Abstract
G-protein coupled receptors (GPCRs) are widely expressed cell surface receptors that have been successfully exploited for the treatment of a variety of human diseases. Recent studies in genetically engineered mouse models have led to the identification of several GPCRs important for lymphatic vascular development and function. The adrenomedullin receptor, which consists of an oligomer between calcitonin receptor-like receptor and receptor activity modifying protein 2, is required for normal lymphatic vascular development and regulates lymphatic capillary permeability in mice. Numerous studies also suggest that lysophospholipid receptors are involved in the development of lymphatic vessels and lymphatic endothelial cell permeability. Given our current lack of pharmacological targets for the treatment of lymphatic vascular diseases like lymphedema, the continued identification and study of GPCRs in lymphatic endothelial cells may eventually lead to major breakthroughs and new pharmacological strategies for the treatment of lymphedema.
Keywords: lymphangiogenesis, lymphedema, genetically altered mice, pharmacological approaches, G-protein coupled receptor
G-protein coupled receptors as drug targets
G-protein coupled receptors (GPCRs) are widely expressed proteins that span the cell membrane 7 times and respond to a variety of stimuli including peptides, proteins, small organic compounds, lipids, amino acids and cations. Recent estimates predict that humans have approximately 800 GPCRs which can be grouped into five major phylogenetic families: Rhodopsin, Secretin, Adhesion, Glutamate and Frizzled/Taste2 families.1 A comprehensive review article exploring the diversity between GPCR families and its significance for drug design was recently published by Lagerstrom & Schioth.2 In summary, GPCRs from every family are highly attractive targets for pharmacological manipulation by either recombinant proteins, small molecule compounds, allosteric ligands or antibodies. There are currently 46 GPCRs that serve as drug targets for the treatment of a multitude of conditions including hypertension, pain, ulcers, allergies, alcoholism, obesity, glaucoma, psychotic disorders and HIV. However, this leaves several hundreds of GPCRs as potential drug targets and among those approximately 150 are still considered orphan receptors (receptors for which the endogenous ligand has yet to be identified).2 One major impediment to increasing the repertoire of pharmacologically useful GPCRs is our general lack of knowledge regarding the association of a putative GPCR with a precise physiological function or disease condition. Therefore, as scientists embark on the journey of elucidating the pathophysiology of complex and poorly treatable diseases, one beneficial approach may be to identify GPCRs associated with the condition, because they may eventually translate into effective drug targets.
Diseases of the lymphatic vascular system and current therapies
Diseases of the lymphatic vascular system serve as an example of how lack of knowledge about normal and diseased tissues has limited our ability to generate many effective pharmacological therapies. The lymphatic vascular system normally works to maintain tissue fluid homeostasis, absorb fatty acids and lipid-soluble vitamins from the gut and traffic antigen-presenting immune cells through the lymph nodes. Therefore, failure of the lymphatic vascular system has devastating consequences.3 Lymphedema is the result of inadequate lymphatic function and if not properly managed can lead to debilitating and painful limb swelling, tissue fibrosis, inflammation and increased susceptibility to infection. Lymphedema can be caused by rare genetically-inherited mutations resulting in abnormal development or function of the lymphatic vascular system either at birth, puberty or adulthood.4 More common causes of lymphedema are due to physical disruption or damage to the lymphatic vasculature, either by surgery, radiation therapy or infection with the mosquito parasites Wuchereria bancrofti or Brugia malayi. In industrialized countries, the occurrence of lymphedema is rapidly increasing, proportional to the increasing use of surgical and radiation therapies for life-saving cancer treatments. Recent estimates show that one third to nearly one half of women develop lymphedema after breast cancer treatments.5, 6 In many tropical and sub-tropical countries, parasitic filarial lymphedema or elephantiasis is endemic and affects approximately 120 million individuals worldwide.7 Regardless of the cause, lymphedema carries with it immense psychological and social sequelae and disability.3
Rockson has recently provided a survey of current treatment strategies for the management of lymphatic vascaular disease.8 Currently, the most effective treatment for lymphedema consists of a multifaceted physiotherapeutic approach for improving lymphatic function through application of lymphatic-specific massage techniques, remedial exercise, fitted compression garments and skin care.8 Although this all-inclusive approach is largely successful among compliant patients9, the daily treatments and changes in lifestyle can cause undesirable financial, physical and psychological strain for many patients.
Recent surgical approaches have provided limited relief to patients with severe lymphedema. For example, liposuction followed by sustained intense compression can relieve tissue congestion caused by collagen and fat deposition.10, 11 However, liposuction only provides temporary relief from swelling and does not directly improve lymphatic function. Reconstructive microsurgery through lymphavenous anastomoses (in effect, lymphatic bypass surgery) can provide minimal relief but is largely ineffective.12
Pharmacological therapies for lymphedema are extremely limited and largely controversial. Coumarin has been shown to reduce lymphedema, but its overall effectiveness and functional mechanism remain controversial.13-15 Moreover, long term systemic treatment with coumarin is correlated with a high rate of hepatotoxicity.13, 16 Antioxidents, including selenium and flavonoids, have also been explored as potential therapies, but preliminary investigations into their effectiveness have remained inconclusive.17 The treatment for parasitic filarial lymphedema has had better success. Massive drug delivery programs, consisting of dual treatment with diethylcarbamazine and albendazole (anti-parasitic agents), can effectively target and eliminate infecting parasites and reduce the burden of filarial lymphedema in large populations.18 However, treatment strategies for filariasis do not repair the previously damaged lymphatic vasculature within an individual.
Perhaps the most exciting progress toward pharmacological treatments for lymphedema has come from vascular endothelial growth factor C (VEGFC)-based therapies. As described below, VEGFC is a potent growth and migratory factor for lymphatic endothelial cells. In animal models of lymphedema, VEGFC-based therapies have been demonstrated to promote lymphangiogenesis.19-23 Even more promising has been the recent discovery that adenovirally-delivered VEGFC can induce the formation of functional collecting lymphatics as well as improve the outcomes of lymph node transplantations in mice.22 Other growth factors, including VEGFD, VEGFA, fibroblast growth factor-2 and hepatocyte growth factor have also shown exciting promise as therapeutic lymphangiogenic agents in animal models.24, 25
Nevertheless, it remains clear that the identification of additional drug targets for the modulation of lymphatic growth or permeability is highly desirable. Because GPCRs are pharmacologically-tractable cell-surface receptors and are widely used for the treatment of human diseases, the identification of potentially useful GPCR targets for the modulation of lymphatic vascular growth or function would represent a major advancement in the field. In the following sections, we highlight recent discoveries from animal models that have uncovered novel roles for several GPCRs in lymphatic vascular development and function.
