Abstract
In 1856 Virchow proposed a triad of causes for venous thrombosis, postulating that stasis, changes in the vessel wall or changes in the blood could lead to thrombosis. We now know that abnormally high levels of some coagulation factors and defects in the natural anticoagulants contribute to thrombotic risk. Among these, factor V Leiden, which renders factor Va resistant to activated protein C, is the most prevalent with approximately 5% of the Caucasian population having this genetic alteration. These genetically controlled variants in coagulation factors work in concert with other risk factors, such as oral contraceptive use, to dramatically increase thrombotic risk. While these abnormalities in the blood coagulation proteins are associated with thrombotic disease propensity, they are less frequent contributors to thrombosis than age or cancer. Cancer increases thrombotic risk by producing tissue factor to initiate coagulation, by shedding procoagulant lipid microparticles or by impairing blood flow. Age is the strongest risk factor for thrombosis. Among possible reasons are fragility of the vessels potentially contributing to stasis, increased coagulation factor levels, impaired function of the venous valves, decreases in the efficacy of natural anticoagulants associated with the vessel wall, increased risk of immobilization and increased risk of severe infection.
Keywords: Venous thrombosis, venous valves, P-selectin, tissue factor, ischemia, obesity, sex hormones, stasis, microparticles
A. Introduction
Virchow's triad predicts that the causes of thrombosis are changes in blood coaguability, changes in the vessel wall or stasis (Figure 1). More recent studies have provided a mechanistic understanding for some of the processes that cause each of these alterations to contribute to thrombosis. A combination of genetically manipulated mouse models and human epidemiology have revealed that a variety of genetic risk factors can contribute to venous thrombosis, but the site of the thrombotic risk varies depending on the defect1,2.
Figure 1.
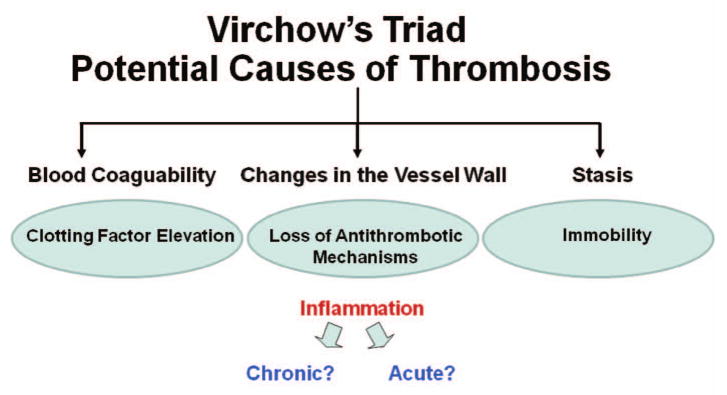
A modified version of Virchow's triad focusing on the findings that chronic low level inflammation has little impact on venous thrombosis (unlike arterial thrombosis), but that acute inflammation does increase venous thrombosis.
One of the major concepts involved in either hemostasis or thrombosis is that the processes are localized. Simply increasing coagulation enzyme concentrations with or without added negatively charged phospholipid vesicles leads to thrombin generation, but this thrombin generation is widespread, usually leading to disseminated intravascular coagulation rather than either hemostasis or thrombosis3,4.
A. Where does venous thrombosis begin and why?
Except in thrombosis associated with surgery, examination of the thrombus in the human veins seldom indicates evidence of injury5, raising the question of how venous thrombosis is initiated. Venous thrombosis is believed to begin at the venous valves1,6. These valves play a major role in helping with blood circulation in the legs. They are also areas where stasis and hypoxia may occur. Direct evidence from autopsy studies and phlebography have established the venous valvular sinus as a frequent location of thrombosis initiation5,7-9. This phenomenon has been attributed to stasis, one of the components of Virchow's triad. Contrast media lingers in valve sinuses taking an average of 27 min to clear post-venography10. Valvular sinus stasis has also been associated with hypoxia and increased hematocrit11, constituting a potentially hypercoagulable micro-environment. Furthermore, in animal models, oxygen tension drops very rapidly once blood flow is halted 11. Abnormalities in these valves as a contributor to thrombotic risk have not been studied extensively at the molecular level. In a recent preliminary study, several of the important vessel based antithrombotic proteins, including thrombomodulin and endothelial protein C receptor (EPCR), were shown to be regionally expressed on the valves12. Furthermore, the expression of these proteins showed considerable inter-individual variation. Since expression of these anticoagulant proteins is sensitive to the environment, either hypoxia or inflammation could lead to down regulation, possibly contributing to the initiation of thrombosis13-15. In addition, hypoxia can lead to up-regulation of procoagulant activity including tissue factor on endothelium15-17. Further studies are needed to explore the possibility that changes in the ratio of procoagulant to anticoagulant properties of the valves make a contribution to venous thrombotic risk.
