Abstract
Despite the rapid advances in laparoscopic surgery in the past 2 decades, the initial entry still accounts for approximately 40% to 50% of laparoscopic complications and should be considered the most dangerous step of a laparoscopic procedure. In this review, the authors share a technique for initial umbilical entry, and provide alternative entry sites in cases where umbilical entry is contraindicated.
Key words: Laparoscopic surgery complications, Laparoscopic surgical technique, Laparoscopic umbilical entry, Veres needle
Despite the rapid advances in laparoscopic surgery in the past 2 decades, the initial entry still accounts for approximately 40% to 50% of laparoscopic complications and should be considered the most dangerous step of a laparoscopic procedure.1,2
A variety of laparoscopic entry methods have been described. The Hungarian physician János Veres first described the use of his Veres needle to induce pneumothorax in the treatment of pulmonary tuberculosis in 1936.3 Laparoscopic entry using a Veres needle followed by the blind insertion of a sharp trocar remains the most common entry method used by gynecologists.4,5 Other entry methods include the open technique (Hasson) and direct trocar entry without a preexisting pneumoperitoneum. Unfortunately, the available literature is not clear as to which form of laparoscopic entry is superior in terms of complication risks, and the most common recommendation is for surgeons to use entry methods with which they feel comfortable.6
We would like to share our technique of initial umbilical entry, as well as our experience with alternative site entry in situations where umbilical entry is contraindicated. The basic principle of our umbilical entry technique is to take advantage of the negative intraperitoneal pressure that is generated by pulling on the abdominal fascia. We have been performing this technique for several years with good success, but recently heard of a similar technique that has been performed successfully for decades by Dr. Sarath De Alwis in the Cayman Islands. In his honor we have named our technique the modified Alwis method. The original Alwis method is described in Table 1.
Table 1.
The Original Alwis Method
| Step 1. Vertical insertion of Veres needle at the umbilicus. Aspirate to check for possible bowel contents. |
| Step 2. If no bowel contents are seen, infuse 0.1–0.2 L CO2 (0.4–0.5 L for obese patients) and rest the Veres needle flat on the abdomen by the assistant. |
| Step 3. Abruptly lift the lower abdomen. This creates an increased negative pressure in the lower abdomen. The noise can be heard, but ideally it should be recorded using a microphone on the skin (like a diaphragm on the stethoscope) connected to a recorder that shows intensity, or pitch of the sound as seen on some radios. If the sound is heard, it is certainly intraperitoneal. If no sound, but you still feel that you are in the correct place, then go to step 4. |
| Step 4. Infuse up to 1 L of CO2, stop, and ballot the abdomen. It should feel like a water bed. If the abdomen is firm or there is no sensation of a water bed, the placement is preperitoneal. Rarely the abdomen can be tight and the water bed sign negative if the patient is not adequately paralyzed. |
| Factors for Sensitivity and Specificity of the Test |
| 1. If the sound is heard at 0.1–0.2 L (0.4–0.5 L in obese patients), then the Veres needle is 100% certain to be in the intraperitoneal space. |
| 2. If no sound is heard, the needle is either: |
| A. Preperitoneal, or |
| B. There is blood, fluid, air, or excess gas (CO2) in the pelvis and there is no surface tension to create a negative-pressure. |
| Principle of the Test |
| The visceral organs have a thin layer of peritoneal fluid, on the peritoneal surface, that exerts surface tension. For example, when a person stands on the head, the bowels remain in the anatomical positions due to the surface tension. |
| When you abruptly lift the abdominal wall after 100–400 cc of gas or air, the negative pressure rises and the air from the positive pressure rushes into the area of the negative pressure, making a distinct sound that can be heard in a quiet setting or recorded using a microphone. |
Umbilical Entry: Modified Alwis Method
The insufflator is set on high flow from the outset and the goal intraperitoneal pressure is set at 15 mm Hg (Figure 1).
A hemostat is used for exposure to gain access to the deepest portion of the belly button, where an incision is made using a 15-blade knife (Figure 2). Care is taken to go through only the epidermis and dermis; we do not bury the blade here to avoid injury to underlying organs. It is important to make the incision in the deepest portion of the belly button because this is the thinnest portion of the abdominal wall, even in very obese patients.
