Abstract
The Sonic Flashlight is an ultrasound device that projects real-time ultrasound images into patients using a semi-reflective/transparent mirror. We evaluated the feasibility of using the Sonic Flashlight for clinical PICC placements, originally with the mirror located inside a sterile cover (15 patients), then with the mirror outside (11 patients). Successful access was obtained in all cases. Results show that this new design improved visibility, as judged subjectively first-hand and in photographs. Our study demonstrated the feasibility of the Sonic Flashlight and the new design to help assure sterility without degrading visibility, allowing further clinical trials involving both physicians and nurses.
Introduction
Peripherally Inserted Central Catheters (PICC) are increasingly being used as safe alternatives to direct placement of central lines, allowing longer dwell times compared to peripheral intravenous lines. This makes PICCs the preferred access method for many uses including long term chemotherapy, hyperalimentation, repeated administration of blood products, and repeated venous sampling. As superficial antecubital and forearm veins become hard to access after multiple punctures, the upper arm becomes the optimal placement site for PICCs. Cannulation at this location requires ultrasound (US) guidance and is most reliably performed by experienced users. The recent trend in miniaturization of inexpensive US machines has prompted an increase in attempted PICC placement at the bedside, but the success rate remains variable, ranging from 67% to 92% according to three separate studies [1-3]. Improving this success rate would help alleviate the bottleneck caused by PICC placement in the interventional radiology (IR) suite and reduce the risk posed by transporting patients.
Much of the difficulty in learning conventional ultrasound guided procedures stems from the displaced sense of hand-eye coordination that occurs when the operator looks away from the operating field to see the US display, requiring mental computation of the relationship between the needle and the underlying anatomy. Eliminating this cognitive process could make it easier and faster to learn US guided vascular access procedures, allowing more PICCs to be placed by bedside personnel instead of by experienced interventionalists in the IR suite.
To address this difficulty, some researchers have explored methods for viewing the US image, patient, instrument, and operator’s hands in a single environment. Head-mounted display systems have been developed to superimpose the US image within the patient [4-7]. These systems track the location of the US transducer relative to the head-mounted display, so the image can be computed and superimposed by the head-mounted display with the correct stereoscopic perspective and location. To the person wearing the head-mounted display, the US image appears within the patient at its actual physical location. Despite their promise, head-mounted display systems have yet to overcome significant obstacles, including lag time, low resolution, limited field of view, significant weight, and expense. Furthermore, if multiple observers are cooperating in a procedure, each observer requires a separate head-mounted display to see the same in-situ US image.
The Sonic Flashlight (Figure 1) utilizes a novel means to display real-time US images inside the patient without using positional tracking or a head-mounted display system [8-9]. The Sonic Flashlight fixes the relative geometry of the transducer, display, and a half-silvered mirror to produce a virtual image of the US display inside the patient (Figure 2). Looking through the half-silvered mirror, the US image appears to float within the patient, with each pixel of the scan seeming to emanate from its correct anatomic location within the patient. Using the Sonic Flashlight, the US image, patient, instrument, and operator’s hands are all merged into a single environment. This makes US-guided interventional procedures as simple as aiming for the US image itself. The Sonic Flashlight display is viewpoint-independent, meaning that users looking through the mirror from any vantage point will see the US image properly registered with the internal anatomy.
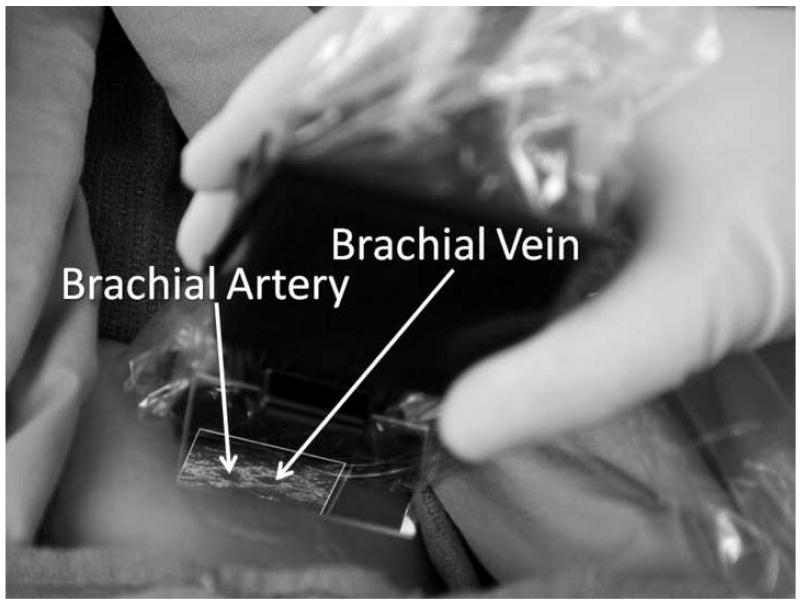
Figure 1.