A. The role of blood cells versus vascular contribution to venous thrombosis
In addition to modulating the pro and anticoagulant properties of the endothelium, hypoxia also up regulates the expression of P-selectin on endothelium leading to the recruitment of leukocytes or leukocyte microparticles containing tissue factor which can serve as the nidus for initiation of the thrombotic response18,19 (Figure 2). Microparticles bearing tissue factor appear to play a role in thrombus formation20,21. This contrasts to the conventional notion that initiation of coagulation involves exposure of tissue factor on cells surrounding the vessel other than endothelium. This conventional model is attractive because as soon as the vessel is compromised blood comes in contact with extravascular tissue factor sealing the lesion22.
Figure 2. A model venous valve involvment in the initiation of thrombosis.
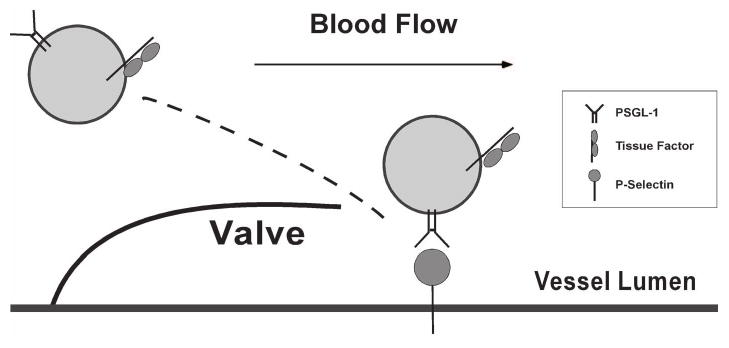
The region just downstream of the valve is prone to hypoxia leading to endothelial cell activation. This upregulates adhesion molecules like P-selectin, which in turn can bind to leukocytes or leukocyte microparticles. Since the microparticles contain tissue factor, the interaction with the activated endothelium results in concentrating tissue factor to trigger coagulation that is rapid enough to result in thrombus formation.
There is general agreement that venous thrombosis involves tissue factor as the initiator of the coagulation response. The source of the tissue factor remains somewhat controversial in part because of the model systems used to induce the thrombus in animal models. Most of these involve some type of overt vessel damage. There are clear examples of model systems in which blood borne tissue factor, probably associated with blood cells or microparticles derived from the blood cells, probably leukocytes, is involved in the genesis of the thrombus. One of the first examples where this was shown involved passing human native blood over glass plates covered in collagen. Fibrin clots developed over the slides and this thrombus formation was blocked by antibodies to tissue factor 21.
Under arterial and venous flow conditions, thrombus also appears to involve P-selectin, an adhesion molecule that can contribute to cell-cell interactions with cells expressing PSGL-1, a major ligand for P-selectin. Under arterial flow conditions, thrombus formation was blocked by inhibitors of P-selectin23. Tissue factor and P-selectin appear to both be necessary for thrombus formation and they appear to both be resident on microparticles derived from monocytes, as indicated by the presence of monocyte proteins on the microparticles19,20. In a baboon venous stasis model of thrombosis, P-selectin inhibition was found to prevent thrombus development and facilitate clot resolution24,25. In most of these models, it is difficult to determine whether the tissue factor-P-selectin involvement in thrombus formation is due to cellular interactions or microparticles26.
It is possible that the interference with thrombosis caused by selectin inhibition is due to inhibiting platelet function or the interaction of platelets with leukocytes and/or leukocyte derived particles in the thrombus. A venous clot is composed of two regions. The red cell rich fibrin clot that appears to lie adjacent to the apparently intact endothelium and lines of platelet rich white thrombus, sometimes called the lines of Zahn, further inside the clot that separate regions of red thrombus5,27. It would seem possible that disrupting the white thrombus areas might render the clot more fragile and/or more susceptible to clot lysis.
A different view of tissue factor involvement in venous thrombosis comes from studies of mice where tissue factor is selectively dramatically reduced in blood cells28. In these mice, the blood borne tissue factor contributed little to stasis induced venous thrombosis, indicating that the tissue factor is derived from the vessel wall.
Obviously, these two models seem to be at odds with each other raising questions about why this may be the case. Perhaps the major problem is that each of the models involves vessel injury but the nature and extent of the injury varies. As mentioned previously, except in thrombosis associated with surgery, examination of the human thrombus in the vein seldom indicates evidence of vein injury in the region5 and thus most human deep vein thrombosis differs from animal models where injury of the vein, even if only by ligation, is usually an initiating event. By injuring the vein, procoagulant membrane surfaces are exposed and adhesive molecules are made available so that leukocytes and platelets will be recruited to the injury site.
A. Additional potential mechanisms for stasis induced venous thrombosis
Many of the anticoagulant pathways are triggered by endothelial cell surface components including thrombomodulin, EPCR, tissue factor pathway inhibitor and heparin like proteoglycans. EPCR and thrombin bound to thrombomodulin initiate the protein C pathway responsible for the inactivation of critical cofactors Va and VIIIa, tissue factor pathway inhibitor blocks tissue factor initiated coagulation and heparin like protoglycans stimulate antithrombin's inhibitor activity toward coagulation enzymes like thrombin, reviewed in29. Although the concentration of these proteins does vary somewhat among vascular beds, a major difference is determined by the ratio of endothelial cell surface to blood volume30. Therefore, as the blood moves from the larger vessels into the microcirculation, the efficacy of the natural anticoagulants increases dramatically31,32, in large part because of the vastly greater endothelial cell area exposed to blood in the capillaries compared to the major arteries or veins. Presumably, by stasis increasing the residence time in the large vessels, the natural mechanisms for controlling coagulation through interaction with the anticoagulants in the microcirculation are impaired and the propensity to develop thrombi increases with residence time of the blood in the large vessels. This model would be consistent with the known importance of these vascular anticoagulants in preventing thrombosis and the observation that stasis is a major contributor to thrombotic risk33,34.
