Borderline personality disorder (BPD) is a major mental disorder characterized by instability in interpersonal relationships, affect, self-identity, behavior, and cognition (American Psychiatric Association, 2000). The prevalence of BPD may be as high as 5.9% (99% CI = 5.4 to 6.4), according to a recent national epidemiologic survey (Grant, Chou, Goldstein, et al, 2008). Previous estimates have been lower, ranging from 0.2% to 1.8% in the general population (Torgersen, Kringlen, & Cramer, 2001). Because of the population rate and the seriousness of the disorder, individuals with BPD utilize a disproportionately large percentage of mental health services (Bender et al., 2001; Zanarini, Frankenburg, Khera, & Bleichmar, 2001).
BPD is associated with a particularly high risk for self-inflicted injury (SII), both suicide attempts and nonsuicidal self-injury. Up to 10% of individuals with BPD die by suicide (Stone, Stone, & Hurt, 1987; Paris, Brown, & Nowlis, 1987; Pompili, Girardi, Ruberto, & Tatarelli, 2005) and approximately 75% have attempted suicide (Frances, Fyer, & Clarkin, 1986; Stone, Hurt, & Stone, 1987; Shearer, Peters, Quaytman, & Wadman, 1988). In recent psychological autopsy studies, 25% to 33% of completed suicides have been reported to meet criteria for BPD (Schneider B, Wetterling T, Sargk D et al, 2006; Runeson, & Beskow, 1991). As many as 69 to 75% of patients with BPD have engaged in SII at least once (Clarkin, Widiger, Frances, Hurt, & Gilmore, 1983; Grove & Tellegen, 1991; Stone, 1993). Thus, there is an urgent need to clarify the factors that maintain these behaviors among persons with BPD.
Despite diverging theoretical perspectives regarding the core features of BPD, a common thread across theories is that SII is related to severe emotion dysregulation in BPD (Conklin & Westen, 2005; Linehan, 1993; Linehan, Bohus, & Lynch, 2006; Putnam & Silk, 2005). Linehan's (1993) biosocial theory of BPD emphasizes the importance of self-invalidation and shame in the development and maintenance of self-inflicted injury (SII). Similar to others (Baumeister, 1990; Chapman, Gratz, & Brown, 2006; Maris, 1981; Shneidman, 1993), the biosocial model of BPD poses that SII functions to escape and/or avoid aversive emotions.
Although Linehan has suggested that BPD is characterized by dysregulation across a range of both positive and negative emotions (Linehan, Bohus, & Lynch, 2006), it has been argued that shame is the emotion in BPD most strongly linked with chronic suicidality, non-suicidal self-injury (NSSI), anger, and impulsivity (Linehan, 1993; Lester, 1998; Stiglmayr, Grathwol, Linehan, Ihorst, Fahrenberg, Bohus, 2005). Shame is a highly aversive self-conscious emotion, similar to self-contempt, involving a global belief that one is socially unacceptable or immoral (Lewis, 1971; Crow, 2004; Tangney & Dearing, 2002), sometimes referred to as internal shame (Gilbert, 1998). When individuals experience shame they also frequently believe that others view them in a similar negative manner, sometimes referred to as “external shame”, which is associated with tendencies to hide aspects of the self or behaviors that could lead to being rejected by others (Gilbert, 1998). In contrast, guilt is emotional distress associated with a focus on one's particular misdeeds and action tendencies to fix the problem behaviors and to repair damaged relationships.
A variety of verbal and nonverbal behaviors occur during and following shame (Tracey et al, 2007). For instance, for some individuals, action tendencies that accompany shame include hiding (to prevent further social rejection) and acting submissive (to appease others). For others, displays of anger toward other people occurs to alleviate suffering by redirecting attention from the self toward others (Keltner & Harker, 1998).
There are several reasons to hypothesize that shame is a specific emotional precursor of both suicidal behaviors and NSSI among persons with BPD. A recent study found that women with BPD demonstrated higher levels of shame-proneness on both explicit self-report measures and implicit association measures of shame, compared with non-psychiatric controls and controls with social phobia (Rüsch, Lieb, Göttler, Hermann, Schramm, Richter, Jacob, Corrigan, & Bohus, 2007). Another study found that women with BPD and PTSD did not show greater shame proneness (on both implicit and explicit shame measures) compared with women with BPD who did not have PTSD (Rüsch, Corrigan, Bohus, Kühler, Jacob, Lieb, 2007). Therefore, there is evidence that heightened shame-proneness is more specific to BPD than other disorders, and is not related to trauma symptoms per se. Further, some researchers have even conceptualized BPD as a chronic shame response – the intense feeling that one will never be good enough (Crowe, 2004).
Several empirical studies have specifically examined the relationship of shame-related constructs with suicide ideation and behavior. Two studies found that current and future suicide ideation is associated with shame (Hastings, Northman, & Tangney, 2000; Lester, 1998) and negative self-concept (Kaplan & Pokorny, 1976). Negative self-concept predicted, independently of depression, both suicide attempts (Lewinsohn, Rohde, & Seeley, 1994) and suicide (Beck, & Stewart, 1989). One longitudinal study found that shame-proneness in the 5th grade predicted later suicide attempts by young adulthood (Tangney & Dearing, 2002). Three studies showed that a substantial proportion of overdoses occurred in the presence of shame-related thoughts and emotions: 45% of overdoses were reported to occur when participants were feeling lonely or unwanted (e.g., sadness and shame), 45% occurred when participants were feeling like a “failure” (e.g., shame) (Bancroft, Skrimshire, & Simkins, 1976; Birtchnell & Alarcon, 1971; Hawton, Cole, O'Grady, & Osborn, 1982). Baumeister (1990) suggested that suicide may be sought as a complete and permanent way to escape from painful self-awareness and hide from the shameful scrutiny of others, especially when individuals feel hopeless about changing their shameful qualities (cf. Rizvi & Linehan, 2005).
