Abstract
Objective
Document working mothers infant feeding practices, and delineate factors that may shape infant feeding.
Methods
Cross-sectional data were obtained from a community sample of working women with 8 month-old infants (n=199).
Results
Nearly all working mothers used commercially prepared foods like infant cereals, fruits, and vegetables. Approximately one-fifth fed infants French Fries, sweetened beverages, and sweetened deserts. Unhealthy infant feeding was elevated among unmarried mothers and those with less education, and those with nonstandard work schedule.
Conclusions
Working mothers use commercially prepared foods for infant feeding. Socially disadvantaged working mothers’ infant feeding may pose health and developmental risks.
Keywords: Infant feeding, maternal employment, work-family, infant health, nonstandard work schedules
INTRODUCTION
Feeding patterns during infancy have several health-related implications. In the short term, the introduction of some foods such as nuts and seeds are choking hazards,1 and they along with shellfish, and eggs can produce allergic reactions.2–4 In many cases reactions may be minor, but in some cases they are severe producing substantial family distress and potentially death. In the longer term, food choices and nutrition affect growth and development,5,6 and they may influence long term food preferences and health outcomes. 7–11 Infants given sugared beverages develop greater preference for sweetened beverages later in life,12 and heavy frequent use of sugared beverages increases preference for these beverages.13 Children’s consumption of sweetened beverages may contribute to pediatric obesity,14–16 although this link is not firmly established.17–19
Despite its importance, surprisingly little is known about what infants are fed. Most infant feeding research has emphasized consumption of breast milk, formula, and cow’s milk, or it has emphasized the introduction of specific types of solid food. Estimates from the Infant Feeding Practices Study II (IFPS II) indicated that use of breast milk declines across the first year while use of formula increases, and that nearly 20% of women fed their infants cow’s milk before the one-year mark recommended by the American Academy of Pediatrics.20 Further, estimates from the IFPS II indicated that one-quarter of mothers were feeding their infants French fries as well as candy, cookies or cakes by the time infants were one year old.20 Similar results were obtained from the earlier Feeding Infants and Toddlers Study (FITS) which concluded that too many infants were being fed cow’s milk prior to one year of age, and that a concerning percentage of infants were being fed foods containing excess sugar (eg, fruit juices, sugar sweetened beverages) and not being fed fruits and vegetables.21 These and other estimates from the IFPS II and the FITS22 suggest that infant feeding during the infants’ first year is complex, and that the diet of a substantial proportion of infants may create long-term health or developmental problems.
Maternal employment likely shapes infant feeding. Nearly twice as many mothers of infants are engaged in the labor force today compared to 30 years ago.23 Employed mothers working 30 or more hours per week are less likely to initiate and sustain exclusive breast feeding.24–26 Working mothers have been found to rely heavily on commercial and pre-packaged food sources27,28 for family meal planning, and that they are increasingly reliant on commercially prepared foods from restaurants or other take-and-go meal purveyors, which are typically more calorie dense.29 Working mothers confront substantial time demands,30 which may translate into systematic differences in the types of foods fed to infants. Despite the substantial demands and challenges confronted by working mothers research to date has focused primarily on the extent to which employment interferes with breastfeeding: there has been no research documenting feeding patterns used by working mothers beyond breast versus formula feeding. Research on working mothers infant feeding behavior is needed, especially during the second half of infants’ first year when new foods are introduced and infant feeding becomes increasingly more complex.20–21
The goal of this study is to expand understanding of the potential role of maternal employment in infant feeding. To achieve this goal, this study accomplishes 2 specific aims. First, this study documents the types of food fed to 8 month-old infants of working mothers. The focus on 8 month-old infants captures a period of development when infants remain exclusively dependent on caregivers for feeding while the types of food is rapidly expanding. Published estimates from the IFPS II20 and the FITS,21 both national samples containing data from employed and non-employed mothers, are used to contextualize estimates obtained from our sample of mothers who are employed full-time. We then delineate the individual and work-related characteristics associated with selected feeding behaviors that pose potential health or developmental threats to children including sugar-sweetened beverages, French fries, starches, and foods implicated in allergies (ie, nuts and seeds, eggs, and fish and shellfish).
METHODS
The data for this study were from a community-based sample of employed mothers of newborns in Forsyth County, NC (Winston-Salem). The study was designed to document the strategies employed mothers use to balance their work and family lives, and to determine if variation in mothers’ strategies for combining work and family contribute to differences in women’s and infants health. Data were collected at 4 points: when infants were 4, 8, 12, and 16 months of age. Infant feeding was assessed only during the 8-month assessment; consequently only data collected at baseline (descriptive characteristics) and the 8-month assessment (infant feeding) were used in this analysis.
