensed practical nurses, degree programme registered nurses and nurses with bachelors or masters training. Table 1 also reports the health- and weight-related measures. One-fifth of the participants reported having high cholesterol. With respect to BMI, 28% were classified as obese and 37% as overweight. While 30% reported a clinician had recommended they lose weight, a majority (62%) reported they were currently trying to lose weight. As illustrated in Figure 1, the participants’ reported perception of their weight was significantly associated with their BMI, as was their report that a clinician had recommended they lose weight, and current efforts to lose weight.
Table 1.
Participant personal characteristics (demographic, health and weight measures)
| Measure | % |
|---|---|
| Age | |
| ≤ 40 | 35.7 |
| 41–50 | 38.4 |
| >50 | 25.9 |
| Gender | |
| Female | 92.6 |
| Male | 7.4 |
| Race/ethnicity | |
| White | 93.5 |
| Other | 6.5 |
| Marital status | |
| Married (live together) | 74.9 |
| All others | 25.1 |
| Education | |
| 1–3 years college | 47.2 |
| College graduate+ | 52.8 |
| Hypertension | |
| Yes | 13.6 |
| High cholesterol | |
| Yes | 21.5 |
| Current smoker | |
| Yes | 5.9 |
| BMI | |
| <25 | 34.6 |
| 25–29.9 | 37.2 |
| ≥30 | 28.2 |
| Weight perception | |
| Under/just right | 18.8 |
| A little overweight | 42.0 |
| Moderately overweight | 24.2 |
| Very overweight | 15.0 |
| Clinician recommend weight loss | |
| Yes | 29.6 |
| Trying to lose weight | |
| Yes | 61.7 |
BMI, body mass index.
Figure 1.
Weight-related variables by BMI.
Table 2 reports the job-related measures for the participants. A substantial proportion (77%) had been employed at the hospital for more than 3 years. The majority (81% and 80%, respectively) agreed or strongly agreed that the work environment was stressful and that their job was stressful. Seventy-seven per cent, however, agreed or strongly agreed that they were satisfied overall with their job. Table 2 also reports the means, standard deviations and quartiles of the nurses’ perceptions of the environment health norms measures. Rating of perceived organizational support to health were modest, with a mean of 2.7 (SD = 0.70) out of a possible range of 1 to 5. Ratings of co-worker eating habits (mean = 3.3; SD = 0.74) were higher than ratings of co-worker physical activity behaviours (mean = 1.4; SD = 0.87).
Table 2.
Job-related measures
| Measure | % | ||||
|---|---|---|---|---|---|
| Years at hospital | |||||
| 0–3 | 22.9 | ||||
| 3.1–15.9 | 32.8 | ||||
| 16+ | 44.3 | ||||
| Hours work/week | |||||
| 20–35 | 57.4 | ||||
| 36+ | 42.6 | ||||
| Work second job | |||||
| Yes | 10.2 | ||||
| Shift | |||||
| First | 52.5 | ||||
| Second | 15.6 | ||||
| Third | 19.4 | ||||
| Split/mixed | 12.5 | ||||
| Work environment stressful | |||||
| SD/D/NS | 18.6 | ||||
| Agree | 45.8 | ||||
| Strongly agree | 35.6 | ||||
| Job stressful | |||||
| SD/D/NS | 19.8 | ||||
| Agree | 53.0 | ||||
| Strongly agree | 27.2 | ||||
| Overall satisfied | |||||
| SD/D/NS | 23.1 | ||||
| Agree | 60.5 | ||||
| Strongly agree | 16.4 | ||||
| Measure | Mean | SD | P25 | P50 | P75 |
|
| |||||
| Perceived environmental norms | |||||
| Organizational support | 2.73 | 0.705 | 2.25 | 2.75 | 3.25 |
| Co-worker eating | 3.25 | 0.742 | 2.8 | 3.2 | 3.6 |
| Co-worker activity | 1.43 | 0.867 | 1.0 | 1.5 | 1.75 |
Table 3 reports the diet and activity behaviors reported by the participants. The average servings of fruits and vegetables per day (4.0) was lower than government guidelines, and the average percentage of calories from fat (34.0%) was higher than government guidelines (US Department of Agriculture 2007). The range in number of flights walked up and down varied, and the vast majority did not walk on breaks.