A. Changes in blood coaguability
Increased levels of coagulation factors, particularly factor VIII, von Willebrand factor, factor VII and prothrombin are associated with an increased risk of thrombosis, reviewed in2,35. The increased risk of thrombosis with the elevation in factor VIII may be due to its inherent instability following activation and hence the need for replenishment to obtain a stable thrombus. In the case of prothrombin, in addition to the potential increase in thrombin generation, prothrombin is also an effective inhibitor of activated protein C anticoagulant activity36 and hence elevation in prothrombin may function as a double edged sword by directly enhancing thrombin production and by decreasing inhibition of the prothrombin activation.
In thrombophilic families, deficiencies of the main coagulation inhibitors occur in 15%, prothrombin 20210 A occurs in 20% and factor V Leiden occurs in 40-60%37. Among the most common changes in blood that increase blood coaguability are defects in natural anticoagulants pathways. There are three major natural anticoagulant pathways; the heparin-antithrombin pathway, the protein C anticoagulant pathway and the tissue factor inhibitor pathway. Of these, defects in antithrombin, and each of the components of the protein C anticoagulant pathway, protein C37,38, protein S39, thrombomodulin40 and possibly EPCR41, are associated with increased risks of thrombotic disease in humans. Tissue factor pathway inhibitor defects in human disease remain uncertain, in large part because the majority of the protein is associated with the endothelium and as a result, measuring circulating TFPI levels may not be informative. For all three systems, one or more components of the pathway function at the vessel wall and hence may be sensitive to vascular diseases including inflammation and hypoxia.42-44
A. The influence of aging on thrombosis risk
The risk of thrombosis increases dramatically with aging (Figure 3). The basis for this increase in thrombotic risk with aging remains uncertain. From a population perspective, all of the following increase with age: there are increases in procoagulant levels with age without concomitant increases in natural anticoagulants like protein C45, there is an increase in body mass with age46, activity decreases often with extended periods of immobilization due to illness, the frequency of acute serious infections rises, frailty increases and the number of co-morbidities tends to mount with age47. Surprisingly, although exercise decreases the risk of venous thrombosis slightly in younger individuals, exercise increases this thrombotic risk in the elderly48. In addition to the dramatically increased risk of venous thrombosis associated with age, there are also increases in markers of intravascular coagulation such as D-dimer and prothrombin fragment 1-245 indicating that there is a persistent hypercoaguable state. At present, we do not know if this is due primarily to changes in the vessel wall, perhaps the valves, or the blood. The extent of changes in the circulating blood cells as opposed to the plasma components that might contribute to the increased coagulation is also not known. A better understanding of the basis for the age dependent hypercoaguability might aid in more effective therapies. This is especially important since the bleeding risk on oral anticoagulants rises sharpely in the elderly49, making patient management more complex.
Figure 3. The relationship between age and venous thrombotic risk.
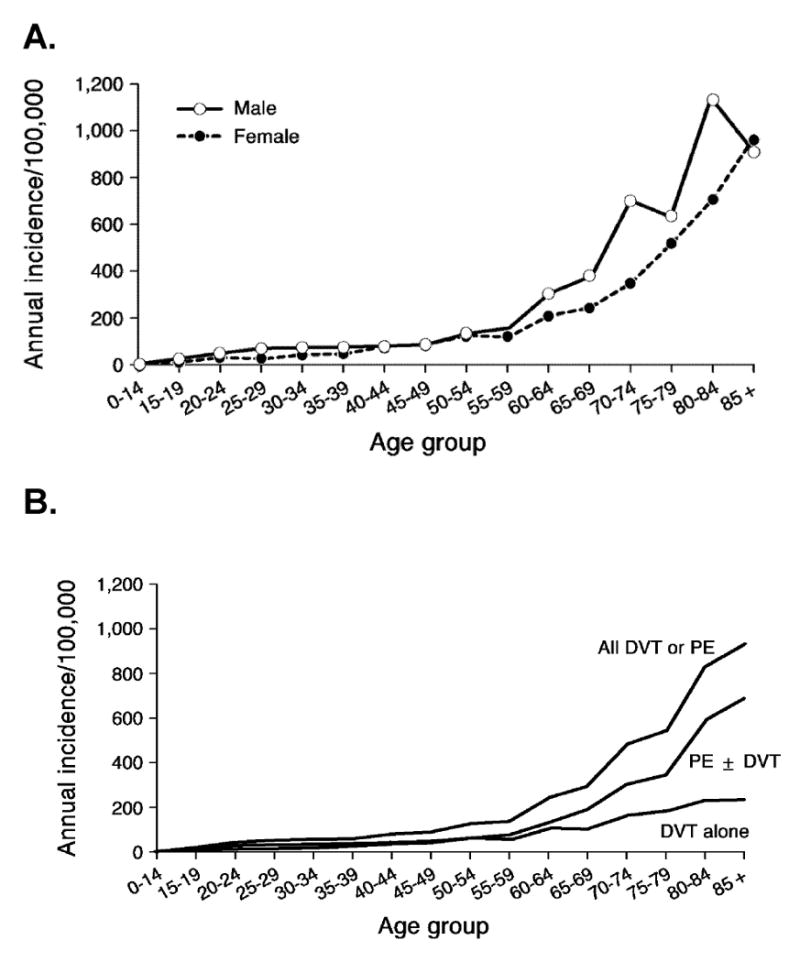
Figure 3 a: The risk of deep vein thrombosis (DVT) rises markedy with increasing age in both men and women. Figure 3b: The risk of pulmonary embolism (PE) also rises with increasing age. (Reproduced by kind permission of American Medical Association from Silverstein et al: Trends in the incidence of deep vein thrombosis and pulmonary embolism. A 25-year population-based study. Arch Intern Med, Mar 23, 158:585-593, copyright © (1998) American Medical Association. All rights reserved.)
