Abstract
Nursing homes serve many severely ill poor people, including large numbers of racial/ethnic minority residents. Previous research indicates that blacks tend to receive care from lower quality nursing homes (Grabowski, 2004). Using the Institute of Medicine (IOM) definition of racial-ethnic disparities, this study decomposes nursing home disparities into within and across facility components. Using detailed person-level nursing home data, we find meaningful black-white disparities for one of the four risk-adjusted quality measures, with both within and across nursing home components of the disparity. The IOM approach, which recognizes mediation through payer status and education, has a small effect on measured disparities in this setting. Although we did not find disparities across the majority of quality measures and alternate disparity definitions, this approach can be applied to other health care services in an effort to disentangle the role of across and within facility variation and the role of potential mediators on racial/ethnic disparities.
Introduction
A great deal of recent policy interest focuses on racial and ethnic disparities in health care settings (Institute of Medicine, 2003). Nursing home quality has been a serious concern for several decades and there is a consensus that nursing home disparities exist between black and white residents (Konetzka & Werner, 2008). However, existing nursing home research generally considers disparities without recognizing the role of mediating factors such as socioeconomic status (SES). The contribution of within and across facility variation to disparities is also critical to understand for directing policy, and these two sources of disparities have not been emphasized in research to date.
As in much of the rest of health services research, nursing home regression-based disparities research focuses on estimated coefficients of race/ethnicity variables without relating these coefficients to any explicit definition of a disparity. The Institute of Medicine (IOM) (2003) defines a disparity as a difference in treatment provided to members of different racial or ethnic groups not justified by the underlying health conditions or treatment preferences of the patient.1 This definition requires modification of typical regression methodologies for the empirical assessment of disparities, including in particular a different interpretation of SES differences associated with race. Because whites and minorities differ markedly in income and other mediators, SES-related sources of racial/ethnic disparities may be missed in the traditional approach that controls for these factors.
Recent disparities research has emphasized that health care disparities should be decomposed into their proximate causes with respect to “across facility” variation (i.e., certain patients are admitted to facilities with poorer care practices) and “within facility” variation (i.e., certain patients are treated differently within a facility) (Chandra & Skinner, 2003). Both sources of variation can lead to poorer outcomes for certain payer groups or minority populations, but the difference lies in the policy implications. In the case of across facility disparities, policymakers may wish to consider initiatives that improve the patient's choice set, address broader geographic disparities in resources, and guard against discriminatory admission practices. Within facility variation involves the internal workings of specific health care facilities, and bias by the provider or poor information about health needs of the residents may underlie such disparities. If discriminatory behaviors on the part of providers are the cause of racial or ethnic disparities for example, policymakers may wish to provide further oversight of care practices in an effort to ensure more uniform quality.
Drawing on the literature on disparities research more broadly, this paper incorporates several empirical perspectives into the assessment of black-white nursing home disparities. First, following the definition of disparities proposed by the IOM (2003), we recognize disparities mediated through socioeconomic status indicators of residents (specifically, in our data, payer status and education). Second, we decompose disparities into within and across nursing home components, recognizing that part of the disparity problem is that minority populations are more frequently served by lower quality providers. Finally, we specify and estimate separate models by race allowing for differences in race effects for all covariates. This most general specification raises some new issues in assessment of disparities that have been faced elsewhere in labor economics, but not so far as we know in disparities research. In particular, we propose an approach to “adjust for” differences due to health status to implement the IOM definition when the effect of health status may differ for black and white nursing home residents. Moreover, we employ risk-adjusted individual-level processes of care. Specifically, we examine the use of physical restraints, catheters, anti-psychotics and feeding tubes, all of which, as we discuss later, are subject to “overuse” and can serve as negative indicators of quality of care.
We have available a census of nursing home residents across seven states, tracked quarterly between the fourth quarter of 1998 and the fourth quarter of 2002. We have data on more than 1.6 million person-quarters on residents from more than 1,500 nursing homes. We employ simple linear models to estimate the effects of interest.
Quality and Disparities in Nursing Home Care
The consensus from the existing literature is that minority elders do not receive nursing home care of comparable quality to whites (Fennel et al., 2000; Konetzka & Werner, 2008). For example, blacks were admitted to nursing homes that exceeded the mean state number of reported deficiencies by 1.32 in a study using the Medical Expenditure Panel Study (Grabowski, 2004). Blacks had a 63% greater probability of being untreated for pain relative to whites within a study of elderly cancer patients (Bernabei et al., 1999). Additionally, blacks and Hispanics were less likely to have advance care plan documents such as living wills in a nationally representative sample of nursing home residents (Degenholtz et al., 2002). Finally, blacks were concentrated in facilities with lower ratings of cleanliness, or maintenance, and lighting in a study of nearly 250 nursing homes and residential care or assisted living facilities (Howard et al., 2002). However, it is important to note that the majority of the existing studies focus exclusively on across facility variation, and they do not attempt to decompose disparities into their within and across facility components.
