Abstract
The aim of the study was to assess whether long-term antiretroviral therapy (ART) is associated with the risk of coronary plaques in HIV-infected cardiovascularly asymptomatic African Americans. Between August 2003 and December 2007, 176 HIV-infected cardiovascularly asymptomatic African Americans were consecutively enrolled in an observational study investigating the effects of ART on subclinical atherosclerosis in Baltimore, Maryland. Computed tomography coronary angiography was performed to detect coronary plaques. The overall prevalence rate of coronary plaques was 30%. After adjusting for gender, total cholesterol, and cocaine use, logistic regression analysis revealed that exposure to ART for more than 18 months (adjusted odds ratio [OR]: 2.20, 95% confidence interval [CI]: 1.01, 4.79) was independently associated with the presence of coronary plaques. A higher HIV viral load was univariately associated with the presence of noncalcified plaques. Use of ART (>18 months) was independently associated with the presence of noncalcified plaques (adjusted OR: 7.61, 95% CI: 1.67, 34.7), whereas cocaine use (>15 years) was independently associated with the presence of calcified plaques (adjusted OR: 2.51, 95% CI: 1.11, 5.67). This study suggests that long-term exposure to ART may be associated with coronary plaques. Because long-term use of ART and HIV replication may be associated with the presence of noncalcified plaques, some of which may be more vulnerable to rupture, an intensive lifestyle intervention to reduce traditional risk factors for coronary artery disease (CAD) is ultimately vital to those who are on ART. This study also suggests that cocaine cessation is the single most effective strategy to prevent CAD in HIV-infected cocaine users.
Introduction
Since the introduction of highly active antiretroviral therapy (HAART), there has been a dramatic improvement in survival among persons with HIV infection. As HIV-infected individuals now live longer, cardiovascular complications have emerged. However, the etiologies of cardiovascular complications in HIV-infected persons remain poorly understood since investigations of the etiologies may have been confounded by a variety of factors, including severity of HIV infection, classes of antiretroviral therapy (ART), and drug use. A pathologic study showed that HIV directly infected human arterial smooth muscle cells, suggesting that HIV infection per se might explain the exacerbated atherosclerosis and vasculopathy in HIV-infected individuals.1 The long-term effects of ART on clinically symptomatic coronary artery disease (CAD) in HIV-infected persons have been reported, but the findings are not consistent.2–5 Recent studies suggest that ART might promote subclinical atherosclerosis,6 and certain class of ART may be associated with a lower cardiovascular risk.7 Although compared to those investigations, some large, much better controlled studies suggest no impact on subclinical atherosclerosis of either HIV infection alone or the use of ART or protease inhibitors (PIs) as a class, when individual drugs were evaluated (such as ritonavir and non-nucleoside reverse transcriptase inhibitor (NNRTI), an association was seen.8,9 The prevalence of carotid plaque and carotid artery intima-media thickness and their relation to HIV infection and ART have been reported10; however, little work has been done to investigate the effects of HIV infection and ART on coronary plaques. Although underlying traditional risk factors have been implicated in cardiovascular complications in HIV-infected individuals, their relative contributions to CAD, especially early-stage CAD, in this population have not been addressed. Furthermore, little is known about how some nontraditional risk factors, such as use of illicit drugs, may interact with ART and traditional risk factors and thus may have additional impact on CAD.
In a study using computed tomography (CT) coronary angiography, the authors recently found that long-term use of ART (≥6 months) was independently associated with the presence of significant coronary stenosis (defined as ≥50%).11 However, since the prevalence of significant coronary stenosis was low (15%), the power to identify factors that were independently associated with significant coronary stenosis was limited. The aim of the present study was to examine the long-term effects of ART and other factors on coronary plaques, an early stage of CAD. The primary objectives of this study were (1) to estimate the prevalence of the presence of coronary plaques by using contrast-enhanced CT coronary angiography in HIV-infected persons and (2) to examine the individual and combined effects of ART and other factors, including cocaine use, on the presence of coronary plaques and plaque composition in African Americans with HIV infection.
Methods
Study participants
Between August 2003 and December 2007, 176 HIV-infected African American participants were consecutively enrolled in an observational study investigating the effects of antiretroviral regimens on subclinical atherosclerosis at the Johns Hopkins Hospital, Baltimore, Maryland.
Inclusion criteria were age between 25 and 54 years and African American race (self-designated). Exclusion criteria were (1) any evidence of hypertension or CAD, (2) any symptoms believed to be related to CAD, (3) any evidence of renal insufficiency, (4) known allergy to the contrast used for the CT, and (5) pregnancy. Each subject was interviewed to obtain information on sociodemographic characteristics, cigarette smoking, alcohol use, illicit drug-use behaviors, medical history, and all medications used. Cocaine use was defined as long-term use of cocaine by any route for at least 6 months, administered at least four times a month. Information was collected about the frequency (how many times a day in the past week, in the past month), patterns/forms of cocaine (speedball, crack, etc.), administration mode (injection, smoking, etc.), and duration of cocaine use. Information was also collected about use of other drugs, such as opiates, benzodiazepines, or methamphetamine. A medical chart review was used to confirm information on medical history and medications that was provided by the subjects. Each subject also had a physical examination, and several tests were performed: namely, a fasting lipid profile, high-sensitivity C-reactive protein (hs-CRP) test, contrast-enhanced 64-slice multidetector computed tomography (MDCT) for coronary artery calcium (CAC), and CT coronary angiography.
