Abstract
Objective
To examine the extent to which early postpartum depression is associated with weight retention 1 year after childbirth.
Methods and Procedures
In a prospective cohort study of 850 women enrolled in Project Viva, mothers reported depressive symptoms on the Edinburgh Postnatal Depression Scale (EPDS) at midpregnancy and 6 months postpartum. A score >12 indicated probable depression. We assessed associations of antenatal and postpartum depression with risk of substantial weight retention (at least 5 kg) 1 year after childbirth.
Results
Seven-hundred thirty-six women (87%) were not depressed during or after pregnancy, 55 (6%) experienced antenatal depression only, 22 (3%) experienced both antenatal and postpartum depression, and 37 (4%) experienced postpartum depression only. At 1 year, participants retained a mean of 0.6 kg (range −16.4 to 25.5), and 12% retained at least 5 kg. In multivariate logistic regression analyses, after adjustment for weight-related covariates, maternal sociodemographics, and parity, new-onset postpartum depression was associated with more than a doubling of risk of retaining at least 5 kg (odds ratio (OR): 2.54, 95% confidence interval (CI): 1.06, 6.09). Antenatal depression, either alone or in combination with postpartum depression, was not associated with substantial weight retention.
Discussion
New-onset postpartum depression was associated with substantial weight retention in the first postpartum year. Interventions to manage depressive symptoms may help reduce excess weight retained postpartum and aid in the prevention of obesity among women.
Introduction
Obesity prevalence among young women has increased markedly in recent decades, a worrisome trend that is associated with a rise in comorbid illness and premature death (1–4). In 1999–2004, 29.0% of women between 20 and 39 years of age were obese (BMI ≥ 30 kg/m2), and an additional 24.6% were overweight (BMI 25–29.9 kg/m2) (1). This reflects an almost doubling in prevalence since 1960 (1). Young adulthood appears to be a time of heightened vulnerability for excess weight gain in women (5), suggesting that there may be factors operating during late adolescence and early adulthood that predispose to obesity. Childbearing has been identified as one such factor (6), as it is a period characterized by profound changes in weight.
For many women, returning to prepregnancy weight is a challenge (6,7). Approximately 14–25% of women are at least 5 kg heavier 1 year after delivery (6,8,9), placing them at increased risk for obesity and its consequences (8). Identified risk factors for retaining at least 5 kg at 1 year postpartum include higher prepregnancy weight and gestational weight gain (6,8), black race (10,11), primiparity (6), and behaviors including inadequate sleep (12), low physical activity, high trans fat intake, and frequent television viewing (13).
Few studies have examined the association of psychosocial factors, particularly depression, with weight retention and obesity postpartum. Carter et al. (14) reported a strong correlation between depression and BMI at 4 months postpartum, although these findings were limited by a small sample size, cross-sectional design, and use of a suboptimal post-partum depression instrument. The paucity of prospective data postpartum is surprising, as numerous longitudinal studies in non-pregnant women have reported that depressive symptoms predict obesity onset (15–19). Data also suggest that non-gravid depressed women have poorer weight loss treatment outcomes (20), implying that once established, psychosocial factors may make obesity management more difficult.
Postpartum depression is common, with prevalence estimates ranging between 10 and 15% (21). It is associated with substantial morbidity to both mother and infant (22–25), but whether an additional consequence includes weight retention and postpartum obesity merits further investigation. Because postpartum depression is a potentially modifiable condition, determining its relationship to weight retention after childbirth could provide information that might identify women at higher risk for weight-related problems and lead to the design of effective obesity prevention programs for young mothers.
In this study, we used data from a longitudinal cohort study of pregnant women to examine the extent to which early postpartum depression is associated with substantial weight retention at 1 year after delivery. We hypothesized that postpartum depression would act as a barrier to weight loss, and therefore increase the risk of retaining at least 5 kg at the end of the first postpartum year.
Methods AND PROCEDURES
Study population and design
Between 1999 and 2002, we recruited women into Project Viva at their first prenatal visit from one of eight urban and suburban obstetric offices associated with a multispecialty group practice in Eastern Massachusetts (26). Eligibility criteria included fluency in English, gestational age <22 weeks, and a singleton pregnancy. All mothers provided written informed consent, and all procedures were in accordance with ethical standards for human experimentation. Institutional review boards of participating sites approved the study.
