Abstract
A 47-year-old woman complained of abdominal pain, and a computed tomography scan indicated compressive obstruction of the celiac axis and a 4-cm retropancreatic aneurysm. An angiogram identified the aneurysmal vessel as the posterior pancreaticoduodenal artery. All foregut structures were supplied by this aneurysmal vessel. Via an open approach, the inflow and outflow of the aneurysm were ligated, and blood flow to the celiac axis was reconstructed via a bypass from the supraceliac aorta. A follow-up scan indicated complete thrombosis of the aneurysm. The patient is now symptom free. Open reconstruction of the celiac axis is mandatory when ligation of a pancreaticoduodenal aneurysm results in foregut ischemia. Ligation and reconstruction can be done safely and effectively in the elective setting.
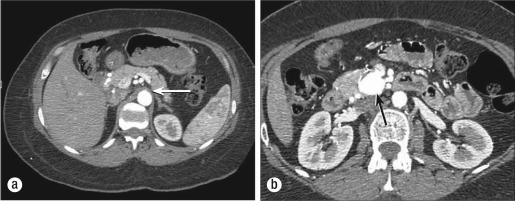
Several months before presentation, a 47-year-old woman noted the onset of reflux with increasing abdominal and flank pain. She denied any history of pancreatitis. A computed tomography (CT) scan indicated a large aneurysm posterior to the pancreas (Figure 1). An angiogram indicated occlusion of the celiac axis and identified the aneurysmal vessel to be the posterior pancreaticoduodenal artery. Collateral flow via the aneurysmal artery supplied all foregut structures (Figure 2).
Figure 1.
CT scan upon presentation showing (a) the occluded origin of the celiac axis (arrow) and the cross-section of proper hepatic and splenic arteries just anterior to the aorta and (b) the ancreaticoduodenal aneurysm posterior to the pancreas (arrow).
Figure 2.
Angiogram showing (clockwise) the splenic artery (dotted black arrow); the superior mesenteric artery at the level of the inferior pancreaticoduodenal artery origin (small solid white arrow); aneurysm (large white arrow); hypertrophied gastroduodenal artery (double white arrows); and right hepatic artery (black arrow).
At operation the abdomen was entered through a midline incision. The celiac axis was dissected from its surrounding tissues. It was occluded at its origin and surrounded by dense fibrous bands. The splenic, right gastric, and common hepatic arteries were dissected free and controlled with vessel loops. The common hepatic artery was followed to its bifurcation, and the gastroduodenal artery (GDA) was isolated. The GDA was followed to the level of the duodenum. Three centimeters distal to this point, posterior to the pancreas, a large aneurysm was palpable. A vessel loop was placed around the GDA above the aneurysm. The superior mesenteric artery was identified at the inferior border of the pancreas and dissected down to the level of the lateral takeoff of the inferior pancreaticoduodenal artery. This artery was controlled, and a test occlusion was performed. Real-time ultrasound indicated absence of flow in the aneurysm, the GDA, and the isolated branches of the celiac axis.
Revascularization of the foregut was undertaken. The patient was systemically heparinized. An 8-mm Hemashield Dacron graft was used to construct bypass from the supraceliac aorta to the celiac axis. A second test occlusion of the inflow to the aneurysm was performed. There was now excellent signal in all branches of the celiac axis via the bypass. The inferior pancreaticoduodenal artery and GDA were ligated. Real-time ultrasound was used to confirm absence of flow in the aneurysm and brisk flow in all foregut structures. The liver appeared well vascularized. Heparinization was reversed, the abdomen was closed, and the patient was moved to the recovery room, having tolerated the procedure well.
DISCUSSION
Median arcuate ligament syndrome is a known cause of foregut ischemia. The syndrome is the result of compression of the celiac axis by the median arcuate ligament of the diaphragm. In 1965, Dunbar and colleagues presented a series of 15 patients with foregut ischemia and compression of the celiac axis (1). They found that division of the median arcuate ligament relieved pain in these patients. Lord et al documented actual injury to the celiac trunk in 1968. They reported 12 patients treated at the University of California, eight of whom required reconstruction secondary to persistent stenosis after lysis of the arcuate ligament (2). On histological analysis, fibrotic intimal thickening was noted.
Aneurysms of the pancreaticoduodenal artery are rare and represent <2% of all reported visceral artery aneurysms (3). In their extensive review of the literature, Coll et al found 83 reported cases (4). Pancreaticoduodenal aneurysms associated with celiac axis occlusion are even less common. Bellosta et al reported only 38 cases in their review (5). Sutton and Lawton speculated that aneurysmal degeneration was secondary to increased flow through normally small collateral vessels of the foregut (6).
