Abstract
Seventy six individuals with a principal diagnosis of generalized anxiety disorder (GAD) were randomly assigned to receive either an MI pretreatment or no pretreatment (NPT), prior to receiving CBT. Significant group differences favoring the MI-CBT group were observed on the hallmark GAD symptom of worry and on therapist-rated homework compliance, which mediated the impact of treatment group on worry reduction. Adding MI pretreatment to CBT was specifically and substantively beneficial for individuals with high worry severity at baseline. There was evidence of relapse at 6-month follow-up for high severity individuals who received MI-CBT, but significant moderator effects favoring the high severity MI-CBT group were again apparent at 12-months post-treatment. Pending replication in a more controlled test, these findings suggest that MI may be a promising adjunct to CBT for GAD for those of high severity, a group which has been less responsive to CBT in past research.
Keywords: Motivational Interviewing, generalized anxiety, cognitive behavioral therapy, worry, motivation
Generalized Anxiety Disorder (GAD) is a chronic condition characterized by excessive and uncontrollable worry. It is associated with significant personal (Mendlowicz & Stein, 2000) and economic (Katon et al., 1990) costs as well as low rates of spontaneous remission (Hirschfeld, 1996). In addition, worry may be a core developmental feature of other anxiety and mood disorders (Brown & Barlow, 2002).
The most extensively researched treatments for GAD consist of variations of Cognitive Behavior Therapy (CBT; Borkovec & Costello, 1993; Borkovec & Mathews, 1988; Borkovec, Newman, Pincus, & Lytle, 2002). Although outcome studies have yielded significant effects (Barlow, Allen, & Basden, 2007), relatively weak outcomes have been found for GAD compared to outcomes for other anxiety disorders. For example, a recent paper by one of the leading GAD research teams concluded that while effective, CBT has the lowest average effect size for GAD when compared to effect sizes of CBT for other anxiety disorders (Newman, Castonguay, Borkovec, Fisher, & Nordberg, 2008).
Improving Response Rates to CBT for GAD
In an attempt to improve response rates, investigators have developed CBT-based therapies that target core processes in GAD, such as intolerance of uncertainty (Ladouceur et al., 2000), meta-cognitive factors such as erroneous beliefs about worry (Wells & King, 2006), and interpersonal problems and emotional avoidance (Newman et al., 2008). Both the intolerance of uncertainty model of Dugas and colleagues (e.g., Dugas & Robichaud, 2006) and the metacognitive model of Wells and colleagues (e.g., Wells & King, 2006) incorporate an explicit focus on positive and negative beliefs about worry itself. Promising findings with each of these adaptations of CBT are being reported.
In the present study, we chose to provide an initial test of the value of adding a motivational pretreatment to an established form of CBT for GAD. Motivational Interviewing (MI; Miller & Rollnick, 2002), an approach designed to increase intrinsic motivation for and decrease ambivalence about change might be a particularly good fit for GAD. Numerous studies have demonstrated that although clients with GAD see worry as a problem, they also hold positive beliefs about worry (e.g., it is motivating; it helps solve problems) and are therefore ambivalent about relinquishing it (Borkovec & Roemer, 1995; Freeston, Rheaume, Letarte, Dugas, & Ladouceur, 1994). Moreover, worry itself has been found to have important avoidant and self-reinforcing functions, protecting the individual from experiencing frightening emotional arousal (Borkovec, 1994). Similar themes of the adaptive functions of worry have emerged in case study work of clients with GAD (Westra & Arkowitz, in press; Westra, 2004). If much ambivalence is not addressed, it seems likely that clients will show relatively low motivation for change in therapy.
Motivational Interviewing as a Pretreatment
MI was originally developed by Miller and Rollnick (2002) who defined it as “a client-centered, directive approach designed to enhance intrinsic motivation for change through understanding and resolving ambivalence about change”. The relational context, which is called the MI spirit, consists of collaboration, evocation, and preserving client autonomy. In MI, the therapist does not take the role of change advocate, but instead tries to help the client become the advocate for change. Four central principles of MI are: (1) express empathy; (2) develop discrepancy between the undesirable behaviors and values that are inconsistent with those behaviors; (3) roll with resistance rather than confronting it directly; and, (4) support self-efficacy. Several of the MI skills come directly from Rogers’ client-centered therapy (1951) and include: asking open-ended questions, listening reflectively, affirming, and summarizing. However, one method – eliciting and reinforcing change talk -is intentionally but subtly directive and specific to MI. MI therapists also employ decisional balance procedures to help clients explore and weigh the pros and cons of change while using other MI skills to help tip the balance toward change.
More than 100 randomized controlled trials of MI have been published, along with several meta-analytic reviews (e.g. Burke, Arkowitz, & Menchola, 2003; Hettema, Steele, & Miller, 2005). These reviews have found strong evidence for MI as a brief pretreatment followed by more directive non-MI interventions in the areas of substance dependence and health-related behaviors.
Recently, researchers have begun to apply MI to other clinical problems including anxiety disorders (Arkowitz, Westra, Miller, & Rollnick, 2008). Consistent with the early stage of this research, much of this work has involved case studies or small, uncontrolled pilot studies (Buckner, Roth Ledley, Heimberg, & Schmidt, in press; Simpson, Zuckoff, Page, Franklin, & Foa, 2008; Westra, 2004). For example, Westra and Dozois (2006) found that an MI pretreatment enhanced the efficacy of group CBT for a mixed anxiety disorders group compared to those who received only the group CBT.
The present study is an initial controlled test of whether adding an MI pretreatment to CBT for GAD specifically would enhance outcome. Utilizing 76 clients with a principal diagnosis of GAD, we compared the efficacy of a brief MI pretreatment followed by CBT (MI-CBT) with a group that received no pretreatment (4 week wait) followed by CBT (NPT-CBT). Although this study did not equate for therapist contact time across the 2 treatment groups, it does provide an important first step in evaluating the viability of adding MI to CBT for GAD which can help determine whether more rigorous future tests are indicated. If indicated, the present study can also help inform the design of such future studies.
Hypotheses
Our first hypothesis was that the MI-CBT group would show greater improvements in worry and anxiety than the comparison, NPT-CBT group. The second hypothesis was that the MI-CBT group would show greater homework compliance in CBT than the NPT-CBT group. In addition, we hypothesized that improved response in the MI-CBT group compared to the NPT-CBT group would be mediated by increased homework compliance. Finally, we were interested in exploring individual differences which might serve as indications for adding MI to CBT. In addition to examining motivation in this regard, we investigated severity as a potential moderator of outcome given findings from others studies suggesting that adding MI may be particularly beneficial for those of high symptom severity (Hodgins & Diskin, 2008; Handmaker, Miller, & Manicke, 1999). Theoretically, high severity worriers may be more ambivalent or skeptical about change than those of moderate worry severity and/or may have higher levels of interpersonal problems, and thus might preferentially benefit from a treatment such as MI which aims to enhance motivation through the creation of a strong therapeutic relationship.
Method
All measures and procedures in the present study were approved by a local Institutional Ethics Review Board for research involving human participants.
Participants
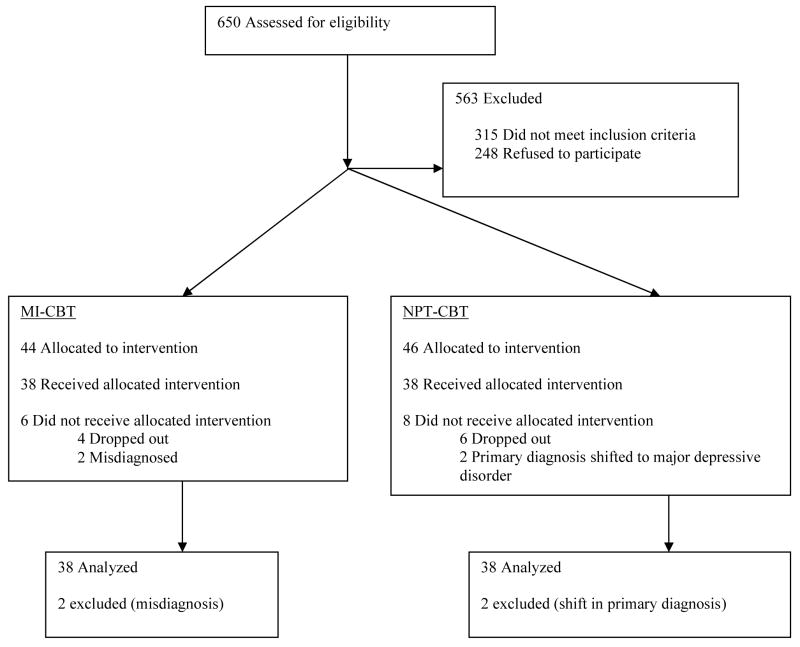
Participants were recruited from community advertisements in the greater Toronto area targeting individuals who worry excessively. No participant was paid for his or her involvement with the study. Figure 1 presents number of participants enrolled, randomized, and included in the analysis (Altman et al. & CONSORT group, 2001). The high number of participants screened out at the phone intake level is largely due to the significant travel time required from many locations within Toronto in order to reach the study site, since York University is not accessible by subway. Seventy-five percent of individuals who contacted the clinic self-selected out of the study for this reason.
