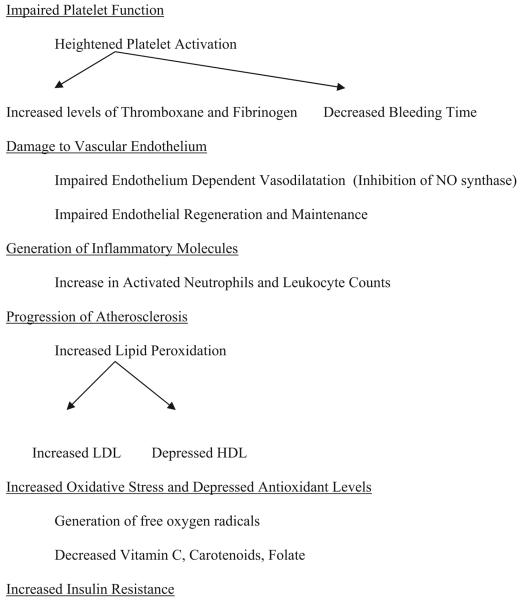
Passive smoking causes approximately 50 000 deaths annually in the United States, with the vast majority of these deaths due to heart disease.1 The effects of secondhand smoke on many pathophysiological mediators of coronary artery disease are nearly as large as those of active smoking, including impaired platelet function,2 damage to vascular endothelium and its associated repair mechanisms,3 a rise in inflammatory molecules, and dysfunctional lipid metabolism (Figure).2 The large literature on passive smoking is not limited to cardiovascular disease. Passive smoking causes lung cancer, head and neck cancers, respiratory infections, and obstructive lung disease (chronic obstructive pulmonary disease, asthma) and has been linked with breast cancer in younger women.1,4 Although as of 2008, more than half of the United States was covered by legislation that limits tobacco use in public places and workplaces, the Centers for Disease Control and Prevention found that nearly one half of US nonsmokers continue to be exposed to secondhand smoke.5
Figure.
Effects of passive smoking on biological mediators of vascular disease.2,3 NO indicates nitric oxide.
In this issue of Circulation, He et al6 document yet another example of the dangers associated with secondhand smoke exposure: peripheral arterial occlusive disease (PAOD). This is the first study to identify an association between exposure to secondhand smoke and the development of PAOD in any population, particularly among the nonsmoking Chinese women they studied. PAOD is a surrogate marker for coronary artery disease, resulting from similar pathophysiological mechanisms: development of atherosclerosis that leads to vascular stenosis and ischemia, which is manifested as claudication in the extremities. Given the similar underlying mechanisms, the results of the study by He et al6 are not surprising, but they are important nonetheless.
The cross-sectional study by He et al6 of a large population of Chinese nonsmoking women who were exposed to secondhand smoke at home and in the workplace found that their risk of developing PAOD was nearly twice that of nonex-posed, nonsmoking Chinese women ([OR 1.87, 95% CI 1.30 to 2.68] defined by presence of intermittent claudication and [OR 1.67, 95% CI 1.23 to 2.16] defined by intermittent claudication and measurements of ankle-brachial index). They arrived at these results even after accounting for 13 recognized risk factors for vascular disease, including age, daily level of exercise, body mass index, alcohol consumption, hypertension, hyperlipidemia, diabetes mellitus, and a family medical history of illness.
Two of the more highly publicized risk factors for vascular disease that He et al6 account for include diet and exercise habits, issues that are particularly relevant to American culture. While US citizens, including North American Chinese, struggle with obesity, which makes them more vulnerable to heart, vascular, and other disease, people in China consume less fat, have lower rates of obesity, and maintain higher exercise levels.7 Chinese in China consume 22% of their daily calories from fat compared with 35% for North American Chinese.7 Chinese in China also spend more time in vigorous physical activity and fewer hours sitting than Chinese in North America.7 Overall, Chinese in China weigh less and are leaner than North American Chinese.7 These differences are significant when considering the implications of the findings by He et al6 for Americans, because Chinese in China minimize 2 known risk factors for vascular disease and yet still have an increased risk of PAOD due to high rates of active and passive smoking.