Table 3.
Participant behaviours
| Measure | Mean | SD | P25 | P50 | P75 |
|---|---|---|---|---|---|
| Diet behaviours | |||||
| Fruit/vegetables per day | 4.0 | 1.5 | 3.3 | 4.0 | 4.8 |
| Per cent calories from fat | 34.0 | 4.8 | 31.1 | 34.1 | 37.1 |
| Activity behaviours | |||||
| IPAQ work sub-score(kcals/week) | 4961.8 | 5149.2 | 0 | 4237.9 | 7883.4 |
| Flights up/day | 2.82 | 3.37 | 0 | 2 | 4 |
| Flights down/day | 3.28 | 3.21 | 1 | 2 | 5 |
| Days/week walk on break | % | ||||
| None | 89.5 | ||||
| 1 or more | 10.5 | ||||
IPAQ, International Physical Activity Questionnaire.
Diet and physical activity behaviours were compared across the demographic, weight and job characteristics. Statistically significant findings are presented below. Men reported significantly more servings of fruits and vegetables per day, lower percentage of calories from fat, walking up and down more flights and were more likely to walk on breaks than women. Nurses over age 40 years were more likely to walk on breaks than younger women, and those who were not married consumed significantly less percentage of calories from fat. Nurses with more education were less likely to walk on breaks than those with less education. History of hypertension was associated with lower percentage of calories from fat. Those who perceived themselves as overweight reported fewer fruit and vegetable servings than those who perceived themselves as just right or underweight. The difference was significant for those who perceive themselves to be ‘a little overweight’ (P = 0.03), and was marginally significant for those who perceive themselves to be ‘very overweight’ (P = 0.08).
Those working the 3rd or split shifts reported significantly fewer flights up and down. Respondents who had BMI ≥ 30 or reported being very overweight reported significantly fewer flights up. Those working over 36 hours per week consumed a lower percentage of calories from fat. Those who strongly agreed that their job is stressful reported significantly more servings of fruits and vegetables than those who disagreed or were unsure about job stress. Those with more job stress also reported greater work-related calories expended. Those reporting a more stressful work environment reported greater work-related calories expended and more flights up. Nurses reporting higher perceived co-worker activity reported lower percent of calories from fat, were more likely to walk on breaks and reported greater work-related calories expended. Otherwise, there were few significant differences with respect to perceived environmental norms.
Discussion
A better understanding of nurses’ weight and work is important from three perspectives: the individual’s health and well-being, the organization’s interest to foster a healthy workforce and nurses’ potential to serve as health role models for patients. Concerns have been expressed about the nursing shortage, downsizing, long working hours (Trinkoff et al. 2006a,b) and stressful conditions (Shader et al. 2001, Trinkoff et al. 2006a,b, Zangaro & Soeken 2007). This study contributes information about individual nurse’s behaviours, as well as about important assessments of their work environment.
From a human resources perspective, attention to obesity management is prudent and ‘good business’. Increased disability, decreased quality of life, increased use of the health care system, decreased workplace productivity and increased absenteeism lead to higher costs to businesses and society, and obesity is one factor in these issues (Thompson 2007). The increase in back-related injuries related to being obese include the poor body mechanics resulting from not being able to hold heavy items close to the body when lifting, and overweight and obesity also impact productivity, performance, attendance and fitness to work (Thompson 2007).
The respondents to this survey reflected selected characteristics of the national nursing workforce, according to the National Sample Survey of Registered Nurses (US Department of Health and Human Services; Health Resources and Services Administration; Bureau of Health Professions 2004). For example, nationwide approximately 5.8% of registered nurses are men, compared with 7.4% of this study population. The average age of nurses nationally is 46.8 years, compared with 44.7 in this study. There are a substantial proportion of nurses nationwide with education at the college plus level, as was observed in this study.