Measuring and Decomposing the Sources of Disparities
In studies using secondary survey data, the health services research literature employs any of three definitions of disparity: 1) the unadjusted difference between blacks and whites (to use these groups as an example), 2) differences adjusted for all available covariates, or 3) all differences except those due to health status or preferences (Cook et al., forthcoming)2. In the course of this study, we will estimate disparities according to all three of these measures, but emphasize the third definition—the one proposed by the IOM (2003). We stress the IOM definition because it isolates what the IOM argues are the unfair parts of differences. Definition 1 is not necessarily unfair: if, for example, differences are due to health status—blacks tend to be younger and therefore healthier than whites in nursing homes—or preferences about care, then these differences should not be part of disparities. Differences due to the independent effect of race (Definition 2) are part but not all of what is unfair between groups. If blacks are more likely to be poor and/or more likely to live in areas with lower access and lower quality of care, differences mediated through income and geography should be considered unjust disparities.
Given that we have no measures of preferences in our nursing home data, we cannot adjust for any preference contribution to differences. However, because the overuse of physical restraints, catheters, anti-psychotics and feeding tubes are processes associated with worse care outcomes, “preferences” seem an unlikely explanation for differences in the nursing home quality measures studied here.
The broader health care literature has found that geography plays a large role in disparities (Baicker et al., 2004). Location contributes to disparities if minorities are more likely to live in areas in which care quality is poor. This is particularly relevant for nursing homes in the context of the finding that the nursing home sector is more segregated than geographically-similar hospitals or neighborhoods (Smith, 1993; Smith et al., 2007). Mor and colleagues (2004) found that nursing homes located in the poorest counties have a greater proportion of black and Medicaid residents, as well as fewer resources. These facilities have more health-related regulatory deficiencies and are more likely to be terminated from the Medicare and Medicaid programs.
Our paper contains three sets of analyses explained next. We discuss these in the context of the linear model we apply in this paper. Given the size of our dataset, least squares models estimations of linear probability regression models are presented. Although this approach does not recognize the binary nature of the quality measures, as discussed below, it does facilitate the tractable estimation of these models, which are based on a large number of observations and an expansive set of regression controls. Using a sub-sample of the data, however, the linear probability estimates were robust to those obtained using a logit model.
Three Measures of Disparities in a Basic Linear Model
The three measures of disparities noted above can be operationalized in the context of an empirical model determining the outcome variable, an indicator of quality of care. Our base model is the linear (1):
| (1) |
where
y is a (0,1) outcome variable
B is a (0,1) variable indicating black race
HS is a set of health status measures
SES is a set of measures of socioeconomic status
For purposes of discussion, we refer to the three measures of disparities as Differences, Coefficient, and Mediated, respectively. Estimating Differences, of course, does not require modeling and can be based simply on differences in means. We need (1) to estimate the other two measures:
| (2) |
Bars over variable names indicate mean values and the subscript indicates group. Thus, is the mean value of the outcome variable for blacks and is the mean value for whites. The Difference estimate is straightforward. The Coefficient estimate addresses how much more or less a black nursing home resident receives relative to a white resident, adjusted for all measured SES and HS factors. The Mediated estimate can be operationalized in one of two equivalent ways: as the sum of the race coefficient plus the effect of race-based differences in SES, or alternatively, as the total difference less the difference due to health status differences between the groups. The IOM definition is phrased as the right-hand side of the equality. In our analysis below, we will use both of these equivalent measures depending on which is more illuminating and convenient.
Methods for estimating each of these three measures of disparities have been developed for non-linear models (see Cook et al. (forthcoming), which relates these to methods in linear models such as those we use here). Linear models are much more straightforward to use, however, particularly when issues of decomposition are addressed. Decomposition methods have been applied to linear models for many years (Oaxaca, 1973; Blinder, 1973)
Within and Across Nursing Home Sources of Disparities
A second analysis decomposes the disparities measure (1) into within and across facility components by adding fixed effects for the approximately 1,537 nursing homes in the data by estimating (3):
| (3) |
When nursing home fixed effects are included in the linear model, estimated coefficients on all covariates capture only the average within nursing home effects on quality. For example, we could find a negative main effect (coefficient a1) of race in (1), which could be due to blacks being served in nursing homes with low average quality after adjusting for other factors. If, within a nursing home, blacks and whites might get similar quality, but blacks are at a disadvantage because of where they reside, by including nursing home fixed effects, the main effect of race should fall to zero in (3). We would then conclude that according to the Coefficient measure, all of disparities are across nursing homes, not within nursing homes. (Note that because disparities are across nursing homes does not imply there are no disparities, but rather that they are associated with which nursing homes are used by different races.) Linearity allows us to estimate the contribution of within and across nursing home disparities in a straightforward fashion:
| (2') |
Disparities in a Fully Interacted Linear Model
The most general specification of race in a model of quality is to estimate separate models for blacks and whites, or, equivalently, to estimate one model interacting black race with all health status and SES covariates. We estimate such a model here:
| (4) |
What are disparities by the various definitions within this fully interactive model? The generalization of the Coefficient estimate is what has been called the Residual Direct Effect (RDE) of a variable (Graubard & Korn, 1999). In this case the RDE captures the full effect of the black race indicator. We compute disparities based on the RDE of race as follows. Consider all black residents, whose sample mean has a value of a quality indicator equal to . We can then use (4) to estimate their quality of care if they had been white. In other words, given values for HS and SES for the black residents, we fit the values of quality using the white coefficients by substituting B=0. In a linear model, this can be done with the white coefficients and and to predict the quality blacks would have received if they were white. The disparity is then the difference between this estimate and the actual care received, shown in model (5) below. This is analogous to the coefficient of black race in a non-interacted model.
