Abstract
There are limited data regarding gender-related differences in electrocardiographic (ECG) presentation in patients after myocardial infarction (MI) and prognostic value of ECG variables in women. We analyzed a series of ECG parameters in 838 patients (216 females and 622 males) using a standard ECG acquired 5-7 days after first MI, and evaluated their associations with gender and the risk of cardiac events defined as cardiac death, nonfatal MI, or unstable angina. Heart rate was faster and QTc duration was longer whereas QRS duration was shorter in females as compared to males. Females had more lateral ST depressions and more T wave inversions in anterior and lateral region. During mean 2-year follow-up, there were 138 events in males and 65 in females; females had 38% higher risk of recurrent events (adjusted hazard ratio HR=1.38, p=0.031). In multivariate Cox regression analysis, ST segment elevation in leads V1-4 on the 5th -7th day after MI was associated with increased risk of recurrent events in females (adjusted HR=2.16, p=0.003), but not in males (adjusted HR= 0.81, p=0.32). ST depressions in leads V5-6, I or AVL (adjusted HR=1.70, p=0.006) in males but not in females (adjusted HR=0.98, p=0.93) were identified as a risk factor for recurrent events. In conclusion, there are gender-related differences in ECG presentation and prognostic significance of ECG findings after MI. ST segment elevation in anterior leads is a significant predictor of events in females whereas ST depression in lateral leads is in males.
Epidemiological data indicate that females are affected by coronary artery disease approximately 10 years later than males.1 Mortality rates differ significantly between males and females.1,2 In all age groups, females had worse clinical outcomes when compared to males.2 Epidemiological data and population studies evaluated gender-related differences and predictive value of electrocardiographic (ECG) parameters.3-7 However, most of these studies concentrated on asymptomatic, relatively healthy individuals with limited data on the gender-related differences in baseline ECG in the setting of an acute myocardial infarction. There is a need for studies to demonstrate the value of ECG parameters for better risk stratification in women. We hypothesized that there are significant differences in ECG parameters between genders among survivors of myocardial infarction (MI), and that these parameters might have different association with the risk of cardiac events in males and females after MI. To test these hypotheses, we performed a retrospective analysis of ECG parameters from a large post-infarction study with a long-term follow-up.
Methods
The study population for this analysis consisted of patients enrolled in the multicenter Thrombogenic Factors and Recurrent Coronary Events (THROMBO) study. Detailed description of the THROMBO study has been published previously.8 Briefly, patients of either sex who were≥ 21 years (no upper age cutoff) had been admitted to a coronary care unit at 13 participating hospitals with a documented acute myocardial infarction (symptomatic, confirmed by cardiac enzymes, and with ECG changes), and who survived 2 months after an index MI were eligible for enrollment. The index acute MI could be either a first or a recurrent infarction. Between October 1, 1994, and June 30, 1997, 1,045 were enrolled in the study. Exclusion criteria for the THROMBO study included the following: presence of significant co morbid illness such as malignancy; severe hepatic, renal, or cerebrovascular disease; coronary artery bypass graft surgery during the hospital phase of index event; suspected noncompliance due to psychosocial reasons; refusal to sign the informed consent. In our analysis, we concentrated on 838 patients with an index event defined as a first acute MI.
The outcome cardiac event was defined as unstable angina pectoris requiring hospitalization (chest pain with ECG changes indicating ischemia), recurrent nonfatal myocardial infarction or cardiac death, whichever occurred first. The follow-up started after hospital discharge and was prospectively ascertained during 3.5 years of the study.
