Abstract
Easily utilized questionnaires estimating dietary calcium intake would be a valuable asset to promoting skeletal health and a helpful research tool. Two calcium questionnaires, one online and one printed, were each compared to dietary calcium intake measured by a three-day diet record. Women completed the questionnaires in a randomized order and kept a 3-day food record at home, returning it by mail. The ethnicity of the 140 study participants was 102 Caucasian, 12 African American, 16 Asian, and 10 Latin women. The average age was 49 ± 15 years (mean ± SD) with a range of 22.7 to 89.9 years. Measures utilized included an online calcium quiz, a printed calcium food frequency questionnaire and one three-day diet record. Data analysis was conducted using Pearson correlation coefficients. Sub-analyses were conducted by ethnicity. The correlation between each questionnaire and the daily calcium intake from the diet records was 0.37, p<0.001. Among the ethnic subgroups, the correlations were highest for African American women, followed by Caucasian women. There was also a trend toward higher correlations in younger women. These simple calcium assessment tools, taking less than five minutes to complete, have correlation values with diet records similar to more complex food frequency questionnaires reported in the literature. These questionnaires may provide valuable tools to estimate calcium intake in research, clinical and community settings.
Introduction
Adequate calcium intake remains the cornerstone of nutritional advice to maximize skeletal health. Increased calcium intake from dietary sources or supplements has been shown to improve measures of skeletal health in adolescents, adults and older individuals [1–4]. Despite the benefit of adequate calcium intake, dietary intake of calcium remains suboptimal, as demonstrated in the National Health and Nutrition Examination Survey (NHANES) [5;6]. Adolescents continue to consume only 938 mg/day of calcium compared to the recommended 1300 mg/day and individuals over 60 years of age fare even worse, consuming only 721 mg/day of calcium compared to the recommended 1200 mg/day [5].
While there are validated calcium questionnaires available for research and clinical use [7–14], there are no widely available, validated calcium assessment tools specifically designed for the lay public to self-administer. Easy-to-use educational interventions promoting adequate calcium intake would be a valuable asset for optimizing skeletal health as well as reducing risk of chronic diseases such as hypertension and colon cancer.
This project was undertaken to validate two publicly available calcium intake questionnaires against a three-day food record.
Methods
Food Frequency Questionnaires
The two food frequency questionnaires used in this study were an online food frequency questionnaire available at http://www.blindedwebsite and a written calcium food frequency questionnaire in a lay educational brochure [15].
The questionnaire in the publication was developed by registered dietitians at blinded organization and asks participants to consider the food items and beverages they consumed the previous day. The questionnaire provides a list of calcium-containing foods divided into those containing “high” and “medium” amounts of calcium. For assessing calcium intake, the questionnaire instructs participants that three medium-calcium food servings equal one high-calcium food serving. Participants then add up their total number of calcium servings and compare that total to the number of calcium servings that are recommended each day.
The online calcium quiz also asks participants to recall the foods and beverages consumed the previous day. The quiz lists 34 calcium-containing foods, along with a serving size. The participant enters how many servings of each listed food he or she consumed the previous day into a fill-in box. By clicking a button labeled “check my calcium intake” at the bottom of the questionnaire, the participant receives his or her total calcium intake for that day and the recommended intake for his or her age and gender. The main differences between the two questionnaires are the route of administration, the inclusion of a calcium-fortified foods section on the online questionnaire, and that the online questionnaire does not require any calculations by the participant. The study was reviewed and approved by the UCSF Committee on Human Research (IRB). All participants provided informed consent. The trial was registered at www.clinicaltrials.gov (NCT00512733).
Subjects
Participants were ambulatory, community-dwelling women over the age of 18 with self-reported good health recruited through advertisements and direct mailings. Participants were screened through an initial telephone call for inclusion and exclusion criteria and given a complete description of the study on the telephone. To maximize generalizability of the results, exclusion criteria were minimal, excluding individuals with health conditions that limited food selection, those unable to keep a diet record or those unable to understand and provide informed consent.
Procedures
Women who passed screening and were interested in participating were invited to attend a single study visit. Informed consent was obtained and participants then completed the questionnaires of interest. The order of questionnaire administration was randomized for each participant. Participants were provided with the written questionnaire in the booklet and a laptop set to the calcium quiz webpage to complete the online questionnaire. The research dietitian was available for questions; however, participants were encouraged to primarily utilize the instructions accompanying each questionnaire in order to approximate a self-administration setting as much as possible.