Theories regarding shame also suggest that this emotion may be specifically associated with NSSI. One important function of shame is to restore important relationships and community bonds by motivating the individual to acknowledge wrongdoing and accept punishment (Keltner & Harker, 1998). When the global self-evaluations of being bad or immoral become extreme, the self-hatred can lead to self-punishment. SII is often an extreme act of self-punishment among persons with BPD (Brown et al., 2002). Indeed, self-punishment is a strategy they may distinguish individuals with BPD from persons with other clinical disorders such as depression (e.g., Rosenthal, Cukrowicz, Cheavens, & Lynch, 2006), and is a common motive for engaging in NSSI among persons with BPD (Brown, Comtois, & Linehan, 2002; Kleindienst, Bohus, Ludaescher, Limberger, Kuenkele, Ebner-Priemer, Chapman, Reicherzer, Stieglitz, & Schmahl, 2008). Typical triggers for shame, such as rejection and failure, also trigger a majority of nonsuicidal SII acts (Herpertz, 1995).Furthermore, shame can interfere with changing dysfunctional behaviors such as SII. People with BPD frequently report shame both about things that trigger their SII and about their own SII actions (Kleindienst et al., 2008). A common action tendency associated with shame involves hiding or concealing the personal characteristics (e.g., sexual orientation), past experiences (e.g., childhood sexual abuse), or behaviors (e.g., SII) that the person believes are socially unacceptable. As a result, people who feel shame in relation to their SII may be especially likely to continue SII, because concealment of the problems from other people interferes with getting help. Although other emotions are likely associated with SII, the link between shame and SII may be especially strong since shame is most associated with self-hatred and hiding problems in therapy.
Several key limitations have characterized the research on emotions and SII. First, studies have often relied on self-report measures of emotions. Given that the emotion system is complex and includes many different components (Gross, 1998), there is a need to assess emotions using a multi-method approach. Furthermore, these studies are often primarily based on questionnaires that ask about general levels of emotions without contextual prompts related to SII. As emotional experiences frequently fluctuate in response to a variety of internal and external stimuli, time of day, and other factors, these context-free ratings of emotional state are less likely to capture the types of emotional experiences directly related to SII. It is likely that measures of emotional states in the presence of contextual prompts related to SII will be more effective predictors of SII than measures of general levels of emotion. Third, few studies have examined emotional states as prospective predictors of SII. Studies have examined emotion or personality variables in relation to past history of SII among persons with BPD (e.g., Dulit, Fyer, Leon, Brodsky, & Frances, 1994), but factors related to past history of SII do not necessarily predict the future occurrence of these behaviors. To our knowledge, no published study has examined the association of shame with future suicidal or non-suicidal SII in BPD.
Our primary objective in the present study was to examine the prospective association of shame with the occurrence of future SII. We addressed the limitations of prior studies in several ways. We examined shame as a prospective predictor of SII among persons with BPD over a 12-month period, using a multi-method approach. We measured shame as well as other emotional states in three different ways: self-report of emotions, facial coding of emotional expressions, and observer ratings of state emotions. Furthermore, we measured these emotional states while participants discussed the events that triggered their recent episodes of SII, allowing us to examine emotional states that occur in the presence of relevant contextual prompts.
We hypothesized that women with BPD who evidence higher levels of shame while discussing the triggering events for their own previous SII will be likely to more quickly repeat SII in the future. Further, we hypothesized that shame would be specifically and uniquely associated with prospective SII beyond the influence of other negative emotions. To test this hypothesis, we controlled for other emotions that also showed a positive association to SII in order to test if the observed correlations can be explained by unique aspects of shame rather than general negative emotionality. Finally, supplemental exploratory analyses examined whether shame or other emotions predicted the level of suicide intent (intent to produce death as a result of SII) associated with episodes of SII.
Method
Participants
Participants were 77 women (Mage = 30.0 years, SD = 7.3) enrolled in a randomized clinical trial of Dialectical Behavior Therapy (DBT; Linehan, 1993) for BPD and self-inflicted injury (SII; i.e., either suicide attempts, NSSI or both)1. Inclusion criteria were: (a) diagnosis of BPD; (b) female gender; (c) 18-45 years of age; (d) current and repeated SII (operationalized as at least one SII episode within the last eight weeks and at least one additional episode in the past 5 years); and (e) consent to outpatient therapy for treatment of suicidal behavior. Exclusion criteria were: (a) psychotic disorders (except independent diagnoses of psychotic depression, brief psychotic disorder, or substance-induced psychotic disorder); (b) bipolar disorder, (c) epilepsy or other severe seizure disorder; (d) problems that require priority intervention including life-threatening anorexia or current and chronic absence of shelter); (e) IQ of less than 70, (f) conditions that precluded freely dropping-out of treatment (e.g. court order); and (g) received prior DBT.
General Procedures and Assessment Schedule
Participants who met the screening criteria completed questionnaire measures of state emotions, in addition to repeated assessments of suicide attempts and NSSI. After completing all pre-treatment assessments, participants received weekly individual therapy for one year – either DBT or Community Treatment by Experts in the Seattle community, representing a variety of non-behavioral theoretical orientations (see Linehan, Comtois, Murray, Brown, Gallop, Heard, Korslund, Tutek, Reynolds, & Lindenboim,. 2006, for complete description of treatment conditions). Assessments occurred at 4-, 8- and 12-months. Four participants who failed to complete an assessment beyond pre-treatment have been excluded from the analyses, resulting in a final sample size of 73 participants.
Structured Interview Measures
Borderline personality disorder diagnosis was made with the Personality Disorders Examination (PDE; Loranger, 1995) and confirmed on the Structured Clinical Interview for DSM-IV (SCID-II; First, Spitzer, Gibbon, & Williams, 1997). The SCID was also used to assess Axis I diagnoses (SCID-I; First, Spitzer, Gibbon, & Williams, 1995). The raters agreed perfectly on the presence of BPD diagnosis using the PDE and the SCID-II. Inter-rater reliability was acceptable for Axis I disorders (κ =.79 to .97, above 80 percent agreement for low-prevalence disorders).
The Suicide Attempt - Self-Injury Interview – long version (SASII; Linehan, Comtois, Brown, Heard, & Wagner, 2006) is a 47-item semi-structured interview of SA and NSSI that measures the topography, suicidal and other intent, medical severity, expectation of death, social context, precipitating and concurrent events, and outcomes for single episodes (or clusters of multiple similar acts undistinguishable on any factor other than time). Based on all information obtained, the interviewer classifies the episode as a suicide attempt or NSSI.
Using the SASII, the interviewer classifies SII at the level of an act or an episode. An act consists of a single act of SII, whereas an episode is a discrete cluster of acts that occur so repetitively and closely in time that each individual act within the cluster cannot be distinguished from other acts (e.g., cutting for 15 days in a row) (Linehan, Comtois, Brown, et al., 2006). The focus of our study was on episodes of SII. The initial validation study of the SASII, which included the present sample, found that SASII ratings of SII corresponded highly with the occurrence of SII episodes recorded in the therapists’ notes and participants’ daily self-monitoring forms within specified time frames (Linehan, Comtois, Brown, et al., 2006).
