ABSTRACT
OBJECTIVE
To survey program directors of family medicine–emergency medicine (CCFP[EM]) training programs regarding current and future emergency medicine ultrasonography (EMUS) training.
DESIGN
A Web-based survey using a modified Dillman method. Two academic emergency physicians reviewed the validity and reliability of the survey.
SETTING
Canada.
PARTICIPANTS
Program directors of all 17 Canadian CCFP(EM) residency training programs in 2006.
MAIN OUTCOME MEASURES
Characteristics of EMUS training currently offered and program directors’ perceptions of needs for future EMUS training.
RESULTS
The survey, performed in 2006, had a response rate of 100% (17/17), although not all respondents answered all questions. At the time of the study, 82.4% of respondents’ programs used EMUS. Although all program directors recommended that residents attend introductory EMUS courses, only 71.4% (10/14) of programs offered such courses; 60.0% (9/15) of those were mandatory. In one-third of the programs, more than 75% of the attending staff used EMUS. A total of 76.5% of program directors thought that introductory courses in EMUS should be mandatory; 62.5% (10/16) believed that residents were able to acquire sufficient experience to use EMUS independently to make practice decisions before completion of their residency; and 88.2% believed that EMUS should be a part of the scope of practice for emergency medicine physicians. Only 58.8% believed that there should be questions about EMUS on the CCFP(EM) Certification examination. Open responses indicated that funding, resources, and standardization were issues that needed to be addressed.
CONCLUSION
Formal EMUS training for CCFP(EM) programs is being introduced in Canada. Quality assurance needs to be strengthened. Most program directors thought that an introductory course in EMUS should be mandatory. Fewer directors, however, believed EMUS should be on the CCFP(EM) Certification examination until further funding, resources, and standardization of EMUS programs were in place.
RÉSUMÉ
OBJECTIF
Questionner les directeurs des programmes de résidence en médecine familiale-médecine d’urgence du (CMFC[MU]) sur la formation actuelle et future à l’utilisation de l’échographie en médecine d’urgence (EMU).
TYPE D’ÉTUDE
Enquête via le Web selon une méthode Dillman modifiée. Deux urgentistes universitaires ont révisé la validité et la fiabilité de l’enquête.
CONTEXTE
Canada.
PARTICIPANTS
Les directeurs de 17 programmes canadiens de résidence en CMFC(MU) en 2006. Caractéristiques de la formation actuellement offerte en EMU et perception des directeurs de programme quant aux besoins pour la formation future en EMU.
PRINCIPAUX PARAMÈTRES À L’ÉTUDE
Caractéristiques de la formation en EMU actuellement offerte et opinion des directeurs de programme sur les besoins futurs de la formation en EMU.
RÉSULTATS
L’enquête effectuée en 2006 a eu un taux de réponse de 100% (17/17), quoique les répondants n’aient pas tous répondu à toutes les questions. Au moment de l’enquête, 82,4 % des programmes étudiés incluaient l’EMU. Même si tous les directeurs recommandaient aux résidents de suivre les cours d’introduction à l’EMU, seulement 71,4 % (10/14) des programmes offraient ce cours; 60 % de ces cours étaient obligatoires. Dans un tiers des programmes, plus de 75 % du personnel en place utilisaient l’EMU. Un total de 76,5 % des directeurs de programme estimaient que le cours d’introduction à l’EMU devrait être obligatoire; 62,5 % (10/16) croyaient que les résidents pouvaient acquérir suffisamment d’expérience pour utiliser l’EMU de façon indépendante pour prendre des décisions dans leur pratique avant la fin de leur résidence; et 88,2 % croyaient que l’EMU devrait faire partie du champ de pratique des médecins de médecine d’urgence. Seulement 58,8 % croyaient que l’examen de certification du CMFC(MU) devrait inclure des questions sur l’EMU. Dans les questions ouvertes, on mentionnait que les questions du financement, des ressources et de la standardisation devaient être abordées.
CONCLUSION
De plus en plus de programmes CMFC(MU) au Canada ont recours à une formation en EMU. Le contrôle de la qualité doit être amélioré. La plupart des directeurs de programme croyaient qu’un cours d’introduction à l’EMU devrait être obligatoire. Toutefois, peu d’entre eux croyaient que l’EMU devrait faire partie de l’examen de certification du CMFC(MU) aussi longtemps que le financement, les ressources et la standardisation des programmes d’EMU n’auront pas été réglés.