Treatment of the pancreaticoduodenal artery aneurysm is considered mandatory because of the >50% mortality associated with rupture (3). Endovascular treatment for the pancreaticoduodenal artery aneurysm is well described. Murata et al had excellent technical and clinical success in their small series. Nine of 10 patients with pancreaticoduodenal artery aneurysms were successfully treated using microcoils or microcoils combined with sponges (7). Despite this and other excellent reported results, surgery must remain first-line treatment in cases of rupture with hemodynamic instability, unfavorable anatomy, and possible resultant foregut ischemia. Surgical morbidity and mortality in elective cases is low (0–5%) (8).
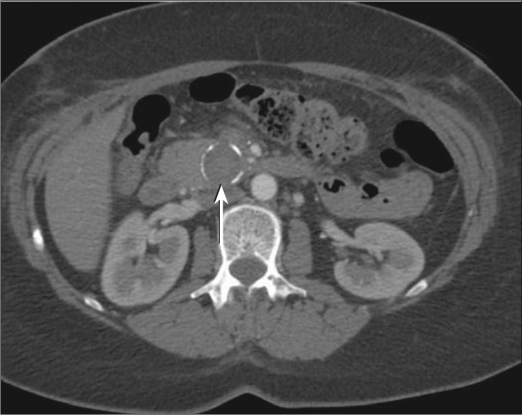
In this case, profusion to the foregut was entirely dependent on the aneurysmal vessel, mandating open reconstruction. Options for bypass included the supraceliac bypass as described above, simple reconstruction of the celiac axis with or without patch angioplasty, or other bypass procedures such as aortomesenteric bypass to a vessel of the celiac axis such as the common hepatic artery. The patient did well after the procedure and was released from the hospital on postoperative day 5. She has been pain free. A follow-up CT scan indicated complete thrombosis of the aneurysm (Figure 3).
Figure 3.
CT scan after surgery, showing the thrombosed aneurysm (arrow), with calcifications around its rim.
References
- 1.Dunbar JD, Molnar W, Beman FF, Marable SA. Compression of the celiac trunk and abdominal angina. Am J Roentgenol Radium Ther Nucl Med. 1965;95(3):731–744. doi: 10.2214/ajr.95.3.731. [DOI] [PubMed] [Google Scholar]
- 2.Lord RS, Stoney RJ, Wylie EJ. Coeliac-axis compression. Lancet. 1968;2(7572):795–798. doi: 10.1016/s0140-6736(68)92455-0. [DOI] [PubMed] [Google Scholar]
- 3.Hildebrand P, Esnaashari H, Franke C, Bürk C, Bruch HP. Surgical management of pancreaticoduodenal artery aneurysms in association with celiac trunk occlusion or stenosis. Ann Vasc Surg. 2007;21(1):10–15. doi: 10.1016/j.avsg.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Coll DP, Ierardi R, Kerstein MD, Yost S, Wilson A, Matsumoto T. Aneurysms of the pancreaticoduodenal arteries: a change in management. Ann Vasc Surg. 1998;12(3):286–291. doi: 10.1007/s100169900155. [DOI] [PubMed] [Google Scholar]
- 5.Bellosta R, Luzzani L, Carugati C, Melloni C, Sarcina A. Pancreaticoduodenal artery aneurysms associated with celiac axis occlusion. Ann Vasc Surg. 2005;19(4):534–539. doi: 10.1007/s10016-005-5042-6. [DOI] [PubMed] [Google Scholar]
- 6.Sutton D, Lawton G. Coeliac stenosis or occlusion with aneurysm of the collateral supply. Clin Radiol. 1973;24(1):49–53. doi: 10.1016/s0009-9260(73)80114-x. [DOI] [PubMed] [Google Scholar]
- 7.Murata S, Tajima H, Fukunaga T, Abe Y, Niggemann P, Onozawa S, Kumazaki T, Kuramochi M, Kuramoto K. Management of pancreaticoduodenal artery aneurysms: results of superselective transcatheter embolization. AJR Am J Roentgenol. 2006;187(3):W290–W298. doi: 10.2214/AJR.04.1726. [DOI] [PubMed] [Google Scholar]
- 8.Pulli R, Dorigo W, Troisi N, Pratesi G, Innocenti AA, Pratesi C. Surgical treatment of visceral artery aneurysms: a 25-year experience. J Vasc Surg. 2008;48(2):334–342. doi: 10.1016/j.jvs.2008.03.043. [DOI] [PubMed] [Google Scholar]