Abstract
Cameroon lacks the capacity for routine Pneumocystis pneumonia (PcP) diagnosis thus, the prevalence of Cameroonian exposure to this microbe is unknown. It is known that Pneumocystis infecting different mammalian host species represent diverse phylogenetic backgrounds and are now designated as separate species. The highly sensitive nature of ELISA and the specificity afforded by using human-derived P. jirovecii Msg peptides has been shown to be useful for serological analysis of human sera. Thus, sera from patients in Yaoundé, the capital city of Cameroon, were analyzed for anti-P. jirovecii antibodies by enzyme-linked immunosorbent assay (ELISA) using three recombinant major surface glycoprotein (Msg) peptide fragments, MsgA1, MsgB, and MsgC1. Based on serum recognition of one or more of the three fragments, 82% of the total samples analyzed was positive for antibodies to P. jirovecii Msg, indicating high prevalence of P. jirovecii infection or colonization among Cameroonians. Different Msg fragments appear to be recognized more frequently by sera from different geographic regions of the globe. Antibodies in the Cameroonian serum samples recognized MsgA>MsgC>MsgB, suggesting that different P. jirovecii strains exist in different parts of the world and/or human populations differ in their response to P. jirovecii. Also, HIV+ patients diagnosed with respiratory infections (such as TB and pneumonia) and maintained on trimethoprim/sulfamethoxazol prophylaxis had relatively lower anti-Msg titers. Whether PcP prophylaxis has significant effects on the quality of life among HIV+ patients in Cameroon warrants further investigation.
Keywords: glycoprotein (Msg), recombinant protein, serology, sub-Sahara Africa
1. Introduction
Pneumocystis pneumonia (PcP) is a lung infection that occurs primarily in individuals with a weakened immune system, such as malnourished infants, persons receiving drugs for organ transplants, cancer treatment or HIV/AIDS patients. The disease agent, Pneumocystis, is an opportunistic fungal pathogen that proliferates in the extracellular environment of the immunodeficient mammalian host lung. Pneumocystis organisms are host species-specific; P. jirovecii is the species found in humans and most people become sero-positive for Pneumocystis in early childhood and remain sero-positive throughout adulthood indicating widespread and frequent exposure (Kaneshiro and Smulian, 2007; Morris, 2008; Pifer et al., 1978; Smulian et al., 1993; van Oosterhout et al., 2007; Vargas et al., 2001; Walzer, 1999; Walzer and Cushion, 2004). Pneumocystis is ubiquitous with worldwide distribution, although the presence of P. jirovecii in many underdeveloped countries has not been documented. Reports of P. jirovecii infections in Africa are limited to only a few studies (Aderaye et al., 2007; Aderaye et al., 2008; Bii et al., 2006; Dini et al., 2006; Kazanjian et al., 2005; Robberts et al., 2007; Walzer and Cushion, 2004).
Cameroon, a country in sub-Sahara West Africa, has all the known HIV types and subtypes which are rapidly evolving thus creating genetic heterogeneity of the virus in this country (Lee et al., 2007). Also, epidemic HIV/AIDS is thought to have emerged in this region of Africa by transmission of the virus from chimps to humans (Keele et al., 2006). Since opportunistic infections (OIs) such as microsporidiosis (Nkinin et al., 2007) and PcP are often described as having emerged with AIDS, it is of particular interest to examine OIs among the native population of this country.
Although PcP remains a major immediate cause of death among AIDS patients in the USA and Europe (Morris, 2008; Walzer, 1999; Walzer et al., 2008) pulmonary tuberculosis (TB) is the most serious opportunistic infection in HIV/AIDS in sub-Sahara Africa and pulmonary infections in HIV/AIDS patients there are mostly attributed to TB (Kazanjian et al., 2005). However, most HIV patients in these countries are not tested for PcP due to the invasive and costly clinical procedures required and the lack of diagnostic laboratory capacity. DNA amplification of samples obtained by relatively noninvasive methods (e.g., induced sputum) is not routinely performed in any country and its sensitivity and utility for PcP diagnosis remains questionable. A high rate of exposure to P. jirovecii among Cameroonians would be expected since Pneumocystis colonization is assumed to be nearly universal. However, since PcP in HIV/AIDS patients in Africa is often not reported and the full importance of PcP in Africa is unknown, it is important to collect additional data on seropositivity to this opportunistic pathogen.