We enrolled 63% of eligible participants, resulting in 2,128 women who delivered live infants. We collected data by questionnaire in early pregnancy, 28 weeks’ gestation, 6 months and 1 year postpartum, and by in-person interview at childbirth. We excluded from analysis women with missing information on prepregnancy BMI (n = 15) or gestational weight gain (n = 22), who had incomplete or no measurement of antenatal depression (n = 484) or postpartum depression (n = 376), who did not report 1 year postpartum weight (n = 265), or who became pregnant in the first year postpartum (n = 116), leaving 850 women available for inclusion in this analysis. Compared with the 1,278 women who were not included, the 850 women in this analysis were somewhat older (mean of 33.0 vs. 31.0 years, P < 0.0001), more likely to be white (79% vs. 58%, P < 0.0001), college educated (77% vs. 56%, P < 0.0001), and to pregnancy (mean prepregnancy BMI of 24.2 vs. 25.4 kg/m2, P < 0.0001), but had only slight differences in mean gestational weight gain (15.7 vs. 15.4 kg, P = 0.37), antenatal depression scores (5.2 vs. 5.5, P = 0.17), and 6-month postpartum depression scores (4.8 vs. 5.3, P = 0.05).
Main exposure—depression
We assessed depression with the 10-item Edinburgh Postnatal Depression Scale (EPDS), a widely used self-report screening measure, at midpregnancy (mean of 28 weeks’ gestation) and 6 months postpartum. We chose the EPDS because it has been validated for antenatal and postpartum use (27–29) and does not include somatic items, such as weight change, loss of energy, and tiredness that may be misleading as indicators of depression in the puerperal period (30). A score >12 indicates probable depression (27,31,32). Validation of the scale against diagnostic clinical interviews indicated a specificity of 78% and a sensitivity of 86% for all forms of depression (27).
We also collected data about a history of depressive symptoms prior to pregnancy via midpregnancy questionnaire. We defined prepregnancy depression as an endorsement of the question, “Before this pregnancy, was there ever a period of time when you were feeling depressed or down or when you lost interest in pleasurable activities most of the day, nearly every day, for at least 2 weeks?” along with an indication that a professional had previously diagnosed or treated the participant for depression.
Outcome—postpartum weight retention
We collected information on postpartum weight through a question-naire mailed to participants at 1 year after delivery. Weight retention was calculated as the difference between self-reported 1-year postpartum weight and prepregnancy weight. We defined our primary out-come as substantial postpartum weight retention, a weight excess of at least 5 kg, as data suggest this cut-point predicts later obesity and its consequences (6,8). Comparison of prepregnancy self-reported weights with clinically measured weights among a sample of 170 women in this cohort revealed a tight correlation (r = 0.99), with a mean systematic underreport of 1 kg that did not vary by maternal race/ethnicity, gestational age at enrollment into the study, or weight itself (13). The very high correlation indicates that ranking of individuals is well preserved. Although we did not perform a similar validation at 1 year postpartum, the magnitude of any underreporting is likely to have been similar, and our use of a dichotomous outcome measure would further minimize any potential bias due to self-report.
Covariates
Using a combination of questionnaires and interviews at the first study visit during early pregnancy (~10 weeks’ gestation), we collected information about maternal race/ethnicity, age, education, parity, and household income. Pregravid BMI (kg/m2) was calculated from self-reported height and weight. We used prenatal medical records to obtain serial pregnancy weights, and calculated gestational weight gain as the difference between the last clinically recorded weight before delivery and prepregnancy weight. Based on Institute of Medicine criteria (33), we classified gestational weight gain as inadequate, adequate, or excessive. These guidelines recommend that women with a “normal” prepregnancy BMI (19.8–26.0 kg/m2) should gain 11.5–16 kg, that women with a BMI <19.8 kg/m2 should gain 12.5–18 kg, that women with a BMI of 26.0–29.0 kg/m2 should gain 7–11.5 kg, and that women with a BMI > 29.0 kg/m2 should gain at least 6.0 kg. We set an upper limit of 11.5 kg for these heaviest women (33).
At 6 months postpartum, participants reported the average weekly hours they spent watching television or videos and in leisure-time physical activity. Walking was of primary interest as a measure of physical activity because of results from Project Viva that indicated an association between less time spent walking and substantial postpartum weight retention (13). We asked each participant to report, “In the past month, on average, how many hours per week have you spent walking (include walking for fun or exercise, walking to work, but not walking at work)?” We assessed dietary intake via the PrimeScreen brief food frequency questionnaire (34), which included 21 questions about intake of foods and food groups since delivery, including questions quantifying intake of stick margarine, baked products, and deep-fried foods, which are the chief sources of trans fats. A priori, we decided to focus only on trans fat intake because this nutrient has been associated with weight and weight gain in nonpregnant populations, and it appeared to be the lone independent dietary predictor of weight retention within our study population (13). Mothers also reported infant feeding history, smoking habits, employment, and daily sleep duration on the 6-month questionnaire.
Data analysis
Although our primary aim was to examine the association of postpartum depression with substantial postpartum weight retention, we were also interested in the interactive and independent effects of depression before and during pregnancy. Preliminary analyses stratified by the presence or absence of prepregnancy depression did not differ, so we disregarded this variable for simplicity. We were left with four exposure groups: those with neither antenatal nor postpartum depression, those with antenatal depression only, those with antenatal and postpartum depression, and those with postpartum depression only. We used women without depression at either time point as the reference group.