| (5) |
Next consider the disparities measure including mediation, as proposed by the IOM. Model (4) is equivalent to separate models for blacks and whites. In labor economics, Blinder (1973) and Oaxaca (1973) initiated a line of research that decomposes the factors accounting for wage differences between groups into differences in the means of factors contributing to wages (such as education) and differences in the contribution of these factors to wages for each group. Kirby and colleagues (2006) use Blinder-Oaxaca methods in the context of racial-ethnic disparities. They assess how much of the difference in health care use between whites and members of racial and ethnic minorities can be attributed to differences in means of factors affecting use, such as insurance, language, sociodemographics, health system capacity, and others. They do not, however, distinguish SES and health status factors as we do here in the application of the IOM approach.
As far as we know, the IOM definition has not been applied in a model in which there are separate coefficients estimated for health status and SES variables. The approach we propose uses whites as the baseline and then adjusts for health status using the white coefficients. In other words:
| (2") |
This can also be readily implemented in a linear model using mean substitution methods.3
Data
Our data are a census of all nursing home residents from seven states obtained from the Minimum Data Set (MDS) for nursing homes. Based on a federal requirement, the MDS instrument collects over 350 discrete data elements including socio-demographic information, numerous clinical items ranging from degree of functional dependence to cognitive functioning, and include a checklist for staff to indicate the presence of the most common geriatric diagnoses (Morris et al., 1994). Typically, the MDS form is filled out a by a registered nurse (RN) working at the facility. Assessments are performed on admission, upon significant change, and at least quarterly, so that there is a panel of assessments for the same individual over time. When there were multiple assessments within a quarter, we used the assessment closest to the mid-point of the quarter.
We have access to the MDS beginning in the fourth quarter of 1998 through the fourth quarter of 2002 (see Table 1 for descriptive statistics). As such, our data are a combination of existing residents (those admitted prior to the fourth quarter of 1998) and new admissions (those admitted in the fourth quarter of 1998 or later).
Table 1.
Descriptive Statistics by Race
| Blacks N=146,891 (9.1%) | Whites N=1,458,823 (90.9%) | Total N=1,605,714 (100%) | |
|---|---|---|---|
| Quality Indicators | |||
| Physical restraints | 0.098 | 0.088 | 0.089 |
| Catheters | 0.086 | 0.075 | 0.076 |
| Anti-psychotics | 0.199 | 0.193 | 0.193 |
| Feeding tube | 0.159 | 0.057 | 0.066 |
| Demographics | |||
| Age | 75.615 | 81.063 | 80.563 |
| Female | 0.649 | 0.732 | 0.724 |
| Married | 0.148 | 0.195 | 0.191 |
| Never married | 0.181 | 0.124 | 0.129 |
| Widowed | 0.493 | 0.582 | 0.574 |
| Divorced/separated | 0.178 | 0.098 | 0.106 |
| Socioeconomic Status | |||
| Medicaid | 0.858 | 0.632 | 0.653 |
| Private payer | 0.111 | 0.340 | 0.319 |
| Other payer | 0.025 | 0.038 | 0.037 |
| Less than high school | 0.278 | 0.166 | 0.176 |
| High school | 0.141 | 0.170 | 0.168 |
| Some college | 0.047 | 0.065 | 0.063 |
| College or greater | 0.018 | 0.035 | 0.033 |
| Education missing | 0.516 | 0.564 | 0.560 |
| Health Status | |||
| Length of stay (days) | 967.318 | 928.958 | 932.285 |
| ADL score (0–24) | 14.362 | 14.018 | 14.048 |
| CPS Score (0–6) | 3.080 | 2.898 | 2.915 |
Notes: ADL = activities of daily living; CPS = cognitive performance score
The analysis was restricted to seven states because accurate payer source information was not available for other states. Payer source on admission was nearly always recorded on the MDS form, but in many instances, the payer source field was not updated in subsequent MDS assessments. Thus, we were not able to obtain accurate payer source information over time for the majority of states.
Our primary variable of interest is the race of the nursing home resident. The race/ethnicity field on the MDS form has five mutually exclusive categories: 1) American Indian/Alaskan Native, 2) Asian/Pacific Islander, 3) black, not of Hispanic origin, 4) Hispanic, and 5) white, not of Hispanic origin. For the purposes of our analyses, we exclude categories 1, 2 and 4 and focus on black-white comparisons.
