Abstract
Objective
We assessed the relation between prepregnancy body mass index (BMI) and the likelihood of major depressive disorder (MDD) during pregnancy and test whether this association was modified by gestational weight gain.
Method
Women (n=242) were enrolled at <20 weeks gestation into a prospective cohort study. Diagnosis of MDD was made with the Structured Clinical Interview for DSM-IV at 20, 30, and 36 weeks. Gestational weight gain was compared with the 1990 Institute of Medicine weight gain recommendations. To assess the independent association between prepregnancy BMI and the odds of MDD, MDD at each time point was used as the dependent measure in a multivariable longitudinal logistic regression model employing generalized estimating equations.
Results
There was a strong, positive dose-response association between prepregnancy BMI and the likelihood of MDD (p=0.002). Compared with a BMI of 18, the adjusted odds ratios (95% confidence interval) for BMIs of 23, 28, and 33 were 1.4 (1.1, 1.7), 1.9 (1.3, 2.9), and 2.6 (1.4, 4.3), respectively. Gestational weight gain significantly modified this effect. Among women with weight gains within and above the 1990 IOM recommendations, pregravid overweight was associated with a greater likelihood of major depression. In contrast, all women with weight gains below recommended levels had an elevated odds of depression, regardless of their pregravid BMI (p<0.05).
Conclusions
Because pregravid overweight, poor gestational weight gain, and major depression all pose substantial risks for fetal development and birth outcomes, health care providers should monitor depression levels in these women to facilitate appropriate depression intervention.
Introduction
In U.S. women, obesity is a substantial and escalating health problem. It is the second leading cause of preventable death, 1 and dramatically increases morbidity associated with many chronic diseases.2 Nearly 2 of 3 adult women are classified as overweight (body mass index (BMI) >25 kg/m2) and one in three is obese (BMI >30 kg/m2). 3 Over the past 30 years, the prevalence of obesity in women aged 20 to 74 has doubled. 4
Not surprisingly, more women are entering pregnancy overweight. It is estimated that one in five U.S. women is overweight at the start of pregnancy, a figure that has risen 70% in the last decade.5 Obesity during pregnancy poses unique risks to the mother and fetus. High maternal prepregnancy BMI has been linked with countless adverse perinatal outcomes, including preeclampsia, miscarriage, congenital malformations, stillbirth, neonatal death, gestational diabetes, operative delivery, and infant macrosomia.6 Little is known about the consequences of prepregnancy obesity on maternal mental health outcomes, including major depression. Moreover, the effect of major depression on the development of obesity has also been underexplored.
Research in nonpregnant adults indicates that obesity is associated with depressive symptoms,7,8 lifetime diagnosis of major depression,9 and history of depression.10 Moreover, obesity has been shown to not only predict the onset of major depression, 11, 12 but also result from major depression.13–15 There is some suggestion that the positive association between obesity and depression is stronger in women than men.16,17 Whether these findings can be generalized to pregnant women remains largely unknown.
Pregnancy is a unique developmental stage involving weight gain. Thus, the association between weight and mood must be viewed in the context of a woman’s prepregnancy weight as well as her gestational weight gain. Adequate weight gain is necessary for the growth and development of maternal and fetal tissues.18 Consequently, women may positively attribute weight at conception and gestational weight gain to ensuring the health of the infant. Indeed, pregnancy is often accompanied by positive behavioral and attitudinal changes with regard to weight and nutrition,19 yet evidence suggests that negative weight gain attitudes and dissatisfaction with weight/shape may resurface as pregnancy advances.20,21 Because changes in appetite and body weight are among the diagnostic criteria for major depression, extremes of both prepregnancy BMI and total gestational weight gain may be markers of antenatal depression. An understanding of the interaction between prepregnancy weight and gestational weight gain on antenatal depression may help to identify high-risk groups that will benefit from depression screening and intervention.
Our objectives were twofold. First, we sought to assess the relation between prepregnancy BMI and the likelihood of major depression during pregnancy. Second, we tested whether this association was modified by gestational weight gain. We hypothesized that pregravid overweight was associated with antenatal major depression regardless of gestational weight gain, and that lean women with inadequate and excessive weight gain also had a higher prevalence of depression.
Method
Data came from the Antidepressant Use during Pregnancy Study, an observational cohort study designed to investigate the effects of maternal depression and antidepressant use on pregnancy outcomes and childhood development 22. Women with or without major depression and/or antidepressant use in the index pregnancy were invited to enroll at <20 weeks gestation. We did not separate the exposures based upon whether the depressive episode during the pregnancy was the first episode or recurrent. Recruitment was by self- and physician-referral, advertising and screening in the obstetrical ultrasound suite. Consultation about depression management during pregnancy was provided to women with depression or antidepressant exposure and a summary was sent both to the woman and her physician(s). Enrollment did not depend upon acceptance of recommendations or treatment choice. No intervention was prescribed by the study team.
