Abstract
Indices of P wave duration and dispersion are accessible from the surface electrocardiogram. Their prolongation reflects inhomogeneous atrial depolarization secondary to insults such as chronically elevated atrial pressure, ischemia, or metabolic stress. In turn, these insults promote atrial structural remodeling and provide a substrate for atrial fibrillation (AF). P wave indices have been examined in cardiac and non-cardiac disease states. Prolonged P wave indices have been associated with hypertension, obesity and diabetes, all of which are risk factors for AF. Similarly, prolonged P wave duration and dispersion have been associated with AF recurrence in patients with paroxysmal AF and following cardioversion, and with incident AF following cardiothoracic surgeries.
Our review describes the current field of P wave indices. We report the methodology for determining P wave indices. We also describe the strengths and limitations of the current literature on the clinical correlates and prognosis of P wave indices. We suggest future clinical and research directions for P wave indices.
Keywords: P wave indices, P wave dispersion, PR interval, electrocardiography, atrial fibrillation, risk factors
The P wave indices of maximum duration and dispersion have received increasing attention and have been examined in a broad range of clinical settings. The electrocardiogram, as a vectorcardiogram,1 quantifies the magnitude and direction of electrical propagation and depolarization. Insults such as chronically elevated atrial pressure, ischemia, and metabolic stress lead to atrial remodeling marked by inflammation, fibrosis and poor cellular coupling. The electrophysiologic result is slowed conduction with inhomogeneous recovery, defining a substrate for atrial fibrillation (AF).2 Investigators hypothesize that P wave prolongation is an intermediate step in the accumulation of insults ultimately leading to AF. Thus, initial studies sought to demonstrate significant differences between samples with a history of AF and healthy referents, arguing that prolonged P wave duration and dispersion predict recurrent AF. Further studies have employed P wave indices to compare multiple samples with and without cardiac diseases. The most recent iteration of studies has extended use of P wave indices beyond cardiac pathology to distinguish a variety of disease entities and comparison groups; the wide array of disease samples studied is listed in Table 1. Given such broad clinical applications, automated reporting of the P wave duration in electrocardiographic measurement for screening purposes has been advocated.3
Table 1.
Clinical conditions studied utilizing P wave indices.
| Risk Factors | Hypertension26;58;66 |
| Obesity5;28–30 | |
| Diabetes27 | |
| Noninvasive measures | Diastolic indices26;31 |
| Miscellaneous conditions | Hemodialysis38 |
| Hyperthyroidism39 | |
| Rheumatoid arthritis40 | |
| Scleroderma41 | |
| Pregnancy42 | |
| Obstructive sleep apnea67 | |
| Cardiovascular disease | Aortic stenosis17 |
| Mitral stenosis and balloon valvuloplasty35 | |
| Secundum atrial septal defect, prior and following surgical repair36;37 | |
| Post-Fontan procedure68 | |
| Atrial Fibrillation | Incident AF4;9;11;12;14;59 |
| Following pacemaker implantation64;65 | |
| Recurrence post-cardioversion57 | |
| Post-coronary artery bypass graft surgery24;61;62 | |
| Post-thoracic surgery63 | |
| Ischemia or angina32–34 | |
| Atrioventricular nodal re-entry tachycardia and ablation13 | |
| Accessory pathway and ablation6 | |
The variety of studies has resulted in varying methodologies and yielded conflicting results. Many areas in P wave indices research remain uncertain, including their clinical correlates and distribution in the community, and the extent to which P wave indices are associated with AF, predict its occurrence, are heritable phenotypes, or serve as biomarkers of other cardiovascular insults. The present review was undertaken to assess the current evidence for use of P wave indices with attention towards study design, strengths and remaining questions surrounding their clinical application.
Literature search methods
We conducted a literature search of PubMed and OVID databases to identify articles published from January, 1985 through December, 2007. We searched using the Medical Subject Headings and key words of P wave dispersion, P wave indices, dispersion, atrial fibrillation, and electrocardiogram, both separately and together with predict and prediction. We reviewed reference lists of retrieved articles to identify additional publications for inclusion. Because of the volume of research in this area and the duplicative nature of the field’s research, we excluded studies with less than 100 subjects unless they described a novel clinical application of P wave indices. Studies were described as cohort, case control, or cross-sectional. Case reports, scientific abstracts and articles published in languages other than English were excluded.
Measurement and reproducibility of P wave indices
Quantification
Maximum and minimum P wave durations are calculated from the standard electrocardiogram (ECG) during sinus rhythm. P wave dispersion is derived by subtracting the minimum P wave duration from the maximum in any of the twelve ECG leads. The term dispersion in the context of P wave indices describes atrial conduction and not the repolarization conveyed by T wave dispersion. Some studies report visualizing P wave onset and offset in a minimum of eight to nine leads as an inclusion criterion, although a minimum of three leads has been employed to determine P wave duration.4
We did not identify a report examining correlations of P wave indices measured in different electrocardiographic leads. Currently, P wave indices are calculated from the absolute difference between the shortest and longest P waves from the surface ECG. Use of adjacent leads with shared vectorial orientation may provide greater sensitivity for distinguishing the inhomogeneity of atrial activation. Future studies should analyze lead heterogeneity in findings, and report results highlighting the lead(s) from which they were derived.