Arterial thrombotic risk rises with age in part, presumably, because of increased systemic inflammation such as an increase in IL-6 or C reactive protein50 but these modest constitutive changes in inflammation appear to have little influence on venous thrombotic risk51. However, acute infections do increase risk markedly of both venous thrombosis and pulmonary embolism52. Whether the increases in risk are attributable to the acute inflammatory response, increased immobilization or both remains to be determined.
A. Venous thrombosis
A single factor abnormality is seldom enough to cause venous thrombosis leading to “the multiple hit hypothesis.” Although based on human population studies, it is clear that coagulation factor or natural anticoagulant factor levels influence the risk of venous thrombosis, it is equally clear that other factors contribute to thrombotic risk. For example, in some families with protein C deficiency, the incidence of thrombosis is low whereas in other families it is high. In one extended family, the high and low frequencies of thrombosis segregates in certain branches of the family with the protein C deficiency53 suggesting that there is a strong synergy between multiple factors. Other examples are that while obesity and oral contraceptives independently increase the risk of venous thrombosis, the two together increase the risk synergistically54. After correcting for age and sex, obesity >30 Kg/m2 increased the risk of thrombosis two-fold54. Obese individuals have increased levels of coagulation factor VIII and IX possibly contributing to the increased risk of thrombosis, but the risk associated with obesity remains even after adjustment for clotting factor levels. Oral contraceptives increase the risk of thrombosis approximately fourfold, and this risk increases to approximately seven-fold for patients with factor V Leiden and 35-fold for patients with factor V Leiden who use oral contraceptives37. Likewise, Factor V Leiden and hetozygous protein C deficiency have similar cooperative influences on the risk of thrombosis and this risk remains elevated in the elderly37. All of this suggests that there is a thrombosis threshold where the propensity to generate thrombin is not adequately regulated by antithrombotic mechanisms.
A. Pregnancy
Like oral contraceptives55, pregnancy carries an increased risk of developing venous thrombosis56 that is increased still further in patients with thrombophilia. This increased risk is present in all trimesters of pregnancy and in the post partum period. Potential contributing factors might be disturbed blood flow and hormonal changes56.
A. Cancer
Cancer is a major risk factor for venous thrombosis, increasing the risk about 6-10 fold57-60. Patients with cancer contribute approximately 20% of the new cases of venous thrombosis occuring in the community61. Tumors shed membrane particles that contain procoagulant activity62 including tissue factor63 and membrane lipids that propogate the coagulation response. Adhesion molecules on the shed particles can help to concentrate the particles at sites where the appropriate ligands for the receptors are present, for instance P-selectin in ischemic areas. By concentrating the procoagulant and procoagulant lipid particles, it is possible to develop a localized thrombus rather than DIC, although DIC is found in some cancer patients. In addition, some tumors may compress one or move veins contributing to stasis.
A. Lupus Anticoagulants
Paradoxically the presence of lupus anticoagulants in patients is associated with an increased risk of thrombosis despite the fact that these lupus anticoagulant antibodies increase coagulation times in vitro. There are two major mechanisms that might contribute to the thrombotic risk. The antibodies bind to the platelets and endothelium possibly eliciting an inflammatory response64,65. These antibodies also lead to complement activation which appears to contribute to fetal loss66. These inflammatory contributions may help to explain why some patients with lupus anticoagulants have increased risks of arterial and/or venous thrombosis. On the venous side, one frequently observed candidate is inhibition of the protein C anticoagulant pathway67-70. In addition, antibodies against thrombomodulin are often found in this patient group and in patients with idiopathic thrombosis,71 potentially leading to impairment of the protein C anticoagulant pathway.