View of the brachial artery and vein through the half-silvered mirror of the Sonic Flashlight. The perceived location of the vessels is independent of viewpoint.
Figure 2.
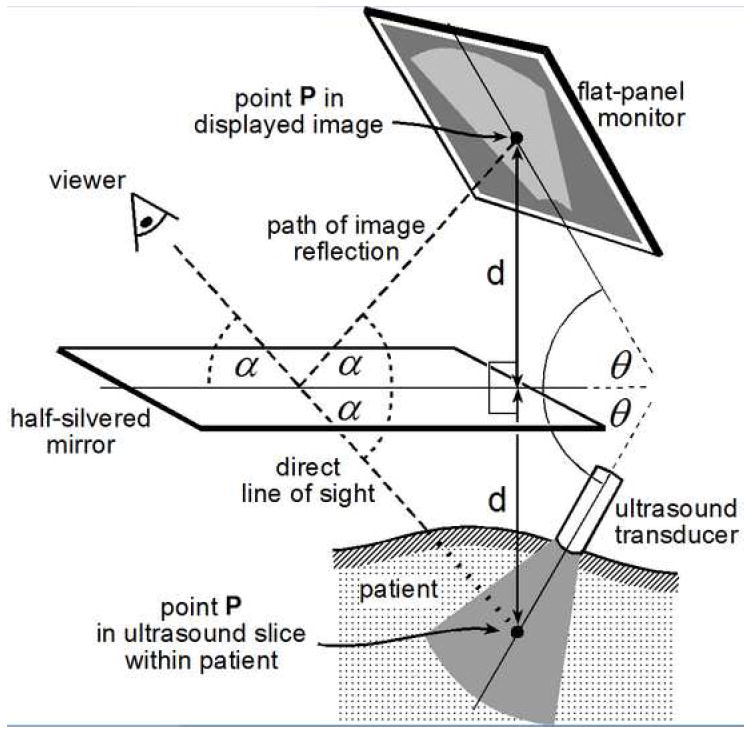
Geometric relationships for Real Time Tomographic Reflection (RTTR). The mirror bisects the angle between the display and the virtual image. By fundamental laws of optics, the virtual image will appear at its physical location, independent of viewer position.
Unlike most conventional ultrasound displays, which are magnified to permit greater resolution of fine detail, the Sonic Flashlight display cannot be magnified. It is necessary for the Sonic Flashlight to display the US scan at its actual scale, so that the images of the underlying structures can appear at their correct locations. This lack of magnification can be a disadvantage for some applications involving very small structures. However, for PICC placement purposes, the true anatomic size is sufficient for identification of the underlying anatomy.
The Sonic Flashlight directly addresses many of the head-mounted display-related issues and has been proven effective in cadaveric retrobulbar injection of the eye [10] and cadaveric jugular vein access [11]. It has been shown that, compared to conventional ultrasound, vascular access in phantoms with the Sonic Flashlight is faster and easier for experienced US users [12], as well as faster to learn for US novices [13]. Precise psychophysical experiments have shown particular advantages in using the Sonic Flashlight over conventional ultrasound by reducing errors in judging target location [14, 15]. The present paper describes the first clinical trial in which an experienced interventional radiologist used the device to place PICCs in patients in the IR suite.
Materials and Methods
During eight years of development, there have been multiple prototypes of the Sonic Flashlight. The first version ready for clinical use employed a 10 MHz US system (Terason, Burlington, MA, Model 2000), the probe of which was fitted with a small flat-panel display (Kodak, Rochester, NY, AM550L organic light emitting diode) and a dedicated half-silvered mirror. A standard transparent disposable sterile probe cover (BARD Access Systems, Salt Lake City, UT., #9001C0197) was fitted over the Sonic Flashlight to eliminate cross-contamination between patients. For the first 15 patients the mirror was attached directly to the Sonic Flashlight inside the sterile cover. For the remaining 11 patients, a subsequent design was employed, using a disposable mirror clipped on outside the sterile cover. To avoid variability between different ultrasound systems, we used the same Terason ultrasound probe with its laptop-based display as the conventional ultrasound for comparison.