Payer status is coded on each quarterly MDS assessment based on ten categories measuring nursing home payment via (i) a Medicaid per diem, (ii) Medicare per diem, (iii) Medicare ancillary part A, (iv) Medicare ancillary part B, (v) CHAMPUS per diem, (vi) VA per diem, (vii) self or family pays full per diem, (viii) Medicaid resident liability or Medicare co-payment, (ix) private insurance per diem (including co-payment), and (x) other per diem. Importantly, these categories are not mutually exclusive. For example, in order to qualify for the Medicaid per diem payment (category i), some individuals face a co-payment (category viii) for any income they have above the state Medicaid income threshold. In an effort to create three payment categories, we used a series of decision rules in placing residents into the Medicaid, private-pay, and other payer groups. First, because we are interested in the primary payer within this study, we did not use ancillary Medicare payments (categories iii and iv) in the assignment to payer groups. Second, because we are interested in chronic (and not rehabilitative) nursing home care, we excluded those Medicare assessments from the analysis. That is, any assessment coded in category (ii) was dropped from our dataset. Third, any individual in category (vii) or category (ix) was considered private-pay. Fourth, we categorized all individuals from group (i) as Medicaid, regardless of whether they faced some co-payment (viii). Finally, we created an other payer group for individuals in the Civilian Health and Medical Program of the Uniformed Services (CHAMPUS) (category v), Veterans Administration (VA) (category vi) and other (category x).
There is no single preferred measure of nursing home quality in the MDS data, so we have formed 4 process-based indicators of quality based on the available information (U.S. General Accounting Office, 2002). The process-based measures are physical restraints, in-dwelling catheters, feeding tubes and anti-psychotics. Immobility resulting from the use of physical restraints may increase the risk of pressure ulcers, depression, mental and physical deterioration, and mortality (Zinn, 1993). Urethral catheterization places the resident at greater risk for urinary tract infection, and other long-term complications including bladder and renal stones, abscesses, and renal failure. Feeding tubes can result in complications including self-extubation, infections, aspiration, unintended misplacement of the tube, and pain. Overuse of anti-psychotics may result in mental and physical deterioration (Harrington et al., 1992).
A number of patient-level covariates were available from the MDS. In order to capture the need for services, an Activities of Daily Living (ADL) score was created for each resident assessment. The ADL score is based on the individual's need for help with bathing, bed mobility, dressing, eating, toileting, and transferring. For each of these six areas, the individual is scored as a zero (independent), one (supervised), two (limited assistance), three (extensive assistance) or four (total dependence). Thus, the total ADL score ranges between zero and twenty-four. For the analyses, we included 24 dummy variables in our regressions. We also included dummy variables for the Cognitive Performance Scale (CPS), which ranges from zero to six in value (Morris et al., 1994). We used a dummy variable for each category to avoid assumptions about the marginal effect of these scores. These variables capturing health status are important in determining the likelihood of our four outcome measures. The marginal effect of a change in the ADL, for example, is much greater in the higher (more severe) ranges of this variable. The large number of observations in the data gave us the scope to fit the effect of health status without functional form assumptions.
We also include a set of dummy variables measuring length-of-stay. Specifically, we created a dummy variable to approximate length of stay for each quarter up through 10 years in the nursing home. The final dummy variable measures length of stay greater than 10 years. Thus, we have 40 dummy variables to model length of stay. Finally, we also include age, gender, education, and marital status. We regard education and payer to be SES variables, and all other variables with the exception of race to be indicators of HS. Importantly, because there a large number of observations with missing information on education, we include a dummy variable for “education missing” allowing us to keep these observations in our multivariate models.
Results
Table 1 contains descriptive results on our quality measures as well as demographic, socioeconomic and health factors potentially affecting these measures. In general, blacks fare worse on the quality measures, experiencing more physical restraints, catheterizations, more anti-psychotic medication, and, in the largest quantitative difference, much more frequent use of feeding tubes. All of these differences are statistically significant within our very large sample size. The descriptive results from Table 1 will be used to construct a first measure of unfair differences by race.
The demographic and socioeconomic status characteristics also differ between the races. Blacks are younger, more likely to be male, and less likely to be currently or previously married. Blacks are more likely to be currently on Medicaid and to be in the lower educational groups. Importantly, there are a large number of observations with missing information on education—for both blacks and whites. However, blacks are less likely to have missing education information. The length of time in the nursing home differs little between the races. Blacks have slightly higher ADL and CPS scores, indicating they are both more physically and cognitively disabled (despite being younger on average).
Table 2 displays results from a series of regressions based on specifications (1) and (3) above. Extensive demographic and health status measures are included in the models, but we report only those coefficients pertinent to our disparity calculations: the estimate of the race effect and the SES variables through which racial disparities might be mediated. There are two models for each quality indicator. Odd number models do not include nursing home fixed effects, while the even ones do; otherwise, the models are identical.
Table 2.