The large majority of studies employed the P wave of longest or shortest duration; few studies determined a mean value from multiple measurements.5;6 The largest studies (n=500 to 1,353) to examine the relation of P wave duration and dispersion showed correlations ranging from 0.427 to 0.66.8
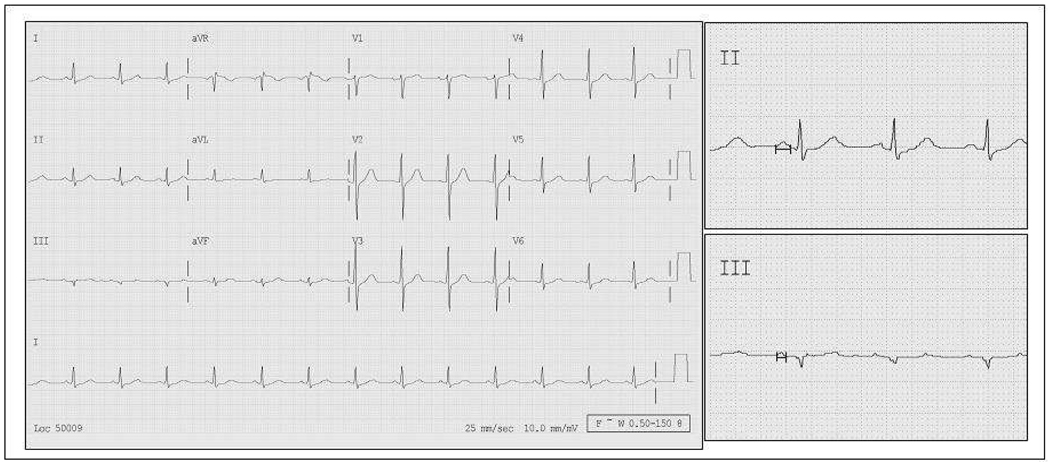
P wave indices have been calculated by measurements on paper or digitized images. Manual measurement with calipers has entailed increasing the ECG rate to 50 mm/sec and the voltage to 1 to 2 mv/cm,9;10 accompanied by use of magnification. There is potential for discrepancy in the two methods, and as reviewed below, the data consistently demonstrate that hand-held caliper measurements have less accuracy compared with digital measurments.10 The Figure demonstrates measurement of P wave indices in a normal ECG at 25 mm/sec using a digital measurement technique. Reliability of P wave indices calculation requires accurate determination of the P wave on-set and off-set.
Figure 1.
Twelve lead electrocardiogram with normal sinus rhythm and normal intervals. Measurement of leads II and III (side panels) demonstrated maximum and minimum P wave durations, respectively: 113 and 61 msec, and P wave dispersion 52 msec.
Reproducibility
Comparing paper and digital measurements, for maximum P wave duration measurements, the intraobserver relative errors were reduced from 16% to 7% and the interobserver relative errors were diminished from 17% to 8%. Similarly, the relative errors for P wave dispersion were reduced from 24% to 13% for intraobserver, and from 30% to 14% for interobserver comparing paper and digital measurement acquisition.11
The literature has varied in reproducibility metrics reported. Studies have described mean interobserver percent error ranging from 2%12 to 14%.11 Coefficients of variation have ranged from 2%13 to 5%.9 Intraobserver reproducibility has been shown to be strong, with correlation coefficients ranging from r=0.7814 to r=0.97.15
Distribution of P wave indices reported in the literature
The distribution of P wave indices has been studied in community, ambulatory, and hospitalized cohorts. Table 2 describes representative studies of P wave indices reported in the literature, including measurements reported for the referent or control cohorts from selected studies. For most of these studies, referent cohorts are comprised of matched patients serving as controls. In these studies the maximum P wave duration ranged from 93±1016 to 108±7.017 msec. P wave dispersion ranged broadly from 27±109 to 52±212 msec. In the largest identified community study of 1353 healthy air force servicemen, mean age 24 years (range 18 to 41), the mean maximum and minimum P wave durations were 95.6 and 57.2 msec, respectively.8 P wave dispersion mean was 38.4 msec, range of 13–80 msec; the median was not reported. In the same cohort the P wave duration prevalence ≥110 msec was 9.1% and ≥120 msec was 1.6%.18 A large, prospective cohort (n=8166) of patients following coronary artery bypass surgery had a median P wave duration of 112 msec (interquartile range 100–120 msec).19
Table 2.
Summary of P wave Indices in referent cohorts and selected studies
| Author, year. | Study design; clinical context. | N (referent or control cohort). | Maximum P wave duration (ms) [Range] |
P wave dispersion (ms) [Range] |
|---|---|---|---|---|
| Dilaveris, 1998.14 | Cross-sectional; PAF. | 40 | 101.0 ± 10.0 | 28.0 ± 7.0 |
| Andrikopoulos, 2000.11 | Cross-sectional; PAF. | 50 | 101.4 ± 10.1 | 29.8 ± 8.7 |
| Aytemir, 2000.9 | Cross-sectional; PAF. | 70 | 101.0 ± 11.0 | 27.0 ± 10.0 |
| Tukek, 2002.16 | Cross-sectional; COPD. | 33 | 93.0 ± 13.0 | 39.0 ± 7.0 |
| Gialafos, 2003.8 | Military cohort, young men. | 1353 | 96.0±11.0 [62.0–142.0] | 38.0 ± 10.0 [13.0–80.0] |
| Guray, 2003.36 | Cross-sectional; ASD. | 47 | 102 ± 13 | 31 ± 9 |
| Turhan, 2003.17 | Cross-sectional; AS. | 98 | 108.0 ± 7.0 | 32.0 ± 5.0 |
| Yigit, 2003.12 | Observational study; impact of exercise on P wave indices. | 155 | 94.0 ± 2.3 | 52.1 ± 2.0 |
| Gunduz, 2005.31 | Cross-sectional; diastolic dysfunction. | 60 | 104 ± 9 | 43 ± 9 |
| Ariyarajah, 2006.25 | Cross-sectional, ambulatory patients. | 469 | [40–170] | |
| Dagli, 2007.26 | Cross-sectional; hypertension. | 60 | 64 ± 10.2 | 30.3 ± 6.6 |
| De Bacquer, 2007.59 | Nested case-control. | 120 | ||
| Lauer, 2007.19 | Prospective following CABG. | 8166 |
PAF denotes paroxysmal atrial fibrillation; CABG, coronary artery bypass graft.
Although the criteria for abnormal P wave indices vary by study, several investigators have examined the prevalence of P wave duration exceeding various cutpoints. The prevalence of P wave duration ≥110 msec has been estimated as high as 41%,20 and ≥120 msec as high as 47%21 in hospitalized samples prompting the description of this finding as “pandemic”.22 A community-based sample of individuals ≥65 years identified 400 of 678 (59%) subjects as having a P wave duration ≥110 msec.23 The prevalence among men and women was similar (58.5% and 59.4%, respectively). Prior to coronary artery bypass surgery 56% of patients (868 of 1553 subjects) had a P wave duration >110 msec.24 Screening for P wave duration ≥120 msec increases the specificity of identifying prolonged P wave duration.25
In summary, studies suggest a large range for P wave indices in the community and ambulatory settings, with an increased prevalence of prolonged P wave indices with advancing age. To our knowledge, no large, community-based study has described the distribution of P wave indices in a reference sample without disease or risk factors, and then applied these values to define the range in a broad sample.