Although diet and exercise are clearly important variables in the equation for development of vascular disease, smoking must be recognized as one of the most important modifiable causes of PAOD. Current smokers have 5 times the odds of developing PAOD compared with nonsmokers (OR 4.46, 95% CI 2.25 to 8.84).8 Compared with other recognized risk factors for vascular conditions, cigarette smoking exceeds hypertension (OR 1.75, 95% CI 0.97 to 3.15, P>0.05), diabetes (OR 2.71, 95% CI 1.03 to 7.12), hyperlipidemia (OR 1.68, 95% CI 1.09 to 2.57), and depressed kidney function (OR 2.00, 95% CI 1.08 to 3.70) as a risk factor for PAOD.8 With the present study by He et al,6 passive smoking is added as an important risk factor for PAOD, with effects that are as large as the other established risk factors.
He et al6 further show that Chinese nonsmoking women exposed to secondhand smoke are nearly 60% more likely to have an ischemic stroke than nonexposed, nonsmoking women. This study is similar to the 2005 analysis by Zhang et al9 of stroke risk among nonsmoking Chinese women exposed to spouses who smoke. They showed a clear dose-response relationship between degree of exposure and stroke risk after controlling for potential confounding variables such as age, body mass index, medical history, and level of activity.9 He et al6 similarly showed a clear dose-response relationship between exposure and risk for PAOD and ischemic stroke.
China's population consumes more cigarettes than any other country in the world, in part because the Chinese government and medical community do little to control tobacco.10 The smoking prevalence in China is 31%, with 57% of men and 3% of women who smoke, and current estimates predict that 52% of nonsmokers in China are exposed to secondhand smoke at home or at work.10 Cigarette smoking in China accounts for 7.9% of all preventable, premature deaths, surpassing physical inactivity and poor nutrition.11 Vascular disease and cancer— both caused by tobacco— have become the leading causes of death in China.11 Ischemic heart disease due to secondhand smoke causes an estimated 33 800 deaths and the loss of more than one quarter of a million years of healthy life.12 Moreover, although the burden of disease caused by active smoking occurs mostly among men, women bear nearly 80% of the total health hazards caused from passive smoking.12
Unfortunately, rates of smoking among Chinese physicians have been reported to be as high as 23% (41% among men and 1% among women), with fewer than one third of physicians reporting implementation of smokefree work-places and as many as 37% actively smoking in front of their patients.13 Despite the clear health risks associated with active and passive smoking, it is not surprising that China faces significant obstacles in their treatment of tobacco dependence.13 If Chinese healthcare professionals continue to smoke and expose their patients to secondhand smoke, how can they promote successful cessation and protection from passive smoking?
The research by He et al6 not only adds to the literature on the dangers of passive smoking but also highlights the ongoing need to educate physicians and patients on the dangers associated with secondhand smoke. With increasing information on the adverse health effects of active and passive smoking, the healthcare community must realize that counseling patients against tobacco use involves addressing more than the risks to the active smoker; healthcare providers must also stress to their patients and their families the harm their cigarette smoke can cause others.
Furthermore, therapeutic interventions designed to promote cessation should extend to family and friends, who must learn ways to protect parents and grandparents. The study by He et al6 focuses on an older population of nonsmoking, nonexposed Chinese women who are at greater risk for development of vascular disease and other comorbid conditions. As individuals age, the prevalence of chronic disease and disability increases.
In America, for many families, nursing homes and assisted-living facilities become new sources of extended home and health care. Current labor laws14 often exempt nursing facilities from smokefree policies so that smokers can consume tobacco in either indoor or outdoor designated areas, thereby serving as another source of exposure for everyone else. The frail and elderly are often not in a position to advocate for smokefree homes. Clearly, minimizing exposures that may compromise health in an already weakened population is an important way to reduce premature morbidity and mortality.
Although clinician and patient education is needed to encourage complete cessation, public health policies that support smokefree homes (including nursing homes and assisted-living facilities) and workplaces are important, not only to minimize the burden of disease, including cardiovascular mortality, but to create an environment that motivates and helps smokers quit.15 The combination of patient and physician education coupled with public health activism can reduce active and passive smoking, resulting in immediate health benefits, particularly with regard to cardiovascular disease.16,17
Acknowledgments
Sources of Funding
This editorial was conducted with the support of the National Cancer Institute (grant CA-113710). The funding agency played no role in the preparation of the editorial.
Footnotes
Disclosures
None.