Lessons in lymphangiogenesis from gene knockout models
In the past 10 years, phenotypic characterization of gene knockout mouse models has resulted in remarkable progress toward identifying genes important in the development and function of the lymphatic vascular system. The impact that gene targeting has had on driving the field forward is unparalleled, and so it is fitting that the 2007 Nobel Prize in Physiology or Medicine was awarded to Smithies, Capecchi and Evans in recognition of their efforts toward developing gene targeting approaches. Several elegant and fully comprehensive reviews have recently been published with in depth details and insights on how the phenotypes of gene targeted animal models have built the foundation for understanding lymphangiogenesis.26-28
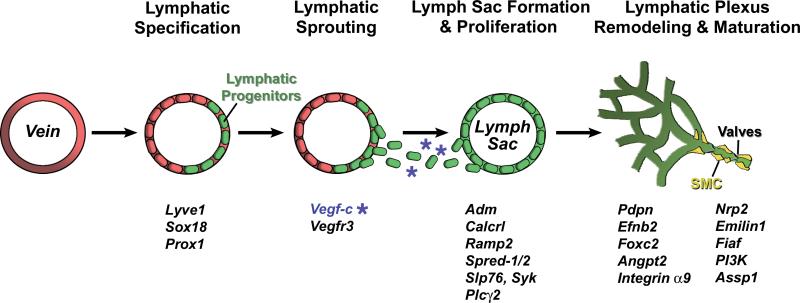
Figure 1 summarizes our current understanding of the stepwise process of lymphangiogenesis and lists numerous genetic factors that have been identified as important for lymphangiogenesis through gene targeting approaches. Development of the lymphatic vascular system is initiated when lymphatic-endothelial-hyaluronan-receptor-1 (LYVE1)-expressing endothelial cells of the cardinal vein begin to express the transcription factor sex determining region Y-box 18 (Sox18) which drives expression of prospero-related homeobox 1 (Prox1) in a polarized manner.29 Sox18 and Prox1 transcriptionally reprogram venous endothelial cells so that they become specified toward a lymphatic fate.29, 30 The up-regulation of the VEGFC receptor, VEGFR3, in lymphatic endothelial cells confers their ability to sprout from the cardinal vein and migrate toward an ectopic gradient of growth-promoting VEGFC.31 The lymphatic endothelial cells organize into primary lymph sacs which eventually separate from the cardinal vein in a process dependent on several genes, including tyrosine kinase Syk and adaptor protein Slp76, phospholipase C gamma 2 (Plcγ2) and sprouty-related, EVH1 domain 1 and 2 (Spred1&2).32-34 Subsequent rounds of proliferation lead to the formation of a primary lymphatic plexus which is later remodeled with mural cells and luminal valves to form the fully functional lymphatic vascular network.
Figure 1. Stepwise process of lymphangiogenesis.
The development of the lymphatic vasculature begins with specification of lymphatic endothelial cells from venous precursors. The chemoattractant and growth promoting properties of numerous growth factors, including VEGFC, causes lymphatic endothelial cells to sprout and separate from veins to form primitive lymph sacs. Proliferation of lymph sacs leads to the formation of a primary lymphatic plexus which is later remodeled into the mature lymphatic vascular system. Below each step is a list of genes for which a functional role has been demonstrated using genetically engineered mouse models.
Progress toward elucidating these developmental steps has been steadfast over the past 10 years, with a handful of new genetic players identified every year. But only recently have GPCRs become implicated in lymphangiogenesis and the following sections highlight these new discoveries with an emphasis on how these receptors may be pharmacologically beneficial.
Calcitonin receptor-like receptor
The calcitonin receptor-like receptor (CALCRL) belongs to the Secretin family of GPCRs; a small family of 15 receptors that bind peptide hormones and have extended extracellular N’ terminal hormone-binding domains.2 A distinguishing feature of several Secretin family receptors is their ability to associate with single-pass transmembrane proteins that can alter receptor trafficking, ligand binding and downstream signaling.35 The identification and characterization of these 3 mammalian receptor activity modifying proteins (RAMP1−3) was first established with CALCRL, such that RAMP1 association with CALCRL produces a receptor with high affinity for calcitonin gene-related peptide (CGRP) whereas association with RAMP2 or RAMP3 produces a receptor with preferential binding to adrenomedullin (AM).36 Recently, a third endogenous peptide ligand, intermedin, was also shown to signal through CALCRL-RAMP complexes.37 Therefore, whether a cell to responds to either CGRP, AM or intermedin is largely dependent on the extent of RAMP expression. The unique ability of RAMPs to modulate receptor ligand binding properties has already been exploited in drug design. Two small molecule compounds that antagonize CGRP binding to the CALCRL-RAMP1 oligomer are currently in clinical trials for the management of pain associated with migraine.38 Although no compounds have yet been described for CALCLR-RAMP2 oligomers, our recent studies in genetically engineered mouse models suggest that CALCRL-RAMP2 oligomers may represent ideal drug targets for the lymphatic vasculature.
Several years ago, our laboratory began to systematically generate and comparatively phenotype gene knockout mice for all mammalian RAMPs, CALCRL and AM with the hopes of identifying conserved (or divergent) phenotypes in which the use of RAMP-based compounds could be beneficial for the treatment of human diseases.39-42 The most striking of phenotypes, embryonic lethality at mid-gestation, occurs in knockout mice for AM, CALCRL and RAMP2.42 Remarkably, each of these knockout mice shares a highly conserved appearance of generalized edema without hemorrhage, which not only provides compelling evidence that AM-CALCRL-RAMP2 constitutes a physiologically relevant signaling pathway but also suggests that the development of the lymphatic vascular system is abnormal. Indeed, the AM, CALCRL and RAMP2 knockout mice all suffer from substantially smaller jugular lymphatic vessels due to significantly reduced proliferation of lymphatic endothelial cells compared to venous endothelial cells during mid-gestation.42 Elegant studies by Jin and colleagues also show that AM-treatment of adult mice with tail lymphedema significantly improves lymphedema and promotes in vivo lymphangiogenesis.43
Although several studies demonstrate that AM can affect the proliferation, permeability and growth of the blood vasculature44, 45, the prevalence of the lymphatic vascular defects in the knockout models is supported by numerous other studies. For example, comparative gene profiling studies between blood endothelial cells (BECs) and lymphatic endothelial cells (LECs) consistently demonstrate that CALCLR and RAMP2 are preferentially up-regulated in the lymphatic lineage.46, 47 While some of this up-regulation can be attributed to transcriptional regulation by the lymphatic-specific transcription factor Prox142, recent studies also suggest that down-regulation of RAMP2 levels by a blood-enriched microRNA may equally contribute to the enhanced expression of RAMP2 in LECs (personal communication, Dr. Michael Detmar, Univ. Zurich, Switzerland). Comparative gene profiling experiments also reveal that Complement Factor H, the serum binding protein for AM that enhances AM peptide activity by 2-fold48, is significantly enriched in LEC compared to BECs.49 Finally, mice with genetic deletion of the enzyme required for functionally activating AM peptide through amidation, peptidylglycine alpha-amidating monooxygenase (PAM), precisely phenocopy the AM, CALCRL and RAMP2 knockout mice50; though in depth characterization of the lymphatic vasculature has not yet been performed. Taken together, these studies demonstrate that several mechanisms are in place to ensure that the local bioactivity of AM peptide and the sensitivity to CALCRL-RAMP2 signaling are highly enriched in the lymphatic vasculature. This is further supported by our recent study demonstrating that the principal effect of subcutaneous AM peptide injection is to significantly decrease local lymphatic permeability in the dermal lymphatic vessels of the mouse tail.51 So, although the broad tissue distribution of CALCRL-RAMP2 may cause some hesitation for drug design (due to undesirable off-target side effects), the inherent sensitivity and up-regulation of AM receptors in the lymphatic endothelium may prove to be highly beneficial.
