Abstract
AIM: To study the possible association between chronic pancreatitis (CP) and liver cirrhosis (LC) of alcoholic etiology, after excluding any other causes.
METHODS: One hundred and forty consecutive alcoholic patients were subdivided into three groups: CP (n = 53), LC (n = 57), and asymptomatic alcoholic (n = 30). Clinical, biochemical and morphological characteristics, Child-Pugh index, indocyanine green test, and fecal pancreatic elastase-1 test were assessed.
RESULTS: In patients with cirrhosis, major clinical manifestations of CP such as pancreatic pain and steatorrhea, as well as imaging alterations of CP such as calcifications, duct dilation and pseudocysts were absent; insulin-dependent diabetes was present in 5.3% of cases, and elastase-1 test was altered in only 7%, and severely altered in none. In patients with CP, clinical characteristics of cirrhosis such as ascites, encephalopathy and gastrointestinal hemorrhage were present in one case, Child-Pugh grade > A in 5.7%, and altered indocyanine green test in 1.9% cases. In asymptomatic alcoholism, there was only a non-coincident alteration of elastase-1 test and indocyanine test in 14.8% and 10%, respectively, but other characteristics of cirrhosis or CP were absent. An inverse correlation (r = -0.746) between elastase-1 test and indocyanine test was found in alcoholic patients.
CONCLUSION: There is a scarce coincidence in clinical and morphological alterations among patients with CP or LC of alcoholic etiology, but an inverse correlation between pancreatic and liver function tests. These findings support that these alcoholic diseases evolve in a different manner and have different etiopathogenesis.
Keywords: Alcoholic chronic pancreatitis, Alcoholic liver cirrhosis, Alcoholism, Pancreatic function, Hepatic function
INTRODUCTION
Chronic alcoholism is a well-known etiologic factor associated with chronic and irreversible pancreatic and liver disorders. Excessive alcohol consumption is the most frequent cause of chronic pancreatitis (CP) in Western countries[1]. There is a correlation between increased ethanol consumption over many years and the risk of developing CP[2,3]. Nevertheless, it has recently been estimated that < 5% of alcoholic subjects develop CP[1,4,5]. This low percentage, together with the absence of adequate experimental models of alcoholic CP, suggest that ethanol is only a cofactor in the development of CP, and therefore other predisposing factors may be involved[6].
An excessive consumption of alcohol is also associated with liver cirrhosis (LC), again with a correlation between increased ethanol consumption and the risk of LC[7,8]. The development of LC also requires chronic alcoholism over several years[8,9]. For decades, it was considered that around 10%-35% of subjects with chronic alcoholism developed alcoholic LC[10]. However, more recent prospective studies have shown that the prevalence in alcoholics is indeed much lower, around 2%[7,8], once having excluded the confusing cases of hepatitis B or C[11,12]. Experimental models of chronic alcoholism have not provided insights into the pathophysiological mechanisms responsible for the different outcome in CP and LC[13].
There is still controversy about the frequency of coincidence between CP and LC in alcoholic patients. This lack of coincidence may rely on differences in methodology, retrospective versus prospective studies[14], and evaluated parameters such as clinical[15], functional[16], imaging[17] or histopathological[18,19]. In addition, there are diagnostic difficulties in the initial stages[20], as well as several confounders hindering this question, such as the presence of hepatitis B or C virus[14,19], and age-related pancreatic alterations[21,22].
It is worth noting that pancreatic function is often increased in patients with alcoholic LC, leading to the hypersecretory status of the pancreas[16,23]. Thus, Hayakawa et al[24] have reported that pancreatic secretion, measured with the pancreozymine-secretine test, increases with severity of liver damage in alcoholic liver disease. It has been suggested that this hypersecretory status diminishes protein and calcium concentration in pancreatic juice, protecting against formation of protein plugs and pancreatic stones[16].
In clinical practice, the coincidence of both diseases, LC and CP, is rare[15,24]. Furthermore, these two diseases do not share risk factors apart from alcohol consumption[15]. In alcoholic CP, the duration of chronic alcoholism is shorter than in LC, and liver disease is found at older ages[14]. Nakamura et al[15] have recently assessed the genotypes of alcohol dehydrogenase (ADH), ductal anatomy by endoscopic retrograde cholangiopancreatography (ERCP) and the Child-Pugh classification in Japanese alcoholics, and reported a lack of association between the risk of LC and CP. In addition, no clear genetic predisposition has been found so far in studies of genetic polymorphisms in alcoholic CP[25] and alcoholic LC[26].
To the best of our knowledge, there are no previous studies comparing clinical, functional, morphological and biochemical parameters in alcoholic subjects with a definitive diagnosis of CP or LC. In this study, we therefore aimed to assess the association of CP and LC, both with definitive diagnosis, in subjects with chronic alcoholism, based on clinical, functional and morphological parameters.
MATERIALS AND METHODS
Case-control study with two groups of consecutive patients who attended the University Clinic Hospital of Valencia, Spain for 3 years included: (1) alcoholic CP (n = 53); and (2) alcoholic LC (n = 57). Controls were 30 asymptomatic alcoholic (ASA) patients. The diagnosis of CP was based on the Cambridge and Marseille criteria[27,28]. The diagnosis of cirrhosis was histologically proven in 27 patients and based on compatible clinical, laboratory and ultrasonographic finding in the others[29]. Daily ethanol intake was over 40 g for more than 5 years in alcoholic subjects[7,8] and before entering the study a period of 60 d of alcohol abstinence was required. Exclusion criteria for alcoholic LC were the presence of antigens or antibodies against B or C virus, as well as liver diseases not related to chronic alcoholism such as hemochromatosis or any other causes. Exclusion criteria for CP were the presence of toxic-metabolic (other than alcohol), genetic, autoimmune, and obstructive factors considered as confounders[6]. Other exclusion criteria for the study were gastric or liver surgery, pancreatic surgery prior to diagnosis, and gastrointestinal neoplasia. Smoking was considered when more than 10 cigarettes were consumed daily[30,31].
Characteristic manifestations of LC[13] were assessed in all patients, including hemorrhage in the digestive tract secondary to portal hypertension, ascites, hepatic encephalopathy, alterations of the Quick index, and Child-Pugh index (PI)[32]. PI was classified according to the following scoring system: A (5-6 score), B (7-9 score), and C (10-15 score)[32]. The following characteristic manifestations of CP[27,28] were also assessed in all patients: pancreatic pain, non-insulin-dependent diabetes mellitus (NIDDM), insulin-dependent diabetes mellitus (IDDM), and chronic diarrhea/steatorrhea. Liver function was assessed by indocyanine green clearance test (ICG test). Pancreatic function was assessed by determination of fecal pancreatic elastase-1 test (E1 test) and oral glucose tolerance test (OGTT). The presence of esophageal varices, splenomegaly, portal hypertension, pancreatic calcifications, pseudocysts or alterations of the pancreatic duct were assessed by ultrasonography (US), computer tomography (CT), magnetic resonance cholangiopancreatography (MRCP), or ERCP. Splenomegaly was considered when the size of the spleen was ≥ 135 mm. Portal hypertension was established according to the following criteria: Portal vein diameter > 12 mm and/or presence of esophageal varices and/or splenomegaly. Alterations in the Quick index were established when the international normalized ratio (INR) was higher than 1.2[33].