A. Post operative thrombosis
Post operative thrombosis is a complication of surgery especially knee, hip and cancer surgery61,72. In the case of knee and hip surgery, damage to the veins in combination with stasis are thought to be major contributing factors72. In addition, materials released into the blood stream from the surgical sites can augment coagulation. In the case of cancer surgeries, candidates for contributing to thrombosis include the release of tumor procoagulants, host inflammatory responses and responses to chemotherapeutics.61
A. Conclusion
While epidemiology has identified factors which predispose to venous thrombotic risk, we still lack fundamental knowledge of the basis for the initiation of thrombosis, how exactly the valves are involved in the process and what specific factors are altered with advancing age that contribute so markedly to thrombotic risk. Given the increased risk of major bleeding in the elderly on oral anticoagulants, a better understanding of the basis for the increased risk of thrombosis in the elderly could provide information essential to the design of safer antithrombotics.
A. Research Agenda
Prediction of thrombotic risk in the elderly
Underlying mechanisms of increasing thrombotic risk with age
Basis for increased bleeding risk on oral anticoagulants with age
The role of the venous valves in thrombus initiation
Establishing better animal models of venous thrombosis
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Aird WC. Vascular bed-specific thrombosis. J Thromb Haemost. 2007;5:283–291. doi: 10.1111/j.1538-7836.2007.02515.x. [DOI] [PubMed] [Google Scholar]
- 2.Lane DA, Grant PJ. Role of hemostatic gene polymorphisms in venous and arterial thrombotic disease. Blood. 2000;95:1517–1532. [PubMed] [Google Scholar]
- 3.Giles AR, Mann KG, Nesheim ME. A combination of factor Xa and phosphatidylcholine-phosphatidylserine vesicles bypasses factor VIII in vivo. Br J Haematol. 1988;69:491–497. doi: 10.1111/j.1365-2141.1988.tb02405.x. [DOI] [PubMed] [Google Scholar]
- 4.Taylor FB, Jr, He SE, Chang ACK, et al. Infusion of phospholipid vesicles amplifies the local thrombotic response to TNF and anti-protein C into a consumptive response. Thromb Haemost. 1996;75:578–584. [PubMed] [Google Scholar]
- 5.Sevitt S. The structure and growth of valve-pocket thrombi in femoral veins. J Clin Pathol. 1974;27:517–528. doi: 10.1136/jcp.27.7.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Friedman SA. Peripheral Venous Disease. In: Beers MH, Berkow R, editors. The Merck Manual of Geriatrics. 3rd. Whitehouse Station, NJ: Merck Research Laboratories; 2000. pp. 923–932. [Google Scholar]
- 7.Paterson JC, McLachlin J. Precipitating factors in venous thrombosis. Surg Gynecol Obstet. 1954;98:96–102. [PubMed] [Google Scholar]
- 8.Gottlob M, May R. Part III. Pathologic Venous Valves. In: Gottlob R, May R, editors. Venous Valves: Morphology, Function, Radiology, Surgery. New York, NY: Springer-Verlag; 1986. pp. 82–92. [Google Scholar]
- 9.Lund FL, Diener L, Ericsson JLE. Postmortem intraosseous phlebography as an aid in studies of venous thromboembolism: with application on a geriatric clientele. Angiology. 1969;20:155–176. doi: 10.1177/000331976902000306. [DOI] [PubMed] [Google Scholar]
- 10.McLachlin AD, McLachlin JA, Jory TA, Rawling EG. Venous stasis in the lower extremities. Ann Surg. 1960;152:678–683. doi: 10.1097/00000658-196010000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamer JD, Malone PC, Silver IA. The PO2 in venous valve pockets: its possible bearing on thrombogenesis. Br J Surg. 1981;68:166–170. doi: 10.1002/bjs.1800680308. [DOI] [PubMed] [Google Scholar]
- 12.Brooks E, Wadsworth M, Taatjes D, et al. Valves of the deep venous system: The overlooked risk factor. 110. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esmon CT. Inflammation and the activated protein C anticoagulant pathway. Sem Thromb Hemost. 2006;32(Suppl 1):49–60. doi: 10.1055/s-2006-939554. [DOI] [PubMed] [Google Scholar]
- 14.Dufourcq P, Seigneur M, Pruvost A, et al. Membrane thrombomodulin levels are decreased during hypoxia and restored by cAMP and IBMX. Thromb Res. 1994;77:305–310. doi: 10.1016/0049-3848(95)91617-t. [DOI] [PubMed] [Google Scholar]
