Abstract
Underlying maternal vascular disease has been implicated as one of several pathways contributing to preterm delivery (PTD) and psychosocial factors such as hostility, anomie, effortful coping, and mastery may be associated with PTD by affecting maternal vascular health. Using data from the Pregnancy Outcomes and Community Health (POUCH) study, we included 2,018 non-Hispanic White and 743 African American women from 52 clinics in 5 Michigan, USA communities who were interviewed at 15−27 weeks’ gestation and followed to delivery. We found that relations between psychosocial factors and PTD subtypes (i.e. medically indicated, premature rupture of membranes, spontaneous labor) varied by race/ethnicity and socioeconomic position (Medicaid insurance status). Among African American women not insured by Medicaid, anomie levels in mid-pregnancy were positively associated with medically indicated PTD after adjusting for maternal age and education. Among all women not insured by Medicaid, hostility levels were positively associated with spontaneous PTD after adjusting for maternal race/ethnicity, age, and education. Failure to detect links between psychosocial factors and PTD risk in poorer women may be due to their excess risk in multiple PTD pathways and/or a more complex web of contributing risk factors.
In a subset of 395 women monitored for blood pressure, anomie scores were positively associated with systolic blood pressure and heart rate and hostility scores were positively associated with systolic and diastolic blood pressure, heart rate and mean arterial pressure in models that included time, awake/asleep, race/ethnicity, and age as covariates. Further adjustment for body mass index and smoking attenuated the anomie-vascular relations but had little effect on the hostility-vascular relations. Overall this study of pregnant women provides some physiologic evidence to support findings linking levels of anomie and hostility with risk of PTD.
Keywords: premature birth, hostility, anomie, social class, social environment, blood pressure, pregnancy, USA
Introduction
Preterm delivery (PTD) accounts for at least one third of all infant deaths in the United States (Callaghan, MacDorman, Rasmussen, Qin, & Lackritz, 2006) and the importance of this recalcitrant problem is widely recognized. The epidemiology of PTD is changing in the United States, reflecting recent increases in multiple births (Russell, Petrini, Damus, Mattison, & Schwarz, 2003) and medically indicated PTD's (Ananth, Joseph, Oyelese, Demissie, & Vintzileos, 2005), resulting in a preterm birth rate of 12.7% for 2004−2005, a 20% increase since 1990 when the rate was 10.6% (Hamilton, Martin, & Ventura, 2006). Although progesterone (Meis et al., 2003), infection (Goldenberg, Hauth, & Andrews, 2000); maternal vascular disease (Hatch et al., 2006) and elevated corticotropin-releasing hormone (CRH) (Lockwood, 1999), have all been associated with PTD, our understanding of these factors and the processes of preterm birth is incomplete, particularly those that mediate its social disparities. It is clear that PTD risk is inversely related to socio-economic status (Kramer, Seguin, Lydon, & Goulet, 2000; Thompson, Irgens, Rasmussen, & Daltveit, 2006) and is higher in African American (17.8%) than non-Hispanic White infants (11.5%) (Martin et al., 2005).
Psychosocial factors have long been suspected of playing a causal role in the incidence of adverse birth outcomes, and since the 1960's a growing body of research has addressed these potential relationships. Recent publications include studies linking PTD with life events, anxiety, stress (Dole et al., 2003; Hobel & Culhane, 2003; Wadhwa et al., 2001), social support and other resources (Dole et al., 2003), depression (Orr & Miller, 1995) and mastery, optimism and self esteem (Rini, Dunkel-Schetter, Wadhwa, & Sandman, 1999). Separate research has also explored the relationships of psychosocial variables and racial health disparities (Dole et al., 2004). Evidence is equivocal, however, indicating better specified models are needed to find the subset of psychosocial factors most strongly associated with PTD (Dole et al., 2003; Dunkel-Schetter & Rimi, 2004) and the causal pathways linking psychosocial factors and PTD (Kramer et al., 2001). In this study we test the hypotheses that particular psychosocial factors (hostility, anomie, effortful coping and mastery) are linked to ambulatory blood pressure and PTD.
Background
Criteria for Choice of Psychosocial Measures
In the Pregnancy Outcomes and Community Health (POUCH) study, the goal was to identify proximate physiologic and pathologic changes and upstream psychosocial factors within PTD pathways. One pathway was characterized by evidence of maternal vascular disease. Several psychosocial instruments used in the POUCH study were considered particularly pertinent to this pathway because they: 1) had proved relevant in previous studies of cardiovascular health in pregnant and non-pregnant populations; and/or 2) represented outward (societal anomie) and inward (effortful coping, mastery, hostility) forces that might promote or prevent chronic stimulation of the sympathetic nervous system.
First, hostility and John Henryism (effortful coping) were chosen because of their previous association with vascular reactivity (Fichera & Andreassi, 1998; Jain, Dimsdale, Roesch, & Mills, 2004), and in some cardiovascular studies reactivity in blood pressure has been linked to gestational age at delivery (Hatch et al., 2006) and spontaneous PTD (Samadi & Mayberry, 1998). Finally, links between hostility and blood pressure are especially interesting in women because of the mismatch of hostility with some of the cultural norms that regulate women's lives (Spicer & Chamberlain, 1996).
Second, anomie, a construct related to varying degrees of alienation from social norms, was chosen to expand the psychosocial construct beyond the individual to reflect more complex interactions with the larger sociocultural environment. Anomic individuals do not see themselves to be invested in society, reflecting a hopeless participation in the social world, and anticipation of failure in social involvement. Anomie may also reflect a woman's sense of lacking social status. Although not previously investigated in relation to PTD, anomie has been associated with larger community health effects, including the effects of violence on an inner-city community (Fullilove et al., 1998). Anomie also represents long-standing features of a woman's life that exact a cumulative toll (McEwen & Stellar, 1993), and may induce alterations in vascular reactivity or other vascular pathways.
Third, we were interested in personal resource variables, mastery and effortful coping which may reflect individual differences in responses to environmental stressors. Mastery is one of the most salient psychosocial variables identified from the more than three dozen studies on stress and PTD (Dunkel-Schetter & Rimi, 2004) and work by Hobfoll (1989) has suggested that mastery functions to mitigate untoward effects of exposure to stressors. Effortful coping was included because it was originally found to be related to ethnicity and the risk of cardiovascular disease (CVD) (James, 1994). A more recent study has found an association with African American CVD biomarkers and effortful coping (Geronimus, Hicken, Keene, & Bound, 2006); while others have not, (Peters, 2006).