The ICG test was performed by pulsidensitometry (Limon PC5000, Pusion Medical Systems, Munich RFA). Briefly, ICG was intravenously administered at a dose of 0.5 mg/kg, monitoring the blood concentration of ICG to determine the plasma disappearance rate (PDR, %/min). It was considered that the ICG clearance was altered when PDR was < 15%, and severely altered when PDR was < 10%[34,35].
Pancreatic fecal elastase-E1 activity was determined by ELISA (Pancreatic Elastase stool test, Schebo-Biotech, Giessen RFA). E1 activity was considered altered when it was < 200 μg/g, and severely altered when it was < 100 μg/g[36] in at least two consecutive determinations. Fecal fat was determined by the van de Kamer method[37].
The body mass index (BMI) was measured in all subjects as index of nutritional status. BMI values < 20 were considered malnutrition, whereas values > 28 were considered as indicative of being overweight[38].
Statistical analysis
Proportions for qualitative variables and mean ± SD for quantitative variables were calculated. Means were compared by t test or ANOVA and post-hoc Scheffe test. According to the Kolmogorov-Smirnov test, when quantitative variables did not fit a normal distribution, medians and ranges and consequently Kruskal-Wallis test were used. Qualitative variables were analyzed by χ2 test or Fisher’s exact test when appropriate. Odds ratios (ORs) with 95% confidence intervals (95% CI) were also calculated. Spearman’s rank correlation coefficient between E1 test and indocyanine green test (ICG test) or PI was calculated. P < 0.05 was considered statistically significant.
RESULTS
General characteristics of patients: Alcohol consumption, smoking, and nutritional status
Table 1 shows the general characteristics of each group of subjects. Although the age of patients when entering the study was not different between CP and LC, the age at the moment of diagnosis was significantly lower in CP than LC patients. Most patients were men in all groups, especially in the CP group.
Table 1.
General characteristic of patients with ACP, ALC or ASA
| ACP (n = 53) | ALC (n = 57) | ASA (n = 30) | P | |
| Age at the beginning of the study | 51.8 ± 9.7 | 56.1 ± 9.9 | 49.9 ± 7.9 | CP vs LC, CP vs ASA, NS; LC vs ASA, P = 0.010 |
| Men (%) | 98 | 84 | 70 | CP vs LC, P = 0.011; CP vs ASA, P = 0.001; LC vs ASA, NS |
| Age at diagnosis | 39 ± 9.2 | 51.5 ± 9.6 | - | P = 0.001 |
| Alcohol intake (g/d) | 120 ± (75-250) | 118 (70-255) | 121 (70-400) | NS |
| Years of alcoholism | 20 (10-35) | 25 (10-52) | 18.5 (9-36) | CP vs LC, P = 0.01; LC vs ASA, P = 0.006; CP vs ASA, NS |
| Ethanol, kg of total intake | 876 (273-2920) | 1095 (481-3832) | 965 (229-3358) | NS |
| Smoking | 94.3% | 80.7% | 96.7% | CP vs LC, P = 0.030; CP vs ASA, NS; LC vs ASA, P = 0.035 |
| BMI | 23.4 ± 3.6 | 26.5 ± 4.4 | 24.8 ± 4.6 | CP vs LC, P = 0.001 |
Data are expressed as mean ± SD, percentage or median (minimum-maximum). NS: Not significant.
Regarding the alcohol consumption, the daily alcohol intake did not differ among groups. The percentages of heavy drinkers (daily consumption > 150 g) were 30.2%, 33.3%, and 45.0% for CP, LC and ASA groups, respectively, without significant differences among the groups. The duration of alcohol consumption was lower in CP than in LC patients. However, there was no significant difference between CP and LC in the percentage of patients with more than 20 years of alcohol consumption (41.6% and 52.6% for CP and LC subjects, respectively). The percentage of patients with more than 20 years of alcohol consumption was significantly higher in LC than in ASA patients (52.6% vs 33.7%). The total amount of ethanol consumed before diagnosis did not differ among groups (Table 1).
The percentage of cigarette smokers was slightly higher in CP than in LC patients. The BMI was higher in LC than in CP patients. The percentage of patients with overweight (BMI > 28) was also higher in LC than in CP group, but it was no different when compared to ASA patients (7.5%, 26.8% and 9% for CP, LC and ASA subjects, respectively) (Table 2). The percentage of patients with malnutrition (BMI < 20) was low in all groups, without significant differences among them (13.3%, 7.0% and 13.3% for CP, LC and ASA subjects, respectively).
Table 2.
Potential risk factors for CP or LC: Distribution of frequencies and OR in patients with ACP or ALC n (%)
| ACP 53 | ALC 57 | OR (95% CI) | P | |
| Gender (female) | 1 (1.9) | 9 (15.8) | 9.7 (1.1-79.8) | 0.017 |
| BMI > 28 | 4 (7.5) | 15 (26.8) | 4.5 (1.4-14.5) | 0.008 |
| BMI < 20 | 7 (13.2) | 4 (7) | 0.49 (0.13-1.8) | 0.280 |
| Age > 45 yr at diagnosis | 14 (26.4) | 41 (71.9) | 7.1 (3.1-16.6) | 0.001 |
| Smoking | 50 (94.3) | 46 (80.7) | 0.25 (0.06-0.95) | 0.044 |
| Alcohol > 150 g/d | 16 (30.2) | 19 (33.3) | 1.12 (0.5-2.5) | 0.775 |
| Years alcoholism > 20 | 22 (41.5) | 30 (52.6) | 1.56 (0.73-3.32) | 0.243 |
Features of alcoholic CP in CP, LC and ASA subjects
It is worth noting that there was absence of the two major clinical manifestations of CP, pancreatic pain and diarrhea/steatorrhea in patients with LC (Table 3). IDDM was frequent in CP (35 cases, 68%), but was found only in three LC cases (5.3%) and in none with ASA. Among these three LC patients with IDDM, one exhibited reduced E1 test (164 μg/g) as the unique altered pancreatic parameter. However, the percentage of patients with NIDDM was higher in the LC group (19.3%) than in the CP group. Diarrhea/steatorrhea was present in many patients with CP (54.7%), but absent in the other two groups (Table 3).
Table 3.