Women were excluded if they had psychosis, bipolar disorder, active substance use disorder (identified by self report or urine drug screen), gestational exposure to benzodiazepines or prescription drugs in the FDA-defined category of D or X 23 (other than selective serotonin reuptake inhibitors (SSRI)), a multifetal gestation, or a pregestational chronic disease. Study visits occurred at approximately 20, 30, and 36 weeks gestation. At baseline, data on sociodemographic characteristics, health behaviors, medication exposures, and prepregnancy weight were collected via interview, and maternal height was measured. At each study visit, maternal depression was assessed by an experienced, trained clinician (details below) and maternal weight was measured. Approval was obtained from the University of Pittsburgh Institutional Review Board, and all women provided informed, written consent.
A total of 251 eligible women enrolled into the study. We excluded women who lacked data on prepregnancy weight or height (n=1) or covariates in our final model (n=2). One woman was excluded because she was too heavy to be weighed on the study scale. We also excluded 5 observations that represented a second pregnancy to the same woman. The final analytical sample was 242 women. Of these, 71.1% had depression assessments at all 3 pregnancy study visits, while a smaller proportion had depression data available at only one (15.7%) or two (13.2%) visits. Therefore, a total of 624 person-observations were included in the prepregnancy BMI analysis. Gestational weight measurements at each study visit were missing for some women, so the sample size for the analyses involving gestational weight gain was reduced to 239 women contributing 552 person-observations.
Definition of study variables
At each visit, the diagnosis of major depressive disorder was made according to the Structured Clinical Interview for DSM-IV (SCID) 24 by an experienced, trained clinician. We adapted the timeline technique 25 to chart major depression course by month across pregnancy.26 Depression severity was assessed with the 29-item Structured Interview Guide for the Hamilton Rating Scale for Depression--Atypical Depression Symptoms Version (SIGH-ADS),27 which includes all versions of the Hamilton Rating Scale for Depression (HRSD).28
Prepregnancy BMI [weight (kg)/height (m)2] was based on measured height and maternal self-report of prepregnancy weight at enrollment. BMI was categorized as underweight (BMI <18.5), normal weight (BMI 18.5–24.9), overweight (BMI 25.0–29.9), and obese (BMI ≥30.0). 29 Gestational weight gain at each visit was calculated by subtracting the prepregnancy weight from the measured weight. Gestational weight gain was compared with the prepregnancy BMI-specific 1990 Institute of Medicine weight gain recommendations.18 Each woman’s actual observed weight gain was divided by her expected weight gain at the gestational age that corresponded with each study visit.18 Weight gain was classified as below the lower cut-off of 1990 IOM recommendations, within the IOM recommended range, or above the upper cut-off of recommendations as we have done in previous analyses.30
Maternal ethnicity/race was based on self-report. Data on maternal age, parity (primiparous, multiparous), smoking status (smoker, nonsmoker), education (less than high school, high school or equivalent, some college), marital status (married, unmarried), and work status (full-time, part-time or none) were also available. Gestational age was determined by maternal report of the date of the last menstrual period and was confirmed with ultrasound when available. Self-reported SSRI use at each visit was verified using serum concentrations.
Statistical analysis
To assess the independent association between prepregnancy BMI and the odds of depression, depression status at each time point during the index pregnancy was used as the dependent measure in a longitudinal logistic regression model employing generalized estimating equations, which account for intraindividual correlation of depression measurements.31 To assess the dose-response relation between BMI and depression, we used published methods 32 to determine the most appropriate specification of BMI in our models. We tested numerous spline terms and fractional polynomials, but the best fit was found using BMI as a continuous, linear variable in all models.
We fit parsimonious regression models by specifying full models with potential confounding variables: race/ethnicity, maternal age, height, education, marital status, work status, parity, smoking status, SSRI use, and gestational age at study visit. Effect modification by gestational weight gain, race/ethnicity, SSRI use, and study visit was tested using Wald p-values (α=0.10) and examining stratum-specific results. Potential confounders were considered to not be influential and were removed from the model if their inclusion did not satisfy our a priori criteria: a change of the main-effect odds ratio (OR) by ≥10%. Study visit gestational age was included in all models regardless of its effect on the point estimates. Maternal education met our definition of confounding in the final BMI model, and education and work status met our definition of confounding in the BMI-weight gain model.
Results
Most of the 242 women in the study were white, aged 26 to 30 years, college-educated, married, non-smokers, and had at least one previous live birth (Table 1). Nearly half of the sample was overweight or obese at the start of pregnancy. At baseline, approximately 25% of women had a diagnosis of major depression and 20% were using SSRIs for treatment of depression. Mean (SD) depressive symptom scores using the 29-item SIGH-ADS were 9.2 (5.4) among women without a diagnosis of current major depression women and 21.9 (4.7) among women diagnosed with major depression at enrollment. Women in the SSRI treated groups had the expected therapeutic benefit, that is, they had less depression than the women in the depression group (data not shown).