Following the completion of the questionnaire, a registered dietitian taught the participant how to keep a three-day food record. Each participant kept the food record for two weekdays and one weekend day of her choice. The dietitian instructed each subject to record her intake of all foods and beverages from all meals and snacks for these three days. The subject was instructed to use measuring cups or measuring spoons to assess the portion size of each bulk item and to record other foods in common terms such as number of eggs or slices of bread. Plastic food models and handouts were used to educate the subject on portion sizes. Written instructions were provided to the subjects, including guidelines for carefully describing food, methods of preparation, portion estimation and listing brand names whenever possible. All supplies needed by the subject to complete the dietary record were provided. Each participant was also provided with a stamped, addressed envelope to return the food record by mail.
Immediately upon receipt, the food diaries were examined for completeness and legibility. Any missing or unclear items were corrected by telephoning the participant. Food records were entered into Food Processor Plus software (ESHA Research, Salem, OR) to determine nutrient content. Nutrient content of any food items recorded by participants that were not in the software’s database was determined by examination of labels, contact with food manufacturers, search of the USDA nutrient database, or estimation from ingredient content by a dietitian.
Calcium intake from the questionnaires was calculated using the built-in calculator on the webpage for the online questionnaire and calculated by hand following the instructions in the booklet as described above.
Data Analysis
The mean calcium intake as assessed by each questionnaire was compared to the mean intake determined by the food record using two tailed t-tests. Pearson’s correlation was used to determine the correlation coefficient for each type of questionnaire and the food record. Bland-Altman plots, a graphical technique used to compare two methods of quantifying the same variable—in this case dietary calcium intake—were constructed. For each participant, the difference in dietary calcium intake as assessed by the two measurement methods was plotted against the dietary calcium intake from the two methods averaged together. All analyses were conducted using STATA (version 8.2, StataCorp LP, College Station, TX).