Sampling
The goal of this study was to create a sample of full-time working mothers in Forsyth County, NC reflecting the general racial composition of the county. A sample frame was constructed because no pre-existing lists of new mothers, particularly new mothers working 30 or more hours per week, exist. All infants born in Forsyth County receive care through a single mother-infant unit at one local hospital during the first week of life. A member of the investigative team monitored the daily census of the mother-infant unit and identified mothers who were 18 years of age or older, resided in Forsyth County, and reported working during pregnancy. Criteria were obtained from each patient’s electronic medical record. Identified women were approached in their hospital room after their infant was born but prior to discharge to briefly introduce the study and identify whether the mother was willing to be contacted within the following 3 months. A total of 704 mothers were approached, 630 (89%) provided approval for subsequent contact. No racial or ethnic differences were present in the proportion of women granting approval for subsequent contact
Recruitment
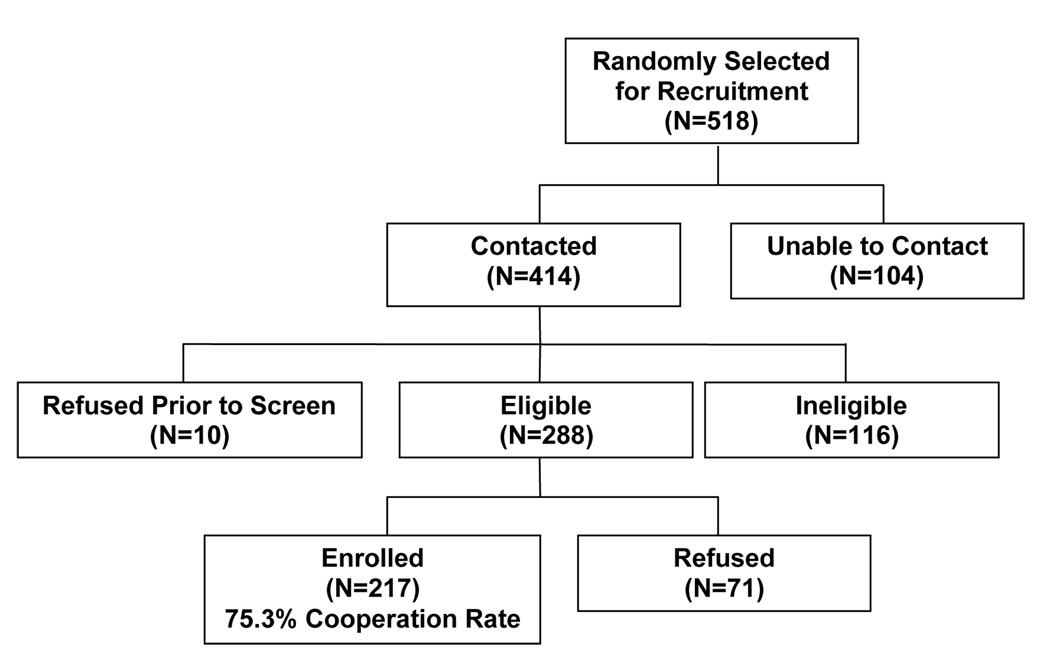
Five hundred eighteen mothers were randomly selected for contact and potential recruitment. To be eligible for the study women needed to be 18 years of age, currently working at least 30 hours per week, or planning to return to work 30 or more hours per week by 4 months post-partum (when their infant was 4 months old). Women whose child had a special health care need were excluded from the study. Overall recruitment success is illustrated in Figure 1. By way of summary, 104 of the randomly selected mothers were unreachable. Of the 414 contacted women, 10 refused to participate before determining eligibility, and 116 mothers were determined ineligible primarily because they decided not to return to work within 4 months post-partum (n=51) or they worked less than 30 hours per week (n=47). Of the 288 eligible mothers, 217 agreed to participate and completed a baseline interview. Power calculations indicated that the initial sample of 217 participants would have 80% power to achieve the overall aims of the broader project. The overall cooperation rate among study-eligible mothers was 75.3%. Of the 217 enrolled participants, 199 were re-interviewed at the 8 month interview (91.7%)
Figure 1.
Summary of Sampling and Recruitment
Sample
Study participants were, on average, 30 years of age (SD=5.6). By design, 30% (n=65) of the sample was Black and the remaining participants were non-Hispanic white. The vast majority of participants (77.0%) were married or in a marriage-like relationship. The largest proportion of mothers reported having a trade degree or some college education (34.1%), but several mothers had either a college (28.6%) or a post-graduate degree (18.4%). However, nearly one-fifth (18.9%) of mothers had not completed high school. By design, mothers work hours per week averaged 39.5 (SD=6.5). Infants of study participants were 34.9 weeks (8.1 months) of age and predominantly boys (53.8%). For 42.4% of participants the infant was their first child, while 39.2% had one other child, and the remainder had 2 or more other children.
Data collection
Data were obtained via interviewer-administered survey questionnaires. All data were collected by a team of 6 trained interviewers. Over 10% of participants were recontacted for purposes of quality control to verify key data elements from completed interviews. No cases of falsified data have been identified.
Measures
Infant feeding
Measures of infant feeding were obtained from survey items originally developed for the Infant Feeding Practices Study (IFPS) II, conducted jointly by the Food and Drug Administration and Centers for Disease Control and Prevention.31 Specifically, items included in the IFPS assessments asked participants how frequently (per day or per week) infants were fed a variety of foods, including milks, dairy products, fruits and vegetables, meats, and sweets. In the present study, IFPS items were modified so mothers were asked whether they had fed each type of food at any point in the past 7 days. Affirmative responses for each food type were coded one; zero otherwise. For a select group of foods (ie, fruit juice, fruits, vegetables, and meats, chicken and combination dinners) affirmative responses were also probed to determine if these foods were sold as specially designed for babies. For each of these foods, categorical variables were created reflecting “none,” “fed non-infant food,” and “fed infant food”.