The Committee on Human Research at the Johns Hopkins School of Medicine approved the study protocol, and all study participants provided written informed consent. All procedures used in this study were in accordance with institutional guidelines.
Coronary CT angiography with a 64-slice Siemens MDCT scanner
A noncontrast MDCT scan was performed on a Sensation 64 Cardiac Siemens Medical Solutions scanner (Erlangen, Germany) to determine the CAC score with a sequential scan of 3-mm slices with prospective ECG triggering, 30 × 0.6-mm detector collimation, and tube current 135 mÅs at 120 kV. Subsequently, CT coronary angiography (CTA) was performed on the same equipment using 80 mL of isosmolar contrast agent (320 mg iodine per milliliter) injected at 4–5 mL/s. CAC score, volume, and mass were measured on a workstation (Leonardo, Syngo, Siemens Medical Solutions, Malvern, PA). Regions of interest were placed over each of the coronary arteries with the threshold for pixels greater than 130 HU for determining calcified plaque.
Two reviewers (H.P. and E.K.F.) independently evaluated (both were blinded to the risk profile of participants) the contrast-enhanced MDCT scans by examining the axial slices, curved multiplanar reformations, and thin-slab maximum intensity projections. The coronary artery tree was segmented according to the modified American Heart Association (AHA) classification, and the segments were investigated for plaque and lumenal narrowing.12 The coronary arteries were divided into proximal, mid-, and distal segments, with each segment investigated for lumenal narrowing. Plaques were classified as calcified or noncalcified. Noncalcified atherosclerotic plaque was defined as a soft tissue attenuation structure in the coronary artery wall with a CT density that was less than that of calcified plaque, as well as less than that of the contrast in the lumen, but was greater than the adjacent epicardial fat. For determining the mean attenuation of noncalcified plaques, the vessel segment was displayed in the short axis plane orthogonal to the vessel or the long-axis plane of the vessel on 0.75-mm-thick slices in multiplanar reformation. The plane that demonstrated the thickest width of the plaque was selected for measuring the attenuation. The largest possible region of interest was then manually placed on the plaque, avoiding overlap with adjacent tissue or vessel lumen.
Statistical analysis
Statistical analysis was performed with SAS (SAS, Cary, NC). All continuous parameters were summarized by medians and interquartile ranges (IQRs), and all categorical parameters were summarized as proportions. To compare between-group differences, the nonparametric Wilcoxon two-sample test was used for continuous variables, and the Fisher's exact test was used for categorical variables. The Clopper-Pearson approach was used to calculate 95% exact binomial confidence intervals. A logistic regression model was used to examine associations between factors and the presence of coronary plaques.13 Univariate logistic regression models were first fitted to evaluate the crude association between the presence of coronary plaques and each of the factors—age, gender, total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides, hsCRP, cigarette smoking, alcohol use, glucose level, blood pressure (BP), body mass index, current CD4 cell count, current HIV RNA quantification, ART, and cocaine or other illicit drug use, individually. Variables on cocaine and other illegal drug use included frequency, forms, administration mode (injection, smoking, etc.), and duration of use. Since the median years of cocaine use was 16, cocaine use was categorized as both a dichotomous variable “cocaine use >15 years vs. otherwise” and a trichotomous variable “never used, used for ≤15 years, or used for >15 years.” ART was categorized on the basis of exposure to three classes—nucleoside reverse transcriptase inhibitors (NRTIs), NNRTIs, and PIs —and the duration of ART use. Those factors that were significant at the p ≤ 0.10 level in the univariate models were put into the multiple logistic regression models to identify the factors that were independently associated with coronary plaques. Those variables that ceased to make significant contributions to the models were deleted in a stagewise manner, yielding the final models. To explore whether short-term (up to 6 months) use of ART increased or decreased the CAD risk, duration of ART use was categorized as trichotomous (ART naïve or use for ≤6 months, use for between 6.1 and 18 months, or use for >18 month). The Framingham risk score was calculated to estimate the CAD risk.14
To evaluate the magnitude of potential risk associated with ART, the squared multiple correlation coefficient R2 proposed for the logistic regression model was used to measure the proportion of variation explained (PVE) by potential risk factors.15 This measure is similar to the multiple R2 of the general linear model and has an intuitively clear interpretation. The p values reported are two-sided. A p value <0.05 indicated statistical significance.
Results
General characteristics
The general and clinical characteristics of the study participants, with or without coronary plaques, are presented in Table 1.
Table 1.