Under IRB approval, we recruited 26 subjects from patients who had been referred to the IR suite at our institution to have a PICC placed. After obtaining informed consent from each patient, an experienced interventional radiologist scanned the upper arm with both the Sonic Flashlight and conventional ultrasound. The same radiologist performed the procedures on all subjects. Identification of the basilic vein, brachial veins, and brachial artery were compared and recorded with each modality. If the identifications by both modalities agreed, then it was considered a successful identification. If the basilic vein was visualized using the Sonic Flashlight, the Sonic Flashlight was used to guide a needle (21 gauge, 7cm) into the basilic vein. The basilic vein was favored since it typically is more superficial and does not present with an accompanying artery, reducing the risk of complications due to arterial puncture. If the basilic vein was determined to be an inappropriate target, such as if it is because it was thrombosed or collapsed, a brachial vein was used instead. If vascular access was unsuccessful after three attempts with the Sonic Flashlight, the radiologist was to revert to using conventional ultrasound for the procedure (although this never occurred in the present study). If successful access was gained in the selected vein, the procedure continued as in a standard PICC procedure.
Results
Our first set of clinical trials involved 15 of the 26 patients [16]. The vessels were visualized in-situ using the Sonic Flashlight. The identities of the vessels were confirmed by comparison to conventional ultrasound. The needle was easily aimed and inserted into the basilic or brachial vein in all cases, and the needle tip was visualized at its expected location. Successful access was obtained in all 15 subjects: 13 on the first attempt, and 2 on the second attempt. Thus no one had to be converted to conventional ultrasound guidance. A problem was noted, however, due to the probe cover, which enveloped the entire Sonic Flashlight device including the mirror, to ensure sterility. Commercial probe covers currently marketed as “transparent” are not actually designed to prevent all distortion of visible light. Resulting image blurriness was noted as inconvenient during 3 procedures although it did not affect outcome (Figure. 3 bottom).
Figure 3.
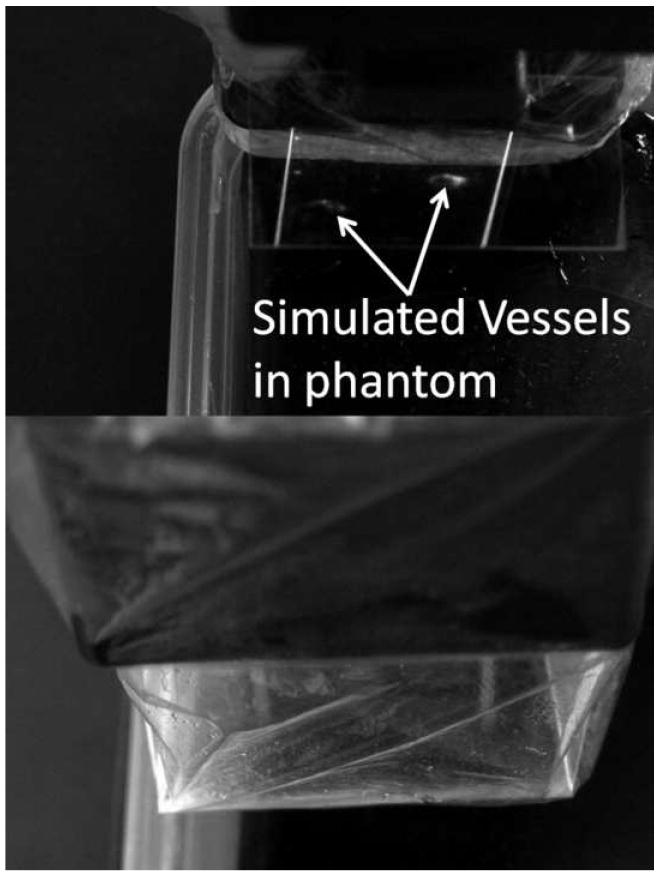
(Top) Virtual image of 2 simulated vessels in a phantom seen through the half-silvered mirror with the plastic probe cover over the base only. (Bottom) The same virtual image seen through the half-silvered mirror with the plastic probe cover over the mirror. Note the degradation of image quality.
In reviewing the initial trial, it was decided that a redesign of the Sonic Flashlight was required to solve this problem. Accordingly, we created a separate mirror holder that snapped onto the flat panel display, holding the plastic probe cover flat over the organic light emitting diode display. This greatly reduced the diffusive effect of the probe cover on the display (Figure. 4). In the process, the mirror was moved entirely outside the cover, eliminating any effect of the cover on the direct line of sight. An optional darkened hood was also added that could be snapped onto the entire apparatus to reduce reflection form ambient light.
Figure 4.