Individual characteristics
Maternal age was categorized based on sample tertiles (< 27, 28–33, and > 34). Tertiles were used to avoid the assumption of a linear association of age with infant feeding practices while also capturing identifiable groups (eg, younger versus older) with sufficient cell sizes to support analyses. Race was dichotomized such that Black women were coded 1, zero otherwise. Education was also dichotomized such that mothers who graduated from college were coded 1 whereas those with less than a college degree were coded zero. Sensitivity analyses indicated that results for education did not differ depending on whether it was divided into 2, 3 or 4 discrete categories, so the dichotomous variable was used for parsimony. Marital/partner status was coded such that those who were married or in marriage-like relationship were coded 1, zero otherwise), and household income was dichotomoized such that those whose household income was below the federal poverty line for their household size coded 1, zero otherwise.
Employment characteristics
Work hours was assessed in terms of the total number of hours per week worked on all jobs, and then categorized (ie, <40, 40 – 44, > 44). Work schedule was assessed by 2 questions, the first asking the days of the week women reported typically working and the second asking the hours of the day typically worked. Responses were used to create a dichotomous indicator of work schedule where the code of one reflected having a nonstandard schedule job as indicated by working weekend days, evening or night hours, or having a variable schedule in terms of days of the week or times. All other women were coded zero, representing a standard work schedule or a Monday thru Friday, 8 to 5 type schedule. Schedule control was assessed with a validated, 7-item instrument asking how often the individual is able to have influence over different aspects of their work schedule (eg, “The length of your workday “ or “The scheduling of your work shifts “.32 Response options ranged from “not at all” (1) to “always” (5). Responses were summed (α = 0.80) and then categorized based on sample tertiles. Physical job demand was assessed with 5 items from the Job Content Questionnaire asking whether participants’ jobs required different levels of exertion (eg, “I am often required to move or lift very heavy loads on my job.”) or awkward postures (eg, “I am required to work for long periods with my head or arms in physically awkward positions.”).33 Response options ranged from “strongly disagree” (1) to “strongly agree” (4). Items were summed and categorized based on sample tertiles.
Analyses
Infant feeding practices were described with counts and frequencies. To contextualize the description of infant feeding practices, we provide comparative data using estimates from IFPS II20 for 7.5 month old infants (n=1990) and the FITS for 7 – 8 month old infants (n=483).21 The IFPS II is a longitudinal cohort of women who were identified through a consumer opinion panel as being pregnant, and were followed for up to one year postpartum.31 The FITS is a general population sample of new mothers.34 Comparisons with the IFPS II and the FITS need to be made carefully as the level of maternal employment after birth, as well as the timing and intensity (ie, hours per week) of employment among working mothers in these studies have not yet been reported.
Bivariate associations of individual and employment characteristics with infant feeding practices were examined by fitting a series of simple logistic regression models. All individual and employment characteristics that were significantly associated with an infant feeding practice (P<.05) were then advanced to a multivariate model. Backward selection was used in the final multivariate logistic regression models to avoid over-fitting the model and conserve degrees of freedom. The backward selection used a Wald chi-square significance level of 0.1 for an effect to remain in the model. Odds ratios and corresponding 95% Wald confidence intervals were calculated for the final predictors in each model.
RESULTS
The vast majority of participants feed their infants a few core food staples (Table 1). Over fourth-fifths reported feeding their infants formula (86.4%), while nearly all participants reported feeding fruits (92.0%), vegetables (93.4%) and cereal (92.4%) that are specifically designed for infants. Approximately one-half of participants reported feeding their children dairy products other than milk (50.8%), such as cheese, yogurt or ice cream. A similar percentage reported feeding their infants juices (51.8%) as well as meat, chicken and combination dinners (57.7%) specifically packaged for infants. Approximately one in 4 mothers (23.7%) fed their infants breast milk. Only 13.6% (n=27) reported exclusive breast feeding without formula supplementation. Approximately one in 5 mothers (22.2%) reported feeding their infant French fries, while a similar percentage (18.4%) reported feeding their infants sweetened beverages such as Kool-Aid and soda, or other sweets such as candy, cookies, and cake (22.3%). Approximately one in 5 participants reported feeding their infants foods frequently associated with food allergies such as eggs (17.7%), peanut butter or other nuts (5.6%), or fish or shellfish (2.5%).
Table 1.