The major surface glycoprotein (Msg) is commonly used as antigen for serologic analyses because it is the most antigenic and there is some cross-reactivity between Msg from different Pneumocystis species (Bauer et al., 1993; Kovacs et al.1988; Kovacs et al., 1989; Kutty et al., 2008; Meuwissen et al., 1977; Tanabe et al., 1989; Walzer and Linke, 1987; Walzer and Cushion, 2004; Walzer et al., 2008; Walzer et al., 2009). However, Pneumocystis organisms are host species-specific and Msg molecules in any given Pneumocystis species are diverse (∼80 distinct genes in P. carinii) (Stringer 2007; Stringer and Keely, 2001). Thus, interpretation of earlier serologic studies to evaluate P. jirovecii exposure or infection has been difficult (Bauer et al.,1993; Walzer and Linke, 1987) since antigens used for serology were not those of human-derived P. jirovecii but from organisms isolated from rats (P. carinii), mice (P. murina) or other mammals. The reactivity of anti- P. jirovecii Msg antibodies with P. carinii or P. murina Msg would not be expected to be as high or specific compared to P. jirovecii Msg. The development of a serological test specifically for P. jirovecii antibody titers has clinical and human epidemiological applications and protocols specific for immunoserological assays of P. jirovecii recombinant Msg have been developed (Daly et al., 2002; Daly et al., 2004; Daly et al., 2006; Daly et al., in press; Kovacs et al., 1989; Walzer et al., 2009). An ELISA protocol has been developed employing three overlapping recombinant Msg fragments (MsgA1, MsgB, MsgC1) that span the entire length of a P. jirovecii Msg. In the present study, we analyzed the reactivity of serum samples from subpopulations in Cameroon to three recombinant P. jirovecii Msg fragments, MsgA1, MsgB and MsgC1.
2. Materials and methods
2.1. Serum samples
A cross-sectional study was performed on sera from outpatients visiting clinics and hospitals in Yaoundé, the capital city of Cameroon. There were 349 randomly obtained samples from that were made available of which 175 tested positive for HIV+ and 171 that were HIV-; discrepant HIV status were found for 3 samples. Serum samples were obtained between January and June, 2004 from either (i) the Jamot Tuberculosis Hospital (JTH) which serves the general population but specializes in tuberculosis (TB) treatment, (ii) the Etoug-Ebe Baptist Health Center (EBC), an outpatient clinic that serves the general population and also runs a prenatal counseling center for pregnant women, and (iii) the Espoir HIV Clinic (EC), a privately run clinic restricted to HIV/AIDS patients. People from most regions of Cameroon are treated at health institutions in the capital city of Yaoundé hence serum samples analyzed in this study were not only from patients living in this city. When samples were collected, some HIV+ patients in public health institutions in Cameroon were under HAART but drugs were often taken sporadically and some people discontinued this therapy.
Approximately 70% of EC patients are maintained on trimethoprim/sulfamethoxazole (TMP/SMZ) for prophylaxis against opportunistic infections (Victor Anomah Ngu, personal communication). Data for PcP prophylaxis was not available for JTH and EBC patients. EC is known for its practice of a controversial ‘auto-biotherapy’, a procedure by which a preparation is made from the HIV+ patient’s blood then injected back into that donor using a schedule of daily and then monthly boosters (Abalaka, 2004; Ngu et al., 2002; Ngu et al., 2007; Lehner, 2005; Spier, 2004). It is claimed that this therapy reduces HIV load and has converted a few HIV+ patients to sero-negativity for the virus (Ngu et al., 2002; Ngu et al., 2007). This controversial treatment is contested by many in the Cameroon scientific community but its practice is widely accepted in the country.
Serum samples and other demographic data (gender, age, occupation, residence, CD4+ counts (available only for EC patients); respiratory infections (bacterial pneumonia, pulmonary TB) were obtained from patients at the three health institutions. Approvals for obtaining serum samples were obtained from all source institutions and from the University of Cincinnati Institutional Review Board. The samples were preserved in 15% (w/v) sodium azide, dispensed into aliquots and stored at -20 °C until analyzed.
2.2. Isolation and expression of Msg fragments
Recombinant Msg fragments were designed to minimize errors that could occur from cloning and expressing entire large Msg proteins. Overlapping fragments help minimize eliminating potential amino acid sequence epitopes. The design and preparation of P. jirovecii recombinant Msg fragments used in this study (Fig. 1) were as previously described. These and several other recombinant Msg fragments have been used in ELISA studies to determine reactivity to human sera obtained from HIV+ and HIV- donors in the USA, Europe, South Korea and South Africa (Daly et al., 2002; Daly et al., 2004; Daly et al., 2006; Daly et al., in press). Since Msg molecules are coded by a multicopy gene family consisting of 50--100 copies in P. jirovecii (Kutty et al., 2008; Stringer, 2007) oligonucleotides were designed based on the known sequences of msg genes of P. jirovecii and are specific for the conserved regions of these genes. The oligonucleotides were used in PCR with DNA isolated from P. jirovecii-infected human lung as template and Amplitaq enzyme (Applied Biosystems, Foster City, CA) to generate msg gene segments. The PCR products were cloned into the pCR 2.1-TOPO vector (Invitrogen, Madison, WI) for restriction mapping and nucleotide sequencing, and were then inserted into the pET30 vector (Novagen, Madison, WI) in the correct orientation for expression in Escherichia coli of recombinant Msg peptides. The recombinant peptides were expressed in E. coli inclusion bodies and were purified by standard methods as previously described (Daly et al., 2002; Daly et al., 2004; Daly et al., 2006; Daly et al., in press). Briefly, bacterial cultures expressing recombinant proteins were harvested by centrifugation, the cell pellet was sonicated and washed three times in binding buffer without urea (5 mM imidazole, 0.5 M NaCl, and 20 mM Tris-HCl, pH 7.9), and the final pellet was dissolved in binding buffer containing 6 M urea. The recombinant peptides were purified by affinity chromatography using HIS-binding resin (Novagen, Madison, WI), with the urea being removed during the wash stages. Eluted proteins were dialyzed overnight against PBS (pH 7.4) and aliquots were frozen at -20 °C until used. Recombinant protein expressed from the pET30 vector without insert was used as a control antigen. Protein concentration was determined by A280 nm using a standard curve generated with bovine serum albumen.