Maternal vascular indices and Psychosocial Measures
Although high hostility has frequently been associated with cardiovascular risk factors (lower heart rate variability and increased blood pressure reactivity) (Adams, Aubert, & Clark, 1999; Spicer & Chamberlain, 1996), suggesting links to cardiovascular disease and deleterious outcomes, data is lacking for pregnant women. Some studies have linked maternal blood pressure response to lab stress tests and birth outcome, but without measures of hostility or anomie (Hatch et al., 2006); while others have only linked hypertension and spontaneous PTD in African American women, again without psychosocial measures (Samadi & Mayberry, 1998). Socio-economic status has also been shown to interact with high hostility in the development of cardiovascular disease, (Wielgosz & Nolan, 2000) but again this interaction has not been investigated in pregnant or racially diverse samples. Finally, ambulatory blood pressure studies in pregnant women are numerous, but mostly to document circadian variability (Ayala, Hermida, Mojon, Fernandez, & Iglesias, 1997), normal patterns (Hermida et al., 2000), or links to fetal growth/birth weight or other outcomes of pregnancy (Bellomo et al., 1999; Waugh et al., 2000). In the POUCH study, we had an opportunity to compare scores on psychosocial measures with maternal vascular indices measured in an economically diverse subset of African American and non-Hispanic White women who, as part of the study protocol, wore an ambulatory blood pressure monitor for 24 hours in mid-pregnancy.
Methods
Study population
The Pregnancy Outcomes and Community Health (POUCH) study is a prospective cohort study of pregnant women sampled from 52 participating clinics in five Michigan communities. Study protocols were approved by institutional review boards at Michigan State University and at eight hospitals in five Michigan communities.
Women were recruited in the clinics by means of a one-page description of the POUCH study attached to their prenatal screening form. Eligibility included maternal age greater than 14 years, screening for maternal serum alpha fetoprotein (MSAFP) at < 22 weeks’ gestation, a singleton pregnancy with no known congenital or chromosomal abnormalities, and no history of pre-pregnancy diabetes mellitus. Women were sampled into the cohort from strata defined by race/ethnicity and unexplained high MSAFP levels, a biomarker of interest in relation to pregnancy outcomes.
During the period of the study (September, 1998 to June, 2004), 3038 women were enrolled in their 15th −27th week of pregnancy. Nineteen women were lost to follow up resulting in 3019 cohort women overall. Due to the Health Insurance Portability and Accountability Act (HIPAA) regulations it was not possible to determine an exact response rate or to compare characteristics of participants with those who declined enrollment in the POUCH study. However comparisons were made between POUCH study data and data recorded on birth certificates of women who delivered in the five study communities in the year 2000. Ethnic-specific analyses (non-Hispanic White and African American) weighted by the proportion of women enrolled from each community showed that the POUCH sample was very similar to community mothers for most factors measured, i.e. age, parity, education level, and the proportion of women with Medicaid insurance, PTD, previous stillbirth, previous preterm infant, and previous low birthweight infant. The one exception was that the percentage of African Americans over 30 years of age, was lower in POUCH (14%) than in community birth certificates (21%) (see Holzman, Bullen, Fisher, et al., 2001 for a more detailed description of the study).
Demographic and Psychosocial data
At enrollment participating women met with a study nurse in their respective communities to sign consent forms, have biological samples collected, and complete an in-person interview and a self-administered questionnaire. The analyses of psychosocial and pregnancy outcome data reported here include the 2761 study participants who were either non-Hispanic White (N=2,018) or African American (N=743). Women who selected multiple categories for their ethnicity were asked to choose a single category.
The psychosocial questions for this study came from several standardized instruments. Mastery was measured using the 7-item Mastery Scale (Pearlin & Schooler, 1978). There were two positively worded items, e.g. “What happens to me in the future depends mostly on me” and five negatively worded items that were reverse scored, e.g. “There is really no way I can solve some of the problems I have”. Participants rated each item on a scale ranging from 1 (strongly disagree) to 5 (strongly agree), with higher scores reflecting greater mastery.
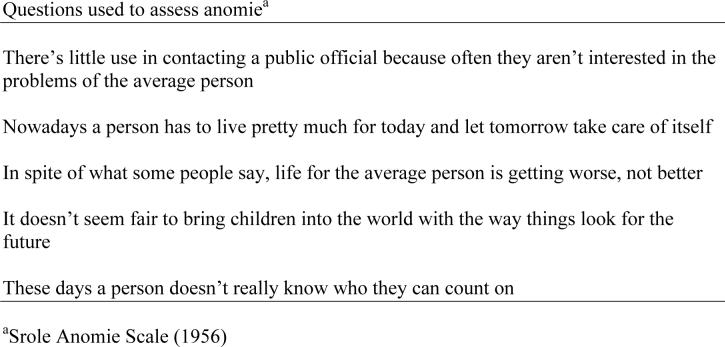
Anomie was measured by using the 5 item version of the Srole Anomie Scale (1956) (see Appendix). Response options varied from 0 (strongly disagree) to 3 (strongly agree). Each of the five questions was scored 0 (if response was 0−1) and 1 (if response was 2−3), according to the approach used by Srole (1956). Items were then summed, resulting in scores from 0−5, with higher scores reflecting greater anomie.
Hostility was assessed using the abbreviated 9 item Cook-Medley Hostility Scale (Barefoot, Larsen, von der Lieth, & Schroll, 1995). Items were endorsed on a true or false basis and scored so that a “true” response indicated greater hostility, with one item reverse scored (“I am not easily angered”). The items were summed so that higher scores reflected greater hostility. John Henryism, an “effortful coping” style, was assessed using an 8 item scale developed by James, Hartnett & Kalsbeek (1983). Items pertained to issues such as persistence until a job is done, hard work, and getting ahead in life. Women rated each item ranging from 1 (not true), to 2 (somewhat true) to 3 (very true), with higher scores reflecting more effortful coping.
Covariates of interest were selected based on findings in other studies on PTD (Savitz & Pastore, 1999), and included maternal age, parity, education level, week of pregnancy at enrollment, Medicaid status (a low-income insurance plan used as a socioeconomic indicator), pre-pregnancy body mass index (BMI), and smoking. Medicaid insured was defined as having Medicaid insurance before or during pregnancy. Only 14 POUCH women (2%) were insured by Medicaid before, and not during, the current pregnancy. Smoking was categorized into four levels: never smoked during current pregnancy, smoked in pregnancy but quit prior to study enrollment, currently smoking < ½ pack per day, and currently smoking ≥ ½ pack per day.
Pregnancy outcome
PTD was defined as births before 37 weeks’ gestation. Gestational week at delivery was calculated using date of the last menstrual period (LMP) or gestational age estimate from ultrasound (US) if LMP and US estimate differed by more than two weeks. Previous research has suggested that clinically defined subtypes of PTD are not etiologically distinct, but assessing overlapping and non-overlapping risk factors can provide further clues to underlying pathways. Here PTD was categorized by its clinical presentations based on a medical record review: medically indicated (MI), premature rupture of the membranes (PROM), and spontaneous preterm labor (PTL). MI PTD was defined as delivery < 37 weeks that begins by induction or C-section in the absence of spontaneous labor (cervix dilated ≥ 2cm and regular contractions) or rupture of membranes as an initiating event. PROM was defined as rupture of membranes prior to or simultaneous with onset of labor.