A growing number of clinicians are using emergency medicine ultrasonography (EMUS) at the bedside in order to answer specific and focused questions relating to patients’ conditions.1,2 Generally, EMUS is considered to be an adjunct to the physical examination. It is a brief and focused procedure that primarily answers a binary question: Is the condition present or not?2,3 After its introduction in Europe and Japan in the 1980s, EMUS started appearing in the United States.4–6
Emergency medicine ultrasonography is a timely examination that improves outcomes in acute patients.7–10 In Canada, it is primarily used to recognize free fluid in trauma (focused assessment with sonography in trauma), to identify intrauterine pregnancy in the first trimester, to identify abdominal aortic aneurysms, to identify pericardial effusions and cardiac activity, or to assist in central venous catheterization. For the indications listed, EMUS seeks to answer a yes or no question only.
Training in EMUS is an essential part of residency in the United States and is listed in the Model of the Clinical Practice of Emergency Medicine.11 In 2002, 92% of emergency medicine residency programs reported offering EMUS instruction in the United States.12
As of 2008, EMUS proficiency became an official core competency of the Royal College of Physicians and Surgeons of Canada (RCPSC) emergency medicine standards.13 The Canadian Association of Emergency Physicians (CAEP) has published a position statement indicating that emergency departments should strive to have emergency department targeted ultrasound (EDTU) immediately available 24 hours a day, 7 days a week. The CAEP position statement also states that EDTU should be incorporated into emergency medicine residency programs of the RCPSC and the College of Family Physicians of Canada.14
The Collège des médecins du Québec has published guidelines regarding emergency ultrasound performed by nonradiologists.15 These describe instructions for competency as well as the importance of ultrasound training in emergency medicine programs.
In 2007, only a basic understanding of the roles of ultrasonography in trauma and first-trimester pregnancy was mentioned in Educational Objectives. National Guidelines: Family Medicine–Emergency Medicine Residency Programs. There was no mention of who should perform and interpret ultrasound scans. The objectives were revised in February 2009 and now include the performance and interpretation of EDTU.16
The objectives of this study were to determine the current state of EMUS training for family medicine-emergency medicine (CCFP[EM]) residents and the perceptions of program directors regarding needs for future training in EMUS for CCFP(EM) residents.
METHODS
All CCFP(EM) program directors across Canada were invited to participate in the study. (Universities offering CCFP(EM) training programs are listed in Box 1.) Site directors were excluded. The study was performed using a modified Dillman technique.17 Two academic, residency-trained, CCFP(EM) emergency physicians reviewed the survey for validity and reliability. The survey was pilot-tested by another academic, residency-trained, CCFP(EM) emergency physician. The Ottawa Hospital Research Ethics Board approved the study.
Box 1.
Canadian universities offering emergency medicine residency programs
Memorial University of Newfoundland
Dalhousie University
Laval University
University of Sherbrooke
University of Montreal
McGill University
University of Ottawa
Queen’s University
Northern Ontario School of Medicine
University of Toronto
McMaster University
University of Western Ontario
University of Manitoba
University of Saskatchewan
University of Alberta
University of Calgary
University of British Columbia
In November 2006, potential participants were e-mailed a link to a Web-based questionnaire to be completed anonymously. The questionnaire consisted of 17 yes-no and open-ended questions designed to assess current EMUS training and program directors’ perceptions about the needs for future EMUS training for CCFP(EM) residents. Nonrespondents were sent a reminder e-mail 2 weeks later. Descriptive statistics were used to analyze the data.
RESULTS
All 17 program directors invited to participate responded to the survey, although not all of them answered all of the questions. Overall, 82.4% of programs used EMUS. Although all the respondents recommended that CCFP(EM) residents attend introductory EMUS courses, only 71.4% (10/14) of programs actually offered introductory EMUS courses. Of those that offered such courses, only 60.0% (9/15) made them mandatory for residents. However, 76.5% of program directors thought that introductory EMUS courses should be mandatory in the future.
Less than half (42.9% [6/14]) of programs had formal quality assurance processes for EMUS. One program required 25 scans to be performed for each indication before residents could use EMUS independently, while the rest of the programs with such a process required 50 scans for each indication. Only half of programs required residents to have a minimum number of supervised or reviewed scans before using EMUS to influence clinical care. None of the programs had a compulsory requirement for residents to have a designated number of scans before completion of their residency.
