Abstract
Aims:
We investigated the effects of the nuclear factor kappa B (NFκB) blocker pyrrolidine dithiocarbamate (PDTC) on high-fat diet (HFD)-induced metabolic and renal alterations in obese and lean Zucker rats (OZR and LZR, respectively).
Main methods:
Rats were fed a HFD resembling the typical “Western” diet or a regular diet (RD) and allowed free access to tap water or tap water containing PDTC (150 mg/kg body weight) for 10 weeks; rats were then sacrificed. Total ROS production rates were measured using electron paramagnetic resonance spectroscopy, and superoxide production was measured with lucigenin assay. Blood, plasma, and urine were analyzed. Semi-quantitative reverse transcriptase-polymerase chain reaction and electrophoretic mobility shift assay were conducted to assess NFκB mRNA levels and DNA binding activities, respectively; immunofluorescence was performed to assess protein levels.
Key findings:
OZR-HFD rats exhibited significantly higher levels of total renal cortical reactive oxygen species production, plasma lipids, insulin, C-reactive protein, blood urea nitrogen, creatinine, and urinary albumin excretion than all other groups (p<0.05); these changes were accompanied by a significant decrease in plasma high density lipoprotein levels (p<0.05). Gene expression levels of desmin, cytokine and oxidative stress genes were significantly higher in the renal cortical tissues of OZR-HFD; NFκB p65 DNA binding activity was also significantly higher in these animals. PDTC attenuated these changes.
Significance:
Our data suggest that NFκB blockade may prove beneficial in treating the nephropathy often associated with metabolic syndrome.
Keywords: Metabolic syndrome, oxidative stress, kidney, diet
INTRODUCTION
In metabolic syndrome (MetS), underlying factors, such as obesity and insulin resistance, give rise to several interrelated metabolic risk factors, including dyslipidemia, hypertension, and hyperglycemia (Reaven 1988; Grundy, Cleeman et al. 2005). The risks for developing type 2 diabetes (DM) and renal dysfunction increase dramatically as the number of MetS components in the patient increase (Mundy, Haas et al. 2007). Diabetic nephropathy occurs in 30% - 40% of diabetics, and is the leading cause of end-stage renal disease (kidney failure requiring transplantation or dialysis) in the United States (Friedman and Friedman 2007).
Four risk factors for MetS (dyslipidemia, hyperglycemia, obesity, and hypertension) are each independently characterized by increased oxidative stress and a proinflammatory state (Bae, Bassenge et al. 2001; Keaney, Larson et al. 2003; Riccardi, Giacco et al. 2004; Ridker, Wilson et al. 2004; Fortuno, San Jose et al. 2006; Giugliano, Ceriello et al. 2006; Picchi, Gao et al. 2006; Mundy, Haas et al. 2007; Ceriello 2008). Further, an atherogenic diet (high in saturated fat and/or cholesterol), which resembles the typical “Western” diet (Kris-Etherton, Eckel et al. 2001; Mansouri, Bauge et al. 2008), is also known to exacerbate oxidative stress and inflammation and contribute to MetS (Riccardi, Giacco et al. 2004; Grundy, Cleeman et al. 2005). The transcription factor nuclear factor kappa B (NFκB) is required to maximize transcription of several pro-inflammatory mediators believed to be important in the inflammatory response. These include cytokines such as IL-1β, IL-6 and TNF-α, chemokines such as monocyte chemoattractant protein-1 (MCP-1) and enzymes such as inducible nitric oxide synthase (iNOS) (Blackwell and Christman 1997; Christman, Lancaster et al. 1998; Christman, Blackwell et al. 2000). Regulation of these molecules occurs predominantly at the transcriptional level; thus, it has been inferred that NFκB is a critical intracellular mediator of the inflammatory cascade (Christman, Blackwell et al. 2000) in several chronic inflammatory conditions, including metabolic syndrome and nephritis (Guijarro and Egido 2001; de Mello, Kolehmainen et al. 2008; Li, Reddy et al. 2008). However, the exact role of NFκB in contributing to the renal and metabolic disturbances seen in metabolic syndrome remains unknown.
The obese Zucker rat (OZR) shares many characteristics with human MetS (such as insulin resistance, obesity, inflammation and hyperlipidemia) and spontaneously develops nephropathy, and is therefore considered a model of metabolic syndrome, type 2 DM, and diabetic nephropathy (Coimbra, Janssen et al. 2000; Gassler, Elger et al. 2001). OZR develop glomerular hypertrophy by approximately 3 months of age (Lavaud, Michel et al. 1996), and albuminuria around 14 weeks of age (Kasiske, Cleary et al. 1985); however, they don't exhibit glomerulosclerosis until 6-7 months of age (Kasiske, Cleary et al. 1985; Danis and Yang 1993). The OZR is also known to exhibit increased oxidative stress (Banday, Marwaha et al. 2005; Russo, Del Mese et al. 2008), which likely has a role in some of the renal injury seen in these animals (Chander, Gealekman et al. 2004; Banday, Marwaha et al. 2005).
An atherogenic diet is known to perpetuate some components of MetS; thus, we fed young OZR (fa/fa) and heterozygous LZR (fa/+) this type of diet for ten weeks, to induce oxidative stress and renal damage earlier in the life span, and assessed metabolic and renal structural and functional parameters in these animals and in animals supplemented with PDTC. We examined the effects of high-fat feeding on the kidney, since the kidney is largely responsible for blood pressure control and for some of the excess glucose release seen in the hyperglycemia of MetS and DM (Meyer, Woerle et al. 2004), and since nephropathy is the most common cause of ESRD in diabetic patients (Schena and Gesualdo 2005; Friedman and Friedman 2007). We quantified ROS and superoxide production in renal cortical tissue and histologically evaluated glomeruli from all groups, to test the hypothesis that PDTC treatment would attenuate high-fat diet-induced renal and metabolic changes, and improve renal function and metabolic profiles in Zucker rats.
MATERIALS AND METHODS
Animals
Five-week old heterozygous LZR (fa/+) and homozygous OZR (fa/fa), with initial body weights of approximately 120 grams, were purchased from Harlan and housed in individual metabolic cages in a temperature- (23 ± 2° C), humidity-, and light- (12 hour light/dark cycle) controlled environment. Animals were fed either standard rodent chow (Rodent Diet 5001, with 14% fat derived calories, 29% protein-derived calories, and 58% carbohydrate-derived calories; LabDiet, Richmond, IN) or high-fat diet (HFD; modified AIN-93G, with 35% fat-derived calories, 15% protein derived calories, and 50% carbohydrate-derived calories; Dyets Inc., Bethlehem, PA), as previously described (Ebenezer, Mariappan et al. 2009), depending on group assignments.