Clinical manifestations, functional parameters and imaging characteristics of CP in patients with ACP, ALC or ASA
| ACP (n = 53) | ALC (n = 57) | ASA (n = 30) | P | |
| Pancreatic pain | 85% | 0% | 0% | < 0.001 |
| IDDM | 68% | 5.3% | 0% | < 0.001 |
| NIDDM | 5.7% | 19.3% | 10% | CP vs LC, P = 0.03; CP vs ASA, LC vs ASA, NS |
| Diarrhoea/steatorrhoea | 54.7% | 0% | 0% | < 0.001 |
| Calcifications | 77.4% | 0% | 0% | < 0.001 |
| Dilatation of pancreatic duct | 67.9% | 0% | 0% | < 0.001 |
| Pancreatic pseudocysts | 58.5% | 0% | 0% | < 0.001 |
NS: Not significant.
The major morphological alterations such as calcification, dilatation of the pancreatic duct, and pseudocysts were found only in CP patients.
Features of alcoholic LC in CP, LC and ASA subjects
Clinical manifestations characteristic of LC such as ascites, encephalopathy, or upper gastrointestinal hemorrhage were found in most patients with LC, in one case (1/53) with CP and in none with ASA (Table 4). This particular case with CP exhibited gastrointestinal hemorrhage and portal vein thrombosis secondary to pancreopathy, splenomegaly, a PI of 6, with serum albumin level of 2.9 g/dL, severe steatorrhea, severe diabetes mellitus and malnutrition. Nevertheless, his ICG test was normal (23.8%/min).
Table 4.
Clinical manifestations, functional parameters and imaging characteristics of LC in patients with ACP, ALC or ASA
| ACP (n = 53) | ALC (n = 57) | ASA (n = 30) | P | |
| Ascites | 0% | 66.7% | 0% | |
| Haemorrhage in upper digestive tract | 1.9% | 45.6% | 0% | < 0.001 |
| Child-Pugh index > 5 | 5.7% | 98.2% | 0% | < 0.001 |
| INR > 1.2 | 0% | 73.7% | 0% | < 0.001 |
| Esophageal varices | 1.9% | 77.2% | 0% | < 0.001 |
| Splenomegaly | 1.9% | 77.2% | 0% | < 0.001 |
| Portal hypertension | 3.8% | 96.5% | 0% | < 0.001 |
The PI was > 5 in almost all cases (56/57) with LC, in three (3/53) with CP and in none (0/30) with ASA (Table 4). According to Child-Pugh classification, 35% (20/57) of LC patients were ascribed to class A, 35% (20/57) belonged to class B, and 30% (17/57) belonged to class C. Three cases of CP had a PI of 6. One was the previously described patient with gastrointestinal hemorrhage. In another case, a liver biopsy was available and ruled out the diagnosis of cirrhosis; however, the patient had an elevated Quick index (1.5 INR) at the moment of inclusion which could be attributed to severe steatorrhea because it normalized after parenteral treatment with vitamin K. The third CP case had a CPI of 6, and at the moment of inclusion exhibited cholestasis (total serum bilirubin = 2.6 mg/dL) due to compression of the common bile duct secondary to pancreopathy. This patient had a normal ICG test (28.9% min) and did not exhibit signs of hepatopathy.
Esophageal varices were found in 77% of LC patients, in one case (1/53) with CP and in none with ASA (Table 4). In this CP patient, there were no manifestations of hepatopathy, and varices were secondary to pancreopathy involving portal vein thrombosis. This patient had a large pseudocyst (50 mm × 50 mm) in the head of the pancreas, which caused obstructive jaundice that required surgical treatment, but the ICG test later at the moment of inclusion was normal (PDR = 28.9%/min).
Splenomegaly was also found in 72.2% of LC patients, in one case with CP and in none with ASA (Table 4). This CP case was the one with upper gastrointestinal hemorrhage, which has been previously described.
Portal hypertension was present in almost all LC patients (96.5%), in two patients with CP and in none with ASA (Table 4). In these two CP cases, portal hypertension was secondary to pancreatic disease, as previously described, with normal ICG test.
Pancreatic fecal elastase E1 in CP, LC and ASA subjects
Fecal E1 test was significantly lower (P < 0.001) in CP patients [9 (0.1-228) μg/g feces] than in LC patients [400.0 (130-614) μg /g feces] and ASA subjects [388 (121-675) μg/g feces] (Figure 1). Moreover, 94.3% of CP patients (50/53) exhibited E1 test lower than the normal limit of 200 μg/g feces, whereas 84.9% (45/53) had very low levels (i.e. < 100 μg/g feces), and among them 29, (64.4%) with diarrhea/steatorrhea. All these percentages were markedly higher (P < 0.001) than those in the LC and ASA groups.
Figure 1.
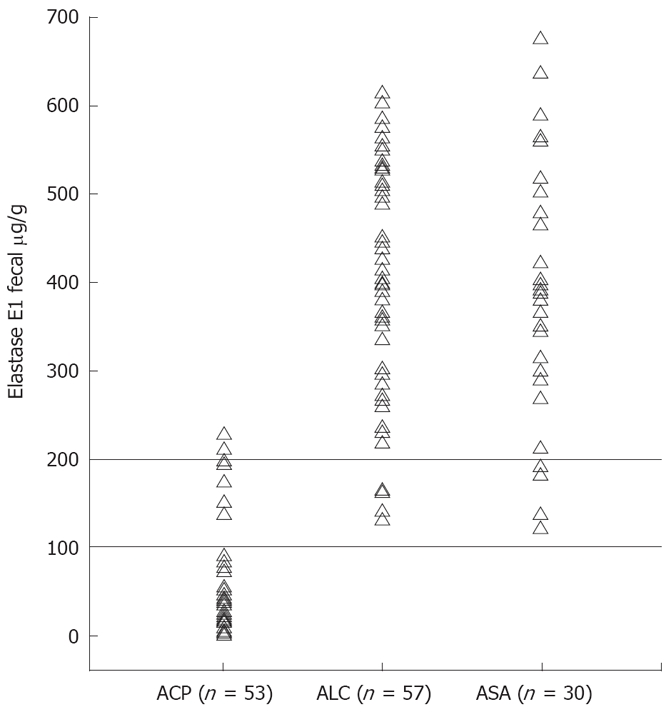
Fecal E1 test (μg/g feces) in patients with ACP, ALC or ASA. Reference lines for altered E1: < 200 μg/g, and severely altered E1: < 100 μg/g. ACP vs ALC, P < 0.001; ACP vs ASA, P < 0.001; ALC vs ASA, P = 0.747.
In the LC group, E1 test was < 200 μg/g only in four of 57 cases (7%), and in none of them was it < 100 μg/g. As mentioned before, none of the LC patients exhibited diarrhea/steatorrhea or pancreatic alterations assessed by imaging studies.
Among the 27 ASA subjects, E1 test was reduced only in four (14.8%), but it was never < 100 μg/g. As mentioned, none of the ASA subjects exhibited diarrhea/steatorrhea or pancreatic alterations assessed by imaging studies.