Univariate distribution of the outcome, main exposures, and covariates were examined. Differences in distribution for each covariate by exposure status were assessed using Student’s t-tests, Wilcoxon-rank sum, and χ2 analyses. We used multivariate logistic regression to examine the extent to which antenatal and postpartum depression were each independently associated with substantial postpartum weight retention. Covariates were considered based on the review of the literature and included if they were independent predictors of weight retention or confounded associations of depression with postpartum weight retention. We grouped similar covariates and entered them into regression models in succession. We started with an initial model composed of the depression variables only (model 1). We then included weight-related variables such as prepregnancy BMI and gestational weight gain (model 2), followed by the addition of parity and maternal sociodemographic factors, including age, education, marital status, income, and race/ethnicity (model 3). We did not find breastfeeding duration, employment status, gestation length, or smoking habits to result in material changes in the magnitudes of the observed associations between depression and substantial postpartum weight retention, and therefore did not include them in the final models. We constructed an additional model (model 4) that added postpartum behaviors, such as walking, television viewing, sleep duration, and trans fat intake, which we have previously found to be independent predictors of substantial postpartum weight retention in the Project Viva cohort (12,13) and might serve as intermediates in the pathway. We used SAS version 9.1 (SAS Institute, Cary, NC) to carry out all analyses.
Results
Approximately 21% of participating women were nonwhite; 23% had not graduated from college. Mean age was 33.0 years (s.d. 4.7) and prepregnancy BMI was 24.2 (4.7) kg/m2. Fifty percent of participants had excessive weight gain during pregnancy, and 48% were nulliparous. At 6 months postpartum, women reported a mean (s.d.) of 0.7 (0.7) h of walking, 1.7 (1.3) h of television viewing, and 6.7 (1.2) h of sleep per day. Mean (s.d.) reported daily intake of trans fat was 1.3% (0.6) of total energy (Table 1).
Table 1.
Distribution of characteristics by depression status among 850 participantsa in Project Viva.
| Maternal characteristics | No antenatal or postpartum depression n = 736 (86%) (mean (s.d.) or percent) |
Antenatal depression only n = 55 (6%) (mean (s.d.) or percent) |
Both antenatal and postpartum depression n = 22 (3%) (mean (s.d.) or percent) |
Postpartum depression only n = 37 (4%) (mean (s.d.) or percent) |
|---|---|---|---|---|
| Pregnancy | ||||
| Sociodemographics | ||||
| Age (years) | 33.1 (4.6) | 31.5 (4.7)* | 33.6 (5.7) | 32.6 (5.1) |
| White | 80% | 64%* | 82% | 81% |
| College graduate | 78% | 69% | 77% | 68% |
| Household income ≤ $70,000 | 29% | 39% | 55%* | 39% |
| Married or cohabitating | 97% | 87%* | 73%* | 95% |
| Parous | 52% | 55% | 50% | 43% |
| Prepregnancy depression history | 10% | 29%* | 45%* | 25%* |
| Prepregnancy BMI (kg/m2) | 24.1 (4.6) | 23.9 (4.3) | 25.7 (5.9) | 25.6 (6.0) |
| Gestational weight gain (IOM categories) | ||||
| Excessive | 50% | 42% | 55% | 62% |
| Adequate | 37% | 36% | 41% | 22% |
| Inadequate | 13% | 22% | 5% | 16% |
| 6 months postpartum | ||||
| Breastfed exclusively | 26% | 29% | 14% | 30% |
| Walking (h/day) | 0.75 (0.7) | 0.66 (0.7) | 0.73 (0.8) | 0.59 (0.7)* |
| Television viewing (h/day) | 1.7 (1.2) | 1.7 (1.4) | 2.3 (2.2) | 1.5 (1.3) |
| Smoker | 4% | 7% | 9% | 0% |
| Employed | 71% | 65% | 73% | 76% |
| Dietary trans fat intake (% of energy) | 1.2 (0.6) | 1.2 (0.6) | 1.5 (0.9) | 1.3 (0.5) |
| Sleep duration | ||||
| ≤5 h/day | 11% | 16% | 23% | 27%* |
| 6 h/day | 28% | 31% | 27% | 32% |
| 7 h/day | 36% | 29% | 23% | 19% |
| ≥8 h/day | 25% | 24% | 27% | 22% |
IOM, Institute of Medicine.
We had small amounts of missing data for income (3%), employment (1%), smoking (1%), walking (1%), trans fat intake (1%).
P < 0.05 for the comparison to women with no antenatal or postpartum depression (reference group).