Experimental design
Rats were divided into eight groups (n = 8 each) as follows: Group I: LZR-regular diet (LZR-RD); Group II: LZR high fat diet (LZR-HFD); Group III: LZR-RD-PDTC; Group IV: LZR-HFD-PDTC); Group V: OZR regular diet (OZR-RD); Group VI: OZR-HFD; Group VII: OZR-RD-PDTC); Group VIII: OZR-HFD-PDTC. Groups I and V were fed a regular diet and allowed free access to drinking water. Groups II and VI were fed a high fat diet and allowed free access to drinking water and groups III, IV, VII and VIII were allowed free access to water containing PDTC (150mg/kg) (Yu, Kang et al. 2007) for a total of 10 weeks. The PDTC dose used in these experiments is based on previous studies from our laboratory (Elks, Mariappan et al. 2008; Ebenezer, Mariappan et al. 2009). We chose to treat the animals from the age 5 weeks to age 15 weeks, since the first signs of renal damage (albuminuria and glomerular hypertrophy) are usually manifested by this age (Kasiske, Cleary et al. 1985; Lavaud, Michel et al. 1996). All experimental procedures were approved by the Louisiana State University Institutional Animal Care and Use Committee, and were in accordance with EC Directive 86/609/EEC of the European Commission.
Blood pressure measurements
Tail systolic and mean arterial blood pressures (SBP and MAP) were measured as previously reported (Guggilam, Haque et al. 2007; Elks, Mariappan et al. 2009).
Non-fasting blood, plasma, and urine analyses
Blood glucose was estimated with an Ascensia Elite glucometer according to the manufacturer's instructions (Bayer Corporation, Elkhart, IN, USA). Plasma insulin levels were measured using an ultra-sensitive rat insulin ELISA kit (Crystal Chem Inc., IL, USA) according to the manufacturer's instructions. Urine albumin concentration was determined using a Nephrat II Albumin Kit (Exocell, Inc., Philadelphia, PA, USA).
Blood urea nitrogen (BUN), creatinine (Cr), and BUN/Cr in plasma were determined using a Stat Profile Critical Care Xpress Analyzer (Nova Biomedical, USA) according to the manufacturer's instructions. C-reactive protein (CRP) was measured in plasma by a kit method (Alpco Diagnostics, NH, USA) according to the manufacturer's protocol. Levels of total cholesterol, high-density lipoprotein (HDL) and low-density lipoprotein/very low-density lipoprotein (LDL/VLDL) in plasma were quantified by a kit method (Biovision, CA, USA) as per the manufacturer's instructions.
Measurement of total ROS
Total ROS in the kidney cortex was measured by electron paramagnetic resonance spectroscopy (EPR) as described earlier (Elks, Mariappan et al. 2009).
Lucigenin assay
Lucigenin-enhanced chemiluminescence was used to measure NADPH-dependent superoxide production in kidney cortex as described earlier (Li, Gao et al. 2007; Ebenezer, Mariappan et al. 2009).
Histological measurements
Histological evaluations using light microscopy were performed as described earlier (Ebenezer, Mariappan et al. 2009). Longitudinal sections of one kidney from each animal were fixed in 10% buffered formalin, embedded in paraffin, cut into 5μm-thick sections, and then stained with H&E. Slides were then examined at 20X magnification and measurements of glomeruli and mesangial area and perimeter were performed. Forty glomeruli per section were randomly selected and measured by an observer (Z.S.) blinded to the phenotype and treatment of each rat.
Transmission electron microscopy
TEM studies were carried out as described earlier (Mariappan, Soorappan et al. 2007). Briefly, the kidney cortices were fixed in 2% paraformaldehyde and 1.25% glutaraldehyde in sodium cocadylate buffer, pH 7.4, post fixed in 1% OsO4, incubated overnight in uranyl acetate, dehydrated in an ethanol series, infiltrated, and embedded in epon-araldite resin. Thin (80nm) sections were cut on a MT-XL ultra tome (RMC Product, Tucson, AZ) and examined with a Jeol TEM-1011 electron microscope.
Immunofluorescence detection of desmin
Immunofluorescence studies were carried as previously described (Khaleduzzaman, Francis et al. 2007; Ebenezer, Mariappan et al. 2009). Lack of nonspecific staining was confirmed by using no primary antibody controls.
Real-time reverse transcriptase polymerase chain reaction (RT-PCR)
The mRNA expression levels for desmin, tumor necrosis factor alpha (TNF-α), nuclear factor kappa B (NFκB) and NOX-1 were assessed by real-time RT-PCR. Total RNA was extracted from kidney cortex using Trizol reagent (Invitrogen) and reverse-transcribed using oligo (dT) and reverse transcriptase as described earlier (Guggilam, Haque et al. 2007; Ebenezer, Mariappan et al. 2009).
Electrophoretic mobility shift assay (EMSA)
EMSA was performed as described previously (Cornelussen, Gupta et al. 2001). The NFκB sequence 5'AGT TGA GGG GAC TTT CCC AGG C-3′ and its complementary strand were used as the probes.
Statistical analysis
Values are expressed as means ± SEM. Statistical analysis was performed using one way ANOVA with repeated measurements. Post hoc pairwise mean comparisons were conducted with Bonferroni procedures. For lucigenin assay, a two-way repeated measures ANOVA was used. A p-value less than 0.05 were considered statistically significant.
RESULTS
Effects of PDTC on blood pressure and metabolic parameters
As expected, the systolic blood pressures (SBP) and mean arterial pressures (MAP) of OZR-HFD animals were significantly higher than those of OZR-RD and OZR-HFD-PDTC animals (Table 1). No changes in SBP or MAP were noted among any of the LZR. OZR-HFD animals also had significantly higher body weights and average weight gain than other OZR, with a similar trend observed in LZR. OZR-RD animals consumed a significantly higher quantity of food than all other OZR. PDTC treatment had no effect on food intake in LZR. OZR animals fed a HFD exhibited significant increases in liver, kidney, and abdominal fat pad weight (Table 1).
Table 1.
Blood pressures, food intakes, body and organ weights of rat groups.