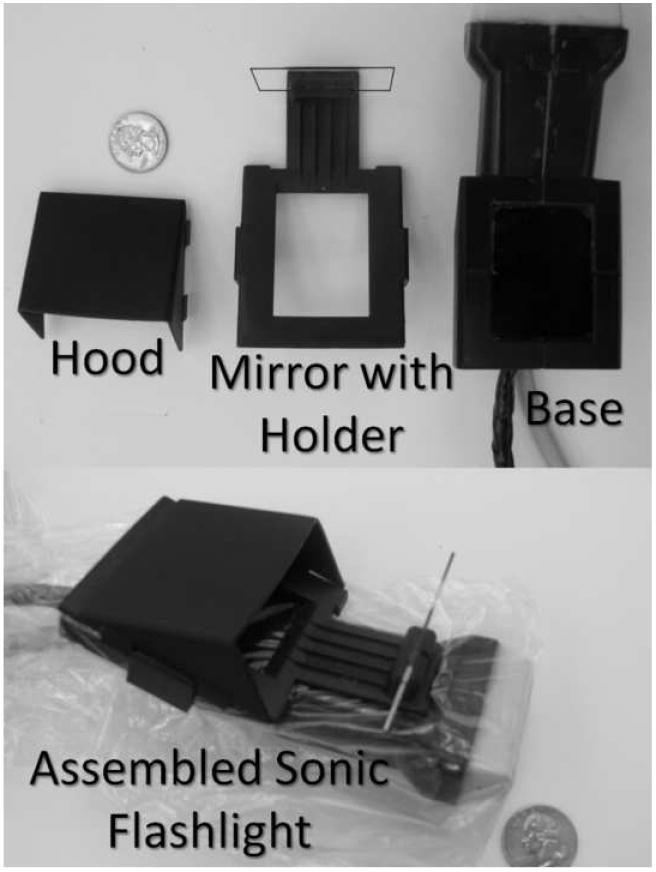
(Top) The Sonic Flashlight, separated into 3 pieces, from left to right: hood, mirror with holder, and base. (Bottom) The assembled Sonic Flashlight with the plastic probe cover enveloping only the base.
The resulting image (Figure. 3 top) shows little or no light distorting effect. Since the mirror and hood are now unprotected by the probe cover, they must be sterilized for each patient. We chose to make them disposable, to eliminate any risk of cross-patient contamination.
Using this new model, successful access was obtained in the remaining 11 subjects: 8 on the first attempt, 2 on the second, and 1 on the third. The vessels were visualized in-situ with substantially greater clarity, as judged by the radiologist, than in the first set of clinical trials. The identities of the vessels were again confirmed by comparison to conventional ultrasound. The needle was easily aimed and inserted into the basilic or brachial vein as before, and the needle tip was clearly visualized inside the vessels.
Discussion
This two-stage study validated our basic design for the Sonic Flashlight and the improvements made to it with the disposable sterile mirror assembly. It showed that the basilic and brachial veins can be safely accessed using the Sonic Flashlight for guidance. While there are insufficient patient numbers to show a statistically significant difference between our previous design and current design, we believe the improved visualization can only aid cannulation. The overall success rate on first puncture attempt by our interventional radiologist was 78%, which is within the 67% to 92% range referred to above for conventional ultrasound guidance. A larger trial would be required for a more accurate comparison.
This initial trial lays the groundwork for an expanded clinical trial comparing bedside personnel’s ability to place PICCs using the Sonic Flashlight versus conventional ultrasound. While the Sonic Flashlight does not solve subsequent line placement problems such as the inability to advance a PICC centrally, we believe it will help with the initial needle access to the vessel. The Sonic Flashlight permits direct freehand aiming at structures without a needle guide. We hope to show the utility of Sonic Flashlight in facilitating the use of ultrasound guidance by non-radiologists, with the goal of reducing the number of patients who need to be transported to the IR suite for PICC placement. We also hope to show the utility of the Sonic Flashlight in helping interventional radiologists place lines in the jugular, subclavian, and femoral veins.
Acknowledgments
This study was funded by NIH grants R01-HL074285 and R01-EB00860. The authors would like to thank the staff in the IR suite, especially Thomas Killcrece RT, at the University of Pittsburgh Medical Center Presbyterian Hospital for their support in this project.
Footnotes
This material has not been presented at any SIR annual meeting.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Nikhil Amesur, Email: amesurnb@upmc.edu.
David Wang, Email: wangdavid@gmail.com.
Wilson Chang, Email: wmchang@gmail.com.
David Weiser, Email: david@david-weiser.com.