Clinical correlates associated with P wave dispersion
Demographics
We are unaware of prior studies that have systematically examined the relations of P wave indices with a broad range of clinical risk factors; rather the studies have tended to examine one risk factor at a time. Most previous studies have reported that P wave duration increases with advancing age.21 However, because most prior studies have not adjusted for the increases in risk factors and disease that occur with advancing age, it is uncertain whether aging per se increases P wave indices. Men and women in an older population (≥ 65 years) have been shown to have equivalent prevalence of P wave duration ≥110 msec.23 Similarly, ethnic/racial differences in P wave indices have been understudied.
Risk factors
Cross-sectional studies have examined the relations between risk factors and P wave indices. Subjects with uncontrolled hypertension have been shown to have significantly prolonged P wave duration and dispersion.26 In an unadjusted cross-sectional case-control study subjects with diabetes (n=76) had significantly longer P wave indices than controls (n=40).27 Several studies have examined the relations of P wave indices to obesity and have shown individuals with obesity had significantly longer P wave indices compared to control groups.28;29 Body mass index was moderately correlated (r=0.50) with P-wave dispersion,28 even in analyses adjusting for other clinical variables.29 Of interest, a decrease in P wave indices has been observed following weight loss.5 Similarly, bariatric surgery in a severely obese cohort was associated with a significant reduction in P wave indices over a twelve month period.30
Subclinical and clinical cardiac disease
Cross-sectional studies have assessed diastolic function and P wave indices and associated diastolic dysfunction with prolonged P wave indices compared to referent cohorts.26;31 P wave indices and diastolic dysfunction may comprise markers of a common pathophysiologic process. P wave indices and diastolic dysfunction may influence each other in a bidirectional fashion, one may predispose to the other, or their association may be due to confounding resulting from a more complex pathophysiologic process. The associations identified by these studies raise multiple hypotheses which merit further elucidation.
Studies meeting inclusion criteria examining P wave indices and coronary syndromes ranged in size from 9532 to 147 individuals.33 P wave dispersion before and after coronary intervention decreased from 69.5 to 52.4 msec.34 These values are substantively longer than those reported by the other identified studies32;33 evaluating the association between P wave indices and ischemia.
P wave indices have been examined in structural and valvular disease. They were significantly longer in subjects with aortic stenosis compared to controls.17 A single-center, case control study identified a significant decrease in P wave indices at one month following mitral balloon valvuloplasty for mitral stenosis.35 Similarly, subjects with a secundum atrial septal defect have had longer maximum P wave duration and P wave dispersion compared to matched controls;36 surgical repair of atrial septal defects has resulted in regression of P wave indices.37
Noncardiac conditions
Studies have examined P wave indices in a variety of non-cardiac conditions. The largest identified study (n=32) examining the effect of hemodialysis on P wave indices reported that maximum P wave duration and P wave dispersion increased significantly post-dialysis.38 A study reported that individuals with hyperthyroidism (compared to euthyroid individuals) had greater baseline maximum P wave duration and P wave dispersion, and that hyperthyroidism suppressive therapy was associated with a decrease in indices.39 Other efforts have determined positive association between P wave indices and rheumatoid arthritis40 or scleroderma.41 A larger, single-center study compared P wave indices of 162, healthy pregnant women to 150 matched controls,42 and found the pregnant cohort had a decreased minimum P wave duration.
Summary of clinical correlates
P wave indices have been evaluated in multiple clinical contexts including cardiac and non-cardiac disease states. Of particular interest are the relations between prolonged P wave indices and advancing age, hypertension, diabetes, and obesity, each of which has been identified as an independent risk factor for AF.43–45 Increased atrial pressures due to structural heart disease also clearly potentiate prolongation of P wave indices. These disease states may share common pathways of atrial inflammation and fibrosis46 that yield to atrial remodeling and inhomogeneity of conduction.
The investigations of P wave indices with clinical correlates, cardiovascular and non-cardiac conditions have limitations. Most studies were small to moderate in sample size, involved referral cohorts, and consequently had limited power and generalizability. Furthermore, the cross-sectional studies generally did not assess for either confounding or effect modification between advancing age, and clinical correlates in relation to P wave indices. The long-term impact of treating most risk factors or disease states such as hypertension and diabetes has not been assessed systematically and merits elucidation. Multiple clinical correlates in the community have yet to be investigated.
Electrocardiographic and electrophysiologic correlates of P wave indices
Electrophysiological studies have demonstrated significantly increased effective refractory periods, conduction times, and heterogeneity in right atrial conduction in older patients with no history of AF compared to younger cohorts.47 Consistent with prior studies the investigators noted a positive correlation (r=0.60) between mean age and P wave duration (measured only in lead II).47 Slowed interatrial conduction velocity has been demonstrated in a similarly small cohort with a history of AF.48 P wave loops may have an application towards further predicting risk of AF. Modification of P wave loops, and electroanatomical descriptions of P wave propagation, have been demonstrated by pulmonary vein isolation.49
Limitations included small sample sizes, lack of adjustment for covariates, and cross-sectional design. However, these studies generate hypotheses about pathways involving aging, inflammation and other insults resulting in atrial fibrosis, and the accompanying increased atrial heterogeneity reflected in prolonged P wave indices. Such a nuanced phenotypic model is perhaps more descriptive of P wave prolongation than describing P wave prolongation as “interatrial block,” and distinguishes electrophysiologic atrial activity from atrial size; atrial fibrosis is not indicative of atrial enlargement.
The electrocardiographic correlates of P wave indices are incompletely described. Our search did not identify studies assessing the relations of P wave indices with PR interval or QRS duration. Heart rate (i.e., RR interval) had a significant but modest association with P wave duration ≥110 msec in a large cohort of healthy young men (odds ratio 1.027 per beats/minute, 95% confidence interval 1.01 – 1.04)18 A clinical trial assessing the effect of exercise on P wave indices control subjects had a slight decrease in mean P wave duration (94.0 to 92.1 msec) and increase in mean dispersion (52.1 to 53.0) between rest and peak exercise.12
Signal Average ECG
Signal average ECGs (SAECG) have been used for predicting AF. Applications of SAECG are similar to P wave indices’ described above. Prolonged P wave SAECGs have been associated with recurrence of AF following cardioversion;50 comparison of hypertensive subjects with paroxysmal AF and those without;51 AF following cardiothoracic surgery;52;53 and transition from paroxysmal to permanent AF.54 Advantages of SAECG include its incorporation of information from hundreds of data points and lack of reliance on distinguishing P wave on-set and off-set, which improve the reliability and accuracy of the technique. Disadvantages of P wave SAECG are that it requires high fidelity, and highly specialized equipment that is not in wide clinical usage. The need for patients to lie completely still for 3–5 minutes in a room with no electrical interference also limits its broad implementation.