| Parameters | LZR-RD | LZR-HFD | LZR-RD-PDTC | LZR-HFD-PDTC | OZR-RD | OZR-HFD | OZR-RD-PDTC | OZR-HFD-PDTC |
|---|---|---|---|---|---|---|---|---|
| SBP (mmHg) | 123.2 ± 3.3 | 125.2 ± 2.1 | 122.2 ± 4.1 | 119.1 ± 3.2 | 142.3 ± 4.2 | 158.6 ± 6.6* | 140.6 ± 4.8 | 133.1 ± 5.1‡ |
| MAP (mmHg) | 101.1 ± 4.1 | 102.4 ± 3.1 | 102.1 ± 2.6 | 99.1 ± 1.4 | 126.1 ± 5.4 | 130.8 ± 5.4* | 125.6 ± 4.1 | 108.2 ± 6.1‡ |
| Body weight (g) | 377 ± 2.24 | 400.5 ± 2.6§ | 281.60 ± 7.0 | 349.3± 2.6¶ | 544.8 ± 2.04 | 397.20 ± 12.6 | 615.60 ±7.92 | 551.0 ± 2.3‡ |
| Food intake (g) | 22.7±0.48 | 20.6±0.9 | 20.80 ± 1.18 | 19.75 ± 0.93 | 23.8 ± 1.1 | 18.5 ± 0.94* | 24.00 ± 0.80 | 16.5 ± 0.7‡ |
| Kidney (g) | 1.18±0.03 | 1.28±0.04 | 1.24 ± 0.02 | 1.17±0.01 | 1.47 ± 0.08 | 1.46±0.04* | 1.47 ± 0.03 | 1.40±0.04 |
| Liver (g) | 11.19±0.18 | 14.34±0.53§ | 11.67 ± 0.29 | 11.04±0.04¶ | 18.49 ± 0.83 | 24.3±0.98* | 19.66 ± 0.85 | 23.75±1.01 |
| Abdominal fat (g) |
2.5±0.16 | 16.55±0.93§ | 4.39 ± 0.33 | 5.08±0.80¶ | 19.10 ± 0.53 | 36.86±1.53* | 28.88 ± 0.84 | 32.49±0.82‡ |
| Weight gain (g) | 179.2 ± 5.4 | 282.3 ± 3.8§ | 122.40 ± 4.1 | 226 ± 2.7¶ | 381.2 ± 10.1 | 460.3 ± 11.3* | 179.20 ± 10.8 | 391 ± 7.1‡ |
The parameters of 15 week old rats were compared. Values are expressed as means ±S.E.M. Statistical analysis was performed using one way ANOVA with repeated measurements. Post hoc pairwise mean comparisons of each treatment group to its respective control were conducted with Dunnett's test. P ≤ 0.05 were considered significant.
p < 0.05 LZR-RD Vs LZR-HFD,
p < 0.05 LZR-HFD Vs LZR- HFD-PDTC,
p<0.05 OZR-RD vs. OZR-HFD;
p<0.05 OZR-HFD vs. OZR-HF-PDTC.
Effect of PDTC on plasma chemistries and plasma lipids
Plasma Cr, BUN, urine albumin excretion, and CRP (an inflammatory marker) were all significantly higher in OZR-HFD animals than in OZR-RD animals; PDTC normalized these parameters in OZR (Table 2). LZR–HFD animals also had increased plasma CRP levels when compared to LZR-RD animals, and PDTC treatment significantly attenuated this increase.
Table 2.
Metabolic characteristics and lipid profiles of lean and obese Zucker rats at study end.
| Parameter | LZR-RD | LZR-HFD | LZR-RD- PDTC |
LZR-HFD- PDTC |
OZR-RD | OZR-HFD | OZR-RD- PDTC |
OZR-HFD- PDTC |
|---|---|---|---|---|---|---|---|---|
| METABOLIC PARAMETERS | ||||||||
| Glucose (mg/dl) | 167.0 ± 4.7 | 217 ± 13.13§ | 177.40 ± 2.22 | 186.0 ± 7.9¶ | 200.67 ± 11.93 | 301.0 ± 9.60* | 200 ± 2.80 | 264.80 ± 8.71‡ |
| BUN(mg/dl) | 18 ± 0.5 | 26 ± 0.5§ | 11.82 ± 0.20 | 14 ± 0.89¶ | 20.80 ± 0.78 | 52.80 ± 1.13* | 14.36 ± 0.22 | 20.50 ± 0.88*‡ |
| Creatinine(mg/dl) | 0.48 ± 0.007 | 0.71 ± 0.03§ | 0.30 ± 0.01 | 0.41 ± 0.004¶ | 0.58 ± 0.026 | 1.12 ± 0.03* | 0.48 ± 0.01 | 0.7 ± 0.01‡ |
| BUN/Cre(mg/mg) | 37.19 ± 1.9 | 37.14 ± 1.8 | 36. 66± 1.32 | 34.14 ± 1.07 | 37.33 ± 2.14 | 47.70 ± 1.29* | 29.16 ± 1.01 | 28.58 ± 1.22‡ |
| CRP (ng/ml) | 29.50 ± 0.32 | 83.91 ± 2.33§ | 22.71 ± 0.59 | 54.32 ± 0.81¶ | 49.27 ± 0.54 | 96.17 ± 1.19* | 32.30 ± 0.59 | 58.42 ± 0.93‡ |
| Insulin (ng/ml) | 1.94 ± 0.01 | 10.41 ± 0.17§ | 2.21 ± 0.14 | 7.2 ± 0.31¶ | 22.78 ± 0.85 | 91.99 ± 2.72* | 21.40 ± 1.09 | 31.89 ± 1.2‡ |
| Urinary albumin excretion (UAE) |
11.13 ± 0.18 | 33.09 ± 0.23§ | 11.02 ± 0.62 | 16.15 ± 0.33¶ | 60.14 ± 1.42 | 116.2 ± 2.14* | 63.45 ± 2.35 | 76.23 ± 2.84‡ |
| PLASMA LIPIDS | ||||||||
| Triglycerides (mmol/L) |
1.39 ± 0.04 | 2.23 ± 0.04§ | 1.33 ± 0.21 | 0.81 ± 0.02¶ | 2.50 ± 0.08 | 10.55 ± 0.17* | 2.41 ± 0.9 | 1.45 ± 0.33‡ |
| Cholesterol (mmol/L) |
0.65 ± 0.06 | 0.90 ± 0.06§ | 0.38 ± 0.01 | 0.76 ± 0.03¶ | 1.65±0.07 | 4.27 ± 0.10* | 1.22 ± 0.03 | 1.86 ± 0.10‡ |
| HDL-c (mmol/L) | 0.25 ± 0.01 | 0.14 ± 0.01§ | 0.26 ± 0.004 | 0.40 ± 0.005¶ | 0.38 ± 0.01 | 0.27 ± 0.007* | 0.40 ± 0.01 | 1.26 ± 0.01‡ |
| VLDL-c (mmol/L) | 0.12 ± 0.02 | 0.19 ± 0.006§ | 0.033 ± 0.001 | 0.08 ± 0.004¶ | 0.17 ± 0.001 | 0.33 ± 0.009* | 0.088 ± 0.001 | 0.21 ± 0.01‡ |
The parameters of 15 week old rats were compared. Values are expressed as means ±S.E.M. Statistical analysis was performed using one way ANOVA with repeated measurements. Post hoc pairwise mean comparisons of each treatment group to its respective control were conducted with Dunnett's test. P ≤ 0.05 were considered significant.
p < 0.05 LZR-RD Vs LZR-HFD;
p < 0.05 LZR-HFD Vs LZR- HFD-PDTC,
p<0.05 OZR-RD vs. OZR-HFD,
p<0.05 OZR-HFD vs. OZR-HF-PDTC.
Plasma glucose and insulin levels were significantly higher in OZR-HFD animals when compared with OZR-RD animals. LZR–HFD animals also demonstrated increased plasma glucose and insulin levels when compared to LZR-RD animals. PDTC treatment significantly attenuated this increase in OZR and LZR.