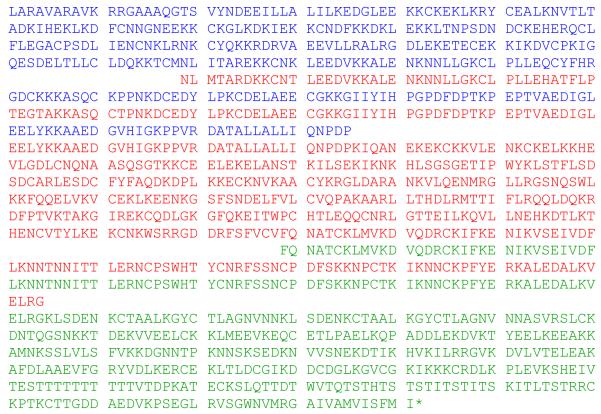
Fig. 1.
Predicted amino acid sequence of recombinant P. jirovecii Msg fragments used in ELISA in this study. Blue, MsgA1; red, MsgB; green, MsgC1. * Indicates stop codon.
2.3. ELISA
ELISA was performed according to methods previously reported (Daly et al., 2004). All serum specimens to be analyzed, as well as a standard reference serum, were tested against the recombinant Msg fragments. Duplicate wells of a 96-well plate were coated with antigen (5 μg/mL, 100 μl/well) in PBS, pH 7.4 overnight; PBS without antigen was used as a negative control. The plates were washed in wash buffer (PBS with 0.05% Tween-20) and treated with blocking buffer (wash buffer with 5% non-fat milk; 200 μL/well) for 2 hr at room temperature. The plates were washed again and human serum, diluted 1/100 and 1/200 in blocking buffer, was added to each well (100 μL/well). The plates were rocked overnight at 4 °C, washed, and HRP-labeled goat anti-human IgG (heavy and light chains) was added to each well (100 μL/well at 1/10,000 dilution in blocking buffer). The plates were incubated at room temperature for 1 hr, washed, and developed by adding 3,3′,5,5′-tetramethylbenzidine (TMB) substrate (100 μL/well). Product color was allowed to develop for 4 min then the reaction was stopped by the addition of 100 μL of H2SO4 (0.18 mol/L) to each well. The color in each well was read at A450 nm, and the mean absorbance (mean OD) for each pair of wells determined. The reactivity of each serum specimen to a given Msg fragment (mean OD Msg) was corrected by subtracting the reactivity of that serum to PBS (mean OD PBS). PBS was selected as negative control as the ability to determine a priori what might constitute appropriate negative control serum samples is indeed problematic. For example, one could argue that it cannot be known for certain that cord blood or serum from infants and naïve young children would not contain antibodies to ubiquitous organisms (antigens) that could have been obtained from maternal sources.
The results were quantified by using a standard serum preparation consisting of 4--6 pooled serum samples with high reactivity to a specific Msg fragment construct (Bishop and Kovacs, 2003). This pooled serum sample was diluted to establish a standard curve, which was generated for each construct on each day of analysis and was used to calculate the units of reactivity to the Msg fragment constructs. Each pooled serum standard was assigned a value of 100 Units of reactivity (100 U) to its target Msg construct in 100 μL of a 1/100 dilution of serum. Test sera were assayed at 1/100--1/200 dilutions that resulted in the linear portion of the standard curves and units of reactivity were calculated and corrected for dilution factors.. Since values were log-transformed, samples with the lowest detectable values in each individual set of assays were assigned the value of 1 U.
2.4. Statistics
Statistical analyses were performed using GraphPad Prism (GraphPad Software, San Diego, CA). Data were log-transformed to approximate normalcy and statistical significance was calculated using unpaired t-tests (Mann-Whitney). P values of <0.05 were considered significant. The Pearson product-moment correlation coefficient was used to identify relationships between various study groups.
3. Results
3.1. Patient HIV status and demographics
A total of 349 serum samples were obtained from three health institutions in Yaoundé; 175 tested positive for HIV-1 & 2; 171 serum samples tested negative for HIV-1 & 2. One sample was designated HIV+ by tests done in Seville against HIV-1 & 2 but HIV- by analysis done in Yaoundé. Also, two were HIV- by the Seville analysis but HIV+ by analysis done in Yaoundé. CD4+ counts were available for all the 104 HIV+ patients at EC but not for patients at the JTH or EBC. This entire study group in the present report included samples from 121 males and 228 females; the average age (mean ± S.D.) of HIV+ patients was 33.7 ± 9.2 and 27.4 ± 10.0 of HIV- patients.