Thirteen percent of women had a history of depression prior to pregnancy, one-third of whom went on to develop depression during or after pregnancy. Mean antenatal EPDS score was 5.2 (s.d. 4.7; range 0–25); mean postpartum EPDS score was 4.8 (s.d. 4.5; range 0–25). An EPDS score >12 during and/or after pregnancy occurred in 114 women (13% of total); 55 of whom had antenatal depression only, 22 had both antenatal and postpartum depression, while 37 had new-onset depression in the postpartum period. Seven-hundred thirty-six women (87% of total) did not have depression in either period (Table 1).
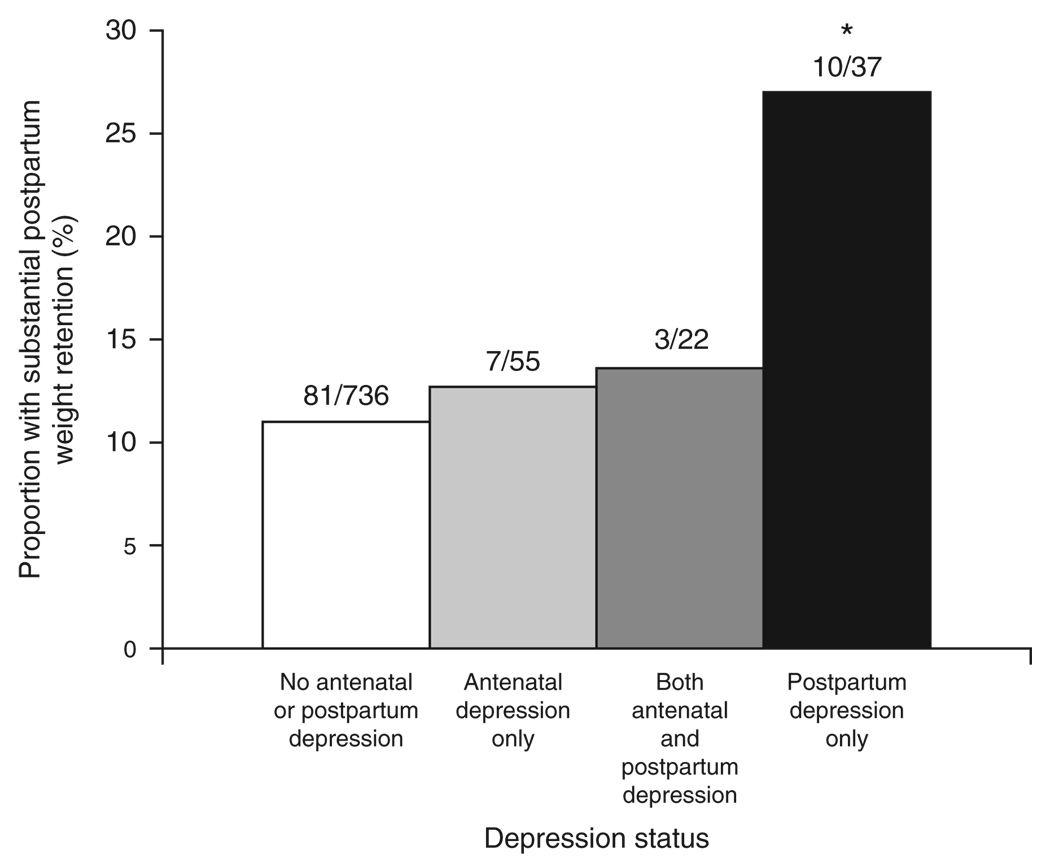
At 1 year, participants retained a mean of 0.6 kg (range −16.4 to 25.5), and 101 women (12%) retained at least 5 kg. Twenty-seven percent of the 37 women with new-onset postpartum depression had substantial postpartum weight retention, while only 11% of women without antenatal or postpartum depression retained at least 5 kg (P = 0.003, Figure 1). The proportions of women who retained at least 5 kg with antenatal depression only (13%) and depression during both periods (14%), however, did not markedly differ from those without depression at either timepoint (P = 0.70 for both comparisons).
Figure 1.
Proportion of women retaining at least 5 kg at 1 year postpartum according to depression status. *P = 0.003 for the comparison between postpartum depression only and no antenatal or postpartum depression, via χ2-test.
In unadjusted logistic regression analyses, new-onset postpartum depression was associated with a threefold increased risk of substantial postpartum weight retention (Table 2). Full adjustment for weight-related covariates and maternal sociodemographics modestly attenuated the effect estimate (odds ratio (OR): 2.54, 95% confidence interval (CI): 1.06, 6.09). When we added the postpartum behaviors to the model, the risk associated with postpartum depression decreased slightly further (OR: 2.38, 95% CI: 0.96, 5.88), suggesting that the impact of postpartum depression on substantial postpartum weight retention may be partly explained by lack of sleep or physical inactivity that may accompany depression. Antenatal depression, either alone or in combination with postpartum depression, was not associated with an increased risk of retaining at least 5 kg at 1 year after delivery (adjusted OR for women with antenatal depression only: 0.61, 95% CI: 0.20, 1.79; for women with depression during both periods: 0.68, 95% CI: 0.16, 2.99).