- 15.Ogawa S, Gerlach H, Esposito C, Pasagian-Macaulay A, Brett J, Stern D. Hypoxia modulates the barrier and coagulant function of cultured bovine endothelium: increased monolayer permeability and induction of procoagulant properties. J Clin Invest. 1990;85:1090–1098. doi: 10.1172/JCI114540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shreeniwas R, Ogawa S, Cozzolino F, et al. Macrovascular and microvascular endothelium during long-term hypoxia: Alterations in cell growth, monolayer permeability, and cell surface coagulant properties. Journal of Cellular Physiology. 1991;146:8–17. doi: 10.1002/jcp.1041460103. [DOI] [PubMed] [Google Scholar]
- 17.Yan SF, Mackman N, Kisiel W, Stern DM, Pinsky DJ. Hypoxia/hypoxemia-induced activation of the procoagulant pathways and the pathogenesis of ischemia-associated thrombosis. Arterioscler Thromb Vasc Biol. 1999;19:2029–2035. doi: 10.1161/01.atv.19.9.2029. [DOI] [PubMed] [Google Scholar]
- 18.Closse C, Seigneur M, Renard M, et al. Influence of hypoxia and hypoxia-reoxygenation on endothelial P-selectin expression. Thromb Res. 1996;85:159–164. doi: 10.1016/s0049-3848(96)00233-2. [DOI] [PubMed] [Google Scholar]
- 19.Myers DD, Hawley AE, Farris DM, et al. P-selectin and leukocyte microparticles are associated with venous thrombogenesis. J Vasc Surg. 2003;38:1075–1089. doi: 10.1016/s0741-5214(03)01033-4. [DOI] [PubMed] [Google Scholar]
- 20.Falati S, Liu Q, Gross P, et al. Accumulation of tissue factor into developing thrombi in vivo is dependent upon microparticle P-selectin glycoprotein 1 and platelet P-selectin. J Exp Med. 2003;197:1585–1598. doi: 10.1084/jem.20021868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Giesen PLA, Rauch U, Bohrmann B, et al. Blood-borne tissue factor: another view of thrombosis. Proc Natl Acad Sci (USA) 1999;96:2311–2315. doi: 10.1073/pnas.96.5.2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Drake TA, Morrissey JH, Edgington TS. Selective cellular expression of tissue factor in human tissues: Implications for disorders of hemostasis and thrombosis. Am J Pathol. 1989;134:1087–1097. [PMC free article] [PubMed] [Google Scholar]
- 23.Li R, Riordan F, Hu GF. Nuclear translocation of human angiogenin in cultured human umbilical artery endothelial cells is microtubule and lysosome independent. Biochem Biophys Res Commun. 1997;238:305–312. doi: 10.1006/bbrc.1997.7290. [DOI] [PubMed] [Google Scholar]
- 24.Myers DD, Jr, Rectenwald JE, Bedard PW, et al. Decreased venous thrombosis with an oral inhibitor of P selectin. J Vasc Surg. 2005;42:329–336. doi: 10.1016/j.jvs.2005.04.045. [DOI] [PubMed] [Google Scholar]
- 25.Wakefield TW, Strieter RM, Schaub R, et al. Venous thrombosis prophylaxis by inflammatory inhibition without anticoagulation therapy. J Vasc Surg. 2000;31:309–324. doi: 10.1016/s0741-5214(00)90162-9. [DOI] [PubMed] [Google Scholar]
- 26.Yamauchi T, Umeda F, Inoguchi T, Nawata H. Antithrombin III stimulates prostacyclin production by cultured aortic endothelial cells. Biochem Biophys Res Commun. 1989;163:1404–1411. doi: 10.1016/0006-291x(89)91135-2. [DOI] [PubMed] [Google Scholar]
- 27.Paterson JC, McLachlin J. Precipitating factors in venous thrombosis. Surg Gynec Obstet. 1954;98:96–102. [PubMed] [Google Scholar]
- 28.Day SM, Reeve JL, Pedersen B, et al. Macrovascular thrombosis is driven by tissue factor derived primarily from the blood vessel wall. Blood. 2005;105:192–198. doi: 10.1182/blood-2004-06-2225. [DOI] [PubMed] [Google Scholar]
- 29.Esmon CT. Blood coagulation. In: Nathan DG, Orkin SH, Ginsburg D, Look AT, editors. Nathan and Oski's Hematology of Infancy and Childhood. 6th. Vol. 2. Philadelphia, PA: W.B. Saunders Company; 2003. pp. 1475–1496. [Google Scholar]
- 30.Busch C, Cancilla P, DeBault L, Goldsmith J, Owen W. Use of endothelium cultured on microcarriers as a model for the microcirculation. Lab Invest. 1982;47:498–504. [PubMed] [Google Scholar]
- 31.Esmon CT, Owen WG. Identification of an endothelial cell cofactor for thrombin-catalyzed activation of protein C. Proc Natl Acad Sci (USA) 1981;78:2249–2252. doi: 10.1073/pnas.78.4.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Esmon CT. The roles of protein C and thrombomodulin in the regulation of blood coagulation. J Biol Chem. 1989;264:4743–4746. [PubMed] [Google Scholar]
- 33.Lane DA, Mannucci PM, Bauer KA, et al. Inherited thrombophilia: Part 1. Thromb Haemost. 1996;76:651–662. [PubMed] [Google Scholar]