3.2. Reactivities to P. jirovecii recombinant Msg fragments
Reactivity of serum samples to the different Msg fragments varied over a wide range, and the protocol used in this study did not clearly define the lower limits of positive reactivity to the Msg fragments or enable comparisons across Msg fragments. Hence, we conservatively defined a positive reaction as ELISA scores greater than the geometric mean (the nth root of a product of ‘n’ values) for each Msg fragment and that a positive reaction to one or more Msg fragment indicated recognition of the P. jirovecii Msg molecule.
Sera from Cameroonian patients showed overall high recognition of the P. jirovecii recombinant Msg fragments (Table 1). The prevalence of people in this country with antibodies against one or more P. jirovecii Msg fragment was approximately 82% indicating a high percentage of Cameroonians are exposed to P. jirovecii (infection or transient colonization). With respect to those with and without HIV infection, analysis of the total collection of sera obtained in this study indicated that a higher proportion of sera from HIV+ patients recognized one or more Msg fragment compared to sera from HIV- patients (Table 2). HIV+ sera had a relatively higher reactivity to MsgB (4.50 U) compared to sera from HIV- patients (2.99 U) (Table 2; P = 0.0002) whereas HIV+ and HIV- serum reactivity to P. jirovecii MsgA1 and MsgC1 fragments were not significantly different.
Table 1.
Prevalence of antibodies to P. jirovecii recombinant Msg fragments in Cameroonian serum samples
| ELISA-positive (% of total samples)a |
||||
|---|---|---|---|---|
| Patient group | at least 1 fragmentb | MsgA1 | MsgB | MsgC1 |
| Totalc | 82 (286/349) | 60 (210/349) | 49 (171/349) | 55 (192/349) |
| JTH + EBC | 82 (201/245) | 60 (146/245) | 43 (102/245) | 55 (134/245) |
| EC | 81 (84/104) | 52 (54/104) | 50 (52/104) | 58 (60/104) |
With ELISA scores > geometric mean. All samples with ELISA scores >geometric mean (the nth root of a product of all mean OD values; n = number of samples) for the specific Msg fragment antigen were considered positive and therefore indicative of exposure to Pneumocystis.
Sera that reacted higher than the geometric means of one or more recombinant Msg fragment were considered positive for anti-P. jirovecii Msg antibodies.
All serum samples analyzed in this study (JTH + EBC + EC).
Table 2.
Reactivity (Ua) of patient sera from different medical institutions in Cameroon to MsgA1, MsgB, and MsgC1
| Geometric mean of U [95% confidence interval] | ||||
|---|---|---|---|---|
| Patient group | ELISA % seropositiveb | MsgA1 | MsgB | MsgC1 |
| Total | ||||
| HIV- (n = 170) | 79 (134/170) | 17.5 [13.6 - 22.6] | 3.0 [2.5 - 3.5] | 10.1 [8.3 - 12.1] |
| HIV+ (n = 175) | 85 (149/175) | 13.6 [10.4 - 17.7] | 4.5 [3.9 - 5.2] | 10.8 [9.2 - 13.2] |
| Pc | 0.2892 | 0.0002 | 0.4347 | |
| EBC + JTH | ||||
| HIV- (n = 170) | 79 (134/170) | 17.5 [13.6 - 22.6] | 3.0 [2.5 - 3.5] | 10.1 [8.3 - 12.1] |
| HIV+ (n = 71) | 92 (65/71) | 34.1 [24.6 - 47.0] | 4.2 [3.2 - 5.5] | 14.3 [10.7 - 19.1] |
| P | 0.0038 | 0.0334 | 0.0359 | |
| HIV+ | ||||
| EBC + JTH (n = 71) | 92 (65/71) | 34.1 [24.6 - 47.0] | 4.2 [3.2 - 5.5] | 14.3 [10.7 - 19.1] |
| EC (n = 104) | 81 (84/104) | 7.2 [5.15 - 10.19] | 4.7 [4.0 - 5.7] | 9.2 [7.3 - 11.6] |
| P | <0.0001 | 0.3136 | 0.0131 | |
Reactivity units as defined in Material and Methods
Sera that reacted higher than the geometric means of one or more recombinant Msg fragments were considered positive for anti-P. jirovecii Msg antibodies. The geometric mean is used because the data are log transformed.
Significance determined by the Mann-Whitney unpaired t-test. Bolded values indicate statistically significant differences.
Evaluation of patients treated at different health care institutions in Cameroon showed that the HIV+ patients at JTH and EBC had significantly higher antibody titers against all three Msg fragments than HIV- patients at these health institutions (Table 2). Comparing sera from HIV+ patients at JTH and EBC with those from EC (all HIV+), reactivity to MsgA1 and MsgC1 were found to be significantly higher in patients at JTH and EBC.