The Percentage of 8-month Old Infants Being Fed Different Types of Foods (N=199)
| Employed | Comparative Data | |||
|---|---|---|---|---|
| Mothers | IFPS IIa | FITS b | ||
| Food | % | (n) | % | % |
| Breast milk | 23.7% | (47) | 45.9% | 25.7% |
| Infant formula | 86.4% | (171) | 68.9% | 74.1% |
| Dairy Products | ||||
| Cow’s milk | 3.5% | (7) | 1.5% | 2.9% |
| Other milk (soy, goat) | 4.5% | (9) | 1.0% | 0.5% |
| Other dairy (cheese, yogurt, ice cream) | 50.8% | (101) | 14.5% | 9.4% |
| Fruits & Vegetables | ||||
| Juices | ||||
| None | 35.0% | (69) | n/a | n/a |
| Non-infant juices | 13.2% | (26) | n/a | n/a |
| Infant juices | 51.8% | (102) | 50.3% | n/a |
| Fruit | ||||
| None | 1.5% | (3) | n/a | 24.5% |
| Non-infant fruits | 6.5% | (13) | n/a | 14.3% |
| Infant fruits | 92.0% | (183) | 91.3% | 67.9% |
| Vegetables | ||||
| None | 0.5% | (1) | n/a | 34.5% |
| Non-infant vegetables | 6.1% | (12) | n/a | 19.0% |
| Infant vegetables | 93.4% | (185) | 92.7% | 54.5% |
| French Fries | 22.2% | (44) | 3.8% | 2.9% |
| Grains | ||||
| Infant cereal | 92.4% | (183) | 86.2% | 81.2% |
| Other starches (eg, crackers, teething biscuits) | 73.1% | (144) | 39.3% | 51.8% |
| Meats or Proteins | ||||
| Meat, chicken or combination dinners (MCCD) | ||||
| None | 37.2% | (73) | n/a | 56.7% |
| Non-infant MCCD | 5.1% | (10) | n/a | 4.6% |
| Infant MCCD | 57.7% | (113) | 47.2% | 39.8% |
| Other protein sources | ||||
| Eggs | 17.7% | (35) | 4.5% | 2.9% |
| Peanut butter, nuts, and seeds | 5.6% | (11) | 0.6% | 0.5% |
| Fish and shellfish | 2.5% | (5) | 1.0% | 0.5% |
| Sweets and drinks | ||||
| Sweetened beverages (eg, Kool-Aid, soda) | 18.4% | (36) | 4.2% | 7.5% |
| Candy, cookies, or cake | 22.3% | (44) | 3.9% | 9.7% |
Estimates from the Infant Feeding Practices Study II (IFPS II) are for 7.5 month old infants (n=1,990) abstracted from Grummer-Strawn and colleagues.20
Estimates from the Feeding Infants and Toddlers Study (FITS) are for 7−8 month old infants (n=483) abstracted from Fox and colleagues.21 Percentages within food groups may not total 100% because categories are not mutually exclusive.
Infant feeding practices of working mothers in this sample are notably different from mothers in the IFPS II and the FITS samples. Use of any breast milk is similar for mothers in our sample and those in the FITS; however, fewer mothers in the current study than the IFPS II fed their infant breast milk. Over fourth-fifths (86.4%) of working mothers in this sample reported using formula. By contrast fewer approximately 70% of women in the IFPS II and the FITS used formula. A similar percentage of mothers in our sample of working mothers and those in the IFPS II fed their infants fruit juices, fruits, and vegetables specifically designed for infants. Comparatively more mothers in this sample of working mothers than in both the IFPS II and the FITS fed their infants cereals, other starches, as well as meat and combination meals specifically designed for infants.
Potentially problematic feeding behaviors were common in this sample of employed mothers. Approximately one in 5 (22%) 4 working mothers in this sample fed their 8-month old infant French fries. By contrast, fewer than 5% of mothers in the IFPS II and the FITS reported feeding their infants French fries. Turning to foods associated with food allergies, 17.7% of mothers in this sample fed their 8 month-old infants eggs, and 5.6% fed their infants peanut butter, nuts or seeds in the past week. By contrast, fewer than 5% of mothers from the other samples fed their infants eggs and less than 1% fed their infants nut- or seed-based foods. Finally, 18.4% of working mothers fed their infants sugar-sweetened beverages, and 22.3% fed their infants candy, cookies, or cake. Less than 10% of mothers in the IFPS II and the FITS reported these feeding behaviors.
Results of simple logistic regression models indicate that educational attainment and marital status are the personal characteristics most consistently associated with infant feeding (Table 2). Working mothers aged 28–33, relative to those 34 or older, were more likely to engage in exclusive breastfeeding and less likely to feed their infants French fries. The odds of exclusive breastfeeding were lower for Black mothers than for white mothers, while the odds of feeding infants French fries were greater for Black mothers than white mothers. Estimated odds ratios for each outcome, except exclusive breastfeeding, ranged from 2.79 to 3.40 indicating that the odds of several potentially negative infant feeding behaviors are greater for those with less than a college education relative to those with a college degree. Similarly, the odds of several potentially negative infant feeding behaviors are 2.8 to 5.5 times greater for unmarried working mothers relative to married or partnered working mothers. Feeding infants cookies, cakes and desserts or feeding infants French fries was greater in households that were below the poverty line relative to those above the poverty line.
Table 2.