All ECG parameters were obtained from a standard 12-lead ECG recorded 5 to 7 days after the index MI, and were analyzed by central ECG core laboratory for the study (St. Luke Roosevelt Hospital, New York). The PR interval and QRS duration were measured in lead II. ECG abnormalities were defined according to the guidelines of ECG classification for post-infarction trials.9 ST depression was defined as ST-segment depression ≥1.0 mm, 80 ms beyond the J point. The atrial abnormalities were defined as a terminal deflection of the P wave at least 0.1 mV deep and 40 ms in duration in lead V1. The QT interval was measured manually from the beginning of the QRS complex to the end of the T wave in the limb lead II. Bazett's formula was used to obtain heart rate-corrected QT values (QTc). Automated system for ECG analysis was not used for the interval measurement. The nonspecific intra-ventricular conduction delay was defined as a QRS of at least 100 ms with presence of notches or slurring. (This definition was used by the ECG core lab of the study to acknowledge the presence of notches and slurring in QRS even with QRS not reaching 110-120 ms. When analysis was done using currently accepted definition (>100 ms) there were 6 patients who met this criterion in comparison to 22 patients using the core lab definition). The left bundle branch block and right bundle branch block were determined according to the usual accepted morphologic changes with the QRS ≥ 120 ms. The diagnosis of left ventricular hypertrophy required voltage for S wave in lead V2 plus R wave in lead V5 to be ≥ 35 mm and ST- T segment strain pattern in the lateral pre-cordial leads. Q waves were classified as pathologic if their duration was ≥ 30 ms. Myocardial infarction were classified as: 1. Q wave MI – significant Q waves in anterior, lateral or inferior regions with additional criteria of R loss in lateral leads and tall R in posterior infarction; 2. Non-Q-wave infarction – Q waves were absent and coved ST elevation and symmetric T wave inversions were present (J point elevation without upward coving of the ST segment does not satisfy this criteria); 3. ST depression and positive cardiac enzymes – horizontal or downsloping ST depression 1.00 mm deep 0.08 second after completion of the QRS in the absence of Q wave, hypertrophy or conduction disorders.
Baseline characteristics were compared using a chi-square test for dichotomous variables. Two-sample t-test was used for normally distributed continuous variables and two - sample Wilcoxon rank-sum test for not normally distributed variables. The logistic regression analysis model was used to estimate the strength of associations between ECG variables and gender. The association of different ECG parameters with the end point was examined using Kaplan Meier survival curves and the log-rank statistic p value. Multivariate analysis was performed using the Cox proportional hazards regression model. Stepwise selection was used to identify clinical predictors and a p value <0.10 was used for removing a variable in constructing baseline clinical model. Analyses were performed with the use of SAS software (version 9.1). A 2-sided P<0.05 was considered statistically significant.
Results
Among 838 patients enrolled in the study with an index event defined as first acute MI, there were 216 females (26%) and 622 males (74%). The baseline clinical variables are described in Table 1A. Women were older, had more diabetes and hypertension, and presented more frequently with pulmonary congestion than men. Thrombolytic therapy was used less frequently in women. Men in the study were more likely to be Caucasian and current or ex-smokers. Heart rate at baseline ECG was faster, QTc was longer, and QRS duration was shorter in females compared to males, whereas QRS voltage was higher in males than females (Table 1B). There was no difference in the frequency of Q wave MI and non-Q wave MI between males and females. However, males had more Q waves in inferior leads than females (44% vs. 35%, p=0.03). The presence of Q waves in other locations was similar in males and females.