Measures of Emotional States during the SASII Interview
Current emotional states were measured during and following parts of the pre-treatment SASII interview in which participants described in detail the triggering events for their most recent pre-treatment SII episode, including corresponding thoughts and emotions. The multi-modal measurement of emotional states occurred in the following manner: (1) the Positive and Negative Affect Schedule (PANAS; Watson & Clark, 1988) was administered before and after these interview segments, (2) the Emotion Facial Affect Coding System (EMFACS; Ekman & Friesen, 1975, 1978) emotion coding occurred throughout the interview segments, and (3) the assessor made observer ratings of emotional state using the PANAS before and after the SASII. The segments began when the interviewer asked, “So tell me a little about what led up to your hurting yourself, how you did it and how it all turned out,” and ended with the answers to specific questions about triggering events, thoughts, and emotions for self-injury (M = 14.8 min). Other studies have successfully used similar structured recall methods to experimentally replicate the emotional experiences that surround self-mutilation (Haines, Williams, Brain, & Wilson, 1995). Shame was the independent variable, and anger, contempt, disgust, fear and sadness were used as covariates when they showed positive associations to SII.
The Positive and Negative Affect Schedule-Revised (PANAS; Watson & Clark, 1988) is a self-report measure that includes scales for four specific emotional states relevant to our study: shame (1 item), guilt (1 item), sadness (1 item), anger (2 items), and fear/anxiety (4 items). For the current study, six of the shame items (“Self-conscious,” “Stupid,” “Deserving of criticism,” “Helpless,” “Embarrassed,” “Regretful”) from the Personal Feelings Questionnaire (Harder & Lewis, 1987) were added to the original 20-item PANAS for a total of 7 shame items. Participants rated emotion adjectives on the extent to which they described their emotional states “right now... at the present moment” on a 5-point Likert scale. The Cronbach's alpha for the new shame scale indicated good internal consistency (α = .91). Consistent with standard emotion taxonomies (e.g., Shaver, Schwartz, Kirson, & O'Conner, 1987), fear and anxiety were collapsed into a single category (contempt and disgust are not measured on the PANAS). The PANAS was given immediately before (pre-SASII) and after (post-SASII) the emotionally-evocative segment of the SASII. The internal consistencies (Cronbach's alphas) were high for pre-SASII ratings made by participants: fear (.864), anger (.718), shame (.890), and for post-SASII ratings: fear (.937), anger (.945), shame (.961). As mentioned, assessors also made observer pre- and post-SASII PANAS ratings of participants’ emotional state. The internal consistencies (Cronbach's alpha) for pre-SASII ratings made by assessors were: fear (.824), anger (.883), shame (.912), and for post-SASII ratings: fear (.953), anger (.962), shame (.973). The guilt and sadness items were not analyzed in this study because of the poor reliability of single-item scales.
The Emotion Facial Affect Coding System (EMFACS) and Shame Coding
Nonverbal emotion behaviors were coded from videotapes of the emotionally-evocative SASII segments. The investigator (MB) and an undergraduate research assistant learned FACS through the standard self-study course (Ekman & Friesen, 1978). After passing the FACS certification test (reliability with FACS authors), these individuals coded videotapes until inter-rater reliability was achieved. Two other research assistants (who did no EMFACS coding) watched videotapes with the investigator to determine the threshold to use in assigning dichotomous codes to continuous shame behaviors (i.e., the presence versus absence of eye and head movements downward). After achieving agreement on coding thresholds, they coded videotapes until inter-rater reliability was achieved. Videotapes of participants in other research studies were used for training in EMFACS and shame coding. To assess inter-rater reliability, the investigator coded randomly selected 90-second intervals for each tape using EMFACS (22% of total time). Most tapes coded by the investigator were done in the reverse order as the primary coder to help ensure that the coding is consistent between coders and is also consistent over time (i.e., no coder “drift”). The coding data from the investigator was not used in any analysis. To assess the reliability of shame coding, the second shame coder recorded shame behaviors for 29 (51%) of the tapes. To minimize bias, all tapes were coded without sound and in random order. The research assistant performed EMFACS coding on two smaller segments within the larger emotionally-evocative SASII segments (mean total time = 5.0 min; coding only several minutes of videotape is the standard in EMFACS research, Ekman & Rosenberg, 1997). The first segment was the first two minutes of the answer to the first SASII question about recent SII triggers. The second segment was the complete answer to the final three questions, which ask about specific environmental events, emotions, thoughts, and behaviors that triggered the SII.
Anger, contempt, fear, and sadness were coded according to established EMFACS guidelines (Ekman & Friesen, 1975, 1978). EMFACS is an abbreviated version of the Facial Action Coding System (FACS). This method is an anatomically based method to code the facial action combinations that most uniquely identify anger, contempt, disgust, fear, and sadness (Ekman & Friesen, 1975, 1978). The primary investigator (MZB) and the undergraduate coder passed the FACS certification test (reliability with FACS authors). Coding occurred in real time, but frame-by-frame (slow-motion) viewing was used as necessary. Rather than having coders generate emotion inferences, EMFACS coders record specific objective facial movements that are later translated into emotion categories once coding is completed. Many studies have demonstrated the reliability and validity of EMFACS (Biehl, Matsumoto, Ekman, Hearn, Heider, Tsutomu, & Ton, 1997; Ekman & Friesen, 1975, 1978; Ekman & Rosenberg, 1997; Gosselin, Kirouac, Dore, 1995; Matsumoto, 1992).
Shame, which is not coded in the EMFACS, was coded in this study based on empirical descriptions of shame behaviors, which emphasize eye gaze downward and head lowering (Izard, 1971; Keltner & Harker, 1998). A single undergraduate student recorded the duration that each participant did not make eye contact with the interviewer (including eyes lowered, covered, or closed) and lowered the head. The shame analysis variable was computed by adding the proportion of time during which the participant displayed no eye contact with the proportion of time during which the participant's head was lowered. Unfortunately, there is no known method for coding nonverbal guilt behaviors.
To assess inter-rater reliability of EMFACS coding, the primary investigator conducted facial coding for one randomly-selected 90-second interval for each video (within the emotionally-evocative segment). To assess inter-rater reliability of the shame coding, a second shame coder (an undergraduate student) recorded shame behaviors for the entire the emotionally-evocative segment for 29 (51%) of the videos. Pearson correlations yielded the following reliability coefficients: anger, .77; contempt, .82; disgust, .91; sadness, .77; fear, .78; shame, .90. The validity of the shame coding is suggested by Pearson correlations showing that higher nonverbal shame scores were associated with more shame reported before (pre-SASII PANAS; r = .55, p < .001) and after the coded segment (post-SASII PANAS; r = .26, p = .06). Emotion blends (i.e., concurrent expressions of different emotions) were not analyzed in this study.