Table 1.
Characteristics of the sample (n=242).
| Percent | |
|---|---|
| Maternal race | |
| White | 80.2 |
| Black | 16.5 |
| Other | 3.3 |
| Maternal age (years) | |
| <25 | 21.1 |
| 26 to 30 | 31.4 |
| 31 to 35 | 28.1 |
| ≥36 | 19.4 |
| Education | |
| High school or less | 19.0 |
| Some college | 19.0 |
| College graduate | 37.2 |
| Some graduate school | 24.8 |
| Work status | |
| Full-time work or school | 50.0 |
| Part-time or none | 50.0 |
| Marital status | |
| Unmarried | 26.5 |
| Married | 73.6 |
| Parity | |
| 0 | 41.3 |
| 1 or more | 58.7 |
| Current smoking status | |
| Non-smoker | 85.5 |
| Smoker | 14.5 |
| Prepregnancy BMI (kg/m2) | |
| <18.5 | 2.5 |
| 18.5–24.9 | 50.4 |
| 25.0–29.9 | 21.5 |
| ≥30.0 | 25.6 |
| Diagnosis and SSRI use at baseline | |
| Not depressed, not medicated | 64.5 |
| Depressed, not currently medicated | 15.3 |
| Medicated, not currently depressed | 10.3 |
| Depressed, currently medicated | 9.9 |
SSRI, selective serotonin reuptake inhibitors
One subject was missing data on smoking status.
The prevalence of major depression varied significantly across prepregnancy BMI categories (Table 2). Depression was least common in normal weight women and increased in prevalence among overweight and obese women. Estimates were imprecise for underweight women due to the small sample size. After adjustment for education and visit gestational age, the odds ratios (95% confidence intervals (CI)) for major depression compared with normal weight women were 2.3 (0.5, 11.1) for underweight women, 1.7 (0.9, 3.4) for overweight women, and 2.9 (1.5, 5.6) for obese women.
Table 2.
Prevalence of major depression at 20, 30, and 36 weeks by prepregnancy body mass index category1
| 20 weeks | 30 weeks | 36 weeks | ||||
|---|---|---|---|---|---|---|
| Total | Major | Total | Major | Total | Major | |
| n | depression* (%) | n | depression* (%) | n | depression** (%) | |
| Underweight | 6 | 33.3 | 6 | 33.3 | 5 | 20.0 |
| Normal weight | 122 | 17.2 | 106 | 16.0 | 96 | 11.5 |
| Overweight | 52 | 21.3 | 43 | 25.6 | 37 | 24.3 |
| Obese | 62 | 41.9 | 48 | 43.8 | 41 | 31.7 |
p<0.01;
p<0.05
Prepregnancy body mass index (BMI, kg/m2) was categorized as underweight (BMI <18.5), normal weight (BMI 18.5–24.9), overweight (BMI 25.0–29.9), and obese (BMI ≥30.0) 29.
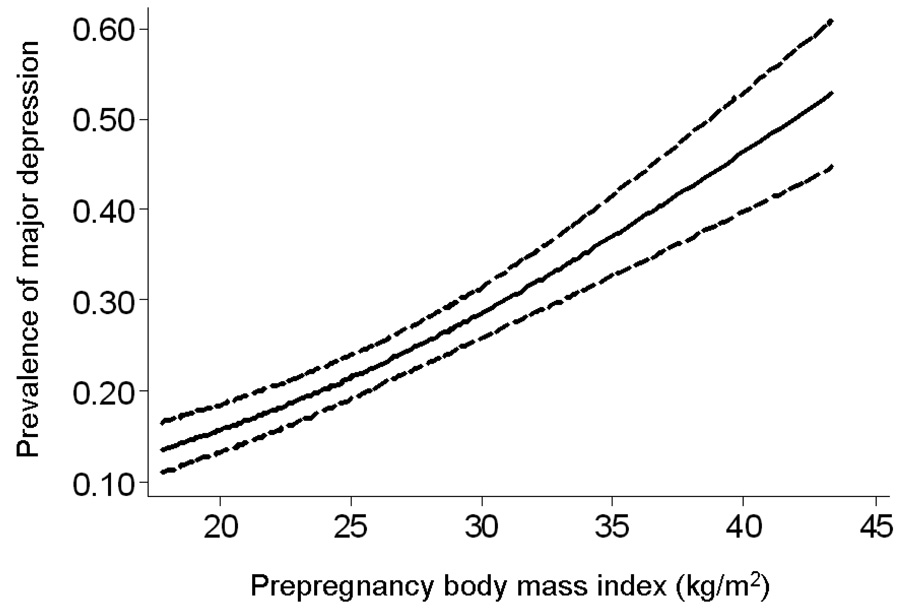
There was a strong, positive dose-response association between prepregnancy BMI and the likelihood of major depression (Figure 1; p=0.002). Compared with women who had a BMI of 18, the odds of depression among women with a BMI of 28 and 33 were 1.9-fold and 2.6-fold higher, respectively, after confounder adjustment (Table 3). Importantly, even normal-weight women with a BMI of 23 had a 40% increased adjusted odds of major depression when compared with the same referent. There was no evidence that this effect varied by race/ethnicity, gestational age at study visit, or SSRI use.