Maternal vascular indices
After initiation of the POUCH study, an at-home data collection protocol was added, directly following enrollment at 15−27 weeks (Jones, Holzman, Zanella, Leece, & Rahbar, 2006). Eighty-three percent of the eligible cohort agreed to the at-home protocol, but due to the limited number of ambulatory blood pressure monitors (ABPMs), these data were collected on a smaller sample. The availability of an ABPM was random and depended only on return of a monitor from a previous POUCH participant with time to recalibrate for the next participant. Analyses presented here comparing psychosocial data with 24 hour ABPM indices include 395 study participants (289 non-Hispanic White, 106 African American). Women were excluded if they were a racial/ethnic category other than African American or non-Hispanic White (n=45), or if they had insufficient data i.e. <3 awake or asleep ABPM reading or incomplete awake and sleep notations in their diaries (n=57).
At the end of the enrollment encounter, study nurses selected a blood pressure cuff size based on the arm circumference of each participant, then fitted the ABPM and validated the initial readings. The ABPM was programmed to record systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), mean arterial pressure (MAP, equal to 2/3 DBP + 1/3 SBP), and pulse pressure (PP) every half hour from 9AM to 9PM and every hour during the remainder of the time for a total of 36 time points. Approximately 75% of women in these analyses had ABPM data recordings for ≥ 32 programmed time points and only 5% of women had fewer than 27 time points.
Analytic strategy
For psychosocial measures, missing values were imputed (Raghunathan, Solenberger, & Van Hoewyk, 1998) for those scales having at least seven items and for those records having no more than one missing value within that scale. In the Cook-Medley Hostility Scale (9 items), 31 of 41 records with missing values were imputed; in the Pearlin & Schooler Mastery Scale (7 items), 16 of 22 records were imputed; and in the John Henryism Effortful Coping Scale (8 items), 29 of 35 records were imputed. Missing values in the Srole Anomie Scale (5 items) could not be imputed due to the small number of items in the scale, leaving 23 women with missing anomie scores.
Initial descriptive analyses showed that each of the four psychosocial factors, although normally distributed, appeared to have different means in groups defined by race/ethnicity and Medicaid insurance status. Analysis of variance (ANOVA) was used to test for differences in means across these groups, followed by pair-wise comparisons when ANOVA F-test p-value was <.05. In race/ethnic specific analyses, other maternal characteristics were modeled as categorical independent variables and evaluated in relation to a vector of the four psychosocial factors by using multivariate analysis of variance (MANOVA). A maternal characteristic with a significant F-test (p<0.05 using Wilks’ Lambda) in a MANOVA model was then incorporated into a series of one-way analysis of variance (ANOVA) models to test differences in mean psychosocial measures across maternal categories. Maternal characteristics with an F-test p<0.10 in ANOVA models were considered for multi-covariate regression models.
Polytomous logistic regression models were used to assess the association between the independent variable, a psychosocial measure expressed as a continuous score, and the dependent variable, pregnancy outcome expressed as categories, i.e. MI PTD, PROM PTD, PTL PTD and term delivery as the referent. Only one psychosocial measure was entered into each model. Final models examined two-way interactions between racial/ethnic group and psychosocial measure, and between Medicaid insurance status and psychosocial measure and three-way interactions with all three variables. All analyses were repeated after removing the 7% of women with high MSAFP, a group preferentially sampled for the cohort, to make certain that this oversampling did not significantly alter results and inferences.
In maternal vascular analyses, outlier ABPM measurements defined as DBP > 140, SBP > 250, or measures three standard deviations below the mean were excluded. SBP, DBP, HR, and MAP were modeled separately as dependent variables in generalized linear models (GLM with the PROC Mixed with a ‘time’ variable indicating repeated measures over 24 hours) to assess associations with psychosocial measures and account for within subject correlation between ABPM measures over time. Time of each measurement, recorded by the monitor, was included as a continuous variable in all models. In addition each ‘time’ measure was labeled as an asleep time or an awake time based on the woman's diary entries, and the ‘asleep/awake’ variable was also a time varying covariate in all models. To maintain the data structure and avoid small numbers in a stratum, rare ABPM measures were coded as missing, i.e. asleep measures from 10:30AM through 10:00PM and awake measures from 1:00AM through 5:00AM. In addition, only fourteen women had a score of zero on the hostility scale and several of these women had unusually high blood pressures. This resulted in a very large variance for this small stratum and made it difficult to arrive at meaningful interpretations of this unusual group; we therefore elected to exclude these fourteen women. For each vascular outcome (SBP, DBP, HR, and MAP) there were a series of longitudinal models that included covariates and interaction terms that were significant at P<0.05. Model 1 included a psychosocial measure and both ‘time’ and ‘asleep/awake’ as covariates. Model 2 then added two demographic covariates, maternal age (continuous) and race/ethnicity, and a 3-way interaction between race/ethnicity, time, and sleep/awake. Model 3 added BMI (continuous) and smoking (categorical), which were considered potential mediating variables in the pathway between psychosocial score and the maternal vascular measure. Due to sample size constraints we did not directly test a mediating hypothesis, i.e. ambulatory BP as a mediator of the association between hostility and anomie and PTD subtypes. Analyses were conducted in SAS, version 9.1, software (SAS Institute., 2006).
RESULTS
Psychosocial measures and PTD risk
Of the 2761 women in this study, 15% were under 20 years of age, 17% completed less than 12 years of education, 47% were Medicaid insured, 27% were African American, 72% were between 20−24 weeks pregnant, and 11.2% delivered preterm. Race and social class differences in PTD rates mirror that seen in previous studies (Table 1). Correlation coefficients between each set of pairs of the four psychosocial measures indicated moderate significant correlations between anomie and hostility (0.36); anomie and mastery (−0.37); hostility and mastery (−0.36) and mastery and effortful coping (0.25) in African Americans, and between anomie and hostility (0.45); anomie and mastery (−0.38); hostility and mastery (−0.35); and mastery and effortful coping (0.31) in non-Hispanic Whites. The correlations between coping and anomie and coping and hostility were weak, ranging from 0.03 to 0.12 in both African American and non-Hispanic White women.
TABLE 1.