Regression Results from Basic Specification
| Physical Restraints | Catheters | Anti-psychotics | Feeding Tubes | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Variable | ||||||||
| Black | −.00232** | −.0190** | −.00669** | −.00586** | −.00670** | −.03279** | .06211** | .03712** |
| Private Pay | −.00104* | 0.00325** | .00267** | .00312** | −.01504** | −.00836** | −.00082* | .00033 |
| Other Payer | −.0196** | −.00161 | .01190** | .02736** | .00721** | .00625* | −.01885** | −.00383** |
| High School | −.00946** | −.00493** | .00466** | .00153* | −.01265** | −.00618** | −.00135* | −.00061 |
| Some College | −.00900** | −.00293** | .00893** | .00644** | −.02160** | −.01199** | −.00414** | −.00012 |
| College | −.00753** | −.00093 | −.00028 | .00002 | −.02016** | −.00981** | −.00347** | .00067 |
| Education Missing | −.00138* | .00340** | −.01402** | −.01561** | −.01864** | −.01047** | −.00435** | −.00076 |
| Home F.E. | No | Yes | No | Yes | No | Yes | No | Yes |
| N | 1,545,356 | 1,545,356 | 1,545,372 | 1,545,372 | 882,505 | 882,505 | 1,545,369 | 1,545,369 |
| Adjusted R-squared | .103 | 0.1559 | 0.0757 | 0.0963 | 0.0559 | 0.0836 | 0.1957 | 0.2202 |
Models also include age, gender, indications for length-of-stay by quarter, marital status, dummy variables for limitations in activities of daily living, dummy variables for cognitive performance score, and time indicated by quarters.
= statistically significant at 5% level;
= statistically significant at 1% level.
Recall that we will use the odd-numbered models to compute two measures of disparities, one based on the race coefficient and a second one adding payer and educational status mediated effects of race. Because “more is worse” for all of our quality indicators, a positive coefficient on the race variable is consistent with disparities. Thus, the small, negative coefficients on race in models 1, 3 and 5 do not indicate disparities. For example, the estimated race effect of −.00232 for Restraint use in Model 1 means that blacks are 0.232 percentage points less likely to have restraints applied adjusting for all SES and health status variables in the model. The only quality indicator with meaningful disparities as measured by the estimated race coefficient is feeding tube use where blacks are 6.2 percentage points more likely to have feeding tubes after adjusting for all other variables. This is somewhat less than the 10.2 percentage point unadjusted mean difference in feeding tube use from Table 1.
The results in Table 2 are used in the calculation of disparities, allowing for SES mediation as recommended by the IOM. The specific variables used for mediation are the payer status and education variables listed in the table. All are indicator variables. For example, private-pay status is a binary measure (0,1) of whether a resident paid out-of-pocket or used insurance during that quarter. Medicaid is the omitted category and we expect both private-pay and the less frequently observed other payer to be associated with higher quality because of the generally higher prices nursing homes are paid from these sources. We see exactly this relationship in the case of physical restraint use where both variables have a negative coefficient.
The mediation analysis works as follows: the estimated effect of private pay is −.00104, suggesting there is a small (0.1 percentage point) decrease in the likelihood of restraint use for a resident with private sources of payment compared to Medicaid. How much does this contribute to disparities? From Table 1, we know that 34.0% of whites pay privately, but only 11.1% of blacks do. Thus, the effect of private payment on disparities is the black-white disadvantage in this favorable variable (.111–.340) times the effect of the variable (−.001). This product is positive, meaning it does contribute to disparities, but the magnitude, in this case, is small at +.02 percent. All of the indicator variables in Table 2 are expected to be favorable in terms of an impact on quality in relation to the omitted categories, Medicaid in the case of the payer variable, and “not completing high school” in relation to the education variables. The negative sign on all of these variables in Model 1 is consistent with this expectation. The negative sign pattern holds for physical restraints, antipsychotics and feeding tubes, but not so clearly for catheter use.
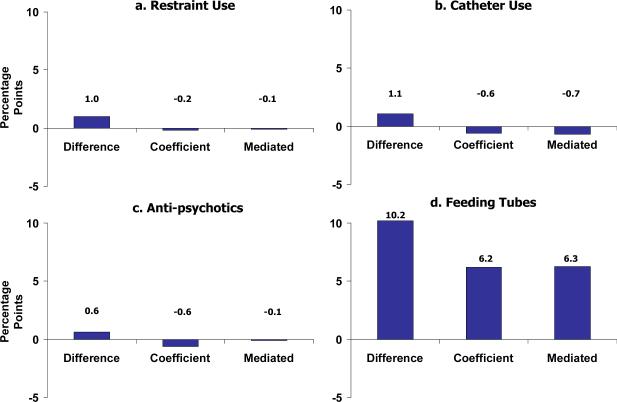
Blacks have a less favorable payer and education profile than whites; therefore, because the black-white difference for these variables is always negative, a negative sign on the variable indicates that mediation contributes to disparities. Thus, in general, with the mainly negative coefficients on these variables in Table 2, the recognition of mediation will increase measured disparities. The calculation of the mediation impact of disparities is straightforward following from formula (2) above. The magnitude of these increments to the disparity measures is depicted in Figures 1a–1d, along with the mean differences from Table 1.