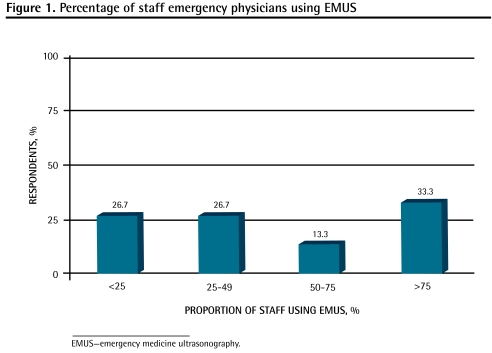
Figure 1 shows the proportion of staff emergency physicians from all the programs using EMUS.
Figure 1.
Percentage of staff emergency physicians using EMUS
Just over half of respondents (62.5% [10/16]) believed that CCFP(EM) residents were able to acquire sufficient experience to use EMUS independently and make subsequent practice decisions before completion of their residency, and 70.6% thought that EMUS should be a mandatory component of the CCFP(EM) curriculum. Most (88.2%) believed that EMUS should be a part of the scope of practice for CCFP(EM) practising physicians, yet only 58.8% believed that there should be questions about EMUS on the CCFP(EM) examination. Open responses indicated that funding, resources, and standardization of equipment were issues that needed to be addressed before training could become mandatory.
DISCUSSION
There continues to be increased access to ultrasound machines and experienced physicians performing EMUS in both community and academic centres. Many community and academic emergency departments advertising job positions recognize EMUS as an asset or even a requirement.
Training in EMUS usually involves an introductory course followed by supervised scanning by a competent instructor for a minimum number of cases. There is currently limited evidence on the number of scans required for competency; however, Canadian guidelines indicate that a minimum of 50 scans for each of free-fluid identification, abdominal aortic aneurysms, intrauterine pregnancy in the first trimester, and cardiac (pericardial effusion or activity) should be required.14,18,19 The time required to complete this training depends on a number of factors, but it can take more than 25 hours.
Given this reality, program directors face the challenge of incorporating EMUS training into a short residency period without detracting from the other learning opportunities. The CAEP position statement regarding EMUS indicates that training should be incorporated into emergency medicine residency programs and that a strong quality improvement process is integral in the safe practice of EDTU.14 Only 42.9% (6/14) of respondents indicated that their programs had formal quality assurance processes. Given that only half of programs required residents to perform a specified number of supervised or reviewed scans before using EMUS to influence clinical care and that no programs required this number to be completed before graduation, it is possible that very few graduating CCFP(EM) residents are competent in EMUS. Formal quality assurance programs should be strengthened to assure the safe use of EMUS.
Although EMUS requires substantial training time, education, and resources, 76.5% of program directors still believed that it should be a mandatory component of the CCFP(EM) curriculum. However, about two-thirds of program directors believed that residents were able to acquire sufficient experience during their residency to use EMUS independently and make subsequent practice decisions.
Many residency training programs use EMUS; however, less than half the programs have more than 50% of their staff emergency physicians using EMUS. Minimal attending staff using EMUS might be a barrier to resident use and training.20
Since the RCPSC made EMUS an official core competency in 2008, many academic centres have increased training and education for both attending staff and residents. This has resulted in programs providing or looking to provide training for their residents. Some CCFP(EM) program directors believed that EMUS training should not be mandatory during residency until standardization of equipment, teaching, and funding were in place. Circumstances in the United States, however, suggest that support might never come unless the certifying colleges make EMUS training mandatory first.21
Most CCFP(EM) program directors (88.2%) believed that EMUS should be part of the scope of practice for practising emergency physicians. Some comments suggested that there should be no difference in this training between the RCPSC emergency medicine programs and the CCFP(EM) programs. If, however, EMUS is not made mandatory for CCFP(EM) training, a substantial difference could arise between programs that do and do not include this skill.
At the time of this study, CCFP(EM) program directors recommended exposing residents to EMUS and requiring participation in introductory EMUS courses. That said, they did not recommend that the ability to use EMUS be a core competency for CCFP(EM) physicians.
Limitations
The study elicited the perceptions of program directors, which might not reflect the position of the actual programs or that of the College of Family Physicians of Canada. In addition, this is a survey of CCFP(EM) residency training and it does not address the practice-eligible route for CCFP(EM) training. It is important to note that one of the authors (C.N.) is a program director. In order to adequately reflect all programs, his responses as the program director were included. Given that we had a response rate of 100%, the survey results should be interpreted with this in mind.