We also compared the anti-Pneumocystis antibody titers in samples from HIV+ patients that were also clinically diagnosed with TB or pneumonia to those that were not diagnosed with these respiratory infections. The patients from EBC and JTH diagnosed with a respiratory infection had higher antibody titers to all Msg fragments compared to those at EC (Table 3); the difference for MsgA1 was statistically significant. There was a significantly higher reactivity to MsgC1 in sera of HIV- patients without respiratory infection compared to HIV- patients with respiratory infection (P = 0.0199), but the number of samples in the latter group was only 4. Other comparisons of antibody titers in patients with respiratory disease between other subgroups and Msg fragments did not reveal any significant differences.
Table 3.
Reactivity to recombinant P. jirovecii Msg fragments of serum samples from total and HIV+ patients with diagnosed respiratory diseasea at the Etoug-Ebe Baptist Health Center (EBC) and the Jamot Tuberculosis Hospital (JTH) compared to patients at the Espoir HIV Clinic (EC) (geometric mean [95% confidence level]). The geometric mean is used because the data are log transformed
| % seropositiveb | MsgA1 | MsgB | MsgC1 | |
|---|---|---|---|---|
| Total in study (n = 34) | 82 (28/34) | |||
| HIV- (n = 4) | 75 (3/4) | |||
| HIV+(n = 30) | 90 (27/30) | |||
| HIV+ | ||||
| EBC + JTH (n = 13) | 92 (12/13) | 49 [19.9 - 120.8] | 5.8 [2.8 - 12.2] | 19.1 [9.7 - 37.3] |
| Espoir HIV Clinc (n = 17) | 88 (15/17) | 4.8 [2.1 - 10.8] | 5.4 [3.5 - 8.5] | 12.4 [8.8 - 17.3] |
| P | 0.0007 | 1.000 | 0.0753 | |
Tuberculosis or pneumonia.
Sera that reacted higher than the geometric means of one or more recombinant Msg fragment were considered positive for anti-P. jirovecii Msg antibodies.
Significance determined by the Mann-Whitney unpaired t-test. Bolded number indicates the difference is statistically significant.
With the exception of significantly higher antibody titers to MsgA1 in sera from 82 males compared to 162 females at EBC and JTH (P = 0.0186), there were no statistically significant differences between gender in the total study group. CD4+ counts were available only for patients at EC. No statistically significant correlation was observed between the CD4+ counts and serum reactivity to the peptide fragments MsgA1 (r = -0.018; P = 0.427), MsgB (r = -0.079, P = 0.213), and MsgC1 (r = -0.015, P = 0.427) in this patient population.
4. Discussion
4.1. Prevalence of P. jirovecii in Cameroon
Using different analytical methods and organism preparations obtained from infected rodent or human lungs as antigen, a number of studies have indicated ∼76% of human populations are seropositive to P. jirovecii antigens (Walzer and Cushion, 2004). Daly et al. (2002) reported 65% seropositivity for serum samples from South Africa tested by Western blot analysis. Although PcP is not routinely diagnosed in Cameroon, the data obtained in the present study are among the first indicating widespread exposure to P. jirovecii among the Cameroonian population, and hence verifies the ubiquitous distribution of this species worldwide. The 82% prevalence among Cameroonians with anti-P. jirovecii Msg antibodies estimated here are similar to results obtained in a preliminary study using rat-derived P. carinii antigens in Western blot analyses and a separate set of sera from Cameroonians [Nkinin, S.W., Asonganyi, T., Medrano, F.J., Respaldiza, N., Calderón, E. and Kaneshiro, E.S.; 2004. Evidence for Widespread Occurrence of Pneumocystis jirovecii in Cameroon and Spain, 104th General Meetings, American Society for Microbiology, New Orleans, LA.]. In that preliminary study, 86% (51/60) of HIV- and 80% (36/46) of HIV+ sera tested positive for anti-Pneumocystis Msg antibodies. This is the first report in which ELISA data resulting from employing P. jirovecii recombinant Msg has been used to evaluate prevalence of seropositivity to this organism.
Earlier Western blot analysis indicated that the middle fragment MsgB and MsgC located at the C-terminus of a P. jirovecii Msg isoform (Daly et al., 2002) was most frequently recognized by sera from various countries of the world including the USA. More recent ELISA studies on sera from healthy USA donors recognized MsgC>MsgA>MsgB and that patients with prior history of PcP had higher reactivity to MsgC compared to tghose without this history (Daly et al., 2004). A study focusing on MsgC showed differences in reactivity betweenSpanish and USA sera to various isoforms of MsgC (Daly et al., in press). In contrast, the present study of Cameroonian sera indicated that the N-terminal MsgA1 was most frequently recognized. These data suggest that the immunogenicity of different parts of Msg proteins found in Cameroonian P. jirovecii is different from those found in organisms in other regions of the world but similar enough to cross react with these proteins and/or there are differences in human populations with respect to their responses to P. jirovecii Msg molecules.