Demographic, Laboratory, and Clinical Factors in Relation to the Risk of Presence of Coronary Plaques
| |
|
Presence of coronary plaques |
|
|
|---|---|---|---|---|
| Characteristic | Total (n = 176) | No (n = 124) | Yes (n = 52) | p value |
| Age (years) | 44.2 (39.9–47.3) | 42.9 (38.6–46.0) | 47.3 (43.5–49.5) | <0.0001 |
| Female (%) | 36.9 | 44.4 | 19.2 | 0.002 |
| Family history of CAD (%) | 23.8 | 22.6 | 26.9 | 0.54 |
| CD4 (count/mm3) | 344 (177–498) | 346 (177–516) | 314 (216–498) | 0.67 |
| Plasma HIV viral load (copies/mL) | 581 (30–14789) | 638 (30–22771) | 300 (30–12852) | 0.60 |
| Cocaine use (%) | 90.9 | 88.7 | 96.2 | 0.12 |
| Cocaine use ≥15 y (%) | 34.1 | 27.4 | 50.0 | 0.004 |
| Cigarette smoking (%) | 86.4 | 85.5 | 88.5 | 0.60 |
| Cigarette smoking ≥15 y (%) | 77.8 | 75.0 | 84.6 | 0.53 |
| Alcohol use (%) | 89.8 | 88.7 | 92.3 | 0.47 |
| hs-CRP ≥2 mg/dL (%) | 41.7 | 42.7 | 39.2 | 0.67 |
| hsCRP (mg/dL) | 1.5 (0.6–4.1) | 1.5 (0.6–4.4) | 1.5 (0.6–3.4) | 0.62 |
| Systolic BP (mm Hg) | 111 (103–120) | 111 (103–119) | 111 (108–121) | 0.24 |
| Diastolic BP (mm Hg) | 74 (69–81) | 73 (69–81) | 77 (66–82) | 0.44 |
| Glucose (mg/dL) | 84 (78–90) | 84 (78–89) | 86 (80–94) | 0.14 |
| BMI (kg/m2) | 23.8 (21.5–27.3) | 24.1 (21.9–27.3) | 23.7 (21.4–27.2) | 0.71 |
| Total cholesterol (mg/dL) | 161 (142–186) | 158 (137–181) | 170 (157–196) | 0.005 |
| LDL-C (mg/dL) | 86 (70–107) | 81 (67–107) | 94 (80–113) | 0.019 |
| HDL-C (mg/dL) | 49 (38–60) | 48 (38–59) | 51 (35–63) | 0.80 |
| Triglycerides (mg/dL) | 107 (73–151) | 100 (72–138) | 132 (78–173) | 0.025 |
| Years of cocaine use | 13 (5–20) | 11 (5–17) | 16 (6–22) | 0.013 |
| Duration of ART use (mo) | ||||
| NRTIs | 0 (0–12) | 0 (0–12) | 0 (0–30) | 0.048 |
| NNRTIs | 0 (0–0) | 0 (0–0) | 0 (0–15) | 0.0017 |
| PIs | 0 (0–12) | 0 (0–6) | 0 (0–24) | 0.06 |
| All | 3 (0–24) | 1 (0–20) | 19 (0–47) | 0.001 |
| Coronary calcification (%) | 25.6 | 4.8 | 75.0 | <0.0001 |
| Framingham risk score | 3.5 (2.0–5.0) | 3 (2–4) | 5 (4–8) | <0.0001 |
| Framingham score ≥3.0 (%) | 69.5 | 61.3 | 90 | <0.0001 |
Median (interquartile range) for continuous variables, proportion (%) for categorical variables.
CAD, coronary artery disease; CD4, CD4 cell count; HIV, human immunodeficiency virus; hs-CRP, high sensitivity C-reactive protein; BP, blood pressure; glucose, fasting glucose; BMI, body mass index; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; Framingham score, Framingham risk score; NRTIs, nucleoside reverse transcriptase inhibitors; NNRTIs, nonnucleoside reverse transcriptase inhibitors; PIs, protease inhibitors; ART, antiretroviral therapy.
According to the Framingham risk score algorithm, 94 (53.4%) of the total 176 participants (63 of the 111 men and 31 of the 65 women) had low risk of CAD; 22 (42.3%) of the 52 participants with coronary plaques (18 of the 42 men and 4 of the 10 women) had low risk of CAD.9
Prevalence of coronary plaques
The overall prevalence of the presence of coronary plaques was 29.5% (52/176, 95% CI: 22.9%, 36.9%), whereas the prevalence in those who never used cocaine and were not on ART was 6.7% (1/15, 95% CI: 0.2%, 32.0%).
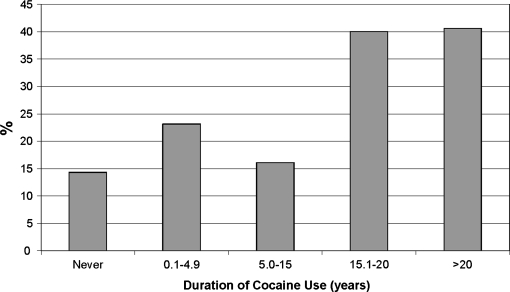
Prevalence by duration of ART use
There was no statistical difference between the prevalence of coronary plaques in those who were ART naïve (20.8%) and those who used ART for 6 months or less (15.8%; p > 0.6); therefore, ART-naïve and ART 6 months or less subjects were further analyzed as a single group. The prevalences of the presence of coronary plaques, noncalcified plaques, and calcified plaques, by duration of ART use, are presented in Figure 1.