Nurses in this study had a rate of overweight and obesity that is similar to the general US adult population (Ogden et al. 2006). This highlights the importance of improving the eating and activity behaviours of this potential pool of health role models (Goel & McIsaac 1999).
Participant report that a health care provider had recommended weight loss was significantly related to BMI, yet 34% of obese participants did not report that a clinician had suggested they lose weight. Perhaps physicians are less likely to provide this type of counselling to patients who they feel should ‘know better’. This could, however, be viewed as a missed opportunity, given the growing evidence about the effectiveness of patient-centred counselling during routine medical encounters (Zapka 1999, Serdula et al. 2003, Glasgow et al. 2006).
While respondents’ perception of being overweight was directly related to measured BMI, a proportion of overweight and obese nurses do not perceive themselves as such. Report of effort to lose weight was also significantly related to BMI (P < 0.01), although 45% of those with a BMI < 25 reported they are currently trying to lose weight suggesting less than optimal motivation, self-efficacy and/or skill to manage weight (Hoppe & Ogden 1997, Piazza et al. 2001). Focusing on those who are not trying to lose weight among BMI ≥ 25 represents a challenge to intervention and message design.
According to the National Sample Survey of Registered Nurses (US Department of Health and Human Services; Health Resources and Services Administration; Bureau of Health Professions 2004), 52.5% of hospital-based nurses reported in 2004 being moderately or extremely satisfied with their jobs. Although the samples of the national study and this study are not directly comparable, a high proportion in this sample (77%) reported they agreed or strongly agreed they were satisfied with their job overall. This is interesting particularly in view of the reports of work environment and job stress. In a 2002 survey of New York State registered nurses, nurses in hospitals and nursing homes reported highest levels of both workload stress and stress frequency (2/3 of sample) (New York State Education Department Office of the Professions 2003).
In this study, we found that work characteristics, including reported job stress and overall satisfaction, were not related to BMI (data not shown). Brunner et al. (2007) found that chronic work stress predicts general and central obesity, but Overgaard et al. (2004) in a review of 10 studies concluded data were not supportive of an association between psychological workload and general and central obesity. Our results support this conclusion, as respondents reporting greater job stress and a stressful work environment reported healthier eating and activity patterns.
Certainly other work-related issues not studied may impact nurses’ efforts to increase physical activity during the work day. For example, low back pain is common among nurses. Additionally, nurses may feel that on-the-job walking is substantial and perhaps a hazard. One study found that hospital nurses walked 4–5 miles during a 12-hour shift and 1/3–1/2 mile per hour worked, although somewhat variable by shift and number of assigned patients (Welton et al. 2006). Perceived activity and benefits/hazards warrant further study.
Nurses also encounter situations which may work against their best intentions. For example, patients often want to show their appreciation for the care they have received during a hospitalization. Families may bring in cookies, other foodstuffs or boxes of candy. Cheung (2003) surveyed nursing staff and found that nursing staff averaged 5.4 chocolates each day, and the explanation for consumption was as simple as the fact that they were there. One-third recognized the detrimental effect on their well-being while twenty-five per cent would have been pleased to receive a healthier alternative (Cheung 2003).
There are several limitations to this study. The response rate of 54% may reflect selection bias. Additionally, respondents come from a small number of hospitals from one geographical area, so findings may have limited generalizability. As with all self-reports of lifestyle behaviours, responses may reflect recall error or social desirability bias. A strength of this study was that BMI was physiologically measured, not self-reported, as surveys suffer from inaccuracy and underestimate obesity (Ezzati et al. 2006). Certainly, other factors besides those in the work environment impact lifestyle behaviours, including community factors, the home environment, and social support and interaction (Newey & Hood 2004, Allison 2005), and these are not addressed in this analysis.