Results
In all, 209 women passed telephone screening and were scheduled for participation. Out of that number, 164 women completed the study visit, completed both questionnaires and were provided materials for the three-day food record to be completed at home. Five women reported sending in a food record, but no record was received. An additional 19 women did not return a three-day food record. Thus, complete data (two calcium questionnaires and three days of food records) were available for 140 women.
The ethnicity distribution among the 140 study participants was 102 Caucasian, 12 African American, 16 Asian, and 10 Latin women. The average age was 49 ± 15 years (mean ± SD) with a range of 22.7 to 89.9 years.
The average daily calcium intake was 834.4 ± 554.1 mg/d for the online calcium quiz, 719.5 ± 521.9 mg/d for the printed questionnaire and 901.8 ± 355.9 mg/d for the food record. Mean calcium intake did not differ significantly between the online quiz and the food record. However, mean calcium intake as assessed by the printed questionnaire was significantly lower than that of the food record (p<0.001).
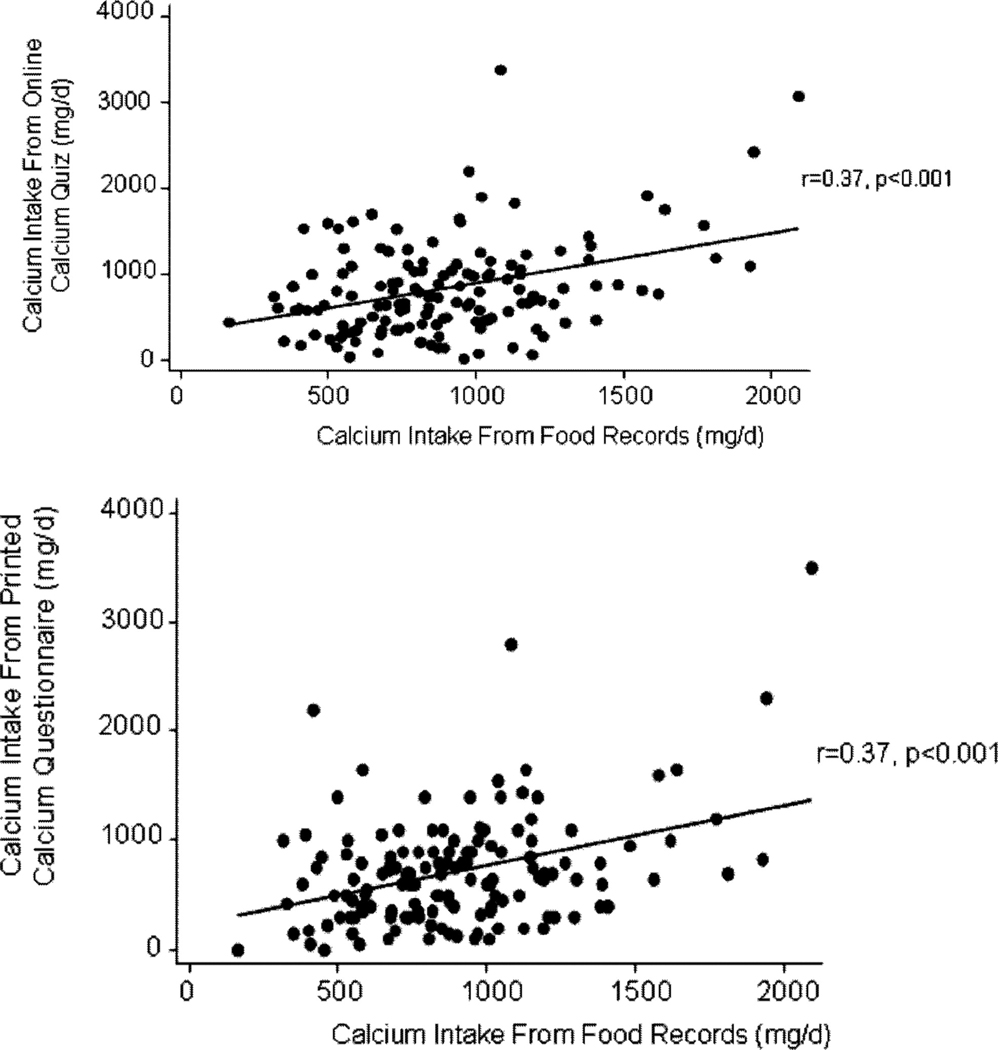
There was a significant correlation between each questionnaire and the three-day food record. The correlation coefficient was r=0.37, p<0.001 for each questionnaire, compared with the three-day calcium intake average from the food record (Figure 1).
Figure 1.
Correlations between each food frequency questionnaire and the three-day diet
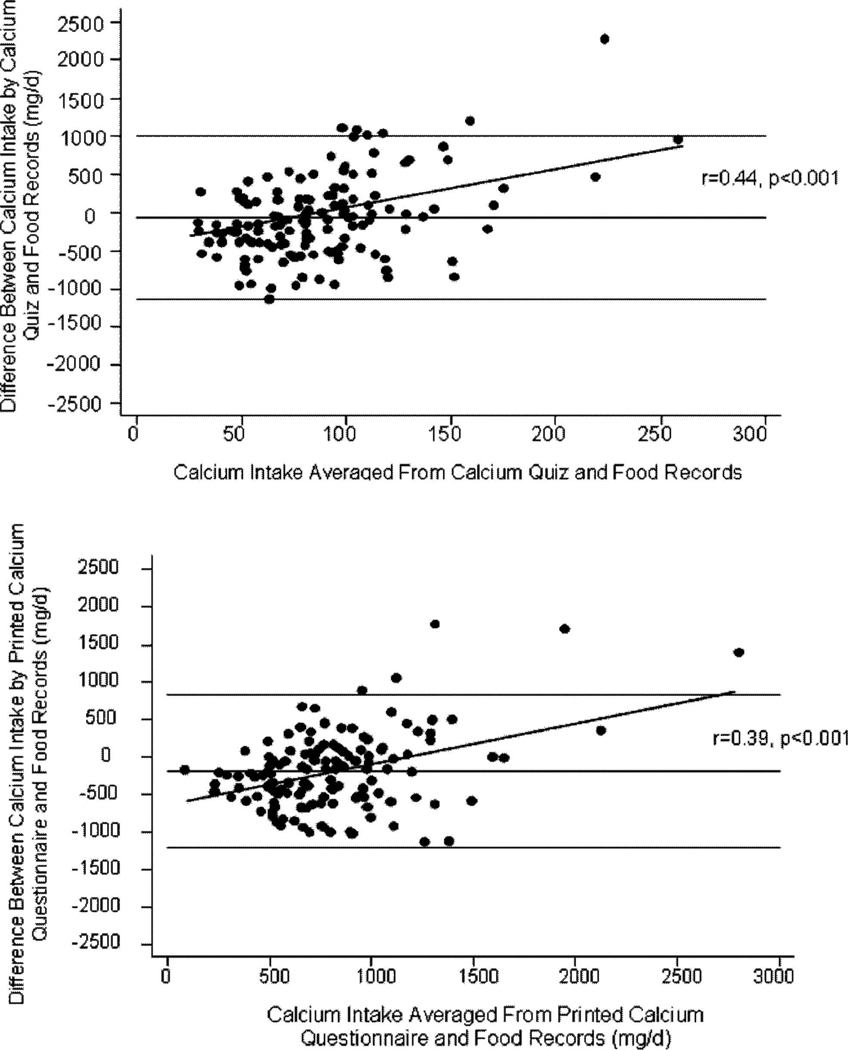
The Bland-Altman comparisons demonstrated that the printed questionnaire had a systematic bias and underestimated dietary calcium intake by 182 mg/day (95% CI−268 to −97mg/d). The online calcium quiz did not demonstrate a systematic bias, with calcium intake estimated by the quiz slightly lower than the food record with a confidence interval that included zero (−67 mg/day [95% CI −157 to +22 mg/day]). For both questionnaires, the Bland-Altman plots demonstrate that at the higher average intakes, the difference between the calcium intake estimated by the questionnaires and the calcium intake from the food records is higher than at average or even low intakes. The correlations between the difference between the two methods and the average calcium intake were significant with r=0.39, p<0.001 for the calcium booklet and r=0.44, p<0.01 for the calcium quiz (Figure 2).
Figure 2.
Bland-Altman plots of each questionnaire compared to the three-day food record.