Genetic Variation and P Wave Indices
We were unable to find studies describing the heritability or genetic associations of P wave indices. In contrast, PR interval has been demonstrated as a heritable phenotype and has been associated with genetic variants in a community-based genome wide association study.55 Understanding the genetic contribution towards variability of P wave indices may provide endophenotypes or intermediate traits, which will aid in dissecting the contribution of genetic variation to inhomogeneous of atrial conduction. Such an investigation may be combined with results from other genome wide association studies that have examined genetic variants and AF,56 and may contribute insights into pathophysiology and propensity for the development of AF.
P Wave Indices and AF
Much of the literature on P wave indices has focused on their association with AF. Selected studies meeting the inclusion criteria for this review and pertinent to P wave indices and AF are summarized in Electronic Supplement Table 1. Cross-sectional studies have identified significantly prolonged P wave indices in individuals with a documented history of AF compared to a control cohort with no history of AF.9;11;12;14
P wave indices and AF recurrence
Subjects with recurrent AF have been shown to have significantly longer P wave indices and longer documented history of AF duration compared to individuals that maintained sinus rhythm. The largest cohort study included 64 subjects, and found the 28 with recurrence had significantly longer P wave indices.57
Association with incident AF
Prolonged P wave indices have been associated with increased risk for incident AF. A retrospective cohort study followed 97 patients with essential hypertension for a mean duration of 25±3 months, identifying incident AF in 20%.58 Adjusting for age attenuated the odds ratio from 2.09 to 1.34 for prolonged P wave indices (maximum duration ≥130 msec and dispersion ≥40 msec) to predict AF. In a case-control study of 308 hospitalized subjects, the prevalence of P wave duration ≥110 msec was 52% in the cohort with AF, compared to 18% of the 308 subjects in a referent cohort.4 This study had a large age range (26 to 93 years) and calculated P wave duration from three leads. A nested case-control study from a population-based study found that 70% of 40 elderly subjects who developed AF after 10 years had baseline P wave durations >120 msec, compared to 41% of the 120 controls.59 P wave duration remained predictive of AF following adjustment for covariates of body mass index and hypertension. Finally, in a prospective cohort of patients presenting with myocardial infarctions, patients whose presentation was complicated by AF had longer P wave indices.33
P wave indices and association with AF following cardiothoracic surgery
AF following cardiac surgery is associated with significant morbidity from prolonged hospitalization and an array of complications.60 Three retrospective studies examined P wave indices prior to cardiothoracic surgery to determine their relation to AF.24;61;62 The studies ranged in size from 12062 to 1553,24 and analyzed P wave duration as >100 or 110 msec. In multivariable analysis increased P wave duration was a significant predictor of AF.24;61 In a single center cohort analysis of 300 patients, mean P wave duration increased significantly following bypass surgery and predicted post-operative AF in multivariable analysis.61 Median P wave dispersion was similarly prolonged following thoracic surgery in a cohort which developed AF.63 In the cardiac surgery studies age,62 body surface area,61 prior AF or low cardiac output24 had a greater odds ratio for predicting post-operative AF than P wave duration.
Pacing cohort
Studies have examined P wave indices and the development of AF in cohorts with pacemakers. P wave indices, paced or non-paced, did not predict AF in 109 subjects with sick sinus syndrome.64 A large (n=660), prospective observational study followed a cohort paced for sinus bradycardia and found prolonged P wave indices were associated with AF hospitalization.64;65 Furthermore, subjects with longer P wave duration (≥100 msec) had significantly longer paced P wave durations.
P wave indices, other dysrhythmias, and incidence of AF
In unique small (n=72 and 78) studies of individuals referred for electrophysiologic study of atrioventricular nodal re-entry tachycardia13 or accessory pathways6 subjects with a history of AF had significantly greater maximum P wave duration and P wave dispersion.
Summary of relation of P wave indices to AF
Larger, more clinically robust studies with longer follow-up are necessary to determine the clinical relevance of P wave indices to incident AF. Limitations in the studies described above include lack of adjustment for covariates, short duration of follow up, small to moderate sample sizes, and treatment of P wave duration as a binary trait rather than a continuous variable.
Conclusion
Summary
P wave indices have been applied in a wide range of clinical contexts. They have been associated with clinical risk factors for AF, recurrence and incident AF in small to moderate sized referral cohorts of individuals with risk factors, structural heart disease or undergoing cardiothoracic surgery. The current research on P wave indices has been limited by studies with modest sample size, cross-sectional or limited follow-up, and lack of accounting for confounders. Most studies referenced in Table 1 have less than 100 subjects.
Despite the volume of studies, P wave indices reference (“normal”) values have not been standardized. P wave duration cut-offs of 110 or 120 msec have been proposed, but the large prevalence of hospitalized patients found to meet these criteria suggests a low specificity and poor screening utility. No prospective, community-based study has developed reference values by identifying a reference population, articulating measurements of indices, and then applying those measurements to a broad sample with cardiovascular disease, risk factors, and the covariates identified here.
Measurement techniques have not been standardized. Investigators continue to use magnification and hand-held calipers, yet have reported measuring P wave duration to the hundredth of a millisecond with this technique. A single study compared measurement techniques and found improved quality control with digitized measurements.10 Quality control assessments have been limited. Most investigators employed measurements surrounding the mean, potentially inflating reproducibility. Robust statistical measures for vigorous quality control are lacking. The deficits of standardized techniques and quality control severely limit the application of P wave indices.
Substantive questions remain concerning the correlations of calculated P wave indices and invasive electrophysiologic studies. Agreement between these two methods will be essential to verify the validity of P wave indices. There has not been adequate comparison of SAECG and P wave indices. Finally, interlead heterogeneity has not been incorporated into the assessment of P wave indices.