Figure 1.
Unadjusted association between prepregnancy body mass index (BMI) and the likelihood of major depression in pregnancy (n=242 women contributing 642 depression measurements at 20, 30, and 36 weeks gestation).*
* The solid line represents the point estimate and the dotted lines represent the 95% confidence bands around the estimate (p=0.002). Results were truncated at a BMI of 45, as only 1% of the sample had values greater than 45. Curves were estimated by calculating predicted probabilities based on an unadjusted logistic regression model employing generalized estimating equations.
Table 3.
Association between prepregnancy BMI and the likelihood of major depression at 20, 30, and 36 weeks (n=242 women contributing 624 measurements). Odds ratios are shown for a 1- kg/m2 increase in BMI as well as for representative BMI values compared with a BMI of 20.
| Adjusted* odds ratio (95% CI) |
|
|---|---|
| BMI, 1-kg/m2 increase | 1.07 (1.02, 1.11) |
| BMI = 18 | 1.0 (referent) |
| BMI = 23 | 1.4 (1.1, 1.7) |
| BMI = 28 | 1.9 (1.3, 2.9) |
| BMI = 33 | 2.6 (1.4, 4.3) |
Adjusted for maternal education and gestational age. Further adjustment for maternal age, marital status, smoking status, race/ethnicity, and parity had no meaningful impact on the results.
More than half of women gained above the BMI-specific 1990 IOM recommended weight gain ranges at weeks 20 (53.2%), 30 (57.5%) and 36 (60.3%), with the remaining gaining below or within recommended ranges. Low weight gain was more common than weight gains within the recommended ranges at 20 weeks (30.4% vs. 16.5%) and 30 weeks (24.7% vs. 17.8%). At 36 weeks, 23.4% of women gained within the IOM recommended range, while 16.3% gained below the recommended range.
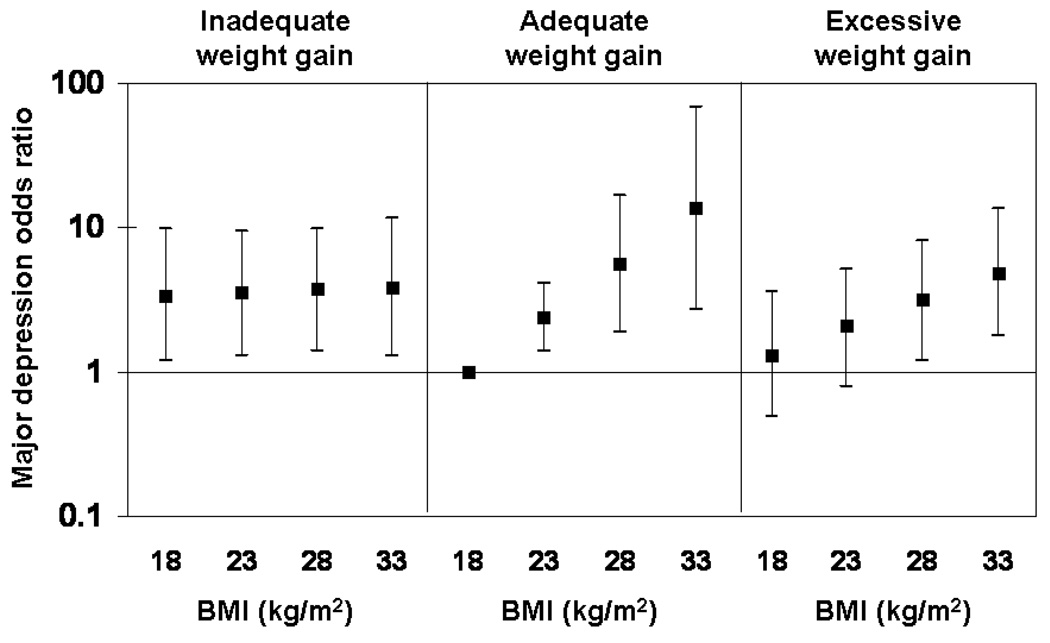
Gestational weight gain significantly modified the effect of prepregnancy BMI on the likelihood of major depression (Figure 2; p=0.01 for interaction). Among women with weight gain less than the 1990 IOM recommendations, there was no association between prepregnancy BMI and the odds of depression independent of work status, education, and gestational age at study visit. Women who gained below the 1990 IOM recommendations were about 3.5 times as likely to have antenatal depression as lean women with adequate weight gain, regardless of their pregravid BMI (p<0.05). In contrast, among women who gained within the 1990 IOM weight gain range, there was a strong, positive linear relation between pregravid BMI and depression. Each 5-unit increase in BMI was associated with a 2.4-fold (95% CI: 1.4, 4.1) increase in the likelihood of major depression after confounder adjustment. This association was slightly attenuated in women who gained above the 1990 IOM recommendations. Only women who gained above the recommendations and whose BMI values were 28 or more had a significant increase in the adjusted odds of depression compared with lean women gaining within the recommended range (e.g., OR (95% CI) for BMI 28: 3.2 (1.2, 8.1); BMI 33: 4.9 (1.8. 13.4)). This association was not further modified by race/ethnicity or gestational age at study visit.