FIG. 1.
Demographic, Laboratory, and Clinical Factors in Relation to the Risk of Presence of Coronary Plaques
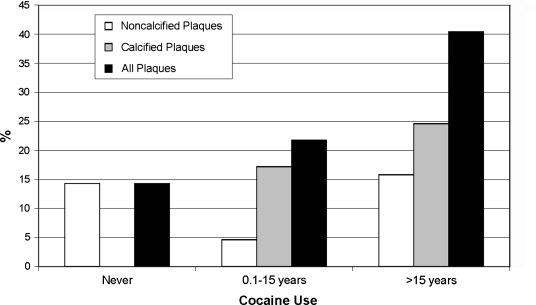
Prevalence, by duration of cocaine use
The prevalences of plaques, by the duration of cocaine use, are presented in Figure 2. The difference in prevalence between those who had never used cocaine (13.0%) and those who had used cocaine for 15 years or less (24.7%) was not significant (p > 0.2); however, the prevalence in those who used cocaine for more than 15 years (43.3%) was significantly higher than that in those who had not used cocaine (p < 0.01) and that in those who used cocaine for 15 years or less (p < 0.01).
FIG. 2.
Demographic, Laboratory, and Clinical Factors in Relation to the Risk of Presence of Coronary Plaques
The prevalences of noncalcified plaques, by the duration of cocaine use, are shown in Figure 3. The prevalences of noncalcified plaques were 13.0% (3/23), 4.3% (4/93), and 15.0% (9/60) in those who had never used cocaine, who had used cocaine for 15 years or less, and who had used cocaine for more than 15 years, respectively. The prevalences of calcified plaques were 0.0% (0/23), 20.4% (19/93), and 28.3% (17/60) in those who had never used cocaine, who had used cocaine for 15 years or less, and who had used cocaine for more than 15 years, respectively.
FIG. 3.
Demographic, Laboratory, and Clinical Factors in Relation to the Risk of Presence of Coronary Plaques
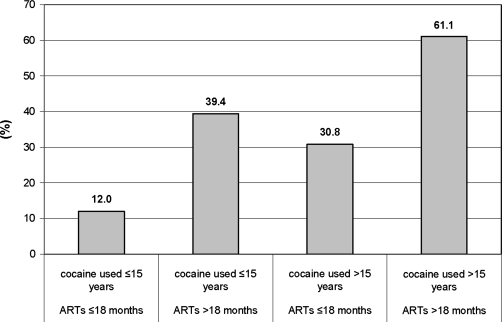
Prevalence, by duration of cocaine use and ART exposure
The prevalences were 15.2% (12/79) in those who had never used cocaine or used it 15 years or less and were never on ART or were on ART 18 months or less; 37.8% (14/37) in those who had never used cocaine or had used it 15 years or less but were on ART more than 18 months; 35.0% (14/40) in those who used cocaine for more than 15 years and never were on ART or on ART 18 months or less; and 60.0% (12/20) in those who had used cocaine more than 15 years and were on ART 18 months or more (Figure 4).
FIG. 4.
Demographic, Laboratory, and Clinical Factors in Relation to the Risk of Presence of Coronary Plaques
Factors associated with the presence of coronary plaques
By univariate logistic regression analyses, traditional risk factors associated with the presence of coronary plaques included age 50 years or more, male gender, total serum cholesterol ≥160 mg/dL, triglycerides ≥130 mg/dL, and Framingham risk score 3 or more. Nontraditional risk factors associated with the presence of coronary plaques included cocaine use for more than 15 years, and the use of NRTIs, NNRTIs, and PIs for more than 18 months, use of NNRTIs for more than 18 months (Table 2).
Table 2.