Future research directions
Significant challenges remain with regard to our implementation of P wave indices as a relevant component of screening. Reference values from large, community-based studies will assist with standardizing indices for sex and height. Correlations with heart rate, PR interval, and QRS duration will assist with understanding the electrocardiographic significance and interrelation of electrocardiographic parameters.
To date, no direct study between P wave SAECG and P wave indices has been performed; such a comparison will be an important advance for the field. Comparing P wave indices and data from electroanatomical mapping will elucidate the correspondence between a non-invasive and invasive assessment of atrial electrophysiology. Such an undertaking has the potential to demonstrate further the utility of P wave indices for screening purposes.
Clinical correlation with cardiac and non-cardiac disease states with attention to the influence of advancing age will provide further insights. For instance, cohort studies examining the associations of multiple cardiovascular risk factors and P wave indices will validate the findings of studies described in this review. Echocardiographic and magnetic resonance imaging features also will assist with determining the impact of structural heart diseases on P wave indices. P wave indices may be heritable traits, and provide valuable endophenotypes to contribute to the research community’s understanding of the genetic basis of electrocardiographic and electrophysiologic traits.
The utility of P wave indices as a clinically useful biomarker remains ambiguous. The chief question in establishing the relevance of a biomarker is whether such a measurement merely reflects pathophysiologic processes or provides unique, complementary insights to predict adverse outcomes. Large size, community-based cohort studies are necessary to achieve adequate power and adjustment for covariates. Such an effort will determine the utility of P wave indices to predict incident AF, heart failure, and overall mortality, and whether they provide additional data beyond already established clinical, echocardiographic and electrocardiographic covariates. P wave indices have potential to influence the treatment of AF. P wave indices may predict success with strategies such as elimination of triggers, i.e. pulmonary vein isolation, or substrate modification by pharmacologic intervention and risk factor management. Inexpensive and non-invasive, P wave indices may provide a cost effective screening mechanism. Further research is necessary to establish whether P wave indices will contribute independent information towards the ability predict the development of AF, adverse cardiovascular outcomes, and mortality.
Acknowledgments
Sources of Funding: Supported by NIH/NHLBI contract N01-HC-25195, HL076784, AG028321, 6R01-NS 17950.
Footnotes
Disclosures: None.
References
- 1.Michelucci A, Bagliani G, Colella A, Pieragnoli P, Porciani MC, Gensini G, Padeletti L. P wave assessment: state of the art update. Card Electrophysiol Rev. 2002;6:215–220. doi: 10.1023/a:1016368723033. [DOI] [PubMed] [Google Scholar]
- 2.Spach MS. Mounting evidence that fibrosis generates a major mechanism for atrial fibrillation. Circ Res. 2007;101:743–745. doi: 10.1161/CIRCRESAHA.107.163956. [DOI] [PubMed] [Google Scholar]
- 3.Uhley H. It is time to include P-wave duration. Pacing Clin Electrophysiol. 2007;30:293–294. doi: 10.1111/j.1540-8159.2007.00668.x. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal YK, Aronow WS, Levy JA, Spodick DH. Association of interatrial block with development of atrial fibrillation. Am J Cardiol. 2003;91:882. doi: 10.1016/s0002-9149(03)00027-4. [DOI] [PubMed] [Google Scholar]
- 5.Duru M, Seyfeli E, Kuvandik G, Kaya H, Yalcin F. Effect of weight loss on P wave dispersion in obese subjects. Obesity (Silver Spring) 2006;14:1378–1382. doi: 10.1038/oby.2006.156. [DOI] [PubMed] [Google Scholar]
- 6.Aytemir K, Amasyali B, Kose S, Kilic A, Abali G, Oto A, Isik E. Maximum P-wave duration and P-wave dispersion predict recurrence of paroxysmal atrial fibrillation in patients with Wolff-Parkinson-White syndrome after successful radiofrequency catheter ablation. J Interv Card Electrophysiol. 2004;11:21–27. doi: 10.1023/B:JICE.0000035925.90831.80. [DOI] [PubMed] [Google Scholar]
- 7.Ariyarajah V, Frisella ME, Spodick DH. Incremental prevalence of fractionated and inhomogeneous propagation of sinus impulses with increasing atrial depolarization abnormality among outpatients. Int J Cardiol. 2008;127:368–371. doi: 10.1016/j.ijcard.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 8.Gialafos EJ, Dilaveris PE, Synetos AG, Tsolakidis GF, Papaioannou TG, Andrikopoulos GK, Richter DJ, Triposkiadis F, Gialafos JE. P wave analysis indices in young healthy men: data from the digital electrocardiographic study in Hellenic Air Force Servicemen (DEHAS) Pacing Clin Electrophysiol. 2003;26:367–372. doi: 10.1046/j.1460-9592.2003.00051.x. [DOI] [PubMed] [Google Scholar]
- 9.Aytemir K, Ozer N, Atalar E, Sade E, Aksoyek S, Ovunc K, Oto A, Ozmen F, Kes S. P wave dispersion on 12-lead electrocardiography in patients with paroxysmal atrial fibrillation. Pacing Clin Electrophysiol. 2000;23:1109–1112. doi: 10.1111/j.1540-8159.2000.tb00910.x. [DOI] [PubMed] [Google Scholar]
- 10.Dilaveris P, Batchvarov V, Gialafos J, Malik M. Comparison of different methods for manual P wave duration measurement in 12-lead electrocardiograms. Pacing Clin Electrophysiol. 1999;22:1532–1538. doi: 10.1111/j.1540-8159.1999.tb00358.x. [DOI] [PubMed] [Google Scholar]