Odds Ratios Estimating Simple Associations of Maternal Personal and Employment Characteristics with Distinct Feeding Behaviors (N=199)
| Exclusive Breastfeeding | Food Allergen | Sugar-Sweetened Beverage | Candies, Cookies, & Cakes | French Fries | |
|---|---|---|---|---|---|
| OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
|
| Personal Characteristics | |||||
| Age | |||||
| ≤27 | 3.15 (0.95 – 10.46) |
0.70 (0.32 – 1.57) |
0.85 (0.37 – 1.97) |
0.64 (0.29 – 1.42) |
0.54 (0.24 – 1.19) |
| 28 – 33 | 3.57 (1.09 – 11.71) |
0.42 (0.17 – 1.02) |
0.48 (0.19 – 1.22) |
0.49 (0.21 – 1.14) |
0.40 (0.17 – 0.93) |
| ≥34 | Reference | Reference | Reference | Reference | Reference |
| Ethnicity | |||||
| Non-minority | Reference | Reference | Reference | Reference | Reference |
| Minority | 0.18 (0.04 – 0.80) |
1.84 (0.88 – 3.84) |
1.82 (0.84 – 3.93) |
1.86 (0.91 – 3.81) |
3.35 (1.65 – 6.78) |
| Education | |||||
| Less than college | 0.60 (0.27 – 1.38) |
2.79 (1.33 – 5.86) |
3.40 (1.50 – 7.69) |
2.83 (1.38 – 5.82) |
3.12 (1.49 – 6.50) |
| College graduate | Reference | Reference | Reference | Reference | Reference |
| Marital Status | |||||
| Not married | 0.26 (0.06 – 1.16) |
2.86 (1.34 – 6.14) |
4.12 (1.89 – 9.00) |
4.30 (2.04 – 9.03) |
5.48 (2.60 – 11.53) |
| Married or partnered | Reference | Reference | Reference | Reference | Reference |
| Household Income | |||||
| Below poverty | 0.40 (0.05 – 3.16) |
2.01 (0.65 – 6.23) |
2.19 (0.71 – 6.73) |
4.64 (1.58 – 13.62) |
5.40 (1.88 – 15.50) |
| Above poverty | Reference | Reference | Reference | Reference | Reference |
| Employment Characteristics | |||||
| Work hours | |||||
| < 40 hours/week | Reference | Reference | Reference | Reference | Reference |
| 40 – 44 hours/week | 1.17 (0.46 – 3.00) |
0.64 (0.30 – 1.37) |
0.64 (0.28 – 1.44) |
0.46 (0.22 – 0.98) |
0.64 (0.30 – 1.35) |
| > 44 hours/week | 0.50 (0.10 – 2.56) |
0.62 (0.20 – 1.95) |
0.54 (0.16 – 1.87) |
0.33 (0.10 – 1.12) |
0.54 (0.17 – 1.67) |
| Work Schedule | |||||
| Nonstandard | 1.09 (0.46 – 2.57) |
2.32 (1.13 – 4.73) |
8.47 (3.72 – 19.28) |
3.30 (1.64 – 6.66) |
3.04 (1.52 – 6.08) |
| Standard | Reference | Reference | Reference | Reference | Reference |
| Schedule Control | |||||
| Low | 0.05 (0.11 – 1.00) |
1.58 (0.70 – 3.54) |
2.39 (0.99 – 5.78)C |
0.94 (0.42 – 2.08) |
1.63 (0.75 – 3.57) |
| Medium | 0.65 (0.32 – 2.05) |
0.90 (0.37 – 2.27) |
1.27 (0.47 – 3.45) |
0.98 (0.42 – 2.24) |
0.82 (0.33 – 2.00) |
| High | Reference | Reference | Reference | Reference | Reference |
| Physical Demand | |||||
| Low | Reference | Reference | Reference | Reference | Reference |
| Medium | 1.39 (0.50 – 3.87) |
1.33 (0.53 – 3.37) |
0.75 (0.24 – 2.34) |
0.59 (0.21 – 1.66) |
1.61 (0.62 – 4.20) |
| High | 1.22 (0.47 – 3.20) |
1.99 (0.88 – 4.47) |
2.77 (1.20 – 6.41) |
2.31 (1.08 – 4.95) |
3.37 (1.47 – 7.71) |
Two employment characteristics were associated with several infant feeding behaviors in bivariate analyses. The odds of feeding infants foods that are allergenic, sugar-sweetened beverages, sweets like candies and cookies, and French fries were all greater for mothers with a nonstandard work schedule than for those with a standard Monday thru Friday from 8 to 5 work schedule. The odds of feeding infants sugar-sweetened beverages, sweets like candies and cookies, and French fries were greater for mothers scoring in the highest tertile of job-related physical demands than those in the lowest tertile. Work hours and level of schedule control were not associated with infant feeding behaviors.
Results obtained from multivariate models identified 3 primary correlates of infant feeding behaviors (Table 3). The odds of feeding infants one or more foods associated with allergies is greater for working mothers with less than a college education relative to those with a college degree. Similarly, lower education is associated with greater odds of feeding infants sugared-sweetened beverages, as well as French fries. Relative to working women who are married or in a marriage-like relationship, unmarried mothers were more likely to report feeding their infants one or more foods associated with allergies, sweets like candy, cookies, and cake, and French fries. In comparison to mothers with a standard work schedule, those with a nonstandard work schedule are more likely to feed their infants sugar-sweetened beverages and other sweets. Multivariate models also indicated that the odds of exclusive breastfeeding are lower for ethnic minorities than whites.
Table 3.
Personal and Employment Characteristics Associated with Mothers’ Feeding Behaviors of 8 Month-old Infants (N=199)a
| Exclusive Breastfeeding | Food Allergen | Sugar-Sweetened Beverage | Candies, Cookies, & Cakes | French Fries | |
|---|---|---|---|---|---|
| OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
OR (95% CI) |
|
| Education | |||||
| Less than college | 2.21 (1.01 – 4.85) |
2.75 (1.11 – 6.79) |
2.19 (1.00 – 4.82) |
||
| College graduate | Reference | Reference | Reference | Reference | |
| Marital Status | |||||
| Not married | 2.24 (1.00 – 5.02) |
3.50 (1.57 – 7.80) |
4.13 (1.89 – 9.01) |
||
| Married or partnered | Reference | Reference | Reference | ||
| Schedule | |||||
| Nonstandard | 6.88 (2.96 – 15.98) |
2.18 (1.01 – 4.69) |
|||
| Standard | Reference | Reference | |||
| Ethnicity | |||||
| Non-minority | Reference | ||||
| Minority | 0.18 (0.04 – 0.78) |
Estimated odds ratios obtained from logistic regression models using backward stepwise progression with variables removed based upon Wald statistics. Variables entered into each model included age, maternal ethnicity, maternal education, maternal marital status, poverty status, hours worked per week, work schedule, level of schedule control, and level physical demand required by the job.