Figure 1.
Flow diagram of movement of participants through the trial.
All clients who were currently on antidepressant medication had been stabilized on this medication for at least 2 months and all agreed to maintain the current medication and dosage throughout treatment. Using checks at every other therapy session, 1 client reported beginning a new antidepressant late in treatment (NPT-CBT) and another reported using a benzodiazepine infrequently for sleep (MI-CBT). Both of these clients were permitted to complete treatment and were included in the final sample. Also, using checks at each therapy session, all clients reported fulfilling the study requirement of not beginning any other psychotherapy during the course of their treatment within the study.
Design & Procedure
Selection
Clients were enrolled over a 2-year period from November 2005 to November, 2007. Potential participants who passed the initial telephone screening were administered the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV: Brown, DiNardo, & Barlow, 1994). The phone screen emphasized the criteria for GAD and only those who had a high probability of meeting criteria for a diagnosis of GAD were invited to complete the ADIS-IV interview. ADIS-IV interviews were conducted by advanced clinical psychology graduate students who were trained to criterion in the administration of this diagnostic instrument. Interviewers also completed severity ratings of GAD and of comorbid diagnoses. Inter-rater reliability based on a random sample of 20% of audiotaped interviews for those who were successfully enrolled in the study was good, with an overall kappa for all diagnoses of .75, and 1.0 for GAD. The correlation between raters for GAD severity was r = .794, p<.001. Additional selection criteria included being at least 16 years of age, receiving a GAD severity score on the ADIS-IV of at least 4, absence of concurrent psychotherapy, no concurrent substance dependence, no history of psychotic or bipolar mood disorder, no evidence of neurological problems, major cognitive impairment or learning disability, and no use of benzodiazepines for at least 2 months prior to enrollment in the study. The ADIS-IV was also readministered at 12-months post-treatment by interviewers who were blind to client pretreatment group status. Clients were randomly assigned to treatment condition by the research co-ordinator using a random numbers table.
Measures
Outcome Measures: The Penn State Worry Questionnaire (PSWQ, Meyer, Miller, Metzger, & Borkovec, 1990)
The PSWQ, a widely used 16-item instrument assessing trait worry, was employed as the principal outcome measure. The PSWQ possesses high internal consistency and temporal stability, as well as good convergent and discriminant validity (Brown, Antony, & Barlow, 1992; Meyer et al., 1990). It also differentiates individuals with GAD from those with other anxiety disorders (Brown et al., 1992). Scores range from 16–80, with higher scores indicating greater worry.
The Depression Anxiety Stress Scales (DASS, Lovibond & Lovibond, 1995)
The 42-item DASS has been recommended for inclusion in the assessment of GAD (e.g., Campbell & Brown, 2002) since it may be a better measure of the tension and persistent arousal characteristic of GAD than other commonly used measures of somatic arousal. The DASS demonstrates good reliability and validity and is a better discriminator between anxiety and depression than many other commonly used measures (Antony, Bieling, Cox, Enns, & Swinson, 1998; Lovibond & Lovibond, 1995). The factor structure of the measure has been replicated in nonclinical (Lovibond & Lovibond, 1995) and clinical (Brown, Chorpita, Korotitscw, & Barlow, 1997) samples. Scores on each subscale (depression, anxiety, stress) range from 0–42, with higher scores reflecting a higher level of the construct being assessed.
The Sheehan Disability Scale (SDS: Sheehan, 1983)
This 3-item commonly used scale, assesses the degree of functional impairment in the domains of work, social life, and family life (Bieling, McCabe, & Antony, 2004). Scores range from 0–30, with higher scores reflecting higher levels of disability. The internal reliability of the SDS is high (coefficient alpha = .89) and adequate construct validity has been established (Sheehan, Harnett-Sheehan, & Raj, 1996).
The Meta-Cognitions Questionnaire – Short Form (MCQ30)
The MCQ30 (Wells & Cartwright-Hatton, 2004) is a short form of the original MCQ (Cartwright-Hatton & Wells, 1997) and measures beliefs about worry. It consists of 5 factor-analytically derived subscales: positive beliefs about worry, beliefs about controllability and danger, beliefs about cognitive competence, negative worry beliefs, and cognitive self-consciousness. The MCQ30 has been found to have a factor structure nearly identical to the original scale and has good internal consistency, convergent and construct validity (Wells & Cartwright-Hatton, 2004). Total scores range from 30–120, with higher scores reflecting higher levels of worry beliefs.
The Clinical Global Impression Scale (CGI, Guy, 1976)
This widely used clinician-rating scale, assesses the overall severity of symptoms as well as changes in functioning over time. Validity of the CGI is supported through findings of significant correlations with self-report and clinician-administered measures of symptom severity in anxiety (Zaider, Heimberg, Fresco, Schneier, & Liebowitz, 2003). Scores on the CGI also appear sensitive for discriminating between responders and nonresponders in CBT (e.g., Heimberg et al., 1998) for anxiety. Scores range from 1–7, with higher scores reflecting higher client severity, and greater levels of improvement, respectively.
Motivation Measure: The Client Motivation for Psychotherapy Scale (CMOTS, Pelletier, Tuscon, & Haddad, 1997)
The CMOTS is a 24-item measure of client motivation for therapy based on the self-determination theory of Deci and Ryan (1985) which postulates 6 different types of motivation. For the purpose of this study, we administered only the intrinsic motivation subscale since Miller and Rollnick (2002) have hypothesized that the efficacy of MI is in part due to its ability to increase intrinsic motivation. Although the measure consists of only 4 items, its construct validity has been demonstrated through findings that participants with greater intrinsic motivation reported greater intentions to persist in therapy. Also, therapists who provided more autonomy and less control had clients who scored higher on intrinsic motivation (Pelletier, Tuson, & Haddad, 1997). Scores range from 4–28, with higher scores reflecting greater intrinsic motivation.
Homework Compliance Scale (HCS: Primakoff, Epstein, & Covi, 1986)
Clients and therapists rated the degree of client homework compliance throughout CBT using the single item HCS. Higher scores on the HCS have been associated with more positive outcome in CBT (Bryant, Simons, & Thase, 1999; Taft, Murphy, King, Musser, & DeDeyn, 2003). Scores range from 0–6, with higher scores reflecting higher levels of homework compliance.
Outcome measures were completed by patients in a self-report format at the clinic at baseline, after the pretreatment period, post-CBT, and at 6- and 12-months post-treatment. The order of the presentation of the tests at each assessment point was randomized for each subject. The clinician-rated Clinical Global Impression Scale (CGI) was completed by the CBT therapists after session 1 of CBT and post-CBT. The measure of motivation (CMOTS) was administered at baseline and after the pre-treatment period. Finally, the patient and therapist versions of the homework compliance scale (HCS) were completed after sessions 2, 4, 6, and 8 of CBT. The comprehensive battery of tests is consistent with studies in this area which assess a range of relevant constructs (depression, disability, worry beliefs, etc.) in addition to the core symptom of worry in order to gage breadth of treatment effects.
Treatment Integrity
MI adherence was assessed using the Motivational Interviewing Treatment Integrity Code Version 2.0 (MITI; Moyers, Martin, Manuel, Hendrickson, & Miller, 2005). Five clinical graduate students were trained by a student of one of the original developers of the MITI. Ratings were derived from a random 20 minute segment of 90% of the MI sessions. Working in pairs, raters first independently made 2 global ratings (empathy and MI spirit), each on a 7-point scale with higher scores reflecting higher levels of the construct. Then disagreements were resolved by discussion to establish consensus. Regular group meetings were also held to reduce rater drift. The intraclass correlation coefficients calculated from a random sample of 15% of tapes that were independently double-coded, were .74 for empathy and .72 for MI spirit.
Treatment integrity for the CBT was assessed using the Cognitive Therapy Rating Scale (CTRS: Young & Beck, 1980). Ratings are made on 11 different dimensions including interpersonal skills (e.g., collaboration, understanding), and specific CT skills (e.g., focus on key cognitions, application of CBT techniques), and also for overall session quality. Scores range from 0–66 with higher scores reflecting higher levels of CBT adherence. A random subsample of 20% of cases for each CBT therapist was chosen, including 3 sessions per client (from the beginning, middle, and end of CBT) for each treatment group. Three clinical psychology graduate students were trained to criterion by the first and third authors (both highly experienced CBT clinicians). Raters were blind to client pretreatment group assignment. They worked in pairs, making ratings independently and then resolving disagreements through discussion to achieve consensus. Double coding a subset of 15% of independently coded tapes to assess rater reliability, yielded an intra-class correlation coefficient of .84.