The low reactivity to MsgB was consistently seen in sera from North America (Daly et al., 2004; Daly et al., 2006). It cannot be ruled out that the ELISA is strongly influenced by the specific Msg molecules expressed in organisms in the human host. Although it is generally agreed that only one Msg is expressed in an individual organism (Stringer and Keely, 2001; Walzer and Linke, 1987) a single host can harbor several Pneumocystis organisms expressing different Msg molecules at any given time (Angus et al., 1996). The high-level reactivity seen in this ELISA indicate that there are sufficiently close similarities in Msg proteins being expressed by individual P. jirovecii organisms in an individual host as well as in different hosts representing human populations worldwide.
4.2. Differences in antibody titers between patients from different health institutions
Serum samples from patients at JTH and EBC had higher antibody titers to P. jirovecii Msg fragments than patients at EC. It is known that approximately 70% of the EC patients are maintained on prophylaxis (TMP/SMZ), which is intended to prevent opportunistic infections such as toxoplasmosis. However, the percentage of HIV+ patients at other institutions (JTH and EBC) that were on prophylaxis was not known but this value is expected to be lower than that of patients attending the private HIV Clinic, EC. If this were the case, the differences observed in anti-P. jirovecii antibody titers between patients at the EC and those at other locations (JTH and EBC) might be explained by the prevention of PcP due to TMP/SMZ prophylaxis among a higher percentage of patients at EC..
Since PcP diagnosis is not readily available in Cameroon health institutions, the results of higher anti-P. jirovecii Msg antibodies observed among HIV+ patients at JTH and EBC co-infected with pneumonia or TB compared to their counterparts at EC might be relevant to health care of these patients in this country. As a high proportion of EC patients are maintained under TMP/SMZ prophylaxis, these data suggest that pulmonary TB and bacterial pneumonia patients who are not under a prophylaxis regimen for opportunistic infections are likely to also harbor yet another lung pathogen, P. jirovecii (Vray et al., 2008). It cannot be ruled out that in cases where pulmonary TB and bacterial pneumonia patients fail therapy for their lung diseases in Cameroon, inclusion of PcP prophylaxis might prove helpful.
Acknowledgments
The authors thank Victor Anomah Ngu and Christopher Kuaban for facilitating serum sample collections and patient information, Enrique Calderón for facilitating HIV status analysis performed in his institution in Seville, Judith V. Koch for assistance with ELISA, and Ken Petren for advise on statistical analyses.
Supported in part by NIAID grants RO1 AI64084 to ESK and RO1 AI062492 and RO1 HL-090335 to PDW, a Sigma Xi research award to SWN, ERA-NET PathoGenoMics Coordination Action of the European Commission, and Consejería de Salud de la Junta de Andalucía #32/02.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abalaka JOA. Attempts to cure and prevent HIV/AIDS in central Nigeria between 1997 and 2002: opening a way to a vaccine-based solution to the problem? Vaccine. 2004;22:3819–3828. doi: 10.1016/j.vaccine.2004.06.033. [DOI] [PubMed] [Google Scholar]
- Aderaye G, Bruchfeld J, Aseffa G, Nigussie Y, Melaku K, Woldeamanuel Y, Lebaard M, Lindquist L. Pneumocystis jiroveci pneumonia and other pulmonary infections in TB smear-negative HIV-positive patients with atypical chest X-ray in Ethiopia. Scand. J. Infect. Dis. 2007;39:1045–1053. doi: 10.1080/00365540701474508. [DOI] [PubMed] [Google Scholar]
- Aderaye G, Woldeamanue Y, Asrat D, Lebbad M, Beser J, Worku A, Fernandez V, Lindquist L. Evaluation of Toluidine Blue O staining for the diagnosis of Pneumocystis jiroveci in expectorated sputum sample and bronchoalveolar lavage from HIV-infected patients in a tertiary care referral center in Ethiopia. Infection. 2008;36:23–243. doi: 10.1007/s15010-007-7191-8. [DOI] [PubMed] [Google Scholar]
- Angus CW, Tu A, Vogel P, Qin M, Kovacs JA. Expression of variants of the major surface glycoprotein of Pneumocystis carinii. J. Exp. Med. 1996;183:1229–1234. doi: 10.1084/jem.183.3.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer NL, Paulsrud JR, Bartlett MS, Smith JW, Wilde CE. Pneumocystis caninii organisms obtained from rats, ferrets, and mice are antigenically different. Infect. Immun. 1993;61:1315–1319. doi: 10.1128/iai.61.4.1315-1319.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bii CC, Kose J, Taguchi H, Amukoye E, Ouko TT, Muita LC, Mugasia O, Wamae N, Kamiya S. Pneumocystis jirovecii and microbiological findings in children with severe pneumonia in Nairobi, Kenya. Int. J. Tuberc. Lung Dis. 2006;10:1286–1291. [PubMed] [Google Scholar]