Table 1.
| Table 1A. Clinical Characteristics of Females and Males after Myocardial Infarction. | |||
|---|---|---|---|
| Variables | Females (N=216) |
Males (N=622) |
P value |
| Age (years) | 63±13 | 57±11 | <0.001 |
| Caucasian | 71% | 78% | 0.014 |
| African American | 19% | 12% | |
| Other | 10% | 10% | |
| Diabetes mellitus | 22% | 13% | 0.001 |
| Hypertension | 59% | 38% | <0.001 |
| Ever Smoker | 51% | 62% | 0.004 |
| Ejection fraction (%) * | 50 | 50 | 0.290 |
| Event type: | |||
| Q wave MI | 47% | 53% | |
| Non-Q wave MI | 39% | 32% | 0.250 |
| ST segment depression with elevated cardiac enzymes | 14% | 15% | |
| Pulmonary Congestion | 25% | 14% | 0.001 |
| Angina pectoris within 1 month prior to the index event | 35% | 29% | 0.110 |
| Coronary angioplasty | 11% | 13% | 0.650 |
| Use of intravenous thrombolytic | 28% | 37% | 0.040 |
| Medical therapy | |||
| Aspirin | 77% | 85% | 0.02 |
| Beta-blockers | 75% | 78% | 0.45 |
| Angiotension converting enzyme inhibitors | 41% | 33% | 0.05 |
| Calcium channel blockers | 19% | 19% | 0.91 |
| Diuretics | 27% | 10% | <0.0001 |
| Statins | 29% | 33% | 0.34 |
| Oral anticoagulant (warfarin or coumadin) |
17% | 18% | 0.70 |
| Table 1B. Electrocaridographic Parameters in Females and Males after Myocardial Infarction. | |||
|---|---|---|---|
| ECG Parameters | Females (N=216) |
Males (N=622) |
|
| Heart Rate (bpm) * | 74 | 70 | <0.001 |
| QRS (msec)* | 80 | 90 | <0.001 |
| QTc (msec)* | 441 | 419 | <0.001 |
| Sum of voltage SV2 and RV5 (mm) | 20±9 | 22±8 | 0.046 |
| Atrial Abnormalities | 12% | 9% | 0.170 |
| Frequencies of Q waves | |||
| Anterior (V1-4) | 27% | 27% | 0.850 |
| Lateral (V4-6, I, aVL) | 11% | 13% | 0.400 |
| Inferior (II, III, aVF) | 35% | 44% | 0.030 |
| Frequencies of ST depression | |||
| Anterior (V1-4) | 4% | 2% | 0.14 |
| Lateral (V4-6, I, aVL) | 36% | 19% | <0.001 |
| Inferior (II, III, aVF) | 5% | 8% | 0.10 |
| Frequencies of T wave Inversion | |||
| Anterior (V1-4) | 38% | 29% | 0.012 |
| Lateral (V4-6, I, aVL) | 63% | 52% | 0.004 |
| Inferior (II, III, aVF) | 48% | 48% | 0.950 |
- Wilcoxon rank-sum test used
When analyzing changes in ST-T segment, females had ST segment depression in lateral leads (V5-6, I, aVL) significantly more often as compared to males. There was no significant difference in the frequency of ST depression in other locations. Women had more frequent T wave inversions in anterior and lateral location with no difference in inferior location in comparison to men.
In multivariate logistic regression analysis, the following clinical variables were associated with female gender: advanced age, history of diabetes, and hypertension. When ECG parameters were tested after adjustment for the above clinical variables, lateral ST depression, faster heart rate, and longer QTc were positively associated with female gender, whereas longer QRS duration and higher sum of SV2 and RV5 voltage were more likely to occur in males (Table 2).
Table 2. Clinical and Electrocardiographic Parameters Associated with Female Gender in the Multivariate Logistic Regression Analysis.
| Variables | Odds Ratio | 95% CI | P value |
|---|---|---|---|
| Age | 1.02 | 1.00- 1.04 | 0.008 |
| Diabetes mellitus | 1.52 | 0.96- 2.41 | 0.07 |
| Hypertension | 2.11 | 1.43- 3.10 | <0.001 |
| ECG Variable | |||
| Heart Rate (by 10 beats increase) | 1.70 | 1.43- 2.02 | <0.001 |
| Lateral ST Depression | 2.34 | 1.54- 3.56 | <0.001 |
| Voltage (SV2+RV5) (mm) | 0.96 | 0.94- 0.99 | 0.003 |
| QTc Interval (by each 100mm) | 1.22 | 1.15- 1.31 | <0.001 |
| QRS Interval (by each 100mm) | 0.70 | 0.60- 0.82 | <0.001 |
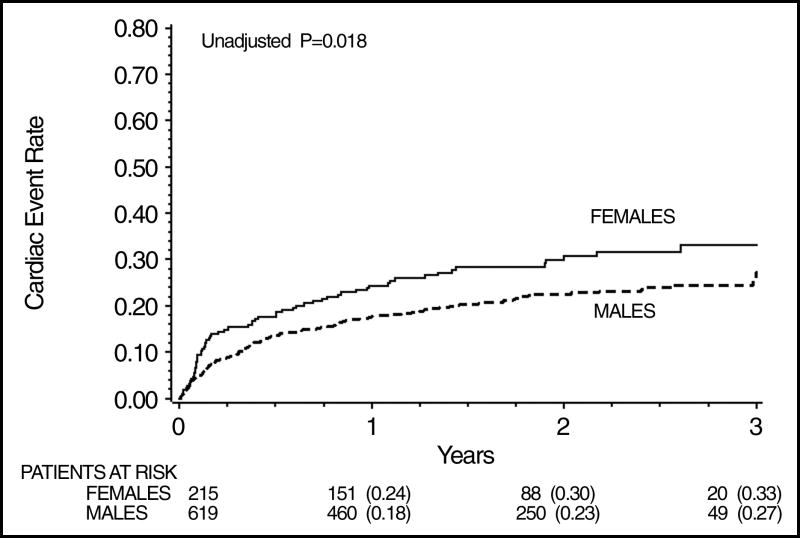
During mean follow-up time of 688 ± 279 days, there were 138 cardiac events in males and 65 in females (events rate males vs. females 22% vs. 30%, p=0.02). There were 79 combined end-points of death or non-fatal MI (10% in males vs. 8% in females, p=0.52) and 10 cardiac deaths (1% in males vs. 1% in females, p=0.71). Females had a higher likelihood of combined cardiac events compared to males (Figure 1).