Therapist Blindness
At the completion of treatment, CBT therapists were asked to guess each client’s pretreatment condition and to indicate whether or not the client had mentioned their pretreatment condition during the CBT and/or they somehow became aware of the client’s pretreatment status.
Therapists and Therapist Training
In the present study, different therapists delivered the MI and the CBT. Four experienced female therapists delivered the MI pretreatment. Two were Ph.D. level clinical psychologists, one of whom was the first author, and 2 were senior clinical doctoral students. Each therapist saw at least 7 clients (range 7–12). The 4 CBT therapists (2 female, 2 male) included 1 Ph.D. psychologist, 2 senior and 1 junior clinical psychology graduate student. Each CBT therapist saw at least 13 clients (range 13 to 34) and an equal number of clients from the 2 treatment groups. Clients were randomly assigned to therapists within both the MI and CBT, within the constraint of therapist availability.
Therapist Training
Training for both treatments consisted of readings, at least 30 hours of discussion and role-play, and weekly group supervision with the study authors (separately for the MI and the CBT) including review of videotapes. Two highly experienced MI therapists (HW, HA) trained and supervised the MI therapists, and 2 highly experienced CBT therapists (HW, DD) trained and supervised the CBT therapists.
Treatment Conditions
MI Pretreatment
Participants in the MI pretreatment condition (MI-CBT) received 4 individual 50-minute weekly MI sessions. The MI followed the principles and methods described by Miller and Rollnick (2002), but with a focus on ambivalence and motivation to change worry and related problems. Treatment followed the manual developed by Westra and Dozois (2003) adapting MI for the treatment of anxiety1. More detailed descriptions of this treatment for anxiety in general, and for GAD in particular, can be found in Westra and Dozois (2008) and Westra and Arkowitz (in press), respectively. This manual describes the 2 phases of MI, with phase 1 focused on understanding and exploring ambivalence and phase 2 focused on developing self-efficacy. Application of MI principles and a description of various exercises for use within each phase are outlined in the manual (e.g., decisional balance in phase 1, role plays for strengthening change talk in phase 2), in additional to explicating how MI differs from CBT.
CBT
After MI pretreatment (or a 4-week waiting period for individuals in the NPT condition), participants received individual CBT for GAD. Treatment followed the manual developed by Borkovec and his colleagues (Borkovec & Costello, 1993; Borkovec & Mathews, 1988; Borkovec et al., 2002) which focuses the core features of GAD: chronic hyperarousal, uncontrollable worry, and inhibited emotional reprocessing secondary to worry. Treatment consisted of training in self-monitoring, applied relaxation, cognitive therapy, behavioral approach tasks, and exposure to worry and worry cues. Therapy sessions consisted of 6 weekly 2-hour sessions, followed by 2 1-hour sessions, for a total of 14 hours of CBT for each group. Therapists were instructed to deliver each component in the course of treatment, but the timing and duration of their delivery were left to the judgment of the therapists based on the needs, feedback, and responsiveness of the client to each treatment element. Interventions consistent with MI were disallowed.
Results
Sample Characteristics
Characteristics of those who completed treatment are presented in Table 1. The sample was ethnically diverse, generally well-educated, had a chronic worry problem, and 63% had at least 1 other clinically significant diagnosis beyond GAD. The most common Axis I comorbidities were social phobia (N=10 MI-CBT, N=9 NPT-CBT), specific phobia (N=3 MI-CBT, N=6 NPT-CBT), dysthymia (N=6 MI-CBT, N=9 NPT-CBT) and major depressive episode (N=3 MI-CBT, N=4 NPT-CBT). Ten individuals (9% of the sample) dropped out of treatment: 6 from the NPT-CBT group and 4 from the MI-CBT group, X2 (1) = 0.35, p=.552 (see Figure 1).
Table 1.
Sample Characteristics by Treatment Group
| Measure | MI-CBT (N=38) | NPT-CBT (N=38) |
|---|---|---|
| Gender | 24 Female | 27 Female |
| 14 Male | 11 Male | |
| Age | M=42.97, SD=13.11 | M=40.89, SD=11.73 |
| Ethnicity | 21 Caucasian | 22 Caucasian |
| 8 Asian | 9Asian | |
| 5 Hispanic | 4 Hispanic | |
| 4 African Canadian | 3 African Canadian | |
| Marital status | 19 married/cohabitating | 19 Married/cohabitating |
| 10 Never Married | 14 Never Married | |
| 9 Divorced/Widowed/Separated | 5 Divorced/Widowed/Separated | |
| Employment status | 10 unemployed/not in school | 8 unemployed/not in school |
| 28 employed/in school | 30 employed/in school | |
| Highest level of education | 1 Elementary | 3 elementary |
| 8 high school | 10 high school | |
| 21 post-secondary | 21 post-secondary | |
| 8 graduate school | 4 graduate school | |
| Average family income | 14 less than $40,000 | 13 less than $40,000 |
| 13 $40–80,000 | 15 $40–80,000 | |
| 11 greater than $80,000 | 10 greater than $80,000 | |
| Worry chronicity | M=21.8 years (Range 2.08 to 60) | M=20 years (Range 0.6 –57.5) |
| Concurrent antidepressant use | 8 Yes | 9 Yes |
| 30 No | 29 No | |
| Past psychotropic medication use | 17 Yes | 19 Yes |
| 21 No | 19 No | |
| Previous counseling | 26 Yes | 27 Yes |
| 12 No | 11 No | |
| Comorbidity | 13 Anxiety Disorder | 12 Anxiety Disorder |
| 9 Depression/Dysthymia | 14 Depression/Dysthymia | |
| Previous depressive episodes | M=1.19, SD=1.82 | M=1.24, SD=1.78 |
Treatment Integrity
The overall quality of the MI pretreatment sessions was high with global ratings of empathy on the MITI averaging 5.79/7 (SD=1.08) and MI spirit averaging 5.62/7 (SD=1.05). The overall rating of the CBT sessions was good, with total scores on the CTRS averaging 41.92 (SD=13.84). This compares favorably with the average score of 41.28 (SD=4.24) on the CTRS in the CBT group of the Depression Collaborative Research Program (Shaw et al., 1999).
Penetration of the blind
A chi-square analysis was conducted on the judgments of the CBT therapists as to whether their clients received MI pretreatment or no pretreatment. Those clients (N=10; 7 MI, 3 NPT) who disclosed their pretreatment group assignment to their CBT therapists were eliminated from this analysis in order to retain only those cases for whom therapists had to guess at treatment group assignment. Results revealed clear evidence of blind penetration, X2(1) = 10.29, p<.001. CBT therapists correctly guessed the treatment condition of 54% of the MI pretreatment group and 83% of the no pretreatment group.
Preliminary Analyses
Table 2 displays means and standard deviations (SDs) of the measures over time for each treatment group. Between groups t-tests indicated no significant group differences at baseline on any measure including demographic variables, concurrent medication use, diagnostic comorbidity, or treatment history variables. For the calculation of between group effect sizes, the following formula was used: (Mean of MI-CBT minus Mean of NPT-CBT)/pooled SD.
Table 2.