SUMMARY AND CONCLUSIONS
The two calcium questionnaires estimated dietary calcium intake reasonably well, with correlations to the three-day food records that are similar to the ranges of correlations seen in previous studies of limited-item calcium food frequency questionnaires [7–14;16]. The average calcium intake assessed by each questionnaire was similar to both the food records obtained as part of the study and to that seen in population-based data [6].
Calcium intake on both questionnaires was somewhat lower than that measured by the food record. The questionnaires intentionally contain a limited number of food items to enable their quick completion. The food records are much more extensive, recording all the foods eaten during the recording period. Thus, it is not surprising that calcium intakes are lower on the questionnaires than on the food records. Despite this, the online calcium quiz did not show a systematic bias when compared to the food records, with an average difference in calcium intake of less than 70 mg/day that was not significantly different. The calcium booklet questionnaire did show a degree of systematic bias, underestimating calcium intake by about 190 mg/day on average. However, this degree of underestimation is relatively small, amounting to less than one serving of calcium-rich food. The calcium booklet questionnaire focuses on servings of foods categorized as “high” and “medium” calcium-containing foods, estimating that three servings of medium-calcium foods will approximately equal one high-calcium food. This ratio may be altered, depending on portion sizes that are not assessed by the questionnaire, but would be captured on the food record.
The difference between each questionnaire and the food record increased with increasing calcium intake. In particular, the questionnaires tended to overestimate dietary calcium intake compared to the food records when intakes exceeded approximately 1500 mg/day. This may reflect a lack of portion-size assessment by the questionnaires and greater underestimation of calcium intake among those consuming larger portions. However, the primary goal of these questionnaires is to help consumers assess whether they are consuming sufficient calcium. While it would be preferable for the questionnaires to perform equally well at all intakes, accuracy is of particular importance at the range of typical as well as goal intakes in the population, both of which are below 1500 mg/day.