- 11.Andrikopoulos GK, Dilaveris PE, Richter DJ, Gialafos EJ, Synetos AG, Gialafos JE. Increased variance of P wave duration on the electrocardiogram distinguishes patients with idiopathic paroxysmal atrial fibrillation. Pacing Clin Electrophysiol. 2000;23:1127–1132. doi: 10.1111/j.1540-8159.2000.tb00913.x. [DOI] [PubMed] [Google Scholar]
- 12.Yigit Z, Akdur H, Ersanli M, Okcun B, Guven O. The effect of exercise to P wave dispersion and its evaluation as a predictor of atrial fibrillation. Ann Noninvasive Electrocardiol. 2003;8:308–312. doi: 10.1046/j.1542-474X.2003.08408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amasyali B, Kose S, Aytemir K, Kilic A, Turhan H, Celik T, Kursaklioglu H, Iyisoy A, Ozturk C, Isik E. P wave dispersion predicts recurrence of paroxysmal atrial fibrillation in patients with atrioventricular nodal reentrant tachycardia treated with radiofrequency catheter ablation. Ann Noninvasive Electrocardiol. 2006;11:263–270. doi: 10.1111/j.1542-474X.2006.00114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dilaveris PE, Gialafos EJ, Sideris SK, Theopistou AM, Andrikopoulos GK, Kyriakidis M, Gialafos JE, Toutouzas PK. Simple electrocardiographic markers for the prediction of paroxysmal idiopathic atrial fibrillation. Am Heart J. 1998;135:733–738. doi: 10.1016/s0002-8703(98)70030-4. [DOI] [PubMed] [Google Scholar]
- 15.Boriani G, Diemberger I, Biffi M, Camanini C, Valzania C, Corazza I, Martignani C, Zannoli R, Branzi A. P wave dispersion and short-term vs. late atrial fibrillation recurrences after cardioversion. Int J Cardiol. 2005;101:355–361. doi: 10.1016/j.ijcard.2004.03.039. [DOI] [PubMed] [Google Scholar]
- 16.Tukek T, Yildiz P, Akkaya V, Karan MA, Atilgan D, Yilmaz V, Korkut F. Factors associated with the development of atrial fibrillation in COPD patients: the role of P-wave dispersion. Ann Noninvasive Electrocardiol. 2002;7:222–227. doi: 10.1111/j.1542-474X.2002.tb00167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turhan H, Yetkin E, Atak R, Altinok T, Senen K, Ileri M, Sasmaz H, Cehreli S, Kutuk E. Increased p-wave duration and p-wave dispersion in patients with aortic stenosis. Ann Noninvasive Electrocardiol. 2003;8:18–21. doi: 10.1046/j.1542-474X.2003.08104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gialafos E, Psaltopoulou T, Papaioannou TG, Synetos A, Dilaveris P, Andrikopoulos G, Vlasis K, Gialafos J, Stefanadis C. Prevalence of interatrial block in young healthy men<35 years of age. Am J Cardiol. 2007;100:995–997. doi: 10.1016/j.amjcard.2007.04.041. [DOI] [PubMed] [Google Scholar]
- 19.Lauer MS, Martino D, Ishwaran H, Blackstone EH. Quantitative measures of electrocardiographic left ventricular mass, conduction, and repolarization, and long-term survival after coronary artery bypass grafting. Circulation. 2007;116:888–893. doi: 10.1161/CIRCULATIONAHA.107.698019. [DOI] [PubMed] [Google Scholar]
- 20.Jairath UC, Spodick DH. Exceptional prevalence of interatrial block in a general hospital population. Clin Cardiol. 2001;24:548–550. doi: 10.1002/clc.4960240805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asad N, Spodick DH. Prevalence of interatrial block in a general hospital population. Am J Cardiol. 2003;91:609–610. doi: 10.1016/s0002-9149(02)03320-9. [DOI] [PubMed] [Google Scholar]
- 22.Ariyarajah V, Asad N, Tandar A, Spodick DH. Interatrial block: pandemic prevalence, significance, and diagnosis. Chest. 2005;128:970–975. doi: 10.1378/chest.128.2.970. [DOI] [PubMed] [Google Scholar]
- 23.Ninios I, Pliakos C, Ninios V, Karvounis H, Louridas G. Prevalence of interatrial block in a general population of elderly people. Ann Noninvasive Electrocardiol. 2007;12:298–300. doi: 10.1111/j.1542-474X.2007.00178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amar D, Shi W, Hogue CW, Jr, Zhang H, Passman RS, Thomas B, Bach PB, Damiano R, Thaler HT. Clinical prediction rule for atrial fibrillation after coronary artery bypass grafting. J Am Coll Cardiol. 2004;44:1248–1253. doi: 10.1016/j.jacc.2004.05.078. [DOI] [PubMed] [Google Scholar]
- 25.Ariyarajah V, Frisella ME, Spodick DH. Reevaluation of the criterion for interatrial block. Am J Cardiol. 2006;98:936–937. doi: 10.1016/j.amjcard.2006.04.036. [DOI] [PubMed] [Google Scholar]
- 26.Dagli N, Karaca I, Yavuzkir M, Balin M, Arslan N. Aremaximum P wave duration and P wave dispersion a marker of target organ damage in the hypertensive population? Clin Res Cardiol. 2007 doi: 10.1007/s00392-007-0587-8. [DOI] [PubMed] [Google Scholar]
- 27.Yazici M, Ozdemir K, Altunkeser BB, Kayrak M, Duzenli MA, Vatankulu MA, Soylu A, Ulgen MS. The effect of diabetes mellitus on the P-wave dispersion. Circ J. 2007;71:880–883. doi: 10.1253/circj.71.880. [DOI] [PubMed] [Google Scholar]
- 28.Kosar F, Aksoy Y, Ari F, Keskin L, Sahin I. P-wave duration and dispersion in obese subjects. Ann Noninvasive Electrocardiol. 2008;13:3–7. doi: 10.1111/j.1542-474X.2007.00194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seyfeli E, Duru M, Kuvandik G, Kaya H, Yalcin F. Effect of obesity on P-wave dispersion and QT dispersion in women. Int J Obes (Lond) 2006;30:957–961. doi: 10.1038/sj.ijo.0803233. [DOI] [PubMed] [Google Scholar]
- 30.Russo V, Ammendola E, De C I, Docimo L, Santangelo L, Calabro R. Severe obesity and p-wave dispersion: the effect of surgically induced weight loss. Obes Surg. 2008;18:90–96. doi: 10.1007/s11695-007-9340-7. [DOI] [PubMed] [Google Scholar]