Means and SDs for all Measures Across Time by Treatment Group
| Measure & Condition | Baseline | After-Pretreatment | Post-CBT | 6-months | 12-months | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| PSWQ | M | SD | M | SD | M | SD | M | SD | M | SD |
| MI-CBT | 67.34 | 8.20 | 62.34 | 11.00 | 35.63 | 10.75 | 40.61 | 14.78 | 39.86 | 12.71 |
| NPT-CBT | 66.63 | 8.34 | 66.18 | 9.02 | 42.62 | 15.46 | 43.54 | 15.17 | 42.76 | 16.59 |
| DASS | ||||||||||
| Depression | ||||||||||
| MI-CBT | 13.76 | 10.47 | 11.47 | 9.01 | 5.53 | 7.36 | 7.78 | 6.97 | 7.39 | 9.58 |
| NPT-CBT | 15.76 | 11.29 | 13.50 | 10.32 | 5.13 | 5.21 | 6.68 | 5.49 | 6.34 | 7.25 |
| Anxiety | ||||||||||
| MI-CBT | 11.82 | 7.89 | 9.74 | 7.65 | 4.21 | 4.23 | 4.44 | 3.11 | 5.14 | 4.76 |
| NPT-CBT | 10.53 | 7.80 | 10.61 | 7.12 | 4.76 | 4.80 | 4.68 | 3.12 | 4.91 | 5.11 |
| Stress | ||||||||||
| MI-CBT | 22.53 | 10.13 | 17.74 | 8.74 | 9.92 | 8.30 | 12.36 | 7.73 | 13.14 | 8.54 |
| NPT-CBT | 21.0 | 8.95 | 22.08 | 9.74 | 10.50 | 6.31 | 11.32 | 6.08 | 11.41 | 7.62 |
| SDS | ||||||||||
| MI-CBT | 17.68 | 5.57 | 15.59 | 6.87 | 7.30 | 5.69 | 8.94 | 6.44 | 8.36 | 7.74 |
| NPT-CBT | 17.61 | 7.27 | 15.84 | 7.98 | 8.55 | 5.97 | 8.30 | 5.92 | 8.31 | 7.03 |
| ADIS: GAD severity | ||||||||||
| MI-CBT | 6.03 | 0.97 | --- | --- | --- | --- | --- | --- | 2.29 | 2.01 |
| NPT-CBT | 6.03 | 0.75 | --- | --- | --- | --- | --- | --- | 2.73 | 2.32 |
| CGI: Severity | ||||||||||
| MI-CBT | --- | --- | 5.41 | 1.21 | 2.57 | 1.39 | --- | --- | --- | --- |
| NPT-CBT | --- | --- | 5.19 | 1.13 | 2.57 | 1.12 | --- | --- | --- | --- |
| CGI: Improvement | ||||||||||
| MI-CBT | --- | --- | 4.05 | 0.32 | 6.55 | 0.69 | --- | --- | --- | --- |
| NPT-CBT | --- | --- | 3.92 | 0.36 | 6.32 | 0.67 | --- | --- | --- | --- |
| MCQ30 (Total) | ||||||||||
| MI-CBT | 72.29 | 14.24 | 74.31 | 15.07 | 54.84 | 12.85 | 56.17 | 14.17 | 55.81 | 14.46 |
| NPT-CBT | 68.82 | 12.64 | 69.05 | 14.92 | 55.76 | 9.82 | 55.74 | 10.28 | 53.03 | 10.37 |
Effects of Adding an MI Pretreatment to CBT on Worry
To examine our main hypothesis that adding MI to CBT would improve response to CBT, an ANCOVA with treatment group (MI-CBT, NPT-CBT) as the independent variable was conducted on the principal outcome measure, the PSWQ, with baseline PSWQ scores serving as the covariate. A significant effect was obtained, F (1,73) = 5.51, p = .022; participants who received MI-CBT demonstrated significantly lower post-treatment PSWQ scores than participants who received NPT-CBT. The between-group post-treatment effect size of d=.53 was moderate (Cohen, 1988).
When PSWQ scores after the pretreatment period served as the covariate, a marginally significant effect of treatment group was observed on post-CBT PSWQ scores, F(1,74) = 3.77, p = .056, favoring the MI-CBT group. That is, a significant proportion of the additional treatment gains in the MI-CBT group were made in the pretreatment period alone. In particular, an ANCOVA, using post-pretreatment PSWQ scores as the outcome variable (and baseline PSWQ scores as the covariate), revealed a significant treatment group effect, F (1,73) = 4.39, p = .040. Four sessions of MI alone resulted in significantly reduced worry scores compared to no treatment (4 week wait).
In summary, the MI-CBT group significantly outperformed the NPT-CBT group in worry reduction over the entire treatment period, with some of these additional gains being accounted for by MI pretreatment alone (compared to no treatment over the same period) and to a lesser extent, some in the CBT treatment period.
Clinical significance of worry reduction
Recovery status was evaluated using Jacobson and Truax (1991) criteria. Reliable change and clinical cut-off scores were determined for the PSWQ2. In order to be considered a responder, a participant had to exhibit reliable change, with post-CBT scores in the normal range. A partial responder was someone who showed reliable change but did not fall within normal limits post-treatment, and a nonresponder showed no reliable change.
Chi-square analysis showed a significant between group difference in recovery status on the PSWQ, χ2(2) = 9.03, p = .011. The MI-CBT group contained a very high percentage of treatment responders (92%; n=35) and zero nonresponders, whereas the NPT-CBT group had a lower percentage of treatment responders (71%; n=27) and many more nonresponders (21%; n=8). Both groups showed a small and equal percentage of partial responders (8% n=3). In summary, adding MI to CBT was associated with more clinically significant reductions in worry over the course of treatment compared to CBT without any pretreatment.
We also examined clinically significant response following the pretreatment period and before CBT (MI versus no treatment). The effect of treatment group was significant, χ2(2) = 7.73, p = .021, with 21% (n=8) of those receiving MI achieving recovery after the 4 sessions of MI alone compared with 3% (n=1) of the no treatment group. An additional 8% (n=3) of the MI group demonstrated partial response to MI alone, compared with 3% (n=1) of the no treatment group.
Taken together, these findings demonstrate that the MI-CBT group achieved a higher rate of clinically significant recovery with treatment compared to the NPT-CBT group, with some individuals recovering in the MI alone pretreatment period and most recovering with the combination of MI and CBT.
Effects of Adding an MI Pretreatment to CBT on Other Symptom Measures
For the other symptom outcome measures (DASS-depression, DASS-anxiety, DASS-stress, SDS, MCQ30, CGI), a MANCOVA with baseline scores serving as the covariates and post-CBT scores as the outcome measures, revealed no significant treatment group effects, F(7,58) = 1.30, p = .268. Both treatment groups demonstrated significant reductions in depression, F(1,64) = 4.03, p = .049, MCQ30 scores, F(1,64) = 4.71, p = .034, disability, F(1,64) = 15.03, p = .000, and clinician rated severity, F(1,64) = 4.42, p = .039 from baseline to post-CBT. When scores over the pretreatment period were similarly examined, a significant treatment group effect was observed for DASS stress, F(1,64) = 7.48, p = .008, with MI alone resulting in significant reductions in stress compared with no treatment over the same period.
Effect of the MI Pretreatment on Homework Compliance in CBT
To examine our second main hypothesis that adding MI to CBT would improve engagement with CBT, a between groups t-test for therapist-rated homework compliance was conducted. MI-CBT participants were rated by CBT therapists as doing significantly more homework (M=4.59, SD=0.53) than those in the NPT-CBT group (M=4.19, SD=0.80), t(74) = 2.55, p = .013. The effect size for this difference was moderate at d=.59. There were no significant between-groups differences for client-rated homework compliance, t (74) = 1.11, p = .272, with a small effect size of d=.26, favoring the MI-CBT group (MI-CBT: M=4.13, SD=0.78, NPT-CBT: M=3.91, SD=0.92).
Does homework compliance mediate the relationship between treatment group and outcome?
Following recommendations by Baron and Kenny (1986), we used multiple regression to predict changes in PSWQ scores during CBT (i.e., after pretreatment PSWQ to post-CBT PSWQ). Treatment group was a marginally significant predictor of PSWQ scores post-CBT, t = 1.94, p = .056, beta = .22, controlling for PSWQ scores after the pretreatment period. Next, treatment group was significantly associated with therapist-rated homework adherence in CBT, t = 2.69, p = .009, beta = .30, with higher homework compliance reported for the MI-CBT group. In the third step, greater homework compliance in CBT was significantly predictive of lower PSWQ scores post-CBT, controlling for pre-CBT (after pretreatment) PSWQ scores and treatment group, t = 2.75, p = .008, beta = −.31. Finally, the impact of treatment group on PSWQ outcomes over the course of CBT was reduced to nonsignificance when controlling for the proposed mediator, homework compliance, t = 1.02, p = .312, beta = .12. Sobel’s test of mediation (1982) was significant at 2.40, p = .016. In summary, participants in MI-CBT achieved greater worry reductions in CBT compared to those who did not receive pretreatment, in part because they completed more homework as judged by their CBT therapists.
To summarize, our main hypotheses were generally supported through findings that adding MI to CBT, compared to no pretreatment prior to CBT, was associated with significantly greater worry reduction and improved engagement in CBT in terms of increased therapist-rated homework compliance over the course of CBT. Moreover, increased homework compliance in CBT as a function of receiving MI pretreatment fully mediated the impact of treatment group on worry reduction during CBT.
Moderation Effects
Procedures recommended by Baron and Kenny (1986) were used to examine possible moderator effects of individual differences in baseline intrinsic motivation and worry severity. The correlation between motivation and worry severity was −.10 (p = .37), suggesting that these 2 variables assessed different constructs.
Intrinsic motivation
For intrinsic motivation, there appeared to be a stepped relationship such that treatment groups were differentiated in worry reduction at low levels of motivation only. As such, the moderator was dichotomized at the critical step. Baseline scores on the PSWQ did not differ between treatment group within the low motivation (MI-CBT M=69.63, SD=6.59, NPT-CBT M=67.32, SD=8.96), t(30) = 0.78, p = .436 or high motivation (MI-CBT M=66.16, SD=8.82, NPT-CBT M=65.95, SD=7.87), t(42) = 0.08, p = .934, subgroups.