ICG clearance test in CP, LC and ASA subjects
PDR values of the ICG test were markedly more reduced in LC patients [6.1 (3.4-18.2)%/min] than in CP patients [22.6 (14.8-45)%/min] and ASA subjects [22.1 (10.4-30.2)%/min] (Figure 2). Ninety-three percent of LC patients (53/57) had a PDR lower than the normal limit (< 15%/min), and 64% of them exhibited a severe PDR reduction (< 10%/min). However, only one patient with CP (1.9%) showed PDR < 15%/min and none had PDR < 10%/min.
Figure 2.
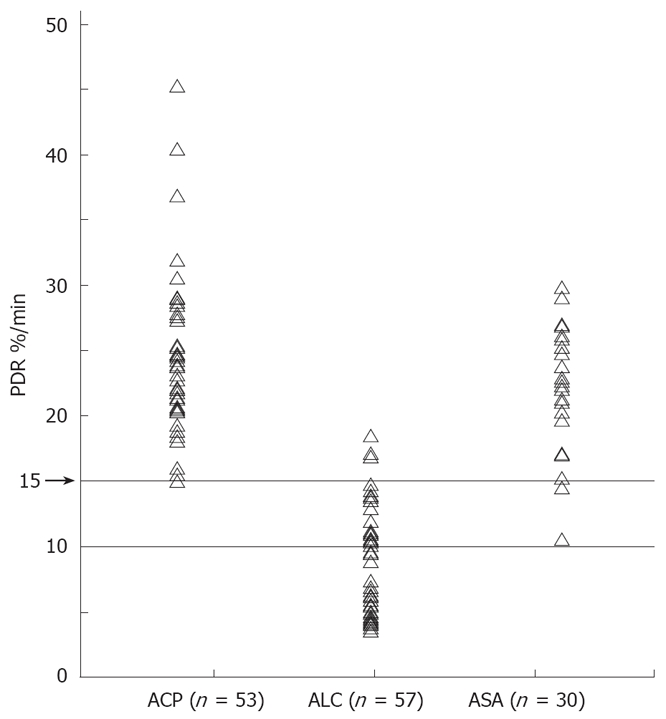
PDR, %/min of ICG in patients with ACP, ALC or ASA. Reference lines for altered PDR: < 15%/min, and severely altered PDR: < 10%/min. ACP vs ALC, P < 0.001; ACP vs ASA, P = 0.048; ALC vs ASA, P < 0.001.
In the ASA group, three of 29 subjects (10%) had reduced PDR (< 15%/min) and none had PDR < 10%/min. These ASA subjects had a normal E1 test, and had no pancreatic or hepatic alterations assessed by imaging studies compatible with CP or LC; all had PI of 5.
It is worth noting that a significant inverse correlation (r = - 0.746; P < 0.001) was found between E1 test levels and PDR values in patients with CP or LC (Figure 3). A significant correlation was also found between E1 test levels and PI (r = 0.759; P < 0.001). Therefore, in general, the reduction of functional hepatic reserve was associated with normal pancreatic function, and vice versa.
Figure 3.
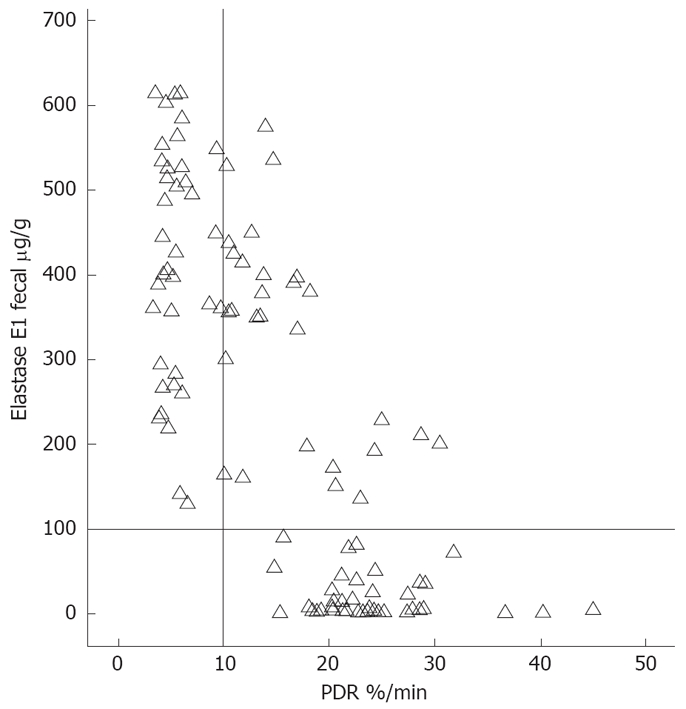
An inverse correlation (r = -0.746, P < 0.001) between indocyanine clearance (PDR, %/min) and fecal E1 test (μg/g feces) in patients with ACP, ALC or ASA. Reference lines: PDR (%/min) = 15; E1 test = 100. Vertical line for PDR (%/min) = 10, and horizontal line for E1 test = 100 are marked in the figure.
The analysis of potential risks of developing CP or LC showed significantly different values for gender, overweight (BMI > 28), age > 45 years at the time of diagnosis, and smoking (Table 2). Nevertheless, these differences were too low to explain the different evolution towards CP or LC. No significant differences were found regarding malnutrition (BMI < 20), elevated alcohol consumption (> 150 g/d) or long-term chronic alcohol consumption (> 20 years).
DISCUSSION
Chronic ethanol consumption is a common and frequent etiological factor in both CP and LC, and their risk correlates very well with the amount of ethanol daily consumed[2,7]. However, only a minority of alcoholics develop these diseases[1,4,5,7,8]; this together with the requirement of several years of ethanol intake, racial factors[39], and the difficulty of developing adequate experimental models have led to the consideration of other associated etiological factors[26].
The presence of a common etiological factor, i.e. alcoholism, for CP and LC could lead to the assumption that both diseases may coincide in some patients. The study of the presence and coincidence of these two diseases and their risk factors may provide new insights into their etiopathogenesis. Nevertheless, there is controversy about the frequencies of the coincidence between CP and LC in the studies published so far[15-19]. Differences in methodology, and particularly, the presence of hepatitis B or C virus are important confounders which hinder an accurate and reliable interpretation of the data. In fact, more than one-third of patients with alcoholic LC exhibit antibodies against hepatitis C virus[11,12].
In the present study, the frequency of the association between alcoholic CP and LC has been assessed after exclusion of main confounders (hepatitis B or C virus, non-alcoholic liver or pancreatic diseases, or surgery) and taken into account the major clinical manifestations, the morphological alterations detected by imaging studies, and the alterations of pancreatic and hepatic functions assessed by specific tests.
Our results clearly showed no overlapping between patients with alcoholic CP and alcoholic LC, not only regarding clinical manifestations, but also in imaging studies and functional tests. Furthermore, an inverse relationship was found between pancreatic and liver function in patients with CP or LC.