Lysophospholipid receptors
Lysophospholipid (LP) receptors belong to the Rhodopsin family of GPCRs and bind bioactive lipids to elicit a wide range of cellular effects. Originally known as endothelial differentiation gene receptors (Edg), these receptors are currently designated as either lysophosphatidic acid receptors (LPA1−3) or sphingosine-1-phosphate receptors (S1P1−5), reflective of their respective lipid ligands.52 LP receptors are nearly ubiquitously expressed and cells may express multiple subtypes.53 The bioactive lipid ligands LPA and S1P are also widely expressed but most highly produced by platelets, which when activated release LPA and S1P into the bloodstream in the micromolar range.54, 55 LP receptor signaling has been shown mediate angiogenesis, permeability, vascular tone, and cardiac function56-59 as well as participate in the immune response through regulation of lymphocyte trafficking.60-63 Currently, several preclinical and clinical stage studies are being undertaken, utilizing both antagonist and agonist of LP receptors, in the hopes of providing therapies against tumor growth and metastasis64-66 and autoimmune disorders including multiple sclerosis, kidney graft rejection, and inflammation.67-71
Recent genetic studies in zebrafish have demonstrated an essential role for LPA signaling in lymphatic vascular development since morpholino-based knockdown of zebrafish LPA (zlpa1) resulted in failure of thoracic duct development.72 Interestingly, this phenotype was partially rescued by VEGFC over-expression, suggesting that LPA and VEGFC signaling may converge to promote lymphatic vessel development.72 In another study, ligand binding to LPA1/3 receptors on human umbilical venous endothelial cells (HUVECs) increased VEGFC expression and secretion.73, 74 Remarkably, LPA stimulation also promoted the formation of Prox1 and podoplanin positive capillary tubes, suggesting that LPA signaling has the ability to confer lymphatic identity.74 Many studies demonstrate that LPA can modulate the paracellular permeability of the endothelial cell barrier.59 Although there are no reports specifically describing LPA-mediated effects on LEC permeability, the broad effects of LPA on endothelial cell function make it likely that LPA also affects LEC permeability. Gene targeted knockout mouse models of LPA1, LPA2, and LPA3 receptors do not display any cardiovascular developmental defects.75-77 However, mice null for autotaxin (ATX), the enzyme necessary for producing bioactive LPA, are embryonic lethal with severe vascular defects, suggesting that the LPA(1−3) receptors may be functionally redundant in the developing vasculature.78 Given the recent evidence that LPA functions as a potent lymphangiogenic factor, extensive re-evaluation of the LPA(1−3) null mice for lymphatic vascular defects may be informative.
Sphingosine-1-phosphate activation of S1P1/3 receptors in LECs also promotes lymphangiogenesis both in vitro and in vivo.79 Compared to HUVECs, LECs expressed more S1P1/3 receptors and following stimulation with S1P, secreted more angiopoeitin-2, a potent lymphangiogenic factor.80 Several studies have demonstrated that S1P signaling decreases endothelial cell permeability through reorganization of junctional proteins at the plasma membrane.58, 81 Recent studies exploring lymphocyte trafficking into the lymphatic sinuses showed that S1P1 stimulation effectively tightened the lymphatic endothelial cell barrier and these effects may be due to enhanced organization of junctional components including ZO-1, CD31, and β-catenin.63, 65, 82 The predominant phenotype of the S1P1 knockout mice is massive hemorrhage at mid-gestation caused by an endothelial-specific failure in vascular smooth muscle cell recruitment and vessel maturation.83, 84 Mice lacking all three S1P receptors (S1P1, S1P2, and S1P3) had exacerbated vascular deficiencies compared to S1P1 knockout mice, while S1P2-S1P3 double knockout mice exhibited partial lethality with fragile endothelial cells prone to hemorrhage.85 These data suggest that S1P receptors have both redundant and cooperative functions during vascular development, but do not preclude the possibility that S1P signaling may play an important role in lymphatic vascular development or function.
Taken together, an increasing number of new studies, both in vivo and in vitro, suggest that lysophospholipid receptors may mediate important biological functions in the lymphatic vasculature, including lymphangiogenesis, vessel integrity, LEC permeability and potential cross-talk with other lymphangiogenic factors. Since LP receptors are already being pharmacologically exploited for the treatment of human disease, future studies focused on the effects of lysophospholipids on the lymphatic vasculature may lead to new GPCR targets for the modulation of lymphatic growth or function.