An ANCOVA on post-CBT worry scores, using baseline worry scores as a covariate, revealed a marginally significant interaction between treatment group and motivation level, F(1,71) = 3.15, p = .080. In particular, for individuals with low levels of intrinsic motivation (n=13 MI-CBT, n=19 NPT-CBT) post-CBT worry scores were lower in the MI-CBT group (M=35.08, SD=10.83) compared to the NPT-CBT group (M=47.42, SD=16.05), with an effect size of d=.90. In contrast, post-treatment worry scores for those of high intrinsic motivation (n=25 MI-CBT, n=19 NPT-CBT) were similar whether they received MI-CBT (M=35.92, SD=10.92) or NPT-CBT (M=37.82, SD=13.59), with an effect size of d=.15.
A MANCOVA on other symptom measures (DASS-depression, DASS-anxiety, DASS-stress, MCQ30, SDS, CGI) revealed no significant multivariate effect, F(7,56) = 1.16, p = .337 and no significant univariate treatment group by motivation group effects.
Worry severity
For baseline worry severity, again, the nature of the relationship between treatment group and changes in the principal outcome measure (PSWQ) over the entire treatment period, appeared to be stepped across the levels of the proposed moderator (baseline PSWQ scores). High levels of baseline severity (n=19 MI, n=18 NPT; 49% of the sample) appeared to be associated with substantively more benefit from MI-CBT compared to NPT-CBT. PSWQ scores below the critical step (n=19 MI, n=20 NPT) were associated with equivalent worry reduction across treatment groups. As a result, severity was dichotomized at the critical step into high and moderate severity groups. Means and SDs across time by severity group and treatment group for each moderator analysis involving severity are presented in Table 3.
Table 3.
Means and SDs Across Time by Severity Group and Treatment Group
| PSWQ | Baseline | Post-Treatment | 6-month | 12-month | ||||
|---|---|---|---|---|---|---|---|---|
| High Severity: | M | SD | M | SD | M | SD | M | SD |
| MI-CBT | 74.26 | 3.41 | 33.84 | 12.67 | 43.47 | 17.23 | 36.31 | 14.77 |
| NPT-CBT | 73.89 | 4.24 | 47.83 | 16.28 | 48.56 | 14.85 | 47.67 | 17.72 |
| Moderate Severity: | ||||||||
| MI-CBT | 60.42 | 5.05 | 37.42 | 8.37 | 38.05 | 12.09 | 42.84 | 10.14 |
| NPT-CBT | 60.10 | 4.97 | 37.93 | 13.39 | 38.23 | 14.02 | 36.87 | 13.41 |
| Intrinsic Motivation | ||||||||
| High Severity: | Baseline | After Pretreatment | ||||||
| MI | 18.16 | 6.05 | 20.26 | 5.11 | ||||
| NPT | 17.06 | 6.05 | 17.11 | 5.18 | ||||
| Moderate Severity: | ||||||||
| MI | 19.84 | 4.31 | 18.16 | 4.80 | ||||
| NPT | 18.90 | 4.99 | 18.60 | 3.72 | ||||
| 4 Sessions MI vs CBT | Baseline | Post 4 Sessions of Therapy | ||||||
| High Severity: | M | SD | M | SD | ||||
| MI | 74.26 | 3.41 | 64.11 | 12.60 | ||||
| CBT | 73.89 | 4.24 | 70.50 | 7.32 | ||||
| Moderate Severity: | ||||||||
| MI | 60.42 | 5.05 | 59.68 | 8.24 | ||||
| CBT | 60.10 | 4.97 | 57.55 | 7.59 | ||||
An ANCOVA on post-treatment PSWQ scores, using baseline PSWQ scores as a covariate, revealed a significant interaction between treatment group and severity group, F(1,72) = 4.88, p = .030. In particular, participants with high severity who received MI-CBT obtained significantly lower worry scores post-treatment than did those in the NPT-CBT group (d=.96). For those of moderate severity, post-treatment worry scores were similar across the MI-CBT and the NPT-CBT groups (d=.05).
Moreover, there was a marginally significant trend toward those meeting criteria for recovery or partial recovery with MI alone, to be from the high severity group, X2(1)=3.20, p=.074. Seventy-three percent of those who achieved partial or full recovery with MI alone, were from the high severity group, and 42% (n=8/19) of those of high severity met partial (n=3) or full (n=5) recovery status with MI alone. That is, those of high severity were more likely to respond to 4 sessions of MI alone compared to those of moderate severity.
A MANCOVA on the other symptom measures revealed no significant multivariate effect, F(7,56) = 0.48, p = .846 and no significant univariate treatment group by severity group interactions. Finally, ANCOVA on intrinsic motivation post-pretreatment, with baseline intrinsic motivation as the covariate, revealed a significant interaction between treatment group and severity group, F(1,71) = 6.52, p = .013. In particular, intrinsic motivation scores following the pretreatment period were higher in the MI-CBT high severity group than either the high severity NPT-CBT group or the moderate severity groups (see Table 3). The effect size comparing high severity individuals across treatment groups was d=.61 and was d= −.10 for those of moderate severity. Moreover, when worry reduction over the pretreatment period was used as an additional covariate, this effect remained significant, F(1,69) = 7.15, p = .009, suggesting that improvements in intrinsic motivation over the course of MI for the high severity group were not merely a product of symptom change.
Comparing 4 sessions of MI with 4 sessions of CBT
Given the benefit of adding MI to CBT for individuals of high severity compared to those who received CBT with no pretreatment, we explored the relative impact of 4 sessions of MI with the equivalent number of CBT sessions for these individuals. Previously, we reported that 4 sessions of MI was superior to no treatment for the high severity group. In the present analysis, we asked whether 4 sessions of MI was superior to 4 sessions of CBT for high severity subjects.
An ANCOVA, using PSWQ scores after 4 sessions of MI for the MI-CBT group and after the first 4 sessions of CBT for the NPT-CBT group, with baseline PSWQ scores as the covariate, revealed a significant treatment group by severity group interaction, F(1,71) = 6.01, p = .017. For individuals with high worry severity, 4 sessions of MI resulted in greater worry reduction than 4 sessions of CBT (d=.62). In contrast, a small effect favoring 4 sessions of CBT over 4 sessions of MI was observed for those of moderate worry severity, d=.27 (see Table 3). These findings suggest that given an equivalent number of therapy sessions3, those of high worry severity responded better to MI than to CBT, whereas individuals with moderate worry severity tended to do better with CBT than MI.
Differences between high and moderate severity worriers at baseline
There were no significant pretreatment differences on intrinsic motivation between high and moderate severity worriers. However, high severity worriers had significantly higher DASS scores (M=58.14, SD=25.30) compared to those of moderate severity (M=37.80, SD=18.94), t(74)=3.98, p=.000. Those of high severity also had a higher number of comorbid Axis I clinical diagnoses t(74)=2.85, p=.006 (High Severity M=1.03, SD=1.14, Moderate Severity: M=0.44, SD=0.60), and reported being more disabled by anxiety, t(73)=1.93, p=.057 (High Severity: M=19.11, SD=6.90; Moderate Severity M=16.28, SD=5.75), compared to those of moderate severity.
Follow-up results
Five individuals (2 MI-CBT, 3 NPT-CBT) did not complete the 6-month follow-up assessment and 8 individuals (3 MI-CBT, 5 NPT-CBT) did not complete the 12-month assessment, resulting in 93% and 90% of individuals completing the 6- and 12-month follow-up assessments, respectively.
ANCOVAs on 6- and 12-month follow-up PSWQ scores (using baseline PSWQ scores as the covariate), revealed that the treatment group effect observed post-treatment was no longer evident at follow-up, F(1,68)=0.56, p=.459 and F(1,65)=0.57, p=.453, respectively (see Table 2). Given the particular and specific benefit of adding MI to CBT for the high severity group, these same analyses were conducted adding severity group as an independent variable. Here, no significant interaction was observed on 6 month PSWQ scores, F(1,66)=0.55, p=.461 but a significant interaction between treatment group and severity group was apparent on 12-month post-treatment PSWQ scores, F(1,63)=6.18, p.016 (see Table 3).