DISCUSSION
Very little is known about the potential role maternal employment plays in infant feeding practices. Despite substantial growth of mothers in the labor force since the 1970s, particularly mothers of infants,23 all that is really known is that employed mothers are less likely to initiate and sustain exclusive breastfeeding.24–26 Although they must be viewed as preliminary given the small sample and cross-sectional study design, the results of this study suggest that employment, in general, and specific job characteristics may influence working mothers’ infant feeding behavior.
The estimates from this study suggest that mothers who work full-time may rely heavily on prepackaged foods for their infants. Indeed, approximately 90% of employed mothers used formula (86.4%), infant fruits (92%) and vegetables (93.4%), and infant cereals (92.4%). It is noteworthy that only 68.9% and 86.2% of IFPS II participants used formula and infant feeding, respectively.20 Direct comparisons cannot be made because each study used different sampling and data collection techniques. Nevertheless, the divergence in estimates between the 2 studies is suggestive because the same instruments were used but the studies diverged in mothers’ employment: less than one-third of mothers in the IFPS II (Fein, personal communication, September 9, 2008) were employed at the 7.5 month assessment. Employed mothers’ high use of prepackaged foods for infants may reflect the economic fact that employed mothers have the discretionary income to purchase these food sources. However, it is also possible that employed mothers rely more heavily on these prepackaged food alternatives as one way for easing the hectic pace of life reported by full-time employed mothers with young children.30,35 Future research is needed to determine whether employed mother differ from non-working mothers in their’ infant feeding practices and to explore explanations for possible differences.
The results also highlight clear areas where infant feeding practices used by employed mothers may contribute to subsequent health or developmental problems. A substantial portion of full-time employed women in our sample reported feeding their 8 month old infants fast-food (as indicated by French fries), sugar-sweetened beverages, and other sugary foods like candy, cookies and cakes. These feeding behaviors are concerning because they may promote greater preference for energy dense foods later in life7,11 and contribute to pediatric obesity.14,15 Likewise, the high use of eggs, peanut butter, and fish or shellfish among these working mothers relative to mothers in other samples raises concerns about onset of potential food allergies,2–4 although the role of early exposure to certain foods in the etiology of food allergies remains unclear.36
The overall pattern of infant feeding observed in this study suggests that employed mothers’ infant feeding practices may be shaped by time constraints and convenience. Many of the food items reported by large proportions of mothers, such as infant fruits, vegetables and combination dinners are frequently prepackaged and can be served from the container. Similarly, foods like French fries, whether they are from a restaurant or store-bought and dairy products like cheese, yogurt and ice cream are simple meal complements or snacks that require little preparation. This interpretation is consistent with previous research indicating that employed women rely heavily on commercial and pre-packaged food sources27,28 for family meal planning. Likewise, the results of our descriptive analysis suggest that pre-packaged foods are a dominant strategy used by full-time employed mothers to meet their infant’s food needs. Of course, because mothers were not asked why they chose the foods fed to their infants, it remains an empirical question whether mothers used these food deliberately because of convenience or for some other reason.
Results from our bivariate and multivariate analyses also provide suggestive evidence about infant feeding and health problems that may emerge from poor infant feeding behavior. Results indicated that potentially negative infant feeding practices were more common among unmarried working mothers and those with less than a college education. These results are consistent with other evidence indicating that socially and economically disadvantaged parents may have greater difficulty adhering with recommended parenting guidelines,37 and they suggest that differences in infant feeding practices may help create a foundation for subsequent health disparities among children and young adults.6 The multivariate analyses also produced suggestive evidence indicating that being employed in a job requiring a nonstandard work arrangement was associated with greater odds of feeding infants excess processed sugar. Although the links between sugar consumption per se and children’s behavioral problems is equivocal,38 the artificial colors frequently accompanying these foods have been associated with behavioral problems39 and may explain why children of women with nonstandard work schedules have more behavioral problems.40,41
The results of this study need to be interpreted in light of their limitations. The primary limitation is that infant feeding practices were based on data obtained from relatively crude measures. Future research should rely on more sophisticated dietary recall techniques, such as those used in the FITS. Readers are also reminded that direct comparisons of estimates obtained from this sample relative to those obtained in the IFPS II and FITS cannot be made: estimates from the data are only provided for comparative purposes only to help readers contextualize the behaviors reported by working mothers in this study. Although our sample is reflective of working mothers in Forsyth County, NC, a racially and ethnically diverse metropolitan area, the results of our study may not generalize to other areas. The IFPS II and the FITS were not designed to study maternal employment and therefore lack refined measures of employment characteristics; nevertheless, researchers are encouraged to use these comprehensive data sources to further examine the potential implications of maternal employment on infant feeding.
CONCLUSIONS
In conclusion, the results of this study suggest that employment may play a role in shaping working mothers’ infant feeding behaviors. Mothers who work full-time appear to rely heavily on prepackaged foods for meeting their infants’ feeding needs. Although some prepackaged foods may be beneficial, such as iron fortified infant cereals, others including sugar-sweetened drinks, cakes, candies and cookies, and French fries are potentially problematic. Research using larger more representative samples with a control group, as well as stronger assessments of feeding practices is needed; nevertheless, the results of this study suggest that feeding practices used by employed mothers may create added risk for short-term and long-term health and developmental problems among children.
Acknowledgments
This research was supported by a grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (R21 HD48601).
Contributor Information
Joseph G. Grzywacz, Department of Family and Community Medicine, Wake Forest University School of Medicine; Medical Center Boulevard, Winston-Salem, NC 27157-1084; (336)-716-2237 (T); (336)-716-3206 (F); grzywacz@wfubmc.edu.