Figure 1.
Cumulative probability of recurrent events by the gender in patients after MI.
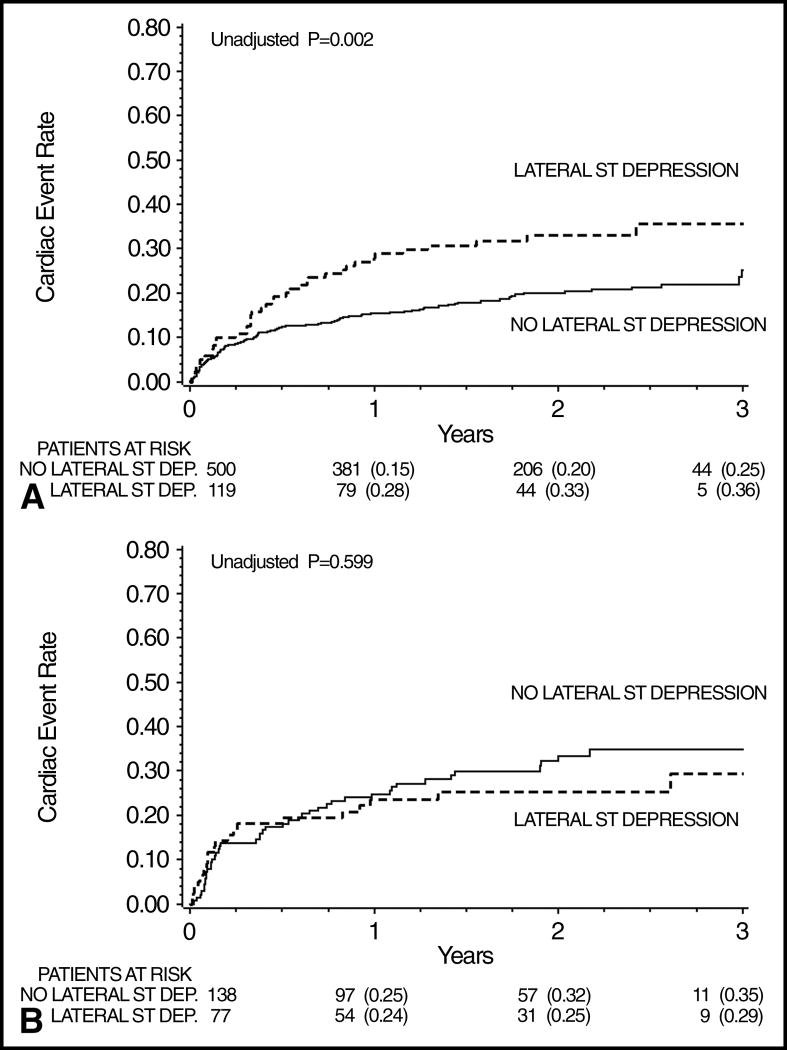
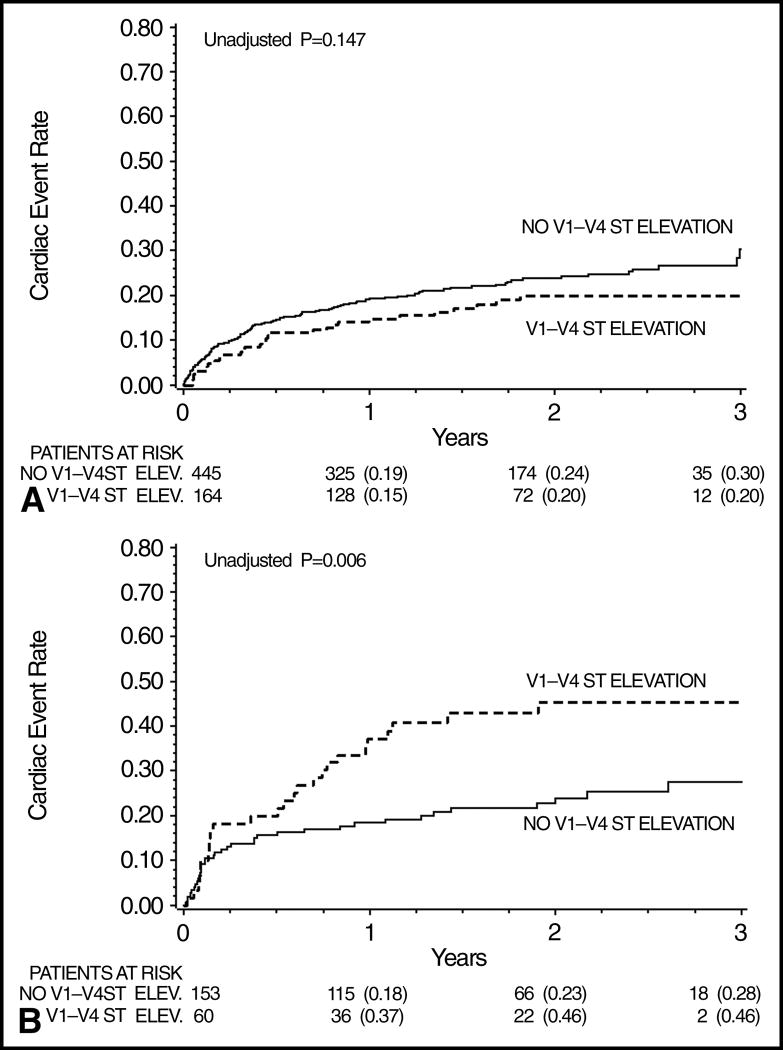
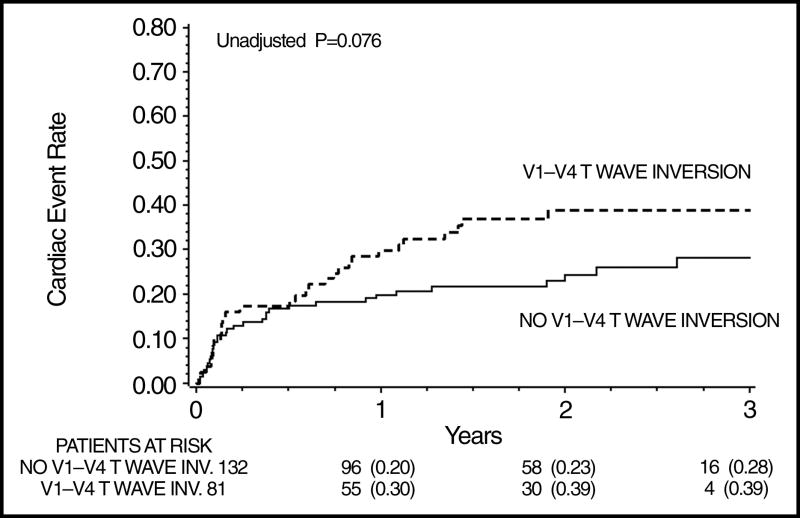
Age, Caucasian ethnicity, history of diabetes mellitus, hypertension, pulmonary congestion, type of MI (Q wave vs. non-Q wave), history of smoking, and therapies with ACE-I, aspirin, beta-blockers and diuretics were considered in stepwise Cox analyses model. The only predictive variable that entered the model was the type of MI (Q wave vs. non-Q wave). After adjustment for the type of index event (Q wave MI vs. non-Q wave), females had a 38% higher risk of cardiac events compared to males (adjusted HR= 1.38, 95% CI 1.03-1.86, p= 0.03). Among all tested ECG variables, only lateral ST depression in males (Figure 2A and 2B) and persistent anterior ST segment elevation in females were associated with significantly increased risk of recurrent cardiac events (Figure 3A and 3B). In addition, anterior T wave inversions in females had a positive trend toward worsened outcome (Figure 4). After adjusting for type of index event (Q wave vs. non-Q wave), lateral ST depressions among males and persistent anterior ST elevations among females were the only significant ECG predictors of recurrent cardiac events. The interaction between gender and anterior ST segment elevation was significant. Anterior T wave inversions did not reach statistical significance level (Table 3).
Figure 2.
Figure 2A Cumulative probability of recurrent events among males by presence of lateral ST depressions.
Figure 2B Cumulative probability of recurrent events among females by presence of lateral ST depressions.
Figure 3.