In our clinical study, the median age of patients at the moment of diagnosis was around a decade higher in LC than in CP (Table 1), due to the different natural history of these diseases[1,2,6,40]. Nevertheless, the age of patients at the time of inclusion in the study was not significantly different. As previously reported in other studies, the percentage of men was higher than that of women in all groups of alcoholics[21,41].
Regarding ethanol consumption, only the duration of ethanol intake was different among groups (20, 25 and 18.5 years for CP, LC and ASA, respectively) (Table 1). However, the mean daily ethanol intake and the total amount of ethanol consumed before diagnosis were not significantly different among groups, which is in agreement with those reported by other authors[2,8,19,42]. Moreover, the percentage of patients with ethanol intake > 150 g/d and the percentage of drinkers for more than 20 years were not significantly different. Therefore, the populations of the three groups in this study were homogeneous regarding ethanol intake.
The percentage of smokers was higher in CP (94.3%) and ASA (96.7%) than in LC (80.7%) (Table 1). Previous studies have reported that smoking is a risk factor for CP in alcoholics, which promotes the progression of the disease[31,43-45]. In addition, smoking has also been considered a risk factor in LC induced by hepatitis C virus[46]. The present study demonstrates that smoking is a risk factor not only for alcoholic CP but also for LC.
The BMI was slightly but significantly lower in CP than in LC, but not when compared with ASA. This slight difference may be ascribed to the presence of steatorrhea and diabetes mellitus in CP. In addition, the percentage of patients with BMI > 28 was significantly higher in LC than in CP and ASA, and these differences may by ascribed to retention of liquids in advanced LC.
The diagnosis of alcoholic CP is hindered in the initial stages of the disease due to the lack of specificity of clinical manifestations. Because of the difficulty in obtaining pancreatic biopsy, the diagnosis is established by combination of clinical manifestations, morphological alterations and impairment of the pancreatic exocrine and endocrine function[27,28].
In our study, 94.3% CP patients showed low E1 levels together with a high percentage of steatorrhea and IDDM, indicating that most patients were at an advanced stage of the disease. However, only four LC patients (7%) had E1 levels between 100 and 200 μg/g (Figure 1), and they neither exhibited steatorrhea nor any clinical or morphological manifestations of CP. In a similar fashion, only three LC patients (5.3%) exhibited IDDM, without the other clinical and morphological manifestations of CP. Only one of these patients exhibited 164 μg/g E-1 level; hence, the presence of CP in this patient could not be ruled out. Eleven LC patients exhibited NIDDM, which is common in LC[47] with normal E-1 level, but not a characteristic manifestation of CP[48]. In the ASA group, three subjects exhibited NIDDM, without symptoms of pancreopathy and normal E-1 and ICG tests.
The former studies that assessed the frequency of pancreatic alterations in patients with LC showed contradictory results. The frequency of pancreatic fibrosis compatible with CP in autopsies of LC patients was between 2% and 20% when the presence or absence of hepatitis B or C was not taken into account[14,16,18,19]. In addition, the age-related changes in morphofunctional parameters of the pancreas may be another confounder when the diagnosis of CP is based only on these parameters[49-53]. In a study using endoscopic ultrasonography and ERCP, Hastier et al[17] reported only moderate pancreatic alterations in 5.5% patients with alcoholic LC, without evolution to CP.
Some previous studies[51,54,55] on necropsies of patients with alcoholic LC showed very low frequency of the fibrotic pancreatic alteration characteristic of CP, which is predominantly perilobular fibrosis with heterogeneous distribution. In contrast, these patients exhibited diffuse and intralobular pancreatic fibrosis without calcifications or pseudocysts. Accordingly, these authors suggested that pancreatic morphological lesions in alcoholic LC correspond to a pathological process different from that of alcoholic CP.
It is worth noting that many studies on the association of CP and LC involve patients older than 50 years. It is well known that normal subjects at this age exhibit some morphofunctional pancreatic alterations[21,22,49-51,53] that could be taken for those characteristic of CP, but without evolution towards this disease. Consequently, morphofunctional pancreatic alterations with age may be another confounding factor. These findings might explain some of the discrepancies reported by different authors.
On the other hand, regarding the hepatic alterations, most LC patients in our study were at an advanced stage of the disease and showed ascites, encephalopathy and/or gastrointestinal hemorrhage as well as Child-Pugh B or C and markedly reduced PDR in the ICG test. However, only a few CP patients exhibited these manifestations, which were not ascribed to any hepatic disorder (Table 4).
There is also controversy concerning the frequency of LC in CP patients. Previous studies have reported that the presence of LC in patients with CP was variable, ranging between 5% and 30%[56]. Later, Angelini et al[19] found 12.5% of LC cases in CP patients. Although, in this study, cases with hepatitis C virus were not excluded, the authors did not find any relationship between the grade of hepatic histological alteration and the degree of pancreatic functional severity. Recently, Nakamura et al[15] found no association between liver and pancreatic disease in a population of alcoholics with abdominal pain, after exclusion of patients with viral hepatitis[15]. Accordingly, only 5% of patients who had altered ERCP also exhibited Child-Pugh class B or C[15].
It should be taken into account that many hepatic alterations in patients with alcoholic CP are ascribed to cholestasis secondary to pancreatitis[57,58], and indeed, they are not characteristic of advanced alcoholic liver disease[19,55]. Moreover, most of these cases exhibit regression of liver fibrosis after biliary drainage[59].
In our study, there was no coincidence at all between severe alterations of the pancreatic function assessed by fecal E-1 test and severe alterations of the liver function assessed by ICG test. Furthermore, we found a strong inverse correlation (r = -0.752; P < 0.001) between these functions (Figure 3). Similarly, we found a significant correlation between PI and fecal E-1 test (r = 0.759; P < 0.001). These findings support the hypothesis of a different and independent etiopathogenesis of CP and LC associated with alcoholism[25]. Hayakawa et al[24] reported a negative correlation between pancreatic and liver functions, but only in patients with alcoholic liver disease. In this regard, a general increase in exocrine pancreatic secretion in LC patients has been reported[19,60]. Thus, Dreiling et al[23] have suggested a hypersecretory state of the pancreas in alcoholic LC, with increased volume output[16] and maintaining either normal or elevated bicarbonate and enzyme outputs[16,19,23,24]. This has been considered a washout phenomenon, resulting in a decreased tendency of ductal protein and calcium precipitation in these patients[16].
Hayakawa et al[24] have reported that pancreatic secretion increases in patients with different degrees of alcoholic liver disease, assessed by the cholcystokinin-secretin test, ICG test and liver histopathology. Moreover, these authors have found a significant inverse correlation between bicarbonate secretion and ICG clearance[24].
The hypersecretory state of the pancreas in alcoholics with LC has been ascribed to a reduced inactivation of secretin[60] or even to the increased portal pressure[24]. Recently, it has been confirmed by an experimental result that chronic alcoholism impairs the neurohormonal control of the pancreas, both at the central nervous system and acinar levels, promoting the secretory response to feeding or other stimuli[61]. All these findings regarding the inverse correlation between the alterations of liver and pancreatic function tests may be a reflection of some correlation in the etiology of both diseases.