Figure 1.
Black-White Disparities in the Quality of Nursing Home Care
The mean differences for all four measures were positive, consistent with black-white disparities, but were small in all cases except for feeding tube use. The basic finding with respect to physical restraints, catheters and anti-psychotics is that after adjustment for health status measures, there are no black-white disparities when measured either by the coefficient on black race or when allowing for mediation through SES variables. For these three measures, the race coefficient is negative and therefore not consistent with disparities. Mediation makes the disparity measure slightly less negative in the case of physical restraints and anti-psychotics, but not positive. Mediation actually makes the disparities estimate slightly more negative for catheter use.
The largest mean difference in Table 1 is for feeding tube use: 15.9% for blacks and 5.7% for whites. Adjustment for health status and SES reduces the black coefficient to a 6.2 percentage point difference, but this is still quite large in relation to the mean for whites, suggesting a rough doubling of the risk of feeding tube use. All of the estimated coefficients in Model 7 are negative, indicating that there are also some disparities mediated through payer and educational status. As Figure 1d indicates, however, the magnitude of these measured mediators is small, increasing estimated disparities by only about 1 percentage point.
Results reported in Table 2 can also be used to attribute disparities to within facility versus across facility racial differences. Because we find no disparities in the first three measures, the issue of decomposition is not interesting for these. In the case of feeding tubes, inclusion of nursing home fixed effects reduces the race coefficient from .062 to .037. The .037 is an estimate of the average “within nursing home” race effect adjusting for all other variables. Thus, by our accounting, 60% (.37/.62) of the coefficient-based disparities in feeding tube use are within nursing home disparities, and the balance is across nursing home disparities. Mediation has essentially no effect on the within nursing home estimate of disparities.
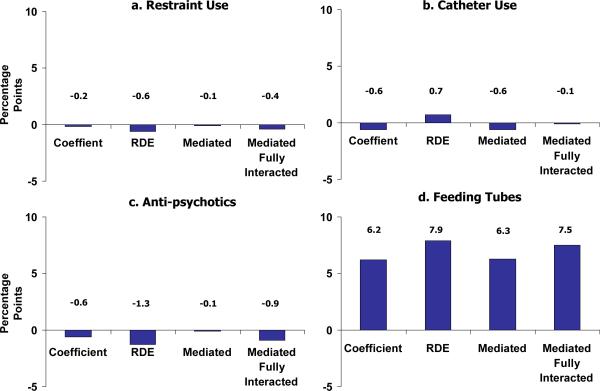
Finally, we turn to our fully interactive model for estimating disparities, the results are displayed graphically in Figure 2 for each of the four quality measures. Regression estimates for the fully interactive model are reported in Table 3. The race-payer status interaction terms are statistically meaningful across all four outcomes, while the race-education terms are generally significant in all cases except for the catheters model. We compare the fully interacted results from (4) to those from the basic model (1). Panel (a) of Figure 2 shows results for physical restraint use. The coefficient estimate of −0.2 percentage points was reported in Figure 1 and is reproduced here to be compared to the RDE estimate, which gathers the main effect and all the interaction effects with black race. The disparity becomes slightly more negative in Panel a than in Panel c. With respect to catheter use (Panel b) and feeding tubes (Panel d), the measured disparity increases quite a bit when comparing the RDE to the simple coefficient estimate. The RDE measure includes effects such as the following: if illness severity as measured by ADL makes it more likely that a resident uses a feeding tube, but that effect is greater for a black resident, the interaction of black and severity will reflect this. The RDE includes all interaction effects, with health status, SES and demographic variables as part of the effect of black race.
Figure 2.
Comparing Disparity Estimates of Basic Model and Fully Interacted Model
Table 3.
Regression Results, Fully Interacted Model
| Physical Restraints | Catheters | Anti-psychotics | Feeding Tubes | |
|---|---|---|---|---|
| Black | −0.0884** | −0.0505** | −0.1784** | −0.0593** |
| Private-pay | −0.0013* | 0.0017** | −0.0147** | −0.0013** |
| Other payer | −0.0230 | 0.0112** | 0.0058* | −0.0172** |
| High School education | −0.0087** | 0.0050** | −0.0136** | −0.0018** |
| Some college education | −0.0082** | 0.0088** | −0.0220** | −0.0046** |
| College education | −0.0062** | −0.0003 | −0.0226** | −0.0036** |
| Education missing | −0.0011 | −0.0137** | −0.0194** | −0.0049** |
| Private-pay * Black | 0.0127** | 0.0263** | 0.0114* | 0.0150** |
| Other payer * Black | 0.0529** | 0.0064 | 0.0133 | −0.0324** |
| High School education * Black | −0.0042 | −0.0018 | 0.0108* | 0.0073** |
| Some college education * Black | −0.0062 | 0.0026 | 0.0051 | −0.0035 |
| College education * Black | −0.0212** | 0.0021 | 0.0326** | −0.0092* |
| Education missing * Black | 0.0004 | −0.0007 | 0.0044 | 0.0125** |
| Home fixed effects | Y | Y | Y | Y |
| N | 1,545,356 | 1,545,372 | 882,505 | 1,545,369 |
Models also include age, gender, indications for length-of-stay by quarter, marital status, dummy variables for limitations in activities of daily living, dummy variables for cognitive performance score, and time indicated by quarters. All of these variables are also interacted with the black dummy variable.