Limitations of this study include that the two questionnaires were administered on the same day for logistical reasons. We attempted to minimize the impact of this by randomizing the order in which they were administered for each subject. There are also potential limitations related to using a food record as the comparison method. Participants knew they were in a study looking at dietary calcium questionnaires and so may have been more aware of calcium-containing foods during their food record collection. Simply recording dietary intake may have altered a participant’s typical intake. In addition, both questionnaires ask the respondent to fill out the questionnaire according to what she ate the day before. While this approach has the strength of assessing specific intakes in a timeframe that was easily recalled for the participants, the previous day may not have reflected their habitual intake, thus reducing the likelihood that the day recorded by the questionnaire would be similar to the days captured on the food record. The issue of assessing “yesterday’s intake” vs. typical intake” on the questionnaires was debated when designing the validation study. The questionnaires had been developed asking about the previous day’s intake, with the rationale that the previous day’s meals would be easy for the respondents to remember accurately. When we undertook the validation study, we were concerned that having the participant complete the questionnaire and do a food record of the same day would result in an extremely high, somewhat artifactual, correlation as they would be recounting the same day’s foods twice in short succession. This did not seem like it would be a credible way to validate the questionnaires. On the flip side, using a more conventional approach of comparing the questionnaire to a three day food record has the limitation that the previous day’s intake may not be reflective of typical intake. We tried to minimize this limitation by having subjects complete the three day diet record within the week of the questionnaire to limit seasonal and travel variations. However, it is quite possible that for some subjects, the previous day was not reflective of their typical intake. This could have diminished the correlation between the questionnaires and the diet record.
Supplement use was not included in the calcium intake totaled from either the calcium food frequency questionnaires or in the three day diet records. We were primarily interested in how well these questionnaires would assess dietary calcium intake. Adding intake from supplements would increase the calcium intake on both the questionnaire and the food record by the same amount, thus not altering the correlation between the two. However, in terms of using these questionnaires as educational tools, adding supplement intake to the dietary intake to provide a total intake would be helpful information for respondents. We will provide feedback to the questionnaire developers for them to consider adding supplement intake to the total calcium assessment.
In conclusion, the two questionnaires performed reasonably well and appear to be quite suitable for screening for insufficient dietary calcium intake. They are considerably shorter than other calcium questionnaires that have shown a higher correlation with food records. Uniquely, these two questionnaires were designed specifically for layperson use. Both are quite simple to understand and complete. In our study, participants were able to quickly complete both questionnaires using only the short accompanying directions. Additionally, the online questionnaire is readily available to anyone with Internet access and performs all calculations for the participant. These short questionnaires with good correlations to calcium intake estimates from food records are valuable tools for the layperson to assess his or her own calcium intake. Web analytics indicate that some consumers complete the quiz two or more times in the same visit to identify how changes in food choices affect their calcium intake providing dietary assessment and education. The questionnaires also may be helpful screening techniques for health care professionals assessing patients for dietary calcium insufficiency.
Acknowledgements
Funding for this study was provided by blinded. This study utilized resources from Grant Number UL1 RR024131-01 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Descriptive Words/Phrases: online and paper calcium food frequency questionnaires, short calcium assessment paper and online tools for consumers
Contributor Information
Hacker-Thompson Andrea, Medicine/Endocrinology, University of California San Francisco, San Francisco, CA, UCSF/Mt Zion Osteoporosis Center, 2200 Post St. C-409, andreah@medicine.ucsf.edu, Phone: (415) 353-7867, Fax: 415.353.9635.
Trina P. Robertson, Dairy Council of California, 2151 Michelson Drive, Suite 235, Irvine, CA 92612, trinar@dairycouncilofca.org, Phone: 949.756.7892, Fax: 949,756.7896.
Deborah E. Sellmeyer, Metabolic Bone Center, The Johns Hopkins Bayview Medical Center, 5200 Eastern Avenue, Mason F. Lord Center Tower, Suite 4300, Baltimore, MD 21224, Phone: 410-550-4229, Fax: 410-550-6864.