Maternal characteristics of the non-Hispanic White and African-American POUCH study women
|
White non-Hispanic (N=2017) Medicaid Insureda |
African-American (N=741) Medicaid Insureda |
|||||||
|---|---|---|---|---|---|---|---|---|
|
Maternal Characteristics |
No |
Yes |
No |
Yes |
||||
| |
No. |
(%) |
No. |
(%) |
No. |
(%) |
No. |
(%) |
| Age (years) | ||||||||
| <20 | 67 | (5) | 141 | (20) | 21 | (14) | 185 | (31) |
| 20−29 | 647 | (50) | 478 | (67) | 84 | (58) | 346 | (58) |
| ≥30 | 593 | (45) | 91 | (13) | 40 | (28) | 65 | (11) |
| Education | ||||||||
| <12 yrs (age<20) | 36 | (3) | 83 | (12) | 17 | (12) | 123 | (21) |
| <12 yrs (age≥20) | 17 | (1) | 87 | (12) | 5 | (3) | 120 | (20) |
| 12 yrs | 257 | (20) | 320 | (45) | 24 | (17) | 215 | (36) |
| >12 yrs | 997 | (76) | 220 | (31) | 99 | (68) | 138 | (23) |
| Week of Pregnancy At Enrollment | ||||||||
| <20 wks | 183 | (14) | 100 | (14) | 18 | (12) | 106 | (18) |
| 20−24 wks | 642 | (72) | 519 | (73) | 106 | (73) | 411 | (69) |
| 25−27 wks | 182 | (14) | 91 | (13) | 21 | (14) | 79 | (13) |
| OB History | ||||||||
| 0 live birth | 587 | (45) | 298 | (42) | 66 | (45) | 232 | (39) |
| ≥1 live birth no previous preterm | 634 | (48) | 323 | (45) | 68 | (47) | 287 | (48) |
| ≥1 live birth with previous preterm | 86 | (7) | 89 | (13) | 11 | (8) | 77 | (13) |
| Pregnancy Outcome | ||||||||
| Term | 1190 | (91) | 631 | (89) | 126 | (87) | 505 | (85) |
| Preterm overall | 117 | (9) | 79 | (11) | 19 | (13) | 91 | (15) |
| Medically Indicated | 39 | (3) | 24 | (3) | 7 | (5) | 27 | (4) |
| PROM | 39 | (3) | 18 | (3) | 5 | (3) | 23 | (4) |
| PTL | 39 | (3) | 37 | (5) | 7 | (5) | 41 | (7) |
Data on Medicaid status missing for 3 women
Unadjusted means for anomie and hostility were lowest in non-Hispanic Whites not insured by Medicaid, were higher and similar in non-Hispanic Whites insured by Medicaid and African Americans not insured by Medicaid, and highest in African Americans insured by Medicaid (Table 2). Unadjusted mean mastery scores were higher in women not insured by Medicaid versus those insured by Medicaid within both race/ethnic models. Effortful coping unadjusted means were higher in African Americans than in non-Hispanic Whites, but unrelated to Medicaid insurance status within race/ethnic groups. Associations between other maternal characteristics and a vector of all four psychosocial measures were first assessed through MANOVA by race/ethnicity. Maternal age, parity, and education level were significantly associated with the four psychosocial measures and were similar across race/ethnic specific models. These maternal characteristics were then evaluated in ANOVA models to identify their specific relation to each of the four psychosocial measures. Lower maternal age and lower education levels were associated with significantly higher mean scores for anomie and hostility in each racial/ethnic-specific model (Table 3). By contrast, these same maternal characteristics, with the exception of lower maternal age in African Americans, were linked to lower means scores for mastery. Maternal characteristics were not strongly related to effortful coping scores. In African Americans, the unadjusted mean anomie score was significantly higher in women who delivered preterm, than that in women who delivered at term. In non-Hispanic Whites the unadjusted mean hostility score was significantly higher in women who delivered preterm, than that in women who delivered at term (Table 3).
TABLE 2.
Unadjusted means and standard deviations (SD) of psychosocial measures ascertained at mid-pregnancy by race/ethnicity and Medicaid insurance status
|
White non-Hispanic (N=2018)a Medicaid Insured |
African American (N=743) Medicaid Insured |
|||
|---|---|---|---|---|
| No |
Yes |
No |
Yes |
|
| Psychosocial measure (range) | ||||
| Anomie (0−5) | 0.9 (1.1) | 1.9 (1.4)bc | 1.6 (1.3)c | 2.3 (1.4)bc |
| Hostility (0−9) | 3.3 (1.9) | 4.5 (2.0)bc | 4.8 (2.0)c | 5.6 (1.8)bc |
| Mastery (7−28) | 22.1 (3.2) | 20.8 (3.4)bc | 22.2 (3.4) | 20.9 (3.4)bc |
| Effortful Coping (8−24) | 18.7 (2.4) | 18.6 (2.6) | 19.7 (2.7)c | 19.6 (2.9)c |
Data missing for 2−12 women in selected variables for each racial/ethnic group
p<0.05 for pair-wise comparisons of Medicaid insured versus not Medicaid insured within race/ethnic group
p<.05 for pair-wise comparisons across both race/ethnic groups with white, no Medicaid as referent
TABLE 3.
Unadjusted means and standard deviations (SD) of psychosocial measures ascertained at mid-pregnancy by demographic and obstetric characteristics (race/ethnicity-specific)
| Anomie (range= 0−5) b |
Hostility (range= 0−9) b |
Mastery (range= 7−28) b |
Effortful Coping (range=8−24)b |
|||||
|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White |
African American |
Non-Hispanic White |
African American |
Non-Hispanic White |
African American |
Non-Hispanic White |
African American |
|
| Maternal Age | ||||||||
| <20 | 2.1 (1.4) a | 2.4 (1.3) a | 5.2 (1.9) a | 6.1 (1.7) a | 20.3 (3.2) a | 20.7 (3.1) | 18.8 (2.8) | 19.9 (2.8) |
| 20−29 | 1.3 (1.3) a | 2.1 (1.4) | 3.9 (2.0) a | 5.2 (1.9) | 21.6 (3.4) a | 21.5 (3.5) | 18.6 (2.5) | 19.6 (2.9) |
| ≥30 (reference) | 0.8 (1.1) | 1.8 (1.6) | 3.0 (1.8) | 5.1 (1.9) | 22.2 (3.2) | 20.7 (3.8) | 18.8 (2.4) | 19.2 (3.0) |
| Parity/ OB History | ||||||||
| 0 live birth | 1.2 (1.3) | 2.1 (1.4) | 3.8 (2.0) | 5.7 (1.8) a | 21.7 (3.4) | 21.3 (3.3) | 18.9 (2.4) a | 19.8 (2.8) |
| ≥1 live birth | 1.2 (1.3) | 2.2 (1.5) | 3.7 (2.0) | 5.3 (1.9) | 21.6 (3.4) | 21.1 (3.6) | 18.5 (2.6) | 19.5 (3.0) |