Table 2.
Associations of antenatal and postpartum depression with weight retention of at least 5 kg at 1 year postpartum
| No antenatal or postpartum depression OR (95% CI) |
Antenatal depression only OR (95% CI) |
Both antenatal and postpartum depression OR (95% CI) |
Postpartum depression only OR (95% CI) |
|
|---|---|---|---|---|
| Model 1: Unadjusted | 1.00 (Referent) | 1.18 (0.52, 2.69) | 1.28 (0.37, 4.41) | 3.00 (1.40, 6.41) |
| Model 2: Model 1+ prepregnancy BMI, gestational weight gain |
1.00 (Referent) | 1.38 (0.59, 3.23) | 1.07 (0.30, 3.78) | 2.76 (1.25, 6.08) |
| Model 3: Model 2 + parity, maternal Sociodemographicsa |
1.00 (Referent) | 0.61 (0.20, 1.79) | 0.68 (0.16, 2.99) | 2.54 (1.06, 6.09) |
| Model 4: Model 3 + potential postpartum mediatorsb |
1.00 (Referent) | — | — | 2.38 (0.96, 5.88) |
Data are from 850 women participating in Project Viva.
CI, confidence interval.
Age, race/ethnicity, income, marital status, and education. N for model 3 = 810.
Sleep, walking, trans fat intake, and television viewing. N for model 4 = 791.
Additional predictors of substantial postpartum weight retention on multivariate analyses were race/ethnicity (OR: 2.71, 95% CI: 1.58, 4.62 for nonwhite vs. white), income (OR: 1.79, 95% CI: 1.08, 2.95 for income ≤ $70,000 per year vs. income > $70,000 per year), marital status (OR: 5.89, 95% CI: 2.33, 14.87 for single vs. married or cohabitating), and gestational weight gain (OR: 2.90, 95% CI: 1.64, 5.11 for excessive vs. adequate gain).
Discussion
In this prospective study, we found that new-onset depression in the early postpartum period was associated with more than a twofold increased risk of substantial weight retention at the end of the first postpartum year after adjustment for weight-related covariates, maternal sociodemographics, and parity. The addition of potential mediators led to a modest attenuation in risk, suggesting that the impact of postpartum depression on weight retention may be partly explained by lack of sleep, diet changes, or physical inactivity that may accompany depression.
The relationship between depression and obesity is complex, and debate exists about directionality. Several recent prospective studies, however, have provided evidence of a causal pathway in which depressive symptoms promote weight gain and weight regain, particularly among women (15–19). Depression may also be a barrier to weight loss in overweight women (20). Among overweight participants seeking weight loss treatment in a large managed care organization, Linde et al. (20) found that women reporting depressive symptoms lost less than half as much weight as women without depression. Our study extends such research to women after childbirth and suggests that depression in the postpartum period may be a barrier to returning to prepregnancy weight.
Previous work evaluating the relationship between BMI and postpartum depression has predominately focused on the hypothesis that an elevated pregravid BMI is associated with depressive symptoms in the postpartum period (14,35). Although women with new-onset postpartum depression in our study had slightly higher prepregnancy BMI and gestational weight gain than those without depression, accounting for pregravid weight and weight gain only slightly attenuated the observed association between postpartum depression and weight retention. Thus, depression appeared to beget postpartum obesity more than follow as a symptom of weight gain.
The need for identifying potentially modifiable determinants of postpartum weight retention is great. Excess weight retained after pregnancy appears to be more physiologically harmful than weight gained at other times in life. This weight is deposited preferentially in central rather than peripheral sites (36), leads to long-term reductions in high-density lipoprotein cholesterol (37), and is associated with adverse maternal and fetal outcomes in subsequent pregnancies (38). If prospective observational and experimental studies confirm that depression precedes postpartum weight retention, new avenues for intervention may be tested before obesity develops.
At least two mechanisms are hypothesized to explain the relationship between postpartum depression and weight retention. In the postpartum period, estrogen and progesterone decline, which is associated with a concomitant fall in serotonin levels (39). Serotonin levels are lower in depressed patients (40). In an effort to regulate serotonin and improve dysphoria, individuals may consume excessive amounts of carbohydrate-rich food, and therefore also increase risk for obesity (19,41,42). Furthermore, low levels of both sex steroids and serotonin may contribute to the dysregulation of hypothalamic–pituitary– adrenal axis functioning (39,40,43), leading to the chronic excessive secretion of cortisol. Higher serum cortisol levels are consistently found in women with postpartum depression (44,45). Cortisol is associated with an increase in appetite and visceral fat accumulation, leading to the development of abdominal obesity (43). Given that excess weight retained after pregnancy appears to be preferentially deposited centrally (36), these neuroendocrine alterations provide a plausible biologic basis for our results.