Demographic, Laboratory, and Clinical Factors in Relation to the Risk of Presence of Coronary Plaques
| |
All plaques |
Noncalcified plaques |
Calcified plaques |
|||
|---|---|---|---|---|---|---|
| Variable | Crude OR (95% CI) | Adjusted OR (95% CI) | Crude OR (95% CI) | Adjusted OR (95% CI) | Crude OR (95% CI) | Adjusted OR (95% CI) |
| Age (y) | ||||||
| <50 | 1.00 | 1.00 | 1.00 | 1.00 | ||
| ≥50 | 4.35 (1.66, 11.4) | 3.11 (1.04,9.30) | 3.00 (0.87, 10.4) | 3.05 (1.14, 8.15) | ||
| Gender | ||||||
| Female | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Male | 3.35 (1.54, 7.27) | 4.23 (1.79, 10.0) | 1.85 (0.57, 5.99) | 3.64 (1.43, 9.31) | 4.32 (1.60, 11.7) | |
| Family history of CAD | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 1. 26 (0.61, 2.66) | 2.07 (0.70, 6.07) | 0.89 (0.37, 2.14) | |||
| CD4 count (cells/mm3) | ||||||
| >200 | 1.00 | 1.00 | 1.00 | |||
| ≤200 | 0.74 (0.28, 1.95) | 0.24 (0.01, 1.77) | 1.29 (0.44, 3.74) | |||
| HIV RNA (copies/mL) | ||||||
| <400 | 1.00 | 1.00 | 1.00 | |||
| ≥400 | 1.26 (0.52, 3.02) | 5.40 (1.10, 26.4) | 0.50 (0.17, 1.46) | |||
| Cocaine use | ||||||
| Never | 1.00 | 1.00 | 1.00 | |||
| Ever | 3.18 (0.70, 14.5) | 0.67 (0.14, 3.26) | not estimable | |||
| Years of cocaine use | ||||||
| ≤15 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| >15 | 2.65 (1.35, 5.18) | 2.67 (1.23, 5.83) | 0.75 (0.97, 7.79) | 2.02 (0.96, 4.26) | 2.51 (1.11, 5.67) | |
| Cigarette smoking | ||||||
| Never | 1.00 | 1.00 | 1.00 | |||
| Ever | 1.30 (0.49, 3.49) | 1.12 (0.24, 5.25) | 1.33 (0.43, 4.18) | |||
| Years of cigarette smoking | ||||||
| ≤15 | 1.00 | 1.00 | 1.00 | |||
| >15 | 1.83 (0.78, 4.32) | 1.26 (0.34, 4.66) | 1.99 (0.71, 5.52) | |||
| Alcohol use | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 1.53 (0.48, 4.88) | 1.78 (0.22, 14.4) | 1.32 (0.36, 4.83) | |||
| hs-CRP (mg/dL) | ||||||
| <2 | 1.00 | 1.00 | 1.00 | |||
| ≥2 | 0.86 (0.44, 1.68) | 0.82 (0.29, 2.38) | 0.92 (0.43, 1.95) | |||
| Systolic BP (mm Hg) | ||||||
| <120 | 1.00 | 1.00 | 1.00 | |||
| ≥120 | 1.36 (0.64, 2.87) | 0.74 (0.20, 2.72) | 1.68 (0.74,3.82) | |||
| Diastolic BP (mm Hg) | ||||||
| ≤80 | 1.00 | 1.00 | 1.00 | |||
| >80 | 1.64 (0.82, 3.28) | 2.97 (0.69, 5.61) | 1.30 (0.59, 2.87) | |||
| Glucose (mg/dL) | ||||||
| <85 | 1.00 | 1.00 | 1.00 | |||
| ≥85 | 1.56 (0.81, 3.00) | 2.17 (0.75, 6.27) | 1.19 (0.57, 2.50) | |||
| BMI (kg/m2) | ||||||
| <24 | 1.00 | 1.00 | 1.00 | |||
| ≥24 | 0.87 (0.45, 1.68) | 0.59 (0.20, 1.69) | 1.11 (0.53, 2.33) | |||
| Total cholesterol (mg/dL) | ||||||
| <160 | 1.00 | 1.00 | 1.00 | 1.00 | ||
| ≥160 | 2.51 (1.27, 4.96) | 2.47 (1.16, 5.27) | 3.20 (0.99, 10.3) | 1.84 (0.86, 3.95) | ||
| LDL-C (mg/dL) | ||||||
| <100 | 1.00 | 1.00 | 1.00 | |||
| ≥100 | 1.83 (0.93, 3.60) | 1.57 (0.55, 4.45) | 1.71 (0.79, 3.66) | |||
| HDL-C (mg/dL) | ||||||
| <50 | 1.00 | 1.00 | 1.00 | |||
| ≥50 | 0.78 (0.41, 1.50) | 0.94 (0.34, 2.63) | 0.75 (0.36, 1.58) | |||
| Triglycerides (mg/dL) | ||||||
| <130 | 1.00 | 1.00 | 1.00 | 1.00 | ||
| ≥130 | 2.54 (1.30, 4.98) | 1.10 (0.38, 3.20) | 3.11 (1.45, 6.66) | 3.39 (1.52, 7.57) | ||
| Framingham score | ||||||
| <3% | 1.00 | 1.00 | 1.00 | |||
| ≥3% | 5.68 (2.11, 15.3) | 3.34 (0.73, 15.2) | 5.74 (1.67, 19.7) | |||
| NRTIs use (mo) | ||||||
| ≤6 (n = 123) | 1.00 | 1.00 | 1.00 | |||
| 6.1–18 (n = 15) | 1.48 (0.47, 4.68) | 4.88 (1.08, 22.0) | 0.60 (0.13, 2.85) | |||
| >18 (n = 38) | 2.16 (1.01, 4.62) | 4.40 (1.38, 14.0) | 1.22 (0.51, 2.90) | |||
| NNRTIs use (mo) | ||||||
| ≤6 (n = 150) | 1.00 | 1.00 | 1.00 | |||
| 6.1–18 (n = 4) | 9.16 (0.95, 90.8) | 6.81 (0.63, 74.1) | 4.00 (0.54, 29.6) | |||
| >18 (n = 22) | 3.67 (1.46, 9.18) | 11.7 (3.68, 37.0) | 0.89 (0.28, 2.82) | |||
| PI use (mo) | ||||||
| ≤6 (n = 125) | 1.00 | 1.00 | 1.00 | |||
| 6.1–18 (n = 18) | 1.17 (0.39, 3.53) | not estimable | 1.71 (0.55, 5.26) | |||
| >18 (n = 33) | 2.85 (1.29, 6.32) | 4.68 (1.60, 13.7) | 1.42 (0.57, 3.55) | |||
| ART exposure (mo) | ||||||
| ≤6 (n = 96) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 6.1–18 (n = 23) | 0.88 (0.22, 3.47) | 0.71 (0.16, 3.23) | not estimable | not estimable | 1.04 (0.26, 4.14) | |
| >18 (n = 57) | 2.52 (1.24, 5.09) | 2.20 (1.01, 4.79) | 7.61 (1.67, 34.7) | 7.61 (1.67, 34.7) | 1.34 (0.62, 2.89) | |
HIV, human immunodeficiency virus; CD4, CD4 cell count; hs-CRP, high sensitivity C reactive protein; BP, blood pressure; glucose, fasting glucose; BMI, body mass index; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; Framingham score, Framingham risk score; NRTIs, nucleoside reverse transcriptase inhibitors; NNRTIs, nonnucleoside reverse transcriptase inhibitors; PIs, protease inhibitors; ART, antiretroviral therapy.