Missing Data
Some of the 77 participants failed to complete some of the measures during the study. The number of participants who completed the SASII at pre-treatment, 4, 8, and 12-month assessments were: 77, 71, 53, and 58, respectively, due to missed or shortened assessments . Videotapes for 20 (26%) participants were not coded for emotions because of video recording errors, leaving 57 participants for subsequent analyses, except where otherwise reported.
Results
Descriptive Statistics
The majority of the 77 participants were Caucasian (84%; 4% African-American, 2% Asian-American, 10% other), had a high-school education (90%; 22% were college graduates), and earned less than $10,000 per year (72%). Eighty two per cent met criteria for current major depressive disorder or dysthymia, 76% met criteria for at least one current anxiety disorder, and 27% met criteria for a current substance use disorder.
See Table 1 for descriptive statistics for self-inflicted injury (SII). In the six months before treatment, 66% of participants reported engaging in a suicide attempt (SA), and 82% reported non-suicidal self-injury (NSSI). During the treatment year, 27% of participants reported SA and 70% reported NSSI (13% reported neither). Descriptive statistics on the emotion predictors are presented in Tables 1 and 2.
Table 1.
Descriptive Statistics for Predictors and Dependent Variables (N = 77)
| Mean | SD | Median | IQ Range | |
|---|---|---|---|---|
| Pre-treatment, last six months | ||||
| Total SII acts | 12.3 | 21.4 | 4.0 | 2.0-10.0 |
| Suicidal acts | 1.2 | 1.5 | 1.0 | 0.0-1.8 |
| Nonsuicidal acts | 11.1 | 21.4 | 2.0 | 1.0-8.0 |
| Days from the most recent SII until the pre-treatment assessment |
27.7 |
21.0 |
22.0 |
14.0-37.5 |
| First four-months of Treatment Year | ||||
| Total SII acts | 5.3 | 14.9 | 2.0 | 0.0-3.0 |
| Suicidal attempts | 0.3 | 0.7 | 0.0 | 0.0-0.0 |
| Nonsuicidal acts |
5.0 |
15.0 |
1.0 |
0.0-3.0 |
| Treatment year | ||||
| Total SII acts | 12.5 | 51.0 | 2.0 | 1.0-6.5 |
| Suicidal acts | 0.5 | 1.0 | 0.0 | 0.0-1.0 |
| Nonsuicidal acts | 12.0 | 51.0 | 2.0 | 0.0-6.0 |
| Days to first SII episode | 82.7 | 98.6 | 40.0 | 22.0-97.0 |
| Days to first suicide attempt | 132.6 | 117.0 | 87.0 | 48.0-168.0 |
| Days to first nonsuicidal SII |
72.0 |
88.1 |
34.0 |
21.0-97.0 |
| Self-Report State Emotion (post-SASII PANAS) | ||||
| Anger | 2.0 | 1.2 | 1.5 | 1.0-2.8 |
| Fear | 2.5 | 1.1 | 2.5 | 1.5-3.3 |
| Shame | 2.9 | 1.2 | 3.1 | 1.9-3.9 |
| Guilt | 2.7 | 1.4 | 3.0 | 1.0-4.0 |
“IQ Range” = Interquartile range; SII=Self-Inflicted Injury; SASII=Suicide Attempt and Self-Injury Interview; PANAS=Positive and Negative Affective States; EMFACS= Emotion Facial Affect Coding System
Table 2.
Descriptive Statistics for Emotion Coding during SASII interview (N = 57)
| % Ss, any | Median | IQ Range | |
|---|---|---|---|
| Shame | 100.0 | 25.6% | 15.9-55.1% |
| Contempt | 98.2 | 1.8 | 0.8-2.8 |
| Sadness | 62.5 | 0.3 | 0.0-0.9 |
| Disgust | 60.7 | 0.2 | 0.0-0.8 |
| Fear, any | 46.4 | 0.0 | 0.0-0.6 |
| Fear, upper face | 33.9 | 0.0 | 0.0-0.3 |
| Anger | 17.9 | 0.0 | 0.0-0.0 |
The percent of time engaging in shame behavior is reported. For all other emotions (EMFACS), number of expressions per minute is reported.
Data Analytic Strategy
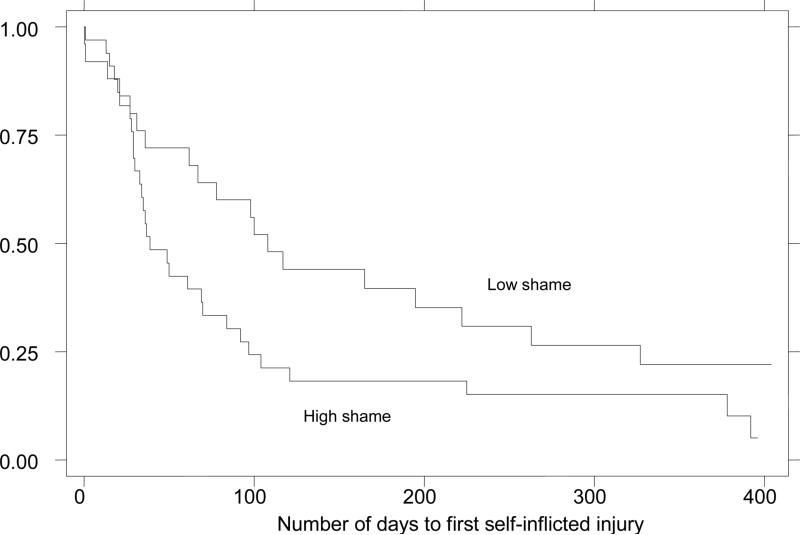
We evaluated shame as a prospective predictor of SII using two Cox regression survival analyses (two-tailed tests) for each of our primary hypotheses. For each hypothesis, we first used standard univariate Cox regression to predict the first SII, followed by a multivariate Cox regression using a marginal model with a robust standard error and stratified by the number of SII episodes to account for the non-independence of SII episodes per individual (Wei, Lin, & Weissfeld, 1989). These two Cox regressions allowed us make use of all relevant information on SII, including whether it occurred during the period of observation, how many times it occurred, and the time to SII episodes. The proportional hazards assumption was met, as can be seen in the Survival graph (Figure 1). For each Cox regression analyses binary predictor variables were used to make the hazard ratio easier to interpret (high vs. low on each emotion computed via a median split), and the number of pretreatment SII episodes (last six months) and other emotion variables were entered as covariates if they significantly predicted SII.
Figure 1.
