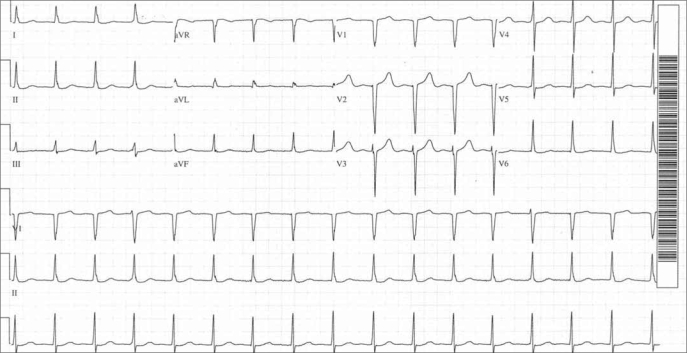
A 62-year-old diabetic, hypertensive woman with prior stenting of her dominant right coronary artery underwent coronary arteriography because of an abnormal stress test. A 90% narrowing of the left circumflex coronary artery beyond the second obtuse marginal branch was stented with a 3 × 18-mm drug-eluting stent. She went to the recovery room in good condition, and an electrocardiogram was recorded (Figure).
Figure.
Electrocardiogram recorded after the coronary angioplasty. See text for explication of the arrhythmia. In addition, nonspecific ST-T changes are present.
The QRS complexes are narrow and occur regularly at a rate of 98 beats/min. At first glance no P waves are visible, but careful inspection of the lead II rhythm strip shows a notch on the downslope of all R waves except the fourth one from the beginning of the tracing and the fourth one from the end. Each of those QRSs has a notch at the beginning of the upslope of the R wave that corresponds to a small upward deflection at the beginning of the QRS in the simultaneously recorded lead V1, whereas all other V1 QRSs are pure QS complexes. The perturbations of the QRS complexes are due to their occurring simultaneously with sinus P waves. Thus, there is isorhythmic dissociation of an accelerated junctional rhythm from sinus rhythm. As is usually the case, the junctional rhythm is perfectly regular or nearly so, and slight sinus arrhythmia is responsible for the P waves being seen at the beginning or at the end of the QRSs. In most cases, the P waves emerge more distinctly from the front or the back of the QRSs, i.e., Ps and QRSs are less synchronized, than is seen here.
Atrioventricular dissociation simply signifies that the atria and the ventricles have independent rhythms, either all of the time, i.e., complete dissociation, or intermittently, i.e., dissociation is incomplete due to atrial and/or ventricular captures. The electrocardiographer must state what rhythms are dissociated and why (1, 2). Although complete atrioventricular block is the quintessence of atrioventricular dissociation, it may occur with other arrhythmias (Table) (2). In many of these the sinus or atrial rhythm is too slow, and a junctional or ventricular escape rhythm has emerged. Alternatively, an accelerated or frankly tachycardic junctional or ventricular rhythm has usurped control of the ventricles, but the atria maintain their own rhythm.
Table.
Some causes of complete atrioventricular dissociation∗
| • Sinus or atrial rhythm with complete antegrade and retrograde atrioventricular block and a junctional or ventricular escape rhythm. |
| • Sinus or atrial bradycardia with a junctional or ventricular escape rhythm. Some degree of antegrade and retrograde atrioventricular block often is necessary to prevent ventricular or atrial captures. |
| • Junctional or ventricular accelerated rhythm or tachycardia. Some degree of retrograde atrioventricular block is necessary to prevent atrial captures, and at slower junctional or ventricular rates some degree of antegrade atrioventricular block is necessary to prevent ventricular captures and fusions. |
| • Synchronization of the sinus or atrial pacemaker with the junctional or ventricular pacemaker so that each discharges in the absolute refractory period of the other and thus cannot capture it. |
∗Modified from reference 2.
In this patient's electrocardiogram the sinus-initiated P waves and the junction-initiated QRSs occur virtually simultaneously, and each occurs in the absolute refractory period of the other so that there are no atrial or ventricular captures. The mechanism of this coordination is unknown. If it is transient, it is termed accrochage; if it persists, it is called synchronization (1). An electrocardiogram recorded 5 hours before this one also showed isorhythmic atrioventricular dissociation, but it was incomplete with occasional capture of the ventricles by the sinus-initiated impulses. The following day there was sinus rhythm with marked sinus arrhythmia and P waves indicating left atrial enlargement. Otherwise the electrocardiogram resembled the one in the figure.
Accelerated junctional rhythm, the underlying mechanism of this patient's atrioventricular dissociation, usually occurs in patients with structural heart disease, as was the case in our patient with diabetes mellitus, systemic arterial hypertension, and coronary arterial disease. The rhythm was present before the procedure as well as afterwards, so the cardiac catheterization and coronary angioplasty with stenting appear to have played no pathogenic role.
References
- 1.Surawicz B, Knilans TK. Chou's Electrocardiography in Clinical Practice: Adult and Pediatric. 5th ed. Philadelphia: WB Saunders; 2001. pp. 367–388. [Google Scholar]
- 2.Bar FW, den Dulk K, Wellens HJJ. Atrioventricular dissociation. In: Macfarlane PW, Lawrie TDV, editors. Comprehensive Electrocardiology: Theory and Practice in Health and Disease. New York: Pergamon; 1989. pp. 933–959. [Google Scholar]