In summary, the present study demonstrates the scarce coincidence in clinical manifestations, morphological alterations and organ function between CP and LC in alcoholic subjects. This finding, together with the inverse correlation between indexes of pancreatic and liver functions in these patients, supports the hypothesis that alcoholic CP and LC evolve in a different manner and have different etiopathogenesis. Accordingly, chronic alcoholism, although a necessary factor, is not a sufficient cause in their etiopathogenesis. Further studies should provide new insights into the different risk factors-other than alcoholism-involved in the etiopathogenesis of alcoholic CP and LC.
COMMENTS
Background
Despite sharing similar risk factors, medical literature regarding the simultaneous occurrence of chronic pancreatitis (CP) and liver cirrhosis (LC) in patients with chronic alcoholism is scarce and the results are uncertain. This lack of coincidence may rely on differences in methodology such as retrospective versus prospective studies, and the evaluated parameters such as clinical, functional, imaging or histopathological. However, it may also reflect the hypothesis that alcoholism is not a sufficient cause, but a cofactor, for the development of such diseases.
Research frontiers
This study has been carefully designed to investigate the coincidence in clinical manifestations, morphological alterations and organ function between CP and LC in alcoholic subjects. The results support the hypothesis that alcoholic CP and alcoholic LC evolve in a different manner and have different etiopathogenesis, despite sharing a common risk factor.
Innovations and breakthroughs
There is a lack of coincidence between CP and LC in alcoholic subjects. There is an inverse correlation between indexes of pancreatic and liver functions in these patients, supporting the hypothesis that chronic alcoholism, although a necessary factor, is not a sufficient cause in their etiopathogenesis.
Applications
This paper suggests the necessity for researching other factors together with chronic alcoholism involved in the development of CP or LC.
Peer review
Authors studied the possible association between CP and LC of alcoholic etiology, after excluding any other causes. This is an interesting study. It was undertaken according to a carefully designed plan and with adequate statistical considerations. The authors successfully provided the evidence, suggesting that CP and LC evolve in a different manner, which will be useful for clinical researchers of these diseases.
Acknowledgments
We thank Mrs. Remedios Gonzalez for her technical help and Mrs. Landy Menzies for her assistance in preparing the English version of the manuscript.
Footnotes
Supported by Grants SAF2006-06963 and CSD2007-00020 from Ministerio de Educación y Ciencia
Peer reviewer: Katsutoshi Yoshizato, PhD, Phoenixbio Co. Ltd., 3-4-1, Kagamiyama, Higashihiroshima 739-0046, Japan
S- Editor Li DL L- Editor Kumar M E- Editor Lin YP
References
- 1.Worning H. Alcoholic chronic pancreatitis. In: Beger HG, Warshaw AL, Buchler MW, Carr-Locke DL, Neoptolemos JP, et al., editors. The pancreas. Oxford: Blackwell Science; 1998. pp. 672–682. [Google Scholar]
- 2.Durbec JP, Sarles H. Multicenter survey of the etiology of pancreatic diseases. Relationship between the relative risk of developing chronic pancreaitis and alcohol, protein and lipid consumption. Digestion. 1978;18:337–350. doi: 10.1159/000198221. [DOI] [PubMed] [Google Scholar]
- 3.Almela P, Aparisi L, Grau F, Sempere J, Rodrigo JM. Influence of alcohol consumption on the initial development of chronic pancreatitis. Rev Esp Enferm Dig. 1997;89:741–746, 747-752. [PubMed] [Google Scholar]
- 4.Lankisch PG, Lowenfels AB, Maisonneuve P. What is the risk of alcoholic pancreatitis in heavy drinkers? Pancreas. 2002;25:411–412. doi: 10.1097/00006676-200211000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Aparisi L, Navarro S, Perez Mateo M, Bautista D. [Prevalence of malnutrition and morphofunctional alterations of the pancreas in asymptomatic chronic alcoholic patients] Med Clin (Barc) 2000;114:444–448. doi: 10.1016/s0025-7753(00)71327-3. [DOI] [PubMed] [Google Scholar]
- 6.Etemad B, Whitcomb DC. Chronic pancreatitis: diagnosis, classification, and new genetic developments. Gastroenterology. 2001;120:682–707. doi: 10.1053/gast.2001.22586. [DOI] [PubMed] [Google Scholar]
- 7.Becker U, Deis A, Sorensen TI, Gronbaek M, Borch-Johnsen K, Muller CF, Schnohr P, Jensen G. Prediction of risk of liver disease by alcohol intake, sex, and age: a prospective population study. Hepatology. 1996;23:1025–1029. doi: 10.1002/hep.510230513. [DOI] [PubMed] [Google Scholar]
- 8.Bellentani S, Saccoccio G, Costa G, Tiribelli C, Manenti F, Sodde M, Saveria Croce L, Sasso F, Pozzato G, Cristianini G, et al. Drinking habits as cofactors of risk for alcohol induced liver damage. The Dionysos Study Group. Gut. 1997;41:845–850. doi: 10.1136/gut.41.6.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grant BF, Dufour MC, Harford TC. Epidemiology of alcoholic liver disease. Semin Liver Dis. 1988;8:12–25. doi: 10.1055/s-2008-1040525. [DOI] [PubMed] [Google Scholar]
- 10.Lelbach WK. Cirrhosis in the alcoholic and its relation to the volume of alcohol abuse. Ann N Y Acad Sci. 1975;252:85–105. doi: 10.1111/j.1749-6632.1975.tb19146.x. [DOI] [PubMed] [Google Scholar]
- 11.Pares A, Caballeria J, Bruguera M, Torres M, Rodes J. Histological course of alcoholic hepatitis. Influence of abstinence, sex and extent of hepatic damage. J Hepatol. 1986;2:33–42. doi: 10.1016/s0168-8278(86)80006-x. [DOI] [PubMed] [Google Scholar]
- 12.Serra MA, Escudero A, Rodriguez F, del Olmo JA, Rodrigo JM. Effect of hepatitis C virus infection and abstinence from alcohol on survival in patients with alcoholic cirrhosis. J Clin Gastroenterol. 2003;36:170–174. doi: 10.1097/00004836-200302000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Nanji AA. Alcoholic liver disease. In: Zakim D, Boyer T, eds , et al., editors. Hepatology. A Texbook of liver disease. 4th ed. Phyladelphia: WB Sauders; 2003. pp. 839–922. [Google Scholar]