| Education | ||||||||
| <12 yrs (age<20) | 2.3 (1.4) a | 2.4 (1.3) a | 5.2 (2.0) a | 6.1 (1.7) a | 20.2 (3.2) a | 20.5 (3.1) a | 18.8 (2.9) | 19.8 (2.9) |
| <12 yrs (age≥20) | 2.1 (1.6) a | 2.6 (1.4) a | 5.0 (1.9) a | 5.7 (1.9) a | 20.5 (3.6) a | 19.8 (3.3) a | 18.3 (2.8) | 19.4 (3.1) |
| 12 yrs | 1.6 (1.4) a | 2.3 (1.5) a | 4.2 (2.0) a | 5.6 (1.8) a | 21.1 (3.3) a | 21.0 (3.4) a | 18.6 (2.6) | 19.7 (3.0) |
| > 12 yrs (reference) | 0.9 (1.1) | 1.7 (1.4) | 3.2 (1.9) | 4.7 (1.8) | 22.2 (3.3) | 22.3 (3.4) | 18.8 (2.4) | 19.7 (2.6) |
| Week of Pregnancy At Enrollment | ||||||||
| <20 wks (reference) | 1.2 (1.3) | 2.3 (1.5) | 3.8 (2.2) | 5.5 (1.8) | 21.4 (3.5) | 20.6 (3.2) | 18.6 (2.6) | 19.4 (2.9) |
| 20−24 wks | 1.3 (1.3) | 2.1 (1.4) | 3.7 (2.0) | 5.5 (1.8) | 21.7 (3.3) | 21.3 (3.5) | 18.7 (2.5) | 19.6 (3.0) |
| 25−27 wks | 1.1 (1.2) | 2.0 (1.4) | 3.7 (2.0) | 5.3 (2.1) | 21.8 (3.4) | 21.0 (3.6) | 18.8 (2.4) | 20.0 (2.6) |
| Pregnancy Outcome | ||||||||
| Term | 1.2 (1.3) | 2.1 (1.4) | 3.7 (2.0) | 5.4 (1.9) | 21.7 (3.4) | 21.2 (3.5) | 18.7 (2.5) | 19.6 (2.9) |
| Preterm | 1.3 (1.2) | 2.4 (1.5) a | 4.1 (2.0) a | 5.5 (1.7) | 21.3 (3.3) | 21.1 (3.4) | 18.7 (2.5) | 20.0 (2.9) |
p<0.05 for race/ethnic specific comparisons of unadjusted mean psychosocial measures by maternal characteristic
Data missing for 2−12 women in selected variables for each racial/ethnic group
In polytomous logistic regression models with multiple covariates, mastery and effortful coping were not significantly associated with any of the PTD subtypes. The model of anomie and PTD subtypes contained two significant interactions, one between anomie and race/ethnicity and one between anomie and Medicaid insurance status. Therefore, results are presented separately for each racial/ethnic and Medicaid insurance stratum (Table 4). Among African American women not insured by Medicaid, anomie levels in mid-pregnancy were positively associated with medically indicated PTD; the odds ratio (referent term delivery) for one unit increase in anomie score = 1.8, (95% CI 1.2, 2.6) after adjusting for maternal age and education. There was no association between anomie score and PTD in the other race/ethnic and Medicaid stratum. The model of hostility and PTD subtypes showed a significant interaction between hostility and Medicaid status and no interaction involving racial/ethnic group. Among all women not insured by Medicaid, hostility levels were positively associated with spontaneous PTD; the odds ratio for one unit increase in hostility score = 1.3 (95% CI 1.2, 2.6) after adjusting for maternal race/ethnicity, age, and education. Hostility scores were unrelated to PTD in women insured by Medicaid. Models of anomie, hostility and PTD were repeated after adding BMI and smoking as covariates and the adjusted odds ratios were unaffected.
TABLE 4.
Associations between psychosocial measures ascertained at mid-pregnancy and preterm delivery subtypes; adjusted odds ratiosd
| Term (referent group) | PTD: Medically Indicated |
PTD: Premature Rupture of Membranes |
PTD: Spontaneous Preterm Labor |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. |
No. |
AOR |
95% CI |
No. |
AOR |
95% CI |
No. |
AOR |
95% CI |
|
| Anomieb | ||||||||||
| Medicaid (+) | ||||||||||
| Non-Hispanic White | 627 | 23 | 0.7 | (0.5, 1.0) | 18 | 1.1 | (0.8, 1.4) | 37 | 1.0 | (0.8, 1.3) |
| African American | 496 | 27 | 1.1 | (0.9, 1.4) | 23 | 1.1 | (0.9, 1.5) | 41 | 1.1 | (0.9, 1.3) |
| Medicaid (-) | ||||||||||
| Non-Hispanic White | 1186 | 38 | 1.1 | (0.8, 1.4) | 38 | 1.3 | (1.0, 1.6) | 39 | 1.1 | (0.9, 1.4) |
| African American | 124 | 7 | 1.8a | (1.2, 2.6) | 5 | 1.3 | (0.9, 2.0) | 7 | 1.2 | (0.8, 2.0) |
| Hostilityc | ||||||||||
| Medicaid (+) | 1131 | 51 | 1.0 | (0.9, 1.2) | 41 | 0.9 | (0.8, 1.1) | 78 | 1.0 | (0.9, 1.2) |
| Medicaid (-) | 1313 | 46 | 1.1 | (1.0, 1.3) | 44 | 1.0 | (0.9, 1.2) | 46 | 1.3a | (1.1, 1.5) |
p<0.05
Adjusted for maternal age and education (categorical): Anomie data missing for 23 women. Medicaid data missing for 3 women. One woman missing both Medicaid and anomie data.
Adjusted for maternal race/ethnicity, age and education (categorical): Hostility data missing for 9 women. Medicaid data missing for 3 women. One woman missing both hostility and Medicaid data.
Odds ratio for one unit increase in score
Psychosocial Measures and Maternal Vascular Indices
In the first series of longitudinal models (Model 1) that included time as a repeated measure indicator and sleep/awake as the only covariate, measures of mastery and effortful coping were unrelated to vascular indices. Anomie scores were positively associated with SBP and HR and hostility scores were positively associated with SBP, HR, and MAP (Table 5). Anomie and hostility were then analyzed in a second set of longitudinal models (Model 2) with the addition of demographic covariates (maternal race/ethnicity, age, and a three-way interaction between race/ethnicity, time, and awake/asleep). Anomie remained associated with SBP (β=0.77, P=.01) and HR (β=0.65, P=.03). Hostility scores were found to be associated with all four vascular indices, SBP (β=0.53, P=.02), DBP (β=0.33, P=.04), HR (β=0.68, P=<.01), and MAP (β=0.43, P=.01). A third series of models (Model 3) incorporating BMI and smoking resulted in a slight attenuation of the anomie-SBP association (β=0.66, P=.03), and a statistically non-significant anomie-HR association (β=0.34, P=.24), but no real changes in the relations between hostility and the four vascular indices.
Table 5.