- 34.Lane DA, Mannucci PM, Bauer KA, et al. Inherited thrombophilia: Part 2. Thromb Haemost. 1996;76:824–834. [PubMed] [Google Scholar]
- 35.Bertina RM. Elevated clotting factor levels and venous thrombosis. Pathophysiol Haemost Thromb. 2004;33:399–400. doi: 10.1159/000083835. [DOI] [PubMed] [Google Scholar]
- 36.Smirnov MD, Safa O, Esmon NL, Esmon CT. Inhibition of activated protein C anticoagulant activity by prothrombin. Blood. 1999;94:3839–3846. [PubMed] [Google Scholar]
- 37.Rosendaal FR. Venous thrombosis: a multicausal disease. Lancet. 2009;353:1167–1173. doi: 10.1016/s0140-6736(98)10266-0. [DOI] [PubMed] [Google Scholar]
- 38.Esmon CT, Schwarz HP. An update on clinical and basic aspects of the protein C anticoagulant pathway. Trends Cardiovasc Med. 1995;5:141–148. doi: 10.1016/1050-1738(95)00054-D. [DOI] [PubMed] [Google Scholar]
- 39.Schwarz HP, Fischer M, Hopmeier P, Batard MA, Griffin JH. Plasma protein S deficiency in familial thrombotic disease. Blood. 1984;64:1297–1300. [PubMed] [Google Scholar]
- 40.Kunz G, Ireland HA, Stubbs PJ, Kahan M, Coulton GC, Lane DA. Identification and characterization of a thrombomodulin gene mutation coding for an elongated protein with reduced expression in a kindred with myocardial infarction. Blood. 2000;95:569–576. [PubMed] [Google Scholar]
- 41.Biguzzi E, Merati G, Liaw PCY, et al. A 23bp insertion in the endothelial protein C receptor (EPCR) gene impairs EPCR function. Thromb Haemost. 2001;86:945–948. [PubMed] [Google Scholar]
- 42.Faust SN, Levin M, Harrison OB, et al. Dysfunction of endothelial protein C activation in severe meningococcal sepsis. New Engl J Med. 2001;345:408–416. doi: 10.1056/NEJM200108093450603. [DOI] [PubMed] [Google Scholar]
- 43.Laszik ZG, Zhou XJ, Ferrell GL, Silva FG, Esmon CT. Down-regulation of endothelial expression of endothelial cell protein C receptor and thrombomodulin in coronary atherosclerosis. Am J Pathol. 2001;159:797–802. doi: 10.1016/S0002-9440(10)61753-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mertens G, Cassiman JJ, Van den Berghe H, Vermylen J, David G. Cell surface heparin sulfate proteoglycans from human vascular endothelial cells. J Biol Chem. 1992;267:20435–20443. [PubMed] [Google Scholar]
- 45.Lowe GDO, Rumley A, Woodward M, et al. Epidemiology of coagulation factors, inhibitors and activation markers: The Third Glasgow MONICA Survey I. Illustrative reference ranges by age, sex and hormone use. Br J Haematol. 1997;97:775–784. doi: 10.1046/j.1365-2141.1997.1222936.x. [DOI] [PubMed] [Google Scholar]
- 46.Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among U.S. adults. Obesity (Silver Spring) 2007;15:216–224. doi: 10.1038/oby.2007.505. [DOI] [PubMed] [Google Scholar]
- 47.Silverstein RL, Bauer KA, Cushman M, Esmon CT, Ershler WB, Tracy RP. Venous thrombosis in the elderly: more questions than anwers. Blood. 2007;110:3097–3101. doi: 10.1182/blood-2007-06-096545. [DOI] [PubMed] [Google Scholar]
- 48.van Stralen KJ, Doggen CJM, Lumley T, et al. The relationship between exercise and risk of venous thrombosis in elderly people. JAGS. 2008;56:517–522. doi: 10.1111/j.1532-5415.2007.01588.x. [DOI] [PubMed] [Google Scholar]
- 49.Torn M, Bollen WLEM, van der Meer FJM, van der Wall EE, Rosendaal FR. Risks of oral anticoagulant therapy with increasing age. Arch Intern Med. 2005;165:1527–1532. doi: 10.1001/archinte.165.13.1527. [DOI] [PubMed] [Google Scholar]
- 50.Rosendaal FR, Van Hylckama Vlieg A, Doggen CJM. Venous thrombosis in the elderly. J Thromb Haemost. 2007;5(Suppl 1):310–317. doi: 10.1111/j.1538-7836.2007.02489.x. [DOI] [PubMed] [Google Scholar]
- 51.Tsai AW, Cushman M, Rosamond WD, et al. Coagulation factors, inflammation markers, and venous thromboembolism: The Longitudinal Investigation of Thromboembolism Etiology (LITE) Am J Med. 2002;113:636–642. doi: 10.1016/s0002-9343(02)01345-1. [DOI] [PubMed] [Google Scholar]
- 52.Smeeth L, Cook C, Thomas S, Hall AJ, Hubbard R, Vallance P. Risk of deep vein thrombosis and pulmonary embolism after acute infection in a community setting. Lancet. 2006;367:1075–1079. doi: 10.1016/S0140-6736(06)68474-2. [DOI] [PubMed] [Google Scholar]
- 53.Bovill EG, Bauer KA, Dickerman JD, Callas P, West B. The clinical spectrum of heterozygous protein C deficiency in a large New England kindred. Blood. 1989;73:712–717. [PubMed] [Google Scholar]