Figure 2.
Major depression odds ratios and 95% confidence intervals by prepregnancy body mass index (BMI) and categories of gestational weight gain, adjusted for maternal education, work status, and gestational age (n=552 person-observations).*
* Estimates were generated based on a multivariable logistic regression model employing generalized estimating equations. Women with a BMI of 18 and adequate weight gain were considered the referent.
None of the results changed meaningfully when we restricted analyses to women who contributed data to all three study visits or further adjusted for maternal age, height, race/ethnicity, marital status, SSRI use, and smoking status (data not shown).
Discussion
We observed a strong, linear dose-response relationship between prepregnancy BMI and the likelihood of antenatal major depression that remained after controlling for measured confounders. When we studied how this effect varied by gestational weight gain, we found that high pregravid BMI was associated with major depression among women who gained within and above the 1990 IOM-recommended ranges. In the subgroup of women with gestational gain below the 1990 IOM recommended ranges, depression was prevalent among all women, regardless of their prepregnancy BMI. To our knowledge, ours is the first study to explore the joint effects of prepregnancy BMI and gestational weight gain on the likelihood of antenatal depression.
Our results relating an increasing BMI to a greater odds of major depression are consistent with the growing body of evidence of a positive association between obesity and depression in adults.7–17 Importantly, as with another investigation,11 we found an increasing likelihood of depression across the linear range of BMI values, such that even small increases within the range of ‘normal weight’ were associated with a higher likelihood of major depression. Few investigators have rigorously explored the association between weight and depression in the context of pregnancy. In a cross-sectional analysis, Cameron and colleagues 33 studied 132 low-income women and found that having a body weight that deviated substantially from the recommended weight in the third trimester was associated with a higher depressive symptom score among white women with low self-esteem. Among white women with high self-esteem, high weight deviations were negatively associated with depressive symptoms. Interestingly, weight deviation was not related to depression among the 36 black women studied. While these findings are intriguing, the authors’ method of characterizing weight prevents the disentanglement of prepregnancy weight from gestational weight gain. Our results contradict those of Carter and colleagues, 19 who reported no correlation between prepregnancy BMI and depressive symptom scores between the fifth and eighth month of pregnancy in 64 middle-class women. However, their results were limited by a reliance on depressive symptom scores rather than psychiatric diagnostic criteria, women’s self-reporting of pregravid weight at 4 months postpartum, lack of data on gestational weight gain, and failure to adjust for confounding variables. Prepregnancy obesity was associated with prevalent postpartum depression in two studies,19, 34 but neither explored the potential modifying effects of gestational weight gain.
In our study, women who entered pregnancy overweight had a high likelihood of major depression regardless of whether they gained gestational weight below, within, or above the 1990 IOM recommended ranges. Therefore, overweight mothers’ antenatal mood may be unaffected by the amount of weight gained, and rather, more strongly associated with weight at conception. The mechanisms underlying the overweight-depression relation are uncertain, but likely involve psychological, sociological, biological, and behavioral factors.35, 36 If obesity precedes depression, the extreme value placed on slimness in today’s society may cause obese women to feel stigmatized and suffer from body-image dissatisfaction that leads to chronic depression that may predate the pregnancy.37 Indeed, comorbid conditions related to weight, such as anxiety and/or eating disorders, may partially mediate this association. Furthermore, unhealthy behaviors common to overweight individuals, such as physical inactivity and poor dietary quality, may also adversely affect mood.38,39 Overweight women are more likely to experience pregnancy complications,6 which may be stressful and increase the likelihood of depressive symptoms. Biological factors such as circulating leptin concentrations may be relevant. Leptin inhibits depressive symptoms in animal models, so the leptin resistance that characterizes obesity may contribute to obese individuals’ higher prevalence of depression.40 It is crucial to underscore that although prospective studies have shown that obesity predicts the onset of major depression,11,12 the causal pathway may be reversed. Preconception depression may cause obesity in some women, as has been illustrated in several studies of nonpregnant women.13–15 Alternatively, depression and obesity may share the same underlying pathophysiology and be manifestations of the same disease.41,42 Unfortunately, we lacked data on pregravid mood and pregravid SSRI use, thereby preventing us from exploring the temporality of the association between prepregnancy BMI and depression in our population. Because it is plausible that the causal pathway goes in either direction between weight and depression, it is imperative that longitudinal data are collected in future studies to clarify the temporality of this relation.