The final multiple logistic regression model indicated that a significant risk of the presence of coronary plaques was associated with previously described conventional risk factors, including age (adjusted OR: 3.11, 95%CI: 1.04, 9.30), male gender (adjusted OR: 4.23, 95% CI: 1.79, 10.0), and total cholesterol ≥160 mg/dL (adjusted OR: 2.47, 95% CI: 1.16, 5.27). The analysis also showed that both cocaine use for more than 15 years (adjusted OR: 2.67, 95% CI: 1.23, 5.83) and use of ART for more than 18 months (adjusted OR: 2.20, 95% CI: 1.01, 4.79) were independently associated with the presence of coronary plaques (Table 2).
Factors associated with the presence of noncalcified coronary plaques
By univariate logistic regression analyses, none of the traditional risk factors previously described was associated with the presence of noncalcified plaques. Among the nontraditional risk factors investigated, a higher HIV viral load and exposure to any ART (NNRTIs, NRTIs, or PIs) for more than 18 months were significantly associated with the presence of noncalcified plaques (Table 2).
The final logistic regression model indicated that only the use of any ART for more than 18 months (adjusted OR: 7.61, 95% CI: 1.67, 34.7) was independently associated with the presence of noncalcified coronary plaques (Table 2).
Factors associated with the presence of calcified coronary plaques
By univariate logistic regression analyses, traditional risk factors associated with the presence of calcified coronary plaques included male gender, triglycerides ≥130 mg/dL, and Framingham risk score 3 or more. The only nontraditional risk factor associated (marginally) with the presence of calcified coronary plaques was cocaine use for 15 years or more (Table 2).
The final multiple logistic regression model indicated that a significant risk of the presence of calcified plaques was associated with previously described conventional risk factors, including male gender (adjusted OR: 4.32, 95% CI: 1.60, 11.7) and triglycerides ≥130 mg/dL (adjusted OR: 3.39, 95% CI: 1.52, 7.57). The analysis also showed that, compared with no cocaine use, use of cocaine for more than 15 years (adjusted OR: 2.51, 95% CI: 1.11, 5.67) was also independently associated with the presence of calcified coronary plaques (Table 2).
Proportion of variation of the presence of coronary plaques explained by duration of cocaine use and duration of ART use
According to the PVE analysis, male gender, cocaine use (used for less than 15 years or used for 15 years or more), total cholesterol concentration (≥160 mg/dL), and use of ART (naïve or used for 6 months or less, used for more than 6 but 18 months or less, or used for more than 18 months) combined explained 20.9% of variation. Male gender, duration of cocaine use, total cholesterol, and duration of ART use explained about 5.6%, 4.7%, 4.1%, and 6.5%, respectively, of variation in the presence of coronary plaques, after adjusting for other covariates.
Discussion
Our findings demonstrate that the overall prevalence of coronary plaques in a population of HIV-infected African Americans was provocatively high—29.5% (52/176, 95% CI: 22.9%, 36.9%). Notably, since this study excluded those with hypertension, a major risk factor for CAD, and those older than 54 years, the prevalence rate in an “unselected” population of African Americans with HIV infection might be even higher. According to our observation, the prevalence rate of coronary plaques in those who were free of HIV infection and drug use and resided in socially and demographically similar neighborhoods was just 21%. Thus, this study highlights a potential impending epidemic of premature CAD in African Americans with HIV infection.
Our study found that short-term use (18 months or less) of ART was not associated with an elevated risk of coronary plaques. This finding is somewhat consistent with the SMART trial, which suggested that short-term use of ART reduced cardiovascular risk.16 Nevertheless, after controlling for traditional risk factors and cocaine use, our study revealed that long-term use of ART (for more than 18 months) was associated with a more than twofold increased risk. According to the PVE analysis, long-term use of ART may be more important than other factors to explain the presence of coronary plaques. The finding differs somewhat from the Data Collection on Adverse Events of Anti-HIV Drugs (DAD) study, which suggests that PIs and possible selected NRTIs, but not NNRTIs, are associated with an increased risk of myocardial infarction (MI).5 Similar to DAD, we found a linear trend suggesting a dose-response relationship effect of ART on the risk of the presence of coronary plaques.