Jenna Tucker, Department of Family and Community Medicine, Wake Forest University School of Medicine, Medical Center Boulevard, Winston-Salem, NC 27157-1084; (336)-716-2129 (T); (336)-716-3206 (F); jetucker@wfubmc.edu.
C. Randall Clinch, Department of Family and Community Medicine, Wake Forest University School of Medicine; Medical Center Boulevard, Winston-Salem, NC 27157-1084; (336)-716-2246 (T); (336)-716-3206 (F); crclinch@wfubmc.edu.
Thomas A. Arcury, Department of Family and Community Medicine; Wake Forest University School of Medicine; Medical Center Boulevard, Winston-Salem, NC 27157-1084; (336)-716-9438 (T); (336)-716-3206 (F); tarcury@wfubmc.edu.
REFERENCES
- 1.Altmann AE, Ozanne-Smith J. Non-fatal asphyxiation and foreign body ingestion in children 0–14 years. Inj Prev. 1997;3:176–182. doi: 10.1136/ip.3.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics. Committee on Nutrition. Hypoallergenic infant formulas. Pediatrics. 2000;106:346–349. [PubMed] [Google Scholar]
- 3.Fiocchi A, Assa'ad A, Bahna S. Food allergy and the introduction of solid foods to infants: a consensus document. Adverse Reactions to Foods Committee, American College of Allergy, Asthma and Immunology. Ann Allergy Asthma Immunol. 2006;97:10–20. doi: 10.1016/s1081-1206(10)61364-6. [DOI] [PubMed] [Google Scholar]
- 4.Host A, Koletzko B, Dreborg S, et al. Dietary products used in infants for treatment and prevention of food allergy. Joint Statement of the European Society for Paediatric Allergology and Clinical Immunology (ESPACI) Committee on Hypoallergenic Formulas and the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) Committee on Nutrition. Arch Dis Child. 1999;81:80–84. doi: 10.1136/adc.81.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drane DL, Logemann JA. A critical evaluation of the evidence on the association between type of infant feeding and cognitive development. Paediatr Perinat Epidemiol. 2000;14:349–356. doi: 10.1046/j.1365-3016.2000.00301.x. [DOI] [PubMed] [Google Scholar]
- 6.Dubois L, Girard M. Social inequalities in infant feeding during the first year of life. The Longitudinal Study of Child Development in Quebec (LSCDQ 1998–2002) Public Health Nutr. 2003;6:773–783. doi: 10.1079/phn2003497. [DOI] [PubMed] [Google Scholar]
- 7.Birch LL. Development of food acceptance patterns in the first years of life. Proc Nutr Soc. 1998;57:617–624. doi: 10.1079/pns19980090. [DOI] [PubMed] [Google Scholar]
- 8.Gunnarsdottir I, Aspelund T, Birgisdottir BE, et al. Infant feeding patterns and midlife erythrocyte sedimentation rate. Acta Paediatr. 2007;96:852–856. doi: 10.1111/j.1651-2227.2007.00324.x. [DOI] [PubMed] [Google Scholar]
- 9.Liem DG, Mennella JA. Sweet and sour preferences during childhood: role of early experiences. Dev Psychobiol. 2002;41:388–395. doi: 10.1002/dev.10067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Owen CG, Whincup PH, Kaye SJ, et al. Does initial breastfeeding lead to lower blood cholesterol in adult life? A quantitative review of the evidence. Am J Clin Nutr. 2008;88:305–314. doi: 10.1093/ajcn/88.2.305. [DOI] [PubMed] [Google Scholar]
- 11.Skinner JD, Carruth BR, Wendy B, Ziegler PJ. Children's food preferences: a longitudinal analysis. J Am Diet Assoc. 2002;102:1638–1647. doi: 10.1016/s0002-8223(02)90349-4. [DOI] [PubMed] [Google Scholar]
- 12.Beauchamp GK, Moran M. Dietary experience and sweet taste preference in human infants. Appetite. 1982;3:139–152. doi: 10.1016/s0195-6663(82)80007-x. [DOI] [PubMed] [Google Scholar]
- 13.Liem DG, de Graaf C. Sweet and sour preferences in young children and adults: role of repeated exposure. Physiol Behav. 2004;83:421–429. doi: 10.1016/j.physbeh.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 14.Dubois L, Farmer A, Girard M, Peterson K. Regular sugar-sweetened beverage consumption between meals increases risk of overweight among preschool-aged children. J Am Diet Assoc. 2007;107:924–934. doi: 10.1016/j.jada.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr. 2006;84:274–288. doi: 10.1093/ajcn/84.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warner ML, Harley K, Bradman A, et al. Soda consumption and overweight status of 2-year-old mexican-american children in california. Obesity. 2006;14:1966–1974. doi: 10.1038/oby.2006.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forshee RA, Anderson PA, Storey ML. Sugar-sweetened beverages and body mass index in children and adolescents: a meta-analysis. Am J Clin Nutr. 2008;87:1662–1671. doi: 10.1093/ajcn/87.6.1662. [DOI] [PubMed] [Google Scholar]
- 18.Johnson L, Mander AP, Jones LR, et al. Is sugar-sweetened beverage consumption associated with increased fatness in children? Nutrition. 2007;23:557–563. doi: 10.1016/j.nut.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Newby PK, Peterson KE, Berkey CS, et al. Beverage consumption is not associated with changes in weight and body mass index among low-income preschool children in North Dakota. J Am Diet Assoc. 2004;104:1086–1094. doi: 10.1016/j.jada.2004.04.020. [DOI] [PubMed] [Google Scholar]
- 20.Grummer-Strawn LM, Scanlon KS, Fein SB. Infant feeding and feeding transitions during the first year of life. Pediatrics. 2008;122 Suppl 2:S36–S42. doi: 10.1542/peds.2008-1315d. [DOI] [PubMed] [Google Scholar]
- 21.Fox MK, Pac S, Devaney B, Jankowski L. Feeding infants and toddlers study: what foods are infants and toddlers eating? J Am Diet Assoc. 2004;104:S22–S30. doi: 10.1016/j.jada.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 22.Mennella JA, Ziegler P, Briefel R, Novak T. Feeding Infants and Toddlers Study: The types of foods fed to Hispanic infants and toddlers. J Am Diet Assoc. 2006;106:S96–S106. doi: 10.1016/j.jada.2005.09.038. [DOI] [PubMed] [Google Scholar]
- 23.U.S. Department of Labor. [Accessed January 16, 2009];U.S. Department of Labor. 2007 Available at http://www.bls.gov/cps/wlf-databook-2007.pdf">.