We also observed that lean women who gained below the 1990 IOM recommended range had an elevated odds of major depression, which is consistent with previous work. Hickey et al. conducted a prospective study of depressive symptoms at 24–26 weeks and inadequate gestational weight gain in a large cohort of low-income, nonobese black and white women. The authors reported that white women in the highest quartile of depressive symptom score were 3.0 (95% CI: 1.2, 6.2) times as likely as women in the lowest quartile to have weight gain below the 1990 IOM-recommended range.43 No relationship was found between depression and low weight gain in black women. In a cohort of over 4,000 Hispanic women, self-reported feelings of depression during the pregnancy were negatively associated with pregnancy weight gain in univariate models, but this variable was no longer significant once other psychosocial factors and maternal characteristics were considered. 44 In cross-sectional studies, high depressive symptoms have been linked with negative attitudes about gaining gestational weight.21,45 Collectively, these findings indicate that weight gain below the 1990 IOM recommended range may be a marker of depression during pregnancy.
Few investigators have explored depression as it relates to gestational weight gain in excess of national recommendations. In a recent study, pregnant women who gained in excess of the 1990 IOM recommendations were more likely to have high depressive symptoms than women who met the weight gain recommendations. 46 In contrast, we found that lean women who gained above the 1990 IOM recommended range were not more likely than lean women who gained within the recommended range to be depressed during pregnancy. We also reported that the association between pregravid BMI and major depression was slightly attenuated among those who gained excessive weight. Because the confidence intervals among adequate and excessive weight gainers at the same BMI value substantially overlaped (figure 2), it is difficult to discern if this is a true finding. However, it is possible that women who gain within the IOM recommended range are more weight-conscious than women who gain more than recommended, and that pregravid obesity in this group would be associated with more psychological distress.
Our study was limited by a lack of data on body image, weight/shape satisfaction, and weight gain attitudes, which may modify the associations we observed. Prepregnancy BMI and gestational weight gain were both calculated based on maternal self-report of pregravid weight. Because women tend to underreport their weight, 47 BMI may have been underestimated and weight gain overestimated. Whether such misreporting varies by depression status, and thus would lead to differential misclassification, is not known. Although we found no evidence that the associations between weight and depression varied by race/ethnicity, we had a relatively small sample of black women (n=40), and therefore limited power to detect two-and three-way interactions among BMI, weight gain, and race. Additionally, because <3% of our population had a pregravid BMI <18.5 kg/m2, we were unable to determine with confidence the likelihood of major depression among underweight women. Unmeasured confounding by factors like comorbid psychiatric conditions, prepregnancy dietary intake and physical activity, prepregnancy access to health care, and/or maternal genetic factors predisposing to obesity and depression may have biased our results, and confounders we did collect may have been measured with error. In the future, large, racially diverse cohorts with wide ranges of BMI and weight gains and data on pre-conception mood and SSRI use, attitudes about weight, and health behaviors are needed to overcome these limitations. Our cohort had a high-risk of major depression, and additional studies are needed to determine whether or not our findings are generalizable to a broader population of pregnant women.
Our results suggest that major depression during pregnancy is prevalent among women who have gestational weight gains below the 1990 IOM recommended range and increases in prevalence as prepregnancy BMI increases. These findings signify an important public health problem, as obesity has reached epidemic proportions 3 and low weight gain occurs commonly.48 Future studies must clarify the temporality of the complex relation between pregravid weight, weight gain, and depression in pregnant women. Because maternal overweight, poor weight gain, and major depression all pose substantial risks for fetal development and birth outcomes, 6, 18, 49 it is critical that health care providers monitor depression levels of obese pregnant women and women with weight gains below the 1990 IOM recommended range in order to facilitate appropriate depression intervention.
Acknowledgements and conflicts of interest
This study was supported by NIH/NIMH grants K01 MH074092 to Dr Bodnar and R01 MH060335 to Dr.Wisner.
Drs. Bodnar, Moses-Kolko, Sit, and Hanusa report no competing interests. Dr. Wisner is on the Speaker’s Bureau of GlaxoSmithKline and receives funding from the NIMH, the Stanley Medical Research Foundation, the American Society for Bariatric Surgery, and Pfizer.
Footnotes
Presented at the Society for Maternal-Fetal Medicine Annual Meeting, Dallas, TX, January 28 – February 2, 2008.