- 14.Ichihara S, Sato M, Kozuka S. Prevalence of pancreatitis in liver diseases of various etiologies: an analysis of 107,754 adult autopsies in Japan. Digestion. 1992;51:86–94. doi: 10.1159/000200881. [DOI] [PubMed] [Google Scholar]
- 15.Nakamura Y, Kobayashi Y, Ishikawa A, Maruyama K, Higuchi S. Severe chronic pancreatitis and severe liver cirrhosis have different frequencies and are independent risk factors in male Japanese alcoholics. J Gastroenterol. 2004;39:879–887. doi: 10.1007/s00535-004-1405-y. [DOI] [PubMed] [Google Scholar]
- 16.Renner IG, Rinderknecht H, Wisner JR Jr. Pancreatic secretion after secretin and cholecystokinin stimulation in chronic alcoholics with and without cirrhosis. Dig Dis Sci. 1983;28:1089–1093. doi: 10.1007/BF01295807. [DOI] [PubMed] [Google Scholar]
- 17.Hastier P, Buckley MJ, Francois E, Peten EP, Dumas R, Caroli-Bosc FX, Delmont JP. A prospective study of pancreatic disease in patients with alcoholic cirrhosis: comparative diagnostic value of ERCP and EUS and long-term significance of isolated parenchymal abnormalities. Gastrointest Endosc. 1999;49:705–709. doi: 10.1016/s0016-5107(99)70286-5. [DOI] [PubMed] [Google Scholar]
- 18.Renner IG, Savage WT 3rd, Stace NH, Pantoja JL, Schultheis WM, Peters RL. Pancreatitis associated with alcoholic liver disease. A review of 1022 autopsy cases. Dig Dis Sci. 1984;29:593–599. doi: 10.1007/BF01347290. [DOI] [PubMed] [Google Scholar]
- 19.Angelini G, Merigo F, Degani G, Camplani N, Bovo P, Fratta Pasini A, Cavallini G, Brocco G, Scuro LA. Association of chronic alcoholic liver and pancreatic disease: a prospective study. Am J Gastroenterol. 1985;80:998–1003. [PubMed] [Google Scholar]
- 20.Ammann RW, Buehler H, Bruehlmann W, Kehl O, Muench R, Stamm B. Acute (nonprogressive) alcoholic pancreatitis: prospective longitudinal study of 144 patients with recurrent alcoholic pancreatitis. Pancreas. 1986;1:195–203. [PubMed] [Google Scholar]
- 21.Anand BS, Vij JC, Mac HS, Chowdhury V, Kumar A. Effect of aging on the pancreatic ducts: a study based on endoscopic retrograde pancreatography. Gastrointest Endosc. 1989;35:210–213. doi: 10.1016/s0016-5107(89)72760-7. [DOI] [PubMed] [Google Scholar]
- 22.Rajan E, Clain JE, Levy MJ, Norton ID, Wang KK, Wiersema MJ, Vazquez-Sequeiros E, Nelson BJ, Jondal ML, Kendall RK, et al. Age-related changes in the pancreas identified by EUS: a prospective evaluation. Gastrointest Endosc. 2005;61:401–406. doi: 10.1016/s0016-5107(04)02758-0. [DOI] [PubMed] [Google Scholar]
- 23.Dreiling DA, Greenstein AJ, Bordalo O. The hypersecretory states of the pancreas. Implications in the pathophysiology of pancreatic inflammation and the pathogenesis of peptic ulcer diathesis. Am J Gastroenterol. 1973;59:505–511. [PubMed] [Google Scholar]
- 24.Hayakawa T, Kondo T, Shibata T, Kitagawa M, Sakai Y, Sobajima H, Ishiguro H, Nakae Y, Kato K. Exocrine pancreatic function in chronic liver diseases. Am J Gastroenterol. 1991;86:201–204. [PubMed] [Google Scholar]
- 25.Whitcomb DC. Genetic predisposition to alcoholic chronic pancreatitis. Pancreas. 2003;27:321–326. doi: 10.1097/00006676-200311000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Stickel F, Osterreicher CH. The role of genetic polymorphisms in alcoholic liver disease. Alcohol Alcohol. 2006;41:209–224. doi: 10.1093/alcalc/agl011. [DOI] [PubMed] [Google Scholar]
- 27.Sarner M, Cotton PB. Classification of pancreatitis. Gut. 1984;25:756–759. doi: 10.1136/gut.25.7.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singer MV, Gyr K, Sarles H. Revised classification of pancreatitis. Report of the Second International Symposium on the Classification of Pancreatitis in Marseille, France, March 28-30, 1984. Gastroenterology. 1985;89:683–685. [PubMed] [Google Scholar]
- 29.Anthony PP, Ishak KG, Nayak NC, Poulsen HE, Scheuer PJ, Sobin LH. The morphology of cirrhosis. Recommendations on definition, nomenclature, and classification by a working group sponsored by the World Health Organization. J Clin Pathol. 1978;31:395–414. doi: 10.1136/jcp.31.5.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Talamini G, Bassi C, Falconi M, Frulloni L, Di Francesco V, Vaona B, Bovo P, Rigo L, Castagnini A, Angelini G, et al. Cigarette smoking: an independent risk factor in alcoholic pancreatitis. Pancreas. 1996;12:131–137. [PubMed] [Google Scholar]
- 31.Klatsky AL, Armstrong MA. Alcohol, smoking, coffee, and cirrhosis. Am J Epidemiol. 1992;136:1248–1257. doi: 10.1093/oxfordjournals.aje.a116433. [DOI] [PubMed] [Google Scholar]
- 32.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 33.Tacke F, Fiedler K, Trautwein C. A simple clinical score predicts high risk for upper gastrointestinal hemorrhages from varices in patients with chronic liver disease. Scand J Gastroenterol. 2007;42:374–382. doi: 10.1080/00365520600930826. [DOI] [PubMed] [Google Scholar]
- 34.Okochi O, Kaneko T, Sugimoto H, Inoue S, Takeda S, Nakao A. ICG pulse spectrophotometry for perioperative liver function in hepatectomy. J Surg Res. 2002;103:109–113. doi: 10.1006/jsre.2001.6328. [DOI] [PubMed] [Google Scholar]
- 35.Serra MA, Rodrigo JM, Guix J, Montes F, Wassel A, Aparisi L, Olmo JA, Bixquert M. The discriminant diagnostic power of liver function tests in hepatic cirrhosis. Acta Med Port. 1981;3:3–10. [PubMed] [Google Scholar]
- 36.Loser C, Mollgaard A, Folsch UR. Faecal elastase 1: a novel, highly sensitive, and specific tubeless pancreatic function test. Gut. 1996;39:580–586. doi: 10.1136/gut.39.4.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van de Kamer J, Huinink B, Woyers H. Rapid method for the determination of fat in feces. J Biol Chem. 1949;177:347–355. [PubMed] [Google Scholar]