= statistically significant at 5% level;
= statistically significant at 1% level.
The second two bars in each panel compare the mediated disparity from the basic model with the mediated estimate in the fully interacted model describe by equation (2"). In effect, the fully mediated estimate excludes differences due to health status differences between blacks and whites using the estimated coefficient for whites. Differences due to SES are included to be consistent with the IOM approach. The difference between the basic and fully interactive mediated estimates are that the basic model weights the differences by the effect of health status for both groups on average, and the fully interacted uses the white coefficients as the standard. This change in coefficient to weight racial differences in health status does not have a major effect on any estimate. It does, however, increase the estimated disparities in the feeding tube case, the one process indicator where we consistently find a black-white disparity.
Discussion
Nursing homes serve large numbers of poor and seriously disabled residents. Many residents are paid for by public funds, and may not be in a position to advocate for themselves or have family to advocate effectively on their behalf. Previous research has shown that nursing homes are among the most racially segregated health care institutions. Against this background, and in light of the impressive body of research documenting disparities in health care, we expected to find evidence of disparities in the quality of care received by black and white residents in nursing homes. Although we did find meaningful disparities in terms of feeding tube use, we did not find disparities in the other three observed process measures of quality after adjusting for controls.
The magnitude of disparities was not much affected by the definition of disparity applied, in contrast to some other studies. Whether measured by unadjusted mean differences, coefficient estimates, or measures allowing for mediation effects of SES racial differences, only one of four quality measures showed evidence of disparities. With the large amount of individual data available to characterize care in nursing homes, estimation of linear models makes the calculation of all measures of disparities relatively straightforward. Decomposition techniques originally developed for labor economics have ready application in disparities research, including methods counting disparities mediated through SES.
The intellectual foundation for empirical research on health care disparities derives in part from research on discrimination in labor economics. This paper is the first, as far as we know, to use a fully interacted model by race to estimate disparities, raising an issue not yet confronted in health services research. Estimating separate coefficients by racial/ethnic group implies that the effect of covariates, in addition to the underlying distribution of the covariates, differs by group. In this case, there is ambiguity in the thought experiment behind much of disparities research: “what care would black patients have received had they had the same health status as white patients?” When evaluating disparities by equating the distribution of health status across groups also equate the effect of health status? In this paper we argue yes, that the white coefficient, as well as the white distribution of health status, is the correct standard. The issues raised by fully interacted models should, however, be given further consideration.
Moving forward, more research is necessary comparing the care received by residents from different payer and racial/ethnic groups. Extension to groups beyond black and white is a natural step, as well as extending analysis to data from all states. The panel structure of the MDS allows for the time-varying adjustment for health status and also the study of a range of outcome measures, such as deterioration in health status or hospitalization from the nursing home. These can be consequences of poor quality of care that matter for social cost and welfare of the resident, and may well differ by population group.
In summary, this paper offers a new method of measuring disparities in the quality of care delivered to nursing home residents. Using detailed person-level nursing home data, we find meaningful black-white disparities for one of the four risk-adjusted quality measures, and evidence for both within and across nursing home disparities. The IOM approach, which allows mediation through payer status and education, had a small effect on measured disparities. Although we did not find disparities across the majority of quality measures and alternate disparity definitions, this approach can be applied to other health care services in an effort to disentangle the role of across and within facility variation and the role of potential mediators on racial/ethnic disparities.
Acknowledgements
Research for this paper was supported by grants K01 AG024403 from the National Institute of Aging, P60 MD002261 from the National Center for Minority Health and Health Disparities, and P50 MH073469 from the National Institute of Mental Health. These data were accessed under CMS data use agreement number 15989. We are grateful to Linda Dynan for helpful comments on an earlier draft.
Footnotes
For discussion of some of the conceptual issues associated with application of the IOM definition, including the problematic role of “preferences,” see McGuire et al. (2006).
The most prominent example of the first definition are the National Healthcare Disparities Reports produced by the Agency for Healthcare Quality and Research (AHRQ, 2007). Although these comprehensive and valuable reports take different approaches to disparities measurement depending on the subject, most of the group comparisons are unadjusted means. The disparities literature is filled with papers focusing on the race coefficient -- the second definition -- within a model of health care use.
See Fairlie (2006) for discussion of similar issues in a nonlinear context.