References
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Calle EE, Thun TJ, Petrelli JM, Rodriguez C, Heath CW. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 3.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 5.Kim SY, Dietz PM, England L, Morrow B, Callaghan WM. Trends in pre-pregnancy obesity in nine states, 1993–2003. Obesity (Silver Spring) 2007;15:986–993. doi: 10.1038/oby.2007.621. [DOI] [PubMed] [Google Scholar]
- 6.Catalano PM. Management of obesity in pregnancy. Obstet Gynecol. 2007;109:419–433. doi: 10.1097/01.AOG.0000253311.44696.85. [DOI] [PubMed] [Google Scholar]
- 7.Heo M, Pietrobelli A, Fontaine KR, Sirey JA, Faith MS. Depressive mood and obesity in US adults: comparison and moderation by sex, age, and race. Int J Obes (Lond) 2006;30:513–519. doi: 10.1038/sj.ijo.0803122. [DOI] [PubMed] [Google Scholar]
- 8.Johnston E, Johnson S, McLeod P, Johnston M. The relation of body mass index to depressive symptoms. Can J Public Health. 2004;95:179–183. doi: 10.1007/BF03403643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simon GE, Von Korff M, Saunders K, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63:824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dong C, Sanchez LE, Price RA. Relationship of obesity to depression: a family-based study. Int J Obes Relat Metab Disord. 2004;28:790–795. doi: 10.1038/sj.ijo.0802626. [DOI] [PubMed] [Google Scholar]
- 11.Bjerkeset O, Romundstad P, Evans J, Gunnell D. Association of adult body mass index and height with anxiety, depression, and suicide in the general population: the HUNT study. Am J Epidemiol. 2008;167:193–202. doi: 10.1093/aje/kwm280. [DOI] [PubMed] [Google Scholar]
- 12.Roberts RE, Deleger S, Strawbridge WJ, Kaplan GA. Prospective association between obesity and depression: evidence from the Alameda County Study. Int J Obes Relat Metab Disord. 2003;27:514–521. doi: 10.1038/sj.ijo.0802204. [DOI] [PubMed] [Google Scholar]
- 13.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 14.Pine DS, Goldstein RB, Wolk S, Weissman MM. The association between childhood depression and adulthood body mass index. Pediatrics. 2001;107:1049–1056. doi: 10.1542/peds.107.5.1049. [DOI] [PubMed] [Google Scholar]
- 15.Hasler G, Pine DS, Gamma A, et al. The associations between psychopathology and being overweight: a 20-year prospective study. Psychol Med. 2004;34:1047–1057. doi: 10.1017/s0033291703001697. [DOI] [PubMed] [Google Scholar]
- 16.Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90:251–257. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158:1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine. Nutrition during Pregnancy. Washington, D.C: National Academy Press; 1990. [Google Scholar]
- 19.Carter AS, Baker CW, Brownell KD. Body mass index, eating attitudes, and symptoms of depression and anxiety in pregnancy and the postpartum period. Psychosom Med. 2000;62:264–270. doi: 10.1097/00006842-200003000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Baker CW, Carter AS, Cohen LR, Brownell KD. Eating attitudes and behaviors in pregnancy and postpartum: global stability versus specific transitions. Ann Behav Med. 1999;21:143–148. doi: 10.1007/BF02908295. [DOI] [PubMed] [Google Scholar]
- 21.DiPietro JA, Millet S, Costigan KA, Gurewitsch E, Caulfield LE. Psychosocial influences on weight gain attitudes and behaviors during pregnancy. J Am Diet Assoc. 2003;103:1314–1319. doi: 10.1016/s0002-8223(03)01070-8. [DOI] [PubMed] [Google Scholar]
- 22.Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. American Journal of Psychiatry. doi: 10.1176/appi.ajp.2008.08081170. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Briggs G, Freeman R, Yaffe S. Drugs in pregnancy and lactation. Baltimore, MD: Williams and Wilkins; 1994. [Google Scholar]
- 24.First MB, Spitzer RL, Gibbon MW, Janet BW, Benjamin L. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II), Version 2.0: Biometrics Research Department. New York State Psychiatric Institute. 1994 [Google Scholar]
- 25.Post RM, Roy-Byrne PP, Uhde TW. Graphic representation of the life course of illness in patients with affective disorder. Am J Psychiatry. 1988;145:844–848. doi: 10.1176/ajp.145.7.844. [DOI] [PubMed] [Google Scholar]
- 26.Wisner KL, Peindl KS, Hanusa BH. Psychiatric episodes in women with young children. J Affect Disord. 1995;34:1–11. doi: 10.1016/0165-0327(94)00097-s. [DOI] [PubMed] [Google Scholar]
- 27.Williams J, Terman M. Structured Interview Guide for the Hamilton Depression Rating Scale with Atypical Depression Supplement (SIGH-ADS) New York: New York State Psychiatric Institute; 2003. [Google Scholar]