Total cholesterol, VLDL cholesterol, and triglycerides were significantly higher in OZR-HFDD animals than OZR-RD animals, with a similar trend observed in LZR animals (Table 2). HDL levels were significantly lower in the OZR-HFD group when compared to the OZR-RD group, with the same trend observed in the LZR groups. PDTC restored HDL to near control levels in both OZR and LZR animals (Table 2).
Effects of PDTC on cortical total ROS and superoxide production
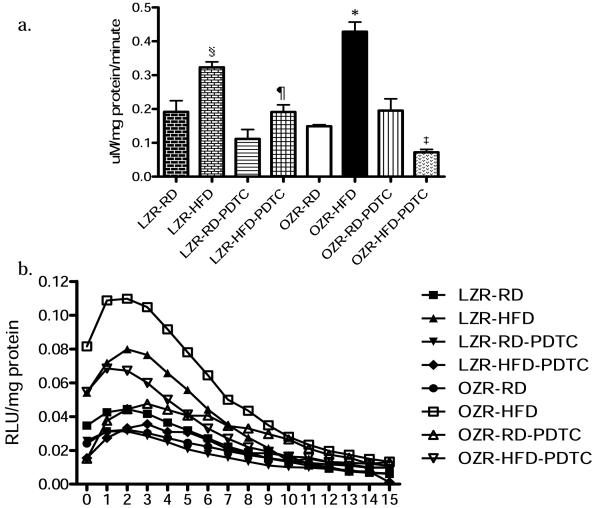
EPR measurements of total ROS production rates in kidney cortex appear in graphical form in Figure 1a. A significant increase in total ROS production was observed in renal cortical tissues of OZR-HFD animals when compared with those of OZR-RD animals; the same trend was noted in LZR. PDTC attenuated these increases in cortical ROS production.
Figure 1.
A) Total ROS production rates (in μM/minute) in cortical tissues of experimental animals as measured by the formation rate of CM· using CM-H. B) Superoxide production in cortical tissue homogenates from experimental animals as measured by lucigenin chemiluminescence. The parameters of 15 week old rats were compared. Values are expressed as means ±S.E.M. Statistical analysis was performed using one way ANOVA followed by a post hoc Bonferroni procedure. P ≤ 0.05 was considered significant. §p < 0.05 LZR-RD Vs LZR-HFD, ¶ p < 0.05 LZR-HFD Vs LZR- HFD-PDTC, *p<0.05 OZR-RD vs. OZR-HFD; ‡p<0.05 OZR-HFD vs. OZR-HF-PDTC.
OZR-HFD animals had higher levels of superoxide production than OZR-RD animals. The same trend was observed in LZR animals. Overall cortical superoxide production was lower in LZR than in OZR. In both OZR-HFD and LZR-HFD animals, PDTC treatment significantly reduced superoxide production. Results are presented graphically in Figure 1b.
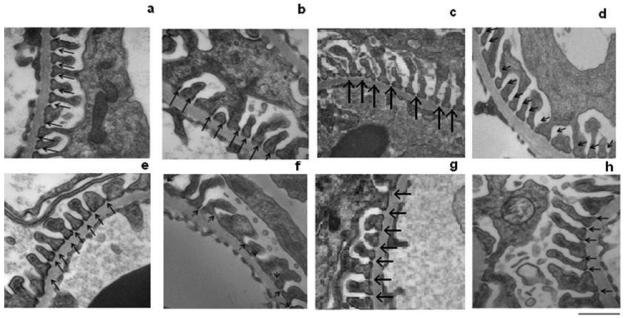
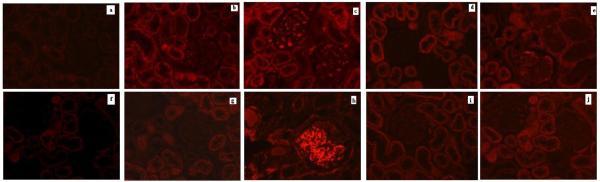
Podocyte morphology and glomerular ultrastructure
Podocyte morphology and glomerular ultrastructure were normal in both the LZR-RD groups and OZR-RD (Figures 2a and 2e). In OZR-HFD animals, podocyte injury was observed (Fig 2f). PDTC treatment normalized podocyte morphology in OZR-HFD animals (Fig 2h). The degree of podocyte damage was compared with the degree of fluorescence observed in the kidney cortex sections by using desmin (podocyte injury marker). Immunofluorescence studies show that desmin expression is absent in LZR-RD (Fig 3a) and OZR-RD (Fig 3b). LZR-HF (Fig 3e) animals showed slight increase in the expression of desmin when compared with LZR-RD or OZR-RD. In contrast, the OZR-HFD animals showed a significant expression of desmin in the glomeruli (Fig 3f). Treatment with PDTC significantly attenuated desmin expression both in LZR as well as OZR fed HFD (Figs. 3i and j).
Figure 2.
Transmission electron microscopy in kidney cortex after 10 weeks of experiments. (60 K magnification; Scale bar 500nm). (a) LZR-RD animals exhibited normal podocyte ultrastructure, including ordered, upright podocyte foot processes. (b) LZR-HFD animals exhibited podocyte damage. (c) LZR-RD-PDTC animals exhibited normal podocytes. (d) LZR-HFD-PDTC animals exhibited almost normal architecture. (e) OZR-RD animals also exhibited normal podocyte ultrastructure (f) OZR-HFD animals exhibited fusion of foot processes, variation of the width of the filtration slits, the broadening of foot processes with a reduction of the number of filtration processes per unit length, and multiple inclusion cysts or vacuoles within the cytoplasm of the podocytes. (g) OZR-RD-PDTC animals exhibited normal podocyte morphology (h) OZR-HFD-PDTC animals showed almost normal architecture.
Figure 3.
Immunofluorescence detection of desmin. (a) Negative control for LZR. (b) Desmin expression is absent in glomeruli from LZR-RD animals. (c) LZR-HFD animals had few desmin positive cells. (d) Absence of desmin expression in LZR-RD animals treated with PDTC. (e) LZR-HFD-PDTC animals showing very few desmin positive cells. (f) Negative control for OZR. (g) In OZR-RD animals, desmin expression was absent. (h) OZR-HFD animals exhibited a large number of desmin positive cells. (i) OZR-RD-PDTC animals had very few desmin positive glomerular cells. (j) PDTC therapy attenuated desmin expression in OZR-HFD animals. (Scale bar = 100 μm; original magnification = 20X).
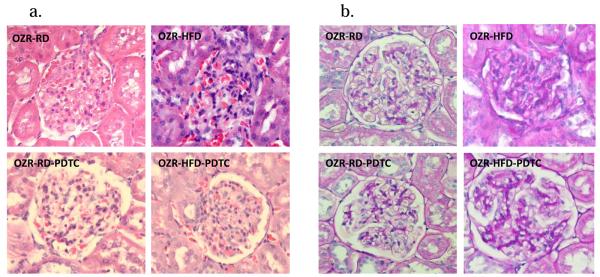
Glomerular histology
Glomerular diameter, area, and circumference were all significantly greater in the OZR-HFD animals than in any other group (Table 3). PDTC treatment attenuated these changes. Representative micrographs appear in Figure 4. No statistically significant changes in glomerular morphology were noted in any of the LZR groups, and they are therefore not included in Figure 4.