- Bishop LR, Kovacs JA. Quantitation of anti-Pneumocystis jiroveci antibodies in healthy persons and immunocompromised patients. J. Infect. Dis. 2003;187:1844–1848. doi: 10.1086/375354. [DOI] [PubMed] [Google Scholar]
- Daly KR, Fichtenbaum C, Tanaka R, Linke MJ, Obert R, Thullen TD, Hui MS, Smulian AG, Walzer PD. Serologic responses to epitopes of the major surface glycoprotein of Pneumocystis jiroveci differ in human immunodeficiency virus-infected and uninfected persons. J. Infect. Dis. 2002;186:644–651. doi: 10.1086/341565. [DOI] [PubMed] [Google Scholar]
- Daly KR, Koch J, Levin L, Walzer PD. Enzyme-linked immunosorbent assay and serologic responses to Pneumocystis jiroveci. Emerg. Infect. Dis. 2004;10:848–854. doi: 10.3201/eid1005.030497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly KR, Koch JV, Shire NJ, Levin L, Walzer PD. Human immunodeficiency virus-infected patients with prior Pneumocystis pneumonia exhibit increased serologic reactivity to several major surface glycoprotein clones. Clin. Vaccine Immunol. 2006;13:1071–1078. doi: 10.1128/CVI.00140-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly K, Koch J, Respaldiza N, de la Horra C, Montes-Cano M, Medrano F, Varela J, Calderon E, Walzer P. Geographic variation in serological responses to recombinant Pneumocystis jirovecii major surface glycoprotein antigens. Clin. Microbiol. Infect. 2009 doi: 10.1111/j.1469-0691.2009.02716.x. Mar 21, Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dini L, Du Plessis M, Wong M, Karstaedt A, Fernandez V, Frean J. Prevalence of DHPS polymorphisms associated with sulfa resistance in South African Pneumocystis jirovecii strains. J. Eukaryot. Microbiol. 2006;53(Suppl):S110–S111. doi: 10.1111/j.1550-7408.2006.00193.x. [DOI] [PubMed] [Google Scholar]
- Kaneshiro ES, Smulian AG. Pneumocystis. In: Mehlhorn H, editor. Encyclopedia of Parasitology. Third edition Springer-Verlag; Berlin, Germany: 2007. pp. 1170–1181. [Google Scholar]
- Kazanjian P, Fisk DT, Meshnick SR. Pneumocystis jirovecii pneumonia in AIDS patients in the developing world. In: Walzer PD, Cushion MT, editors. Pneumocystis Pneumonia. Third edition Marcel Dekker; New York, NY: 2005. pp. 435–450. [Google Scholar]
- Keele BF, Van Heuverswyn F, Li Y, Bailes E, Takehisa J, Santiago ML, Bibollet-Ruche F, Chen Y, Wain LV, Liegeois F, Loul S, Ngole EM, Bienvenue Y, Delaporte E, Brookfield JF, Sharp PM, Shaw GM, Peeters M, Hahn BH. Chimpanzee reservoirs of pandemic and nonpandemic HIV-1. Science. 2006;313:523–526. doi: 10.1126/science.1126531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs JS, Halpern JL, Lundgren B, Swan JC, Parrillo JE, Masu H. Monoclonal antibodies to Pneumocystis carinii: identification of specific antigens and characterization of antigenic differences between rat and human isolates. J. Infect. Dis. 1989;915:60–70. doi: 10.1093/infdis/159.1.60. [DOI] [PubMed] [Google Scholar]
- Kovacs JA, Halpern JL, Swan JC, Moss J, Parrillo JE, Masur H. Identification of antigens and antibodies specific for Pneumocystis carinii. J. Immunol. 1988;140:2023–2031. [PubMed] [Google Scholar]
- Kutty G, Maldarell F, Achaz G, Kovacs J,A. Variation in the major surface glycoprotein genes in Pneumocystis jirovecii. J. Infect. Dis. 2008;198:741–749. doi: 10.1086/590433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Wood O, Tang S, Hu J, Machuca A, Kerby S, Awazi B, Vockley C, Hewlett I. Detection of emerging HIV variants in blood donors from urban areas of Cameroon. AIDS Res. Human Retroviruses. 2007;23:1262–1267. doi: 10.1089/aid.2006.0301. [DOI] [PubMed] [Google Scholar]
- Lehner T. Editorial and report by J. O. A. Abalaka. Attempts to cure and prevent HIV/AIDS in central Nigeria between 1997 and 2002: opening a way to a vaccine-based solution to the problem. Vaccine. 2005;23:1093–1094. doi: 10.1016/j.vaccine.2004.11.047. [DOI] [PubMed] [Google Scholar]
- Meuwissen JH, Tauber I, Leeuwenberg AD, Beckers PJ, Sieben M. Parasitologic and serologic observations of infection with Pneumocystis in humans. J. Infect. Dis. 1977;136:43–49. doi: 10.1093/infdis/136.1.43. [DOI] [PubMed] [Google Scholar]