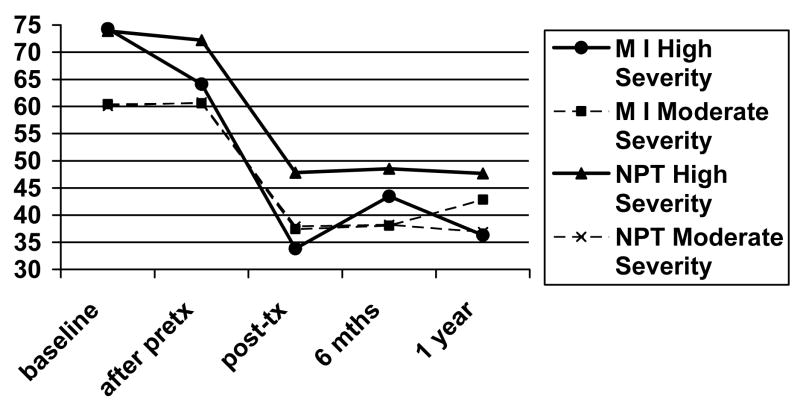
Figure 2 shows the mean PSWQ scores over time as a function of treatment and severity groups. As seen in Figure 2, both moderate severity groups (MI-CBT, NPT-CBT) made considerable gains and maintained these gains over time. The high severity NPT-CBT group made fewer gains than those in the moderate severity group but generally maintained its gains. The high severity MI-CBT group, made the greatest gains during treatment of any subgroup, demonstrated some evidence of relapse at 6 months post-treatment and then recovered some of these additional gains at 12-months post-treatment. Although the high severity MI-CBT did not return to their post-treatment PSWQ scores, the advantage to worry reduction of having received the additional MI pretreatment compared to receiving no pretreatment for individuals of high severity is again apparent at 12-month follow-up. The effect size favoring the MI-CBT group over the CBT alone group when comparing high severity individuals of d=.96 observed immediately post-treatment, drops to d=.32 at 6-months post-treatment and then improves to d=.70 at 12-months post-treatment. Moreover, the moderate severity MI-CBT group tended to have higher worry scores 12-months post treatment than those of moderate severity receiving CBT alone.
Figure 2.
PSWQ scores over time as a function of treatment group and severity group.
Findings for diagnostic status at 12-months post-treatment largely converge with the pattern of findings for the PSWQ. Twelve months post-treatment, 74% of the MI-CBT group no longer met criteria for GAD compared with 61% of the NPT-CBT group. This difference was not statistically significant, X2(1)=1.45, p=.228. Among those of high worry severity, 81% (n=13/16) of those receiving MI-CBT no longer met diagnostic criteria for GAD at 12 months post-treatment, compared with 56% (n=10/18) of those receiving CBT alone (NPT-CBT), X2(1)=2.56, p=.110. While not statistically significant, these findings do suggest an enduring relative advantage of MI-CBT over CBT alone for those of high severity. Again, for those of moderate worry severity, there was no advantage of adding MI to CBT and 68% (n=13/19) and 67% (n=10/15) of these individuals no longer met GAD criteria at the 12-month post-treatment diagnostic interview across the MI-CBT and NPT-CBT groups, respectively.
Discussion
This study provided a preliminary randomized controlled investigation of the potential efficacy of adding an MI pretreatment to CBT in the treatment of GAD. The results suggest the possibility that adding an MI pretreatment to CBT may facilitate reduction in worry – the hallmark symptom of GAD. Participants given MI pretreatment followed by CBT showed significantly greater reductions in worry, which were clinically significant in magnitude, than participants who received CBT alone (i.e., with no pretreatment). The greater gains in worry reduction in the MI augmented CBT group compared to those receiving CBT alone were made during the MI pretreatment period as well as during CBT. Moreover, improved worry in the MI-CBT subjects was mediated by greater therapist-rated homework compliance compared to those receiving CBT alone. These findings are consistent with the results of Westra and Dozois (2006) who found that the addition of an individual MI pretreatment to group CBT for a heterogeneous group of anxiety disorders led to significantly better outcomes than for CBT only. Moreover, findings of increased homework compliance in the MI-CBT group converge with findings from a qualitative study by Kertes, Westra, Angus, and Marcus (in press) of post-CBT client interviews of experiences of CBT in this trial. In particular, using clients of high symptom severity, Kertes et al (in press) found that individuals who received MI pretreatment reported experiencing the CBT therapist as an ‘evocative guide’ and themselves as actively involved in therapy, compared with those not receiving MI prior to CBT who described the therapist as ‘directive’ and their own role as involving more passive compliance.
In terms of symptom change however, our findings of the benefit of adding MI to CBT were restricted to the principal outcome measure of worry. That is, both groups improved significantly on other symptom measures including depression, anxiety, beliefs about worry, disability, and clinician rated severity, with no significant differences between them.
The results consistently suggested that the effects of adding an MI pretreatment to CBT on worry reduction may be specific to individuals with high worry severity at baseline. Stated differently, the overall superior worry reduction of the MI-CBT group in this study was driven by the subgroup (49% of the sample) of high symptom severity subjects. The effect size comparing high worry severity individuals across treatment groups was large, whereas there was virtually no effect of adding MI pretreatment to CBT for those of moderate severity. Moreover, when both high and moderate severity individuals received the MI pretreatment, only those of high severity showed significant increases in intrinsic motivation.
As might be expected receiving some treatment (4 sessions of MI) was more effective for worry reduction than receiving no treatment (4 week wait) over the same period. However, we also wondered whether, for the high severity worriers, MI would be more effective than the same number of sessions of another active treatment - CBT (4 sessions). Here, we found that the high severity group showed significantly more benefit from the equivalent number of sessions of MI than CBT, while the reverse was true for moderate severity subjects who showed more benefit from CBT than MI. Although this comparison is preliminary since the MI and CBT were not delivered at the same time, it does suggest the possibility that given equivalent treatment contact, MI may hold promise in improving treatment response specifically for those with high symptom severity. Conversely, MI may not be indicated for those of moderate severity who responded better to the equivalent number of sessions of CBT and showed better maintenance of gains at 12-month follow-up with CBT alone. This is consistent with findings of Durham et al. (2004) who reported that a small dose of CBT (5 sessions) produced good treatment response among those with GAD of good prognosis, which included having lower symptom severity at baseline.
The possibility that adding MI to CBT may be particularly beneficial for individuals of high symptom severity is consistent with two other MI studies with other problems (e.g., gambling, Hodgins & Diskin, 2008; drinking during pregnancy: Handmaker, Miller, & Manicke, 1999). Moreover, severity of GAD has been identified as an important factor differentiating individuals with the disorder, with higher severity being associated with higher intolerance of uncertainty and more negative problem orientation (Dugas et al., 2007), greater cognitive avoidance (Gosselin et al., 2007), and greater negative beliefs about worry (Ruscio & Borkovec, 2004) than less severe worry.
It may be that high severity worriers may be less motivated to change and more ambivalent or skeptical about change than those of moderate worry severity. Although we found that the high severity group improved in intrinsic motivation if they received MI, they were not lower on intrinsic motivation at baseline initially compared to their high severity no pretreatment counterparts. As such, in part, this may be an issue of developing better measures of ambivalence and intrinsic motivation. Another possibility is that participants with high severity may also have higher levels of interpersonal problems, which leading theorists in the study of GAD have noted are not adequately addressed in existing models of CBT for GAD (Newman et al., 2008). As such, individuals with higher levels of interpersonal problems might preferentially benefit from a treatment such as MI which places heavy emphasis on the therapeutic relationship. In part, this may also explain the significant response to MI alone observed in the present study (since 73% of those who recovered or partially recovered with MI alone were of high severity). If the moderator effect of worry severity is replicated, these are worthwhile questions to address in future research.
Overall group differences in worry reduction at post-treatment were no longer evident at follow-up assessments. This appears to be due to evidence of worry relapse in the high severity group (the group most responsive to the addition of MI pretreatment) at follow-up, especially at 6 months. The high severity MI-CBT group recovered some of their additional gains at 12-month post-treatment follow-up but they did not resume their post-treatment levels of worry. Despite some loss of treatment gains in worry reduction after treatment ended, individuals with high severity were still significantly better off at 12 months after the completion of treatment if they received the additional MI pretreatment than if they received no pretreatment prior to CBT (d=.70).
Given that individuals of high severity are typically less responsive to CBT alone, as observed both in this study and previous studies (Butler, 1993; Durham et al., 2004), future research is indicated to investigate the possibility of augmenting CBT with MI to achieve better recovery rates for this group. Durham et al. (2004) specifically examined those with GAD of poor prognosis on a number of indicators, including high severity, and found that only 56% of these individuals no longer met criteria for the diagnosis post-CBT with a further decline to 40% at 6-months post-CBT. Similarly, in the present study, only 56% of individuals of high severity who received CBT alone (NPT-CBT) no longer met diagnostic criteria for GAD at 12 months post-treatment. However, 81% of those of high severity who received the additional MI pretreatment before receiving CBT no longer met diagnostic criteria for GAD one-year after treatment. Thus, compared to previous studies, the impressive recovery rate of the high severity group who received MI prior to CBT strongly suggests that future research should investigate this effect further. Future studies will also need to pay particular attention to relapse prevention in this subgroup since they may be at greater risk for relapse than those with less severe worry, as indicated both in this study and the Durham et al. (2004) study.