Conclusion
Most programs use EMUS and program directors believe EMUS should be part of the scope of practice for CCFP(EM) physicians. Some EMUS training is available in most CCFP(EM) programs, but quality assurance programs need to be strengthened. Most directors thought that an introductory course in EMUS should be mandatory; however, fewer directors believed EMUS should be on the CCFP(EM) Certification examination until further funding, resources, and standardization of EMUS programs are in place.
Acknowledgment
We would like to thank the program directors for participating in the study.
EDITOR’S KEY POINTS
A growing number of clinicians are using emergency medicine ultrasonography (EMUS) at the bedside in order to answer specific and focused questions relating to patients’ conditions, and various guidelines and position statements support the need for emergency medicine physicians to have the skills to perform EMUS. Training in EMUS in 2006, when the survey was undertaken, was not yet an essential part of emergency medicine residency.
This study aimed to assess program directors’ perspectives on the EMUS training currently offered in emergency medicine residency programs and what training should look like in the future.
Given that only half of the programs required residents to perform a specified number of supervised or reviewed scans before using EMUS to influence clinical care and that no programs required this requisite to be completed before graduation, it is possible that very few graduating residents are competent in EMUS. As use of EMUS continues to increase, training and quality assurance will have to be strengthened, and funding, resources, and standardization of equipment will need to be addressed.
POINTS DE REPÈRE DU RÉDACTEUR
De plus en plus de cliniciens utilisent l’échographie en médecine d’urgence (EMU) au lit du malade pour répondre à des questions spécifiques et précises concernant la condition des patients, et diverses directives et déclarations de principe viennent appuyer le fait que les médecins de médecine d’urgence doivent être en mesure d’utiliser l’EMU. En 2006, au moment où l’enquête a été menée, la formation en EMU n’était pas encore une partie essentielle de la résidence en médecine d’urgence.
Cette étude voulait connaître l’opinion des directeurs de programme sur la formation à l’EMU actuellement offerte dans les programmes de résidence en médecine d’urgence et sur ce qu’ils souhaitaient qu’elle soit dans l’avenir.
Comme seulement la moitié des programmes exigeaient que les résidents effectuent un certain nombre de tomodensitogrammes supervisés ou révisés avant d’utiliser l’EMU comme moyen d’influencer les soins cliniques, et qu’aucun des programmes n’avait une telle exigence avant d’attribuer le diplôme, il est possible que très peu de résidents diplômés soient compétents en EMU. À mesure que l’utilisation de l’EMU augmente, la formation et le contrôle de la qualité devront être renforcés et il faudra régler les questions de financement, de ressources et de standardisation de l’équipement.
Footnotes
This article has been peer reviewed.
*Full text is available in English at www.cfp.ca.
Contributors
Drs Woo, Nussbaum, and Lee conceived the study, designed and participated in the trial, and drafted and revised the manuscript. Dr Lee provided statistical advice on study design and analyzed the data.
Competing interests
None declared
References
- 1.Society for Academic Emergency Medicine. Emergency ultrasonography. Lansing, MI: Society for Academic Emergency Medicine; [Accessed 2009 Aug 31]. Available from: www.saem.org/saemdnn/Home/Communities/Fellows/Fellowship/EmergencyUltrasonography/tabid/189/Default.aspx. [Google Scholar]
- 2.American College of Emergency Physicians. ACEP emergency ultrasound guidelines—2001. Ann Emerg Med. 2001;38(4):470–81. [PubMed] [Google Scholar]
- 3.Heller MB, Mandavia D, Tayal VS, Cardenas EE, Lambert MJ, Mateer J, et al. Residency training in emergency ultrasound: fulfilling the mandate. Acad Emerg Med. 2002;9(8):835–9. doi: 10.1111/j.1553-2712.2002.tb02174.x. [DOI] [PubMed] [Google Scholar]