- 28.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.NHLBI Expert Panel. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Obes Res. 1998;6:51S–209S. [PubMed] [Google Scholar]
- 30.Bodnar LM, Siega-Riz AM, Arab L, Chantala K, McDonald T. Predictors of pregnancy and postpartum iron status in low-income women. Public Health Nutr. 2004;7:701–711. doi: 10.1079/phn2004597. [DOI] [PubMed] [Google Scholar]
- 31.StataCorp. Stata Statistical Software: Release 8.0. College Station, TX: Stata Corporation; 2003. [Google Scholar]
- 32.Witte JS, Greenland S. A nested approach to evaluating dose-response and trend. Ann Epidemiol. 1997;7:188–193. doi: 10.1016/s1047-2797(96)00159-7. [DOI] [PubMed] [Google Scholar]
- 33.Cameron RP, Grabill CM, Hobfoll SE, Crowtherx JH, Ritter C, Lavin J. Weight, self-esteem,ethnicity, and depressive symptomatology during pregnancy among inner-city women. Health Psychol. 1996;15:293–297. doi: 10.1037//0278-6133.15.4.293. [DOI] [PubMed] [Google Scholar]
- 34.La Coursiere DY, Baksh L, Bloebaum L, Varner MW. Maternal Body Mass Index and Self-Reported Postpartum Depressive Symptoms. Matern Child Health J. 2006 doi: 10.1007/s10995-006-0075-1. [DOI] [PubMed] [Google Scholar]
- 35.Friedman MA, Brownell KD. Psychological correlates of obesity: moving to the next research generation. Psychol Bull. 1995;117:3–20. doi: 10.1037/0033-2909.117.1.3. [DOI] [PubMed] [Google Scholar]
- 36.Ross CE. Overweight and depression. J Health Soc Behav. 1994;35:63–79. [PubMed] [Google Scholar]
- 37.Friedman KE, Reichmann SK, Costanzo PR, Musante GJ. Body image partially mediates the relationship between obesity and psychological distress. Obes Res. 2002;10:33–41. doi: 10.1038/oby.2002.5. [DOI] [PubMed] [Google Scholar]
- 38.Bodnar LM, Wisner KL. Nutrition and depression: implications for improving mental health among childbearing-aged women. Biol Psychiatry. 2005;58:679–685. doi: 10.1016/j.biopsych.2005.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brown WJ, Ford JH, Burton NW, Marshall AL, Dobson AJ. Prospective study of physical activity and depressive symptoms in middle-aged women. Am J Prev Med. 2005;29:265–272. doi: 10.1016/j.amepre.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 40.Lu XY. The leptin hypothesis of depression: a potential link between mood disorders and obesity? Curr Opin Pharmacol. 2007;7:648–652. doi: 10.1016/j.coph.2007.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosmond R. Obesity and depression: same disease, different names? Med Hypotheses. 2004;62:976–979. doi: 10.1016/j.mehy.2003.12.030. [DOI] [PubMed] [Google Scholar]
- 42.Bornstein SR, Schuppenies A, Wong ML, Licinio J. Approaching the shared biology of obesity and depression: the stress axis as the locus of gene-environment interactions. Mol Psychiatry. 2006;11:892–902. doi: 10.1038/sj.mp.4001873. [DOI] [PubMed] [Google Scholar]
- 43.Hickey CA, Cliverx SP, Goldenberg RL, McNeal SF, Hoffman HJ. Relationship of psychosocial status to low prenatal weight gain among nonobese black and white women delivering at term. Obstet Gynecol. 1995;86:177–183. doi: 10.1016/0029-7844(95)00161-j. [DOI] [PubMed] [Google Scholar]
- 44.Siega-Riz AM, Hobel CJ. Predictors of poor maternal weight gain from baseline anthropometric, psychosocial, and demographic information in a Hispanic population. J Am Diet Assoc. 1997;97:1264–1268. doi: 10.1016/s0002-8223(97)00303-9. [DOI] [PubMed] [Google Scholar]
- 45.Stevens-Simon C, Nakashima I, Andrews D. Weight gain attitudes among pregnant adolescents. J Adolesc Health. 1993;14:369–372. doi: 10.1016/s1054-139x(08)80009-2. [DOI] [PubMed] [Google Scholar]
- 46.Webb JB, Siega-Riz AM, Dole N. Psychosocial Determinants of Adequacy of Gestational Weight Gain. Obesity (Silver Spring) 2008 doi: 10.1038/oby.2008.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brunner Huber LR. Validity of self-reported height and weight in women of reproductive age. Matern Child Health J. 2007;11:137–144. doi: 10.1007/s10995-006-0157-0. [DOI] [PubMed] [Google Scholar]
- 48.National Research Council and Institute of Medicine. Influence of Pregnancy Weight on Maternal and Child Health. Committee on the Impact of Pregnancy Weight on Maternal and Child Health. Board of Children Y, and Families, Division of Behavioral and Social Sciences and Education and Food and Nutrition Board, Institute of Medicine, ed. Washington, DC: The National Academies Press; 2007. Workshop Report. [Google Scholar]
- 49.Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. 2007;20:189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]