Alternatively, and perhaps concurrently, depression may cause changes in sleep patterns, physical activity, television habits, and dietary intake that by themselves lead to postpartum weight retention. In a recent cross-sectional analysis, George et al. (46) reported that depressive symptoms were associated with less healthful diets at 1 year postpartum. Lox and Treasure (47) found that high stress levels or major life disruptions impeded exercise activities in the postpartum period. Although these studies did not address changes in weight, it is possible that depression may promote obesogenic behaviors that lead to weight retention postpartum. Our data lend some support to this hypothesis, as the risk associated with postpartum depression decreased when we added postpartum diet and activity behaviors to the model.
The lack of an association between antenatal depression and substantial postpartum weight retention was somewhat unexpected and deserves additional exploration. In our data, women with antenatal depression were more likely to have inadequate weight gain during pregnancy, which is consistent with published literature (48,49). Lower levels of gestational weight gain are associated with less weight retention postpartum (6), and may explain these findings. However, the small number of depressed women in our cohort limits our ability to make precise estimates about antenatal depression.
Several limitations to this study exist. Chief among these is the timing of our measurement of postpartum depression. Because the peak incidence of postpartum depression occurs at ~1–2 months postpartum with only one-third still affected at 6 months after delivery (50,51), we may have underestimated the number of women with postpartum depression in our sample. However, ~90% of mothers who report depressive symptoms at 4 months after delivery had onset of these symptoms by the first month postpartum (52). Thus, the large majority of women with postpartum depression in our sample likely had onset of symptoms early in the postpartum period, but remained symptomatic longer. This feature, along with the high levels of education, income, and white women in our cohort, may limit generalizability of our results. Studies that include a more racially and economically diverse group of women, with a shorter duration of postpartum depression, are necessary to confirm our findings. We also had limited power to detect associations among subgroups of race/ethnicity or prepregnancy BMI, and we were lacking information on concurrent antidepressant use. Only 40% of the eligible study population provided enough information to allow their inclusion in this analysis and may have introduced selection bias; however, included participants did not substantially differ from the overall population in terms of the exposure of interest. Furthermore, our depression instrument is a screening tool, rather than clinician diagnosis. Although the EPDS has been validated in a broad range of populations (27), it remains possible that cultural and/or economic factors may have caused women to overreport or underreport depressive symptoms. We also relied on self-reported weight measurements, but any underreporting bias would likely have been similar for both prepregnancy and postpartum weight.
In summary, our study provides evidence that new-onset postpartum depression is associated with substantial weight retention after childbirth. Given the paucity of prospective work in this area, our data provide important insight into the impact of depression on weight loss postpartum. Future work should examine the extent to which management of depression leads to enhanced postpartum weight loss and thus aids in the prevention of obesity among women.
Acknowledgments
We thank the participants and staff of Project Viva and Dr Gunderson, Division of Research, Kaiser Permanente of Northern California, for her helpful suggestions regarding study design and manuscript revisions. This study was supported by grants from the US National Institutes of Health (HD 34568, HD 64925, HL 68041), Harvard Medical School, and the Harvard Pilgrim HealthCare Foundation. S.J.H. was supported by an Institutional National Research Service Award, #5 T32HP1101-19.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
References
- 1.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 3.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 4.van Dam RM, Willett WC, Manson JE, Hu FB. The relationship between overweight in adolescence and premature death in women. Ann Intern Med. 2006;145:91–97. doi: 10.7326/0003-4819-145-2-200607180-00006. [DOI] [PubMed] [Google Scholar]
- 5.Siega-Riz AM, Hobel CJ. Predictors of poor maternal weight gain from baseline anthropometric, psychosocial, and demographic information in a Hispanic population. J Am Diet Assoc. 1997;97:1264–1268. doi: 10.1016/s0002-8223(97)00303-9. [DOI] [PubMed] [Google Scholar]