- 4.Kimura A, Otsuka T. Emergency center ultrasonography in the evaluation of acute hemoperitoneum: a prospective study. J Trauma. 1991;31(1):20–3. doi: 10.1097/00005373-199101000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Aufschnaiter M, Kofler H. Sonographic acute diagnosis in polytrauma [article in German] Aktuelle Traumatol. 1983;13(2):55–7. [PubMed] [Google Scholar]
- 6.Trott A. Ultrasonography in emergency medicine. J Emerg Med. 1984;1(6):549. doi: 10.1016/0736-4679(84)90011-8. [DOI] [PubMed] [Google Scholar]
- 7.Blaivas M, Sierzenski P, Pleque D, Lambert M. Do emergency physicians save time when locating a live intrauterine pregnancy with bedside ultrasonography? Acad Emerg Med. 2000;7(9):988–93. doi: 10.1111/j.1553-2712.2000.tb02088.x. [DOI] [PubMed] [Google Scholar]
- 8.Plummer D, Bruneete D, Asinger R, Ruiz E. Emergency department echo-cardiography improves outcome in penetrating cardiac injury. Ann Emerg Med. 1992;21(6):709–12. doi: 10.1016/s0196-0644(05)82784-2. [DOI] [PubMed] [Google Scholar]
- 9.Plummer D, Clinton J, Matthew B. Emergency department ultrasound improves time to diagnosis and survival in ruptured abdominal aortic aneurysm [abstract] Acad Emerg Med. 1998;5(5):417. [Google Scholar]
- 10.National Quality Forum. Safe practices for better health care. A consensus report. Washington, DC: National Quality Forum; 2003. [Accessed 2009 Aug 3]. Available from: www.qualityforum.org. [Google Scholar]
- 11.Hockberger RS, Binder LS, Graber MA, Hoffman GL, Perina DG, Schneider SM, et al. The model of the clinical practice of emergency medicine. Ann Emerg Med. 2001;37(6):745–70. doi: 10.1067/mem.2001.115495. [DOI] [PubMed] [Google Scholar]
- 12.Moore CL, Gregg S, Lambert M. Performance, training, quality assurance, and reimbursement of emergency physician-performed ultrasonography at academic medical centers. J Ultrasound Med. 2004;23(4):459–66. doi: 10.7863/jum.2004.23.4.459. [DOI] [PubMed] [Google Scholar]
- 13.Royal College of Physicians and Surgeons of Canada. Objectives of training in emergency medicine. Ottawa, ON: Royal College of Physicians and Surgeons of Canada; 2008. [Accessed 2009 Aug 26]. Available from: http://rcpsc.medical.org/residency/certification/objectives/emergmed_e.pdf. [Google Scholar]
- 14.Socransky S Emergency Department Targeted Ultrasound Interest Group, Canadian Association of Emergency Physicians. Emergency department targeted ultrasound: 2006 update. CJEM. 2006;8(3):170–1. 172–4. Eng. Fr. [PubMed] [Google Scholar]
- 15.Collège des médecins du Québec. Les échographies ciblées réalisées à l’urgence par des médecins non radiologistes. Montreal, QC: Collège des médecins du Québec; 2008. [Accessed 2008 Apr 16]. Available from: www.cmq.org/fr/MedecinsMembres/Profil/Commun/AProposOrdre/Publications/~/media/98AB338131B24461B797E47117A16514.ashx?sc_lang=fr-CA&80927. [Google Scholar]
- 16.Mackey DS, Steiner IP, editors. Educational objectives. National guidelines: family medicine–emergency medicine residency programs. Mississauga, ON: College of Family Physicians of Canada; [Accessed 2009 Aug 31]. Available from: www.cfpc.ca/English/cfpc/education/accreditation/default.asp?s=1. [Google Scholar]
- 17.Dillman DA. Mail and Internet surveys: the tailored design method. 2nd ed. New York, NY: John Wiley Co; 2000. [Google Scholar]
- 18.Canadian Emergency Ultrasound Society. Recommended standards. Canadian Emergency Ultrasound Society; 2008. [Accessed 2008 Apr 16]. Available from: www.ceus.ca/002-standards/002-00.standards.htm. [Google Scholar]
- 19.FocusED Sonography. Quality assurance/post course learning. Huntsville, ON: FocusED Sonography; 2008. [Accessed 2008 Apr 16]. Available from: http://feds.resuscitation.ca/FEDS_QualityAssurance.pdf. [Google Scholar]
- 20.Woo MY, Reardon M, Lee AC, Frank JF. Perceived barriers to emergency ultrasound use by emergency medicine residents: pilot study. CJEM. 2005;7(3):203. [Google Scholar]
- 21.Plummer D. Whose turf is it anyway? Diagnostic ultrasonography in the emergency department [comment] Acad Emerg Med. 2000;7(2):186–7. doi: 10.1111/j.1553-2712.2000.tb00525.x. [DOI] [PubMed] [Google Scholar]