The deepest portion of the belly button is grasped with a Kocher clamp, the belly button is elevated, and a Veres needle with the gas tubing connected is inserted vertically next to the Kocher clamp with a finger on the skin to prevent the needle from going too far (Figure 3). The normal distance to the peritoneum is only 2 to 3 cm.
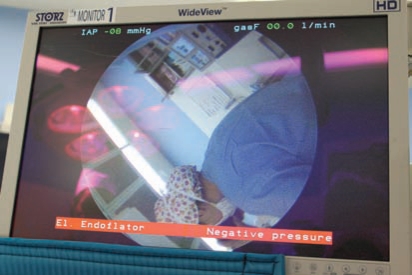
As soon as the peritoneum is entered, a negative pressure warning will appear on the monitor and a warning alarm will sound (Figure 4). This indicates an intraperitoneal location of the Veres needle. It must be noted that this is not true for all insufflators, but works well using the insufflator from Storz. On other types of insufflators there may not be a warning sound, but a negative pressure reading should be accessible.
The gas is turned on and the abdomen is insufflated until the intraperitoneal pressure is 15 mm Hg.
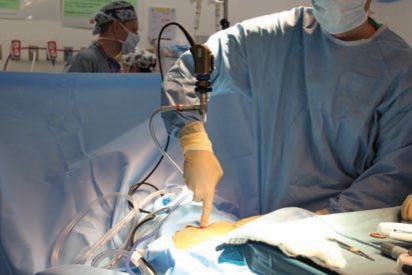
A 5-mm endoscope is inserted into an optical trocar that is inserted through the intraumbilical incision under direct vision (Figure 5). Intra-abdominal entry is confirmed and the area under the umbilicus is inspected for any signs of injury.
Figure 1.
Initial insufflator settings.
Figure 2.
Skin incision at the base of the umbilicus.
Figure 3.
Elevation of the umbilicus and insertion of the Veres needle
Figure 4.
Negative pressure reading on the monitor upon peritoneal entry.
Figure 5.
Entry with an optical trocar.
We have found this to be a very reliable method to confirm intraperitoneal entry of the Veres needle. A caveat is that in severely obese patients it may be difficult to create a negative intraperitoneal pressure by pulling on the umbilicus. Therefore, in cases where intraperitoneal entry is suspected but negative pressure is not displayed, we find it helpful to turn on the gas and use the displayed intraperitoneal pressure for confirmation. In most cases, if the pressure is below 10 mm Hg the placement of the Veres needle can be assumed to be intraperitoneal.
Alternative Site Entry
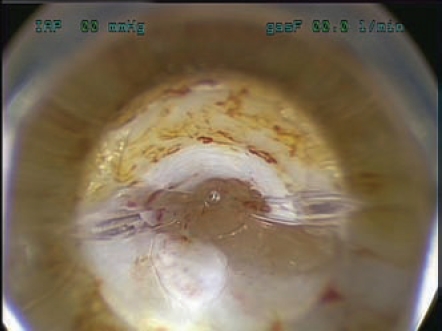
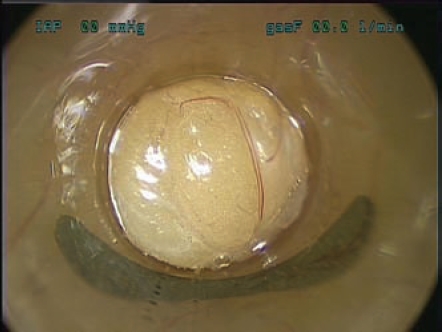
There are situations where umbilical entry may not be suitable. Some common scenarios include a prior vertical skin and/or fascial incision, umbilical hernia, and a prior repair of an umbilical hernia using mesh. In these cases it may be advisable to enter the abdomen at an alternative site because there is a high incidence of adhesions under the umbilicus and open entry does not guarantee against a visceral injury.7 One of the reasons for this may be a scenario depicted in Figure 6, where a loop of small bowel is firmly adherent directly underneath the umbilicus. In this situation, intestinal injury is almost unavoidable with any method during umbilical entry.
Figure 6.
A loop of small bowel is firmly adherent to the inside of the belly button.