Implications for research and practice
The workplace offers a setting in which to try to reverse the trends towards increasing rates of overweight and obesity and, more importantly, to create an environment which prevents weight gain (Thompson 2007). While it is the individuals’ choice to increase their physical activity, improve diet and maintain a healthy weight, the employer and managers can facilitate these healthy choices by providing a supportive working environment (Chambers et al. 2007, Thompson 2007).
While many weight and lifestyle interventions emphasize an individual focus, system-level innovations are key. This has been seen in comprehensive programmes to improve work safety (Grosch et al. 1999). Policy strategies could consider flexible schedules to promote walking on breaks, reassessing staffing patterns and ratios to ensure adequate time and staffing to release nurses from the units for breaks and meals and policies prohibiting unhealthy foods to be eaten in view of patients. Hospital-offered food options should also be a target for change. Administrators can advocate and endorse the offering of healthy options and portion sizes from machine vendors and hospital cafeteria (Zapka et al. 2007). Strategies that provide access and information include seasonal farmer’s markets, healthy nutrition and physical activity newsletters/posters emphasizing healthy choices and the role of nurses as health role models, ‘free’ snacks of seasonal fresh fruit and/or whole grain products on the work units and reasonably priced ‘to go’ box lunches/meals that can be delivered to busy work units. Onsite fitness centres that offer availability of equipment and classes before and after shifts, with adequate locker room space conducive to showering, and promotions by local fitness facilities that offer discounts for hospital workers could improve leisure-time activity. Stairwell improvement initiatives might include carpeting, music and inspirational posters or changing/rotating artwork featuring local artists, themes, or employees’ art work to encourage stair walking. Activities that build social support and camaraderie among nursing staffs, such as offering incentives for team weight loss, should also be considered.
In summary, this study confirmed that a large proportion of nurses were overweight or obese and many were not involved in weight management behaviours. Further, poor diet and physical activity patterns were supported by perceived co-worker norms. Given the importance of the nursing profession as role models to patients, families and the community, as well as their importance in the health care workforce, health care organizations can be leaders in encouraging a systems approach to obesity prevention. A variety of activities supported by leadership at the organizational and work unit levels will reinforce awareness of healthy habits, build social support and encourage individual behaviours.
Ethical approval
A sample was selected from human resources records. Selected employees were mailed an invitation letter between March and December of 2005, signed by the study principal investigator and the hospital president. The letter explained the study and informed the employee they could telephone or email the project coordinator to set up an initial visit, ask questions or refuse participation. Employees who did not actively refuse were offered two alternatives for enrolment; individually scheduled appointments or drop-in sessions. Project staff contacted invitees via work telephone, pager or mail. This research was approved by the Institutional Review Board of the University of Massachusetts Medical School.
Acknowledgments
This research was funded by Grant Number R01 HL079483-01 from the National Institutes for Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Heart, Lung and Blood Institute. The authors would like to thank Victoria Andersen, MS, RD, Amy Borg, MPH, MEd, Denise Jolicoeur, MPH, CHES and Barbara Estabrook, MSPH, CHES for their contributions to intervention development; Kathy Leung, MS for conducting data management; Wenjun Li, PhD for statistical consultation; Betsy Costello for conducting recruitment and assessments, and Christine Foley for conducting recruitment and assessments and assistance with manuscript preparation.