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1.California Environmental Protection Agency: Air Resources Board Proposed identification of environmental tobacco smoke as a toxic air contaminant. Tobacco Control: Surveys and Program Evaluations From Outside UCSF. 2005 June 24; Available at: http://repositories.cdlib.org/tc/surveys/CALEPA2005/. Accessed: September 15, 2008.
- 2.Barnoya J, Glantz SA. Cardiovascular effects of secondhand smoke: nearly as large as smoking. Circulation. 2005;111:2684–2698. doi: 10.1161/CIRCULATIONAHA.104.492215. [DOI] [PubMed] [Google Scholar]
- 3.Heiss C, Amabile N, Lee AC, Real WM, Schick SF, Lao D, Wong ML, Jahn S, Angeli FS, Minasi P, Springer ML, Hammond SK, Glantz SA, Grossman W, Balmes JR, Yeghiazarians Y. Brief secondhand smoke exposure depresses endothelial progenitor cells activity and endothelial function: sustained vascular injury and blunted nitric oxide production. J Am Coll Cardiol. 2008;51:1760–1771. doi: 10.1016/j.jacc.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 4.The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. US Dept of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, Ga: 2006. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Disparities in Secondhand Smoke Exposure–United States, 1988–1994 and 1999–2004. MMWR Morb Mortal Wkly Rep. 2008;57:744–747. [PubMed] [Google Scholar]
- 6.He Y, Lam TH, Jiang B, Wang J, Sai X, Fan L, Li X, Qin Y, Hu FB. Passive smoking and risk of peripheral arterial disease and ischemic stroke in Chinese women who never smoked. Circulation. 2008;118:1535–1540. doi: 10.1161/CIRCULATIONAHA.108.784801. [DOI] [PubMed] [Google Scholar]
- 7.Lee MM, Wu-Williams A, Whittemore AS, Zheng S, Gallagher R, Teh CZ, Zhou L, Wang X, Chen K, Ling C, Jiao D-A, Jung D, Paffenbarger RS., Jr Comparison of dietary habits, physical activity and body size among Chinese in North America and China. Int J Epidemiol. 1994;23:984–990. doi: 10.1093/ije/23.5.984. [DOI] [PubMed] [Google Scholar]
- 8.Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation. 2004;110:738–743. doi: 10.1161/01.CIR.0000137913.26087.F0. [DOI] [PubMed] [Google Scholar]
- 9.Zhang X, Shu XO, Yang G, Li HL, Xiang YB, Gao YT, Li Q, Zheng W. Association of passive smoking by husbands with prevalence of stroke among Chinese women nonsmokers. Am J Epidemiol. 2005;161:213–218. doi: 10.1093/aje/kwi028. [DOI] [PubMed] [Google Scholar]
- 10.Yang GH, Ma JM, Liu N, Zhou LN. Smoking and passive smoking in Chinese, 2002 [in Chinese] Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26:77–83. [PubMed] [Google Scholar]
- 11.He J, Gu D, Wu X, Reynolds K, Duan X, Yao C, Wang J, Chen CS, Chen J, Wildman RP, Klag MJ, Whelton PK. Major causes of death among men and women in China. N Engl J Med. 2005;353:1124–1134. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 12.Gan Q, Smith KR, Hammond SK, Hu TW. Disease burden of adult lung cancer and ischaemic heart disease from passive tobacco smoking in China. Tob Control. 2007;16:417–422. doi: 10.1136/tc.2007.021477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang Y, Ong MK, Tong EK, Yang Y, Nan Y, Gan Q, Hu TW. Chinese physicians and their smoking knowledge, attitudes, and practices. Am J Prev Med. 2007;33:15–22. doi: 10.1016/j.amepre.2007.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cal Labor Code §6404 and §6404.5 [section of the California State Labor Code, specifically relating to smoking in enclosed workplaces] 1988.
- 15.Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ. 2002;325:188. doi: 10.1136/bmj.325.7357.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lightwood JM, Glantz SA. Short-term economic and health benefits of smoking cessation: myocardial infarction and stroke. Circulation. 1997;96:1089–1096. doi: 10.1161/01.cir.96.4.1089. [DOI] [PubMed] [Google Scholar]
- 17.Glantz SA. Meta-analysis of the effects of smokefree laws on acute myocardial infarction: an update. Prev Med. 2008 June 18; doi: 10.1016/j.ypmed.2008.06.007. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]