- 31.Gunduz H, Binak E, Arinc H, Akdemir R, Ozhan H, Tamer A, Uyan C. The relationship between P wave dispersion and diastolic dysfunction. Tex Heart Inst J. 2005;32:163–167. [PMC free article] [PubMed] [Google Scholar]
- 32.Dilaveris PE, Andrikopoulos GK, Metaxas G, Richter DJ, Avgeropoulou CK, Androulakis AM, Gialafos EJ, Michaelides AP, Toutouzas PK, Gialafos JE. Effects of ischemia on P wave dispersion and maximum P wave duration during spontaneous anginal episodes. Pacing Clin Electrophysiol. 1999;22:1640–1647. doi: 10.1111/j.1540-8159.1999.tb00384.x. [DOI] [PubMed] [Google Scholar]
- 33.Baykan M, Celik S, Erdol C, Durmus I, Orem C, Kucukosmanoglu M, Yilmaz R. Effects of P-wave dispersion on atrial fibrillation in patients with acute anterior wall myocardial infarction. Ann Noninvasive Electrocardiol. 2003;8:101–106. doi: 10.1046/j.1542-474X.2003.08202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Celik T, Iyisoy A, Kursaklioglu H, Kilic S, Kose S, Amasyali B, Isik E. Effects of primary percutaneous coronary intervention on P wave dispersion. Ann Noninvasive Electrocardiol. 2005;10:342–347. doi: 10.1111/j.1542-474X.2005.00647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Turhan H, Yetkin E, Senen K, Yilmaz MB, Ileri M, Atak R, Cehreli S, Kutuk E. Effects of percutaneous mitral balloon valvuloplasty on P-wave dispersion in patients with mitral stenosis. Am J Cardiol. 2002;89:607–609. doi: 10.1016/s0002-9149(01)02307-4. [DOI] [PubMed] [Google Scholar]
- 36.Guray U, Guray Y, Yylmaz MB, Mecit B, Sasmaz H, Korknaz S, Kutuk E. Evaluation of P wave duration and P wave dispersion in adult patients with secundum atrial septal defect during normal sinus rhythm. Int J Cardiol. 2003;91:75–79. doi: 10.1016/s0167-5273(02)00598-3. [DOI] [PubMed] [Google Scholar]
- 37.Guray U, Guray Y, Mecit B, Yilmaz MB, Sasmaz H, Korkmaz S. Maximum p wave duration and p wave dispersion in adult patients with secundum atrial septal defect: the impact of surgical repair. Ann Noninvasive Electrocardiol. 2004;9:136–141. doi: 10.1111/j.1542-474X.2004.92532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tezcan UK, Amasyali B, Can I, Aytemir K, Kose S, Yavuz I, Kursaklioglu H, Isik E, Demirtas E, Oto A. Increased P wave dispersion and maximum P wave duration after hemodialysis. Ann Noninvasive Electrocardiol. 2004;9:34–38. doi: 10.1111/j.1542-474X.2004.91529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Katircibasi MT, Deniz F, Pamukcu B, Binici S, Atar I. Effects of short-term propylthiouracil treatment on p wave duration and p wave dispersion in patients with overt hypertyroidism. Exp Clin Endocrinol Diabetes. 2007;115:376–379. doi: 10.1055/s-2007-971066. [DOI] [PubMed] [Google Scholar]
- 40.Guler H, Seyfeli E, Sahin G, Duru M, Akgul F, Saglam H, Yalcin F. P wave dispersion in patients with rheumatoid arthritis: its relation with clinical and echocardiographic parameters. Rheumatol Int. 2007;27:813–818. doi: 10.1007/s00296-007-0307-8. [DOI] [PubMed] [Google Scholar]
- 41.Can I, Onat AM, Aytemir K, Akdogan A, Ureten K, Kiraz S, Ertenli I, Ozer N, Tokgozoglu L, Oto A. Assessment of atrial conduction in patients with scleroderma by tissue Doppler echocardiography and P wave dispersion. Cardiology. 2007;108:317–321. doi: 10.1159/000099102. [DOI] [PubMed] [Google Scholar]
- 42.Ozmen N, Cebeci BS, Yiginer O, Muhcu M, Kardesoglu E, Dincturk M. P-wave dispersion is increased in pregnancy due to shortening of minimum duration of P: does this have clinical significance? J Int Med Res. 2006;34:468–474. doi: 10.1177/147323000603400503. [DOI] [PubMed] [Google Scholar]
- 43.Kannel WB, Abbott RD, Savage DD, McNamara PM. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N Engl J Med. 1982;306:1018–1022. doi: 10.1056/NEJM198204293061703. [DOI] [PubMed] [Google Scholar]
- 44.Wang TJ, Parise H, Levy D, D’Agostino RB, Sr, Wolf PA, Vasan RS, Benjamin EJ. Obesity and the risk of new-onset atrial fibrillation. JAMA. 2004;292:2471–2477. doi: 10.1001/jama.292.20.2471. [DOI] [PubMed] [Google Scholar]
- 45.Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840–844. [PubMed] [Google Scholar]
- 46.Everett TH, Olgin JE. Atrial fibrosis and the mechanisms of atrial fibrillation. Heart Rhythm. 2007;4:S24–S27. doi: 10.1016/j.hrthm.2006.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kistler PM, Sanders P, Fynn SP, Stevenson IH, Spence SJ, Vohra JK, Sparks PB, Kalman JM. Electrophysiologic and electroanatomic changes in the human atrium associated with age. J Am Coll Cardiol. 2004;44:109–116. doi: 10.1016/j.jacc.2004.03.044. [DOI] [PubMed] [Google Scholar]
- 48.Xia Y, Hertervig E, Kongstad O, Ljungstrom E, Platonov P, Holm M, Olsson B, Yuan S. Deterioration of interatrial conduction in patients with paroxysmal atrial fibrillation: electroanatomic mapping of the right atrium and coronary sinus. Heart Rhythm. 2004;1:548–553. doi: 10.1016/j.hrthm.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 49.Date T, Yamane T, Inada K, Matsuo S, Kanzaki Y, Miyanaga S, Shibayama K, Miyazaki H, Sugimoto K, Taniguchi I, Mochizuki S. The effects of pulmonary vein isolation on the morphology of p waves: the contribution of pulmonary vein muscle excitation to the formation of p waves. Pacing Clin Electrophysiol. 2007;30:93–101. doi: 10.1111/j.1540-8159.2007.00570.x. [DOI] [PubMed] [Google Scholar]