Figure 3A Cumulative probability of recurrent events among males by presence of ST elevation in V1-V4 on the 5th -7th post-MI day.
Figure 3 B Cumulative probability of recurrent events among females by presence of ST elevation in V1-V4 on the 5th -7th post-MI day
Figure 4.
Cumulative probability of recurrent cardiac events among females by presence of T waves inversions in leads V1-4.
Table 3. Multivariate Cox Analysis of Electrocardiographic Parameters in Predicting Cardiac Events in Males and Females After Myocardial Infarction.
| Variable | Female | Male | P for Interaction* | ||||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | ||
| Anterior ST elevation | 2.16 | 1.30-3.59 | 0.003 | 0.81 | 0.54-1.22 | 0.32 | 0.003 |
| Lateral ST depression | 0.98 | 0.58-1.66 | 0.93 | 1.70 | 1.16-2.47 | 0.006 | 0.10 |
| Anterior T wave inversion | 1.51 | 0.87-2.61 | 0.14 | 0.88 | 0.55-1.41 | 0.60 | 0.093 |
Adjusted for MI type (Q wave vs. non-Q wave).
Denotes the interaction value for the difference in the risk between males and females for anterior ST elevation, lateral ST depression and anterior T wave inversion.
Discussion
In our analysis, females had faster heart rate, shorter QRS duration and longer QTc than males. Lateral ST segment depression and T wave inversion in anterior and lateral leads were more common in females, whereas inferior Q waves were more common in males. However, there was no difference in overall frequency of Q- wave MI versus non-Q wave MI. Women had higher risk of cardiac events than men. Different ECG variables in men vs. women were associated with cardiac events: lateral ST depression was an independent risk factor in males, while persistent anterior ST elevation was in females.
Several studies demonstrated the gender-related ECG differences in healthy subjects: women had shorter PR interval and QRS duration,3 lower ECG voltage,10-13 longer QT interval,13-15 and more prevalent ST-segment changes.5,6,16 The question asked in our analysis was whether an acute MI alters gender-related differences in ECG parameters. Our findings indicate that heart rate, QRS duration, QRS voltage, and QTc duration remain different in males and females even in the setting of recent MI. The ECG differences by gender among post-MI patients are similar to those observed among healthy individuals.
Previous studies evaluated the prognostic value of ECG parameters in large cohorts of relatively healthy and asymptomatic individuals; Liao et al.4 estimated that ST-T abnormalities are associated with cardiac death among men rather than women. De Bacquer et al.5 concluded that there is similar predictive value of major ECG abnormalities for both men and women free from coronary heart disease. Greenland et al.6 estimated that ST-segment depression and/or T wave abnormalities influence long-term cardiovascular mortality in both genders, however, T wave abnormalities were more significant in males while ST-T abnormalities were more significant in females. In the Women's Ischemia Syndrome Evaluation (WISE) Study (57% of women with angiographically significant epicardial artery stenosis) QRS interval, QTrr (age- and gender adjusted QT interval), QRS-T angle (spatial electrical angle between the QRS complex and the T wave) and ST segment depression in lead V5 were independently associated with cardiac events 7. Rautaharju et al. 17,18 found that ECG parameters such as old MI, wide QRS-T angle, high QRS nondipolar voltage, reduced heart rate variability and QT prolongation, were associated with higher mortality in women.