We have developed a visually controlled direct entry method for this scenario. We found that it was sometimes challenging to confirm correct intraperitoneal entry using a Veres needle because it is more difficult to elevate the abdominal wall adequately. We therefore have foregone the use of the Veres needle for alternative site entry. We most often use the left upper quadrant approach, making a 5-mm skin incision along the midclavicular line approximately 4 to 5 cm cephalad from the umbilicus. We make certain that the patient has a gastric tube in place prior to trocar insertion. However, in cases where patients have had left upper quadrant surgery, we prefer to use an alternative site of entry, such as the right upper quadrant or anywhere else on the abdominal wall where there are no adjacent scars or underlying organs.
The steps are described below. The case illustrated in Figure 6 involved a right upper quadrant entry in a patient with a history of multiple midline incisions with mesh and gastric bypass surgery.
A 5-mm incision is made in the right upper quadrant and a 5-mm optical trocar with an endoscope is inserted into the incision (Figure 7).
Initially, fat is encountered (Figure 8).
Next, an outer fascial layer is seen, followed by a muscle layer (Figure 9).
Once through the muscle layer, the inner fascial layer is seen (Figure 10).
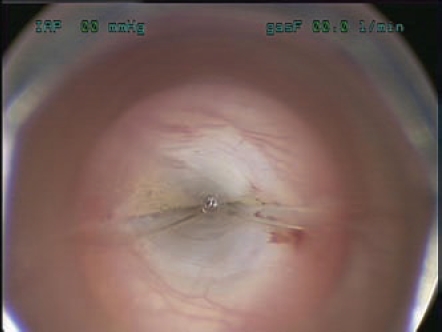
Very shortly thereafter the peritoneum is entered (Figure 11).
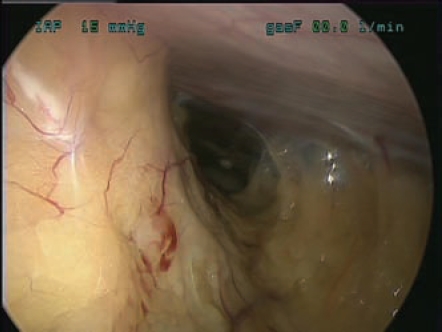
The optical trocar sheath is removed and the lens is placed into the trocar for confirmation of intraperitoneal entry. Usually omentum is seen, but bowel can often be seen peristalsing around the trocar (Figure 12).
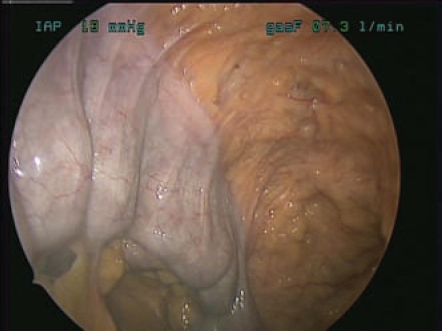
The flow of gas is now started and the intraperitoneal cavity can be examined. In this case severe midline adhesions were noted (Figure 13).
This patient also had small bowel firmly adherent to the inside of the left upper quadrant area (Figure 14).
Figure 7.
Entry with an optical trocar.
Figure 8.
Fatty layer of the abdominal wall.
Figure 9.
Outer fascial layer and muscle layer.
Figure 10.
Inner fascial layer.
Figure 11.
Peritoneal entry.
Figure 12.
Confirmation of peritoneal entry after removal of the optical trocar sheath.
Figure 13.
Severe midline adhesions.
Figure 14.
Small bowel firmly adherent to the abdominal wall in the left upper quadrant.
It is important to note that there is an initial tendency to travel too far with the trocar once the inner fascial layer has been traversed. The distance from the inner fascial layer to the peritoneal cavity is only a few millimeters and therefore it is advisable in the first few cases to have a liberal policy of removing the optical trocar sheath intermittently to see directly what is at the end of the trocar. Once a comfort level has been reached, this technique can be used successfully in a fairly rapid manner. A similar entry method has been described previously by Ternamian8; however, a specially designed trocar is necessary for this entry method.
Discussion
A wide variety of laparoscopic entry techniques exist and several surgeons have developed individualized safe entry methods. Nevertheless, entry-related complications are common and account for a significant amount of morbidity and mortality during laparoscopic surgery.