- 38.Fernandez-Real JM, Vayreda M, Casamitjana R, Saez M, Ricart W. [Body mass index (BMI) and percent fat mass. A BMI > 27.5 kg/m2 could be indicative of obesity in the Spanish population] Med Clin (Barc) 2001;117:681–684. [PubMed] [Google Scholar]
- 39.Lowenfels AB, Maisonneuve P, Grover H, Gerber E, Korsten MA, Antunes MT, Marques A, Pitchumoni CS. Racial factors and the risk of chronic pancreatitis. Am J Gastroenterol. 1999;94:790–794. doi: 10.1111/j.1572-0241.1999.00952.x. [DOI] [PubMed] [Google Scholar]
- 40.Naveau S, Perlemuter G, Balian A. [Epidemiology and natural history of cirrhosis] Rev Prat. 2005;55:1527–1532. [PubMed] [Google Scholar]
- 41.del Olmo JA, Serra MA, Rodriguez F, Escudero A, Gilabert S, Rodrigo JM. Incidence and risk factors for hepatocellular carcinoma in 967 patients with cirrhosis. J Cancer Res Clin Oncol. 1998;124:560–564. doi: 10.1007/s004320050215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mezey E, Kolman CJ, Diehl AM, Mitchell MC, Herlong HF. Alcohol and dietary intake in the development of chronic pancreatitis and liver disease in alcoholism. Am J Clin Nutr. 1988;48:148–151. doi: 10.1093/ajcn/48.1.148. [DOI] [PubMed] [Google Scholar]
- 43.Bourliere M, Barthet M, Berthezene P, Durbec JP, Sarles H. Is tobacco a risk factor for chronic pancreatitis and alcoholic cirrhosis? Gut. 1991;32:1392–1395. doi: 10.1136/gut.32.11.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lowenfels AB, Zwemer FL, Jhangiani S, Pitchumoni CS. Pancreatitis in a native American Indian population. Pancreas. 1987;2:694–697. doi: 10.1097/00006676-198711000-00012. [DOI] [PubMed] [Google Scholar]
- 45.Maisonneuve P, Lowenfels AB, Mullhaupt B, Cavallini G, Lankisch PG, Andersen JR, Dimagno EP, Andren-Sandberg A, Domellof L, Frulloni L, et al. Cigarette smoking accelerates progression of alcoholic chronic pancreatitis. Gut. 2005;54:510–514. doi: 10.1136/gut.2004.039263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hezode C, Lonjon I, Roudot-Thoraval F, Mavier JP, Pawlotsky JM, Zafrani ES, Dhumeaux D. Impact of smoking on histological liver lesions in chronic hepatitis C. Gut. 2003;52:126–129. doi: 10.1136/gut.52.1.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Joffe BI, Bank S, Jackson WP, Keller P, O'Reilly IG, Vinik AI. Insulin reserve in patients with chronic pancreatitis. Lancet. 1968;2:890–892. doi: 10.1016/s0140-6736(68)91055-6. [DOI] [PubMed] [Google Scholar]
- 48.Zakim D, Metabolism of glucose and fatty acids by the liver. In: Zakim D, Bayer T, eds. Hepatology. A textbook of liver disease. 4th ed. Philadelphia: Sauders; 2003. pp. 49–80. [Google Scholar]
- 49.Schmitz-Moormann P, Himmelmann GW, Brandes JW, Folsch UR, Lorenz-Meyer H, Malchow H, Soehendra LN, Wienbeck M. Comparative radiological and morphological study of human pancreas. Pancreatitis like changes in postmortem ductograms and their morphological pattern. Possible implication for ERCP. Gut. 1985;26:406–414. doi: 10.1136/gut.26.4.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kreel L, Sandin B. Changes in pancreatic morphology associated with aging. Gut. 1973;14:962–970. doi: 10.1136/gut.14.12.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Martin E. Different pathomorphological aspects of pancreatic fibrosis correlated with etiology. Anatomical study of 300 cases. In: Gyr R, Singer M, Sarles H, eds , et al., editors. Pancreatitis. Concepts and classification. Amsterdam: Elsevier; 1984. pp. 77–80. [Google Scholar]
- 52.Laugier R, Bernard JP, Berthezene P, Dupuy P. Changes in pancreatic exocrine secretion with age: pancreatic exocrine secretion does decrease in the elderly. Digestion. 1991;50:202–211. doi: 10.1159/000200762. [DOI] [PubMed] [Google Scholar]
- 53.Ikeda M, Sato T, Morozumi A, Fujino MA, Yoda Y, Ochiai M, Kobayashi K. Morphologic changes in the pancreas detected by screening ultrasonography in a mass survey, with special reference to main duct dilatation, cyst formation, and calcification. Pancreas. 1994;9:508–512. doi: 10.1097/00006676-199407000-00014. [DOI] [PubMed] [Google Scholar]
- 54.Martin E, Bedossa P. Diffuse fibrosis of the pancreas: a peculiar pattern of pancreatitis in alcoholic cirrhosis. Gastroenterol Clin Biol. 1989;13:579–584. [PubMed] [Google Scholar]
- 55.Suda K, Takase M, Takei K, Nakamura T, Akai J, Nakamura T. Histopathologic study of coexistent pathologic states in pancreatic fibrosis in patients with chronic alcohol abuse: two distinct pathologic fibrosis entities with different mechanisms. Pancreas. 1996;12:369–372. doi: 10.1097/00006676-199605000-00008. [DOI] [PubMed] [Google Scholar]
- 56.Lankisch PG, Banks PA. Pancreatitis. Berlin: Springer V; 1998. pp. 279–301. [Google Scholar]
- 57.Wilson C, Auld CD, Schlinkert R, Hasan AH, Imrie CW, MacSween RN, Carter DC. Hepatobiliary complications in chronic pancreatitis. Gut. 1989;30:520–527. doi: 10.1136/gut.30.4.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Frey C. The surgical treatment of chronic pancreatitis. In: Go VLW, DiMagno EP, Gardner JD, Lebnthal E, Rever HA, et al., editors. The pancreas. Biology, Pathobiology and disease. 2nd ed. New York: Raven Press; 1986. pp. 707–740. [Google Scholar]
- 59.Hammel P, Couvelard A, O'Toole D, Ratouis A, Sauvanet A, Flejou JF, Degott C, Belghiti J, Bernades P, Valla D, et al. Regression of liver fibrosis after biliary drainage in patients with chronic pancreatitis and stenosis of the common bile duct. N Engl J Med. 2001;344:418–423. doi: 10.1056/NEJM200102083440604. [DOI] [PubMed] [Google Scholar]
- 60.Turnberg LA, Grahame G. Secretion of water and electrolytes into the duodenum in normal subjects and in patients with cirrhosis: the response to secretin and pancreozymin. Gut. 1974;15:273–277. doi: 10.1136/gut.15.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Deng X, Wood PG, Eagon PK, Whitcomb DC. Chronic alcohol-induced alterations in the pancreatic secretory control mechanisms. Dig Dis Sci. 2004;49:805–819. doi: 10.1023/b:ddas.0000030093.25897.61. [DOI] [PubMed] [Google Scholar]