Searching for other GPCRs in lymphatic endothelial cells
Because GPCR proteins are typically expressed at low levels in endogenous tissues, the use of proteomic profiling approaches for identifying lymphatic-specific GPCRs may prove problematic. Also, since antibodies directed against the extracellular domain of GPCRs can be difficult to generate and/or lack specificity, the use of immunohistochemical approaches to identify lymphatic-specific GPCRs may also provide limited benefit. So, perhaps the best approach lies in genome-wide transcriptional profiling approaches, where cohorts of genes that are differentially expressed between LECs and BECs can be identified and compared. Fortunately, several research groups have already performed these very informative and elegant experiments.46, 47, 49 In all of these studies, there exist at least 6 GPCRs that appear to be enriched in LECs, and most of them are still considered orphan receptors with no identified ligand. The importance of GPCR signaling in LECs is also supported by the increased expression in LECs of several GPCR signaling modifiers, like regulator of G-protein signaling 2 (RGS-2), RGS-16 and β-arrestin.47, 49
Olfactory receptors are the largest class of GPCRs, with 388 predicted human receptors, and belong to the Rhodopsin receptor family. Nearly all are considered orphan receptors, and beyond the fragrance industry they have not generally been considered as candidate drug targets for human diseases.2 However, it is interesting to recognize that like the CALCRL-RAMP paradigm, several olfactory receptors have been associated with RAMP-like accessory proteins, called receptor accessory proteins (REEPs).86 Like RAMPs, REEPs can promote the surface expression of olfactory receptors and modulate their function.86, 87 Interestingly, the Petrova et al study showed that REEP1 was overexpressed 2.5-fold more in LECs than in BECs.47 The broad tissue distribution of olfactory receptors beyond the olfactory epithelium suggests they may have other functions beyond smell. In fact, olfactory receptors have recently been implicated in kidney function and sperm chemotaxis.88, 89 Although openly speculative, it is intriguing to consider that olfactory receptors enriched in lymphatic endothelium might serve as chemosensory factors for mediating developmental lymphangiogenesis or for sensing changes in interstitial fluid composition. Of course, future experiments using genetic engineering approaches in mice need to be undertaken to fully explore this hypothesis.
In conclusion, recent studies in genetically engineered mouse models have led to the identification of several GPCRs important for lymphatic vascular development and function. Given our current lack of pharmacological targets for the treatment of lymphatic vascular diseases like lymphedema, the continued identification and study of GPCRs in lymphatic endothelial cells may eventually lead to major breakthroughs and new pharmacological strategies for the treatment of lymphedema.
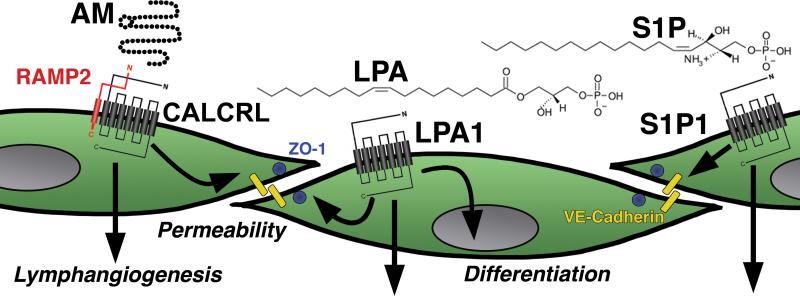
Figure 2. Newly identified GPCRs involved in lymphatic development and function.
Several recent studies have led to the identification of several GPCR signaling paradigms that are required for lymphatic vascular development and function. The receptor complex for adrenomedullin (AM) peptide consists of calcitonin receptor-like receptor (CALCRL) and receptor activity modifying protein 2 (RAMP2). Together, these proteins regulate the proliferation and permeability of lymphatic endothelial cells. The lysophospholipids lysophosphatidic acid (LPA1) and sphingosine-1-phosphate (S1P) signal through their cognate GPCRs, LPA(1−5) and S1P(1−3). Numerous studies demonstrate that lysophospholipid signaling can regulate lymphatic endothelial cell differentiation, proliferation and permeability.
Acknowledgements
The authors wish to thank Dr. Michael Detmar, Zurich, Switzerland for helpful discussions and Kimberly Fritz-Six for her assistance in generation of Figures.
Sources of Funding
This work was supported in part by an AHA Pre-doctoral Fellowship (0815050E) to W.P.D. as well as The Burroughs Wellcome Fund and NIH/NHLBI HL091973 grants to K.M.C.
Footnotes
Disclosures
None.
References
- 1.Gloriam DE, Fredriksson R, Schioth HB. The G protein-coupled receptor subset of the rat genome. BMC Genomics. 2007;8:338. doi: 10.1186/1471-2164-8-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lagerstrom MC, Schioth HB. Structural diversity of G protein-coupled receptors and significance for drug discovery. Nat Rev Drug Discov. 2008;7:339–357. doi: 10.1038/nrd2518. [DOI] [PubMed] [Google Scholar]
- 3.McWayne J, Heiney SP. Psychologic and social sequelae of secondary lymphedema: a review. Cancer. 2005;104:457–466. doi: 10.1002/cncr.21195. [DOI] [PubMed] [Google Scholar]
- 4.Ji RC. Lymphatic endothelial cells, lymphedematous lymphangiogenesis, and molecular control of edema formation. Lymphat Res Biol. 2008;6:123–137. doi: 10.1089/lrb.2008.1005. [DOI] [PubMed] [Google Scholar]
- 5.Hayes SC, Janda M, Cornish B, Battistutta D, Newman B. Lymphedema after breast cancer: incidence, risk factors, and effect on upper body function. J Clin Oncol. 2008;26:3536–3542. doi: 10.1200/JCO.2007.14.4899. [DOI] [PubMed] [Google Scholar]