Table 3.
Glomerular morphological findings from lean and obese Zucker rats from each experimental group
| Parameter | LZR-RD | LZR-HFD | LZR-RD-PDTC | LZR-HFD-PDTC | OZR-RD | OZR-HFD | OZR-RD-PDTC | OZR-HFD- PDTC |
|---|---|---|---|---|---|---|---|---|
| Glomerular diameter (μm) |
8.32±0.08 | 7.45±0.02 | 8.65±0.14 | 8.05±0.19 | 8.93±0.01 | 10.68±0.67¥ | 8.77±0.40 | 8.77±0.06# |
| Glomerular area (μm2) |
55.96±0.62 | 45.01±0.28 | 58.50±2.21 | 54.88±4.12 | 64.60±0.01 | 70.30±1.95¥ | 63.31±2.36 | 61.77±0.31# |
| Glomerular circumference (μm) |
26.21±0.25 | 24.73±0.98 | 25.87±0.00 | 25.58±0.72 | 28.09±0.00 | 37.45±4.94¥ | 27.62±0.48 | 27.56±0.07# |
The parameters of 15 week old rats were compared. Values are expressed as means ± S.E.M. Statistical analyses were performed using one-way ANOVA with repeated measures followed by a Bonferroni procedure. P values ≤ 0.05 were considered significant.
p < 0.05 LZR-RD Vs LZR-HFD,
p < 0.05 LZR-HFD Vs LZR- HFD-PDTC,
p<0.05 OZR-RD vs. OZR-HFD,
p<0.05 OZR-HFD vs. OZR-HFD-PDTC.
Figure 4.
Glomeruli stained with A) hematoxylin and eosin (H&E) and B) periodic-acid Schiff (PAS) used for glomerular morphology measurements and analyses. Original magnification = 20X.
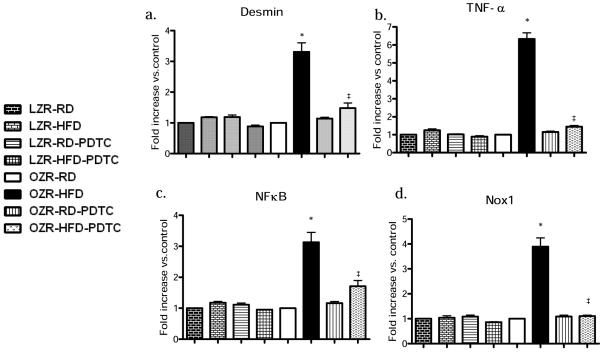
Gene expression profiles
In OZR-HFD animals, increases in expression of desmin, TNF-α, NFκB, and NOX-1 were seen in the kidney cortex (Figures 5a, b, c, and d, respectively); PDTC treatment significantly attenuated the increased expression of these genes. Although not significant, increased expression of desmin, TNF-α, and NFκB mRNA was seen in LZR-HFD rats (1.19-fold, 1.25-fold, and 1.18-fold increases, respectively, when compared to LZR-RD). PDTC attenuated the increases in gene expression seen in these animals.
Figure 5.
Effect of PDTC treatment on (A) desmin, (B) TNF-α, (C) NFκB and (D) NOX-1 gene expression levels. Values are expressed as mean±S.E.M. Statistical analysis was performed using one way ANOVA followed by a post hoc Bonferroni procedure. P ≤ 0.05 was considered significant. §p < 0.05 LZR-RD Vs LZR-HFD, ¶ p < 0.05 LZR-HFD Vs LZR- HFD-PDTC, *p<0.05 OZR-RD vs. OZR-HFD; ‡p<0.05 OZR-HFD vs. OZR-HF-PDTC.
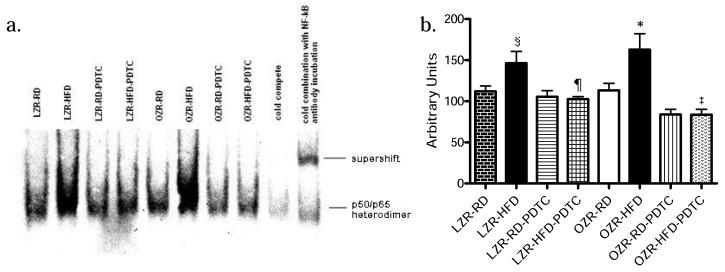
Electrophoretic mobility shift assay (EMSA)
NFκB p65 DNA binding activity was analyzed in renal cortical nuclear extracts with electrophoretic mobility shift assay (Figure 6a). Densitometry analysis revealed significantly higher NFκB p65 DNA binding activity in OZR-HFD animals than in OZR-RD animals (Figure 6b). The same trend was noted with LZR. PDTC attenuated the increases in NFκB p65 DNA binding activity.
Figure 6.
(A) Nuclear NFκB p65 DNA binding activity in LZR and OZR kidney cortex. The DNA-protein complex was resolved from the free-labeled DNA by electrophoresis on a 5% (W/V) native polyacrylamide gel. (B) Densitometric analysis of EMSA bands. Values are expressed as mean±S.E.M. Statistical analysis was performed using one way ANOVA followed by a post hoc Bonferroni procedure. P ≤ 0.05 was considered significant. §p < 0.05 LZR-RD Vs LZR-HFD, ¶ p < 0.05 LZR-HFD Vs LZR- HFD-PDTC, *p<0.05 OZR-RD vs. OZR-HFD; ‡p<0.05 OZR-HFD vs. OZR-HF-PDTC.
DISCUSSION
There is a need for a more thorough understanding of the mechanisms underlying the nephropathies seen in MetS and type 2 DM, as these diseases often result in end stage renal disease. We fed LZR and OZR a high-fat diet, which closely resembles the typical “Western” diet, to accelerate the progression of overt renal disease in MetS, and treated some animals with the NFκB blocker, pyrrolidine dithiocarbamate (PDTC). Our results suggest that HFD induces renal and metabolic alterations by increasing oxidative stress and inflammation, and that PDTC ameliorates these alterations.
These data, along with those from our previous study (Ebenezer, Mariappan et al. 2009), suggest that the renal alterations seen in MetS are driven by oxidative stress. Increased circulating glucose levels are known to increase oxidative stress by inducing excess production of mitochondrial ROS; these mitochondrial ROS can in turn activate other ROS pathways (Nishikawa, Edelstein et al. 2000). Further, the tissue renin-angiotensin system is upregulated in MetS; thus, increased renal angiotensin may induce ROS production by NAD(P)H oxidases (Coughlan, Thallas-Bonke et al. 2007). It is also likely that the overproduction of free radicals triggered excess free fatty acids in OZR-HFD animals to lead to enhanced production of conjugated dienes and lipid hydroperoxides (Inoguchi, Li et al. 2000). Both the NFκB-blocking and antioxidant properties of PDTC led to significant decreases in plasma cholesterol, triglycerides, and LDL, and a significant increase in HDL; these changes may be partly responsible for the improved histological parameters seen in OZR-HFR-PDTC animals.