- 50.Budeus M, Hennersdorf M, Perings C, Wieneke H, Erbel R, Sack S. Prediction of the recurrence of atrial fibrillation after successful cardioversion with P wave signal-averaged ECG. Ann Noninvasive Electrocardiol. 2005;10:414–419. doi: 10.1111/j.1542-474X.2005.00059.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aytemir K, Amasyali B, Abali G, Kose S, Kilic A, Onalan O, Tokgozoglu L, Kabakci G, Ozkutlu H, Nazli N, Isik E, Oto A. The signal-averaged P-wave duration is longer in hypertensive patients with history of paroxysmal atrial fibrillation as compared to those without. Int J Cardiol. 2005;103:37–40. doi: 10.1016/j.ijcard.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 52.Steinberg JS, Zelenkofske S, Wong SC, Gelernt M, Sciacca R, Menchavez E. Value of the P-wave signal-averaged ECG for predicting atrial fibrillation after cardiac surgery. Circulation. 1993;88:2618–2622. doi: 10.1161/01.cir.88.6.2618. [DOI] [PubMed] [Google Scholar]
- 53.Tamis JE, Steinberg JS. Value of the signal-averaged P wave analysis in predicting atrial fibrillation after cardiac surgery. J Electrocardiol. 1998;30 Suppl:36–43. doi: 10.1016/s0022-0736(98)80018-6. [DOI] [PubMed] [Google Scholar]
- 54.Budeus M, Felix O, Hennersdorf M, Wieneke H, Erbel R, Sack S. Prediction of conversion from paroxysmal to permanent atrial fibrillation. Pacing Clin Electrophysiol. 2007;30:243–252. doi: 10.1111/j.1540-8159.2007.00656.x. [DOI] [PubMed] [Google Scholar]
- 55.Newton-Cheh C, Guo CY, Wang TJ, O’Donnell CJ, Levy D, Larson MG. Genome-wide association study of electrocardiographic and heart rate variability traits: the Framingham Heart Study. BMC Med Genet. 2007;8 Suppl:S1–S7. doi: 10.1186/1471-2350-8-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Darbar D, Hardy A, Haines JL, Roden DM. Prolonged signal-averaged P-wave duration as an intermediate phenotype for familial atrial fibrillation. J Am Coll Cardiol. 2008;51:1083–1089. doi: 10.1016/j.jacc.2007.11.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dogan A, Avsar A, Ozturk M. P-wave dispersion for predicting maintenance of sinus rhythm after cardioversion of atrial fibrillation. Am J Cardiol. 2004;93:368–371. doi: 10.1016/j.amjcard.2003.09.064. [DOI] [PubMed] [Google Scholar]
- 58.Ciaroni S, Cuenoud L, Bloch A. Clinical study to investigate the predictive parameters for the onset of atrial fibrillation in patients with essential. Am Heart J. 2000;139:814–819. doi: 10.1016/s0002-8703(00)90012-7. [DOI] [PubMed] [Google Scholar]
- 59.De Bacquer D, Willekens J, De Backer G. Long-term prognostic value of p-wave characteristics for the development of atrial fibrillation in subjects aged 55 to 74 years at baseline. Am J Cardiol. 2007;100:850–854. doi: 10.1016/j.amjcard.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 60.Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, Barash PG, Hsu PH, Mangano DT. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291:1720–1729. doi: 10.1001/jama.291.14.1720. [DOI] [PubMed] [Google Scholar]
- 61.Chandy J, Nakai T, Lee RJ, Bellows WH, Dzankic S, Leung JM. Increases in P-wave dispersion predict postoperative atrial fibrillation after coronary artery bypass graft surgery. Anesth Analg. 2004;98:303–310. doi: 10.1213/01.ANE.0000096195.47734.2F. table. [DOI] [PubMed] [Google Scholar]
- 62.Chang CM, Lee SH, Lu MJ, Lin CH, Chao HH, Cheng JJ, Kuan P, Hung CR. The role of P wave in prediction of atrial fibrillation after coronary artery surgery. Int J Cardiol. 1999;68:303–308. doi: 10.1016/s0167-5273(98)00301-5. [DOI] [PubMed] [Google Scholar]
- 63.Materazzo C, Piotti P, Mantovani C, Miceli R, Villani F. Atrial fibrillation after non-cardiac surgery: P-wave characteristics and Holter monitoring in risk assessment. Eur J Cardiothorac Surg. 2007;31:812–816. doi: 10.1016/j.ejcts.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 64.Kristensen L, Nielsen JC, Mortensen PT, Christensen PD, Vesterlund T, Pedersen AK, Andersen HR. Sinus and paced P wave duration and dispersion as predictors of atrial fibrillation after pacemaker implantation in patients with isolated sick sinus syndrome. Pacing Clin Electrophysiol. 2004;27:606–614. doi: 10.1111/j.1540-8159.2004.00494.x. [DOI] [PubMed] [Google Scholar]
- 65.Padeletti L, Santini M, Boriani G, Botto G, Ricci R, Spampinato A, Vergara G, Rahue WG, Capucci A, Gulizia M, Pieragnoli P, Grammatico A, Platonov P, Barold SS. Duration of P-wave is associated with atrial fibrillation hospitalizations in patients with atrial fibrillation and paced for bradycardia. Pacing Clin Electrophysiol. 2007;30:961–969. doi: 10.1111/j.1540-8159.2007.00793.x. [DOI] [PubMed] [Google Scholar]
- 66.Dilaveris PE, Gialafos EJ, Chrissos D, Andrikopoulos GK, Richter DJ, Lazaki E, Gialafos JE. Detection of hypertensive patients at risk for paroxysmal atrial fibrillation during sinus rhythm by computer-assisted P wave analysis. J Hypertens. 1999;17:1463–1470. doi: 10.1097/00004872-199917100-00015. [DOI] [PubMed] [Google Scholar]
- 67.Can I, Aytemir K, Demir AU, Deniz A, Ciftci O, Tokgozoglu L, Oto A, Sahin A. P-wave duration and dispersion in patients with obstructive sleep apnea. J Cardiol. 2008 doi: 10.1016/j.ijcard.2007.11.037. [DOI] [PubMed] [Google Scholar]
- 68.Wong T, Davlouros PA, Li W, Millington-Sanders C, Francis DP, Gatzoulis MA. Mechano-electrical interaction late after Fontan operation: relation between P-wave duration and dispersion, right atrial size, and atrial arrhythmias. Circulation. 2004;109:2319–2325. doi: 10.1161/01.CIR.0000129766.18065.DC. [DOI] [PubMed] [Google Scholar]