Traditional texts recommend an insertion angle of 45° from horizontal in patients with a body mass index smaller than 30 kg/m2 to avoid a vascular injury.9 However, in our experience we have not had a problem with a vertical orientation of the Veres needle, provided that the umbilicus is significantly elevated and the needle is only inserted a distance of approximately 2 to 3 cm or until a negative pressure is encountered. We use high flow from the outset because the narrow lumen of the Veres needle only allows for a flow rate of approximately 2 to 3 L/min. This does not affect safety, but simplifies the entry process.
There are numerous other tests that assess correct placement of the Veres needle. Some of the more commonly described include the double-click test, the hanging drop test, the aspiration test, and the initial peritoneal pressure of less than 10 mm Hg. The available evidence suggests that of these tests, the initial peritoneal pressure of less than 10 mm Hg is most reliable.10–12
Although we acknowledge that no entry method is foolproof, we have yet to experience an entry-related injury using our methods, with the senior author performing 450 to 500 advanced laparoscopic cases per year. We encourage surgeons to standardize their entry technique as much as possible and to seek guidance from other surgeons if they are encountering frequent complications during laparoscopic entry.
References
- 1.Härkki-Sirén P, Kurki T. A nationwide analysis of laparoscopic complications. Obstet Gynecol. 1997;89:108–112. doi: 10.1016/s0029-7844(96)00390-0. [DOI] [PubMed] [Google Scholar]
- 2.Jansen FW, Kapiteyn K, Trimbos-Kemper T, et al. Complications of laparoscopy: a prospective multicentre observational study. Br J Obstet Gynaecol. 1997;104:595–600. doi: 10.1111/j.1471-0528.1997.tb11539.x. [DOI] [PubMed] [Google Scholar]
- 3.Sandor J, Ballagi F, Nagy A, Rákóczi I. A needlepuncture that helped to change the world of surgery. Homage to János Veres. Surg Endosc. 2000;14:201–202. doi: 10.1007/s004649900101. [DOI] [PubMed] [Google Scholar]
- 4.Jansen FW, Kolkman W, Bakkum EA, et al. Complications of laparoscopy: an inquiry about closed- versus open-entry technique. Am J Obstet Gynecol. 2004;190:634–638. doi: 10.1016/j.ajog.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 5.Lingam K, Cole RA. Laparoscopic entry port visited: a survey of practices of consultant gynaecologists in Scotland. Gynaecol Endosc. 2001;10:335–342. [Google Scholar]
- 6.Merlin TL, Hiller JE, Maddern GJ, et al. Systematic review of the safety and effectiveness of methods used to establish pneumoperitoneum in laparoscopic surgery. Br J Surg. 2003;90:668–679. doi: 10.1002/bjs.4203. [DOI] [PubMed] [Google Scholar]
- 7.Brill AI, Nezhat F, Nezhat CH, Nezhat C. The incidence of adhesions after prior laparotomy: a laparoscopic appraisal. Obstet Gynecol. 1995;85:269–272. doi: 10.1016/0029-7844(94)00352-E. [DOI] [PubMed] [Google Scholar]
- 8.Ternamian AM. A trocarless, reusable, visualaccess cannula for safer laparoscopy; an update. J Am Assoc Gynecol Laparosc. 1998;5:197–201. doi: 10.1016/s1074-3804(98)80091-1. [DOI] [PubMed] [Google Scholar]
- 9.Hurd WH, Bude RO, DeLancey JO, et al. Abdominal wall characterization with magnetic resonance imaging and computed tomography. The effect of obesity on the laparoscopic approach. J Reprod Med. 1991;36:473–476. [PubMed] [Google Scholar]
- 10.Vilos GA, Vilos AG. Safe laparoscopic entry guided by Veress needle CO2 insufflation pressure. J Am Assoc Gynecol Laparosc. 2003;10:415–420. [PubMed] [Google Scholar]
- 11.Teoh B, Sen R, Abbott J. An evaluation of four tests used to ascertain Veres needle placement at closed laparoscopy. J Minim Invasive Gynecol. 2005;12:153–158. doi: 10.1016/j.jmig.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 12.Azevedo OC, Azevedo JL, Sorbello AA, et al. Evaluation of tests performed to confirm the position of the Veress needle for creation of pneumoperitoneum in selected patients: a prospective clinical trial [in Portuguese] Acta Cir Bras. 2006;21:385–391. doi: 10.1590/s0102-86502006000600006. [DOI] [PubMed] [Google Scholar]