Mid-pregnancy maternal ambulatory blood pressure and heart rate indices in relation to psychosocial measures among a subset of POUCH study participants
| SBP |
DBP |
HR |
MAP |
|||||
|---|---|---|---|---|---|---|---|---|
| β | P value | β | P value | β | P value | β | P value | |
| Anomie N=394 | ||||||||
| Model 1: Adjusted for time, and sleep/awake | 0.71 | 0.01 | 0.14 | 0.49 | 0.78 | 0.01 | 0.34 | 0.10 |
| Model 2: Adjusted for time, sleep/awake, and demographicsa | 0.77 | 0.01 | 0.34 | 0.12 | 0.65 | 0.03 | 0.43 | 0.06 |
| Model 3: Adjusted for time, sleep/awake, demographicsa, BMI, and smoking | 0.66 | 0.03 | 0.37 | 0.11 | 0.34 | 0.27 | 0.42 | 0.07 |
| Hostility N=381b | ||||||||
| Model 1: Adjusted for time, and sleep/awake | 0.53 | 0.01 | 0.17 | 0.25 | 0.77 | <0.01 | 0.35 | 0.03 |
| Model 2: Adjusted for time, sleep/awake, and demographicsa | 0.53 | 0.02 | 0.33 | 0.04 | 0.68 | <0.01 | 0.43 | 0.01 |
| Model 3: Adjusted for time, sleep/awake, Demographicsa, BMI, and smoking | 0.51 | 0.03 | 0.34 | 0.04 | 0.60 | 0.01 | 0.43 | 0.01 |
| Mastery N= 395 | ||||||||
| Model 1: Adjusted for time, and sleep/awake | −0.10 | 0.45 | 0.02 | 0.83 | −0.12 | 0.36 | −0.02 | 0.79 |
| Effortful Coping N=395 | ||||||||
| Model 1: Adjusted for time, and sleep/awake | 0.06 | 0.69 | 0.13 | 0.24 | 0.08 | 0.58 | 0.11 | 0.31 |
demographic covariates include age, race/ethnicity and three-way interaction (race/ethnicity, time, sleep/awake)
Fourteen women had hostility score of `0' (outliers) and were excluded from the analyses
DISCUSSION
In our examination of links among psychosocial variables assessed at mid-pregnancy and PTD we found that anomie was associated with medically indicated PTD in African American women not insured by Medicaid (recall that Medicaid is proxy for low socioeconomic status) and hostility was associated with spontaneous PTD in women not insured by Medicaid, irrespective of race/ethnic group. The associations found only among women who were NOT insured by Medicaid may in part be explained by poor women's greater exposure to other risk factors (e.g. infection, substance use, unhealthy diet) that contribute to more complex causal models thereby making the association between psychosocial measures and PTD appear less important. However, in models of anomie and hostility in relation to maternal vascular indices, positive associations were found for all women, irrespective of social class or race/ethnicity. These findings offer support for the vascular hypothesis underlying detectable links between psychosocial factors and PTD, but also may be informative regarding future vascular health of groups of women who score high on anomie and hostility in pregnancy. Also not to be ruled out, is the hypothesis that anomie and hostility may be related to other PTD pathways such as infection and immune status, untested in this study.
Levels of anomie and hostility in pregnancy were correlated and both followed a gradient, i.e. higher levels among those exposed to social class-related or race-related disadvantage. If we assume that anomie reflects both the extent to which a group is integrated into their society, and the extent to which they understand/agree with the norms expected to guide their behavior, then it is reasonable to assume that groups who are more anomic (detached from society) may have a hostile orientation to the world, including negative beliefs about others (Beckham, Calhoun, Glenn, & Barefoot, 2002). Similarly groups who are empowered to cope and master their environment tend to be more connected to the structures and norms of their society. Differing distributions of anomie and hostility by racial/ethnic group and by social class suggest both a different reaction to the larger social environment and an environment not equally inclusive across groups. Macro-level factors such as economic instability, institutional racism, and neighborhood violence shape perspectives and may induce unhealthy physiologic responses creating an escalating spiral among groups most affected. Further, recent research linking loneliness and BP (Hawkley, Masi, Berry, & Cacioppo, 2006) provides an additional context to our results and implications for future research. Although anomie and loneliness are different, they are related constructs as was corroborated in our study results indicating a high correlation (.41).
Despite the moderate correlation between anomie and hostility, they were linked to different outcomes, i.e. anomie with medically indicated PTD and hostility with spontaneous PTD. The reasons are unclear but several factors may be pertinent. The clinical circumstances of PTD are not etiologically distinct and likely share some common pathways (Klebanoff & Shiono, 1995). In addition, there was evidence that anomie and hostility may affect maternal vascular health through different mechanisms. The connection between hostility and maternal vascular indices was more pervasive than that found with anomie. Furthermore, the inclusion of BMI and smoking as covariates tended to diminish relations between vascular indices and anomie but not hostility, suggesting these lifestyle factors may be stronger mediators of anomie. To gain greater insights, future plans include assessing anomie and hostility levels in association with medically indicated PTD subgroups that reflect more distinct entities (e.g. abruption, pre-eclampsia, problems of fetal growth) and with placental pathology findings that identify subtypes of maternal and fetal vascular complications.
This study had several limitations. Linking single psychosocial variables with PTD is just a beginning to uncovering what is likely to be a complex web of relevant social and personal antecedents. Variables representing education and social class (Medicaid) may not fully capture differences in economic disadvantage and therefore residual confounding may have biased results. Furthermore, self-report-based psychosocial assessment of constructs like hostility may be influenced by factors such as self-awareness and item-comprehension difficulties (Barefoot & Lipkus, 1994). We attempted to address this by selecting psychosocial constructs for which there is an established track record, as well as good psychometric properties. But, especially with hostility, alternative, reliable methods using multiple informants and different approaches reveal the strongest association with CVD outcomes (Haney et al., 1996). Data from blood pressure monitoring were available for only a subset of the cohort, and therefore could not be modeled as intervening mechanisms in cohort analyses of psychosocial measures linked to PTD subtypes. Instead we used a two step approach, associating anomie and hostility with PTD subtypes and then anomie and hostility with maternal vascular indices in a subset. Though not all women elected to participate in the blood pressure monitoring when offered, there was no evidence that participation was self-selective by anomie and hostility levels. Finally, our significant results on anomie are based on a small number of African American women who had medically indicated PTD. These results need confirmation in future studies with larger samples.
A considerable strength of this study was the prospective collection of psychosocial data. At baseline measurement during pregnancy neither participants nor data collectors were aware of who would deliver preterm, which reduced the possibility of differential bias. The study sample was also large, represented many prenatal care settings (N=52), and was socioeconomically diverse which contributes to increased generalizability of the reported findings.
In addition, our research suggests there are multiple levels of variables affecting PTD, both personal and contextual. Studies to date have examined the context of income inequality, social disadvantage and socio-economic disparities and PTD (Colen, Geronimus, Bound, & James, 2006; Grady, 2006; Kahn, Wise, Kennedy, & Kawachi, 2000; Thompson, Irgens, Rasmussen, & Daltveit, 2006). And more recent studies have refined the contributory role of context in PTD, examining neighborhood disadvantage by census tract data (Reagan & Salsberry, 2005) and the complexities of segregation (Bell, Zimmerman, Almgren, Mayer, & Huebner, 2006). Our results suggest, in terms of PTD and blood pressure, the effects of context may not be confined to direct effects. Hostility which in the past has been linked to posttraumatic stress disorder (PTSD) (Butterfield, Forneris, Feldman, & Beckham, 2000) and trauma exposure (Zlotnick et al., 1996), was our most pervasive and robust variable. Hostility may represent not only effects on biologic systems, but also a reaction to the larger context. Also important for the contextual literature is our inclusion of alienation from social norms (anomie), one of the first studies, to our knowledge, to do so.
Our findings highlight the importance of linking physiologic measures to individuals’ responses to their environment and adverse pregnancy outcomes, as well as examining the complex, direct and indirect pathways to PTD.
Acknowledgments
This study is supported by grants from the National Institute of Child Health and Human Development (grants R01 HD34543-01 and R01 HD034543-07) and The March of Dimes Perinatal Epidemiological Research Initiative Program (grants 20-FY98-0697 through 20-FY04-37). The authors would also like to acknowledge the Prematurity Study Group who contributed to the psychosocial hypothesizing for this paper: Adrolado Zanella, Elizabeth Seagull, Janet Eyster, Joseph Marshall, Karen Fridericci, Larry VanEgeren, LeeAnne Roman, Pat Senagore, Renee Canady, and Ron Parsons.