- 6.Norman SA, Localio AR, Potashnik SL, Simoes Torpey HA, Kallan MJ, Weber AL, Miller LT, Demichele A, Solin LJ. Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. J Clin Oncol. 2009;27:390–397. doi: 10.1200/JCO.2008.17.9291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wynd S, Melrose WD, Durrheim DN, Carron J, Gyapong M. Understanding the community impact of lymphatic filariasis: a review of the sociocultural literature. Bull World Health Organ. 2007;85:493–498. doi: 10.2471/BLT.06.031047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rockson SG. Diagnosis and management of lymphatic vascular disease. J Am Coll Cardiol. 2008;52:799–806. doi: 10.1016/j.jacc.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Ko DS, Lerner R, Klose G, Cosimi AB. Effective treatment of lymphedema of the extremities. Arch Surg. 1998;133:452–458. doi: 10.1001/archsurg.133.4.452. [DOI] [PubMed] [Google Scholar]
- 10.Brorson H, Ohlin K, Olsson G, Langstrom G, Wiklund I, Svensson H. Quality of life following liposuction and conservative treatment of arm lymphedema. Lymphology. 2006;39:8–25. [PubMed] [Google Scholar]
- 11.Szuba A, Rockson SG. Lymphedema: anatomy, physiology and pathogenesis. Vasc Med. 1997;2:321–326. doi: 10.1177/1358863X9700200408. [DOI] [PubMed] [Google Scholar]
- 12.Damstra RJ, Voesten HG, van Schelven WD, van der Lei B. Lymphatic venous anastomosis (LVA) for treatment of secondary arm lymphedema. A prospective study of 11 LVA procedures in 10 patients with breast cancer related lymphedema and a critical review of the literature. Breast Cancer Res Treat. 2009;113:199–206. doi: 10.1007/s10549-008-9932-5. [DOI] [PubMed] [Google Scholar]
- 13.Badger C, Preston N, Seers K, Mortimer P. Benzo-pyrones for reducing and controlling lymphoedema of the limbs. Cochrane Database Syst Rev. 2004:CD003140. doi: 10.1002/14651858.CD003140.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Casley-Smith JR, Morgan RG, Piller NB. Treatment of lymphedema of the arms and legs with 5,6-benzo-[alpha]-pyrone. N Engl J Med. 1993;329:1158–1163. doi: 10.1056/NEJM199310143291604. [DOI] [PubMed] [Google Scholar]
- 15.Knight KR, Vairo G, Hamilton JA, Lepore DA. Coumarins: macrophage proteinase production and pinocytosis. Res Exp Med (Berl) 1992;192:99–103. doi: 10.1007/BF02576263. [DOI] [PubMed] [Google Scholar]
- 16.Loprinzi CL, Sloan J, Kugler J. Coumarin-induced hepatotoxicity. J Clin Oncol. 1997;15:3167–3168. doi: 10.1200/JCO.1997.15.9.3167. [DOI] [PubMed] [Google Scholar]
- 17.Bruns F, Micke O, Bremer M. Current status of selenium and other treatments for secondary lymphedema. J Support Oncol. 2003;1:121–130. [PubMed] [Google Scholar]
- 18.Michael E, Malecela MN, Zervos M, Kazura JW. Global eradication of lymphatic filariasis: the value of chronic disease control in parasite elimination programmes. PLoS ONE. 2008;3:e2936. doi: 10.1371/journal.pone.0002936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karkkainen MJ, Saaristo A, Jussila L, Karila KA, Lawrence EC, Pajusola K, Bueler H, Eichmann A, Kauppinen R, Kettunen MI, Yla-Herttuala S, Finegold DN, Ferrell RE, Alitalo K. A model for gene therapy of human hereditary lymphedema. Proc Natl Acad Sci U S A. 2001;98:12677–12682. doi: 10.1073/pnas.221449198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saaristo A, Tammela T, Timonen J, Yla-Herttuala S, Tukiainen E, Asko-Seljavaara S, Alitalo K. Vascular endothelial growth factor-C gene therapy restores lymphatic flow across incision wounds. Faseb J. 2004;18:1707–1709. doi: 10.1096/fj.04-1592fje. [DOI] [PubMed] [Google Scholar]
- 21.Szuba A, Skobe M, Karkkainen MJ, Shin WS, Beynet DP, Rockson NB, Dakhil N, Spilman S, Goris ML, Strauss HW, Quertermous T, Alitalo K, Rockson SG. Therapeutic lymphangiogenesis with human recombinant VEGF-C. Faseb J. 2002;16:1985–1987. doi: 10.1096/fj.02-0401fje. [DOI] [PubMed] [Google Scholar]
- 22.Tammela T, Saaristo A, Holopainen T, Lyytikka J, Kotronen A, Pitkonen M, Abo-Ramadan U, Yla-Herttuala S, Petrova TV, Alitalo K. Therapeutic differentiation and maturation of lymphatic vessels after lymph node dissection and transplantation. Nat Med. 2007;13:1458–1466. doi: 10.1038/nm1689. [DOI] [PubMed] [Google Scholar]
- 23.Yoon YS, Murayama T, Gravereaux E, Tkebuchava T, Silver M, Curry C, Wecker A, Kirchmair R, Hu CS, Kearney M, Ashare A, Jackson DG, Kubo H, Isner JM, Losordo DW. VEGF-C gene therapy augments postnatal lymphangiogenesis and ameliorates secondary lymphedema. J Clin Invest. 2003;111:717–725. doi: 10.1172/JCI15830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cao R, Eriksson A, Kubo H, Alitalo K, Cao Y, Thyberg J. Comparative evaluation of FGF-2-, VEGF-A-, and VEGF-C-induced angiogenesis, lymphangiogenesis, vascular fenestrations, and permeability. Circ Res. 2004;94:664–670. doi: 10.1161/01.RES.0000118600.91698.BB. [DOI] [PubMed] [Google Scholar]
- 25.Saito Y, Nakagami H, Morishita R, Takami Y, Kikuchi Y, Hayashi H, Nishikawa T, Tamai K, Azuma N, Sasajima T, Kaneda Y. Transfection of human hepatocyte growth factor gene ameliorates secondary lymphedema via promotion of lymphangiogenesis. Circulation. 2006;114:1177–1184. doi: 10.1161/CIRCULATIONAHA.105.602953. [DOI] [PubMed] [Google Scholar]
- 26.Jurisic G, Detmar M. Lymphatic endothelium in health and disease. Cell Tissue Res. 2009;335:97–108. doi: 10.1007/s00441-008-0644-2. [DOI] [PubMed] [Google Scholar]
- 27.Maby-El Hajjami H, Petrova TV. Developmental and pathological lymphangiogenesis: from models to human disease. Histochem Cell Biol. 2008;130:1063–1078. doi: 10.1007/s00418-008-0525-5. [DOI] [PubMed] [Google Scholar]
- 28.Oliver G, Srinivasan RS. Lymphatic vasculature development: current concepts. Ann N Y Acad Sci. 2008;1131:75–81. doi: 10.1196/annals.1413.006. [DOI] [PubMed] [Google Scholar]
- 29.Francois M, Caprini A, Hosking B, Orsenigo F, Wilhelm D, Browne C, Paavonen K, Karnezis T, Shayan R, Downes M, Davidson T, Tutt D, Cheah KS, Stacker SA, Muscat GE, Achen MG, Dejana E, Koopman P. Sox18 induces development of the lymphatic vasculature in mice. Nature. 2008;456:643–647. doi: 10.1038/nature07391. [DOI] [PubMed] [Google Scholar]