In contrast to these studies, our analysis concentrated on patients recovering from the first acute myocardial infarction. Anterior ST segment elevation on the 5-7th day after acute MI was associated with higher risk among females. This ECG finding could be associated with ventricular aneurysm, left ventricular hypertrophy or as shown in the reperfusion studies less myocardial salvage, impaired microvascular reperfusion and poor left ventricular recovery. 19-21 Unfortunately, we do not have echocardiographic or nuclear scan data that could confirmed or exclude any of those possibilities. In men, lateral ST depressions were associated with events. Lateral ST depressions and atrial abnormalities were the ECG parameters predictive for events in total population of the THROMBO study.23 It has been noted that ST depression might represent the severity of coronary artery disease, degree of LV dysfunction and reversible ischemia. 24-25
Limitations of our study include its retrospective character and low percentage of patients undergoing primary angioplasty and lower percentage of women than men, undergoing any reperfusion therapy. Similar analyses need to be repeated in patients treated according to modern guidelines.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lerner DJ, Kannel WB. Patterns of coronary artery heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J. 1986;111:383–390. doi: 10.1016/0002-8703(86)90155-9. [DOI] [PubMed] [Google Scholar]
- 2.Weaver WD, White HD, Wilcox RG, et al. GUSTO-I Investigators. Comparisons of characteristics and outcomes among women and men with acute myocardial infarction treated with thrombolytic therapy. JAMA. 1996;275:777–782. [PubMed] [Google Scholar]
- 3.Simonson E, Bluckburn H, Puchner TC, Eisenberg P, Ribeiro F, Meja M. Sex difference in the electrocardiogram. Circulation. 1960;23:598–601. [Google Scholar]
- 4.Liao Y, Liu K, Dyer A, Schoenberger JA, Shekelle RB, Collette P, Stamler J. Sex differential in the relationship of electrocaridographic ST-T abnormalities to risk of coronary death: 11.5 year follow-up findings of the Chicago Heart Association Detection Project in Industry. Circulation. 1987;75(2):347–352. doi: 10.1161/01.cir.75.2.347. [DOI] [PubMed] [Google Scholar]
- 5.De Bacquer D, De Becker G, Kornitzer M, Blackburn H. Prognostic value of ECG finding for total, cardiovascular disease, and coronary heart disease death in men and women. Heart. 1998;80:570–577. doi: 10.1136/hrt.80.6.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenland P, Xie X, Liu K, Colangelo L, Liao Y, Daviglus M, Agulnek AN, Stamler J. Impact of minor electrocaridographic ST-segment and/or T-wave abnormalities on cardiovascular mortality during long-term follow-up. Am J Cardiol. 2003;91(9):1068–1074. doi: 10.1016/s0002-9149(03)00150-4. [DOI] [PubMed] [Google Scholar]
- 7.Triola B, Olson MB, Reis SE, Rautaharju P, Merz CNB, Kelsey SF, Shaw LJ, Sharaf BL, Sopko G, Saba S. Electrocaridographic predictors of cardiovascular outcome in women. J Am Coll Cardiol. 2005;46(1):51–56. doi: 10.1016/j.jacc.2004.09.082. [DOI] [PubMed] [Google Scholar]
- 8.Moss AJ, Goldstein RE, Marder VJ, Sparks CE, Oakes D, Greenberg H, Weiss HJ, Zareba W, Brown MW, Liang CS, Lichstein E, Little WC, Gillespie JA, Van Voorhees L, Krone RJ, Bodenheimer MM, Hochman J, Dwyer EM, Jr, Arora R, Marcus FI, Watelet LF, Case RB. Thrombogenic factors and recurrent coronary events. Circulation. 1999;99:2517–2522. doi: 10.1161/01.cir.99.19.2517. [DOI] [PubMed] [Google Scholar]
- 9.Greenberg H, Gillespie J, Dwyer EM., Jr A new electorcardiographic classification for post-myocardial infarction clinical trials. Am J Cardiol. 1987;59:1057–1063. doi: 10.1016/0002-9149(87)90848-4. [DOI] [PubMed] [Google Scholar]
- 10.Casale PN, Devereux RB, Alonso DR, Campo E, Kligfield P. Improved sex-specific criteria of left ventricular hypertrophy for clinical and computer interpretation of electrocardiograms: validation with autopsy findings. Circulation. 1987;75:565–572. doi: 10.1161/01.cir.75.3.565. [DOI] [PubMed] [Google Scholar]
- 11.Okin PM, Roman MJ, Devereux RB, Kligfield P. Gender differences and the electrocardiogram in left ventricular hypertrophy. Hypertension. 1995;25:242–249. doi: 10.1161/01.hyp.25.2.242. [DOI] [PubMed] [Google Scholar]