Appendix
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Claudia B Holzman, Department of Epidemiology; Michigan State University, cholzman@epi.msu.edu.
Eric De Vos, Department of Psychology; Saginaw Valley State University, devos@svsu.edu.
Jia Xu, Department of Epidemiology; Michigan State University, xujia1@msu.edu.
Steve Korzeniewski, Department of Epidemiology, Michigan State University, skorzeniewski@epi.msu.edu.
Mohammad H Rahbar, Department of Epidemiology, Michigan State University, hrahbar@epi.msu.edu.
Monica M Goble, Pediatrics and Human Development; Michigan State University, Monica.Goble@hc.msu.edu.
David Kallen, Pediatrics and Human Development; Michigan State University, kallen@msu.edu.
REFERENCES
- Adams JH, Aubert RE, Clark VR. The relationship among John Henryism, hostility, perceived stress, social support, and blood pressure in African-American college students. Ethn Dis. 1999;9(3):359–368. [PubMed] [Google Scholar]
- Ananth CV, Joseph KS, Oyelese Y, Demissie K, Vintzileos AM. Trends in preterm birth and perinatal mortality among singletons: United States, 1989 through 2000. Obstet Gynecol. 2005;105(5 Pt 1):1084–1091. doi: 10.1097/01.AOG.0000158124.96300.c7. [DOI] [PubMed] [Google Scholar]
- Ayala DE, Hermida RC, Mojon A, Fernandez JR, Iglesias M. Circadian blood pressure variability in healthy and complicated pregnancies. Hypertension. 1997;30(3 Pt 2):603–610. doi: 10.1161/01.hyp.30.3.603. [DOI] [PubMed] [Google Scholar]
- Barefoot J, Lipkus I. The assessment of anger and hostility. In: Siegman AW, Smith TW, editors. Anger, hostility, and the heart. Lawrence Erlbaum Associates; Hillsdale, N.J.: 1994. pp. 43–66. [Google Scholar]
- Barefoot JC, Larsen S, von der Lieth L, Schroll M. Hostility, incidence of acute myocardial infarction, and mortality in a sample of older Danish men and women. Am J Epidemiol. 1995;142(5):477–484. doi: 10.1093/oxfordjournals.aje.a117663. [DOI] [PubMed] [Google Scholar]
- Beckham JC, Calhoun PS, Glenn DM, Barefoot JC. Posttraumatic stress disorder, hostility, and health in women: a review of current research. Ann Behav Med. 2002;24(3):219–228. doi: 10.1207/S15324796ABM2403_07. [DOI] [PubMed] [Google Scholar]
- Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med. 2006;63(12):3030–3045. doi: 10.1016/j.socscimed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Bellomo G, Narducci PL, Rondoni F, Pastorelli G, Stangoni G, Angeli G, et al. Prognostic value of 24-hour blood pressure in pregnancy. Jama. 1999;282(15):1447–1452. doi: 10.1001/jama.282.15.1447. [DOI] [PubMed] [Google Scholar]
- Butterfield MI, Forneris CA, Feldman ME, Beckham JC. Hostility and functional health status in women veterans with and without posttraumatic stress disorder: a preliminary study. J Trauma Stress. 2000;13(4):735–741. doi: 10.1023/A:1007874620024. [DOI] [PubMed] [Google Scholar]
- Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM. The contribution of preterm birth to infant mortality rates in the United States. Pediatrics. 2006;118(4):1566–1573. doi: 10.1542/peds.2006-0860. [DOI] [PubMed] [Google Scholar]
- Colen CG, Geronimus AT, Bound J, James SA. Maternal upward socioeconomic mobility and black-white disparities in infant birthweight. Am J Public Health. 2006;96(11):2032–2039. doi: 10.2105/AJPH.2005.076547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;157(1):14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- Dole N, Savitz DA, Siega-Riz AM, Hertz-Picciotto I, McMahon MJ, Buekens P. Psychosocial factors and preterm birth among African American and White women in central North Carolina. Am J Public Health. 2004;94(8):1358–1365. doi: 10.2105/ajph.94.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel-Schetter C, Rimi C. Pregnancy outcomes: Psychosocial aspects. In: Anderson NB, editor. Encyclopedia of health & behavior. Vol. 2. Sage Publications; Thousand Oaks, Calif.: 2004. pp. 669–671. H-Z. [Google Scholar]
- Fichera LV, Andreassi JL. Stress and personality as factors in women's cardiovascular reactivity. Int J Psychophysiol. 1998;28(2):143–155. doi: 10.1016/s0167-8760(97)00092-5. [DOI] [PubMed] [Google Scholar]
- Fullilove MT, Heon V, Jimenez W, Parsons C, Green LL, Fullilove RE. Injury and anomie: effects of violence on an inner-city community. Am J Public Health. 1998;88(6):924–927. doi: 10.2105/ajph.88.6.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med. 2000;342(20):1500–1507. doi: 10.1056/NEJM200005183422007. [DOI] [PubMed] [Google Scholar]
- Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med. 2006;63(12):3013–3029. doi: 10.1016/j.socscimed.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2005. 2006 Natl Vital Stat Rep Retrieved 1/25/07, from http://www.cdc.gov/nchs/products/pubs/pubd/hestats/prelimbirths05/prelimbirths 05.htm. [PubMed]
- Haney TL, Maynard KE, Houseworth SJ, Scherwitz LW, Williams RB, Barefoot JC. Interpersonal Hostility Assessment Technique: description and validation against the criterion of coronary artery disease. J Pers Assess. 1996;66(2):386–401. doi: 10.1207/s15327752jpa6602_16. [DOI] [PubMed] [Google Scholar]
- Hatch M, Berkowitz G, Janevic T, Sloan R, Lapinski R, James T, et al. Race, cardiovascular reactivity, and preterm delivery among active-duty military women. Epidemiology. 2006;17(2):178–182. doi: 10.1097/01.ede.0000199528.28234.73. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006;21(1):152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Hermida RC, Ayala DE, Mojon A, Fernandez JR, Alonso I, Silva I, et al. Blood pressure patterns in normal pregnancy, gestational hypertension, and preeclampsia. Hypertension. 2000;36(2):149–158. doi: 10.1161/01.hyp.36.2.149. [DOI] [PubMed] [Google Scholar]
- Hobel C, Culhane J. Role of psychosocial and nutritional stress on poor pregnancy outcome. J Nutr. 2003;133(5 Suppl 2):1709S–1717S. doi: 10.1093/jn/133.5.1709S. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Leiberman JR. Effects of mastery and intimacy on anxiety following pregnancy: For whom is support supportive and from whom? Anxiety Research. 1989;1(4):327–341. [Google Scholar]