This study suggests that the prolonged use of ART, including NRTIs, NNRTIs, or PIs, increases the risk of the presence of noncalcified, but not calcified, plaques. In particular, long-term use of any ART was associated with an eightfold increased risk of noncalcified coronary plaques. The precise mechanisms underlying the association between long-term ART use and noncalcified plaques remain unclear. Nevertheless, our data show that a higher HIV RNA level was associated by univariate analysis with the presence of noncalcified plaques (OR = 5.40, 95% CI: 1.10, 26.4), suggesting that HIV replication may play a role in promoting their development.
Noncalcified plaques are early-stage plaques in nature since early stages of atherosclerotic lesions are not associated with significant cell death and, therefore, are largely devoid of calcium.17 Nevertheless, according to the AHA classification, which is based on histologic features rather than functional significance, a large number of vulnerable plaques are predominantly noncalcified and nonstenotic and similar to type IV (atheroma) atherosclerotic lesions.18 The potential clinical significance of type IV lesions can be great, even though this advanced lesion may not cause much narrowing of the lumen.19
According to our data, approximately 30% of the noncalcified plaques had CT density values less than 50 HU, suggesting that these plaques may have a large lipid core and therefore may be more vulnerable to rupture. On the other hand, long-term cocaine use is associated with the presence of calcified plaques, not noncalcified plaques. Long-term cocaine use may cause continuing cell death, leading to calcification of the extracellular matrix within the intima.17 The identification of noncalcified plaques may be of importance since it has been reported that despite having significantly less coronary calcium, African Americans nevertheless have more CHD events (new-onset angina pectoris, MI, or death from CAD) than non-black subjects with similar risk factors.20–22 One possible explanation is that plaque composition, particularly the quantity of coronary calcium, varies with ethnicity, and atherosclerotic plaques in African Americans may be more susceptible to rupture than plaques in non-African American subjects.23 Long-term cocaine use has been implicated with significant coronary stenosis.6
We recognize several limitations to this study. First, the participants were not a random sample of those with HIV infection, and therefore the results may not be generalizable to other populations. Second, since a large majority of participants were cigarette smokers, the effects of cigarette smoking on coronary plaques could not be fully evaluated, either individually or combined. Third, the study is cross-sectional in nature and therefore causality could not be determined. Some potentially confounding factors, such as duration of time with HIV infection and socioeconomic status, were not available. Furthermore, since this study was performed in African Americans living in inner-city Baltimore, where cocaine use is often intertwined with other drug addictions, the effects of these drugs (or multiple-drug interactions) on CAD could not completely be controlled for by statistical analyses. Fourth, although both questionnaire and urine drug-testing were used to identify drug use, the quantity used may not be accurately estimated and drug use could be under-estimated. Fifth, although a synergistic effect of long-term cocaine use and use of ART was suggested (Fig. 4), our sample size probably did not give us sufficient power to detect a significant effect. A larger study will be needed to identify synergistic effects. Lastly, the study did not collect the data on inflammatory conditions (e.g., lupus, psoriasis, inflammatory bowel disease) although those with these conditions may be more likely to acquire CAD since coronary artery disease is a chronic inflammatory condition.
Despite its limitations, this study provides disturbing new evidence of the presence of early-stage CAD in cardiovascularly asymptomatic HIV-infected African Americans. The study also highlights the urgent need for an aggressive reduction of the risk for CAD in HIV-infected persons who are on ART (at least the HAART that was commonly prescribed at the time of this study). Since this study also suggests that long-term ART use and HIV replication might be associated with the risk of noncalcified plaques, an intensive lifestyle intervention to reduce traditional risk factors for CAD is ultimately vital to those who are on ART. Further studies should be conducted to validate this finding since noncalcified plaques may be vulnerable to rupture. This study also suggests that cocaine cessation is the single most effective strategy to prevent CAD in HIV-infected cocaine users.