Kaplan-Meier Survival Plot for High versus Low Self-reported State Shame During Discussion of Recent Self-Inflicted Injury
Figure Note: On the X-axis, 0 days indicates the day of the pre-treatment SASII interview. The Y-axis indicates the proportion of the sample with no SII since pre-treatment. High and low shame groups were formed based on a median split of the post-SASII PANAS shame scores.
To examine emotions as prospective predictors of suicidal intent of SII, multiple regression were used to examine the association of pre-treatment levels of emotions with average suicide intent of SII during the treatment year, with average suicide intent of SII during the past six months entered as a covariate.
Examination of potential covariates
Prior to each analysis of shame as a predictor of SII, we examined the associations of self-reported, non-verbal, and observer-rated anger, fear, and sadness with prospective SII to determine whether these variables should be controlled as covariates. Self-reported and observer-rated fear (post-PHI SASII), and EMFACS sadness were associated with SII, and thus were includes as covariates in their respective analyses. EMFACS fear and the measures of anger, contempt, and disgust showed no positive association to SII; thus, we did not include any of them as covariates.
Self-reported state emotions as predictors of SII
The univariate survival analysis revealed that participants reporting the highest state shame (post-SASII PANAS) had almost twice the risk of subsequent SII compared to those reporting relatively lower state shame (Relative Risk Ratio[RR] = 1.88, 95% confidence interval [C.I.] = 1.04-3.38, p = .036; see Figure 1). The median time to first SII was 39 days for high-shame participants in contrast to 100 days for those with low shame. At 100 days into treatment, 76% of the high shame participants and 50% of the low shame participants had repeated SII. However, shame did not predict the first SII when controlling for fear (RR = 1.68, p = .169). Anger was not entered as a covariate because higher levels of these expressions were not related to higher risk of SII. In the multivariate survival analysis, shame was not associated with a significantly higher risk of multiple SII episodes (RR = 1.41, p = .376).
Observer-rated state emotions as predictors of SII
Participants high in shame, according to the assessors’ post-SASII ratings, had over twice the risk of subsequent self-injury compared to those reporting low state shame, both in the univariate (RR = 2.41, p = .047) and multivariate survival analyses (RR = 2.80, p = .005). However, shame did not predict SII when controlling for fear (RR = 1.61, p = .172). Anger was not entered as a covariate in either survival analysis because higher levels of these expressions were not related to higher risk of SII.
Nonverbal emotion ratings as predictors of SII
The univariate survival analysis revealed that participants showing the most shame behaviors (post-SASII PANAS) had almost twice the risk of subsequent SII compared to those showing fewer shame behaviors (RR = 1.99, 95% C.I. = 1.07-3.69, p = .033; survival graph is very similar to Figure 1). The median time to first SII was 37 days for high-shame participants in contrast to 97 days for those with low shame. At 100 days into treatment, 78% of the high shame participants and 50% of the low shame participants had repeated SII. In this analysis, shame behaviors predicted the first SII while controlling for sadness and fear expressions (RR = 1.86, p = .048). The multivariate survival analysis revealed that participants showing the most shame behaviors had over three times the risk of subsequent SII episodes (RR = 3.54, 95% C.I. = 1.74-7.18, p = .001) compared to those showing fewer shame behaviors, even after controlling for sadness and fear expressions (RR = 3.66, p = .001). Anger, contempt, and disgust, were not entered as covariates in the either survival analysis because higher levels of these expressions were not related to higher risk of SII.
To ensure that the binary emotion predictor variables did not yield misleading results, we repeated all Cox regression analyses using continuous emotion variables, which yielded almost identical results.
Exploratory Analyses
Prospective prediction of suicidal intent of SII over one year (n = 49)
Average suicide intent was calculated for SII episodes during the treatment year for participants who engaged in any SII, was not significantly associated with any of the measures of shame.
Discussion
We hypothesized that individuals with higher levels of shame would have an increased risk of SII, a combination of a higher likelihood of engaging in SII episodes and engaging in SII sooner in the course of psychosocial treatment. Although self-reported shame was associated with an increase risk of SII, this association did not hold up after controlling for fear. This finding could mean that negative self-reported emotions generally, rather than shame specifically, are associated with future SII. This finding could also reflect the fact that an inherent facet of shame is the fear of rejection, which may be the part of shame that drives self-injury. When feeling ashamed, individuals frequently experience other emotions too, including sadness (over their social disconnection) and anger (over being de-valued by others; Tracey et al, 2007). In contrast, the finding that greater levels of non-verbal shame expressions were associated with an increase risk of SII after controlling for sadness and fear suggests that facial expressions of shame during discussions of past SII may uniquely predict future SII. Therefore, our findings provided partial support for our hypothesis that shame is a specific and unique predictor of SII among persons with BPD, supporting the theories of Linehan (1993), Baumeister (1990) and Maris (1981), all of which emphasize the role of self-conscious emotions in SII.
The unique association of facial expressions of shame with future SII must be considered in conjunction with our procedures. Specifically, we coded shame expressions during discussions of previous SII episodes. As a result, heightened shame during such discussions may reflect (a) the individual's actual emotional responses prior to past SII acts, or (b) the individual's typical shame responses following past SII, or (c) the individual's typical response during discussions of events leading up to SII or to SII itself.
All of these possibilities suggest that impaired problem solving may be one possible causal mechanism explaining why shame is associated with future SII. Given that one of the primary behavioral tendencies associated with shame involves hiding (Keltner & Harker, 1998), individuals who feel intense shame may be reluctant to thoroughly discuss in therapy the life events or behaviors, including SII, about which they feel ashamed, thereby missing opportunities to work on the reduction of this behavior in treatment. It is also possible that the intense arousal that accompanies shame interferes with learning and processing new information during problem solving. Baumeister's (1990) theory of suicidal behavior poses that aversive self-focused emotions precipitate a state of “cognitive deconstruction”, involving difficulty thinking and problem solving as well as a narrowing of attention to the proximal goal of eliminating distress. Future research, therefore, might examine the interplay between shame, active problem solving, and SII.
If the levels of state shame among our participants resemble their actual emotional responses prior to past SII acts, then it is possible that shame prior to SII may also be a marker for individuals’ tendencies toward self-denigration or self-punishment. In turn, individuals with greater tendencies toward self-punishment may be especially likely to repeat SII over time, as self-punishment is among the most commonly reported motivations for SII among women with BPD (Brown et al., 2002). Individuals with BPD appear to be especially likely to use self-punishment as an emotion regulation strategy (Rosenthal Cukrowicz, Cheavens and Lynch, 2006), and some evidence suggests high levels of shame prior to the acts of SII (Kleindienst et al., 2008).