- 30.Wigle JT, Oliver G. Prox1 function is required for the development of the murine lymphatic system. Cell. 1999;98:769–778. doi: 10.1016/s0092-8674(00)81511-1. [DOI] [PubMed] [Google Scholar]
- 31.Karkkainen MJ, Haiko P, Sainio K, Partanen J, Taipale J, Petrova TV, Jeltsch M, Jackson DG, Talikka M, Rauvala H, Betsholtz C, Alitalo K. Vascular endothelial growth factor C is required for sprouting of the first lymphatic vessels from embryonic veins. Nat Immunol. 2004;5:74–80. doi: 10.1038/ni1013. [DOI] [PubMed] [Google Scholar]
- 32.Abtahian F, Guerriero A, Sebzda E, Lu MM, Zhou R, Mocsai A, Myers EE, Huang B, Jackson DG, Ferrari VA, Tybulewicz V, Lowell CA, Lepore JJ, Koretzky GA, Kahn ML. Regulation of blood and lymphatic vascular separation by signaling proteins SLP-76 and Syk. Science. 2003;299:247–251. doi: 10.1126/science.1079477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ichise H, Ichise T, Ohtani O, Yoshida N. Phospholipase C{gamma}2 is necessary for separation of blood and lymphatic vasculature in mice. Development. 2009;136:191–195. doi: 10.1242/dev.025353. [DOI] [PubMed] [Google Scholar]
- 34.Taniguchi K, Kohno R, Ayada T, Kato R, Ichiyama K, Morisada T, Oike Y, Yonemitsu Y, Maehara Y, Yoshimura A. Spreds are essential for embryonic lymphangiogenesis by regulating vascular endothelial growth factor receptor 3 signaling. Mol Cell Biol. 2007;27:4541–4550. doi: 10.1128/MCB.01600-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sexton PM, Morfis M, Tilakaratne N, Hay DL, Udawela M, Christopoulos G, Christopoulos A. Complexing receptor pharmacology: modulation of family B G protein-coupled receptor function by RAMPs. Ann N Y Acad Sci. 2006;1070:90–104. doi: 10.1196/annals.1317.076. [DOI] [PubMed] [Google Scholar]
- 36.McLatchie LM, Fraser NJ, Main MJ, Wise A, Brown J, Thompson N, Solari R, Lee MG, Foord SM. RAMPs regulate the transport and ligand specificity of the calcitonin-receptor-like receptor. Nature. 1998;393:333–339. doi: 10.1038/30666. [DOI] [PubMed] [Google Scholar]
- 37.Bell D, McDermott BJ. Intermedin (adrenomedullin-2): a novel counter-regulatory peptide in the cardiovascular and renal systems. Br J Pharmacol. 2008;153(Suppl 1):S247–262. doi: 10.1038/sj.bjp.0707494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Doods H, Arndt K, Rudolf K, Just S. CGRP antagonists: unravelling the role of CGRP in migraine. Trends Pharmacol Sci. 2007;28:580–587. doi: 10.1016/j.tips.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 39.Caron KM, Smithies O. Extreme hydrops fetalis and cardiovascular abnormalities in mice lacking a functional Adrenomedullin gene. Proc Natl Acad Sci U S A. 2001;98:615–619. doi: 10.1073/pnas.021548898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dackor R, Fritz-Six K, Smithies O, Caron K. Receptor activity-modifying proteins 2 and 3 have distinct physiological functions from embryogenesis to old age. J Biol Chem. 2007;282:18094–18099. doi: 10.1074/jbc.M703544200. [DOI] [PubMed] [Google Scholar]
- 41.Dackor RT, Fritz-Six K, Dunworth WP, Gibbons CL, Smithies O, Caron KM. Hydrops fetalis, cardiovascular defects, and embryonic lethality in mice lacking the calcitonin receptor-like receptor gene. Mol Cell Biol. 2006;26:2511–2518. doi: 10.1128/MCB.26.7.2511-2518.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fritz-Six KL, Dunworth WP, Li M, Caron KM. Adrenomedullin signaling is necessary for murine lymphatic vascular development. J Clin Invest. 2008;118:40–50. doi: 10.1172/JCI33302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jin D, Harada K, Ohnishi S, Yamahara K, Kangawa K, Nagaya N. Adrenomedullin induces lymphangiogenesis and ameliorates secondary lymphoedema. Cardiovasc Res. 2008;80:339–345. doi: 10.1093/cvr/cvn228. [DOI] [PubMed] [Google Scholar]
- 44.Temmesfeld-Wollbruck B, Hocke AC, Suttorp N, Hippenstiel S. Adrenomedullin and endothelial barrier function. Thromb Haemost. 2007;98:944–951. doi: 10.1160/th07-02-0128. [DOI] [PubMed] [Google Scholar]
- 45.Nagaya N, Mori H, Murakami S, Kangawa K, Kitamura S. Adrenomedullin: angiogenesis and gene therapy. Am J Physiol Regul Integr Comp Physiol. 2005;288:R1432–1437. doi: 10.1152/ajpregu.00662.2004. [DOI] [PubMed] [Google Scholar]
- 46.Hirakawa S, Hong YK, Harvey N, Schacht V, Matsuda K, Libermann T, Detmar M. Identification of vascular lineage-specific genes by transcriptional profiling of isolated blood vascular and lymphatic endothelial cells. Am J Pathol. 2003;162:575–586. doi: 10.1016/S0002-9440(10)63851-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Petrova TV, Makinen T, Makela TP, Saarela J, Virtanen I, Ferrell RE, Finegold DN, Kerjaschki D, Yla-Herttuala S, Alitalo K. Lymphatic endothelial reprogramming of vascular endothelial cells by the Prox-1 homeobox transcription factor. Embo J. 2002;21:4593–4599. doi: 10.1093/emboj/cdf470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pio R, Martinez A, Unsworth EJ, Kowalak JA, Bengoechea JA, Zipfel PF, Elsasser TH, Cuttitta F. Complement factor H is a serum-binding protein for adrenomedullin, and the resulting complex modulates the bioactivities of both partners. J Biol Chem. 2001;276:12292–12300. doi: 10.1074/jbc.M007822200. [DOI] [PubMed] [Google Scholar]
- 49.Wick N, Saharinen P, Saharinen J, Gurnhofer E, Steiner CW, Raab I, Stokic D, Giovanoli P, Buchsbaum S, Burchard A, Thurner S, Alitalo K, Kerjaschki D. Transcriptomal comparison of human dermal lymphatic endothelial cells ex vivo and in vitro. Physiol Genomics. 2007;28:179–192. doi: 10.1152/physiolgenomics.00037.2006. [DOI] [PubMed] [Google Scholar]