The association between dyslipidemia and metabolic syndrome is well established (Mori, Kawano et al. 1996; Ritz and Stefanski 1996; Isomaa 2003; Kidambi, Kotchen et al. 2007). The increase in LDL cholesterol levels observed in OZR may be due to suppression of LDL receptor activity through lipid peroxidation. PDTC treatment decreased abdominal adipose tissue and total ROS in OZR, and also significantly decreased LDL cholesterol and increased HDL cholesterol in OZR. The changes seen in HDL cholesterol may due to a possible effect of PDTC on PPARa; it has been shown that inactivation of NFκB via activation of PPARa (Yamazaki, Kawano et al. 2008) leads to an increase in apolipoprotein-A1, and therefore, an increase in HDL (Morishima, Ohkubo et al. 2003; Ruan, Zheng et al. 2008). However, confirmatory experiments are needed before this conclusion can be made. Overall, these results suggest PDTC is beneficial in preventing the dyslipidemia associated with metabolic syndrome in OZR.
The phenotype that resulted from feeding a HFD to LZR was quite similar to that of the OZR. In the presence of a regular diet, however, the only appreciable differences in metabolic parameters between LZR and OZR were in plasma insulin and urinary albumin excretion. This can likely be explained by the younger ages of the animals. At age 15 weeks, OZR fed a regular diet exhibit hyperfiltration, which is a renal compensatory mechanism (Kasiske, Cleary et al. 1985); this compensation allows for maintenance of normal urine output, normal plasma creatinine, and normal BUN. Glomerulosclerosis and chronic renal disease generally are not seen in these animals until approximately 6 months of age (Kasiske, Cleary et al. 1985; Danis and Yang 1993).
One of the early signs of nephropathy in Zucker rats is enhanced urinary albumin excretion (Nishikawa, Edelstein et al. 2000). In this study, the OZR-RD and OZR-HFD groups showed significant increases in urinary albumin excretion. Microalbuminuria is associated with endothelial dysfunction, inflammation, and free radical generation (Nishikawa, Edelstein et al. 2000). In the present study, we observed increased urinary albumin excretion, along with increases in other inflammatory markers, which were associated with overproduction of total ROS and superoxide (Figures 1a and 1b) in OZR-HFD animals. The free radicals associated with inflammatory conditions are thought to contribute to MetS and insulin resistance (Coughlan, Thallas-Bonke et al. 2007), and are likely a major cause of the increased inflammation seen in the HFD-fed animals.
It is well-known that proinflammatory cytokines increase superoxide production, which in turn increases activation of NFκB, thereby leading to another cycle of increased proinflammatory cytokines and oxidative stress, thus amplifying the signal and resulting in end organ damage. This vicious cycle makes it difficult to determine whether the oxidative stress or increased NFκB activity comes first in our study. Nonetheless, our EMSA results demonstrate a significant increase in NFκB activity in kidney cortices of OZR-HFD and LZR-HFD animals (Figures 6a and 6b). These results are further supported with the increases in gene expression of desmin, TNF-α, NFκB, and NOX-1; total ROS production levels; and superoxide production (Figures 1a, 1b, and 4a-4d). We also saw differences in gene expression of desmin, TNF-α, NFκB, and NOX-1 between LZR-HFD and OZR-HFD animals, despite their having similar levels of oxidative stress. This may be because the OZR develops a basal level of oxidative stress at a very early age, while in the fa/+ LZR, oxidative stress will only develop in the presence of an external stimulus. Therefore, the OZR has higher oxidative stress at baseline, and, even though overall levels of oxidative stress are similar, the ending message levels of proinflammatory genes may differ.
Although the molecular mechanisms whereby NFκB blockade attenuates oxidative stress and improves metabolic abnormalities were not investigated in the present study, our results do suggest that alterations in pro-inflammatory cytokine expression and in metabolic parameters may affect renal structure and function in OZR fed a high fat diet. Our results clearly show the detrimental effects of ROS on metabolic syndrome and the protective effect of PDTC in attenuating oxidative stress. PDTC reduces total cholesterol and triglyceride, and also causes an increase in HDL levels. In addition, PDTC also seems to exert beneficial action by decreasing microalbuminuria, BUN, and creatinine levels. PDTC caused a 22 to 25 mmHg blood pressure reduction in OZR-HFD animals. This decrease in pressure could be responsible for the amelioration of renal dyfunction and prevention of the renal histological changes associated with high fat diet. The results obtained in this study indicate that renal lesions in OZR fed a high fat diet are well substantiated by biochemical and biophysical studies in a model of MetS and, further, are prevented by NFκB blockade.
In conclusion, we demonstrate for the first time that blockade of the NFκB pathway improves metabolic parameters and attenuates proinflammatory gene expression, thereby contributing to decreased oxidative stress and renoprotection. To the best of our knowledge, this is the first report on the role of NFκB blockade in preventing renal oxidative stress and increasing HDL levels in OZR fed a HFD. Blockade of the NFκB pathway may be a useful therapy for combating the renal and metabolic alterations associated with MetS.
Table 4.
Rat primers used for real time RT-PCR.