Roberta Klatzky, Email: klatzky@cmu.edu.
Gaurav Shukla, Email: gshukla@gmail.com.
George Stetten, Email: george@stetten.com.
References
- 1.Keyes LE, Frazee BW, Snoey ER, Simon BC, Christy D. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Ann Emerg Med. 1999;34(6):711–714. doi: 10.1016/s0196-0644(99)70095-8. [DOI] [PubMed] [Google Scholar]
- 2.Costantino TG, Fojtik JP. Success Rate of Peripheral IV Catheter Insertion by Emergency Physicians Using Ultrasound Guidance. Acad Emerg Med. 2003:487. [Google Scholar]
- 3.Chinnock BF, Thornton S, Hendey GW. Nurse-performed Ultrasound-guided Upper Extremity Venous Cannulation in Emergency Department Patients with Difficult Venous Access. Acad Emerg Med. 2005:35. [Google Scholar]
- 4.Fuchs H, State A, Pisano ED, et al. Towards performing ultrasound-guided needle biopsies from within a head-mounted display. Presented at Visualization in Biomedical Computing; September 22-25, 1996; Hamburg, Germany. [Google Scholar]
- 5.Rosenthal MS, Lee J, Hirota G, et al. Augmented reality guidance for needle biopsies: An initial randomized, controlled trial in phantoms. Med Image Anal. 2002;6:313–320. doi: 10.1016/s1361-8415(02)00088-9. [DOI] [PubMed] [Google Scholar]
- 6.Sauer F, Khamene A, Bascle B, et al. System description, calibration, and features. Presented at the 4th International Symposium on Augmented Reality; October 2001; New York, NY. [Google Scholar]
- 7.State A, Livingston MA, Garret WF, et al. Realizing ultrasound-guided needle biopsies. Presented at SIGGRAPH 96, 23rd International Conference on Computer Graphics and Interactive Techniques; August 4-9, 1996; New Orleans, LA. [Google Scholar]
- 8.Chang WM, Stetten GD, Lobes LL, Jr, Sheldon DM, Tamburo RJ. Guidance of retrobulbar injection with real time tomographic reflection. J Ultrasound Med. 2002;21:1131–1135. doi: 10.7863/jum.2002.21.10.1131. [DOI] [PubMed] [Google Scholar]
- 9.Stetten GD, Chib V. Overlaying ultrasound images on direct vision. J Ultrasound Med. 2001;20:235–240. doi: 10.7863/jum.2001.20.3.235. [DOI] [PubMed] [Google Scholar]
- 10.Chang W, Stetten GD, Lobes L, Shelton D. Guidance of Retrobulbar Injection with Real Time Tomographic Reflection. J Ultrasound Medicine. 2002:1131–1135. doi: 10.7863/jum.2002.21.10.1131. [DOI] [PubMed] [Google Scholar]
- 11.Chang W, Amesur N, Zajko A, Stetten GD. Cadaveric central venous access using the Sonic Flashlight, a novel ultrasound display system. Presented at the 2004 Meeting of the Radiological Society of North America; December 2004; Chicago, IL. [Google Scholar]
- 12.Chang W, Amesur N, Zajko A, Stetten GD. The Sonic Flashlight Is Faster To Learn And Use Compared To Conventional Ultrasound Guidance For Vascular Access. Presented at the 105th Annual Meeting of the American Roentgen Ray Society; May 15-20, 2005; New Orleans, LA. [Google Scholar]
- 13.Chang W, Amesur N, Zajko A, Stetten GD. Sonic Flashlight: A new ultrasound display system that makes vascular access easier. J Vasc Interv Radiol. 2004;15.2.2:S166. [Google Scholar]
- 14.Wu B, Klatzky R, Shelton D, Stetten GD. Psychophysical Evaluation of In-Situ Ultrasound Visualization. Special Issue on Haptics, Virtual and Augmented Reality, IEEE Trans Vis Comput Graph. 2005;6:684–693. doi: 10.1109/TVCG.2005.104. [DOI] [PubMed] [Google Scholar]
- 15.Klatzky R, Wu B, Shelton D, Stetten GD. Learning to perform actions in near space under perceptual vs. cognitive control. ACM Trans Appl Percept. 2008;1:1–23. [Google Scholar]
- 16.Chang W, Amesur N, Wang D, Zajko A, Stetten GD. First Clinical Trial of the Sonic Flashlight - Guiding Placement of Peripherally Inserted Central Catheters. Presented at the 2005 Meeting of the Radiological Society of North America; November 2005; Chicago, IL. [Google Scholar]