References
- Allison S. Biographic and psychobehavioral influences on body mass index in a nursing sample. Western Journal of Nursing Research. 2005;27(1):7–20. 21–7. doi: 10.1177/0193945904265404. [discussion] [DOI] [PubMed] [Google Scholar]
- Block G, Gillespie C, Rosenbaum EH, Jenson C. A rapid food screener to assess fat and fruit and vegetable intake. American Journal of Preventive Medicine. 2000;18(4):284–248. doi: 10.1016/s0749-3797(00)00119-7. [DOI] [PubMed] [Google Scholar]
- Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II Study. American Journal of Epidemiology. 2007;165(7):828–837. doi: 10.1093/aje/kwk058. [DOI] [PubMed] [Google Scholar]
- Chambers RL, Turner LW, Hunt SB. Application of ecological models to risks related to being overweight among nurses. Psychological Reports. 2007;100(3 Pt 1):815–816. doi: 10.2466/pr0.100.3.815-816. [DOI] [PubMed] [Google Scholar]
- Cheung ST. The effects of chocolates given by patients on the well-being of nurses and their support staff. Nutrition and Health (Berkhamsted, Hertfordshire) 2003;17(1):65–69. doi: 10.1177/026010600301700108. [DOI] [PubMed] [Google Scholar]
- Ezzati M, Martin H, Skjold S, Vander Hoorn S, Murray CJ. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. Journal of the Royal Society of Medicine. 2006;99(5):250–257. doi: 10.1258/jrsm.99.5.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Emont S, Miller DC. Assessing delivery of the five ‘As’ for patient-centered counseling. Health Promotion International. 2006;21(3):245–255. doi: 10.1093/heapro/dal017. [DOI] [PubMed] [Google Scholar]
- Goel V, McIsaac W. Health promotion in clinical practice. In: Poland B, Green LW, Rootman I, editors. In Settings for Health Promotion: Linking Theory and Practice. Sage Publications; Thousand Oaks, CA: 1999. pp. 217–241. [Google Scholar]
- Grosch JW, Gershon RR, Murphy LR, DeJoy DM. Safety climate dimensions associated with occupational exposure to blood-borne pathogens in nurses. American Journal of Industrial Medicine. 1999;36(Suppl 1):122–124. doi: 10.1002/(sici)1097-0274(199909)36:1+<122::aid-ajim43>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Hallal PC, Victora CG. Reliability and validity of the International Physical Activity Questionnaire (IPAQ) Medicine & Science in Sports & Exercise. 2004;36(3):556. doi: 10.1249/01.mss.0000117161.66394.07. [DOI] [PubMed] [Google Scholar]
- Hoppe R, Ogden J. Practice nurses’ beliefs about obesity and weight related interventions in primary care. International Journal of Obesity and Related Metabolic Disorders. 1997;21(2):141–146. doi: 10.1038/sj.ijo.0800379. [DOI] [PubMed] [Google Scholar]
- Lemon S, Zapka J, Li W. Multi-Level Associations with Body Mass Index in an Ecological Intervention Promoting Weight Control among Hospital Employees. American Academy of Health Behavior Annual Meeting; Savannah, GA: 2007. [Google Scholar]
- Lemon S, Zapka J, Li W, Estabrook B, Magner R, Rosal MC. Perceptions of supportive worksite environments and body mass index, physical activity and eating behaviors among hospital employees. American Journal of Health Behavior. 2008 (in press) [Google Scholar]
- New York State Education Department Office of the Professions. Registered Nurses in New York State, 2002. Volume II: Organizational Climate Factors, Organizational Commitment, and the Culture of Retention. USNY State Education Department, Office of the Professions and Fiscal Analysis and Research Unit; Albany, NY: 2003. [Google Scholar]
- Newey CA, Hood BM. Determinants of shift-work adjustment for nursing staff: the critical experience of partners. Journal of Professional Nursing. 2004;20(3):187–195. doi: 10.1016/j.profnurs.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Overgaard D, Gyntelberg F, Heitmann BL. Psychological workload and body weight: is there an association? A review of the literature. Occupational Medicine (Oxford, England) 2004;54(1):35–41. doi: 10.1093/occmed/kqg135. [DOI] [PubMed] [Google Scholar]