Limitations of the Present Study
There are important plausible alternative explanations for the results observed in the present study which need to be ruled out in future studies. First, subjects in the MI-CBT group received 4 more therapy sessions than did the NPT-CBT group, and were also aware that they received additional treatment whereas subjects in the NPT-CBT group were aware that they did not receive additional treatment. These confounds may have been particularly likely to affect the high worry severity group who may require more treatment given their high levels of severity and/or may be particularly influenced by knowledge of receiving ‘less’ treatment (i.e., having been assigned to the ‘inferior’ treatment group). Moreover, as with nearly all psychotherapy trials, it was impossible to blind therapists to client treatment condition. This raises the possibility that CBT therapists, having knowledge of who received MI, worked harder with these clients in response to experimental demand and provided inflated homework estimates for this group. In addition, although still powerful enough to yield between group differences given the magnitude of the effects, sample sizes for the subgroups in the severity moderator analyses were small. Moreover, even if replicated, the possibility exists that there is nothing unique about MI as a pretreatment and that any other reasonable pretreatment might have been just as effective. In addition, the high rate of refusal of study participation upon phone screen due to difficulties with travel to the study site restricts inferences that can be made regarding the representativeness of the sample to the larger population of individuals with GAD. Finally, the repeated administration of the PSWQ over the course of treatment might have increased the probability of carry-over effects. Importantly however, the ADIS-IV was readministered at 12-month follow-up and these interview-based results were consistent with those obtained on the PSWQ.
Each of the above constraints limits the conclusions that can be drawn from this study. Both research comparing MI to other pretreatments (or equivalent treatment contact groups) and process research is required to examine if changes with MI are theoretically consistent (e.g., changes in motivation) and mediate outcomes. While not definitive, the findings of the present study do support the continued investigation of adding MI to CBT for GAD. Moreover, the present study also informs future investigations in this area by suggesting important moderator effects that should be systematically studied in future research. Such studies are further indicated considering that the effect sizes for the MI augmented group in this study ranged from 1.35 post-treatment to 0.83 one year-post-treatment when benchmarked against worry reduction in 10 previous CBT for GAD studies (see meta-analysis by Covin, Ouimet, Seeds, & Dozois, 20084). As such, these findings strongly argue for further investigation in this area.
Conclusions
This study represents the first controlled outcome trial to examine the potential viability of adding an MI pretreatment to CBT. The results suggest that adding MI to CBT for GAD may hold promise in reducing the hallmark GAD symptom of worry, particularly among those of high severity. While the study has a number of limitations that constrain inferences that can be drawn, the results do suggest that future research, using more powerful and well-controlled designs, should continue to investigate the potential of augmenting CBT with MI for GAD. In particular, the results of the present study suggest the possibility of enhancing outcomes for those of high symptom severity, who are among the most disabled but who have been less responsive to CBT in previous studies (Butler, 1993; Durham et al., 2004). Given the clinical importance of such findings, they should be replicated and extended in future studies of adding MI to CBT for GAD, and possibly other anxiety disorders.
Acknowledgments
We gratefully acknowledge financial support for this project from the National Institute of Mental Health R34-MH072615 and a New Investigator Award from the Canadian Institute of Health Research awarded to the first author.
We wish to thank Paulette Christopher from the University of New Mexico for her training in the use of the Motivational Interviewing Treatment Integrity Code. We also thank the large team at York who worked diligently on this project including Danuta Stala for her outstanding project co-ordination work, our dedicated therapists and ADIS interviewers, and the many adherence coders who worked diligently on this project.
Footnotes
This manual can be obtained from hwestra@yorku.ca.
Means and SDs for calculations were derived from Gillis, Haaga, & Ford (1995) for normals and from Behar, Alcaine, Zuellig & Borkovec (1993) for GAD.
In this comparison, participants received the same number of actual sessions but received double the therapy hours in CBT (8 hours) compared to MI (4 hours) since the CBT sessions were 2 hours and the MI sessions 1 hour in duration.
The SD for previous trials of 8.86 for GAD subjects was used for the previous studies group, as reported in the normative sample estimates of Molina & Borkovec (1994).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, Gøtzsche PC, Lang T for the CONSORT Group. The Revised CONSORT Statement for Reporting Randomized Trials: Explanation and Elaboration. Annals of Internal Medicine. 2001;134:663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10:176–181. [Google Scholar]
- Arkowitz H, Westra HA, Miller WR, Rollnick S. Motivational Interviewing in the Treatment of Psychological Problems. New York: Guilford Press; 2008. [Google Scholar]
- Barlow DH, Allen LB, Basden SL. Psychological treatments for panic disorders, phobias, and generalized anxiety disorder. In: Nathan PE, Gorman Jack M, editors. A guide to treatments that work. 3. New York: Oxford University Press; 2007. pp. 351–394. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical consideration. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Behar E, Alcaine O, Zuellig AR, Borkovec TD. Screening for generalized anxiety disorder using the Penn State Worry Questionnaire: a receiver operating characteristic analysis. Journal of Behavior Therapy and Experimental Psychiatry. 2003;34:25–43. doi: 10.1016/s0005-7916(03)00004-1. [DOI] [PubMed] [Google Scholar]
- Bieling PJ, McCabe RE, Antony MM. Measurement issues in preventing anxiety and depression: Concepts and instruments. In: Dozois DJA, Dobson KS, editors. The Prevention of Anxiety and Depression: Theory, Research and Practice. Washington: American Psychological Association; 2004. pp. 43–71. [Google Scholar]
- Borkovec TD. The nature, functions, and origins of worry. In: Davey GCL, Tallis F, editors. Worrying: Perspectives on theory, assessment, and treatment. New York: Wiley; 1994. pp. 5–34. [Google Scholar]
- Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1993;57:3–8. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Mathews AM. Treatment of nonphobic anxiety disorders: A comparison of nondirective, cognitive, and coping desensitization therapy. Journal of Consulting and Clinical Psychology. 1988;56:877–884. doi: 10.1037//0022-006x.56.6.877. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70:288–298. [PubMed] [Google Scholar]
- Borkovec TD, Roemer L. Perceived functions of worry among generalized anxiety disorder subjects: Distraction from more emotionally distressing topics? Journal of Behavior Therapy and Experimental Psychiatry. 1995;26:25–30. doi: 10.1016/0005-7916(94)00064-s. [DOI] [PubMed] [Google Scholar]
- Brown TA, Antony MM, Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behaviour Research and Therapy. 1992;30:33–37. doi: 10.1016/0005-7967(92)90093-v. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Classification of anxiety and mood disorders. In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic. New York: Guilford Press; 2002. pp. 292–327. [Google Scholar]
- Brown TA, Chorpita BR, Korotitscw W, Barlow DH. Psychometric properties of the depression anxiety stress scales (DASS) in clinical samples. Behaviour Research and Therapy. 1997;35:79–89. doi: 10.1016/s0005-7967(96)00068-x. [DOI] [PubMed] [Google Scholar]
- Brown TA, DiNardo P, Barlow DH. ADIS: Anxiety Disorders Interview Schedule for DSM IV. Colorado: Graywind Publications; 1994. [Google Scholar]
- Bryant MJ, Simons AD, Thase ME. Therapist skill and patient variables in homework compliance: Controlling an uncontrolled variable in cognitive therapy outcome research. Cognitive Therapy and Research. 1999;23:381–399. [Google Scholar]
- Buckner JD, Roth Ledley D, Heimberg RG, Schmidt NB. Treating comorbid social anxiety and alcohol use disorders: Combining motivation enhancement therapy with cognitive behavioral therapy. Clinical Case Studies. doi: 10.1177/1534650107306877. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Butler G. Predicting outcome after treatment for generalized anxiety disorder. Behaviour Research and Therapy. 1993;31:211–213. doi: 10.1016/0005-7967(93)90075-6. [DOI] [PubMed] [Google Scholar]