References
- AHRQ . National healthcare disparities report, 2007. Agency for Healthcare Research and Quality; Rockville, MD: 2007. [Google Scholar]
- Baicker K, Chandra A, Skinner JS, Wennberg JE. Who you are and where you live: How race and geography affect the treatment of Medicare beneficiaries. Health Affairs (Millwood) Suppl Web Exclusives. 2004:VAR33–44. doi: 10.1377/hlthaff.var.33. [DOI] [PubMed] [Google Scholar]
- Bernabei R, Gambassi G, Lapane K, Sgadari A, Landi F, Gatsonis F, Lipsitz L, Mor V. Characteristics of the SAGE database: a new resource for research on outcomes in long-term care. SAGE (Systematic Assessment of Geriatric drug use via Epidemiology) study sroup. Journals of Gerontology Series A: Biological and Medical Sciences. 1999;54(1):M25–33. doi: 10.1093/gerona/54.1.m25. [DOI] [PubMed] [Google Scholar]
- Blinder A. Wage discrimination – reduced form and structural estimates. Journal of Human Resources. 1973;8:436–455. [Google Scholar]
- Chandra A, Skinner J. Geography and racial health disparities. National Bureau of Economic Research, Inc.; Cambridge, MA: 2003. NBER Working Paper No. 9513. [Google Scholar]
- Cook B, McGuire T, Meara E, Zaslavsky A. Adjusting for health status in nonlinear models of health care disparities. Health Services Outcomes and Research Methodology. doi: 10.1007/s10742-008-0039-6. (forthcoming) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B, McGuire T, Zuvekas S. Measuring trends in racial/ethnic health care disparities. Medical Care Research and Review. doi: 10.1177/1077558708323607. (forthcoming) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenholtz HB, Arnold RA, Meisel A, Lave JR. Persistence of racial disparities in advance care plan documents among nursing home residents. Joural of the American Geriatric Society. 2002;50(2):378–81. doi: 10.1046/j.1532-5415.2002.50073.x. [DOI] [PubMed] [Google Scholar]
- Fairlie R. IZA Discussion Papers. I. f. t. S. o. L. (IZA). Bonn; Germany: 2006. An extension of the Blinder-Oaxaca decomposition technique to logit and probit models. [Google Scholar]
- Fennell ML, Miller SC, Mor V. Facility effects on racial differences in nursing home quality of care. American Journal of Medical Quality. 2000;15(4):174–81. doi: 10.1177/106286060001500408. [DOI] [PubMed] [Google Scholar]
- Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- Grabowski DC. The admission of blacks to high-deficiency nursing homes. Medical Care. 2004;42(5):456–64. doi: 10.1097/01.mlr.0000124307.17380.df. [DOI] [PubMed] [Google Scholar]
- Harrington C, Tompkins C, Curtis M, Grant L. Psychotropic drug use in long-term care facilities: a review of the literature. Gerontologist. 1992;32(6):822–33. doi: 10.1093/geront/32.6.822. [DOI] [PubMed] [Google Scholar]
- Howard DL, Sloane PD, Zimmerman S, Eckert JK, Walsh JF, Buie VC, Taylor PJ, Koch GG. Distribution of African Americans in residential care/assisted living and nursing homes: more evidence of racial disparity? American Journal of Public Health. 2002;92(8):1272–7. doi: 10.2105/ajph.92.8.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . Unequal treatment: Confronting racial and ethnic disparities in healthcare. National Academies Press; Washington, D.C.: 2003. [PubMed] [Google Scholar]
- Kirby JB, Taliaferro G, Zuvekas SH. Explaining racial and ethnic disparities in health care. Medical Care. 2006;55(5 Suppl):I64–72. doi: 10.1097/01.mlr.0000208195.83749.c3. [DOI] [PubMed] [Google Scholar]
- Konetzka RT, Werner RM. Disparities in long-term care: Building equity into policy. University of Chicago; Chicago, IL: 2008. Working paper. [DOI] [PubMed] [Google Scholar]
- McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the IOM definition of disparities: An application to mental health care. Health Services Research. 2006;41(5):1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Quarterly. 2004;82(2):227–56. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V, Lipsitz LA. MDS Cognitive Performance Scale. Journals of Gerontology: Medical Sciencis. 1994;49(4):M174–M182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- Oaxaca RL. Male-female wage differentials in urban labor markets. International Economic Review. 1973;14:693–709. [Google Scholar]
- Smith DB. The racial integration of health facilities. Journal of Health Politics, Policy and Law. 1993;18(4):851–69. doi: 10.1215/03616878-18-4-851. [DOI] [PubMed] [Google Scholar]
- Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: racial segregation and disparities in quality across U.S. nursing homes. Health Affairs (Millwood) 2007;26(5):1448–58. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- U.S. General Accounting Office . Nursing homes: Public reporting of quality indicators has merit, but national implementation is premature. U.S. General Accounting Office; Washington, DC: 2002. [Google Scholar]
- Zinn JS. The influence of nurse wage differentials on nursing home staffing and resident care decisions. Gerontologist. 1993;33(6):721–9. doi: 10.1093/geront/33.6.721. [DOI] [PubMed] [Google Scholar]