- Pate R, Pratt M, Blair S, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. Journal of the American Medical Association. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- Piazza J, Conrad K, Wilbur J. Exercise behavior among female occupational health nurses. Influence of self efficacy, perceived health control, and age. AAOHN Journal: Official Journal of the American Association of Occupational Health Nurses. 2001;49(2):79–86. [PubMed] [Google Scholar]
- Ribisl KM, Reischl TM. Measuring the climate for health at organizations. Development of the worksite health climate scales. Journal of Occupational Medicine. 1993;35(8):812–824. doi: 10.1097/00043764-199308000-00019. [DOI] [PubMed] [Google Scholar]
- Rosner B. Fundamentals of Biostatistics. Thomson Publishers; Belmont, CA.: 2006. [Google Scholar]
- Rush KL, Kee CC, Rice M. Nurses as imperfect role models for health promotion. Western Journal of Nursing Research. 2005;27(2):166–183. 184–187. doi: 10.1177/0193945904270082. [discussion]. [DOI] [PubMed] [Google Scholar]
- Serdula MK, Khan LK, Dietz WH. Weight loss counseling revisited. Journal of the American Medical Association. 2003;289(14):1747–1750. doi: 10.1001/jama.289.14.1747. [DOI] [PubMed] [Google Scholar]
- Shader K, Broome ME, Broome CD, West ME, Nash M. Factors influencing satisfaction and anticipated turnover for nurses in an academic medical center. The Journal of Nursing Administration. 2001;31(4):210–216. doi: 10.1097/00005110-200104000-00010. [DOI] [PubMed] [Google Scholar]
- Thompson DL. The costs of obesity: what occupational health nurses need to know. AAOHN Journal: Official Journal of the American Association of Occupational Health Nurses. 2007;55(7):265–270. doi: 10.1177/216507990705500702. [DOI] [PubMed] [Google Scholar]
- Trinkoff A, Geiger-Brown J, Brady B, Lipscomb J, Muntaner C. How long and how much are nurses now working? The American Journal of Nursing. 2006a;106(4):60–71. 72. doi: 10.1097/00000446-200604000-00030. [quiz] [DOI] [PubMed] [Google Scholar]
- Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J, Lang G. Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. American Journal of Industrial Medicine. 2006b;49(11):964–971. doi: 10.1002/ajim.20330. [DOI] [PubMed] [Google Scholar]
- Ulrich BT, Buerhaus PI, Donelan K, Norman L, Dittus R. How RNs view the work environment: results of a national survey of registered nurses. The Journal of Nursing Administration. 2005;35(9):389–396. doi: 10.1097/00005110-200509000-00008. [DOI] [PubMed] [Google Scholar]
- US Department of Agriculture. [[accessed on 12 October 2007]];Dietary guidelines for Americans 2005 – key recommendations for the general population. 2007 [WWW document]. URL http://www.health.gov/dietaryguidelines/dga2005/recommendations.html.
- US Department of Health and Human Services; Health Resources and Services Administration; Bureau of Health Professions. The Registered Nurse Population: Findings from the March 2004 National Sample Survey of Registered Nurses. US Department of Health and Human Services; Bethesda, MD: 2004. [Google Scholar]
- Welton JM, Decker M, Adam J, Zone-Smith L. How far do nurses walk? Medsurg Nursing. 2006;15(4):213–216. [PubMed] [Google Scholar]
- Wilson JL. The impact of shift patterns on healthcare professionals. Journal of Nursing Management. 2002;10(4):211–219. doi: 10.1046/j.1365-2834.2002.00308.x. [DOI] [PubMed] [Google Scholar]
- Zangaro GA, Soeken KL. A meta-analysis of studies of nurses’ job satisfaction. Research in Nursing & Health. 2007;30(4):445–458. doi: 10.1002/nur.20202. [DOI] [PubMed] [Google Scholar]
- Zapka J. On finding common ground – health promotion in clinical practice. In: Poland B, Green LW, Rootman I, editors. In Settings for Health Promotion: Linking Theory and Practice. Sage Publications; Thousand Oaks, CA: 1999. pp. 242–249. [Google Scholar]
- Zapka J, Lemon S, Estabrook B, Jolicoeur D. Keeping a step ahead – formative phase of a workplace intervention trial to prevent obesity. Obesity. 2007;15:27S–36S. doi: 10.1038/oby.2007.385. [DOI] [PMC free article] [PubMed] [Google Scholar]