- 12.Levy D, Bailey JJ, Garrison RJ, Horton MR, Bak SM, Lyons D, Castelli WP. Electrocardiographic changes with advancing age: a cross-sectional study of the association of age with QRS axis, duration and voltage. J Electrocardiol. 1987;20(suppl):44–47. [PubMed] [Google Scholar]
- 13.Chen CY, Chiang BN, Macfarlane PW. Normal limits of the electrocardiogram in a Chinese population. J Electrocardiol. 1989;22:1–15. doi: 10.1016/0022-0736(89)90018-6. [DOI] [PubMed] [Google Scholar]
- 14.Merri M, Benhorin J, Alberti M, Locati E, Moss AJ. Electrocaridographic quantification of ventricular repolarization. Circulation. 1989;80:1301–1308. doi: 10.1161/01.cir.80.5.1301. [DOI] [PubMed] [Google Scholar]
- 15.Smetana P, Batchvarov VN, Hnatkova K, Camm AJ, Malik M. Sex differences in repolarization heterogeneity and its circadian pattern. Am J Physiol Heart Circ Physiol. 2002;282:H1889–H1897. doi: 10.1152/ajpheart.00962.2001. [DOI] [PubMed] [Google Scholar]
- 16.Dellborg M, Herlitz J, Emanuelsson H, Sweedberg K. ECG changes during myocardial ischemia: differences between men and women. J Electrocardio. 1994;27(suppl):42–45. doi: 10.1016/s0022-0736(94)80042-1. [DOI] [PubMed] [Google Scholar]
- 17.Rautaharju PM, Kooperberg C, Larson JC, LaCroix A. Electorcardiographic abnormalities that predict coronary heart disease events and mortality in postmenopausal women. The Women's Health Initiative. Circulation. 2006;113:473–480. doi: 10.1161/CIRCULATIONAHA.104.496091. [DOI] [PubMed] [Google Scholar]
- 18.Rautaharju PM, Calhoun HP, Chaitman BR. NOVACODE serial ECG classification system for clinical trials and epidemiologic studies. J Electrocardiol. 1992;24(Suppl):179–187. doi: 10.1016/s0022-0736(10)80041-x. [DOI] [PubMed] [Google Scholar]
- 19.Malelzky S, Novikov M, Gruberg L, Freimark D, Feinberg M, Elian D, Novikov I, Di Segni E, Agranat O, Har-Zahav Y, Rabinowitz B, Kaplinsky E, Hod H. The significance of persistent ST elevation versus early resolution of ST segment elevation after primary PTCA. J Am Coll Cardiol. 1999;34(7):1932–1938. doi: 10.1016/s0735-1097(99)00466-0. [DOI] [PubMed] [Google Scholar]
- 20.Claeys MJ, Bosmans J, Veenstra L, Jorens P, De Raedt H, Vrints CJ. Determinants and prognostic implications of persistent ST-segment elevation after primary angioplasty for acute myocardial infarction. Importance of microvascular reperfusion injury on clinical outcome. Circulation. 1999;82(4):465–470. doi: 10.1161/01.cir.99.15.1972. [DOI] [PubMed] [Google Scholar]
- 21.Lee SG, Cheong JP, Shin JK, Kim JW, Park JH. Persistent ST-segment elevation after primary stenting for acute myocardial infarction: its relation to left ventricular recovery. Clin Cardiol. 2002;25(8):372–377. doi: 10.1002/clc.4950250806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gottlieb S, Harpaz D, Shotan A, Boyko V, Leor J, Cohen M, Mandelzweig L, Mazouz B, Stern S, Behar S. Sex differences in management and outcome after acute myocardial infarction in the 1990s: A prospective observational community-based study. Israeli Thrombolytic Survey Group. Circulation. 2000;102(20):2484–2490. doi: 10.1161/01.cir.102.20.2484. [DOI] [PubMed] [Google Scholar]
- 23.Perkiomaki JS, Zareba W, Greenberg HM, Moss AJ. Usefulness of standard electrocaridographic parameters for predicting cardiac events after acute myocardial infarction during modern treatment era. Am J Cardiol. 2002;90(3):205–209. doi: 10.1016/s0002-9149(02)02455-4. [DOI] [PubMed] [Google Scholar]
- 24.Dwyer EM, Jr, Case RB, Gillespie JA, Greenberg HM, Krone RJ, Lichstein E, Moss AJ, Multicenter Myocardial Ischemia Research Group Adverse prognosis of ST depression on the resting electrocardiogram in stable patients following acute myocardial infarction: an analysis of the basis for this association. Ann Noninvasive Electrocardiol. 1996;1:54–62. [Google Scholar]
- 25.Moss AJ, Goldstein RE, Hall WJ, Bigger JT, Jr, Fleiss JL, Greenberg H, Bodenheimer M, Krone RJ, Marcus FI, Wackers FJ, Multicenter Myocardial Ischemia Research Group Detection and significance of myocardial ischemia in stable patients after recovery from an acute coronary event. JAMA. 1993;269:2379–2385. [PubMed] [Google Scholar]