- 6.Gunderson EP, Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev. 1999;21:261–275. doi: 10.1093/oxfordjournals.epirev.a018001. [DOI] [PubMed] [Google Scholar]
- 7.Gore SA, Brown DM, West DS. The role of postpartum weight retention in obesity among women: a review of the evidence. Ann Behav Med. 2003;26:149–159. doi: 10.1207/S15324796ABM2602_07. [DOI] [PubMed] [Google Scholar]
- 8.Ohlin A, Rossner S. Maternal body weight development after pregnancy. Int J Obes. 1990;14:475–478. [PubMed] [Google Scholar]
- 9.Schauberger CW, Rooney BL, Brimer LM. Factors that influence weight loss in the puerperium. Obstet Gynecol. 1992;79:424–429. doi: 10.1097/00006250-199203000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Boardley DJ, Sargent RG, Coker AL, Hussey JR, Sharpe PA. The relationship between diet, activity, and other factors, and postpartum weight change by race. Obstet Gynecol. 1995;86:834–838. doi: 10.1016/0029-7844(95)00283-W. [DOI] [PubMed] [Google Scholar]
- 11.Parker JD, Abrams B. Differences in postpartum weight retention between black and white mothers. Obstet Gynecol. 1993;81:768–774. [PubMed] [Google Scholar]
- 12.Gunderson EP, Rifas-Shiman SL, Oken E, et al. Association of fewer hours of sleep at 6 months postpartum with substantial weight retention at 1 year postpartum. Am J Epidemiol. 2008;167:178–187. doi: 10.1093/aje/kwm298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oken E, Taveras EM, Popoola FA, Rich-Edwards JW, Gillman MW. Television, walking, and diet associations with postpartum weight retention. Am J Prev Med. 2007;32:305–311. doi: 10.1016/j.amepre.2006.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carter AS, Baker CW, Brownell KD. Body mass index, eating attitudes, and symptoms of depression and anxiety in pregnancy and the postpartum period. Psychosom Med. 2000;62:264–270. doi: 10.1097/00006842-200003000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 16.McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? J Consult Clin Psychol. 1999;67:177–185. doi: 10.1037//0022-006x.67.2.177. [DOI] [PubMed] [Google Scholar]
- 17.Pine DS, Goldstein RB, Wolk S, Weissman MM. The association between childhood depression and adulthood body mass index. Pediatrics. 2001;107:1049–1056. doi: 10.1542/peds.107.5.1049. [DOI] [PubMed] [Google Scholar]
- 18.Pine DS, Cohen P, Brook J, Coplan JD. Psychiatric symptoms in adolescence as predictors of obesity in early adulthood: a longitudinal study. Am J Public Health. 1997;87:1303–1310. doi: 10.2105/ajph.87.8.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stice E, Presnell K, Shaw H, Rohde P. Psychological and behavioral risk factors for obesity onset in adolescent girls: a prospective study. J Consult Clin Psychol. 2005;73:195–202. doi: 10.1037/0022-006X.73.2.195. [DOI] [PubMed] [Google Scholar]
- 20.Linde JA, Jeffery RW, Levy RL, et al. Binge eating disorder, weight control self-efficacy, and depression in overweight men and women. Int J Obes Relat Metab Disord. 2004;28:418–425. doi: 10.1038/sj.ijo.0802570. [DOI] [PubMed] [Google Scholar]
- 21.Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB. New parents and mental disorders: a population-based register study. JAMA. 2006;296:2582–2589. doi: 10.1001/jama.296.21.2582. [DOI] [PubMed] [Google Scholar]
- 22.Luoma I, Tamminen T, Kaukonen P, et al. Longitudinal study of maternal depressive symptoms and child well-being. J Am Acad Child Adolesc Psychiatry. 2001;40:1367–1374. doi: 10.1097/00004583-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Murray L. The impact of postnatal depression on infant development. J Child Psychol Psychiatry. 1992;33:543–561. doi: 10.1111/j.1469-7610.1992.tb00890.x. [DOI] [PubMed] [Google Scholar]
- 24.Sinclair D, Murray L. Effects of postnatal depression on children’s adjustment to school. Teacher’s reports. Br J Psychiatry. 1998;172:58–63. doi: 10.1192/bjp.172.1.58. [DOI] [PubMed] [Google Scholar]
- 25.Stein A, Gath DH, Bucher J, et al. The relationship between post-natal depression and mother-child interaction. Br J Psychiatry. 1991;158:46–52. doi: 10.1192/bjp.158.1.46. [DOI] [PubMed] [Google Scholar]
- 26.Gillman MW, Rich-Edwards JW, Rifas-Shiman SL, et al. Maternal age and other predictors of newborn blood pressure. J Pediatr. 2004;144:240–245. doi: 10.1016/j.jpeds.2003.10.064. [DOI] [PubMed] [Google Scholar]
- 27.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 28.Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression Scale (EPDS) J Reprod Infant Psychol. 1990;8:99–107. [Google Scholar]
- 29.Thorpe K. A study of the Edinburgh Postnatal Depression Scale for use with parent groups outside of the postpartum period. J Reprod Infant Psychol. 1993;11:119–125. [Google Scholar]
- 30.Dayan J, Creveuil C, Marks MN, et al. Prenatal depression, prenatal anxiety,and spontaneous preterm birth: a prospective cohort study among women with early and regular care. Psychosom Med. 2006;68:938–946. doi: 10.1097/01.psy.0000244025.20549.bd. [DOI] [PubMed] [Google Scholar]