Existing treatments may reduce shame, but empirical evidence is scarce and few treatment studies measure shame as an outcome variable. Cognitive therapy may be part of an effective therapy for shame since there is evidence that it can improve self-concept (Rush, Beck, Kovacs, Weissenburger, & Hollon, 1982). Another promising approach is the DBT exposure-based intervention called Opposite Action and preliminary evidence suggests its effectiveness in reducing shame among individuals with BPD (Rizvi & Linehan, 2005; Brown & Rizvi, 2006).
Limitations and Future Directions
Several limitations of this study warrant consideration. Although our observer ratings of shame were prospectively associated with SII, further work is needed to examine the reliability and validity of this method of coding shame. Given the clinical importance of shame, and the findings of the present study, it seems the development and refinement of a valid coding system for shame expressions is strongly needed. There is likely an imperfect association of the coded “shame” behaviors with the internal experience of shame, dependent upon the social context of measurement. A variety of verbal and nonverbal behaviors occur during and following shame, including hiding, acting submissive, and showing anger toward other people (Keltner & Harker, 1998; Tracey et al, 2007). In addition, the construct validity of the shame prediction will be improved if future analyses control for guilt to establish whether unique aspects of shame are responsible for SII recurrence. There is considerable overlap between shame and guilt, and several studies have shown that unique aspects of shame (i.e., “shame-free guilt”) are generally much more maladaptive than “guilt-free shame” (Tangney & Dearing, 2002). Although our inclusion of multiple modes of measurement of multiple emotions was a significant strength of this study, an additional limitation was the absence of a measure of emotional states close in time to the actual occurrence of SII episodes. It is possible that our specific context of emotion measurement may have obscured detection of other relevant emotions, such as anger, that other studies have found are common antecedents to self-injury. Additionally, future studies might also include measures of positive emotions, which may serve as protective factors against future SII.
This study also did not analyze the predictors separately for suicide attempts and nonsuicidal SII, although other research suggests that the two behaviors may have somewhat different functions (e.g., Brown et al, 2002). There were too few suicide attempts to analyze with adequate power. It is important that future studies analyze the predictors of suicide attempts separately from nonsuicidal SII. Our analyses of suicide intent somewhat mitigate this limitation.
It is quite possible that the specific pattern of findings for the present study may not generalize to other samples of individuals with BPD. Our sample included treatment-seeking, suicidal women with BPD who were enrolled in a randomized clinical trial. The prospective associations of emotions with SII for individuals receiving ongoing treatment may be different from the associations among these variables for people with BPD under non-treatment, naturalistic conditions. Indeed, the findings of the present study may be considered most relevant to the prediction of treatment outcomes, particularly given that DBT often focuses on the reduction of SII. In addition, this sample was entirely women, predominantly white, highly educated, and unemployed. The demographic characteristics of this sample suggest that we must take caution in generalizing our findings to other individuals with BPD or suicidal behaviors. Another limitation of this study had to do with our somewhat small sample size. These results must be replicated with a larger sample before firm conclusions can be drawn.
Another limitation concerns the issues of sample size, power, and multiple comparisons. As this study had a relatively small sample size, the risk of type-II error was elevated, and some of the associations among variables may have been significant with a larger sample size. A blanket correction for cumulative type I error would have resulted in a further loss of statistical power (Keppel & Wickens, 2004); thus, our approach was most consistent with that of Cohen and colleagues (Cohen, Cohen, West, & Aiken, 2003), who recommend that researchers balance “...Type I and Type II errors in a manner consistent with the substantive issues of the research” (p. 183). Nevertheless, future studies with larger samples are clearly needed.
Our findings have important clinical implications and suggest several future research directions. Future treatment development efforts might focus specifically on ways to help persons with BPD reduce or regulate aversive states of shame in the moment. Such interventions may involve cognitive therapy strategies (e.g., targeting beliefs such as “I am bad and deserve punishment.”) or behavioral exposure-based interventions (Rizvi & Linehan, 2005). Research could also evaluate if the shame effect is specific to SII, or whether it also predicts other dysfunctional behaviors (e.g., non-suicidal drug abuse) among BPD individuals.
ACKNOWLEDGEMENTS
This research was supported by the National Institute of Mental Health Grants 5 RO1 MH34486 and K05 MH01593 to Marsha Linehan, and National Research Service Award to Milton Brown.
The authors extend their gratitude to the therapists, clients, and staff at the Behavioral Research and Therapy Clinics (BRTC), without whom this research would not have been possible. We thank Susan Bland, Linda Dimeff, Heidi Heard, Connie Kehrer, Kelly Koerner, Eric Levensky, Deb McGhee, Evelyn Mercier, Shireen Rizvi, Jennifer Sayrs, Henry Schmidt, Amy Wagner, and Stacy Shaw-Welch for their tireless work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This study was first published as the doctoral dissertation of the first author.
Brown, M. (2002). The Impact of Negative Emotions on the Efficacy of Treatment for Chronic Parasuicide in Borderline Personality Disorder. Doctoral Dissertation, University of Washington.
The total sample size for the trial was 101; however, 14 participants had already entered the trial when this study was initiated and 10 participants entered the trial after the coding was
References
- American Psychiatric Association . Diagnostic and statistical manual for mental disorders (DSM-IV) 4th ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Bancroft J, Skrimshire A, Simkins S. The reasons people give for taking overdoses. British Journal of Psychiatry. 1976;128:538–548. doi: 10.1192/bjp.128.6.538. [DOI] [PubMed] [Google Scholar]
- Baumeister RF. Suicide as escape from self. Psychological Review. 1990;97(1):90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- Beck AT, Stewart B. Clinical and cognitive predictors of suicide. In: Maris RW, Berman AL, Maltsberger JT, Yufit RI, editors. Assessment and prediction of suicide. Guilford Press; New York: 1989. Mentioned in Weishaar & Beck Weishaar, M.E. & Beck, A.T. (1992).
- Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, Shea MT, Zanarini MC, Oldham JM, Gunderson JG. Treatment utilization by patients with personality disorders. American Journal of Psychiatry. 2001;158:295–302. doi: 10.1176/appi.ajp.158.2.295. [DOI] [PubMed] [Google Scholar]
- Biehl M, Matsumoto D, Ekman P, Hearn V, Heider K, Tsutomu K, Ton V. Matsumoto and Ekman's Japanese and Caucasian Facial Expressions of Emotion (JACFEE): Reliability data and cross-national differences. Journal of Nonverbal Behavior. 1997;21(1):3–21. [Google Scholar]
- Birtchnell J, Alarcon J. The motivation and emotional state of 91 cases of attempted suicide. British Journal of Medical Psychology. 1971;44(1):45–52. doi: 10.1111/j.2044-8341.1971.tb02145.x. [DOI] [PubMed] [Google Scholar]
- Brown M, Comtois K, Linehan M. Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. Journal of Abnormal Psychology. 2002;111(1):198–202. doi: 10.1037//0021-843x.111.1.198. [DOI] [PubMed] [Google Scholar]
- Brown M, Rizvi SL. Treatment of shame with exposure therapy and opposite action: A multiple baseline study.. Symposium presentation at the Association for Behavioral and Cognitive Therapies; Chicago, IL. Nov, 2006. [Google Scholar]
- Chapman AL, Gratz KL, Brown M. Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research & Therapy. 2006;44:371–394. doi: 10.1016/j.brat.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Clarkin JE, Widiger TA, Frances A, Hurt SW, Gilmore M. Prototypic typology and the borderline personality disorder. Journal of Abnormal Psychology. 1983;92:263–275. doi: 10.1037//0021-843x.92.3.263. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Erlbaum; Mahwah, NJ: 2003. [Google Scholar]
- Conklin CZ, Westen D. Borderline personality disorder in clinical practice. American Journal of Psychiatry. 2005;162(5):867–75. doi: 10.1176/appi.ajp.162.5.867. [DOI] [PubMed] [Google Scholar]
- Crowe M. Never good enough- part 1: shame or borderline personality disorder? Journal of Psychiatric and Mental Health Nursing. 2004;11:327–334. doi: 10.1111/j.1365-2850.2004.00732.x. [DOI] [PubMed] [Google Scholar]
- Dulit RA, Fyer MR, Leon AC, Brodsky BF, Frances AJ. Clinical correlates of self-mutilation in borderline personality disorder. American Journal of Psychiatry. 1994;151:1305–1311. doi: 10.1176/ajp.151.9.1305. [DOI] [PubMed] [Google Scholar]
- Ekman P, Friesen W. Unmasking the face. Prentice Hall, Inc.; New Jersey: 1975. [Google Scholar]
- Ekman P, Friesen W. Manual for the facial action coding system. Department of Psychiatry, University of California; San Francisco, CA: 1978. [Google Scholar]
- Ekman P, Rosenberg E. What the Face Reveals. Oxford University Press; Oxford: 1997. [Google Scholar]
- First MB, Spitzer R, Gibbon M, Williams JBW. Biometrics Research Department, NY State Psychiatric Institute; New York: 1995. Structured clinical interview for DSM-IV axis I disorders, patient edition (SCID-I/P). [Google Scholar]
- First MB, Spitzer R, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV personality disorders, (SCID-II) American Psychiatric Press; Washington, D.C.: 1997. [Google Scholar]
- Frances A, Fyer M, Clarkin J. Personality and suicide. Annals of the New York Academy of Sciences: Psychobiology of suicidal behavior. 1986;487:281–293. doi: 10.1111/j.1749-6632.1986.tb27907.x. [DOI] [PubMed] [Google Scholar]
- Gilbert . What is shame? Some core issues and controversies. In: Gilbert P, Andrews B, editors. Shame: Interpersonal behavior, psychopathology. 1998. [Google Scholar]
- Gosselin P, Kirouac G, Dore FY. Components and recognition of facial expression in the communication of emotion by actors. Journal of Personality and Social Psychology. 1995;68(1):83–96. doi: 10.1037//0022-3514.68.1.83. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69(4):533–45. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998;2:271–299. [Google Scholar]
- Grove WM, Tellegen A. Problems in the classification of personality disorders. Journal of Personality Disorders. 1991;5:31–41. [Google Scholar]
- Haines J, Williams C, Brain K, Wilson G. The psychophysiology of self-mutilation. Journal of Abnormal Psychology. 1995;104(3):479–489. doi: 10.1037//0021-843x.104.3.471. [DOI] [PubMed] [Google Scholar]
- Harder DW, Lewis SJ. The assessment of shame and guilt. In: Butcher JN, Spielberger CD, editors. Advances in personality assessment. Vol. 6. Erlbaum; Hillsdale, NJ: 1987. pp. 89–114. [Google Scholar]
- Hastings ME, Northman LM, Tangney JP. Shame, guilt, and suicide. In: Joiner T, Rudd MD, editors. Suicide science: Expanding the boundaries. Kluwer Academic Publishers; Boston: 2000. [Google Scholar]
- Hawton K, Cole D, O'Grady J, Osborn M. Motivational aspects of deliberate self-poisoning in adolescents. British Journal of Psychiatry. 1982;141:286–291. doi: 10.1192/bjp.141.3.286. [DOI] [PubMed] [Google Scholar]
- Herpertz S. Self-injurious behavior: Psychopathological and nosological characteristics in subtypes of self-injurers. Acta Psychiatrica Scandinavica. 1995;91:57–68. doi: 10.1111/j.1600-0447.1995.tb09743.x. [DOI] [PubMed] [Google Scholar]
- Izard C. The face of emotion. Appleton-Century-Crofts; New York: 1971. [Google Scholar]
- Kaplan HB, Pokorny AD. Self-derogation and suicide: I. Self-derogation as an antecedent of suicidal responses. Social Science & Medicine. 1976;10(2):113–118. [Google Scholar]
- Keppel and Wickens . Design and Analysis: A Researcher's Handbook. 4th Edition Pearson Prentice Hall; 2004. [Google Scholar]
- Kleindienst N, Bohus M, Ludaescher P, Limberger MF, Kuenkele K, Ebner-Priemer U, Chapman A, Reicherzer M, Stieglitz R-D, Schmahl C. Motives for non-suicidal self-injury among women with Borderline Personality Disorder. Journal of Nervous and Mental Disease. 2008;196:230–236. doi: 10.1097/NMD.0b013e3181663026. [DOI] [PubMed] [Google Scholar]
- Keltner D, Harker L. The forms and functions of the nonverbal display of shame. In: Gilbert, Andrews, editors. Shame: Interpersonal behavior, psychopathology, and culture. Oxford University Press; England: 1998. [Google Scholar]
- Lester D. The association of shame and guilt with suicidality. Journal of Social Psychology. 1998;138(4):535–536. doi: 10.1080/00224549809600407. [DOI] [PubMed] [Google Scholar]