Acknowledgments
The study was supported by grants from the National Institute on Drug Abuse, National Institutes of Health (NIH R01-DA 12777 and DA15020). We thank the study participants for their contributions.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Eugenin EA. Morgello S. Klotman ME, et al. Human immunodeficiency virus (HIV) infects human arterial smooth muscle cells in vivo and in vitro: Implications for the pathogenesis of HIV-mediated vascular disease. Am J Pathol. 2008;172:1100–1111. doi: 10.2353/ajpath.2008.070457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stein JH. Cardiovascular risks of antiretroviral therapy. N Engl J Med. 2007;356:1773–1775. doi: 10.1056/NEJMe078037. [DOI] [PubMed] [Google Scholar]
- 3.Bozzette SA. Ake CF. Tam HK. Chang SW. Louis TA. Cardiovascular and cerebrovascular events in patients treated for human immunodeficiency virus infection. N Engl J Med. 2003;348:702–710. doi: 10.1056/NEJMoa022048. [DOI] [PubMed] [Google Scholar]
- 4.The Data Collection on Adverse Events of Anti-HIV Drugs (DAD) Study Group. Combination antiretroviral therapy and the risk of myocardial infarction. N Engl J Med. 2003;349:1993–2004. doi: 10.1056/NEJMoa030218. [DOI] [PubMed] [Google Scholar]
- 5.The DAD Study Group. Class of antiretroviral drugs and the risk of myocardial infarction. N Engl J Med. 2007;356:1723–1735. doi: 10.1056/NEJMoa062744. [DOI] [PubMed] [Google Scholar]
- 6.Jericó C. Knobel H. Calvo N, et al. Subclinical carotid atherosclerosis in HIV-infected patients: Role of combination antiretroviral therapy. Stroke. 2006;37:812–817. doi: 10.1161/01.STR.0000204037.26797.7f. [DOI] [PubMed] [Google Scholar]
- 7.Sension M. Andrade Neto JL, et al. Improvement in lipid profiles in antiretroviral-experienced HIV-positive patients with hyperlipidemia after a switch to unboosted atazanavir. J Acquir Immune Defic Syndr. 2009;51:153–162. doi: 10.1097/QAI.0b013e3181a5701c. [DOI] [PubMed] [Google Scholar]
- 8.Currier JS. Kendall MA. Henry WK, et al. Progression of carotid artery intima-media thickening in HIV-infected and uninfected adults. AIDS. 2007;21:1137–1145. doi: 10.1097/QAD.0b013e32811ebf79. [DOI] [PubMed] [Google Scholar]
- 9.D:A:D Study Group. Sabin CA. Worm SW, et al. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: A multi-cohort collaboration. Lancet. 2008;371:1417–1426. doi: 10.1016/S0140-6736(08)60423-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaplan RC. Kingsley LA. Gange SJ, et al. Low CD4+ T-cell count as a major atherosclerosis risk factor in HIV-infected women and men. AIDS. 2008;22:1615–1624. doi: 10.1097/QAD.0b013e328300581d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai S. Fishman EK. Lai H, et al. Long-term cocaine use and antiretroviral therapy are associated with silent coronary artery disease in cardiovascularly asymptomatic African Americans with HIV infection. Clin Infect Dis. 2008;46:600–610. doi: 10.1086/526782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cerqueira MD. Weissman NJ. Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–542. doi: 10.1161/hc0402.102975. [DOI] [PubMed] [Google Scholar]
- 13.Hosmer DW. Lemeshow S. Applied Logisitc Regression. 2nd. New York: Wiley; 2000. [Google Scholar]
- 14.Wilson PWF. D'Agostino RB. Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 15.Mittlbock M. Schemper M. Explained variation for logistic regression. Stat Med. 1996;15:1987–1997. doi: 10.1002/(SICI)1097-0258(19961015)15:19<1987::AID-SIM318>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 16.The Strategies for Management of Antiretroviral Therapy (SMART) Study Group. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355:2283–2296. doi: 10.1056/NEJMoa062360. [DOI] [PubMed] [Google Scholar]
- 17.Burke AP. Kolodgie FD. Farb A. Virmani R. Pathogenesis and significance of calcification in coronary atherosclerosis. In: Virmani R, editor; Narula J, editor; Leon MB, editor; Willerson JT, editor. The Vulnerable Atherosclerotic Plaque: Strategies for Diagnosis and Management. Malden, MA: Blackwell; 2007. pp. 77–94. [Google Scholar]
- 18.Hausleiter J. Meyer T. Hadamitzky M. Kastrati A. Martinoff S. Schömig A. Prevalence of noncalcified coronary plaques by 64-slice computed tomography in patients with an intermediate risk for significant coronary artery disease. J Am Coll Cardiol. 2006;48:312–318. doi: 10.1016/j.jacc.2006.02.064. [DOI] [PubMed] [Google Scholar]
- 19.Stary HC. Chandler AB. Dinsmore RE, et al. A definition of advanced types of atherosclerosis lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Atherosclerosis, American Heart Association. Circulation. 1995;92:1355–1374. doi: 10.1161/01.cir.92.5.1355. [DOI] [PubMed] [Google Scholar]
- 20.Tang W. Detrano RC. Brezden OS, et al. Racial differences in coronary calcium prevalence among high risk adults. Am J Cardiol. 1995;75:1088–1091. doi: 10.1016/s0002-9149(99)80735-8. [DOI] [PubMed] [Google Scholar]
- 21.Detrano R. Wong N. Tang W, et al. Prognostic significance of cardiac cine fluoroscopy for coronary calcific deposits in asymptomatic high risk subjects. J Am Coll Cardiol. 1994;24:354–358. doi: 10.1016/0735-1097(94)90287-9. [DOI] [PubMed] [Google Scholar]
- 22.Doherty TM. Tang W. Detrano RC. Racial differences in the significance of coronary calcium in asymptomatic black and white subjects with coronary risk factors. J Am Coll Cardiol. 1999;34:787–794. doi: 10.1016/s0735-1097(99)00258-2. [DOI] [PubMed] [Google Scholar]
- 23.Doherty TM. Detrano RC. Mautner SL, et al. Coronary calcium: The good, the bad, and the uncertain. Am. Heart J. 1999;137:806–814. doi: 10.1016/s0002-8703(99)70403-5. [DOI] [PubMed] [Google Scholar]