- 31.Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ. 2001;323:257–260. doi: 10.1136/bmj.323.7307.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matthey S, Henshaw C, Elliott S, Barnett B. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale:implications for clinical and research practice. Arch Womens Ment Health. 2006;9:309–315. doi: 10.1007/s00737-006-0152-x. [DOI] [PubMed] [Google Scholar]
- 33.Institute of Medicine NAoS. Nutrition During Pregnancy. Washington, DC: National Academy Press; 1990. [Google Scholar]
- 34.Rifas-Shiman SL, Willett WC, Lobb R, et al. PrimeScreen, a brief dietary screening tool: reproducibility and comparability with both a longer food frequency questionnaire and biomarkers. Public Health Nutr. 2001;4:249–254. doi: 10.1079/phn200061. [DOI] [PubMed] [Google Scholar]
- 35.La Coursiere DY, Baksh L, Bloebaum, Varner MW. Maternal body mass index and self-reported postpartum depressive symptoms. Matern Child Health J. 2006;10:385–390. doi: 10.1007/s10995-006-0075-1. [DOI] [PubMed] [Google Scholar]
- 36.Gunderson EP, Murtaugh MA, Lewis CE, et al. Excess gains in weight and waist circumference associated with childbearing: The Coronary Artery Risk Development in Young Adults Study (CARDIA) Int J Obes Relat Metab Disord. 2004;28:252–235. doi: 10.1038/sj.ijo.0802551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gunderson EP, Lewis CE, Murtaugh MA, et al. Long-term plasma lipid changes associated with a first birth: the Coronary Artery Risk Development in Young Adults study. Am J Epidemiol. 2004;159:1028–1039. doi: 10.1093/aje/kwh146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Villamor E, Cnattingius S. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population-based study. Lancet. 2006;368:1164–1170. doi: 10.1016/S0140-6736(06)69473-7. [DOI] [PubMed] [Google Scholar]
- 39.Bethea CL, Lu NZ, Gundlah C, Streicher JM. Diverse actions of ovarian steroids in the serotonin neural system. Front Neuroendocrinol. 2002;23:41–100. doi: 10.1006/frne.2001.0225. [DOI] [PubMed] [Google Scholar]
- 40.Nemeroff CB. The neurobiology of depression. Sci Am. 1998;278:42–49. doi: 10.1038/scientificamerican0698-42. [DOI] [PubMed] [Google Scholar]
- 41.Wurtman J, Wurtman R, Mark S, et al. d-Fenfluramine selectively suppresses carbohydrate snacking by obese subjects. Int J Eat Disord. 1985;4:89–99. doi: 10.1002/1098-108x(198502)4:1<89::aid-eat2260040110>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 42.Wurtman JJ. Depression and weight gain: the serotonin connection. J Affect Disord. 1993;29:183–192. doi: 10.1016/0165-0327(93)90032-f. [DOI] [PubMed] [Google Scholar]
- 43.Bjorntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2:73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 44.Lommatzsch M, Hornych K, Zingler C, et al. Maternal serum concentrations of BDNF and depression in the perinatal period. Psychoneuroendocrinology. 2006;31:388–394. doi: 10.1016/j.psyneuen.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 45.Taylor A, Littlewood J, Adams D, Doré ;C, Glover V. Serum cortisol levels are related to moods of elation and dysphoria in new mothers. Psychiatry Res. 1994;54:241–247. doi: 10.1016/0165-1781(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 46.George GC, Milani TJ, Hanss-Nuss H, Freeland-Graves JH. Compliance with dietary guidelines and relationship to psychosocial factors in lowincome women in late postpartum. J Am Diet Assoc. 2005;105:916–926. doi: 10.1016/j.jada.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 47.Lox CL, Treasure D. Changes in feeling states following aquatic exercise during pregnancy. J App Soc Psychol. 2000;30:518–527. [Google Scholar]
- 48.Hickey CA, Cliver SP, Goldenberg RL, McNeal SF, Hoffman HJ. Relationship of psychosocial status to low prenatal weight gain among nonobese black and white women delivering at term. Obstet Gynecol. 1995;86:177–183. doi: 10.1016/0029-7844(95)00161-j. [DOI] [PubMed] [Google Scholar]
- 49.Siega-Riz AM, Hobel CJ. Predictors of poor maternal weight gain from baseline anthropometric, psychosocial, and demographic information in a Hispanic population. J Am Diet Assoc. 1997;97:1264–1268. doi: 10.1016/s0002-8223(97)00303-9. [DOI] [PubMed] [Google Scholar]
- 50.Beeghly M, Weinberg MK, Olson KL, et al. Stability and change in level of maternal depressive symptomatology during the first postpartum year. J Affect Disord. 2002;71:169–180. doi: 10.1016/s0165-0327(01)00409-8. [DOI] [PubMed] [Google Scholar]
- 51.Gavin NI, Gaynes BN, Lohr KN, et al. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 52.Coates AO, Schaefer CA, Alexander JL. Detection of postpartum depression and anxiety in a large health plan. J Behav Health Serv Res. 2004;31:117–133. doi: 10.1007/BF02287376. [DOI] [PubMed] [Google Scholar]