- Holzman C, Bullen B, Fisher R, Paneth N, Reuss L. Pregnancy outcomes and community health: the POUCH study of preterm delivery. Paediatr Perinat Epidemiol. 2001;15(Suppl 2):136–158. doi: 10.1046/j.1365-3016.2001.00014.x. [DOI] [PubMed] [Google Scholar]
- Jain S, Dimsdale JE, Roesch SC, Mills PJ. Ethnicity, social class and hostility: effects on in vivo beta-adrenergic receptor responsiveness. Biol Psychol. 2004;65(2):89–100. doi: 10.1016/s0301-0511(03)00111-x. [DOI] [PubMed] [Google Scholar]
- James SA. John Henryism and the health of African-Americans. Cult Med Psychiatry. 1994;18(2):163–182. doi: 10.1007/BF01379448. [DOI] [PubMed] [Google Scholar]
- James SA, Hartnett SA, Kalsbeek WD. John Henryism and blood pressure differences among black men. Journal of Behavioral Medicine. 1983;6(3):259–278. doi: 10.1007/BF01315113. [DOI] [PubMed] [Google Scholar]
- Jones NM, Holzman CB, Zanella AJ, Leece CM, Rahbar MH. Assessing mid-trimester salivary cortisol levels across three consecutive days in pregnant women using an at-home collection protocol. Paediatr Perinat Epidemiol. 2006;20(5):425–437. doi: 10.1111/j.1365-3016.2006.00744.x. [DOI] [PubMed] [Google Scholar]
- Kahn RS, Wise PH, Kennedy BP, Kawachi I. State income inequality, household income, and maternal mental and physical health: cross sectional national survey. BMJ. 2000;321(7272):1311–1315. doi: 10.1136/bmj.321.7272.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebanoff MA, Shiono PH. Top down, bottom up and inside out: Reflections on preterm birth. Pediatric and Perinatal Epidemiology. 1995;9:125–129. doi: 10.1111/j.1365-3016.1995.tb00126.x. [DOI] [PubMed] [Google Scholar]
- Kramer MS, Goulet L, Lydon J, Seguin L, McNamara H, Dassa C, et al. Socio-economic disparities in preterm birth: causal pathways and mechanisms. Paediatr Perinat Epidemiol. 2001;15(Suppl 2):104–123. doi: 10.1046/j.1365-3016.2001.00012.x. [DOI] [PubMed] [Google Scholar]
- Kramer MS, Seguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr Perinat Epidemiol. 2000;14(3):194–210. doi: 10.1046/j.1365-3016.2000.00266.x. [DOI] [PubMed] [Google Scholar]
- Lockwood CJ. Stress-associated preterm delivery: the role of corticotropin-releasing hormone. Am J Obstet Gynecol. 1999;180(1 Pt 3):S264–266. doi: 10.1016/s0002-9378(99)70713-1. [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2003. Natl Vital Stat Rep. 2005;54(2):1–116. [PubMed] [Google Scholar]
- McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med. 1993;153(18):2093–2101. [PubMed] [Google Scholar]
- Meis PJ, Klebanoff M, Thom E, Dombrowski MP, Sibai B, Moawad AH, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–2385. doi: 10.1056/NEJMoa035140. [DOI] [PubMed] [Google Scholar]
- Orr ST, Miller CA. Maternal depressive symptoms and the risk of poor pregnancy outcome. Review of the literature and preliminary findings. Epidemiol Rev. 1995;17(1):165–171. doi: 10.1093/oxfordjournals.epirev.a036172. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19:2–21. [PubMed] [Google Scholar]
- Peters RM. The relationship of racism, chronic stress emotions, and blood pressure. Journal of Nursing Scholarship. 2006;38(3):234–240. doi: 10.1111/j.1547-5069.2006.00108.x. [DOI] [PubMed] [Google Scholar]
- Raghunathan TE, Solenberger PW, Van Hoewyk J. IVEware: Imputation and variance estimation software. Survey Methodology Program, Survey Research Center, Institute for Social Research, University of Michigan; Ann Arbor: 1998. [Google Scholar]
- Reagan PB, Salsberry PJ. Race and ethnic differences in determinants of preterm birth in the USA: broadening the social context. Soc Sci Med. 2005;60(10):2217–2228. doi: 10.1016/j.socscimed.2004.10.010. [DOI] [PubMed] [Google Scholar]
- Rini CK, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: the role of personal resources, stress, and sociocultural context in pregnancy. Health Psychol. 1999;18(4):333–345. doi: 10.1037//0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- Russell RB, Petrini JR, Damus K, Mattison DR, Schwarz RH. The changing epidemiology of multiple births in the United States. Obstet Gynecol. 2003;101(1):129–135. doi: 10.1016/s0029-7844(02)02316-5. [DOI] [PubMed] [Google Scholar]
- Samadi AR, Mayberry RM. Maternal hypertension and spontaneous preterm births among black women. Obstet Gynecol. 1998;91(6):899–904. doi: 10.1016/s0029-7844(98)00087-8. [DOI] [PubMed] [Google Scholar]
- SAS Institute . Base SAS 9.1.3 procedures guide. 2nd ed. SAS Pub; Cary, NC: 2006. [Google Scholar]
- Savitz DA, Pastore LM. Causes of Prematurity. In: McCormick MC, Siegel JE, editors. Prenatal care : effectiveness and implementation. Cambridge University Press; Cambridge, UK ; New York, NY: 1999. pp. 63–104. [Google Scholar]
- Spicer J, Chamberlain K. Cynical hostility, anger, and resting blood pressure. J Psychosom Res. 1996;40(4):359–368. doi: 10.1016/0022-3999(95)00546-3. [DOI] [PubMed] [Google Scholar]
- Srole L. Social integration and certain corollaries. American Sociological Review. 1956;21:709–716. [Google Scholar]
- Thompson JM, Irgens LM, Rasmussen S, Daltveit AK. Secular trends in socio-economic status and the implications for preterm birth. Paediatr Perinat Epidemiol. 2006;20(3):182–187. doi: 10.1111/j.1365-3016.2006.00711.x. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD, Culhane JF, Rauh V, Barve SS, Hogan V, Sandman CA, et al. Stress, infection and preterm birth: a biobehavioural perspective. Paediatr Perinat Epidemiol. 2001;15(Suppl 2):17–29. doi: 10.1046/j.1365-3016.2001.00005.x. [DOI] [PubMed] [Google Scholar]
- Waugh J, Perry IJ, Halligan AW, De Swiet M, Lambert PC, Penny JA, et al. Birth weight and 24-hour ambulatory blood pressure in nonproteinuric hypertensive pregnancy. Am J Obstet Gynecol. 2000;183(3):633–637. doi: 10.1067/mob.2000.106448. [DOI] [PubMed] [Google Scholar]
- Wielgosz AT, Nolan RP. Biobehavioral factors in the context of ischemic cardiovascular diseases. Journal of Psychosomatic Research. 2000;48(4−5):339–345. doi: 10.1016/s0022-3999(99)00093-8. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Zakriski AL, Shea MT, Costello E, Begin A, Pearlstein T, et al. The long-term sequelae of sexual abuse: support for a complex posttraumatic stress disorder. J Trauma Stress. 1996;9(2):195–205. doi: 10.1007/BF02110655. [DOI] [PubMed] [Google Scholar]