Reference List
- 1.Stear SJ, Prentice A, Jones SC, Cole TJ. Effect of a calcium and exercise intervention on the bone mineral status of 16–18-y-old adolescent girls. Am J Clin Nutr. 2003;77(4):985–992. doi: 10.1093/ajcn/77.4.985. [DOI] [PubMed] [Google Scholar]
- 2.Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older [comments] N Engl J Med. 1997;337:670–676. doi: 10.1056/NEJM199709043371003. [DOI] [PubMed] [Google Scholar]
- 3.Manios Y, Moschonis G, Trovas G, Lyritis GP. Changes in biochemical indexes of bone metabolism and bone mineral density after a 12-mo dietary intervention program: the Postmenopausal Health Study. Am J Clin Nutr. 2007;86(3):781–789. doi: 10.1093/ajcn/86.3.781. [DOI] [PubMed] [Google Scholar]
- 4.Levers-Landis CE, Burant C, Drotar D, Morgan L, Trapl ES, Colabianchi N, Kwoh CK. A randomized controlled trial for the primary prevention of osteoporosis among preadolescent girl scouts: 1-year outcomes of a behavioral program. J Pediatr Psychol. 2005;30(2):155–165. doi: 10.1093/jpepsy/jsi003. [DOI] [PubMed] [Google Scholar]
- 5.Ervin RB, Wang CY, Wright JD, Kennedy-Stephenson J. Dietary intake of selected minerals for the United States population: 1999–2000. Adv Data. 2004;(341):1–5. [PubMed] [Google Scholar]
- 6.Ma J, Johns RA, Stafford RS. Americans are not meeting current calcium recommendations. Am J Clin Nutr. 2007;85(5):1361–1366. doi: 10.1093/ajcn/85.5.1361. [DOI] [PubMed] [Google Scholar]
- 7.Sebring NG, Denkinger BI, Menzie CM, Yanoff LB, Parikh SJ, Yanovski JA. Validation of three food frequency questionnaires to assess dietary calcium intake in adults. J Am Diet Assoc. 2007;107(5):752–759. doi: 10.1016/j.jada.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blalock SJ, Norton LL, Patel RA, Cabral K, Thomas CL. Development and assessment of a short instrument for assessing dietary intakes of calcium and vitamin D. J Am Pharm Assoc. 2003;43(6):685–693. doi: 10.1331/154434503322642615. [DOI] [PubMed] [Google Scholar]
- 9.Musgrave KO, Giambalvo L, Leclerc HL, Cook RA, Rosen CJ. Validation of a quantitative food frequency questionnaire for rapid assessment of dietary calcium intake. J Am Diet Assoc. 1989;89(10):1484–1488. [PubMed] [Google Scholar]
- 10.Cummings SR, Block G, McHenry K, Baron RB. Evaluation of two food frequency methods of measuring dietary calcium intake. Am J Epidemiol. 1987;126(5):796–802. doi: 10.1093/oxfordjournals.aje.a114716. [DOI] [PubMed] [Google Scholar]
- 11.Chee WS, Suriah AR, Zaitun Y, Chan SP, Yap SL, Chan YM. Dietary calcium intake in postmenopausal Malaysian women: comparison between the food frequency questionnaire and three-day food records. Asia Pac J Clin Nutr. 2002;11(2):142–146. doi: 10.1046/j.1440-6047.2002.00276.x. [DOI] [PubMed] [Google Scholar]
- 12.Green JH, Booth CL, Bunning RL. Assessment of a rapid method for assessing adequacy of calcium intake. Asia Pac J Clin Nutr. 2002;11(2):147–150. doi: 10.1046/j.1440-6047.2002.00279.x. [DOI] [PubMed] [Google Scholar]
- 13.Bertoli S, Petroni ML, Pagliato E, Mora S, Weber G, Chiumello G, Testolin G. Validation of food frequency questionnaire for assessing dietary macronutrients and calcium intake in Italian children and adolescents. J Pediatr Gastroenterol Nutr. 2005;40(5):555–560. doi: 10.1097/01.mpg.0000153004.53610.0e. [DOI] [PubMed] [Google Scholar]
- 14.Sato Y, Tamaki J, Kitayama F, Kusaka Y, Kodera Y, Koutani A, Iki M. Development of a food-frequency questionnaire to measure the dietary calcium intake of adult Japanese women. Tohoku J exp Med. 2005;207(3):217–222. doi: 10.1620/tjem.207.217. [DOI] [PubMed] [Google Scholar]
- 15. [Accessed May 20, 2008];Blinded website.
- 16.Jensen JK, Gustafson D, Boushey CJ, Auld G, Bock MA, Bruhn CM, Gabel K, Misner S, Novotny R, Peck L, Read M. Development of a food frequency questionnaire to estimate calcium intake of Asian, Hispanic, and white youth. J Am Diet Assoc. 2004;104(5):762–769. doi: 10.1016/j.jada.2004.02.031. [DOI] [PubMed] [Google Scholar]