- 50.Czyzyk TA, Ning Y, Hsu MS, Peng B, Mains RE, Eipper BA, Pintar JE. Deletion of peptide amidation enzymatic activity leads to edema and embryonic lethality in the mouse. Dev Biol. 2005;287:301–313. doi: 10.1016/j.ydbio.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 51.Dunworth WP, Fritz-Six KL, Caron KM. Adrenomedullin stabilizes the lymphatic endothelial barrier in vitro and in vivo. Peptides. 2008;29:2243–2249. doi: 10.1016/j.peptides.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rivera R, Chun J. Biological effects of lysophospholipids. Rev Physiol Biochem Pharmacol. 2008;160:25–46. doi: 10.1007/112_0507. [DOI] [PubMed] [Google Scholar]
- 53.Skoura A, Hla T. Lysophospholipid receptors in vertebrate development, physiology and pathology. J Lipid Res. 2008 doi: 10.1194/jlr.R800047-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eichholtz T, Jalink K, Fahrenfort I, Moolenaar WH. The bioactive phospholipid lysophosphatidic acid is released from activated platelets. Biochem J. 1993;291(Pt 3):677–680. doi: 10.1042/bj2910677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yatomi Y, Ruan F, Ohta J, Welch RJ, Hakomori S, Igarashi Y. Quantitative measurement of sphingosine 1-phosphate in biological samples by acylation with radioactive acetic anhydride. Anal Biochem. 1995;230:315–320. doi: 10.1006/abio.1995.1480. [DOI] [PubMed] [Google Scholar]
- 56.Hla T. Physiological and pathological actions of sphingosine 1-phosphate. Semin Cell Dev Biol. 2004;15:513–520. doi: 10.1016/j.semcdb.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 57.Lee H, Goetzl EJ, An S. Lysophosphatidic acid and sphingosine 1-phosphate stimulate endothelial cell wound healing. Am J Physiol Cell Physiol. 2000;278:C612–618. doi: 10.1152/ajpcell.2000.278.3.C612. [DOI] [PubMed] [Google Scholar]
- 58.Lee MJ, Thangada S, Claffey KP, Ancellin N, Liu CH, Kluk M, Volpi M, Sha'afi RI, Hla T. Vascular endothelial cell adherens junction assembly and morphogenesis induced by sphingosine-1-phosphate. Cell. 1999;99:301–312. doi: 10.1016/s0092-8674(00)81661-x. [DOI] [PubMed] [Google Scholar]
- 59.Panetti TS. Differential effects of sphingosine 1-phosphate and lysophosphatidic acid on endothelial cells. Biochim Biophys Acta. 2002;1582:190–196. doi: 10.1016/s1388-1981(02)00155-5. [DOI] [PubMed] [Google Scholar]
- 60.Grigorova IL, Schwab SR, Phan TG, Pham TH, Okada T, Cyster JG. Cortical sinus probing, S1P1-dependent entry and flow-based capture of egressing T cells. Nat Immunol. 2009;10:58–65. doi: 10.1038/ni.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ledgerwood LG, Lal G, Zhang N, Garin A, Esses SJ, Ginhoux F, Merad M, Peche H, Lira SA, Ding Y, Yang Y, He X, Schuchman EH, Allende ML, Ochando JC, Bromberg JS. The sphingosine 1-phosphate receptor 1 causes tissue retention by inhibiting the entry of peripheral tissue T lymphocytes into afferent lymphatics. Nat Immunol. 2008;9:42–53. doi: 10.1038/ni1534. [DOI] [PubMed] [Google Scholar]
- 62.Schwab SR, Cyster JG. Finding a way out: lymphocyte egress from lymphoid organs. Nat Immunol. 2007;8:1295–1301. doi: 10.1038/ni1545. [DOI] [PubMed] [Google Scholar]
- 63.Wei SH, Rosen H, Matheu MP, Sanna MG, Wang SK, Jo E, Wong CH, Parker I, Cahalan MD. Sphingosine 1-phosphate type 1 receptor agonism inhibits transendothelial migration of medullary T cells to lymphatic sinuses. Nat Immunol. 2005;6:1228–1235. doi: 10.1038/ni1269. [DOI] [PubMed] [Google Scholar]
- 64.Ohta H, Sato K, Murata N, Damirin A, Malchinkhuu E, Kon J, Kimura T, Tobo M, Yamazaki Y, Watanabe T, Yagi M, Sato M, Suzuki R, Murooka H, Sakai T, Nishitoba T, Im DS, Nochi H, Tamoto K, Tomura H, Okajima F. Ki16425, a subtype-selective antagonist for EDG-family lysophosphatidic acid receptors. Mol Pharmacol. 2003;64:994–1005. doi: 10.1124/mol.64.4.994. [DOI] [PubMed] [Google Scholar]
- 65.Sanna MG, Wang SK, Gonzalez-Cabrera PJ, Don A, Marsolais D, Matheu MP, Wei SH, Parker I, Jo E, Cheng WC, Cahalan MD, Wong CH, Rosen H. Enhancement of capillary leakage and restoration of lymphocyte egress by a chiral S1P1 antagonist in vivo. Nat Chem Biol. 2006;2:434–441. doi: 10.1038/nchembio804. [DOI] [PubMed] [Google Scholar]
- 66.Visentin B, Vekich JA, Sibbald BJ, Cavalli AL, Moreno KM, Matteo RG, Garland WA, Lu Y, Yu S, Hall HS, Kundra V, Mills GB, Sabbadini RA. Validation of an anti-sphingosine-1-phosphate antibody as a potential therapeutic in reducing growth, invasion, and angiogenesis in multiple tumor lineages. Cancer Cell. 2006;9:225–238. doi: 10.1016/j.ccr.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 67.Kappos L, Antel J, Comi G, Montalban X, O'Connor P, Polman CH, Haas T, Korn AA, Karlsson G, Radue EW. Oral fingolimod (FTY720) for relapsing multiple sclerosis. N Engl J Med. 2006;355:1124–1140. doi: 10.1056/NEJMoa052643. [DOI] [PubMed] [Google Scholar]
- 68.Mandala S, Hajdu R, Bergstrom J, Quackenbush E, Xie J, Milligan J, Thornton R, Shei GJ, Card D, Keohane C, Rosenbach M, Hale J, Lynch CL, Rupprecht K, Parsons W, Rosen H. Alteration of lymphocyte trafficking by sphingosine-1-phosphate receptor agonists. Science. 2002;296:346–349. doi: 10.1126/science.1070238. [DOI] [PubMed] [Google Scholar]
- 69.O'Connor P, Comi G, Montalban X, Antel J, Radue EW, de Vera A, Pohlmann H, Kappos L. Oral fingolimod (FTY720) in multiple sclerosis: two-year results of a phase II extension study. Neurology. 2009;72:73–79. doi: 10.1212/01.wnl.0000338569.32367.3d. [DOI] [PubMed] [Google Scholar]