- Morris A. Is there anything new in Pneumocystis jirovecii pneumonia? Changes in P. jirovecii pneumonia over the course of the AIDS epidemic. Clin. Infect. Dis. 2008;46:634–636. doi: 10.1086/526779. [DOI] [PubMed] [Google Scholar]
- Ngu VA, Ambe F, Boma G. Significant reduction in HIV loads in the sera of patients treated with VANHIVAX. J. Cameroon Acad. Sci. 2002;2:7–10. [Google Scholar]
- Ngu V, Besong-Egbe BH, Ambe F, Ngu JA. The conversion of sero-positive to sero-negative following VANHIVAX. J. Cameroon Acad. Sci. 2007;7:17–20. [Google Scholar]
- Nkinin SW, Asonganyi T, Didier ES, Kaneshiro ES. Microsporidian infection is prevalent in healthy people in Cameroon. J. Clin. Microbiol. 2007;45:2841–2846. doi: 10.1128/JCM.00328-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pifer LL, Hughes WT, Stagno S, Woods D. Pneumocystis carinii infection: evidence for high prevalence in normal and immunosuppressed children. Pediatrics. 1978;61:35–41. [PubMed] [Google Scholar]
- Robberts FJL, Liebowitz LD, Chalkley LJ. Polymerase chain reaction detection of Pneumocystis jiroveci: evaluation of 9 assays. Diag. Microbiol. Infect. Dis. 2007;58:385–392. doi: 10.1016/j.diagmicrobio.2007.02.014. [DOI] [PubMed] [Google Scholar]
- Smulian AG, Sullivan DW, Linke MJ, Halsey NA, Quinn TC, MacPhail AP, Hernandez-Avila MS, Hong ST, Walzer PD. Geographic variation in the humoral response to Pneumocystis carinii. J. Infect. Dis. 1993;167:1243–1247. doi: 10.1093/infdis/167.5.1243. [DOI] [PubMed] [Google Scholar]
- Spier RE. Editorial. Jerimiah Abalaka and HIV in Nigeria. Vaccine. 2004;22:3817–3818. doi: 10.1016/j.vaccine.2004.07.003. [DOI] [PubMed] [Google Scholar]
- Stringer JR, Keely P. Genetics of surface antigen expression in Pneumocystis carinii. Infect. Immun. 2001;69:627–639. doi: 10.1128/IAI.69.2.627-639.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringer JR. Antigenic variation in Pneumocystis. J. Eukaryot. Microbiol. 2007;54:8–13. doi: 10.1111/j.1550-7408.2006.00225.x. [DOI] [PubMed] [Google Scholar]
- Tanabe K, Takasaki S, Watanabe J, Kobata A, Egawa K, Nakamura Y. Glycoproteins composed of major surface immunodeterminants of Pneumocystis carinii. Infect. Immun. 1989;57:1363–1368. doi: 10.1128/iai.57.5.1363-1368.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Oosterhout JJ, Laufer MK, Perez MA, Graham SM, Chimbiya N, Thesing PC, Alvarez-Martinez MJ, Wilson PE, Chagomerana M, Zijlstra EE, Taylor TE, Plowe CV, Meshnick SR. Pneumocystis pneumonia in HIV-positive adults, Malawi. Emerg. Infect. Dis. 2007;13:325–328. doi: 10.3201/eid1302.060462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vargas SL, Hughes WT, Santolaya ME, Ulloa AV, Ponce CA, Cabrera CE, Cumsille F, Gigliotti F. Search for primary infection by Pneumocystis carinii in a cohort of normal, healthy infants. Clin. Infect. Dis. 2001;32:855–861. doi: 10.1086/319340. [DOI] [PubMed] [Google Scholar]
- Vray M, Germani Y, Chan S, Duc NH, Sar B, Sarr FD, Bercion R, Rahallison L, Maynard M, L’Her P, Chartier L, Mayaud C. Clinical features and etiology of pneumonia in acid-fast bacillus sputum smear-negative HIV-infected patients hospitalized in Asia and Africa. AIDS. 2008;22:1323–1332. doi: 10.1097/QAD.0b013e3282fdf8bf. [DOI] [PubMed] [Google Scholar]
- Walzer PD. Immunological features of Pneumocystis carinii infection in humans. Clin. Diagn. Lab. Immunol. 1999;6:149–155. doi: 10.1128/cdli.6.2.149-155.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walzer PD, Cushion MT, editors. Lung Biology in Health and Disease. Third edition Vol. 194. Marcel Dekker; New York, NY: 2004. Pneumocystis Pneumonia; p. 715. [Google Scholar]
- Walzer PD, Linke MJ. A comparison of the antigenic characteristics of rat and human Pneumocystis carinii by immunoblotting. J. Immunol. 1987;138:2257–2265. [PubMed] [Google Scholar]
- Walzer PD, Djawe K, Levin L, Daly KR, Koch J, Kingsley L, Witt M, Golub ET, Bream JH, Taiwo B, Morris A. Long-term serologic responses to the Pneumocystis jirovecii major surface glycoprotein in HIV-positive individuals with and without P. jirovecii infection. Clin. Infect. Dis. 2009;46:625–633. doi: 10.1086/597803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walzer PD, Evans HER, Copas AJ, Edwards SG, Grant AD, Miller RF. Early predictors of mortality from Pneumocystis jirovecii pneumonia in HIV-infected patients: 1985-2006. Clin. Infect. Dis. 2008;46:625–633. doi: 10.1086/526778. [DOI] [PMC free article] [PubMed] [Google Scholar]