- Lewis HB. Shame and guilt in neurosis. International University Press; New York: 1971. [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Psychosocial risk factors for future adolescent suicide attempts. Journal of Consulting and Clinical Psychology. 1994;62(2):297–305. doi: 10.1037//0022-006x.62.2.297. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive behavioral treatment of borderline personality disorder. Guilford Press; New York: 1993. [Google Scholar]
- Linehan MM, Bohus M, Lynch T. Dialectical behavior therapy for pervasive emotion dysregulation: Theoretical and practical underpinnings. In: Gross J, editor. Handbook of Emotion Regulation. Guilford Press; New York: 2006. [Google Scholar]
- Linehan MM, Comtois K, Murray A, Brown M, Gallop R, Heard H, Korslund K, Tutek D, Reynolds S, Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006;63(7):757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Brown MZ, Heard HL, Wagner A. Suicide attempt self-injury interview (SASII): Development, reliability, and validity of a scale to assess suicide attempts and intentional self-injury. Psychological Assessment. 2006;18:303–312. doi: 10.1037/1040-3590.18.3.303. [DOI] [PubMed] [Google Scholar]
- Loranger AW. Personality disorder examination (PDE) manual. Cornell Medical Center; White Plains, NY: 1995. [Google Scholar]
- Maris R. Pathways to Suicide: A survey of self-destructive behaviors. Johns Hopkins University Press; Baltimore: 1981. [Google Scholar]
- Matsumoto D. More evidence for the universality of a contempt expression. Motivation and Emotion. 1992;16(4):363–368. [Google Scholar]
- Paris J, Brown R, Nowlis D. Long-term follow-up of borderline patients in a general hospital. Comprehensive Psychiatry. 1987;28(6):530–535. doi: 10.1016/0010-440x(87)90019-8. [DOI] [PubMed] [Google Scholar]
- Pompili M, Girardi P, Ruberto A, Tatarelli R. Suicide in borderline personality disorder: a meta-analysis. Nordic Journal of Psychiatry. 2005;59(5):319–24. doi: 10.1080/08039480500320025. [DOI] [PubMed] [Google Scholar]
- Putnam KM, Silk KR. Emotion dysregulation and the development of borderline personality disorder. Developmental Psychopathology. 2005;17(4):899–925. doi: 10.1017/s0954579405050431. [DOI] [PubMed] [Google Scholar]
- Rizvi SL, Linehan MM. The treatment of maladaptive shame in borderline personality disorder: A pilot study of opposite action. Cognitive and Behavioral Practice. 2005;12:437–447. [Google Scholar]
- Rosenthal M, Cukrowicz K, Cheavens J, Lynch T. Self-punishment as a regulation strategy in borderline personality disorder. Journal of Personality Disorders. 2006;20:232–246. doi: 10.1521/pedi.2006.20.3.232. [DOI] [PubMed] [Google Scholar]
- Runeson B, Beskow J. Borderline personality disorder in young Swedish suicides. Journal of Nervous and Mental Disease. 1991;179(3):153–6. doi: 10.1097/00005053-199103000-00007. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Lieb K, Göttler I, Hermann C, Schramm E, Richter H, Jacob GA, Corrigan PW, Bohus M. Shame and implicit self-concept in women with borderline personality disorder. American Journal of Psychiatry. 2007;164:500–508. doi: 10.1176/ajp.2007.164.3.500. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Corrigan PW, Bohus M, Kühler T, Jacob GA, Lieb K. The impact of posttraumatic stress disorder on dysfunctional implicit and explicit emotions among women with borderline personality disorder. Journal of Nervous and Mental Disease. 2007;195(6):537–539. doi: 10.1097/NMD.0b013e318064e7fc. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Beck AT, Kovacs M, Weissenburger J, Hollon S. Comparison of the differential effects of cognitive therapy and pharmacotherapy on hopelessness and self-concept. American Journal of Psychiatry. 1982;139:862–866. doi: 10.1176/ajp.139.7.862. [DOI] [PubMed] [Google Scholar]
- Schneider B, Wetterling T, Sargk D, Schneider F, Schnabel A, Maurer K, Fritze J. Axis I disorders and personality disorders as risk factors for suicide. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(1):17–27. doi: 10.1007/s00406-005-0593-7. [DOI] [PubMed] [Google Scholar]
- Shaver P, Schwartz J, Kirson D, O'Conner C. Emotion knowledge: Further exploration of a prototype approach. Journal of Personality and Social Psychology. 1987;52:1061–1086. doi: 10.1037//0022-3514.52.6.1061. [DOI] [PubMed] [Google Scholar]
- Shearer SL, Peters CP, Quaytman MS, Wadman BE. Intent and lethality of suicide attempts among female borderline inpatients. American Journal of Psychiatry. 1988;145:1424–1427. doi: 10.1176/ajp.145.11.1424. [DOI] [PubMed] [Google Scholar]
- Shneidman ES. Suicide as psychache: A clinical approach to self-destructive behavior. Aronson; New Jersey: 1993. [Google Scholar]
- Stiglmayr C, Grathwol T, Linehan M, Ihorst G, Fahrenberg J, Bohus M. Aversive tension in patients with borderline personality disorder: a computer-based controlled field study. Acta Psychiatrica Scandinavica. 2005;111(5):372–379. doi: 10.1111/j.1600-0447.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- Stone MH. Long-term outcome in personality disorders. British Journal of Psychiatry. 1993;162:299–313. doi: 10.1192/bjp.162.3.299. [DOI] [PubMed] [Google Scholar]
- Stone MH, Stone DK, Hurt SW. Natural history of borderline patients treated by intensive hospitalization. Psychiatric Clinics of North America. 1987;10:185–206. [PubMed] [Google Scholar]
- Stone MH, Hurt SW, Stone DK. The PI 500: Long-term follow-up of borderline inpatients meeting DSM-III criteria. I: Global outcome. Journal of Personality Disorders. 1987;1:291–298. [Google Scholar]
- Tangney JP, Dearing RL. Shame and guilt. Guilford Press; New York: 2002. [Google Scholar]
- Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Archives of General Psychiatry. 2001;58:590–596. doi: 10.1001/archpsyc.58.6.590. [DOI] [PubMed] [Google Scholar]
- Tracey JL, Robins RW, Tangney JP. The self-conscious emotions: Theory and research. The Guilford Press; New York: 2007. [Google Scholar]
- Watson D, Clark LA. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wei LJ, Lin DY, Weissfeld L. Regression analysis of mulitvariate incomplete failure time data by modeling marginal distributions. Journal of the American Statistical Association. 1989;84(408):1065–1073. [Google Scholar]
- Zanarini MC, Frankenburg FR, Khera GS, Bleichmar J. Treatment histories of borderline inpatients. Comprehensive Psychiatry. 2001;42:144–150. doi: 10.1053/comp.2001.19749. [DOI] [PubMed] [Google Scholar]