- 24.Fein SB, Mandel B, Roe BE. Success of strategies for combining employment and breastfeeding. Pediatrics. 2008;122 Suppl 2:S56–S62. doi: 10.1542/peds.2008-1315g. [DOI] [PubMed] [Google Scholar]
- 25.Fein SB, Roe B. The effect of work status on initiation and duration of breast-feeding. Am J Public Health. 1998;88:1042–1046. doi: 10.2105/ajph.88.7.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Visness CM, Kennedy KI. Maternal employment and breast-feeding: findings from the 1988 National Maternal and Infant Health Survey. Am J Public Health. 1997;87:945–950. doi: 10.2105/ajph.87.6.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jackson RW, McDaniel SW, Rao CP. Food shopping and preparation: psychographic differences of working wives and housewives. J Consum Res. 1985;12:110–113. [Google Scholar]
- 28.Muller J. Characteristics and domestic management strategies of Australian professional working mothers. Journal of Applied Health Behaviour. 1999;1:10–21. [Google Scholar]
- 29.Kant AK, Graubard BI. Eating out in America, 1987–2000: trends and nutritional correlates. Prev Med. 2004;38:243–249. doi: 10.1016/j.ypmed.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 30.Roxburgh S. 'There just aren't enough hours in the day': the mental health consequences of time pressure. J Health Soc Behav. 2004;45:115–131. doi: 10.1177/002214650404500201. [DOI] [PubMed] [Google Scholar]
- 31.Fein SB, Labiner-Wolfe J, Shealy K, et al. Infant Feeding Practices Study II: Study Methods. Pediatrics. 2008;122 Suppl 2:S28–S35. doi: 10.1542/peds.2008-1315c. [DOI] [PubMed] [Google Scholar]
- 32.Ala-Mursula L, Vahtera J, Linna A, et al. Employee worktime control moderates the effects of job strain and effort-reward imbalance on sickness absence: The 10-town study. J Epidemiol Community Health. 2005;59:851–857. doi: 10.1136/jech.2004.030924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karasek R, Theorell T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life. New York: Basic Books; 1990. [Google Scholar]
- 34.Devaney B, Kalb L, Briefel R, et al. Feeding infants and toddlers study: overview of the study design. J Am Diet Assoc. 2004;104:S8–S13. doi: 10.1016/j.jada.2003.10.023. [DOI] [PubMed] [Google Scholar]
- 35.Bond TJ, Galinsky E, Swanberg . In: The 1997 National Study of the Changing WorkforceBond. Galinsky TJ, Swanberg E, editors. New York: Families and Work Institute; 1998. [Google Scholar]
- 36.Maloney JM, Sampson HA, Sicherer SH, Burks WA. Food allergy and the introduction of solid foods to infants: a consensus document. Ann Allergy Asthma Immunol. 2006;97:559–560. doi: 10.1016/S1081-1206(10)60955-6. [DOI] [PubMed] [Google Scholar]
- 37.Belsky J, Bell B, Bradley RH, et al. Socioeconomic risk, parenting during the preschool years and child health age 6 years. Eur J Public Health. 2007;17:508–513. doi: 10.1093/eurpub/ckl261. [DOI] [PubMed] [Google Scholar]
- 38.Krummel DA, Seligson FH, Guthrie HA. Hyperactivity: is candy causal? Crit Rev Food Sci Nutr. 1996;36:31–47. doi: 10.1080/10408399609527717. [DOI] [PubMed] [Google Scholar]
- 39.McCann D, Barrett A, Cooper A, et al. Food additives and hyperactive behaviour in 3-year-old and 8/9-year-old children in the community: a randomised, double-blinded, placebo-controlled trial. Lancet. 2007;370:1560–1567. doi: 10.1016/S0140-6736(07)61306-3. [DOI] [PubMed] [Google Scholar]
- 40.Strazdins L, Korda RJ, Lim LL, et al. Around-the-clock: parent work schedules and children's well-being in a 24-h economy. Soc Sci Med. 2004;59:1517–1527. doi: 10.1016/j.socscimed.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 41.Daniel SS, Grzywacz JG, Leerkes E, et al. Nonstandard work schedules during infancy: implications for children’s behavior. Infancy & Development. doi: 10.1016/j.infbeh.2008.12.008. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]