| Gene name | Primer Sequences |
|---|---|
| 18S | F: agttggtggagcgatttgtc |
| R: aacgccacttgtccctctaa | |
| Desmin | F: gtgaagatggccttggatgt |
| R: gctggtttctcggaagttga | |
| NFkB | F:ctctcgtcctcctccacaag |
| R:gtccatcctgcccataattg | |
| TNF-α | F: gtcgtagcaaaccaccaagc |
| R: tgtgggtgaggagcacatag | |
| NOX-1 | F: ccctggaacaagagatggac |
| R: attggtctcccaaaggaggt |
ACKNOWLEDGMENTS
These studies were supported by a grant from the National Heart Lung and Blood Institute (RO1 HL080544-01) for Dr. Joseph Francis. We sincerely thank Dr. Olga Borkhsenious for conducting TEM studies, and Ms. Sherry Ring for her assistance with tissue sectioning.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Bae J-H, Bassenge E, et al. Postprandial hypertriglyceridemia impairs endothelial function by enhanced oxidant stress. Atherosclerosis. 2001;155(2):517–523. doi: 10.1016/s0021-9150(00)00601-8. [DOI] [PubMed] [Google Scholar]
- Banday AA, Marwaha A, et al. Tempol Reduces Oxidative Stress, Improves Insulin Sensitivity, Decreases Renal Dopamine D1 Receptor Hyperphosphorylation, and Restores D1 Receptor-G-Protein Coupling and Function in Obese Zucker Rats. Diabetes. 2005;54(7):2219–2226. doi: 10.2337/diabetes.54.7.2219. [DOI] [PubMed] [Google Scholar]
- Blackwell TS, Christman JW. The Role of Nuclear Factor-kappa B in Cytokine Gene Regulation. Am. J. Respir. Cell Mol. Biol. 1997;17(1):3–9. doi: 10.1165/ajrcmb.17.1.f132. [DOI] [PubMed] [Google Scholar]
- Ceriello A. Possible Role of Oxidative Stress in the Pathogenesis of Hypertension. Diabetes Care. 2008;31(Supplement2):S181–184. doi: 10.2337/dc08-s245. [DOI] [PubMed] [Google Scholar]
- Chander PN, Gealekman O, et al. Nephropathy in Zucker Diabetic Fat Rat Is Associated with Oxidative and Nitrosative Stress: Prevention by Chronic Therapy with a Peroxynitrite Scavenger Ebselen. J Am Soc Nephrol. 2004;15(9):2391–2403. doi: 10.1097/01.ASN.0000135971.88164.2C. [DOI] [PubMed] [Google Scholar]
- Christman JW, Blackwell TS, et al. Redox Regulation of Nuclear Factor Kappa B: Therapeutic Potential for Attenuating Inflammatory Responses. Brain Pathology. 2000;10(1):153–162. doi: 10.1111/j.1750-3639.2000.tb00252.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christman JW, Lancaster LH, et al. Nuclear factor k B: a pivotal role in the systemic inflammatory response syndrome and new target for therapy. Intensive Care Medicine. 1998;24(11):1131–1138. doi: 10.1007/s001340050735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coimbra TM, Janssen U, et al. Early events leading to renal injury in obese Zucker (fatty) rats with type II diabetes. Kidney Int. 2000;57(1):167–182. doi: 10.1046/j.1523-1755.2000.00836.x. [DOI] [PubMed] [Google Scholar]
- Cornelussen RN, Gupta S, et al. Regulation of prostaglandin A1-induced heat shock protein expression in isolated cardiomyocytes. J Mol Cell Cardiol. 2001;33(8):1447–54. doi: 10.1006/jmcc.2001.1406. [DOI] [PubMed] [Google Scholar]
- Coughlan MT, Thallas-Bonke V, et al. Combination Therapy with the Advanced Glycation End Product Cross-Link Breaker, Alagebrium, and Angiotensin Converting Enzyme Inhibitors in Diabetes: Synergy or Redundancy? Endocrinology. 2007;148(2):886–895. doi: 10.1210/en.2006-1300. [DOI] [PubMed] [Google Scholar]
- Danis RP, Yang Y. Microvascular retinopathy in the Zucker diabetic fatty rat. Investigative Ophthalmology and Visual Science. 1993;34(7):2367–2371. [PubMed] [Google Scholar]
- de Mello V, Kolehmainen M, et al. Downregulation of genes involved in NFκB activation in peripheral blood mononuclear cells after weight loss is associated with the improvement of insulin sensitivity in individuals with the metabolic syndrome: the GENOBIN study. Diabetologia. 2008;51(11):2060–2067. doi: 10.1007/s00125-008-1132-7. [DOI] [PubMed] [Google Scholar]
- Ebenezer PJ, Mariappan N, et al. Diet-induced Renal Changes in Zucker Rats Are Ameliorated by the Superoxide Dismutase Mimetic TEMPOL. Obesity (Silver Spring) 2009 doi: 10.1038/oby.2009.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elks CM, Mariappan N, et al. Chronic NF-{kappa}B blockade reduces cytosolic and mitochondrial oxidative stress and attenuates renal injury and hypertension in SHR. Am J Physiol Renal Physiol. 2008 doi: 10.1152/ajprenal.90628.2008. 90628.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elks CM, Mariappan N, et al. Chronic NF-{kappa}B blockade reduces cytosolic and mitochondrial oxidative stress and attenuates renal injury and hypertension in SHR. Am J Physiol Renal Physiol. 2009;296(2):F298–305. doi: 10.1152/ajprenal.90628.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortuno A, San Jose G, et al. Phagocytic NADPH Oxidase Overactivity Underlies Oxidative Stress in Metabolic Syndrome. Diabetes. 2006;55(1):209–215. doi: 10.2337/diabetes.55.01.06.db05-0751. [DOI] [PubMed] [Google Scholar]
- Friedman EA, Friedman AL. Is there really good news about pandemic diabetic nephropathy? Nephrol. Dial. Transplant. 2007;22(3):681–683. doi: 10.1093/ndt/gfl735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gassler N, Elger M, et al. Podocyte injury underlies the progression of focal segmental glomerulosclerosis in the fa/fa Zucker rat. Kidney Int. 2001;60(1):106–116. doi: 10.1046/j.1523-1755.2001.00777.x. [DOI] [PubMed] [Google Scholar]
- Giugliano D, Ceriello A, et al. The Effects of Diet on Inflammation: Emphasis on the Metabolic Syndrome. J Am Coll Cardiol. 2006;48(4):677–685. doi: 10.1016/j.jacc.2006.03.052. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, et al. Diagnosis and Management of the Metabolic Syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- Guggilam A, Haque M, et al. TNF-{alpha} blockade decreases oxidative stress in the paraventricular nucleus and attenuates sympathoexcitation in heart failure rats. Am J Physiol Heart Circ Physiol. 2007;293(1):H599–609. doi: 10.1152/ajpheart.00286.2007. [DOI] [PubMed] [Google Scholar]
- Guggilam A, Haque M, et al. TNF-alpha blockade decreases oxidative stress in the paraventricular nucleus and attenuates sympathoexcitation in heart failure rats. Am J Physiol Heart Circ Physiol. 2007;293(1):H599–609. doi: 10.1152/ajpheart.00286.2007. [DOI] [PubMed] [Google Scholar]
- Guijarro C, Egido J. Transcription factor-[kgr]B (NF-[kgr]B) and renal disease. Kidney Int. 2001;59(2):415–424. doi: 10.1046/j.1523-1755.2001.059002415.x. [DOI] [PubMed] [Google Scholar]