- 70.Salvadori M, Budde K, Charpentier B, Klempnauer J, Nashan B, Pallardo LM, Eris J, Schena FP, Eisenberger U, Rostaing L, Hmissi A, Aradhye S. FTY720 versus MMF with cyclosporine in de novo renal transplantation: a 1-year, randomized controlled trial in Europe and Australasia. Am J Transplant. 2006;6:2912–2921. doi: 10.1111/j.1600-6143.2006.01552.x. [DOI] [PubMed] [Google Scholar]
- 71.van der Giet M, Tolle M, Kleuser B. Relevance and potential of sphingosine-1-phosphate in vascular inflammatory disease. Biol Chem. 2008;389:1381–1390. doi: 10.1515/BC.2008.165. [DOI] [PubMed] [Google Scholar]
- 72.Lee SJ, Chan TH, Chen TC, Liao BK, Hwang PP, Lee H. LPA1 is essential for lymphatic vessel development in zebrafish. Faseb J. 2008;22:3706–3715. doi: 10.1096/fj.08-106088. [DOI] [PubMed] [Google Scholar]
- 73.Lin CI, Chen CN, Huang MT, Lee SJ, Lin CH, Chang CC, Lee H. Lysophosphatidic acid upregulates vascular endothelial growth factor-C and tube formation in human endothelial cells through LPA(1/3), COX-2, and NF-kappaB activation- and EGFR transactivation-dependent mechanisms. Cell Signal. 2008;20:1804–1814. doi: 10.1016/j.cellsig.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 74.Lin CI, Chen CN, Huang MT, Lee SJ, Lin CH, Chang CC, Lee H. Lysophosphatidic acid up-regulates vascular endothelial growth factor-C and lymphatic marker expressions in human endothelial cells. Cell Mol Life Sci. 2008;65:2740–2751. doi: 10.1007/s00018-008-8314-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Contos JJ, Fukushima N, Weiner JA, Kaushal D, Chun J. Requirement for the lpA1 lysophosphatidic acid receptor gene in normal suckling behavior. Proc Natl Acad Sci U S A. 2000;97:13384–13389. doi: 10.1073/pnas.97.24.13384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Contos JJ, Ishii I, Fukushima N, Kingsbury MA, Ye X, Kawamura S, Brown JH, Chun J. Characterization of lpa(2) (Edg4) and lpa(1)/lpa(2) (Edg2/Edg4) lysophosphatidic acid receptor knockout mice: signaling deficits without obvious phenotypic abnormality attributable to lpa(2). Mol Cell Biol. 2002;22:6921–6929. doi: 10.1128/MCB.22.19.6921-6929.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ye X, Hama K, Contos JJ, Anliker B, Inoue A, Skinner MK, Suzuki H, Amano T, Kennedy G, Arai H, Aoki J, Chun J. LPA3-mediated lysophosphatidic acid signalling in embryo implantation and spacing. Nature. 2005;435:104–108. doi: 10.1038/nature03505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.van Meeteren LA, Ruurs P, Stortelers C, Bouwman P, van Rooijen MA, Pradere JP, Pettit TR, Wakelam MJ, Saulnier-Blache JS, Mummery CL, Moolenaar WH, Jonkers J. Autotaxin, a secreted lysophospholipase D, is essential for blood vessel formation during development. Mol Cell Biol. 2006;26:5015–5022. doi: 10.1128/MCB.02419-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yoon CM, Hong BS, Moon HG, Lim S, Suh PG, Kim YK, Chae CB, Gho YS. Sphingosine-1-phosphate promotes lymphangiogenesis by stimulating S1P1/Gi/PLC/Ca2+ signaling pathways. Blood. 2008;112:1129–1138. doi: 10.1182/blood-2007-11-125203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jang C, Koh YJ, Lim NK, Kang HJ, Kim DH, Park SK, Lee GM, Jeon CJ, Koh GY. Angiopoietin-2 exocytosis is stimulated by sphingosine-1-phosphate in human blood and lymphatic endothelial cells. Arterioscler Thromb Vasc Biol. 2009;29:401–407. doi: 10.1161/ATVBAHA.108.172676. [DOI] [PubMed] [Google Scholar]
- 81.Garcia JG, Liu F, Verin AD, Birukova A, Dechert MA, Gerthoffer WT, Bamberg JR, English D. Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement. J Clin Invest. 2001;108:689–701. doi: 10.1172/JCI12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Singer II, Tian M, Wickham LA, Lin J, Matheravidathu SS, Forrest MJ, Mandala S, Quackenbush EJ. Sphingosine-1-phosphate agonists increase macrophage homing, lymphocyte contacts, and endothelial junctional complex formation in murine lymph nodes. J Immunol. 2005;175:7151–7161. doi: 10.4049/jimmunol.175.11.7151. [DOI] [PubMed] [Google Scholar]
- 83.Allende ML, Yamashita T, Proia RL. G-protein-coupled receptor S1P1 acts within endothelial cells to regulate vascular maturation. Blood. 2003;102:3665–3667. doi: 10.1182/blood-2003-02-0460. [DOI] [PubMed] [Google Scholar]
- 84.Liu Y, Wada R, Yamashita T, Mi Y, Deng CX, Hobson JP, Rosenfeldt HM, Nava VE, Chae SS, Lee MJ, Liu CH, Hla T, Spiegel S, Proia RL. Edg-1, the G protein-coupled receptor for sphingosine-1-phosphate, is essential for vascular maturation. J Clin Invest. 2000;106:951–961. doi: 10.1172/JCI10905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kono M, Mi Y, Liu Y, Sasaki T, Allende ML, Wu YP, Yamashita T, Proia RL. The sphingosine-1-phosphate receptors S1P1, S1P2, and S1P3 function coordinately during embryonic angiogenesis. J Biol Chem. 2004;279:29367–29373. doi: 10.1074/jbc.M403937200. [DOI] [PubMed] [Google Scholar]
- 86.Saito H, Kubota M, Roberts RW, Chi Q, Matsunami H. RTP family members induce functional expression of mammalian odorant receptors. Cell. 2004;119:679–691. doi: 10.1016/j.cell.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 87.Bush CF, Hall RA. Olfactory receptor trafficking to the plasma membrane. Cell Mol Life Sci. 2008;65:2289–2295. doi: 10.1007/s00018-008-8028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pluznick JL, Zou DJ, Zhang X, Yan Q, Rodriguez-Gil DJ, Eisner C, Wells E, Greer CA, Wang T, Firestein S, Schnermann J, Caplan MJ. Functional expression of the olfactory signaling system in the kidney. Proc Natl Acad Sci U S A. 2009;106:2059–2064. doi: 10.1073/pnas.0812859106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Spehr M, Hatt H. A potential role of odorant receptor agonists and antagonists in the treatment of infertility and contraception. Curr Opin Investig Drugs. 2005;6:364–368. [PubMed] [Google Scholar]