- Campbell LA, Brown TA. Generalized anxiety disorder. In: Antony MM, Barlow DH, editors. Handbook of Assessment and Treatment Planning for Psychological Disorders. New York: Guilford; 2002. pp. 147–181. [Google Scholar]
- Cartwright-Hatton S, Wells A. Beliefs about worry and intrusions: The Metacognitions Questionnaire. Journal of Anxiety Disorders. 1997;11:279–315. doi: 10.1016/s0887-6185(97)00011-x. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Covin R, Ouimet AJ, Seeds PM, Dozois DJA. A meta-analysis of CBT for pathological worry among clients with GAD. Journal of Anxiety Disorders. 2008;22:108–116. doi: 10.1016/j.janxdis.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. New York: Plenum; 1985. [Google Scholar]
- Dugas MJ, Savard P, Gaudet A, Turcotte J, Laugesen N, Robichaud M, et al. Can the components of a cognitive model predict the severity of generalized anxiety disorder? Behavior Therapy. 2007;38:169–178. doi: 10.1016/j.beth.2006.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durham RC, Fisher PL, Dow MGT, Sharp D, Power KG, Swan JS, et al. Cognitive behavior therapy for good and poor prognosis generalized anxiety disorder: A clinical effectiveness study. Clinical Psychology & Psychotherapy. 2004;11:145–157. [Google Scholar]
- Freeston MH, Rheaume J, Letarte H, Dugas MJ, Ladouceur R. Why do people worry? Personality and Individual Differences. 1994;17:791–802. [Google Scholar]
- Gillis MM, Haaga DAK, Ford GT. Normative values for the Beck Anxiety Inventory, Fear Questionnaire, Penn State Worry Questionnaire, and Social Phobia and Anxiety Inventory. Psychological Assessment. 1995;7:450–455. [Google Scholar]
- Gosselin P, Langlois F, Freeston MH, Ladouceur R, Laberge M, Lemay D. Cognitive variables related to worry among adolescents: Avoidance strategies and faulty beliefs about worry. Behaviour Research and Therapy. 2007;45:225–233. doi: 10.1016/j.brat.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Guy W. ECDEU Assessment for psychopharmacology, Revised edition. Rockville, MD: NIMH Publication; 1976. [Google Scholar]
- Handmaker NS, Miller WR, Manicke M. Findings of a pilot study of motivational interviewing with pregnant drinkers. Journal of Studies on Alcohol. 1999;60:285–287. doi: 10.15288/jsa.1999.60.285. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Liebowitz MR, Hope D, Schneier FR, Holt CS, Welkowitz L, Juster HR, Campeas R, Bruch MA, Cloitre M, Fallen B, Klein DF. Cognitive behavioral group therapy versus phenelzine in social phobia: 12-week outcome. Archives of General Psychiatry. 1998;55:1133–1141. doi: 10.1001/archpsyc.55.12.1133. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RMA. Placebo response in the treatment of panic disorder. Bulletin of the Menninger Clinic. 1996;60:A76–A86. [PubMed] [Google Scholar]
- Hodgins D, Diskin KM. Motivational interviewing in the treatment of problem and pathological gambling. In: Arkowitz H, Westra HA, Miller WR, Rollnick S, editors. Motivational Interviewing in the Treatment of Psychological Problems. New York: Guilford Press; 2008. pp. 225–248. [Google Scholar]
- Hunot V, Churchill R, Teixeira V, Silva de Lima M. Psychological therapies for generalized anxiety disorder (review) Cochrane Libraries. 2007:4. doi: 10.1002/14651858.CD001848.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Katon W, Von Korff M, Lin E, Lipscomb R, Russo J, Wagner E, Polk E. Distressed high utilizers of medical care: DSM-III-R diagnoses and treatment needs. General Hospital Psychiatry. 1990;12:355–362. doi: 10.1016/0163-8343(90)90002-t. [DOI] [PubMed] [Google Scholar]
- Kertes A, Westra HA, Angus L, Marcus M. The impact of motivational interviewing on client experiences of cognitive behavioural therapy for generalized anxiety disorder. Cognitive and Behavioral Practice in press. [Google Scholar]
- Ladouceur R, Dugas MJ, Freeston MH, Leger E, Gagnon F, Thibodeau N. Efficacy of a cognitive-behavioral treatment for generalized anxiety disorder: Evaluation in a controlled clinical trial. Journal of Consulting and Clinical Psychology. 2000;68:957–964. [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. American Journal of Psychiatry. 2000;157:669–682. doi: 10.1176/appi.ajp.157.5.669. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York: Guilford; 2002. [Google Scholar]
- Molina S, Borkovec TD. The Penn State Worry Questionnaire: Psychometric properties and associated characteristics. In: Davey GCL, Tallis F, editors. Worrying: Perspectives on theory, assessment and treatment. Oxford: Wiley; 1994. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Nordberg SS. An open trial of integrative therapy for generalized anxiety disorder. Psychotherapy Theory, Research, Practice, Training. 2008;45:135–147. doi: 10.1037/0033-3204.45.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelletier LG, Tuson KM, Haddad NK. Client Motivation for Therapy Scale: A measure of intrinsic motivation, extrinsic motivation, and amotivation for therapy. Journal of Personality Assessment. 1997;68:414–435. doi: 10.1207/s15327752jpa6802_11. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediational models. Behavior Research Methods, Instruments, and Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Primakoff L, Epstein N, Covi L. Homework compliance: An uncontrolled variable in cognitive therapy outcome research. New York: Springer; 1989. [Google Scholar]
- Rogers CR. Client-centered therapy. Oxford, UK: Houghton Mifflin; 1951. [Google Scholar]
- Ruscio AM, Borkovec TD. Experience and appraisal of worry among high worriers with and without generalized anxiety disorder. Behaviour Research and Therapy. 2004;42:1469–1482. doi: 10.1016/j.brat.2003.10.007. [DOI] [PubMed] [Google Scholar]
- Shaw BF, Elkin I, Yamaguchi J, Olmsted M, Vallis TM, Dobson KS, Lowery A, Sotsky SM, Watkins JT, Imber SD. Therapist competence ratings in relation to clinical outcome in cognitive therapy of depression. Journal of Consulting and Clinical Psychology. 1999;67:837–846. doi: 10.1037//0022-006x.67.6.837. [DOI] [PubMed] [Google Scholar]
- Sheehan DV. The Anxiety Disease. New York: Scribner; 1983. [Google Scholar]
- Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. International Journal of Psychopharmacology. 1996;11:89–95. doi: 10.1097/00004850-199606003-00015. [DOI] [PubMed] [Google Scholar]
- Simpson HB, Zuckoff A, Page JR, Franklin ME, Foa EB. Adding motivational interviewing to exposure and ritual prevention for obsessive compulsive disorder: An open trial. Cognitive Behavioural Therapy. 2008;37:38–49. doi: 10.1080/16506070701743252. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptomatic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982;13:290–312. [Google Scholar]
- Taft CT, Murphy CM, King DW, Musser PH, DeDeyn JM. Process and treatment adherence factors in group cognitive-behavioral therapy for partner violent men. Journal of Consulting and Clinical Psychology. 2003;71:812–820. doi: 10.1037/0022-006x.71.4.812. [DOI] [PubMed] [Google Scholar]
- Wells A, Cartwright-Hatton S. A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy. 2004;42:385–396. doi: 10.1016/S0005-7967(03)00147-5. [DOI] [PubMed] [Google Scholar]
- Wells A, King P. Metacognitive therapy for generalized anxiety disorder: An open trial. Journal of Behavior Therapy and Experimental Psychiatry. 2006;37:206–212. doi: 10.1016/j.jbtep.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Westra HA. Managing resistance in cognitive behavioral therapy: The application of motivational interviewing in mixed anxiety and depression. Cognitive Behaviour Therapy. 2004;33:161–175. doi: 10.1080/16506070410026426. [DOI] [PubMed] [Google Scholar]
- Westra HA, Arkowitz H. Combining motivational interviewing and cognitive behavioral therapy to increase treatment efficacy for generalized anxiety disorder. In: Sookman D, Leahy R, editors. Resolving treatment impasses with resistant anxiety disorders. Routledge: in press. [Google Scholar]
- Westra HA, Dozois DJA. Motivational interviewing adapted for anxiety. 2003. Unpublished treatment manual. [Google Scholar]
- Westra HA, Dozois DJA. Preparing clients for cognitive behavioral therapy: A randomized pilot study of motivational interviewing for anxiety. Cognitive Therapy and Research. 2006;30:481–498. [Google Scholar]
- Westra HA, Dozois DJA. Integrating motivational interviewing in the treatment of anxiety. In: Arkowitz H, Westra HA, Miller WR, Rollnick S, editors. Motivational interviewing in the treatment of psychological problems. Guilford Press; 2008. pp. 26–56. [Google Scholar]
- Westra HA, Dozois DJA, Marcus M. Expectancy, homework compliance, and initial change in cognitive-behavioral therapy for anxiety. Journal of Consulting and Clinical Psychology. 2007;75:363–373. doi: 10.1037/0022-006X.75.3.363. [DOI] [PubMed] [Google Scholar]
- Young J, Beck AT. Cognitive therapy scale rating Manual. Philadelphia: University of Pennsylvania; 1980. Unpublished manuscript. [Google Scholar]
- Zaider TI, Heimberg RG, Fresco DM, Schneier FR, Liebowitz MR. Evaluation of the clinical global impression scale among individuals with social anxiety disorder. Psychological Medicine. 2003;33:611–622. doi: 10.1017/s0033291703007414. [DOI] [PubMed] [Google Scholar]