- 54.Abdollahi M, Cushman M, Rosendaal FR. Obesity: risk of venous thrombosis and the interaction with coagulation factor levels and oral contraceptive use. Thromb Haemost. 2003;89:493–498. [PubMed] [Google Scholar]
- 55.Sidney S, Petitti DB, Soff GA, Cundiff DL, Tolan KK, Quesenberry CP., Jr Venous thromboembolic disease in users of low-estrogen combined estrogen-progestin oral contraceptives. Contraception. 2004;70:3–10. doi: 10.1016/j.contraception.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 56.Lim W, Eikelboom JW, Ginsberg JS. Inherited thrombophilia and pregnancy associated venous thromboembolism. BMJ. 2007;334:1318–1321. doi: 10.1136/bmj.39205.484572.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bick RL. Cancer-associated thrombosis. New Engl J Med. 2003;349:109–111. doi: 10.1056/NEJMp030086. [DOI] [PubMed] [Google Scholar]
- 58.Kakkar AK, Levine M, Pinedo HM, Wolff R, Wong J. Venous thrombosis in cancer patients: Insights from the FRONTLINE survey. The Oncologist. 2003;8:381–388. doi: 10.1634/theoncologist.8-4-381. [DOI] [PubMed] [Google Scholar]
- 59.Horton J. Venous thrombotic events in cancer: The bottom line. Cancer Control. 2005;12(Suppl 1):31–37. doi: 10.1177/1073274805012003S06. [DOI] [PubMed] [Google Scholar]
- 60.Piccioli A, Prandoni P, Ewenstein BM, Goldhaber SZ. Cancer and venous thromboembolism. Am Heart J. 1996;132:850–855. doi: 10.1016/s0002-8703(96)90321-x. [DOI] [PubMed] [Google Scholar]
- 61.López JA, Kearon C, Lee AYY. Deep venous thrombosis. Hematology Am Soc Hematol Educ Program Book. 2004:439–456. doi: 10.1182/asheducation-2004.1.439. [DOI] [PubMed] [Google Scholar]
- 62.Dvorak HF, Quay SC, Orenstein NS, et al. Tumor shedding and coagulation. 1981;212:923–924. doi: 10.1126/science.7195067. [DOI] [PubMed] [Google Scholar]
- 63.Rao LV. Tissue factor as a tumor procoagulant. Cancer Metastasis Rev. 1992;11:249–266. doi: 10.1007/BF01307181. [DOI] [PubMed] [Google Scholar]
- 64.de Groot PG, Derksen RHWM. Pathophysiology of the antiphospholipid syndrome. J Thromb Haemost. 2005;3:1854–1860. doi: 10.1111/j.1538-7836.2005.01359.x. [DOI] [PubMed] [Google Scholar]
- 65.Del Papa N, Sala GA, Buccellati C, et al. Endothelial cells as target for antiphospholipid antibodies: Human polyclonal and monoclonal anti-β2-glycoprotein I antibodies react in vitro with endothelial cells through adherent β2-glycoprotein I and induce endothelial activation. Arthritis Rheum. 1997;40:551–561. doi: 10.1002/art.1780400322. [DOI] [PubMed] [Google Scholar]
- 66.Holers VM, Girardi G, Mo L, et al. Complement C3 activation is required for antiphospholipid antibody-induced fetal loss. J Exp Med. 2002;195:211–220. doi: 10.1084/jem.200116116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Atsumi T, Khamashta MA, Amengual O, et al. Binding of anticardiolipin antibodies to protein C via β2-glycoprotein I (β2-GPI): a possible mechanism in the inhibitory effect of antiphospholipid antibodies on the protein C system. Clin Exp Immunol. 1998;112:325–333. doi: 10.1046/j.1365-2249.1998.00582.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Galli M, Ruggeri L, Barbui T. Differential effects of anti-β-glycoprotein I and antiprothrombin antibodies on the anticoagulant activity of activated protein C. Blood. 1998;91:1999–2004. [PubMed] [Google Scholar]
- 69.Smirnov MD, Triplett DT, Comp PC, Esmon NL, Esmon CT. On the role of phosphatidylethanolamine in the inhibition of activated protein C activity by antiphospholipid antibodies. J Clin Invest. 1995;95:309–316. doi: 10.1172/JCI117657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Esmon NL, Safa O, Smirnov MD, Esmon CT. Antiphospholipid antibodies and the protein C pathway. Journal of Autoimmunity. 2000;15:221–225. doi: 10.1006/jaut.2000.0407. [DOI] [PubMed] [Google Scholar]
- 71.Carson CW, Comp PC, Esmon NL, Rezaie AR, Esmon CT. Antibodies to thrombomodulin are found in patients with lupus anticoagulant and unexplained thrombosis. J Rheumatol. 2000;27:384–390. [PubMed] [Google Scholar]
- 72.Weitz JI, Hirsh J. Overview of new anticoagulant drugs. In: Sasahara AA, Loscalzo J, editors. New Therapeutic Agents in Thrombosis and Thrombolysis. 2nd. New York, NY: Marcel Dekker, Inc.; 2003. pp. 61–74. [Google Scholar]