- Inoguchi T, Li P, et al. High glucose level and free fatty acid stimulate reactive oxygen species production through protein kinase C--dependent activation of NAD(P)H oxidase in cultured vascular cells. Diabetes. 2000;49(11):1939–1945. doi: 10.2337/diabetes.49.11.1939. [DOI] [PubMed] [Google Scholar]
- Isomaa B. A major health hazard: the metabolic syndrome. Life Sci. 2003;73(19):2395–411. doi: 10.1016/s0024-3205(03)00646-5. [DOI] [PubMed] [Google Scholar]
- Kasiske B, Cleary M, et al. Effects of genetic obesity on renal structure and function in the Zucker rat. Journal of Laboratory and Clinical Medicine. 1985;106(5):598–604. [PubMed] [Google Scholar]
- Keaney JF, Jr., Larson MG, et al. Obesity and Systemic Oxidative Stress: Clinical Correlates of Oxidative Stress in The Framingham Study. Arterioscler Thromb Vasc Biol. 2003;23(3):434–439. doi: 10.1161/01.ATV.0000058402.34138.11. [DOI] [PubMed] [Google Scholar]
- Khaleduzzaman M, Francis J, et al. Infection of cardiomyocytes and induction of left ventricle dysfunction by neurovirulent polytropic murine retrovirus. J Virol. 2007 doi: 10.1128/JVI.01002-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidambi S, Kotchen JM, et al. Association of adrenal steroids with hypertension and the metabolic syndrome in blacks. Hypertension. 2007;49(3):704–11. doi: 10.1161/01.HYP.0000253258.36141.c7. [DOI] [PubMed] [Google Scholar]
- Kris-Etherton P, Eckel RH, et al. Lyon Diet Heart Study : Benefits of a Mediterranean-Style, National Cholesterol Education Program/American Heart Association Step I Dietary Pattern on Cardiovascular Disease. Circulation. 2001;103(13):1823–1825. doi: 10.1161/01.cir.103.13.1823. [DOI] [PubMed] [Google Scholar]
- Lavaud S, Michel O, et al. Early influx of glomerular macrophages precedes glomerulosclerosis in the obese Zucker rat model. J Am Soc Nephrol. 1996;7(12):2604–2615. doi: 10.1681/ASN.V7122604. [DOI] [PubMed] [Google Scholar]
- Li Y, Reddy MA, et al. Role of the histone H3 lysine 4 methyltransferase, SET7/9, in the regulation of NF-kappa B dependent inflammatory genes: Relevance to diabetes and inflammation. J. Biol. Chem. 2008 doi: 10.1074/jbc.M802800200. M802800200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li YL, Gao L, et al. NADPH oxidase-derived superoxide anion mediates angiotensin II-enhanced carotid body chemoreceptor sensitivity in heart failure rabbits. Cardiovasc Res. 2007;75(3):546–54. doi: 10.1016/j.cardiores.2007.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansouri RM, Bauge E, et al. Atheroprotective Effect of Human Apolipoprotein A5 in a Mouse Model of Mixed Dyslipidemia. Circ Res. 2008;103(5):450–453. doi: 10.1161/CIRCRESAHA.108.179861. [DOI] [PubMed] [Google Scholar]
- Mariappan N, Soorappan RN, et al. TNF-alpha-induced mitochondrial oxidative stress and cardiac dysfunction: restoration by superoxide dismutase mimetic Tempol. Am J Physiol Heart Circ Physiol. 2007;293(5):H2726–37. doi: 10.1152/ajpheart.00376.2007. [DOI] [PubMed] [Google Scholar]
- Meyer C, Woerle HJ, et al. Abnormal renal, hepatic, and muscle glucose metabolism following glucose ingestion in type 2 diabetes. Am J Physiol Endocrinol Metab. 2004;287(6):E1049–1056. doi: 10.1152/ajpendo.00041.2004. [DOI] [PubMed] [Google Scholar]
- Mori S, Kawano K, et al. Relationships between diet control and the development of spontaneous type II diabetes and diabetic nephropathy in OLETF rats. Diabetes Res Clin Pract. 1996;33(3):145–52. doi: 10.1016/0168-8227(96)01290-9. [DOI] [PubMed] [Google Scholar]
- Morishima A, Ohkubo N, et al. NFkappaB regulates plasma apolipoprotein A-I and high density lipoprotein cholesterol through inhibition of peroxisome proliferator-activated receptor alpha. J Biol Chem. 2003;278(40):38188–93. doi: 10.1074/jbc.M306336200. [DOI] [PubMed] [Google Scholar]
- Mundy AL, Haas E, et al. Fat intake modifies vascular responsiveness and receptor expression of vasoconstrictors: Implications for diet-induced obesity. Cardiovasc Res. 2007;73(2):368–375. doi: 10.1016/j.cardiores.2006.11.019. [DOI] [PubMed] [Google Scholar]
- Nishikawa T, Edelstein D, et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature. 2000;404(6779):787–790. doi: 10.1038/35008121. [DOI] [PubMed] [Google Scholar]
- Picchi A, Gao X, et al. Tumor necrosis factor-alpha induces endothelial dysfunction in the prediabetic metabolic syndrome. Circ Res. 2006;99(1):69–77. doi: 10.1161/01.RES.0000229685.37402.80. [DOI] [PubMed] [Google Scholar]
- Reaven G. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595–1607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- Riccardi G, Giacco R, et al. Dietary fat, insulin sensitivity and the metabolic syndrome. Clinical nutrition (Edinburgh, Scotland) 2004;23(4):447–456. doi: 10.1016/j.clnu.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Wilson PWF, et al. Should C-Reactive Protein Be Added to Metabolic Syndrome and to Assessment of Global Cardiovascular Risk? Circulation. 2004;109(23):2818–2825. doi: 10.1161/01.CIR.0000132467.45278.59. [DOI] [PubMed] [Google Scholar]
- Ritz E, Stefanski A. Diabetic nephropathy in type II diabetes. Am J Kidney Dis. 1996;27(2):167–94. doi: 10.1016/s0272-6386(96)90538-7. [DOI] [PubMed] [Google Scholar]
- Ruan X, Zheng F, et al. PPARs and the kidney in metabolic syndrome. Am J Physiol Renal Physiol. 2008;294(5):F1032–47. doi: 10.1152/ajprenal.00152.2007. [DOI] [PubMed] [Google Scholar]
- Russo I, Del Mese P, et al. Resistance to the Nitric Oxide/Cyclic Guanosine 5′-Monophosphate/Protein Kinase G Pathway in Vascular Smooth Muscle Cells from the Obese Zucker Rat, a Classical Animal Model of Insulin Resistance: Role of Oxidative Stress. Endocrinology. 2008;149(4):1480–1489. doi: 10.1210/en.2007-0920. [DOI] [PubMed] [Google Scholar]
- Schena FP, Gesualdo L. Pathogenetic Mechanisms of Diabetic Nephropathy. J Am Soc Nephrol. 2005;16(3suppl1):S30–33. doi: 10.1681/asn.2004110970. [DOI] [PubMed] [Google Scholar]
- Yamazaki Y, Kawano Y, et al. Induction of adiponectin by natural and synthetic phenolamides in mouse and human preadipocytes and its enhancement by docosahexaenoic acid. Life Sci. 2008;82(56):290–300. doi: 10.1016/j.lfs.2007.11.016. [DOI] [PubMed] [Google Scholar]
- Yu Y, Kang YM, et al. Increased cyclooxygenase-2 expression in hypothalamic paraventricular nucleus in rats with heart failure: role of nuclear factor kappaB. Hypertension. 2007;49(3):511–8. doi: 10.1161/01.HYP.0000257356.20527.c5. [DOI] [PubMed] [Google Scholar]